Abstract
Background: Despite the high prevalence of blood pressure (BP) measurement errors in the outpatient setting, little is known about why primary care clinics struggle to achieve consistently accurate BP measurements in routine practice. We investigated barriers affecting measurement of BP for adult patients in primary care. Methods: We conducted a qualitative evaluation in 6 adult primary care clinics. BP measurement was observed during 54 routine patient encounters. Six managers completed semistructured interviews and 18 clinical staff members participated in focus group discussions. We used an inductive, data-driven approach to identify and organize findings into cohesive, overarching themes describing factors affecting BP measurement. Results: Observed errors in BP measurement spanned the entire spectrum of steps required to obtain BP properly. Barriers to proper BP measurement were related to staff knowledge and behavior (inadequate knowledge, training, and feedback); workflow constraints (need to multitask, inadequate time); and equipment issues (BP monitors, seating). Patient characteristics and behavior also affected BP measurement. Conclusions: Correct measurement of BP is affected by a wide range of factors and is challenging to accomplish consistently in primary care. These findings may inform the design of performance improvement programs to maximize the quality of BP measurement in the outpatient setting.
Keywords: hypertension, blood pressure, measurement, office, barriers, qualitative
Introduction
Hypertension (HTN) is the leading cause of death and disability on the planet1 and it affects 29% of US adults.2 Although out-of-office monitoring is recommended for assessing blood pressure (BP) status,3 many practices face challenges in adopting ambulatory BP monitoring and home BP self-monitoring.4 In routine care, office BP measurement remains the de facto method to screen for, diagnose, and monitor treatment of HTN. Furthermore, major HTN trials have used office BP to define eligibility and guide medication titration.5,6
Clinical guidelines emphasize the importance of accurate office BP measurement for diagnostic and treatment decisions.7 Application of guidelines without accurate BP measurement may create a gap between outcomes observed in clinical practice and those observed in clinical trials.8 Accurate BP measurement involves patient preparation and positioning, technique, timing, and equipment.7,9 Clinic staff must be instructed on correct technique, have the skills to apply their knowledge, and have enough time to measure BP correctly. Patient preparation involves ensuring that the patient has not eaten, had caffeine, smoked, or exercised within 30 minutes of the measurement. The patient should empty his or her bladder (if necessary), rest quietly for 5 minutes, and sit in a chair with back and feet supported. A validated BP device should be used, with an appropriately sized cuff placed on the patient’s bare arm supported at the level of the heart. The patient and clinic staff should refrain from talking during measurement. Multiple measurements should be obtained, at least 1 minute apart. Deviation from recommended BP measurement procedures usually produces falsely elevated BP readings,10-12 leading to inappropriate treatment.13
The quality of office BP measurement has been described,12,14,15 but these studies did not explore the reasons why a health care organization may struggle to consistently obtain high-quality BP measurements. Anecdotal observations suggested that there were many barriers to consistent and accurate BP measurement at our outpatient clinics. Although we had trained clinical staff on BP measurement, it was clear that education was not sufficient. Therefore, we conducted a qualitative evaluation to better understand the experiences and barriers affecting measurement of BP for adult patients in primary care clinics.
Methods
The study is reported according to Consolidated Criteria for Reporting Qualitative Research.16 The study was conducted in 2015-2016 in 6 adult primary care (general internal medicine and family medicine) clinics in the faculty practice of McGovern Medical School of The University of Texas Health Science Center at Houston. One clinic is in central Houston, while the other 5 are located more peripherally in the greater Houston area. The clinics were invited to participate because of high patient volume.
The project team included a physician, public health professionals, a doctoral nursing candidate, and a medical student. Team members conducted interviews with clinic managers about BP measurement practices, observed clinic staff (medical assistants and nurses) measuring BP during routine patient care, and held focus groups with clinic staff about their experiences with BP measurement. The data were in the form of detailed field notes from BP measurement observations, interviews, and focus groups. All observations and discussions pertained to measurement of BP in adults with or without a prior diagnosis of HTN. The Committee for the Protection of Human Subjects reviewed and designated the project as a Quality Improvement project.
Field Observations
Team members observed clinical staff measuring BP in a convenience sample of 54 patients in the 6 clinics during routine care. The observations focused on selected aspects of BP measurement procedures related to patient preparation and positioning, timing of measurement, and technique.9 After each observation, the observer transcribed field notes of the encounter. Because the goal was to observe a broad range of behaviors involved in BP measurement rather than to make statistical inferences about the prevalence of such behaviors, the observations are described qualitatively.
Interviews With Clinic Managers
Clinic managers at each site (n = 6) participated in structured one-on-one interviews to provide their perspective on BP measurement in the office setting. Topics included barriers to proper BP measurement, training of clinic staff, and BP measurement devices (Supplementary File 1). Other open-ended questions solicited additional perspectives about BP measurement. Interviews lasted approximately 15 to 20 minutes.
Focus Groups
One focus group discussion was conducted at each of the 6 clinics. Eighteen clinical staff who routinely measure and document BP participated in the focus groups. The purpose of these discussions was to learn about their perspective on how BP is measured in the clinic. Each focus group was led by one moderator while another team member took detailed notes. The moderator asked open-ended questions about experiences related to adherence to recommended BP measurement procedures (Supplementary File 2). Each focus group lasted approximately 40 to 50 minutes.
In reviewing the study with the Committee for the Protection of Human Subjects, concerns were raised that clinic personnel may be reluctant to provide feedback about their experiences if it shed negative light on their supervisors. For example, a medical assistant may be reluctant to report that a physician wants patients to be prepared quickly in a way that does not allow enough time to properly measure BP. Therefore, we emphasized that the interviews and focus groups were confidential, voluntary, were not contributing to performance evaluations, and were not audiotaped. We conducted interviews and focus groups until data saturation was reached, such that no new substantive information was obtained.
Data Analysis
We used an inductive, data-driven approach to thematic analysis. Notes from the field observations, interviews, and focus groups were reviewed and coded by 2 independent reviewers. The project team convened to discuss the coded data. Related codes were organized into cohesive, overarching themes describing factors affecting BP measurement. Conflicts were resolved by consensus of the project team throughout analysis.
Results
Errors in BP measurement observed in 54 unique patient encounters are listed in Table 1. Errors were noted in at least 1 patient for the major recommended steps, such as not having the patient’s feet planted firmly on the ground and not having the patient’s arm elevated at the correct height with palm facing up.
Table 1.
Observed Blood Pressure (BP) Measurement Errors in 54 Unique Patient Encounters in 6 Clinics.
| Both feet not planted firmly on floor (not crossed, dangling, etc.) Patient’s arm was not elevated with palm facing up during BP reading Patient did not rest quietly for at least 5 minutes before BP measurement Patient did not sit upright with back supported Patient talked during BP reading Cuff was not placed directly on skin when taking BP Only obtaining 1 reading, even if the initial reading was ⩾140/90 mm Hg Patient was moving during BP reading Medical assistant used the incorrect cuff size on patient as deemed by cuff markers |
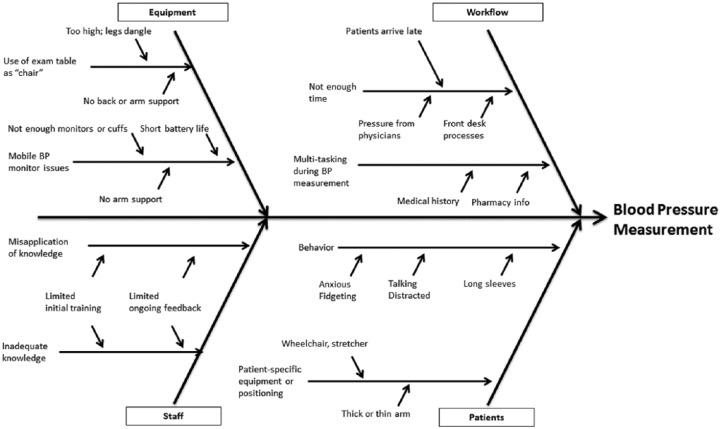
Multiple factors affect the performance of clinic staff in measuring BP according to recommended procedures during a routine patient encounter. Several factors were consistently noted and discussed in the manager interviews and staff focus groups. These factors are broadly categorized into themes related to (a) staff knowledge and behavior, (b) workflow, (c) equipment and layout, and (d) patient characteristics and behavior. These themes have some overlap and are not mutually exclusive.
Staff Knowledge and Behavior
Knowledge regarding proper BP measurement recommendations was a factor in obtaining accurate BP measurement. Clinic staff had brief training on BP measurement during new employee orientation. During orientation, the new staff felt competent to take BP accurately after passing the skills checklist. After they started working in the clinics, there were no consistent processes for proficiency evaluation and feedback related to BP measurement.
Clinic staff also reported that it was challenging to apply the principles discussed during training when working in the “real-world” environment of a busy clinic. For example, staff acknowledged that patients should remain silent during BP measurement, but they reported that it was difficult to enforce silence during the encounter. This was consistent with the field observations where patients were talking during BP measurement. Additionally, focus groups in 4 of 6 sites discussed repeating BP measurements if the first reading deviated from normal (high or low), but the staff did not cite standardized guidelines for when BP measurement should be repeated.
Workflow
Workflow refers to the series of activities, events, and interactions that occur during patient care in the clinic. Barriers to accurate BP measurement can occur during the check-in process at the front desk and continue through the actual BP measurement event.
A major concern expressed by practice managers and the staff was perceived lack of time, which impinges on the recommended 5-minute rest period before the initial BP measurement and the staff’s ability to focus on proper BP measurement technique. The rushed atmosphere was reflected in field observations, as some patients were not given the opportunity to rest quietly before BP measurement. The clinic staff expressed feeling pressured from physicians to room patients quickly in order to maintain the flow of patients through the clinic. Additionally, clinic staff face additional challenges with time constraints if a patient arrives late to the appointment, especially if insurance verification and routine paperwork have not been completed. Any delay only increases the time pressure to measure BP and complete other tasks (eg, verifying medications, allergies, and pharmacy information) before a patient is ready to be evaluated by the physician in the office.
Related to the problem of inadequate time was the practice of multitasking. The clinic staff felt burdened to accomplish many tasks in a short window of time to prepare the patient for the provider visit. While the BP device was obtaining the measurement, the clinic staff might talk with the patient about the chief complaint and recent medical history, update pharmacy information in the electronic health records, or take the patient’s temperature.
Clinic staff said that they tended to repeat BP measurements according to the preferences of the individual providers rather than follow a standardized protocol. Sometimes they had difficulty remembering what each provider wanted. For example, one physician might want the clinic staff to obtain a second BP measurement if the initial reading was 140/90 mm Hg or greater, while another provider might prefer to repeat the BP himself or herself.
Equipment and Layout
Proper BP measurement requires not only appropriate BP devices but also appropriate chairs with arm support. Field observations and focus group discussions revealed factors related to all types of equipment.
Across all clinic sites it was felt that BP devices on rolling stands expedited the BP measurement process and made it easier for clinic staff to follow the recommended BP procedures. But delays occurred when the devices were not immediately available due to battery issues or high patient volume. If only a limited number of BP devices were available, the staff would rush through the BP measurement in order to avoid causing delays for other patients.
The rolling stands had a basket for holding a thermometer and BP cuffs, and sometimes the staff used the basket to support the patient’s arm during BP measurement. However, the basket stood at a fixed height that may not be appropriate for all patients. Otherwise, clinic staff cited no uniform practice of using other surfaces for arm support. For patients with extremely thick or thin upper arms, it was sometimes difficult for staff to locate appropriately sized cuffs for BP measurement.
The site of BP measurement within the clinic also affected the quality of measurement. If the BP had to be measured in a busy triage area or hallway, the chaotic environment could affect the patient (eg, raise stress levels) or clinic staff (eg, feel rushed) during the measurement process. In some clinics, patients would have to walk down a long hallway before having their BP measured, causing concern whether the physical exertion would elevate the BP readings. Depending on the clinic layout and patient volume, the patient is sometimes seated on an exam table instead of a chair for BP measurement. This posed an inherent problem because there was no support for the patient’s arm, feet, or back.
Patient Characteristics and Behavior
Measurement of BP was affected by inherent characteristics and discrete behaviors of the patients. For example, staff reported that it was challenging to measure BP correctly for patients in wheelchairs or stretchers due to difficulty in maneuvering them into the correct position within cramped spaces. Elderly frail patients often found the cuff inflation to be painful.
There was a wide range of patient behaviors that the managers and clinic staff felt had an effect on BP measurement. The behaviors were not seen as purposeful efforts to disrupt BP measurement, but nonetheless had an effect. For example, patients would be anxious, fidget, cross their legs, or talk to the clinic staff or talking on the phone. Some patients would bring their children into the examination area, which served as a distraction during BP measurement. In the winter time, patients would wear multiple long sleeve layers, requiring more time and effort to bare their upper arm for the BP cuff. Many clinic staff do not always feel empowered enough or have time to enforce corrections.
Based on the concepts and themes uncovered during our evaluation, we traced out pathways that would feed into the BP measurement process. These are depicted in the fishbone diagram (Figure 1).
Figure 1.
Factors affecting office blood pressure measurement process.
Discussion
We found that the everyday task of measuring BP in the outpatient office setting is prone to error due to a variety of factors operating at multiple levels, some of which are beyond the control of the clinic staff who obtain the measurements. The predominant factors affecting BP measurement are grouped into themes related to staff knowledge and behavior, workflow, equipment and layout, and patient characteristics and behavior. Correct office BP measurement requires not only that clinical staff possess the underlying knowledge and skills, but that workflow, expectations of others, equipment, clinic layout, and patient factors align to support rather than impede the process. Disruption in any of those areas reduces the quality of BP measurement.
The main strength of the project was the in-depth evaluation of practices, attitudes, and concerns of clinic managers and staff responsible for office BP measurement. We observed behaviors during routine BP measurement and elicited perspectives of clinic managers and staff on the BP measurement process in the context of day-to-day operations.
A limitation was the inclusion of clinics from only one health care system. Clinics at other sites may be dealing with similar factors at different levels of intensity, or different factors entirely, although the latter is doubtful. Another limitation was that field observations of BP measurement were conducted on a convenience sample of patients. The presence of observers may have affected staff behavior. However, even while observed, clinic staff made errors. An additional limitation was that observations were conducted only for 1 day at each clinic.
Our findings add to the literature on BP measurement by illuminating underlying factors affecting adherence to recommended processes. In a survey of primary care practices in Utah, only 58% of clinics reported allowing patients to rest at least 5 minutes before measuring BP and only 59% reported using the mean of 2 measurements.14 Those authors acknowledged that because these were self-reported questionnaires, the figures probably overestimated adherence to recommendations. In a study in Veterans Affairs facilities, providers recorded a repeated BP value in only 45% of office visits.15 Other studies have demonstrated that incorrect BP measurement yields falsely high readings.10-12 For example, in a study of 444 veterans with uncontrolled HTN, there were substantial differences between routine office BP and research quality BP measurements, the latter of which involved taking 2 readings 5 minutes apart.12 The mean clinic systolic BP of 144.9 mm Hg (SD 16.9) was 15.5 mm Hg higher than mean research systolic BP of 129.4 mm Hg (SD 21.5). Only 28% of patients were classified as having controlled SBP (<140 mm Hg) by routine clinic measurement compared to 68% by research measurements.
An estimated 10% to 50% of patients with high office BP readings have normal BP outside the office.17 Improper measurement technique leading to falsely elevated BP measurements can lead to unnecessary initiation or escalation of BP medications with their attendant adverse effects and added costs.
Because clinical decisions are influenced by office BP readings, organizations should examine their BP measurement processes to identify areas for attention. In most settings, it is unlikely that a single approach will produce sustained improvement.18 Strategies that involve systems change, technology, and education may be the most promising. Education of staff is necessary but not sufficient. Proper BP measurement requires an estimated 7 more minutes than a casual measurement.13 Accommodations are needed to reduce this burden or minimize its impact on workflow. Ideally, multiple BP readings should be obtained for each patient. If this is not feasible, then at the very minimum, an initially high BP reading should be repeated.19 If clinic staff struggle to obtain multiple readings, the use of an automated office BP device (AOBP) should be considered,7 as was done in the SPRINT trial.6 With AOBP, the staff member activates the device and leaves the patient alone in the room. After a predetermined rest period, the device automatically obtains multiple readings at fixed intervals and presents the average, allowing staff to complete other tasks. The average of multiple readings obtained by AOBP is comparable to mean awake ambulatory BP.20,21 Clinics that use examination tables for BP measurement should be outfitted with chairs that support of the patient’s arms, back, and feet. Overall, a supportive organizational culture (eg, endorsement from managers and physicians) is needed to establish and maintain improvements in BP measurement.
Experts have called for a regulatory agency to monitor adherence to BP measurement standards.22 The ultimate beneficiaries of proper BP measurement (patients) may serve as the most compelling “regulatory” agents. Patient empowerment has been effective for increasing handwashing among health care workers23 and could be adapted to BP measurement. For example, patients could remind clinic staff to use an appropriately sized cuff and obtain multiple BP measurements.
Our study identified areas for future investigation. A stepped wedge cluster trial might be appropriate for clinic-level BP measurement interventions when consent or randomization by patient or staff member is not feasible.24 Possible evaluation approaches include video observation, use of standardized patients, and tracking outcomes through the electronic health record, such as documentation of multiple BP readings per office visit.
In conclusion, correct measurement of BP is affected by a wide range of factors and is challenging to accomplish consistently in a busy medical office. Considering the frequency of BP measurement and the impact of hypertension on morbidity and mortality, efforts are needed to maximize the quality of BP measurement in the outpatient setting.
Supplemental Material
Supplemental material, Hwang_Suppl_1_manager for Barriers to Accurate Blood Pressure Measurement in the Medical Office by Kevin O. Hwang, Aitebureme Aigbe, Hsiao-Hui Ju, Victoria C. Jackson and Emily W. Sedlock in Journal of Primary Care & Community Health
Supplemental Material
Supplemental material, Hwang_Suppl_2_focus_grp_(1) for Barriers to Accurate Blood Pressure Measurement in the Medical Office by Kevin O. Hwang, Aitebureme Aigbe, Hsiao-Hui Ju, Victoria C. Jackson and Emily W. Sedlock in Journal of Primary Care & Community Health
Author Biographies
Kevin O. Hwang is an associate professor of Medicine at UTHealth McGovern Medical School, Medical Director of the UT General Internal Medicine Center in the Texas Medical Center, and a member of the University of Texas at Houston-Memorial Hermann Center for Healthcare Quality and Safety. He is engaged in resident and student education, research, and quality improvement activities.
Aitebureme Aigbe, DrPH, MPH is a project specialist at the University of Texas at Houston–Memorial Hermann Center for Healthcare Quality and Safety. She earned her Bachelor’s degree in Biology from the University of Maryland. She completed graduate studies at Drexel University and received her Master’s degree in Public Health. She earned her Doctor of Public Health degree at the University of Texas.
Hsiao-Hui Ju, a board certified Family Nurse practitioner, has been serving as a primary care provider for six years. Her academic degrees include a Bachelor of Science in Nursing from Texas Woman’s University, a Master of Science in Nursing and a Doctor of Nursing Practice from The University of Texas Health Science Center in Houston.
Victoria C. Jackson is an internal medicine resident at UT Southwestern Medical Center. She earned her medical degree at UTHealth McGovern Medical School
Emily W. Sedlock is a project specialist at the University of Texas at Houston–Memorial Hermann Center for Healthcare Quality and Safety. Her areas of interest include patient safety event reporting, process improvement, and quality data analysis.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was provided in part by the University of Texas at Houston–Memorial Hermann Center for Healthcare Quality and Safety.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD: Kevin O. Hwang  https://orcid.org/0000-0002-2932-512X
https://orcid.org/0000-0002-2932-512X
References
- 1. GBD 2013 Risk Factors Collaborators; Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287-2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yoon SS, Fryar CD, Carroll MD. Hypertension Prevalence and Control Among Adults: United States, 2011-2014. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 3. Siu AL; US Preventive Services Task Force. Screening for high blood pressure in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778-786. [DOI] [PubMed] [Google Scholar]
- 4. Kronish IM, Kent S, Moise N, et al. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. J Am Soc Hypertens. 2017;11:573-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Drawz PE, Ix JH. BP measurement in clinical practice: time to SPRINT to guideline-recommended protocols. J Am Soc Nephrol. 2018;29:383-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. SPRINT Research Group; Wright JT, Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2017;71:e13-e115. [DOI] [PubMed] [Google Scholar]
- 8. Cohen JB, Townsend RR. The ACC/AHA 2017 hypertension guidelines: both too much and not enough of a good thing? Ann Intern Med. 2018;168:287-288. [DOI] [PubMed] [Google Scholar]
- 9. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1. Blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142-161. [DOI] [PubMed] [Google Scholar]
- 10. Burgess SE, MacLaughlin EJ, Smith PA, Salcido A, Benton TJ. Blood pressure rising: differences between current clinical and recommended measurement techniques. J Am Soc Hypertens. 2011;5:484-488. [DOI] [PubMed] [Google Scholar]
- 11. Houweling ST, Kleefstra N, Lutgers HL, Groenier KH, de Jong BM, Bilo HJ. Pitfalls in blood pressure measurement in daily practice. Fam Pract. 2006;23:20-27. [DOI] [PubMed] [Google Scholar]
- 12. Powers BJ, Olsen MK, Smith VA, Woolson RF, Bosworth HB, Oddone EZ. Measuring blood pressure for decision making and quality reporting: where and how many measures? Ann Intern Med. 2011;154:781-788. [DOI] [PubMed] [Google Scholar]
- 13. Ray GM, Nawarskas JJ, Anderson JR. Blood pressure monitoring technique impacts hypertension treatment. J Gen Intern Med. 2012;27:623-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Woolsey S, Brown B, Ralls B, Friedrichs M, Stults B. Diagnosing hypertension in primary care clinics according to current guidelines. J Am Board Fam Med. 2017;30:170-177. [DOI] [PubMed] [Google Scholar]
- 15. Kerr EA, Zikmund-Fisher BJ, Klamerus ML, Subramanian U, Hogan MM, Hofer TP. The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Ann Intern Med. 2008;148:717-727. [DOI] [PubMed] [Google Scholar]
- 16. Tong A, Sainsbury P, Craig J. Consolidated Criteria for Reporting Qualitative Research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349-357. [DOI] [PubMed] [Google Scholar]
- 17. Gorostidi M, Vinyoles E, Banegas JR, de la Sierra A. Prevalence of white-coat and masked hypertension in national and international registries. Hypertens Res. 2014;38:1-7. [DOI] [PubMed] [Google Scholar]
- 18. Nolan TW. Execution of Strategic Improvement Initiatives to Produce System-Level Results. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2007. [Google Scholar]
- 19. Einstadter D, Bolen SD, Misak JE, Bar-Shain DS, Cebul RD. Association of repeated measurements with blood pressure control in primary care. JAMA Intern Med. 2018;178:858-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Myers MG, Godwin M, Dawes M, et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. BMJ. 2011;342:d286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Myers MG, Valdivieso M. Evaluation of an automated sphygmomanometer for use in the office setting. Blood Press Monit. 2012;17:116-119. [DOI] [PubMed] [Google Scholar]
- 22. Appel LJ, Miller ER, 3rd, Charleston J. Improving the measurement of blood pressure: is it time for regulated standards? Ann Intern Med. 2011;154:838-840. [DOI] [PubMed] [Google Scholar]
- 23. McGuckin M, Taylor A, Martin V, Porten L, Salcido R. Evaluation of a patient education model for increasing hand hygiene compliance in an inpatient rehabilitation unit. Am J Infect Control. 2004;32:235-238. [DOI] [PubMed] [Google Scholar]
- 24. Hemming K, Haines TP, Chilton PJ, Girling AJ, Lilford RJ. The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ. 2015;350:h391. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Hwang_Suppl_1_manager for Barriers to Accurate Blood Pressure Measurement in the Medical Office by Kevin O. Hwang, Aitebureme Aigbe, Hsiao-Hui Ju, Victoria C. Jackson and Emily W. Sedlock in Journal of Primary Care & Community Health
Supplemental material, Hwang_Suppl_2_focus_grp_(1) for Barriers to Accurate Blood Pressure Measurement in the Medical Office by Kevin O. Hwang, Aitebureme Aigbe, Hsiao-Hui Ju, Victoria C. Jackson and Emily W. Sedlock in Journal of Primary Care & Community Health