Abstract
Importance:
Most prior studies of US dietary trends have evaluated broad macronutrient or selected dietary factors. Understanding national trends in multiple key foods/nutrients, and potential disparities in these trends, is crucial to identify challenges and opportunities to improve Americans’ diets.
Objective:
To characterize trends in key dietary factors related to major diseases or special public interest among US adults overall and by age, sex, race/ethnicity, education, and income.
Design, Setting & Participants:
Repeated cross-sectional investigation using up to two 24-hour dietary recalls per participant in nationally representative samples including 33,929 non-institutionalized US adults from 7 consecutive National Health and Nutrition Examination Survey (NHANES) cycles between 1999 and 2012.
Exposures:
Calendar year; and subgroups of age, sex, race/ethnicity, education, and income.
Main outcomes:
Survey-weighted, energy-adjusted mean consumption of 30 food groups and 15 nutrients; and the proportion of adults meeting specific dietary recommendations for key factors.
Results:
Between 1999–2012, several improvements were identified (P-trend<0.01 each), including increases in nuts/seeds (58.8% greater intake), yogurt (+68.3%), whole-grains (+77.0%), whole fruit (+25.7%), dark-green vegetables (+34.9%), red/orange vegetables (+22.8%), fiber (+16.6%), and polyunsaturated fat (+14.9%); and decreases in sugar-sweetened beverages (−28.3%), added sugars (−21.6%), and white potatoes (−17.2%). Over this same period, 100% fruit juice (−25.9%) and milk (−21.6%) decreased, while cheese (+27.5%) and calcium (+20.1%) increased. The proportion of adults eating ≥1 serving/d of whole fruit increased from 17.6% to 21.5%; ≥1 serving/d of whole grains, from 12.5% to 31.6%; and ≥5 servings/wk of nuts/seeds, from 20.2% to 30.8% (P-trend<0.001 each). Many disparities were identified, especially by race/ethnicity, education, and income; and certain disparities worsened (P-interaction<0.05 each), such as greater increases in whole fruits and nuts/seeds among higher income and more educated Americans; decreases in seafood omega-3s for non-Hispanic blacks; and increases in refined grains and sodium among Mexican-Americans.
Conclusions and Relevance:
Significant changes in the American diet have occurred over the last 14 years, including specific improvements yet also other dietary factors with little improvement as well as persistent or worsening disparities over time. These novel findings inform specific emerging successes, relative failures, and corresponding opportunities to improve the diet for all Americans.
Keywords: Adults, diet, diet quality, chronic disease, nutrition surveys, diet surveys, National Health and Nutrition Examination Survey, NHANES
INTRODUCTION
Suboptimal diet is among the leading causes of poor health, particularly related to adverse affects on obesity, diabetes, cardiovascular diseases, and diet-related cancers.1,2 In the US, dietary factors are estimated to account for over 650,000 deaths annually and 14% of all disability-adjusted life years lost in 2010.1 Understanding trends in diet is crucial to inform priorities and policies to improve diets and reduce diet-related illness. In addition, identifying how such trends vary according to specific subgroups is essential to evaluate prevalent, worsening, and potentially improving disparities and inform corresponding intervention strategies. However, most investigations to-date on US dietary trends have focused on a limited number of factors, such as total energy, broad macronutrients, summary diet measures, or a few selected items (e.g., sugar-sweetened beverages [SSBs], added sugars, meat).3–7 Thus, the trends and corresponding disparities across a full range of dietary factors linked to major health outcomes are not well-established. In addition, prior investigations have generally not evaluated relevant subclasses of foods, such as subtypes of whole-grains, fruits, and vegetables, which can reveal important underlying trends in consumption.
To address these major knowledge gaps, we used data from 7 consecutive 2-year cycles of the National Health and Nutrition Examination Survey (NHANES) between 1999–2012 to examine temporal trends in dietary intakes of American adults overall and by age, sex, race/ethnicity, education, and income.
METHODS
Data source, study population & dietary assessment
Our investigation utilized dietary data from American adults ≥20y completing at least one valid 24-hour recall, as determined by National Center for Health Statistics (NCHS) criteria, during 7 two-year cycles of NHANES from 1999–2000 through 2011–12. The survey was approved by the NCHS ethics review board, and all participants provided written informed consent.
All examined participants were eligible for dietary assessment, consisting of one or two 24-hour dietary recalls in which respondents reported all foods and beverages consumed the previous day, midnight to midnight. The protocol and data collection methods are fully documented.8 NHANES interviewers and recalls were monitored with established criteria to evaluate data acceptability. For our investigation focused on population results, the one-day value was used for individuals with single recalls (n=11,721), and two-day means for those with two recalls (n=22,211). For large samples, means of either a single or multiple recalls provides unbiased estimates of the population mean.9
Food groups and nutrients
We evaluated foods/nutrients linked to major health outcomes as well as those of current policy or general public interest.10–22 Table S1 specifies the definitions and serving sizes for each food group. We utilized the USDA Food Patterns Equivalents Database and MyPyramid Equivalents Database, 3,23 which disaggregates mixed foods into their component parts (e.g., a cheeseburger contributes unprocessed red meat, cheese, and refined grains). Overall food groups (e.g. vegetables) were further disaggregated to elucidate within-category trends (e.g., dark-green vegetables vs. potatoes). Nutrients were derived from cycle-specific versions of the Food and Nutrient Database for Dietary Studies.24 Intakes of all dietary factors were energy-adjusted using the residual method9 to evaluate trends independent of the small declines in energy intake during this time period25 (which could relate to changes in nondietary factors such as physical activity) and, more importantly, to minimize measurement error in dietary estimates.9
Population subgroups
To evaluate differences or disparities in trends, findings were stratified by age (20–34, 35–49, 50–64, ≥65y), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican-American), education (<high school graduate, high school graduate/equivalent, some college, ≥college), and family income-to-poverty ratio (<1.3, 1.3–1.84, 1.85–2.99, and ≥3), representing the ratio of family income, adjusted for family size, to the federal poverty level. Race/ethnicity-specific results are presented for Mexican-Americans as opposed to all Hispanics due to changes in sampling of other Hispanics over this time period.
Statistical analysis
We estimated nationally representative population mean intakes for each dietary factor across each of the 7 NHANES cycles. As all individuals completed the first recall, first-day survey weights were used to account for the complex sampling design. The statistical significance of trends was assessed by treating survey year as a continuous variable in a survey-weighted linear regression model. To assess statistical heterogeneity of trends by subgroups, a survey-weighted Wald test was used to test for an interaction term between year and categorical variables (age, gender, race/ethnicity) or ordinal variables (income, education). To assess whether observed trends were driven by demographic shifts, sensitivity analyses adjusted for age and race/ethnicity within each cycle, evaluating statistically significant trend coefficients before and after adjustment and quantifying the percent change in the coefficient.
To place the results within the context of dietary recommendations, we also evaluated the proportion of US adults meeting specific cutpoints for key dietary factors, such as from the 2015 Dietary Guidelines for Americans, Dietary Reference Intakes, Recommend Daily Values, American Heart Association recommendations, and Global Burden of Disease optimal intakes.21,22,26,27 For some foods without clear benchmarks, we utilized a logical integer cutpoint (e.g., 1 serving/d for cheese). To estimate intake distribution, we utilized the established National Cancer Institute (NCI) method to estimate the percent of the population at a specified cutpoint (see Online Supplemental Materials). 28–30
Analyses used Stata 13.1 (College Station, TX) and SAS 9.3 (Cary, NC), two-sided alpha-level=0.05.
RESULTS
In this nationally representative sample of 33,932 American adults, the average response rate was 73.6% (range: 67.4% in 2011–2012 to 78.3% in 2001–2002). Participant demographics by survey cycle are provided in Table S2.
National trends in diet
Detailed national trends from 1999–2000 to 2011–2012 in consumption of key foods and nutrients are presented in Table S3. All trends described below as “increasing”, “decreasing”, or similar terminology were statistically significant (p-trend<0.05).
While total fruit consumption was stable, whole fruit increased by 25.7% (+0.15 servings/d), while 100% fruit juice decreased by 25.9% (−0.11 servings/d) (Figure 1). Similarly, while no change was evident in total vegetables, consumption of dark-green leafy vegetables (e.g., kale/broccoli) and red/orange vegetables (e.g., carrot/red pepper) increased by 34.9% and 22.8% respectively (0.04 and 0.02 servings/d), while consumption of white potatoes (including fried potatoes) decreased by 17.2% (0.07 servings/d). Excluding starchy vegetables (e.g., potatoes, corn, peas), vegetable consumption increased non-significantly by 9.1%, or 0.10 servings/d (P-trend=0.056).
Figure 1.
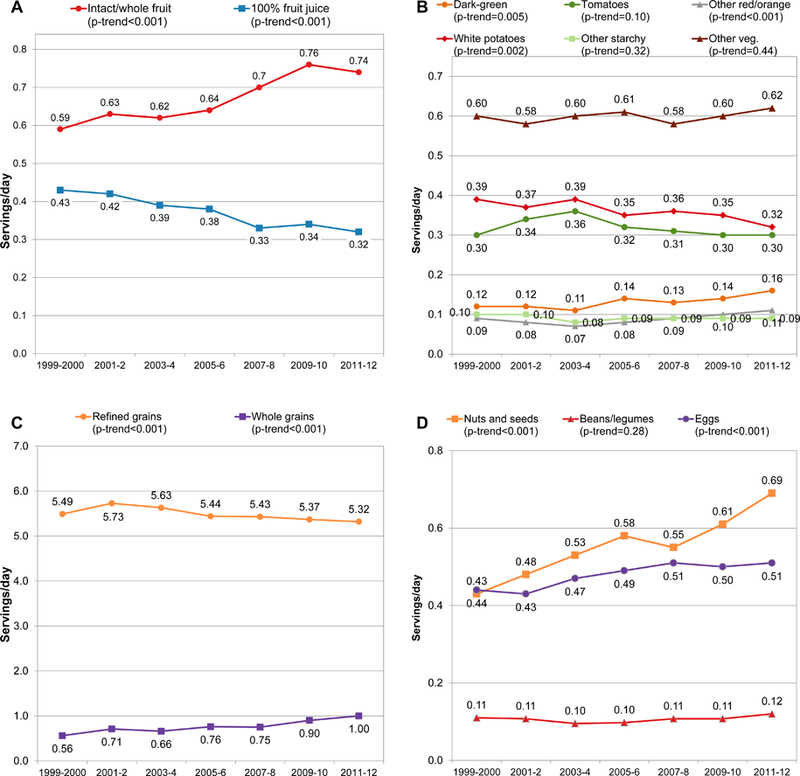
Trends in mean consumption of fruits (Panel A), vegetables (Panel B), grains (Panel C), and nuts/seeds, legumes and eggs (Panel D) among US adults, based on NHANES data from 1999 to 2012. All values energy-adjusted to 2000 kcal/d using the residual method. Serving sizes: fruits, vegetables, legumes: 1 cup; grains, nuts/seeds, eggs: 1-oz equivalents.
From 1999–2000 to 2011–2012, whole-grain consumption increased by 77.0% (from 0.56 to 1.00 servings/d), while refined grain consumption slightly declined from 5.49 to 5.32 servings/d (Figure 1). Nut consumption increased by almost 60% (+0.25 servings/d), and egg consumption by 16.0% (+0.07 servings/d). No change in legume consumption was evident.
Among meats, intakes of both unprocessed red and processed meats were stable, while intake of poultry increased by 9.8% (0.37 to 0.41 servings/d) (Figure 2). Seafood consumption increased by 16.0% (0.16 to 0.19 servings/d), largely due to greater intake of white fish/shellfish lower in omega-3’s (<500 mg per 3 oz).
Figure 2.
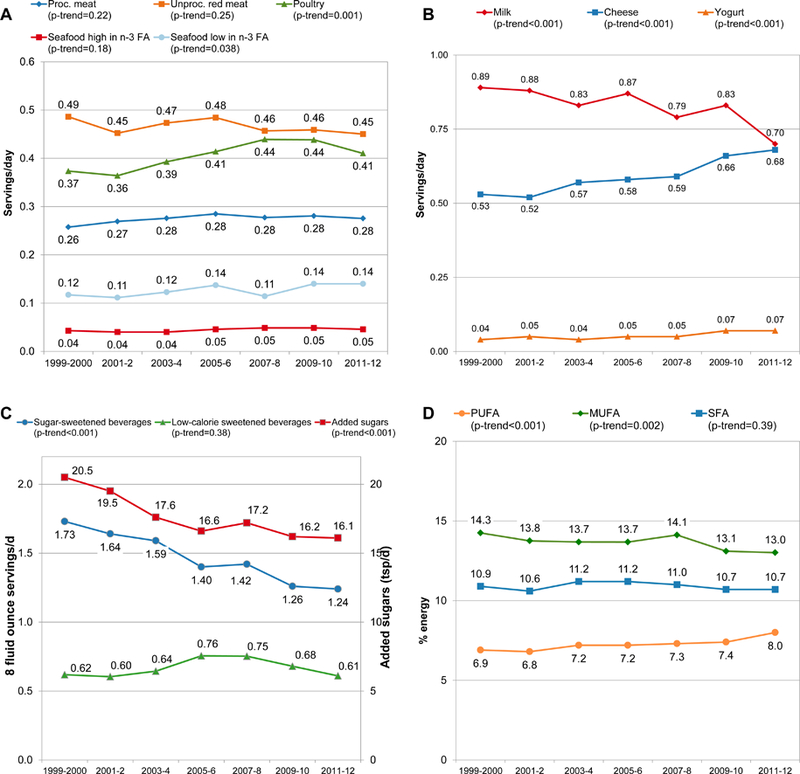
Trends in mean consumption of meats and seafood (Panel A), dairy (Panel B), added sugars, sugar-sweetened beverages, and low/non-calorie sweetened beverages (Panel C), and dietary fats (Panel D) among US adults, based on NHANES data from 1999 to 2012. Values in Panels A-C are energy-adjusted to 2000 kcal/d using the residual method. Serving sizes: meats, seafood: 3.5-oz equivalents; dairy: 1 cup; sugar-sweetened or low-calorie beverages: 8 fluid oz. PUFA=polyunsaturated fatty acid, MUFA=monounsaturated fatty acid, SFA=saturated fatty acid.
Intake of total dairy was stable, yet with notable heterogeneity by subclass (Figure 2). Milk consumption decreased by 21.6% (0.19 servings/d), while cheese and yogurt increased by 27.5% and 68.3%, respectively (+0.15 and +0.03 servings/d). SSB intake decreased by 28.3% (−0.49 servings/d), while intakes of low/non-caloric sweetened beverages were stable overall. Consistent with reduced SSBs, intake of added sugars decreased by 21.6% (−4.4 tsp/d).
Consumption total fat and saturated fat remained stable (Figure 2). Intake of polyunsaturated fat increased by 15% (from 6.9 to 8.0% energy [E]); while monounsaturated fat intake declined by 4.6% (from 14.3 to 13.0%E). Protein intake slightly increased (from 15.4 to 15.8%E), while carbohydrate intake decreased (from 50.7 to 49.1%E) (Table S3). While no change was evident for seafood omega-3 fats, plant omega-3 fats increased by 23.4%, from 134 to 166 mg/d. Increased intakes were also evident for dietary fiber (+16.6%; +2.5 g/d) and calcium (+20.1%; +158 mg/d). Between 1999–2000 and 2011–12, intakes of sodium and potassium were relatively stable.
We further evaluated changes in subtypes of SSBs, nut/seeds and whole-grains (Supplemental Figure 1). The decline in SSBs was largely due to decreased soda/carbonated soft drinks and, to a lesser extent, fruit drinks. Intake of presweetened iced tea was stable, while intake of sports/energy drinks increased. Increases in nuts/seeds were largely attributable to increased peanut butter (+78%; 0.08 to 0.14 servings/d) and tree nuts/seeds (+147%; 0.11 to 0.27 servings/d). Increases in whole-grains were largely driven by increases in whole-grain yeast breads (from 0.14 to 0.38 serving/d) and other whole-grain foods, e.g., pasta/pasta mixed-dishes and crackers (from 0.10 to 0.21 serving/d).
The overall proportional changes in intakes of these foods and nutrients are shown in Figure 3 and Table S3.
Figure 3.
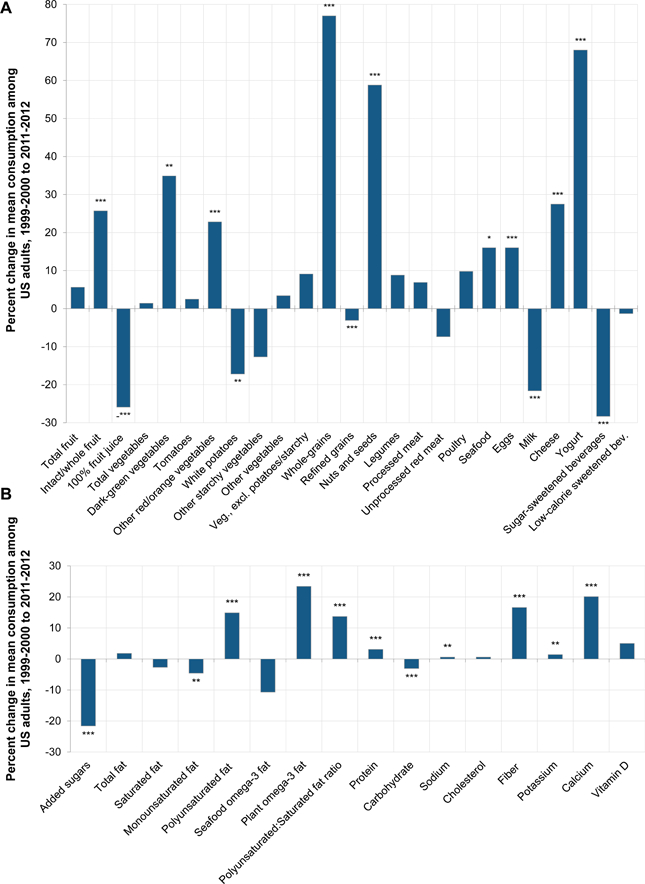
Percent change in intake of food groups (Panel A) and nutrients of interest (Panel B). Analyses are based on energy-adjusted values to 2000 kcal/d using the residual method. * p-trend<0.05; ** p-trend<0.01; *** p-trend<0.001
Proportions of US adults meeting recommendations
We also evaluating trends based on proportions of Americans meeting identified recommended cutpoints (Figure 4, Figure S2, Table S4). For example, the proportion of adults eating ≥2.5 servings/d of vegetables remained stable, but the proportion eating ≥1.8 servings/d of non-starchy vegetables increased by 23.4% (from 12.4% to 15.3%). The proportion eating ≥1 serving/d of whole fruit increased by 22.2%, from 17.6% to 21.5%. The proportion meeting recommendations for whole grains (3+ servings/d) increased but remained very low at 1.6%; as an alternative cutpoint, the proportion consuming at least 1.0 serving/d of whole grains increased 2.5-fold, from 12.5% in 1999–2002 to 31.6% in 2009–2012. The proportion of adults eating at least 5 servings/wk of nuts/seeds increased by 52.5%, from 20.2% to 30.8%. The proportion of adults meeting recommended intakes for seafood and calcium also increased. For foods/nutrients with recommended limits on consumption, improvements were evident for SSBs, added sugars, refined grains, and saturated fat. Changes were not evident for processed meats or sodium.
Figure 4.
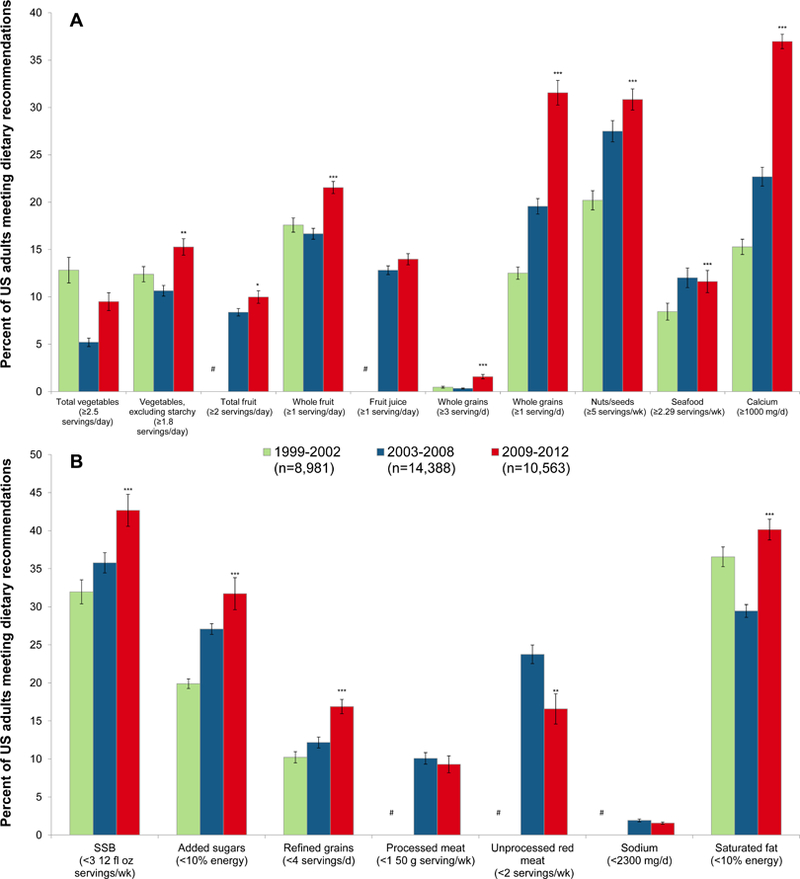
Trends in the proportion of US adults meeting dietary recommendations, based on NHANES data from 1999 to 2012. Recommendation levels are provided and are based on the 2015 Dietary Guidelines for Americans (for total vegetables, vegetables excluding starchy vegetables, total fruit, whole-grains, refined grains, nuts/seeds, seafood, calcium, added sugars, sodium and saturated fat; the American Heart Association 2020 Strategic Impact Goals (sugar-sweetened beverages; the Global Burden of Diseases study optimal intake levels (unprocessed red meat, processed meat); and pragmatic or alternative cutpoints (whole fruit, fruit juice, whole-grains [1+ serving]). Analyses are based on energy-adjusted values to 2000 kcal/d using the residual method. Serving sizes: fruits, vegetables: 1 cup; grains, nuts/seeds: 1-oz equivalents; meats, seafood: 3.5-oz equivalents. * p-trend<0.05; ** p-trend<0.01; *** p-trend<0.001; # 1999–2002 estimates could not be reliably imputed by the NCI method (see Supplemental Materials for details).
When we evaluated trends in proportions of US adults meeting American Heart Association 2020 Goals criteria for poor, intermediate, or ideal dietary quality (continuous scoring system; Table S5), the proportion with a poor diet decreased from 50.3 to 41.0%, the proportion with an intermediate diet increased from 49.0 to 57.5%, and the proportion with an ideal diet increased from 0.7 to 1.5% (P-trend≤0.003 each) (Table S6, Figure S3).
Sensitivity analyses adjusting for demographic changes
Findings for most dietary factors were not materially altered by adjustment for changes in population demographics over time (e.g., such as population aging and a relative decrease in the percentage of non-Hispanic whites) (Table S7). Some exceptions included potassium, sodium, and seafood, for which observed increased intakes over time were partly attenuated after accounting for demographic changes (with relative attenuations of 33.2%, 24.3%, and 24.0%, respectively). In addition, for a few foods, the observed trends in intakes were strengthened following adjustment for demographic changes; examples included total dairy and cheese (+38.1% and +17.5% greater increase, respectively).
Disparities in trends according to population subgroups
Many differences in intakes by age, race/ethnicity, education, and income were relatively stable over time, such as for total vegetables, whole-grains, unprocessed red meat, and milk (Table S8–12). For each of these foods, intakes were higher among Americans of higher vs. lower socioeconomic status, and among non-Hispanic whites vs. non-Hispanic blacks or Mexican-Americans. In contrast, for other factors we identified changes in trends by population subgroups. For instance, national trends in consumption of nuts/seeds were highly variable depending on education (P-interaction<0.001) (Figure 5): no change was evident among Americans with <high school education, and progressively larger increases were seen with greater education; findings were similar by income (Table S12). Trends in both whole fruit and 100% fruit juice also varied by income (p-interaction<0.05 each), with largest increases in whole fruit and declines in 100% fruit juice among those with higher-income. SSB consumption decreased in all age groups, but with the largest declines among youngest adults (P-interaction<0.001).
Figure 5.
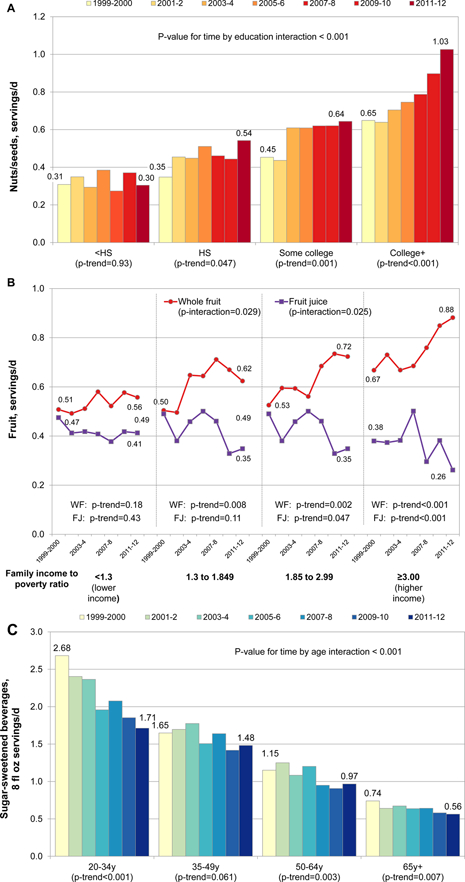
Trends in mean consumption of nuts/seeds by education (Panel A), fruit by family income (Panel B) and sugar-sweetened beverages by age (Panel C) among US adults, based on NHANES data from 1999 to 2012. All values are energy-adjusted to 2000 kcal/d using the residual method. Serving sizes: nuts/seeds: 1-oz equivalent; fruit: 1 cup; sugar-sweetened beverages: 8 fluid oz.
Specific differences in trends were also evident by race/ethnicity (Figure S4-S5, Table S10). For example, refined grain consumption decreased among non-Hispanic whites (−0.33 servings/d) and non-Hispanic blacks (−0.28 servings/d), but increased among Mexican-Americans (+0.76 servings/d) (P-interaction<0.001). Sodium intake remained stable among non-Hispanic whites, but increased among non-Hispanic blacks and especially Mexican-Americans (P-interaction=0.01). Seafood omega-3 consumption was stable among non-Hispanic whites and Mexican-Americans, but decreased among non-Hispanic blacks (P-interaction<0.001). Intake of white potatoes decreased among non-Hispanic whites and Mexican-Americans, but increased among non-Hispanic blacks (P-interaction=0.002).
DISCUSSION
Based on nationally representative data between 1999–2000 and 2011–2012, many aspects of the American diet have improved. Noteworthy changes include increases in whole fruit, whole-grains, nuts/seeds, and yogurt; and decreases in SSBs, added sugars, white potatoes, and refined grains, and 100% fruit juice. Consistent with these trends, we found that Americans have increased their intakes of dietary fiber, calcium, protein, total polyunsaturated fat, and plant omega-3 fat, while reducing their carbohydrate consumption. In comparison, changes in consumption of processed meats, unprocessed red meats, and legumes were not evident. To the best of our knowledge, our novel findings represent the most comprehensive evaluation of contemporary trends in multiple relevant dietary habits among US adults.
Despite observed improvements, small numbers of Americans are attaining recommended levels of most dietary factors. For example, fewer than 1 in 6 adults are consuming sufficient vegetables, fruits, or seafood; and fewer than 1 in 50 are consuming sufficient whole grains. With reductions in SSB intake, nearly 1 in 2 adults is now at or below recommended levels. Yet, less than 1 in 3 is at or below recommended levels for added sugars; less than 1 in 5 at or below recommended levels for refined grains, processed meats, or unprocessed red meats; and less than 1 in 40 at or below recommended levels for sodium. Thus, while many trends are encouraging, much room for improvement remains.
While many of these dietary changes may have implications for health, in particular risk of chronic diseases, estimation of such health effects was beyond the scope of our present investigation. Ecologically, these dietary improvements coincide with continued population (non-drug-treatment) reductions in high blood pressure, dyslipidemia, and cardiovascular mortality;27,31 as well as potential plateauing of obesity. Our results provide relevant data for future analyses to estimate the potential health effects of the identified trends. Several of the observed mean changes in intakes appeared relatively small when considered as daily servings, such as trends in yogurt, dark-green and red-orange vegetables, poultry, seafood, and refined grains. Yet, many of these foods are consumed more occasionally, rather than daily; and small changes in average daily intake sum to more meaningful changes in weekly or monthly consumption. In addition, given low baseline intakes of many healthful foods, modest absolute changes can represent larger relative changes, elucidating emerging dietary trends. Most importantly, small mean changes across an entire population can substantially influence the overall exposure distribution and corresponding risk in that population.32 Consistent with this premise, we identified meaningful changes in proportions of Americans meeting recommendations for several dietary factors of interest.
While identifying drivers of some the observed dietary changes can be challenging, a number of factors likely contributed. For example, both the federal government and advocacy organizations have organized educational campaigns emphasizing the benefits of fruits and vegetables.33–37 Accumulating scientific evidence over this time period has documented clear health benefits of nuts/seeds, polyunsaturated fats, and yogurt;11,14,38 this also led to an FDA-approved qualified health claim for nuts in 2003.14,38–40 Hazards of SSBs have also been documented11,41 and emphasized by policy efforts and media,42–45 likely contributing to decreased intakes; and Americans appear to have even responded to concerns about excessive intakes of 100% fruit juice. Conversely, intakes of sports and energy drinks increased, suggesting that media, advocacy, and policy efforts have less successfully linked these sugar drinks with other SSBs. Harms of refined grains and white potatoes, rich in rapidly digested carbohydrates; and reciprocal potential benefits of whole grains; have also garnered substantial attention; likely influencing national trends. Interestingly, while many popular books and social media have focused on the low-fat vs. low-carb (Atkins, Paleo) debate,46,47 little to no changes were seen in overall fat or carbohydrate intake; instead, Americans appear to be reflecting guidance to not target total fat or carbohydrate intake, but shift from less healthful food sources of carbs and fats toward more healthful food sources of carbs and fats. This is consistent with growing consensus48 that effective dietary guidance should be food-based while also emphasizing increased healthful foods rather than only elimination of certain unhealthful foods. In sum, it appears that progress in nutrition science and increased advocacy efforts are at least partly influencing public (and potentially food industry) choices about what to eat.
Our investigation identified important trends among demographic subgroups. In particular, we found little evidence that dietary disparities improved over this 14-year period, while some actually worsened. For instance, increases in whole fruit and nut/seed consumption were notably larger among higher income and higher educated Americans; intakes of refined grains and sodium increased among Mexican-Americans; and intakes of seafood omega-3’s decreased among non-Hispanic blacks. These results suggest persistent and in some cases worsening disparities in specific US dietary habits among vulnerable populations. Our novel findings highlight the need to understand and address reasons for these differences. In a positive light, for certain items such as SSBs and whole-grains, comparable improvements were observed across socioeconomic and race/ethnicity strata. Careful evaluation of population-specific facilitators and barriers to altering intakes of particular foods is essential to crafting tailored approaches to improving diets.
Prior analyses of US dietary trends have focused on a limited number of dietary factors or overall summary measures (e.g., Alternative Healthy Eating Index).3,49,50 Where overlap exists (e.g. added sugars, SSBs), our findings are consistent with prior reports.3,7,51
Our investigation has several strengths. We utilized the most recent nationally representative data available, providing an up-to-date portrait of the American diet. We evaluated multiple relevant food groups and nutrients, including subtypes, providing a detailed and comprehensive assessment. We simultaneously evaluated multiple food groups and nutrients using consistent methods, facilitating comparisons across dietary factors. We assessed potential differences in intakes and trends by key population subgroups, allowing characterization of persistent and increasing disparities. Sensitivity analyses incorporated changes in national demographics, which did not explain the observed trends.
Potential limitations should be considered. As with any population measure, dietary information is subject to random and systematic error. We took advantage of multiple, interviewer-administered, 24-hour recalls and further adjusted for total energy, each of which reduce measurement error. While subtle systematic bias in reporting over time cannot be excluded, it seems unlikely that such biases would be observed across the entire population for all of the dietary factors we evaluated. A number of statistical tests were performed, meaning that some significant trends may be false-positives. NHANES data by geographic region are not publically available nor representative due to sampling, so we did not assess region-specific findings. Our findings do not provide explanations for the observed dietary trends; newly launched national surveys, such as the National Household Food Acquisition and Purchase Survey, should help facilitate future evaluations.52
CONCLUSION
In conclusion, we identified evidence for significant changes in the American diet over the last 14 years, including several improvements. We also identified key dietary factors with little improvement, and others with persistent or even worsening disparities over time. These novel findings inform specific emerging successes, relative failures, and corresponding opportunities for robust public health nutrition policy to continue to improve the US diet for all Americans.
Supplementary Material
ACKNOLWEDGEMENTS
This work was supported by the National Heart, Lung, and Blood Institute, NIH (5R01HL115189). The funder had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. Dr. Mozaffarian reports ad hoc honoraria or consulting from Bunge, Haas Avocado Board, Amarin, Astra Zeneca, Boston Heart Diagnostics, GOED, and Life Sciences Research Organization; chapter royalties from UpToDate; and scientific advisory boards, Unilever North America (ended 2014) and Elysium Health.
Footnotes
Other authors report no conflicts of interest.
References
- 1.Murray CJ, Atkinson C, Bhalla K, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA 2013;310(6):591–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009;6(4):e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang DD, Leung CW, Li Y, et al. Trends in Dietary Quality Among Adults in the United States, 1999 Through 2010. JAMA Intern Med 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slining MM, Mathias KC, Popkin BM. Trends in food and beverage sources among US children and adolescents: 1989–2010. J Acad Nutr Diet 2013;113(12):1683–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr 2013;98(1):180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daniel CR, Cross AJ, Koebnick C, Sinha R. Trends in meat consumption in the USA. Public Health Nutr 2011;14(4):575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr 2011;94(3):726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Health and Nutrition Examination Survey. MEC In-Person Dietary Interviewers Procedures Manual Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/DietaryInterviewers_Inperson.pdf. Accessed September 28, 2014.
- 9.Willett W Nutritional epidemiology Third edition. ed. Oxford ; New York: Oxford University Press; 2013. [Google Scholar]
- 10.Chowdhury R, Warnakula S, Kunutsor S, et al. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med 2014;160(6):398–406. [DOI] [PubMed] [Google Scholar]
- 11.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. New Engl J Med 2011;364(25):2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010;121(21):2271–2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr 2006;136(10):2588–2593. [DOI] [PubMed] [Google Scholar]
- 14.Afshin A, Micha R, Khatibzadeh S, Mozaffarian D. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta-analysis. Am J Clin Nutr 2014;100(1):278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mozaffarian D, Lemaitre RN, Kuller LH, Burke GL, Tracy RP, Siscovick DS. Cardiac benefits of fish consumption may depend on the type of fish meal consumed: the Cardiovascular Health Study. Circulation 2003;107(10):1372–1377. [DOI] [PubMed] [Google Scholar]
- 16.Cho SS, Qi L, Fahey GC Jr., Klurfeld DM. Consumption of cereal fiber, mixtures of whole grains and bran, and whole grains and risk reduction in type 2 diabetes, obesity, and cardiovascular disease. Am J Clin Nutr 2013;98(2):594–619. [DOI] [PubMed] [Google Scholar]
- 17.Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol 2013;28(11):845–858. [DOI] [PubMed] [Google Scholar]
- 18.He K, Song Y, Daviglus ML, et al. Accumulated evidence on fish consumption and coronary heart disease mortality: a meta-analysis of cohort studies. Circulation 2004;109(22):2705–2711. [DOI] [PubMed] [Google Scholar]
- 19.Huang C, Huang J, Tian Y, Yang X, Gu D. Sugar sweetened beverages consumption and risk of coronary heart disease: a meta-analysis of prospective studies. Atherosclerosis 2014;234(1):11–16. [DOI] [PubMed] [Google Scholar]
- 20.He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev 2013;4:CD004937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(10010):2287–2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2015–2020. 8th Edition, Washington, DC. . [Google Scholar]
- 23.Marriott BP, Cole N, Lee E. National estimates of dietary fructose intake increased from 1977 to 2004 in the United States. J Nutr 2009;139(6):1228S–1235S. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Agriculture, Agricultural Research Service. 2014. USDA Food and Nutrient Database for Dietary Studies 2011–2012. Food Surveys Research Group Home Page, http://www.ars.usda.gov/ba/bhnrc/fsrg.
- 25.Ford ES, Dietz WH. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr 2013;97(4):848–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Food and Drug Administration. Guidance for Industry: A Food Labeling Guide (14. Appendix F: Calculate the Percent Daily Value for the Appropriate Nutrients) Available at: http://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm064928.htm. Accessed 14 January 2016.
- 27.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics−−2015 update: a report from the American Heart Association. Circulation 2015;131(4):e29–322. [DOI] [PubMed] [Google Scholar]
- 28.Tooze JA, Kipnis V, Buckman DW, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med 2010;29(27):2857–2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kipnis V, Midthune D, Buckman DW, et al. Modeling data with excess zeros and measurement error: application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics 2009;65(4):1003–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dodd KW, Guenther PM, Freedman LS, et al. Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc 2006;106(10):1640–1650. [DOI] [PubMed] [Google Scholar]
- 31.Kuklina EV, Carroll MD, Shaw KM, Hirsch R. Trends in high LDL cholesterol, cholesterol-lowering medication use, and dietary saturated-fat intake: United States, 1976–2010. NCHS Data Brief 2013(117):1–8. [PMC free article] [PubMed] [Google Scholar]
- 32.Rose G Sick individuals and sick populations. Int J Epidemiol 2001;30(3):427–432. [DOI] [PubMed] [Google Scholar]
- 33.Levine E, Abbatangelo-Gray J, Mobley AR, McLaughlin GR, Herzog J. Evaluating MyPlate: an expanded framework using traditional and nontraditional metrics for assessing health communication campaigns. J Nutr Educ Behav 2012;44(4):S2–12. [DOI] [PubMed] [Google Scholar]
- 34.United States. Department of Health and Human Services., United States. Department of Agriculture., United States. Dietary Guidelines Advisory Committee. Dietary guidelines for Americans, 2010. 7th ed. Washington, D.C.: G.P.O.; 2010. [Google Scholar]
- 35.United States. Department of Health and Human Services., United States. Department of Agriculture, United States. Dietary Guidelines Advisory Committee. Dietary guidelines for Americans, 2005. 6th ed. Washington, D.C.: G.P.O.; 2005. [Google Scholar]
- 36.United States Department of Agriculture. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Revisions in the WIC Food Packages 7 CFR Part 246. Available at: http://www.fns.usda.gov/sites/default/files/wicfoodpkginterimrulepdf.pdf. Accessed 8 September 2015.
- 37.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]
- 38.Bao Y, Han J, Hu FB, et al. Association of nut consumption with total and cause-specific mortality. N Engl J Med 2013;369(21):2001–2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith LP, Ng SW, Popkin BM. Trends in US home food preparation and consumption: analysis of national nutrition surveys and time use studies from 1965–1966 to 2007–2008. Nutr J 2013;12:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Estruch R, Ros E, Salas-Salvado J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368(14):1279–1290. [DOI] [PubMed] [Google Scholar]
- 41.Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 2004;292(8):927–934. [DOI] [PubMed] [Google Scholar]
- 42.Gostin LO, Reeve BH, Ashe M. The historic role of boards of health in local innovation: New York City’s soda portion case. JAMA 2014;312(15):1511–1512. [DOI] [PubMed] [Google Scholar]
- 43.Pomeranz JL, Chriqui JF. The Supplemental Nutrition Assistance Program: Analysis of Program Administration and Food Law Definitions. Am J Prev Med 2015;49(3):428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization. Guideline: Sugars intake for adults and children. World Health Organization; 2015. [PubMed] [Google Scholar]
- 45.Food Labeling: Revision of the Nutrition and Supplement Facts Labels; Supplemental Proposed Rule To Solicit Comment on Limited Additional Provisions Available at: https://www.federalregister.gov/articles/2015/07/27/2015-17928/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels-supplemental-proposed-rule-to. Accessed 4 November 2015.
- 46.Food Marketing Institute. US Grocery Shopping Trends 2014 Available at: http://www.fmi.org/docs/default-source/research/presentation.pdf?sfvrsn=0 Accessed 14 January 2015. .
- 47.Experian Marketing Services. The Paleo diet is top 2013 diet search Available at: http://www.experian.com/blogs/marketing-forward/2013/01/08/the-paleo-diet-is-top-2013-diet-search/ Accessed 10 January 2016.
- 48.Committee DGA. Scientific Report of the 2015 Dietary Guidelines Advisory Committee Washington (DC): USDA and US Department of Health and Human Services; 2015. [Google Scholar]
- 49.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 2012;142(6):1009–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet 2013;113(4):569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet 2013;113(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tselepidakis E, Kirlin JA. USDA Economic Research Service-FoodAPS National Household Food Acquisition and Purchase Survey 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


