Abstract
Objective
This systematic review examines the medical, psychological and educational literature for training in practising leadership of a team leader in emergencies. The objectives of this paper are (1) describe how literature addresses operational training in practising leadership for the emergency medical team-leader (2) enhance understanding of leadership training in the medical environment.
Background
Worldwide, medical supervisors find it difficult to get students to rise to the occasion as leaders of emergency teams. It appears that many residents feel unprepared to adopt the role as a leader in emergencies.
Method
A systematic review was conducted (May–December 2016) in accordance with the PRISMA 2009 Checklist. A literature search was conducted against a set of inclusion criteria. Databases searched included PubMed, Psycinfo (via Ovid), and ERIC.
Results
27 articles covering the period 1986–2016 were analysed. Four sources of data were identified: Intervention studies practising leadership, intervention studies on simulation and leadership assessment, observation studies assessing leadership, interview/survey studies about the need for leadership training. No workable training in practising leadership in emergencies for doctors was found. The majority of the research projects focused on various different types of taxonomies.
Conclusions
No consistent and workable leadership training for the emergency medical teamleader was identified. One study for paramedics succeeded in training empowering leadership skills. For many years multiple taxonomies and leadership assessment tools have been developed but failed to come to terms with workable leadership training. The literature describes lack of leadership as highly detrimental to performance during a critical, clinical situation.
Keywords: Health profession, Emergency medicine
1. Introduction
Worldwide medical supervisors find it difficult to get students to rise to the occasion when called upon to act as leaders of emergency teams: many residents/rescuers feel unprepared to adopt the leadership role in emergencies [1, 2, 3, 4, 5, 6, 7, 8].
Team leadership in emergencies is reported as being important for the quality of the technical performance of teams [4, 5, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17], for patient outcome, patient safety and patient care [2, 3, 6, 8, 16, 18, 19, 20, 21, 22, 23, 24, 25]. The quality of team leadership may even influence patient mortality and survival rates [3, 6, 8, 13].
The aim of this systematic review is to investigate how literature describes workable and operational leadership training for the emergency medical team leader in exerting/practising leadership.
The scholarly field of leadership and general healthcare-leadership is rich. This study is not aimed at discussing differentiated leadership behaviour at a theoretical level.
2. Background
Leadership is acquired through practice, and therefore leadership competencies should be acquired not through theoretical learning, but through practice as described by Mintzberg [26]. In accordance with this, surgeons learn to sew a wound together by doing it in practice. In order to learn to ride a bike, theoretical knowledge, as well as feedback from educators and experts, is definitely valid but only by getting up on the bike and experiencing the feeling it is possible to acquire this competence. Experience obtained by practice is prerequisite for acquiring learning in certain areas. Only ‘by doing’ is it possible to acquire the feeling and sensation required for being able to execute these skills. The authors of this study do not consider that feedback based on behavioural indicators (leadership measurements tools) is equivalent to workable training of practising leadership in emergencies, it is necessary to exercise practising leadership in order to fully acquire leadership competence. There are many training programmes for leaders in different contexts. We focus our review on real and operational leadership training for physicians in emergency situations in healthcare.
In 1986 Iserson stated: “Most people are not born leaders; they must be taught leadership techniques” [27]. In 2016 Robinson and colleagues asserted: “In the field of cardiac arrest leadership, an increasing weight of evidence supports the notion that individuals can be trained to lead” [8].
There appears to be a lack of clarity about the perception of “good team leadership” in the literature. In 2010 Yukl [28] cited: “there are almost as many definitions of leadership as there are persons who have attempted to define the concept” (Stogdill (1974, p. 259) [29]. And Yukl continues: “The stream of new definitions has continued unabated since Stogdill made his observation, Leadership has been defined in terms of traits, behaviors, influence, interaction patterns, role relationships, and occupation of an administrative position”.
This study will focus on issues related to the training of the leadership role of the clinical team leader in emergencies.
3. Method
The systematic review was conducted in accordance with the Preferred Reporting Items for Systematic review and Meta-Analysis 2009 (PRISMA) Checklist. A search of the databases of Pubmed, Psycinfo (via Ovid), and ERIC was carried out in June–December 2016 with the aid of a research librarian. Appendix I shows the search terms and strategy, to which no time limit or language restrictions were applied. The search strategy was not limited by design or methodology. All types of papers concerning leadership training and education in emergency medical scenarios were included. Technical skills training, organizational leadership and teamwork training without explicit focus on leadership were excluded. During the early stages of the search, systematic reviews and reviews identifying relevant original articles were used as sources. One Systematic Review found (Fond G, et al: Charisma and leadership: New challenges for psychiatry) addressing leadership and charisma in psychiatry [30]. Three identified reviews addressed leadership and ‘Non-Technical Skills’ [18, 19, 31]. Three reviews addressed human factors and leadership: effective communication [13], team interactions and the performance of CPR (focus on gender and hierarchy) [14], and the importance of directive leadership [22]. One review addressed the importance, performance and assessment of hospital trauma teams [12]. Our review differs from these previous mentioned (except Mr. Fond's study) by being systematic and meeting the standards described in the PRISMA Checklist. The search string in Fond's study included ‘psychiatrist’ AND ‘mental health’ while our search did not use these terms but instead ‘train*’, ‘educat*’, ‘emergency’ OR ‘acute’ and thus had different outcome than the result of Fond's search.
The Committees on Health Research Ethics for the Capital Region of Denmark was asked to give ethical approval but a formal review was waived for this study (H-4-2015-FSP).
3.1. Screening articles
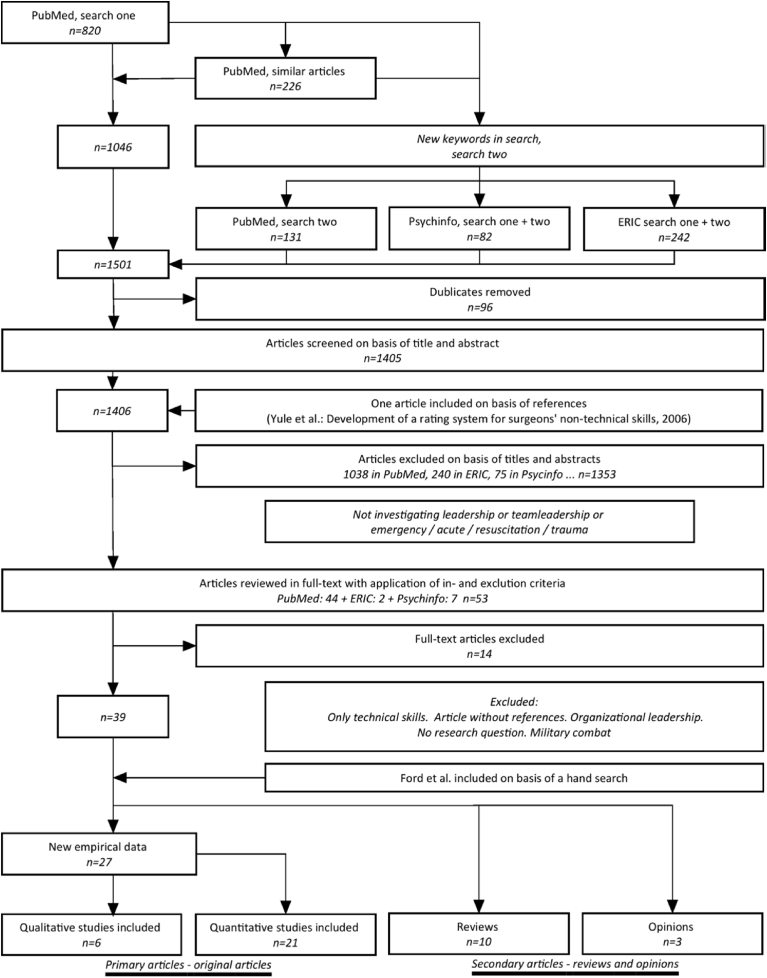
One author (TL) searched PubMed and screened titles including 820 eligible articles. PubMed's feature ‘similar articles’ was used and a further 226 articles were identified. A further search was conducted inspired by the new keywords found in the articles, and another 131 articles were found. The search strategy was applied to a search in the databases of Psycinfo (via OVID) and Eric resulting in 1.177 articles from PubMed, 82 from Psycinfo, and 242 from ERIC. After removing duplicates, two authors (TL and RBH) screened 1.405 titles and abstracts applying the above mentioned inclusion and exclusion criteria. One article was added on the basis of the references (Yule, 2006) [32]. The two authors then read the full text of the 53 potential articles applying inclusion and exclusion criteria. 39 articles were selected. There was a high degree of overall agreement between the two raters (94.45%). Interrater reliability was very good (Cohen's κ coefficient = 0,852). Differences of opinion about inclusion or exclusion were resolved by discussion between TL and RBH. 13 articles were excluded because their content did not meet the inclusion criteria and one article was incomplete because of missing references. Towards the end of the review process one further article, found in an additional manual search in Google (Ford 2016) was added [17]. 40 articles and reports were identified of these 27 were considered primary as they were original articles with interventions and new findings/evidence and 13 articles were considered secondary: 10 reviews and 3 opinions. Fig. 1 (Flowchart).
Fig. 1.
Flowchart of literature search and study selection in accordance with the PRISMA guidelines.
3.2. Quality of body of evidence
A review of qualitative as well as quantitative research papers was conducted. Quantitative articles focusing on practising leadership was to be classed according to PRISMA, Cochrane and GRADE. Qualitative articles according to CASP (Critical Appraisal Skills Programme) if a workable training of the teamleader function in emergencies was identified. Articles were considered primary if they reported empirical data about leadership training or behaviour (i.e., specific reports about leadership taxonomies and findings in questionnaires). Only primary studies are included in this Systematic Review.
This review is subdivided by the following sources (Table 1).
-
•
Training practising leadership and leadership assessment
-
•
Clinical simulation and leadership assessment
-
•
Assessing the quality of leadership
-
•
The need for leadership training
Table 1.
Study characteristics.
| Study | Objective | Content of intervention | Outcome/Conclusions | Teaching |
|---|---|---|---|---|
| Training practising leadership and assessment | ||||
| MANTHA, A. et al. 2016 | NTS curriculum for Indian paramedic trainees focused on strengthening on-scene leadership, teamwork, and public speaking skills | 40 paramedic trainees. Six-day course. Trainees completed self-assessments and delivered two brief video-recorded presentations before and after completion of the curriculum. Independent blinded observers scored 10 randomly selected trainees. | Outcomes of this leadership curriculum demonstrate a significant increase in paramedic trainees' self-perceived confidence, communication, and leadership skills | 6 - day seminar. Presentation of a non-professional topic to classmates. Developed new taxonomy |
| Clinical simulation and leadership assessment | ||||
| YULE, S. et al. 2015 | Demonstrate the effect of non-technical skills coaching on intraoperative behaviours and clinically significant decisions during simulated operations. | 16 surgeons, two groups. Five operations each surgeon. Case group received coaching on NTS after each operation - control not. Operation one and five was video recorded. Blinded assessors | Coaching improved residents' non-technical skills in the simulated OR compared with those in the control group | Non-technical skills coaching. NOTECHS inspired (NOTSS) |
| NICKSA, G.A. et al. 2015 | To educate surgical residents in leadership, teamwork, effective communication, and infrequently performed emergency surgical procedures with the use of inter-professional simulations. | 43 surgical residents PGYs 1 and 2. Interdisciplinary high-risk clinical scenarios. Pre (control) and 6 Mo after Post (case) 37 responded to a survey. Author assessor | The PGY 2 residents improved their skills, but the PGY 1 residents did not. A total of 89% of the residents felt the sessions were of great benefit. | Feedback, facilitated discussion, instructed on areas of knowledge as needed. Modified Oxford NOTECHS |
| CARLSON, J. et al. 2009 | Develop a measurement tool reliable at capturing team behaviour during a high-fidelity simulation. Explore the relationship between the team behaviours measured and the standard of technical medical care delivered specific to the needs of the case. | Study participants (n = 113), 44 teams (2 or 3 team members) During the workshop, every team participated in the same scripted case scenario facilitated by the same training instructor. Raters using the team behaviour measurement tool | The methods used provide a possible method for training and assessing team performance during simulation. The instrument presented in this study offers a possible template for future work | Simulation - facilitator – debriefing. ANTS adapted from NOTECHS |
| FERNANDEZ CASTELAO et al. 2015 | This study assessed the impact of the CRM team leader training on CPR performance and team leader verbalization | Forty-five teams of four members received ALS training. Team leaders in group one attended 90 min. CRM training. All others 90 min. ALS training. Video recorded. Check-list based tool developed by experts. Assessors blinded to the experimental allocation | Training only the designated team leaders in CRM improves performance of the entire team, in particular guideline adherence and team leader behaviour. (Emphasis on training of team leader behaviour appears to be beneficial in resuscitation and emergency medical course performance.) | CRM team leader training and additional ALS-training. |
| GILFOYLE, E. et al. 2007 | Educational intervention. evaluate immediate and long term learning outcomes in order to determine whether residents could acquire and retain team leadership skills in pediatric advanced resuscitation. | Case 15 paediatric residents 2 leader skills training, simulated resuscitation scenarios. Evaluated again 6 months later. Control N = 7 no training. Rating by checklist and self-reported questionnaire | Residents acquired resuscitation team leadership skills following an educational intervention. Six-month follow-up demonstrated skill retention beyond the initial intervention. Control group suggested that this was because participants had attended the first workshop. | Based on the needs assessment learning objectives were developed. Modified CRM checklist |
| HUNZIKER, S. et al.2010 | The aim of this study was to compare leadership instruction with a general technical instruction in simulated CPR scenario | 237 (280) medical stud. in teams of three. CPR simulation, pre-video. Basic instruction 20 min. Two groups. Case: Leadership training. Control: Technical training. CPR simulation, 2 post-video, n = 96 and n = 93. Follow up after 4 Mo. Videotapes coded by two independent blinded researchers | Causal relationship between leadership and performance was proven: Leadership instructions were superior to technical instructions, with more leadership utterances and better overall cardiopulmonary resuscitation performance. | Leadership instruction with pre-specified checklists - LBDQ inspired |
| ROBERTS, N.K. et al. 2014 | To investigate if brief training would have a sustained effect on individual acquisition and retention of knowledge and team practice behaviours and on team behaviours of health care professionals in medical emergency situations… | 57 medical staff members. Pre-test simulated CPR sessions. Then training concluding with a post simulation. Debriefing. Three weeks later third simulation. Video recordings. Two blinded raters. Questionnaire | Participants changed teamwork and communication behaviour on the post-test, and changes were sustained after a 3-week interval, though there was some loss of retention. Brief training exercises can change teamwork and communication behaviours on ad hoc trauma teams. | Simulation - video analysis - simulation - debriefing. 3 weeks later: simulation and questionnaire. LBDQ inspired |
| COOPER, S. et al. 2001 | Develop a course training leaders with the aim of changing behaviour and performance | Three day ALS course. N = 68. Three courses. Day one: ALS training. Day two and three all acted as team leader in a CPR simulation. After day two case group attended a leadership seminar. Control not. Five independent assessors, blinded | The leadership training programme significantly improved candidates leadership performance in the training situation | The experimental group attended a 75-min leadership development seminar. LBDQ inspired |
| Assessing the quality of leadership | ||||
| BRIGGS, A. et al. 2015 | Does team's and team leader's NTSs correlate with technical performance of clinical tasks? | 20 teams. Two separate, high-fidelity, simulated trauma scenarios. Video, divided into 4 consecutive sections. Team leader assessment using NOTSS. Entire team 2 additional raters used T-NOTECHS | The NTSs of trauma teams and team leaders deteriorate as clinical scenarios progress, and the performance of team leaders and teams is highly correlated. Cognitive NTS scores correlate with critical task performance. | Simulations - brief CRM training. Focus on Measuring. T-NOTECHS |
| COOPER, S. et al. 1999 | Determine the relationship between leadership behaviour, team dynamics and task performance | 20 resuscitation attempts were observed. All teams more than five members. A total of 18 leaders. Observers: an ALS instructor and a video rater | Leaders who initiated a structure, distributed tasks, and remained “hands off” improved team performance. An emergency leadership training programme is essential to enhance the performance of leaders and their teams. | Not teaching. LBDQ inspired |
| MARSCH, S.C. et al. 2004 | How human factors affect the team performance during a simulated cardiac arrest. And show correlation between leadership behaviour and outcome | 16 teams, each three health-care workers. Simulator. Video. Data analysis was performed independently by two of the authors using a checklist. | Two thirds of teams composed of qualified health-care workers failed to provide basic life support and/or defibrillation within an appropriate time window. | Simulation - video - debriefing LBDQ inspired |
| HARGESTAM, M. et al. 2016 | Investigate how trauma team members are positioned in the emergency room. How leaders communicate in terms of gaze direction, vocal nuances, and gestures during trauma team training. | 108 participants. Eighteen trauma teams were audio and video recorded during trauma team training. Focus is on team leaders' communication, analysis is performed in relation to both verbal and non-verbal communication. | Non-verbal communication reinforced the team-leaders’ communication. Team-members who are aware of their non-verbal communication can improve their performance. Vague non-verbal communication reinforces ambiguity and can lead to errors | Team training, CRM |
| JACOBSSON, M. et al. 2012 | Analyse how formal leaders communicate knowledge, create consensus, and position themselves in relation to others in the team | Sixteen trauma teams, six members on each team. High fidelity training in an emergency department. Video. | Communication in trauma teams is complex and consists of more than just transferring messages quickly. It also concerns what the leaders express, and even more importantly, how they speak to and involve other team members | High fidelity training –Qualitative content analysis |
| KRAGE, R. et al. 2014 | To invest whether external distractors influence performance during a standardized simulated CPR scenario in general and whether level of experience has an impact | 30 physicians, two simulated CPR. Cross-over study: 1: distractors (radio noise 70 dB, scripted family member, talking at crucial moments) 2: not. Video recorded. Two assessors rated independently | No interaction was observed between additional distractors and experience level. External distractors markedly reduce the quality of cardiopulmonary resuscitation. | Not teaching. Scoring protocol developed. |
| MCCUE, J.D. et al.1986 | To assess the residents' leadership style and the nurses' perceptions of the effectiveness of those styles. | 17 residents. A self-administered, self-rating leadership style indicator, LSI. Self reports and Nurses Reports. Questionnaire. Computerised scale. Not blinded assessors | The present study suggests that female residents may be more likely to use high relationship leadership styles in their interaction with nurses … analysis of leadership style is a potentially useful way of helping residents assume leadership more effectively. | Two-hour discussion about leadership. Not teaching. Leadership style indicator, LSI. |
| The need for leadership training | ||||
| HJORTDAHL, M. et al.2009 | To obtain a deeper understanding of which non-technical skills are important to members of the trauma team during initial examination and treatment of trauma patients. | Twelve semi-structured interviews. 2 authors participated in all 12. | Leadership was perceived as an essential component in trauma management. The ideal leader should be an experienced surgeon, have extensive knowledge of trauma care, communicate clearly and radiate confidence. Lack of leadership was often given as a reason for dysfunctional teamwork. | Not teaching |
| RINGEN, A.H. et al. 2011 | To assess the experience and education of Norwegian trauma team leaders, and allow them to describe their perceived educational needs | Written questionnaires. All 45 hospitals in Norway receiving severely injured trauma victims were contacted, randomly selected weeknight. Team leaders asked to specify what trauma related training programs they had participated in, how much experience they had, and what further training they wished, if any. | Level of experience among team leaders was highly variable and their educational background insufficient according to international and proposed national standards. Team leaders stated that more experience and better training are important to them in order to become better leaders | Not teaching |
| ROBINSON, P.S. et al. 2016 | To assess the perceptions of leadership and team working among members of a cardiac arrest team and to evaluate future training needs | 102 members of a cardiac arrest team. Survey. Responses sought from doctors, nurses and healthcare assistants | We recommend that training in and assessment of leadership skills in emergency scenarios should be an integral component of postgraduate medical training | Not teaching |
| WISBORG, T. et al. 2003 | Does the training of multi professional trauma teams and resuscitation teams for newborns vary? | Survey of training practices. The head nurse at each emergency department (n = 50) and neonatal ward (n = 16) was interviewed in a structured fashion. Asked if their emergency team personnel had participated in practical multi professional training during the previous 6 or 12months. | Regular team training represents an underused potential to improve handling of low-frequency emergencies. | Not teaching |
| HAYES, C.W. et al. 2007 | Determine internal medicine residents' perceptions of the adequacy of their training to serve as inhospital cardiac arrest team leaders | 654 residents were sent a survey, 289 residents (44.2%) responded. Subjects: adequacy of training, perception of preparedness, adequacy of supervision and feedback, and effectiveness of additional training tools | A significant number of internal medicine residents feel inadequately trained, unprepared, and unsupervised to lead cardiac arrest teams in teaching hospitals. | Not teaching |
| ITANI, K.M. et al. 2004 | Assess the perception of surgical residents in leadership skills. | Questionnaire, 43 residents. 1) Residents ranked 18 leadership skills on a scale of 1–4 in importance for career development. 2) Similar scale with regard to their personal confidence and competence in these same areas. 3) Evaluate themselves with regard to five leadership traits. | Traditionally, development of physician leadership has occurred at random in surgical training. It is our job as surgical educators to provide this opportunity to our residents. Ethics was the only area in which 75% of the residents believed themselves to be more than minimally competent | Not teaching |
| KOLEH-MAINEN, C. et al. 2014 | Investigating code leadership as perceived by residents in four areas: (1) learning to be a code leader (2) leadership defines code success (3) ideal code leadership behaviours (4) leadership and gender | 25 residents, semi-structured telephone or in-person interviews. Recorded and transcribed. Three authors analysed three interviews focusing on content areas. Four authors read all transcripts in full | Leadership defines code success. Poor leadership was cited as the major factor to a chaotic code. Participants reported that it was important to be “authoritative”; to have a “strong presence” by being both seen and heard. Female participants described feeling stress from having to violate gender behavioural norms in the role of code leader. | Not teaching |
| YULE S et al. 2006a Developing | Describe the method used to identify surgeons' non-technical skills, and the development of a skills taxonomy and behavioural rating system to structure observation and feedback in surgical training | 27 consultant surgeons. Interview. Identify key non-technical skills and interpersonal skills. Multidisciplinary group developed the interview schedule (psychologists, surgeons and an anaesthetist). | The NOTSS skills taxonomy and marker system presented here has been grounded empirically in surgery, and was developed with domain experts (consultant surgeons) at every stage to ensure that the system is explicit, transparent and has an acceptable degree of construct validity. | Not teaching. Development of a tool - NOTSS |
| LEENSTRA, N.F. et al. 2016 | Need for a taxonomy of leadership skills that specifies the skill components to be learned and the behaviours by which they can be assessed across the five phases of trauma care, the authors developed the Taxonomy of Trauma Leadership Skills, TTLS | 28 interviews w. trauma leaders and 14 raters. Skill elements captured by 67 behavioural markers. Categorized using multiple raters | The TTLS provides a framework for teaching, learning, and assessing team leadership skills in trauma care and other complex, acute care situations | Not teaching. Developed the Taxonomy of Trauma Leadership Skills, TTLS |
| MAKINEN, M. et al. 2007 | The purpose of this study was to assess the resuscitation skills of nurses to facilitate construction of an educational programme | From Finland: 110, Sweden: 40 nurses. Case, leadership training (S), control not (F). Subjects tested in pairs. A checklist used to grade. 5 assessors independently, not blinded | Defining and teaching leadership seems to improve resuscitation performance. | Not teaching. Adapted ANTS (NOTECHS inspired) |
| SADIDEEN, H. et al. 2016 | Video analysis of leadership behaviours within The Burns Suite (a simulation tool to deliver inter professional and team work training). Explore whether Simulation-based team training within TBS can elaborate on key leadership theories. Which leadership models appeared predominant within TBS. | N = 12, 3 simulations, each team 4 members. Video. Focus group interviews after debriefing. Objective to identify leadership skills mapping them on to leadership theory. 2 authors and 2 other authors independently assessors | Effective leadership is essential for successful functioning of work teams and accomplishment of task goals. Leadership in a team-based resuscitation scenario can be considered as distributed, rather than continuously being associated with a specific leader. | Simulation - video - debriefing. |
4. Results
The review included 27 original articles, covering the period from 1986 to 2016. Two authors were responsible for more than one article: Yule [24, 32] and Cooper [33, 34].
4.1. Training practising leadership and assessment
This source demonstrates the identification of workable leadership training focusing on training leadership by practice.
One study was found: Adaptive leadership curriculum for Indian paramedic trainees [35]. The personal challenge of speaking in front of an audience was compared to the personal challenges the paramedic team leader faces in front of the team when working in emergencies. The intervention conducted an extensive six-day course, 8 hours a day. The trainees delivered a short video-recorded presentation before and after completion of the curriculum. Topics were limited to simple, familiar topics: describing family and friends, detailing favourite foods, locations, and sports, and describing the functions of common objects. Blinded raters scored the presentations on overall quality, body language (gestures, posture, and eye contact), emotional engagement (enthusiasm, expressions, and emotions), content (clarity, depth, and organization), auditory delivery (pacing, volume, and tone), and confidence. The leadership function was trained separately to technical clinical skills. This study is the only one that met the purpose of the search in the systematic review. It identified operational training in practising leadership for the emergency medical team leader and consequently, it is the only study evaluated for quality of evidence. The quality assessment of this study is low (Table 2).
Table 2.
Quality assessment. One single study identified demonstrated operational training in practising leadership for the emergency medical team leader and consequently, the only study evaluated for quality of evidence.
| Adaptive leadership curriculum for Indian paramedic trainees. Mantha et al. | ||||
|---|---|---|---|---|
| Objective | Content of intervention | Conclusion | Risk of bias | Validity of evidence |
| NTS curriculum for Indian paramedic trainees focused on strengthening on-scene leadership, teamwork, and public speaking skills | 40 paramedic trainees. Six-day course. Trainees completed self-assessments and delivered two brief video-recorded presentations before and after completion of the curriculum. Independent blinded observers scored 10 randomly selected trainees. | Outcomes of this leadership curriculum demonstrate a significant increase in paramedic trainees' self-perceived confidence, communication, and leadership skills | Performance bias. | Low body of evidence according to GRADE |
4.2. Clinical simulation and leadership assessment
This source demonstrates the identification of studies regarding acquirement/optimizing clinical competence and use of taxonomies including measurement of leadership. In summary, for these studies, leadership training is based on checklists describing behaviours. A typical design for these studies is video recording of simulation training, with or without prior training and subsequent feedback to the trainee based on the learning objectives described in the taxonomy.
4.3. Assessing the quality of leadership
This source demonstrates the identification of observational studies concerning leadership's importance for teamwork or outcome, importance of non-verbal communication, the influence of external distractors on the quality of CPR, and an analysis of leadership style.
4.4. The need for leadership training
This source demonstrates the identification of survey/interview studies concerning the educational needs for leadership training, perception of surgical residents' leadership skills, residents' experiences leading codes, and development of new taxonomies.
Out of 27 included intervention articles 19 [[1], [2], [5], [7], [10], [11], [15], [16], [20], [23], [24], [32], [33], [34], [35], [36], [37], [38], [39]] transformed qualitative statements about the trainees leadership behaviour into quantitative data, by the use of behavioural marker systems. A total of 24 studies found it appropriate to use statistics to prove the measurability of the outcome [1, 2, 3, 4, 5, 7, 8, 9, 10, 11, 15, 16, 20, 23, 25, 32, 33, 34, 35, 36, 37, 38, 39, 40], 15 studies used comparative statistics [1, 2, 3, 5, 7, 10, 11, 15, 23, 32, 33, 34, 35, 37, 38], nine other used descriptive statistics [4, 8, 9, 16, 20, 25, 36, 39, 40].
Six different definitions of leadership were identified [1, 4, 33, 35, 36, 40], the definitions were centred mostly on achieving common aims through collaboration between leader and team. Leadership is implicitly also defined in the Leadership Behaviour Description Questionnaire (LBDQ) checklist [29, 33, 41] (adapted from military, created in 1945), as well as in the Non-Technical Skills checklist (NOTECHS) (adapted from aviation to healthcare for the first time in 2003, Anaesthetists' non-technical skills [42] (ANTS)). No consensus on a clear definition of leadership has been found.
Seven articles stated it could be an advantage to separate leadership training from medical competencies training [3, 5, 8, 10, 23, 35, 36].
The studies were very inhomogeneous but with trauma and resuscitation as the most common clinical situation. In addition the literature was dominated by ‘significant variability in terminology, training modalities and evaluation’ in this field [11, 35, 37].
5. Discussion
5.1. Main findings
No defined and workable leadership training for medical team leaders was identified in scientific literature on leadership training in medical emergencies and no consensus on a clear definition of leadership has been found. For the last three decades, leadership and training leadership have been described as important issues in healthcare.
The majority of the studies were based on leadership as described and defined in numerous taxonomies. It should be emphasized that the current study is not a comprehensive review of the content of the taxonomies as recent studies with this objective have been conducted [43, 44].
5.2. Theoretical significance of the findings
Taxonomies are often used in an educational context as a standardised hierarchical classification of learning objectives often handling affective, psychomotor and cognitive areas. Medical education scholars have leveraged multiple taxonomies too in order to understand and measure how medical students develop and demonstrate team leadership in emergencies.
5.2.1. Quantifiability
An alteration of medicine or treatment in health care requires strong statistical evidence. This is central to clinical research and as such an expression of positivist ontology. “Medical doctors believe that their field is founded on scientific knowledge; where knowledge is defined as facts that can be empirically verified by the biomedical method”, as stated by Prof. Malterud [45]. In order to calculate differences, there is a need to quantify. This is supported by the finding of 24 out of 27 studies proving their results with statistics as mentioned in the results section.
When addressing the importance of human factors for clinical work, it is therefore necessary to be able to measure those factors – and thus taxonomies are given their justification. These taxonomies are based on behavioural marker systems. Medical scholars have sought help in other high-risk professions of military and aviation. With the help of these professions, the medical scholars have theoretically developed “what to measure”. This is accepted by the medical world without distinction to the differences between captains, officers and the young doctor (the resident). Military education and aviation education are aimed at professionals with different prerequisites/conditions than doctors. Officers and pilots in command of aircraft are leaders in their professions, and it could therefore be argued that their situation is essentially different to that of newly qualified young doctors who have not yet been introduced to leadership. In addition, it can be noted that doctors have to cope with several other roles in their profession, in accordance with CanMEDS definition of the seven roles of the doctor [46].
The enthusiasm of the researchers is noticeable when they consider solving the problem as stated by Prof. Yule in 2006 “this study has taken the additional step of identifying explicitly the particular non-technical skills which might be both taught and observed – and therefore measured”. [32] It seems to become a goal in itself to be able to measure.
The challenge of measuring behaviour has been that training methods had to be changed to teaching methods. The question “how to train” becomes substituted with the question “why train” when feedback is given. The student receives feedback on the quantitative score obtained regarding the leadership role but no practical guidance on training in the leadership role. In this review, one single study describes how to optimize the behaviour that gives the trainee a sensation of better control in the situation.
An explanation of this change of focus could be interpreted as ‘substitution’ as described by psychologist Daniel Kahneman. The mechanism of replacing a difficult question with a simpler one is extensively described: “when faced with a difficult question, we often answer an easier one instead, usually without noticing the substitution […] The target question is the assessment you intend to produce. The heuristic question is the simpler question that you answer instead” [47].
In order to show a difference, different academic goals are developed (surrogate marker for leadership). Time to implement various algorithms is measured. E.g. measure on “Time to start cardiopulmonary resuscitation”, “Time to perform critical tasks”, or “time to call for help during bleeding, operative time, and path length of laparoscopic instruments” has been found. However, one could assert that these results were related to how well the doctors knew how to treat the patient, not the actual quality of leadership. Nevertheless, measuring time to perform tasks and giving feedback according to objectives defined in taxonomies mixes professionalism and attempts at leadership training but without taking into account the fact that more and very different mind systems are challenged, described as Systems 1 and 2 by Kahneman [47]. In accordance with Kahneman, it is possible to argue that training in clinical skills and memorizing algorithms, addresses the effortful, slow and rational operations of system 2 while interaction between people (leadership) takes place in the automatic, fast and intuitive system 1. It is difficult to operate in both systems simultaneously and errors can occur if the two systems conflict with each other. This brings a focus on the role of the medical expert (medical competence) in this training and draws attention away from actually practising training of leadership.
The qualitative term “leadership” is difficult to define according to Yukl [28], and Stogdill [29], as the findings in this study have demonstrated in the results section. The problem arises when trying to turn an indefinable qualitative concept to a measurable concept. Leadership in emergencies is basically – isolated from professional ability – a complex and multifaceted social competence. Analysing social interaction or training social competencies, including dissemination, requires an interpretative approach rather than the positivist's need for measurability and testing. Apparently, this strategy has regrettably resulted in ignoring the fact that there is still no methodology developed in order to “train the leadership role”.
However, in recent years researchers have begun to ask questions about the recognized taxonomy-based method of leadership training. Three articles [11, 35, 37] stated, in the background to their study, that it could be difficult to keep track of the actual content of the variety of tools and methods developed. The former described advocate for measuring instruments, Prof. Yule, backtracked when in 2015 he indicated that the focus might be advantageously changed away from the development of new measuring tools: “The rate of developing assessment tools in this area has outpaced development of workable interventions to improve non-technical skills in surgical training and beyond”. [24]
5.3. Practical implications
However, one study for paramedics [35] created an innovative training of practising leadership with focus on personal communicative skills. The intervention in this study was to challenge the student to deliver a short presentation in front of an audience. Thus, by creating a stressful situation which might be characterized as unpleasant and anxiety inducing, the study implies that it is necessary to work with the most personal challenges associated with the intense situation. As a consequence, it is necessary to work with the student's courage, self-confidence and authority when acting as a team leader. It is interesting to note that the only study found providing a workable and effective way of exerting leadership as a practice is designed and implemented by paramedics.
Seven studies pointed out that it could be advantageous to separate leadership training from medical competence training.
5.4. Limitations of the review
The result of this systematic review is negative, no consistent and workable training of practising leadership for the emergency medical team-leader was identified in the scientific literature on leadership training in medical emergencies and it is consequently possible to argue that the study is unsuccessful. However, one can assume, as the authors of the study argue, that the result reveals the deficiency of research in this area in the last 30 years. This can be considered as a substantial contribution adding constructive and important knowledge.
5.5. Conclusion
For many years multiple taxonomies and leadership assessment tools have been developed but failed to come to terms with workable leadership training.
Despite there being no clear definition, the literature describes lack of leadership as highly detrimental to performance during a critical, clinical situation and performance as very variable.
5.5.1. Directions for future research
Does the literature identify learning goals or challenges to be addressed in the training of leadership for residents when acting as team leaders in emergencies?
Declarations
Author contribution statement
Ture Larsen, Randi Beier-Holgersen, Jette Meelby: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Peter Dieckmann, Doris Østergaard: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
Ture Larsen was supported by Tryg Foundation, Laerdal Foundation and Nordsjællands Hospital, Denmark.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Itani K.M., Liscum K., Brunicardi F.C. Physician leadership is a new mandate in surgical training. Am. J. Surg. 2004;187(3):328–331. doi: 10.1016/j.amjsurg.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Gilfoyle E., Gottesman R., Razack S. Development of a leadership skills workshop in paediatric advanced resuscitation. Med. Teach. 2007;29(9):e276–e283. doi: 10.1080/01421590701663287. [DOI] [PubMed] [Google Scholar]
- 3.Hayes C.W., Rhee A., Detsky M.E., Leblanc V.R., Wax R.S. Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: a survey of internal medicine residents. Crit. Care Med. 2007;35(7):1668–1672. doi: 10.1097/01.CCM.0000268059.42429.39. [DOI] [PubMed] [Google Scholar]
- 4.Hjortdahl M., Ringen A.H., Naess A.C., Wisborg T. Leadership is the essential non-technical skill in the trauma team--results of a qualitative study. Scand. J. Trauma Resuscitation Emerg. Med. 2009;17 doi: 10.1186/1757-7241-17-48. 48-7241-17-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunziker S., Buhlmann C., Tschan F., Balestra G., Legeret C., Schumacher C. Brief leadership instructions improve cardiopulmonary resuscitation in a high-fidelity simulation: a randomized controlled trial. Crit. Care Med. 2010;38(4):1086–1091. doi: 10.1097/CCM.0b013e3181cf7383. [DOI] [PubMed] [Google Scholar]
- 6.Kolehmainen C., Brennan M., Filut A., Isaac C., Carnes M. Afraid of being "witchy with a 'b'": a qualitative study of how gender influences residents' experiences leading cardiopulmonary resuscitation. Acad. Med. J. Assoc. Am. Med. Coll. 2014;89(9):1276–1281. doi: 10.1097/ACM.0000000000000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nicksa G.A., Anderson C., Fidler R., Stewart L. Innovative approach using interprofessional simulation to educate surgical residents in technical and nontechnical skills in high-risk clinical scenarios. JAMA Surg. 2015;150(3):201–207. doi: 10.1001/jamasurg.2014.2235. [DOI] [PubMed] [Google Scholar]
- 8.Robinson P.S., Shall E., Rakhit R. Cardiac arrest leadership: in need of resuscitation? Postgrad. Med. 2016 doi: 10.1136/postgradmedj-2015-133738. [DOI] [PubMed] [Google Scholar]
- 9.Wisborg T., Ronning T.H., Beck V.B., Brattebo G. Preparing teams for low-frequency emergencies in Norwegian hospitals. Acta Anaesthesiol. Scand. 2003;47(10):1248–1250. doi: 10.1046/j.1399-6576.2003.00249.x. [DOI] [PubMed] [Google Scholar]
- 10.Marsch S.C., Muller C., Marquardt K., Conrad G., Tschan F., Hunziker P.R. Human factors affect the quality of cardiopulmonary resuscitation in simulated cardiac arrests. Resuscitation. 2004;60(1):51–56. doi: 10.1016/j.resuscitation.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Makinen M., Aune S., Niemi-Murola L., Herlitz J., Varpula T., Nurmi J., ECCE Study Group Assessment of CPR-D skills of nurses in goteborg, Sweden and espoo, Finland: teaching leadership makes a difference. Resuscitation. 2007;72(2):264–269. doi: 10.1016/j.resuscitation.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 12.Georgiou A., Lockey D.J. The performance and assessment of hospital trauma teams. Scand. J. Trauma Resuscitation Emerg. Med. 2010;18 doi: 10.1186/1757-7241-18-66. 66-7241-18-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunziker S., Tschan F., Semmer N.K., Howell M.D., Marsch S. Human factors in resuscitation: lessons learned from simulator studies. J. Emergencies, Trauma, Shock. 2010;3(4):389–394. doi: 10.4103/0974-2700.70764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hunziker S., Johansson A.C., Tschan F., Semmer N.K., Rock L., Howell M.D., Marsch S. Teamwork and leadership in cardiopulmonary resuscitation. J. Am. Coll. Cardiol. 2011;57(24):2381–2388. doi: 10.1016/j.jacc.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 15.Briggs A., Raja A.S., Joyce M.F., Yule S.J., Jiang W., Lipsitz S.R., Havens J.M. The role of nontechnical skills in simulated trauma resuscitation. J. Surg. Educ. 2015;72(4):732–739. doi: 10.1016/j.jsurg.2015.01.020. [DOI] [PubMed] [Google Scholar]
- 16.Leenstra N.F., Jung O.C., Johnson A., Wendt K.W., Tulleken J.E. Taxonomy of trauma leadership skills: a framework for leadership training and assessment. Acad. Med. J. Assoc. Am. Med. Colleges. 2016;91(2):272–281. doi: 10.1097/ACM.0000000000000890. [DOI] [PubMed] [Google Scholar]
- 17.Ford K., Menchine M., Burner E., Arora S., Inaba K., Demetriades D., Yersin B. Leadership and teamwork in trauma and resuscitation. West. J. Emerg. Med. 2016;17(5):549–556. doi: 10.5811/westjem.2016.7.29812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yule S., Flin R., Paterson-Brown S., Maran N. Non-technical skills for surgeons in the operating room: a review of the literature. Surgery. 2006;139(2):140–149. doi: 10.1016/j.surg.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 19.Flin R., Yule S., Paterson-Brown S., Maran N., Rowley D., Youngson G. Teaching surgeons about non-technical skills. Surg. J. Roy. Coll. Surg. Edinb. Ireland. 2007;5(2):86–89. doi: 10.1016/s1479-666x(07)80059-x. [DOI] [PubMed] [Google Scholar]
- 20.Ringen A.H., Hjortdahl M., Wisborg T. Norwegian trauma team leaders--training and experience: a national point prevalence study. Scand. J. Trauma Resuscitation Emerg. Med. 2011;19 doi: 10.1186/1757-7241-19-54. 54-7241-19-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobsson M., Hargestam M., Hultin M., Brulin C. Flexible knowledge repertoires: communication by leaders in trauma teams. Scand. J. Trauma Resuscitation Emerg. Med. 2012;20 doi: 10.1186/1757-7241-20-44. 44-7241-20-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hunziker S., Tschan F., Semmer N.K., Marsch S. Importance of leadership in cardiac arrest situations: from simulation to real life and back. Swiss Med. Wkly. 2013;143:w13774. doi: 10.4414/smw.2013.13774. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez Castelao E., Boos M., Ringer C., Eich C., Russo S.G. Effect of CRM team leader training on team performance and leadership behavior in simulated cardiac arrest scenarios: a prospective, randomized, controlled study. BMC Med. Educ. 2015;15 doi: 10.1186/s12909-015-0389-z. 116-015-0389-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yule S., Parker S.H., Wilkinson J., McKinley A., MacDonald J., Neill A., McAdam T. Coaching non-technical skills improves surgical residents' performance in a simulated operating room. J. Surg. Educ. 2015;72(6):1124–1130. doi: 10.1016/j.jsurg.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 25.Hargestam M., Hultin M., Brulin C., Jacobsson M. Trauma team leaders' non-verbal communication: video registration during trauma team training. Scand. J. Trauma Resuscitation Emerg. Med. 2016;24 doi: 10.1186/s13049-016-0230-7. 37-3016-0230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mintzberg H. Visited Nov. 2017. Rethinking the MBA.https://hbr.org/2009/03/rethinking-the-mba.html Retrieved from. [Google Scholar]
- 27.Iserson K.V. Critical leadership. J. Emerg. Med. 1986;4(4):335–340. doi: 10.1016/0736-4679(86)90016-8. [DOI] [PubMed] [Google Scholar]
- 28.Yukl G. seventh ed. Pearson; New Jersey: 2010. Leadership in Organizations. [Google Scholar]
- 29.Stogdill R.M. 1974. Handbook of Leadership: a Survey of Theory and Research; p. 259. New York-London. [Google Scholar]
- 30.Fond G., Ducasse D., Attal J., Larue A., Macgregor A., Brittner M., Capdevielle D. Charisma and leadership: new challenges for psychiatry. [Charisme et leadership: de nouveaux defis pour la psychiatrie] L'Encephale. 2013;39(6):445–451. doi: 10.1016/j.encep.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 31.Willems A., Waxman B., Bacon A.K., Smith J., Kitto S. Interprofessional non-technical skills for surgeons in disaster response: a literature review. J. Interprof. Care. 2013;27(5):380–386. doi: 10.3109/13561820.2013.791670. [DOI] [PubMed] [Google Scholar]
- 32.Yule S., Flin R., Paterson-Brown S., Maran N., Rowley D. Development of a rating system for surgeons' non-technical skills. Med. Educ. 2006;40(11):1098–1104. doi: 10.1111/j.1365-2929.2006.02610.x. [DOI] [PubMed] [Google Scholar]
- 33.Cooper S., Wakelam A. Leadership of resuscitation teams: "Lighthouse leadership. Resuscitation. 1999;42(1):27–45. doi: 10.1016/s0300-9572(99)00080-5. [DOI] [PubMed] [Google Scholar]
- 34.Cooper S. Developing leaders for advanced life support: evaluation of a training programme. Resuscitation. 2001;49(1):33–38. doi: 10.1016/s0300-9572(00)00345-2. [DOI] [PubMed] [Google Scholar]
- 35.Mantha A., Coggins N.L., Mahadevan A., Strehlow R.N., Strehlow M.C., Mahadevan S.V. Adaptive leadership curriculum for indian paramedic trainees. Int. J. Emerg. Med. 2016;9(1) doi: 10.1186/s12245-016-0103-x. 9-016-0103-x. Epub 2016 Feb 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCue J.D., Magrinat G., Hansen C.J., Bailey R.S., Jan Residents' leadership styles and effectiveness as perceived by nurses. J. Med. Educ. 1986;61(1):53–58. doi: 10.1097/00001888-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Carlson J., Min E., Bridges D. The impact of leadership and team behavior on standard of care delivered during human patient simulation: a pilot study for undergraduate medical students. Teach. Learn. Med. 2009;21(1):24–32. doi: 10.1080/10401330802573910. [DOI] [PubMed] [Google Scholar]
- 38.Krage R., Tjon Soei Len L., Schober P., Kolenbrander M., van Groeningen D., Loer S.A. Does individual experience affect performance during cardiopulmonary resuscitation with additional external distractors? Anaesthesia. 2014;69(9):983–989. doi: 10.1111/anae.12747. [DOI] [PubMed] [Google Scholar]
- 39.Roberts N.K., Williams R.G., Schwind C.J., Sutyak J.A., McDowell C., Griffen D. The impact of brief team communication, leadership and team behavior training on ad hoc team performance in trauma care settings. Am. J. Surg. 2014;207(2):170–178. doi: 10.1016/j.amjsurg.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 40.Sadideen H., Weldon S.M., Saadeddin M., Loon M., Kneebone R. A video analysis of intra- and interprofessional leadership behaviors within "the burns suite": identifying key leadership models. J. Surg. Educ. 2016;73(1):31–39. doi: 10.1016/j.jsurg.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 41.Markham S., Scott K. A component factor analysis of the initiating structure scale of the leadership behavior description questionnaire, form XII. Psychol. Rep. 1983;52:71. [Google Scholar]
- 42.Fletcher G., Flin R., McGeorge P., Glavin R., Maran N., Patey R. Anaesthetists' non-technical skills (ANTS): evaluation of a behavioural marker system. Br. J. Anaesth. 2003;90(5):580–588. doi: 10.1093/bja/aeg112. [DOI] [PubMed] [Google Scholar]
- 43.Wood T.C., Raison N., Haldar S., Brunckhorst O., McIlhenny C., Dasgupta P., Ahmed K. Training tools for nontechnical skills for surgeons-A systematic review. J. Surg. Educ. 2017;74(4):548–578. doi: 10.1016/j.jsurg.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 44.Henrickson Parker S., Yule S., Flin R., McKinley A. Towards a model of surgeons' leadership in the operating room. BMJ Qual. Saf. 2011;20(7):570–579. doi: 10.1136/bmjqs.2010.040295. [DOI] [PubMed] [Google Scholar]
- 45.Malterud K. The art and science of clinical knowledge: evidence beyond measures and numbers. Lancet. 2001;358(9279):397. doi: 10.1016/S0140-6736(01)05548-9. [DOI] [PubMed] [Google Scholar]
- 46.CanMEDS flower. 2017. http://canmeds.royalcollege.ca/en/about Retrieved from. [Google Scholar]
- 47.Kahneman D. Farrar, Straus and Giroux. US; New York, NY, US: 2011. Thinking, Fast and Slow. Thinking, Fast and Slow.499 Pp. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.