Abstract
The current study investigated the mechanisms through which a parenting intervention for military families fosters positive peer adjustment in children. A sample of 336 families with a history of parental deployment enrolled in a randomized controlled trial of the After Deployment Adaptive Parenting Tools (ADAPT) preventive intervention. ADAPT is a 14-week preventive intervention designed to strengthen parenting in military families. The intervention was associated with improvements in mother’s and father’s parental locus of control (i.e., a more internal locus of control) at a 6-month follow-up assessment while controlling for baseline levels. Mothers’ parental locus of control was positively associated with improvements in children’s peer adjustment 12 months following the intervention while controlling for baseline peer adjustment. A significant indirect effect revealed that participation in ADAPT resulted in improved 12-month peer adjustment by improving mothers’ parental locus of control. Implications for supporting youth resilience to stressors associated with deployment are discussed.
Keywords: Military deployment, peer adjustment, parental locus of control, parenting intervention
The United States is in the midst of one of the longest wartime periods in the country’s history. This prolonged period of conflict has resulted in unparalleled deployment of National Guard and Reserve forces. Families coping with deployment face an evolving set of stressors during different stages of deployment process for both active duty and reserve forces. Stages of deployment are commonly described as pre-deployment, deployment, and reintegration (Pincus et al., 2005). Pre-deployment can involve elements of anticipatory loss as the family members who are not deploying prepare for extended separation and the real danger of injury or loss of life. Deployment may result in infrequent and sporadic contact with the deployed parent, including potentially heightened fearfulness for the safety of the deployed parent (Faber et al., 2008). Deployed parents may also feel disconnected from the lives of their families and powerless to provide assistance if needed (Gewirtz, Erbes, Polusny, Forgatch, & DeGarmo, 2011). Upon return from deployment, the reintegration stage begins, and families have to adjust to new norms for family functioning that are drastically different than those during deployment. A household may change from a functionally single-parent family back to a dual-parent family as the service member rejoins family life (Creech, Hadley, & Borsari, 2014; Mancini, Bowen, O’Neal, & Arnold, 2015). The service member could have sustained a physical or mental injury during deployment such as traumatic brain injury, PTSD, or loss of or reduced functioning in a limb. As the service member and her or his family adjusts to these myriad of changes, depression, anxiety, PTSD, substance abuse, and suicidality sometimes accompany these challenges for both active duty and reserve families (Trautman, Alhusen, & Gross, 2015; Gewirtz, Erbes, Polusny, Forgatch, & DeGarmo, 2011).
Given the associated stressors, military deployment is understandably disruptive to parenting and child adjustment. Instances of child abuse and neglect in military families increase by more than 40% during deployment of an active duty parent, suggesting a substantial increase in stress for the non-deployed parent (Gibbs, Martin, Kupper, & Johnson, 2007). Non-deployed spouses have a higher incidence of depression, anxiety disorders, and acute stress reactions (Mansfield et al., 2010). Substance use, suicidal ideation, PTSD, or other battle-related stressors may be experienced by deployed parents upon reintegration in both active duty and reserve forces (Jacobson et al., 2008; Milliken, Auchterlonie, & Hoge, 2007; Shea, Vujanovic, Mansfield, Sevin, & Liu, 2010). These stressors can negatively impact parenting, which in turn, is associated with a negative impact on child functioning (Gewirtz et al., 2011). Children with deployed parents in both active duty and reserve forces show higher rates of anxiety, depression, suicide, substance use, and externalizing behavior symptoms when compared to their peers without deployed parents (Creech, Hadley, & Borsari, 2014). The effects of deployment also extend to children’s peer relationships, with increased reports of peer difficulties in children of deployed military families when compared to non-deployed families (Chandra et al., 2010).
With the many challenges faced by deployed families, it is critical to better understand how to best promote healthy adjustment within this population. A resilience framework encourages the identification of variables that may allow families to not only cope with these stressors but also respond adaptively (Masten, 2001; Rutter, 1987). In this way, positive adjustment in the face of stress is considered an indicator of resilience. Preventive interventions with at-risk populations offer a unique opportunity to evaluate specific mechanisms that may promote successful functioning. While risk factors for military family functioning (e.g., parental mental health) have been clearly delineated, few specific factors associated with child resilience in the context of these stressors have been identified (Chandra et al., 2010; Gewirtz, Polusny, DeGarmo, Khaylis, & Erbes, 2010). The current study sought to better understand the mechanisms through which a parenting intervention for military families fosters positive adjustment in children.
A developmental lens is often necessary to understand processes of resilience in children. The concept of developmental cascades describe interacting systems that have cumulative effects on development (Masten & Cicchetti, 2010). When resilience to stress is promoted and developed at an early age, youth are more likely to experience positive outcomes that spread across domains and over development. Peer relationships are nearly universally identified in developmental cascade models as playing a critical role in positive adjustment in multiple domains from early childhood through adulthood (Blandon, Calkins, Grimm, Keane, & O’Brien, 2010; Burt, Obradović, Long, & Masten, 2008; Lansford, Malone, Dodge, Pettit, & Bates, 2010). The transition from childhood to early adolescence marks a particularly salient developmental period for peer relationships. During this period, children transition to decreased time with their parents and increased time with peer groups (Flannery, Williams, & Vazsonyi, 1999). Perhaps for this reason, early adolescent peer relationships are strongly linked to academic achievement and risk-taking behaviors (Dishion, Andrews, & Crosby, 1995; Wentzel, 1991). Therefore, when youth approaching this developmental period are faced with stressors that potentially undermine the development of positive peer relationships, it is particularly important to better understand factors associated with resilience and outcomes reflecting positive adjustment. Because of the risks for maladaptive peer relationships in children of military families coping with deployments, we identified positive peer adjustment as a primary outcome associated with resilience in this context.
Parenting practices have been consistently implicated in studies of children’s resilience to stressful circumstances (See review by Masten, 2001). Effective parenting may serve to buffer children from exposure to stress and promote positive adjustment (Gewirtz, Forgatch, & Wieling, 2008). While the link between parenting and child adjustment, including peer relationships, has been reliably noted within general populations as well as those experiencing stress or trauma, more limited research has examined this association within military families coping with deployment (Chandra et al., 2010; Gewirtz, Erbes, Polusny, Forgatch, & DeGarmo, 2011; Gewirtz, Forgatch, & Wieling, 2008; Jones & Prinz, 2005). Parenting practices appear to play a significant mediating role in the negative impact of deployment on children (Palmer, 2008). Rather than the stress of parental deployment directly impacting children, maladaptive parenting practices may be a primary mechanism through which this stress is transmitted. Furthermore, supporting parenting practices within military families may reduce the negative impact of deployment on children (Gewirtz et al., 2011).
Parental locus of control (LOC) has been identified as a key aspect of parenting that may be supported through parenting interventions. As opposed to a direct measure of parenting practices, parental LOC reflects the extent that parents feel confident in their ability to parent effectively and control their children’s behavior (Hagekull, Bohlin, & Hammarberg, 2001). High parental LOC reflects a stable, internal sense of parental control and is associated with parenting competence (Jones & Prinz, 2005). Parental LOC has also been associated with calmer, more consistent discipline, as opposed to harsh and reactionary punishments from parents (Kokkinos & Panayiotou, 2007). It is also associated with positive child outcomes, such as fewer externalizing and internalizing symptoms (Hagekull et al., 2001). Thus, as parents feel more able to control their child’s behavior, their parenting practices facilitate the child’s positive adjustment through consistent and effective parenting practices (Hagekull, Bohlin, & Hammarberg, 2001; Kokkinos & Panayiotou, 2007). With regard to peer adjustment, parental LOC may facilitate positive peer relationships through modeling a high quality parent-child relationship, the development of effective child self-regulatory skills, and increased monitoring and supervision of peer activities (Brody, Flor, & Gibson, 1999; Jones & Prinz, 2005).
While many evidence-based programs designed to support parenting practices have been developed, few have been specifically targeted to military families (Gewirtz et al., 2011). After Deployment Adaptive Parenting Tools (ADAPT) is an evidence-based preventive intervention specifically designed to support parenting in military families facing deployment (Gewirtz, Pinna, Hanson, & Brockberg, 2014). ADAPT is a modification of the Parent Management Training-Oregon Model (PMTO). PMTO, derived from Patterson’s (1982;s (2005) Social Interaction Learning model, teaches parents behavioral strategies to improve parenting practices. PMTO has shown extensive effectiveness in improving parenting and child outcomes with diverse populations (Forgatch & Gewirtz, in press; Forgatch, Patterson, & Gewirtz, 2013; Patterson, 1982; Patterson, 2005). ADAPT includes the key components of PMTO (i.e., skills to improve parents’ teaching through encouragement, positive involvement with children, monitoring and supervision, problem solving, and effective non-corporal discipline) tailored for military families. ADAPT also adds content specialized for delivery to military parents, including attention to emotion socialization (i.e. tools to improve parents’ emotion regulation, and effective ways to respond to children’s emotions) and tools to manage the typical family stressors that accompany reintegration (Gewirtz, Pinna, Hanson, & Brockberg, 2014). Data from a randomized controlled trial of group-based ADAPT has demonstrated a range of positive outcomes in military families, including improvements in parenting practices, parental LOC, child psychopathology, and parents’ mental health (Gewirtz, DeGarmo, & Zamir, 2016).
The current study sought to better understand the role of parental LOC in promoting child resilience within National Guard/Reserve military families by looking at peer adjustment outcomes. We examined the impact of the ADAPT preventive intervention on military families, with the following primary research questions: 1) Will participation in ADAPT result in improved parental LOC? 2) Will parental LOC be associated with peer adjustment? And, 3) Will parental LOC mediate the relationship between participation in ADAPT and positive peer adjustment? Previous investigations of parental LOC in response to interventions have revealed differential responses between mothers and fathers (Gewirtz, DeGarmo, & Zamir, 2016; Hagekull, Bohlin, & Hammarberg, 2001). Therefore, we also investigated the distinct roles that mother and father parental LOC may play in influencing children’s peer adjustment. Finally, because of the demonstrated impact of mental health on parenting and peer adjustment, we examined the roles that both parental mental health secondary to deployment (i.e., PTSD symptoms) as well as child mental health may play in the above research questions (Bornstein, Hahn, & Haynes, 2010; Gewirtz et al., 2010).
Methods
Participants
The current sample comprised of 336 families enrolled in a randomized controlled prevention trial of ADAPT, including 313 mothers, 294 fathers, and 336 children. Families were eligible to participate if they had at least one child between the ages of five and twelve, and at least one parent deploy overseas to a combat zone since 2001 (i.e., Operation Iraqi Freedom/OIF, or Operation New Dawn/OND).
Of the 336 families who consented and completed their baseline assessment, 281 were currently married (83.6%). The majority of families reported household incomes between $40,000 to $79,999 (43.5%), or $80,000 to $119,999 (28.2%), with a range of $39,999 or less (13.8%) to $120,000 or more (14.5%). Of the 607 total parents who participated, 541 were white (89%), 19 were African-American (3.1%), 13 were biracial or multiracial (2.2%), 10 were Asian/Asian-American (1.7%), 3 were Native American/Alaska (.5%), 2 were Native Hawaiian/Pacific Islander (.3%), and 20 were missing cases or preferred not to answer (3.2%).
All families who participated in the study experienced a parental deployment in a recent conflict: 86.7% had one parent deploy, while 13.3% had both parents deploy. In 95% of families, it was the father who deployed, while 18.2% of families experienced a mother’s deployment. More than half of parents (51.2%) deployed more than once, with an average of 1.73 deployments since 2001 (SD = 1.16) with a modal duration of more 18 – 24 months spent deployed (and a range of less than 6 months to more than 37 months). Minnesota has no active duty military installations, thus almost all service members were affiliated with the National Guard and Reserves. The majority of parents deployed with the Army (59%) or Air (10.7%) National Guard, while a portion deployed with the Army (12.9%), Navy (6.6%), Air force (2.8%), or Marine Reserves (.3%).
The average age of the 336 children who participated in the study was 8.3 years old (SD = 2.5, range: 4–13 years) at study entry, of whom 179 were female (53.3%) and 157 were male (46.7%). Of the 336 children, 266 were reported by their parents as white (79.2%), 17 were biracial or multiracial (5.1%), 7 were African-American (2.1%), 6 were Asian/Asian-American (1.8%), 6 were Native American/Alaska (1.8%), 2 were Native Hawaiian/Pacific Islander (.6%), and 32 were missing cases or had parents who preferred not to answer (9.5%). Nearly all the children included in the study experienced at least one parental deployment (92%), while 8% were born after their parent returned.
Procedures
Participants were recruited through a variety of methods, including at reintegration events following the recent return from a deployment, through a targeted mailing at a Veterans Affairs Medical Center, through the use of social media (e.g., Facebook) and traditional print and local media, and by word of mouth. After expressing interest, participants were directed to an online screener where they could consent to participate. If eligible, they were transferred to a secure and confidential online survey. Following completion of the survey, study staff contacted each family to set up an in-home assessment, where additional self-report, observational, and physiological data were collected from the parent(s) and a target child who was identified as within the previously identified age range. Each parent who completed an online survey was compensated with a $25 gift card, and each family was compensated with a $50 gift card following completion of the in-home assessment.
After completing the baseline assessment, 60% of families were randomized to participate in the intervention, while 40% were assigned to a control condition, consisting of services-as-usual. Participants in the control condition were emailed a list of print and online parenting resources shortly after the completion of their baseline assessment. The intervention consisted of a group-based, preventive parenting program that was delivered in weekly, 2-hour sessions for 14 weeks. ADAPT was designed to target the five core PMTO parenting practices: positive involvement, skill encouragement, problem-solving, monitoring, and appropriate discipline (Forgatch & Gewirtz, in press) with adaptations specific to military families (e.g. content specific to the common struggles experienced during deployment and reintegration). Each week built on skills learned in the previous sessions with the utilization of active teaching skills, such as role-play and discussion. Parents were invited to attend groups that were held in various locations throughout Minnesota. The number of attendees for each group ranged from 4–15 parents, and dinner and childcare were provided each week to the families who participated, with additional resources (e.g. videos, worksheets) made available online (For more information about the intervention, see Gewirtz, Pinna, et al., 2014). Each group was delivered by two to three facilitators trained in the PMTO model and was videotaped in order to measure fidelity of implementation according to an established fidelity system for PMTO (Knutson, Forgatch, Rains, & Sigmarsdottir, 2009).
Parents completed online surveys again six months post-baseline, and both online surveys and in-home assessments were conducted 12 months after families’ baseline assessment.
Measures
Parental locus of control
Mother and father locus of control was measured at baseline and a six-month follow-up utilizing the Parenting Locus of Control Short Form Revised/PLOC -SFR (Hassall, Rose, & McDonald, 2005), an abridged version of the 47-item Parental Locus of Control Scale (PLOC; Campis, Lyman, & Prentic-Dunn, 1986). The PLOC - SFR consists of 24 self-report items in four domains: parental efficacy (e.g., “My child usually ends up getting his/her way, so why try”), parental responsibility (e.g., “My child’s behavior problems are no one’s fault but my own”), child control of parents’ life (e.g., “My child influences the number of friends I have”), and parental control of child’s behavior (e.g., “My child’s behavior is sometimes more than I can handle”). The response format is a 5-point Likert scale (1 = strongly agree to 5 = strongly disagree). A total mean score for each parent was obtained, with higher scores indicating an internal locus of control, and low scores indicating an external locus of control. Reliability was sufficient for the measure at baseline (mother α = .75; father α =.73).
Child peer relationships
Child peer relationships were measured at the baseline and 12-month assessments using a parent-report version of Describing Friends (DF; Capaldi & Dishion, 1985), a 7-item scale of children’s peer relationships with items including, “To what extent is your child influenced by kids his/her own age,” “Does your child prefer to be with friends or by him/herself,” and “How many new friends has your child made in the past year?” Response formats varied by question, and items were summed to compute a total score for each parent. A composite score was then created by averaging mother and father report, with higher scores indicating better child peer adjustment. Alpha reliabilities were computed for peer adjustment scales (baseline: mother α =.68, father α =.65; 12-months: mother α =.70, father α =.68). While some of these values fall just below the acceptable range (>.7) into the questionable range (.6–.7) by conventional cut-off criteria, the relatively small number of items in each scale may make these criteria overly conservative (Loewenthal, 2004). The mother and father-reported scales demonstrated good consistency across raters at both assessment points (r=.59 at baseline; r = .60 at 12 months). A composite score was computed averaging the mother and father scales in order to reduce the potential for reporter biases and increase validity of the measurement of the construct.
Covariates
Child covariates included child age, calculated from his/her date of birth, and child gender (coded as 1 for males and 2 for females), and child mental health symptoms Child mental health was measured using the Behavior Assessment System for Children (2nd Ed.) – Parent Rating Scale (BASC-2-PRS; Reynolds & Kamphaus, 2004). The BASC-2 is a widely-administered, multidimensional system used to assess broad domains of externalizing problems, internalizing problems, and adaptive skills. Items are rated on a 4-point scale, ranging from 0 = never to 3 = almost always. Two version of the BASC-2-PRS were used because of the age range of the sample, including the child form (normed for ages 6 to 11) and the adolescent form (normed for ages 12 to 21). Age-specific normative scores are calculated using a large, nationally representative sample in the form of T-scores with a mean of 50 and a standard deviation of 10.
Internalizing symptoms composite scores were calculated using the Depression (α =.88), Anxiety (α =.85), and Somatization (α =.79) scales. Externalizing symptoms composite scores were calculated using the Hyperactivity (α =.86), Aggression (α =.87), and Conduct Problems (α =.88) scales. Mother and father scores were first computed separately and then averaged for the purposes of forming mean parent-reported internalizing and externalizing composite scores.
Seventy-six children in the sample were below the age of 6 (including 54 5-year-olds and 22 4-year-olds) when their parents completed the BASC-2-PRS child form. For these children, a downward extension of 6-year-old age norms was used to calculate T-scores. All analysis described below were rerun excluding the scores computed using this downward extension of age norms without any significant changes to model results. It was therefore decided to retain all BASC-2-PRS scores from the full sample for the analyses reported below.
Parent covariates included parents’ marital status, family income, and posttraumatic stress symptoms. Parents’ current marital status was evaluated at study entry (0 = not married; 1 = married) along with annual household income. Family income was coded in 10,000 dollar increments ranging from 1 to 17 (1 = less than $10,000 per year, 2= $10,000 – $19,999… 17= $150,000 or more). Posttraumatic stress symptoms were assessed at baseline using the Posttraumatic Stress Disorder Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993). The PCL is a 17-item standardized, self-report questionnaire assessing PTSD symptoms experienced in the last month based on the in the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994). The military version (PCL-M), detailing traumatic experiences while serving in the military (e.g. “To what extent have you been bothered by repeated, disturbing memories, thoughts or images of a stressful military experience?”), was given to deployed parents, and the civilian version (PCL-C), focusing on other experiences of trauma (e.g. “To what extent have you been bothered by repeated, disturbing memories, thoughts or images of a stressful experience from the past?”), was given to non-deployed parents. Each item was rated on a 5-point scale of severity (0 = not at all, 1 = a little bit, 2 = moderately, 3 = quite a bit, and 4 = extremely). All items were summed to compute a composite score of post-traumatic stress symptom severity, with higher scores indicating a greater number of PTSD symptoms present. The PCL demonstrated excellent internal consistency in both mothers (α = .91) and fathers (α =.95).
Analytic Strategy
A mediational path model was estimated using the structural equation modeling program Mplus version 7.4 (Muthén & Muthén, 1998–2015) in order to address the current research questions. An intent-to-treat (ITT) approach was used to evaluate intervention effects, meaning that all participants were analyzed within their originally assigned intervention group regardless of the extent of their actual participation or completion of programming. Intervention status (ADAPT intervention versus control group) was the primary independent variable. A composite score of mother and father ratings of child peer adjustment at the 12 month follow-up assessment was the dependent variable. Mother- and father-reported parental LOC measured at 6 months post intervention were tested as separate mediating variables simultaneously within the model. Baseline levels of parental LOC and peer adjustment were controlled for in order to model intervention-related change. Covariates were also included in the model, including child variables (i.e., age, gender, internalizing symptoms, externalizing symptoms) and parent variables (i.e., family income, marital status, posttraumatic stress symptoms). Due to the limited representation of ethnic minorities within the sample, we did not examine ethnic minority status as a covariate in analyses.
In order to evaluate the presence of mediation, the indirect effects from intervention status to peer adjustment through each parental LOC variable were tested using the MODEL INDIRECT feature in Mplus (Muthén, 2011). Confidence intervals for indirect effects were estimated using bias-correcting bootstrapping methods (MacKinnon, Lockwood, & Williams, 2004). Missing values were present in the dataset due to the longitudinal nature of the planned analyses. Missing data in all models were managed with the full information maximum likelihood (FIML) procedure used by Mplus version 7. We evaluated fit indices according to Hu and Bentler (1999), who suggest that a CFI greater than .95 and an SRMR below .08 indicate acceptable model fit.
Following estimation of the primary model using the full sample, a two-group model was estimated in order to test for consistency of model parameters across age ranges with the sample. The sample was split into two groups, including a child group (under the age of 9 at baseline; n = 206) and an early adolescent group (age 9 and older at baseline; n = 130). This age range was selected such that all children in the early adolescent group were at least 10 years old by the 12-month follow-up assessment. A chi-square difference test (Δχ2) was used to assess the significance of the differences between the two-group “constrained” models, in which the two groups are assumed to have equivalent parameters, and the two-group “unconstrained” models, in which the groups are not assumed to have identical model parameters. The Δχ2 test indicates a significant difference between models for χ2 distribution p values of less than .05, consistent with an unconstrained parameter resulting in a superior model fit.
Results
Preliminary Analyses
Table 1 depicts correlations and descriptive statistics of the variables examined for the current study. Of note, mother and father PTSD symptoms measured at baseline demonstrated significant negative correlations with their respective baseline PLOC scores (mother: r=−.20, p <.001; father: r=−.25, p<.001). Higher levels of PTSD symptoms were associated with lower PLOC scores (i.e., a greater external LOC) for both parents.
Table 1.
Descriptive Statistics and Correlations
| Measure | BL Father PLOC (n=285) |
BL Mother PLOC (n=305) |
6M Father PLOC (n=195) |
6M Mother PLOC (n=235) |
BL Peer Adjustment (n=335) |
12M Peer Adjustment (n=285) |
Family Income (n=334) |
Marital Status (n=335) |
Child Gender (n=335) |
Child Age (n=336) |
Child Extern. (n=325) |
Child Intern. (n=325) |
Father PTSD (n=287) |
Mother PTSD (n=305) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BL Father PLOC | – | |||||||||||||
| BL Mother PLOC | .25*** | – | ||||||||||||
| 6-Month Father PLOC | .55*** | .17* | – | |||||||||||
| 6-Month Mother PLOC | .21** | .61*** | .39*** | – | ||||||||||
| BL Peer Adjustment | .15* | .20*** | .15* | .26*** | – | |||||||||
| 12-Month Peer Adjustment | .17* | .24*** | .12 | .31*** | .74*** | – | ||||||||
| Family Income | .02 | .12* | .04 | .14* | .09 | .16** | – | |||||||
| Marital Status | −.03 | .11 | −.03 | .10 | .09 | .05 | .25*** | – | ||||||
| Child Female Gender | .04 | .05 | −.02 | .07 | .12* | .15* | .02 | .11* | – | |||||
| Child Age | .13* | .14* | .06 | .14* | −.21*** | −.22*** | .10 | −.03 | −.04 | – | ||||
| Child Externalizing Symptoms | −.27*** | −.46*** | −.18* | −.34*** | −.37*** | −.37*** | −.16** | −.09 | −.23*** | −.08 | – | |||
| Child Internalizing Symptoms | −.16** | .14* | −.14 | −.11 | −.43*** | −.38*** | −.03 | −.06 | .16** | .13* | .37*** | – | ||
| Father PTSD Symptoms | −.25*** | −.09 | −.11 | .01 | −.08 | −.09 | −.13* | −.14* | .00 | −.05 | .22*** | .14* | – | |
| Mother PTSD Symptoms | −.05 | −.20** | −.05 | −.14* | −.15** | −.14* | −.18** | −.10 | −.02 | −.05 | .22*** | .23*** | .12 | – |
|
| ||||||||||||||
| Mean | 3.67 | 3.62 | 3.67 | 3.71 | 3.45 | 3.44 | 8.04 | .84 | 1.5 | 8.39 | 51.94 | 51.08 | 29.97 | 27.31 |
| Standard Deviation | .40 | .42 | .50 | .47 | .57 | .58 | 3.51 | .37 | .50 | 2.52 | 7.57 | 7.90 | 12.39 | 9.67 |
Notes. BL = Baseline; 6M = 6 month; 12M = 12 month; Intern. = Internalizing Symptoms; Extern. = Externalizing Symptoms
p<.05;
p<.01;
p<.001
A series of t-tests on all study variables at baseline revealed no significant group differences between those participants assigned to the ADAPT intervention versus control groups. Additional t-tests were run to evaluate group differences between those who attritted from the study versus those who completed the 12-month assessment (see Table 1 for number of respondents per variable). The 12-month post baseline assessment was completed by 255 (81%) mothers, and 226 (77%) fathers. There were no significant differences in race, income, age, and marital status between those who completed the 12-month assessment and those who dropped out. However, mothers retained at 12-months had more children on average as measured at baseline (M = 2.27, SD = 0.59) than mothers who did not complete the 12-month assessment (M = 2.54, SD = 1.21; t (307) = −2.05, p < .05).
Primary Analyses
The path model included intervention status as the independent variable, mother and father parental 6-month LOC scores as mediators, and child 12-month peer adjustment as the dependent variable (See Figure 1). Baseline levels of parental LOC and peer adjustment were controlled for along with family income, marital status, child age and gender, child externalizing and internalizing symptoms, and mother and father posttraumatic stress symptoms. The model was an acceptable fit for the data (χ2(17) = 20. 11, p=.269, CFI = .99, SRMR= .03).
Figure 1.
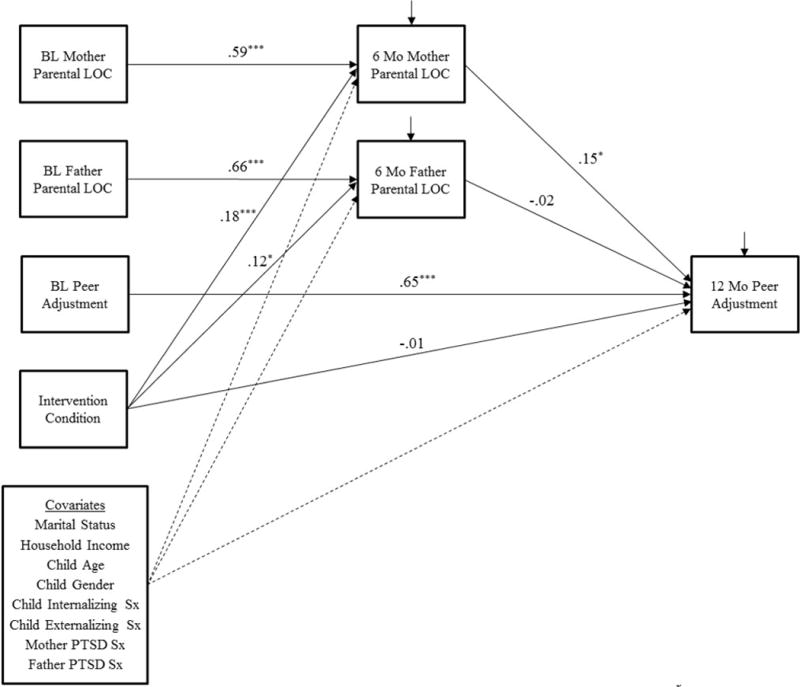
Mediation model depicting parental locus of control as a mediator of the effects of the ADAPT intervention on child peer adjustment.
Research question one examined intervention effects on parental LOC. The model revealed significant intervention effects on both mother and father parental LOC at 6 months (mother: b = .18; β = .19; p < .001; father: b = .12; β = .12; p < .05). Participation in ADAPT was associated with higher scores on the PLOC (reflecting a stronger sense of internal control) for both mothers and fathers. Baseline PLOC scores were strongly associated with PLOC scores at 6 months for both mothers and fathers (mother: b = .59; β = .54; p <.001; father: b = .66; β = .53; p <.001). None of the covariates reliably predicted mother or father PLOC scores.
Research question two evaluated the role of parental LOC in peer adjustment. Mothers’ PLOC at 6 months was a significant predictor of children’s peer adjustment at 12 months (b = .15; β = .12; p <.05). Mothers’ stronger sense of internal control was associated with higher levels of reported peer adjustment. Fathers’ parental LOC at 6 months was not reliably associated with peer adjustment. These effects on peer adjustment at 12 months were evaluated while controlling for baseline levels of reported peer adjustment, which explained a large amount of variance in the construct (b = .65; β = .64; p <.001). Several covariates were significant predictors of peer adjustment. Greater child internalizing symptoms were associated with lower reported peer adjustment (b = −.01; β = −.11; p <.05). Higher family income predicted higher levels of peer adjustment (b = .02; β = .10; p <.05). Marital status was also associated with peer adjustment (b = −.15; β = −.09; p <.05), with married parents surprisingly reporting lower levels of peer adjustment in their children. The other covariates included in the model were not significant predictors of peer adjustment.
The third research question investigated the presence of indirect effects of the intervention on peer adjustment through parental LOC. The intervention did not demonstrate a significant direct effect on children’s peer adjustment at 12 months in the context of the mediational model. However, the model revealed a significant indirect effect from intervention condition to 12-month peer adjustment through mothers’ PLOC at 6 months (b = .03; β = .02; p <.05; 95% bias corrected bootstrapped CI [.01,.07]). The intervention condition was associated with improvements in mothers’ LOC, which in turn, predicted improvements in children’s peer adjustment. The related indirect effect through fathers’ LOC was not significant.
Finally, a two-group model was used to evaluate the consistency of key model parameters across age groups within the sample (i.e., children versus early adolescents). Comparison of the unconstrained two-group model with the constrained two-group model did not reveal a significant improvement in model fit (Δχ2(5) = 1.79, p=.88), supporting generalization of the model across the two age groups.
Discussion
Our findings demonstrate that ADAPT, a parenting program for deployed military parents, appears to set in place a cascade of change within the family system. First, the intervention improved parental LOC at 6 months post baseline (i.e., shortly after completion of the intervention). These initial improvements to mothers’ LOC at posttest then led to improvements in children’s peer adjustment six months later (at 12 months post-baseline). We did not find parallel cascading changes for fathers (i.e., no similar effects of fathers’ improved LOC on peer adjustment).
We speculate that enhancing mothers’ sense of their control over their children may enable them to be more effective in helping their youth to act in prosocial ways, to increase social skills in general, to strengthen prosocial ties with peers and to reduce the likelihood of affiliation with antisocial peers. Specifically, a mother’s perception that she has the capacity to influence her children’s behavior may be empowering and may influence her to learn more about — and then influence — who her children’s friends are, encouraging prosocial friends and discouraging interactions with antisocial peers. Such a perception may play an important role in effectively coping with deployment-related stressors that could easily overwhelm parents and undermine effective parenting practices. Poor monitoring is a key predictor of delinquency (Hoeve et al., 2009), and prevention programs that incorporate monitoring skills prevent or reduce adolescent risk behaviors (e.g., Dishion, Nelson, & Kavanagh, 2003).
Indeed, at no point in development is monitoring more crucial for improving children’s psychosocial adjustment (e.g. reducing internalizing and externalizing problems, improving social adjustment) than at the transition to adolescence when peers replace parents as key socializing agents (Dishion, Nelson, & Bullock, 2004). Because the absence of one or more parents due to deployment may be disruptive to effective monitoring, monitoring and supervision of children is a key component of the ADAPT curriculum. For example, one of the sessions focuses on what questions to ask children when they become old enough to engage in activities alone with friends (e.g., “The four Ws”: Who are you going with? Where are you going? When will you be back? What are you doing?) Home practice aims to consolidate skills via practice, and to help parents to learn about their children’s activities during and after school, who their teachers are, who their friends are, and what they do online.
Improvements to peer adjustment set in place via the intervention’s impact on maternal LOC were consistent across both child and early adolescent age groups within the sample. Maternal LOC appears to play a role in promoting positive peer adjustment within each of these developmental stages. We speculate these improvements will remain and possibly continue to grow over the course of adolescence. Further research on this sample over a longer time period will examine this. However, consistent with developmental cascade models, prior data from prevention programs with civilian populations indicate that program-related improvements to youth adjustment grow over time (e.g., Patterson, Forgatch, & DeGarmo, 2010). For example, using a prevention program to improve parenting among single mothers, Forgatch and colleagues demonstrated how initial improvements to parenting subsequently benefited child depression, then externalizing behavior, then substance use and school outcomes, strengthening youth resilience across adolescence and into emerging adulthood (e.g., Forgatch, Patterson, DeGarmo, & Beldavs, 2009).
We found no direct effects of assignment to the ADAPT condition on peer adjustment, as we would expect given that ADAPT targets parents alone, and there is no youth involvement in the program. In the developmental model on which ADAPT is based, parents are hypothesized to be the agents of change. That is, the social interaction learning model upon which ADAPT is based is a mediation model wherein parenting mediates the associations between stressful family transitions and children’s adjustment. With parenting as the putative mediator between stressful family transitions and children’s adjustment, the intervention to strengthen or buffer parenting could be seen as ‘moderating the mediator.’ Strengthening parenting, in turn, promotes children’s healthy adjustment (Patterson, 2005; Forgatch & Gewirtz, in press).
Parental LOC appears to be a key proximal outcome of ADAPT and PMTO interventions. In a recently published article reporting on a randomized controlled trial of a family-based comprehensive prevention program targeting formerly homeless mothers and their children residing in supportive housing, the program (of which a PMTO intervention was the primary parenting component) demonstrated direct, intent-to-treat improvements in mothers’ LOC, which subsequently led to improvements in observed parenting practices two years post-baseline (Gewirtz, DeGarmo, Lee, Morrell, & August, 2015). In a recently published outcomes study of the current ADAPT program, the intervention’s improvements to parental LOC in both mothers and fathers led to subsequent reductions in both parents’ psychological distress (PTSD and depression symptoms), and suicidal ideation (Gewirtz, DeGarmo, & Zamir, 2016).
The absence of significant indirect effects of fathers’ LOC on children’s peer adjustment is of note, but is not surprising. In the current sample of military families exposed to a parent’s deployment, more than 95% of the fathers had been deployed at least once. Returning from deployment not only requires a father to return to caregiving but also to ‘code shift’ in quite a significant way in the transition from a military to a parenting context. Not surprisingly, given data indicating that mothers typically are primary caregivers even in civilian environments (Kotila, Schopp-Sullivan & Kamp Dush, 2013), recent reports have highlighted the challenges for deployed fathers to fully return to the primary caregiving of children (Walsh et al., 2014). This may be a particular challenge for fathers experiencing posttraumatic stress disorder and related sequelae of combat (e.g., Brockman et al., 2015). In contrast, mothers returning from a military deployment tend to experience an immediate and urgent need to be fully and immediately present in their children’s lives (Gewirtz, Davis, et al., 2014).
In terms of limitations, our data relied on parent report for both the assessment of LOC and child’s peer adjustment; relying on single informants in this way has the potential for shared method variance. Future research should examine teacher and child reports as well as parent reports of peer adjustment. The sample in this study included National Guard and Reserve Component families with school age children, limiting generalizability beyond the Reserve Component (i.e., to the Active Duty military) and among families with young children or older adolescents. The data also indicated a single difference on measured variables between parents retained in the study and those who attrited: the former had more children, on average. It is possible that parents with more children were more motivated to participate in the study because they perceived a greater need for parenting support, which could affect the results. Additionally, a small number of children included in the study were born after their parent returned from deployment. While the stressors associated with deployment do not end upon reintegration of the deployed parent into the family, the experiences of these youth may have been unique from those youth who were born prior to their parents’ deployment. Finally, the current analysis utilized an intent-to-treat analytic strategy and did not take into account the extent of parental participation in the intervention or other measures of intervention engagement. Further research with this dataset could examine the role that these indices played in the current findings.
Notwithstanding several limitations, the current study demonstrated the impact of the ADAPT program — the first military parenting program to be rigorously evaluated in a randomized controlled trial — on parents’ LOC. Improved mothers’ LOC in turn mediated subsequent improvements in children’s peer adjustment. The risks associated with a parent’s deployment to war for children’s psychosocial outcomes, particularly in early adolescence (Sullivan et al., 2015) suggest that interventions to support resilience among youth in this population are critically needed. The current study reports evidence from one such intervention to outline a potential path to youth resilience.
Acknowledgments
This study was supported by grant DA030114 to Abigail Gewirtz from the National Institute of Drug Abuse’s Prevention Research Branch.
References
- Blandon AY, Calkins SD, Grimm KJ, Keane SP, O’Brien M. Testing a developmental cascade model of emotional and social competence and early peer acceptance. Development and Psychopathology. 2010;22(4):737–748. doi: 10.1017/S0954579410000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein MH, Hahn C, Haynes OM. Social competence, externalizing, and internalizing behavioral adjustment from early childhood through early adolescence: Developmental cascades. Development and Psychopathology. 2010;22(Special Issue 04):717–735. doi: 10.1017/S0954579410000416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird S, Quattlebaum J, Schmidt N, Pauldine M, Elish K, Schrepferman L, Zettle R, DeGarmo D. Relationship of service members’ deployment trauma, PTSD symptoms and experiential avoidance to postdeployment family reengagement. Journal of Family Psychology. 2015 doi: 10.1037/fam0000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Flor DL, Gibson NM. Linking maternal efficacy beliefs, developmental goals, parenting practices, and child competence in rural single parent African American families. Child development. 1999;70(5):1197–1208. doi: 10.1111/1467-8624.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt KB, Obradović J, Long JD, Masten AS. The interplay of social competence and psychopathology over 20 years: Testing transactional and cascade models. Child Development. 2008;79(2):359–374. doi: 10.1111/j.1467-8624.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- Campis LK, Lyman RD, Prentice-Dunn S. The parental locus of control scale: Development and validation. Journal of Clinical Child Psychology. 1986;15:260–267. doi: 10.1207/s15374424jccp1503_10. [DOI] [Google Scholar]
- Capaldi DM, Dishion TJ. Describing Friends Questionnaire. 1985 Unpublished manual. [Google Scholar]
- Chandra A, Lara-Cinisomo S, Jaycox LH, Tanielian T, Burns RM, Ruder T, Han B. Children on the homefront: The experience of children from military families. Pediatrics. 2010;125(1) doi: 10.1542/peds.2009-1180. [DOI] [PubMed] [Google Scholar]
- Creech SK, Hadley W, Borsari B. The impact of military deployment and reintegration on children and parenting: A systematic review. Professional Psychology: Research and Practice. 2014;45(6):452–464. doi: 10.1037/a0035055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Andrews DW, Crosby L. Antisocial boys and their friends in early adolescence: Relationship characteristics, quality, and interactional process. Child Development. 1995;66(1):139–151. doi: 10.1111/j.1467-8624.1995.tb00861.x. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Nelson SE, Bullock BM. Premature adolescent autonomy: parent disengagement and deviant peer process in the amplification of problem behaviour. Journal of Adolescence. 2004;27(5):515–530. doi: 10.1016/j.adolescence.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Nelson SE, Kavanagh K. The family check-up with high-risk young adolescents: Preventing early-onset substance use by parent monitoring. Behavior Therapy. 2003;34(4):553–571. [Google Scholar]
- Faber AJ, Willerton E, Clymer SR, MacDermid SM, Weiss HM. Ambiguous absence, ambiguous presence: A qualitative study of military reserve families in wartime. Journal of Family Psychology. 2008;22(2):222. doi: 10.1037/0893-3200.22.2.222. [DOI] [PubMed] [Google Scholar]
- Finkel LB, Kelley ML, Ashby J. Geographical mobility, family, and maternal variables as related to the psychosocial adjustment of military children. Military Medicine. 2003;168(12):1019–1024. [PubMed] [Google Scholar]
- Flannery DJ, Williams LL, Vazsonyi AT. Who are they with and what are they doing? Delinquent behavior, substance use, and early adolescents’ after-school time. American Journal of Orthopsychiatry. 1999;69(2):247–253. doi: 10.1037/h0080426. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Gewirtz AH. Evolution of Parent Management Training- the Oregon Model: A dynamic model of an empirically supported intervention. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. 3rd. New York: Guilford Press; (in press) [Google Scholar]
- Forgatch MS, Patterson GR, Degarmo DS, Beldavs ZG. Testing the Oregon delinquency model with 9-year follow-up of the Oregon Divorce Study. Development and Psychopathology. 2009;21:637–660. doi: 10.1017/S0954579409000340. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Patterson GR, Gewirtz AH. Looking forward the promise of widespread implementation of parent training programs. Perspectives on Psychological Science. 2013;8(6):682–694. doi: 10.1177/1745691613503478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs DA, Martin SL, Kupper LL, Johnson RE. Child maltreatment in enlisted soldiers’ families during combat-related deployments. JAMA. 2007;298(5):528–535. doi: 10.1001/jama.298.5.528. [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Davis L, McMorris B, Hanson S. Family adjustment of deployed and non-deployed mothers in families with a parent deployed to Iraq or Afghanistan. Professional Psychology: Research & Practice, Advance online publication. 2014 doi: 10.1037/a0036235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo D, Lee S, August GJ. Twenty-four month outcomes from the Early Risers Supportive Housing prevention trial. Journal of Family Psychology. 2015;29:242–252. doi: 10.1037/fam0000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo D, Zamir O. Effects of a military parenting program on parental distress and suicidal ideation: After Deployment Adaptive Parenting Tools. Suicide and Life Threatening Behaviors. 2016;46(S1):S23–S21. doi: 10.1111/sltb.12255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Erbes CR, Polusny MA, Forgatch MS, DeGarmo DS. Helping military families through the deployment process: Strategies to support parenting. Professional Psychology: Research and Practice. 2011;42(1):56–62. doi: 10.1037/a0022345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Forgatch M, Wieling E. Parenting practices as potential mechanisms for child adjustment following mass trauma. Journal of Marital and Family Therapy. 2008;34(2):177–192. doi: 10.1111/j.1752-0606.2008.00063.x. [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Pinna KL, Hanson SK, Brockberg D. Promoting parenting to support reintegrating military families: After deployment, adaptive parenting tools. Psychological Services. 2014;11(1):31–40. doi: 10.1037/a0034134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, Erbes CR. Posttraumatic stress symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology. 2010;78(5):599–610. doi: 10.1037/a0020571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagekull B, Bohlin G, Hammarberg A. The role of parental perceived control in child development: A longitudinal study. International Journal of Behavioral Development. 2001;25(5):429–437. doi: 10.1080/016502501316934851. [DOI] [Google Scholar]
- Hassall R, Rose J, McDonald J. Parenting stress in mothers of children with an intellectual disability: The effects of parental cognitions in relation to child characteristics and family support. Journal of Intellectual Disability Research. 2005;49:405–418. doi: 10.1111/j.1365-2788.2005.00673.x. [DOI] [PubMed] [Google Scholar]
- Hoeve M, Dubas JS, Eichelsheim VI, Van der Laan PH, Smeenk W, Gerris JR. The relationship between parenting and delinquency: A meta-analysis. Journal of Abnormal Child Psychology. 2009;37(6):749–775. doi: 10.1007/s10802-009-9310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson IG, Ryan MAK, Hooper TL, Smith TC, Amoroso PJ, Boyko EJ, Bell NS. Alcohol use and alcoholrelated problems before and after military combat deployment. Journal of American Medical Association. 2008;300:663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: A review. Clinical Psychology Review. 2005;25(3):341–363. doi: 10.1016/j.cpr.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Parent management training: Evidence, outcomes, and issues. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(10):1349–1356. doi: 10.1097/00004583-199710000-00016. [DOI] [PubMed] [Google Scholar]
- Kokkinos CM, Panayiotou G. Parental discipline practices and locus of control: Relationship to bullying and victimization experiences of elementary school students. Social Psychology of Education. 2007;10(3):281–301. [Google Scholar]
- Kotila LE, Schoppe-Sullivan SJ, Kamp Dush CM. Time in Parenting Activities in Dual-Earner Families at the Transition to Parenthood. Family Relations. 2013;62:795–807. doi: 10.1111/fare.12037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansford JE, Malone PS, Dodge KA, Pettit GS, Bates JE. Developmental cascades of peer rejection, social information processing biases, and aggression during middle childhood. Development and Psychopathology. 2010;22(3):593–602. doi: 10.1017/S0954579410000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenthal KM. An introduction to psychological tests and scales. 2nd. Hove, UK: Psychology Press; 2001. [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini JA, Bowen GL, O’Neal CW, Arnold AL. Relationship provisions, self-efficacy and youth well-being in military families. Journal of Applied Developmental Psychology. 2015;40:17–25. [Google Scholar]
- Mansfield AJ, Kaufman JS, Marshall SW, Gaynes BN, Morrissey JP, Engel CC. Deployment and the use of mental health services among U.S. Army wives. New England Journal of Medicine. 2010;362(2):101–109. doi: 10.1056/NEJMoa0900177. [DOI] [PubMed] [Google Scholar]
- Masten AS. Ordinary magic: Resilience processes in development. American Psychologist. 2001;56(3):227–238. doi: 10.1037/0003-066X.56.3.227. [DOI] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. Journal of the American Medical Association. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Muthén B. Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. 2011 www.statmodel.com.
- Muthén LK, Muthén BO. Mplus user’s guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- Palmer C. A theory of risk and resilience factors in military families. Military Psychology. 2008;20(3):205–217. doi: 10.1080/08995600802118858. [DOI] [Google Scholar]
- Patterson GR. Coercive Family Process. Eugene, OR: Castalia; 1982. [Google Scholar]
- Patterson GR. The next generation of PMTO models. The Behavior Therapist. 2005;28(2):25–32. [Google Scholar]
- Patterson GR, Forgatch MS, DeGarmo DS. Cascading effects following intervention. Development and Psychopathology. 2010;22:949–970. doi: 10.1017/S0954579410000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus S, House R, Christenson J, Adler L. The emotional cycle of deployment: A military family perspective. 2005 Retrieved from http://www.hooah4health.com/deployment/familymatters/emotionalcycle2.htm.
- Reynolds CR, Kamphaus RW. Behavior Assessment System for Children. 2nd. Circle Pines, MN: American Guidance Service; 2004. [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57(3):316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Haith MM. The five to seven year shift: The age of reason and responsibility. Chicago, IL: University of Chicago Press; 1996. [Google Scholar]
- Shea MT, Vujanovic AA, Mansfield AK, Sevin E, Liu F. Posttraumatic stress disorder symptoms and functional impairment among OEF and OIF National Guard and Reserve veterans. Journal of Traumatic Stress. 2010;23:100–107. doi: 10.1002/jts.20497. [DOI] [PubMed] [Google Scholar]
- Sullivan K, Capp G, Gilreath TD, Benbenishty R, Roziner I, Astor RA. Substance abuse and other adverse outcomes for military-connected youth in California: results from a large-scale normative population survey. JAMA pediatrics. 2015;169(10):922–928. doi: 10.1001/jamapediatrics.2015.1413. [DOI] [PubMed] [Google Scholar]
- Trautmann J, Alhusen J, Gross D. Impact of deployment on military families with young children: A systematic review. Nursing Outlook. 2015;63(6):656–679. doi: 10.1016/j.outlook.2015.06.002. [DOI] [PubMed] [Google Scholar]
- Walsh TB, Dayton CJ, Erwin MS, Muzik M, Busuito A, Rosenblum KL. Fathering after military deployment: Parenting challenges and goals of fathers of young children. Health & Social Work. 2014;39(1):35–44. doi: 10.1093/hsw/hlu005. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. Oct, [Google Scholar]
- Wentzel KR. Relations between social competence and academic achievement in early adolescence. Child Development. 1991;62(5):1066–1078. doi: 10.1111/j.1467-8624.1991.tb01589.x. [DOI] [PubMed] [Google Scholar]


