Abstract
Background and Aims:
Recovery from alcohol use disorder (AUD) is often narrowly defined by abstinence from alcohol and improvements in functioning (e.g., mental health, social functioning, employment). This study used latent profile analysis to examine variability in recovery outcomes, defined by alcohol use, alcohol-related problems, and psychosocial functioning at three years following treatment. Secondary analysis investigated pre-treatment, post-treatment, and one- and three-year post-treatment covariate predictors of the latent profiles.
Design:
Secondary analysis of data from a randomized clinical trial.
Setting:
USA
Participants:
We used data from the outpatient arm of Project MATCH (n=805; 29.7% female, 22.2% non-White).
Measurements:
Recovery was defined by latent profile analyses including measures of psychosocial functioning and life satisfaction (Psychosocial Functioning Inventory), unemployment and mental health (Addiction Severity Index), alcohol and other drug use (Form 90), and alcohol-related consequences (Drinker Inventory of Consequences) three years following treatment. Mixture modeling was used to examine correlates of profiles.
Findings:
We identified four profiles at three years following treatment: 1) poor functioning frequent heavy drinkers, 2) poor functioning infrequent heavy drinkers, 3) high functioning occasional heavy drinkers, and 4) high functioning infrequent non-heavy drinkers. There were relatively few differences on indicators of functioning and treatment-related variables between the high functioning infrequent non-heavy drinkers and the high functioning occasional heavy drinkers, other than high functioning occasional heavy drinkers having lower alcohol dependence severity (OR=0.94, 95% CI: 0.90, 0.98), fewer post-treatment coping skills (OR=0.54, 95% CI: 0.27, 0.81), and lower three-year post-treatment abstinence self-efficacy (OR=0.37, 95% CI: 0.27, 0.47), and AA involvement (OR=0.87, 95% CI: 0.74, 0.99). The two high functioning profiles showed the greatest improvements in functioning from baseline through the 3-year follow-up, whereas the low functioning profiles showed the least amount of improvement. High functioning occasional heavy drinkers had higher purpose in life than the poor functioning profiles.
Conclusions:
Some individuals who engage in heavy drinking following treatment for alcohol use disorder may function as well as those who are mostly abstinent with respect to psychosocial functioning, employment, life satisfaction, and mental health.
Keywords: alcohol use disorder, alcohol treatment, recovery, mixture models, Project MATCH
Introduction
The term “recovery,” with respect to alcohol use disorder (AUD) is often defined as a period of sustained abstinence from alcohol [1,2]. Broader definitions of recovery often incorporate physical and mental health, social, recreational, and leisure activities, and work, family, or community engagement [3–9]. In two qualitative studies of individuals who self-identified as “in recovery” [4] and treatment providers [9], participants indicated abstinence, physical and mental health, housing, social functioning, and well-being as important in defining recovery. Thus, recovery community members and practitioners embrace broader definitions of recovery that consider a range of psychological, physical, and social functioning outcomes, with abstinence included in the definition.
Many predictors of recovery outcomes have been studied. Individuals who are married, female, and older [10], with fewer heavy drinkers in their social network [11], greater coping skills [12], fewer psychiatric disorders [10], lower levels of depression and anger [13,14], higher levels of purpose in life and Alcoholics Anonymous (AA) attendance [15,16], and a higher level of abstinence self-efficacy [17,18] tend to have better outcomes following treatment. Higher alcohol dependence severity is associated with an increased odds of an abstinent recovery (defined as abstinence from alcohol and remission from alcohol dependence symptoms), but decreased odds of a non-abstinent recovery (defined as low risk drinking and remission from alcohol dependence symptoms) [19].
Current Study
Researchers, policy makers, and government agencies have advocated for a broader definition of AUD recovery to incorporate functioning outcomes and for a better understanding of the critical elements that support recovery. Yet, prior studies have relied on a limited definition of alcohol use (abstinence) in considering broader definitions of recovery [4,19–21], and no prior studies have considered a range of outcomes in which both alcohol use and functioning define recovery. Accordingly, the primary purpose of this study was to use latent profile analysis to examine variability in recovery outcomes, defined by alcohol use, alcohol-related problems, and psychosocial functioning at three years following treatment. Based on prior studies that have found low risk drinkers to be similar to abstainers on outcomes [23–25], we hypothesized that at least two profiles would be identified: abstinent or low risk drinking with high functioning (i.e., recovery), and heavy drinking with low functioning (i.e., not recovered). A second aim of this study was to investigate pre-treatment, post-treatment, and one- and three-year post-treatment covariate predictors of the latent profiles.
Method
Participants and Procedure
The current study was a secondary analysis of data from the outpatient arm of Project MATCH [22], a randomized clinical trial of three psychosocial treatments for AUD: Cognitive Behavioral Therapy (CBT) [23], Motivational Enhancement Therapy (MET) [24], and Twelve-Step Facilitation (TSF) [25]. Participants (n=952) were recruited from nine research centers in the United States and included individuals who were seeking outpatient treatment. Of the 952 recruited patients, 806 patients (84.7%) had drinking data available during the three-year follow-up period and were included in the present analyses. All participants met DSM-III-R criteria for alcohol abuse (n=74, 9.2%) or dependence (n=732, 90.8%). Measures were assessed at baseline, during 12 weeks of treatment, immediately post-treatment (3-months post-baseline), six months post-treatment (9-months post-baseline), 12 months post-treatment (15-months post-baseline), and three years following treatment (39-months post-baseline).
Measures
Three-Year Follow-Up Latent Profile Indicators
Alcohol and other drug use.
Alcohol and drug use were measured using the Form-90 [26], a calendar-based method to obtain reports of alcohol/drug use in the previous 90-day period. Summary alcohol use variables included percent drinking days (PDD), percent heavy drinking days (PHDD, i.e., 4 or more drinks in a day for women, 5 or more drinks in a day for men), and drinks per drinking day (DDD). Marijuana and other illicit drug use were coded as binary (0=no use, 1=any use).
Alcohol-related negative consequences.
The Drinker Inventory of Consequences (DrInC)[27] was used to measure alcohol-related negative consequences. Clients reported the frequency of 45 alcohol-related consequences (e.g., “I have gotten into trouble because of drinking”) on a 4-point scale (1=never, 4=daily or almost daily). Internal consistency of DrInC in this sample was α=0.97.
Psychosocial functioning and employment.
The Psychosocial Functioning Inventory (PFI)[28] was used to measure social functioning. The social behavior subscale was calculated from 10 items of the PFI and included items that assess the frequency of problematic social behavior and social interactions in the past 30 days (e.g., “Demanded others do things your way”). Higher scores on the social behavior subscale indicate better psychosocial functioning. Internal consistency of the PFI social behavior subscale was α=0.83. We also selected four items to reflect satisfaction with life and social functioning over the past 30 days: “How happy have you been… with life?”; “…with your living situation?” and “…with your relationships?”; and “Did you feel satisfied with leisure, social, and recreational activities?” (0=satisfied/happy; 1=dissatisfied/unhappy). The internal consistency of these four items was α=0.79.
The Addiction Severity Index (ASI)[29] was used to measure employment and experiences of “serious depression,” cognitive difficulty (“trouble understanding, concentrating, or remembering”), and “serious anxiety or tension” in the past 30 days. All items were binary indicators where 0=employed or symptom not present, and 1=unemployed or symptom present. Given prior evidence of poor measurement properties of the ASI composites, we followed a recommendation to examine individual items [30]. The internal consistency of the four ASI items was α=0.63.
Covariates
Covariate predictors of profile membership were included based on prior studies examining predictors of AUD treatment outcomes [10,17,31–34] and availability of measures in the Project MATCH dataset. Three time periods were represented: pre-treatment (i.e., baseline), end of treatment (three months following baseline), and follow-up (one and three years post-treatment).
Pre-treatment predictors of recovery outcomes included (1) demographic variables (age, sex, race, marital status), (2) treatment condition, (3) baseline alcohol dependence severity assessed by the Alcohol Dependence Scale [35], and (4) social network support for drinking assessed by the Important People and Activities Instrument [36].
End of treatment predictors of recovery outcomes included (1) coping as measured by the Process of Change Questionnaire [37,38], and (2) achieving a mostly low risk pattern of drinking or abstinence during treatment, as derived in prior analyses of during treatment drinking [32].
One year post-treatment predictors included (1) depression scores assessed by the Beck Depression Inventory [39], (2) anger scores assessed by the Spielberger State-Trait Anger Expression Scale [40], (3) purpose in life assessed by the Purpose in Life test [41], and (4) psychiatric severity assessed by the Addiction Severity Index [29].
Three-year post-treatment predictors included (1) self-efficacy as assessed by the Alcohol Abstinence Self-Efficacy Scale, Confidence subscale [42]; (2) social support from family and friends assessed by the Social Support Questionnaire short form [43,44]; (3) Alcoholics Anonymous involvement [45]; and (4) cigarettes smoked per day assessed by the Form 90 [26].
Analytic Approach
Descriptive Analyses
Descriptive analyses were conducted using levels of drinking during the three-year follow-up assessment as a grouping variable with three observed groups: abstainers, low risk drinkers (i.e., non-abstinent individuals with no heavy drinking days), and heavy drinkers.
Latent Profiles of Three Year Outcomes
Latent profile analyses were conducted in Mplus version 8 [46] using a weighted maximum likelihood function, which provides the estimated variance-covariance matrix for all available data, thus all data were included in the models (n=806). Model fit of the latent profile models without covariates was examined using the Lo Mendell Rubin Likelihood Ratio test (LRT), Bayesian Information Criterion (BIC) and sample-size–adjusted BIC (aBIC). Lower BIC and aBIC indicate better fitting models and a significant LRT indicates a significantly better fit for a k profile model (e.g., four profiles) versus a k-1 profile model (e.g., three profiles) [47]. A non-significant LRT indicates that adding an additional profile does not significantly improve model fit [47]. Classification precision (relative entropy) was used to evaluate how well the latent profile solution classified individuals into latent profiles (entropy>0.80 was considered good classification precision). Models were tested initially using a split-half validation and replication approach. Final models were tested with the full sample.
Change in Functioning from Baseline by Latent Profiles
Once latent profiles at three years following treatment were identified, we examined average functioning (means and 95% confidence intervals) from baseline (month 0), end of treatment (month 3), and following treatment (months 9 and 15) by latent profile membership. Only outcomes assessed at baseline and 3-, 9-, and 15-months in the Project MATCH data were examined, including alcohol consumption, drinking consequences, marijuana use, other illicit drug use, PFI social behavior, PFI satisfaction with leisure, social, and recreational activities, and depression, tension, and difficulty concentrating.
Correlates of Latent Profiles
Finally, we examined the association between covariates and profiles using a model-based multinomial logistic regression. For all models we examined associations with covariates that were assessed closest in time to the three-year follow-up assessment. Given different levels of missingness for each of the covariates (complete case analysis n=491), we used multiple imputation with 20 imputed datasets for the covariate models, thus the full sample (n=806) was used for the covariate analyses.
Results
Descriptive Analyses
Among the outpatient sample included in the present study (n=806; 84.6% of the MATCH outpatient sample), 29.7% were female, 22.2% were non-White (77.8% non-Hispanic White, 13.5% Hispanic, 5.7% Black, 2.0% American Indian or Alaska Native, 0.7% “other,” and 0.2% Asian or Pacific Islander), and the mean age was 38.1 (SD=10.5). Reasons for not completing the 3-year follow-up assessment included being lost to follow-up (4.7%), refused participation (7.7%), and being deceased (2.9%).
The means (standard deviations) for continuous outcomes and number endorsing (%) for binary outcomes at three years following treatment are provided in Table 1. We also examined the means and endorsement by observed abstinence (n=237; 29.4%), low risk drinking (n=91; 11.3%), and heavy drinking (n=478; 59.3%) status at three-years post-treatment. Abstainers and low risk drinkers were not significantly different from one another on nearly all non-drinking outcomes (ps>0.05), with only one exception: abstainers were significantly more unhappy with life compared to low risk drinkers (χ2(1)=4.31; p=0.04).
Table 1.
Means (SD) and Number Endorsing (%) Outcomes Three Years Post-Treatment in the Total Sample and by Observed Drinking Categories Three Years Post-Treatment
| Continuous Indicators | Total Sample N=806 M (SD) |
Abstainers n=237 M (SD) |
Low risk drinkers n=91 M (SD) |
Heavy drinkers n=478 M (SD) |
| Percent drinking days (PDD) | 30.9% (35.6%) | 0.0% (0.0%) | 26.3% (32.5%) | 47.1% (34.5%) |
| Percent heavy drinking days (PHDD) | 19.9% (29.8%) | 0.0% (0.0%) | 0.0% (0.0%) | 33.5% (32.2%) |
| Drinks per drinking day (DDD) | 4.64 (5.33) | 0.00 (0.00) | 1.78 (1.16) | 7.49 (5.23) |
| DrInC total score | 33.25 (24.89) | 6.20 (8.99) | 13.77 (14.09) | 37.20 (24.64) |
| PFI social behavior subscale score | 3.43 (0.47) | 3.51 (0.41) | 3.54 (0.41) | 3.37 (0.50) |
| Binary Indicators | Total Sample N (%) |
Abstainers N (%) |
Low risk drinkers N (%) |
Heavy drinkers N (%) |
| Unemployment | 118 (14.8) | 37 (15.7%) | 11 (12.4%) | 70 (14.7%) |
| Depressed | 139 (17.3%) | 32 (13.5%) | 12 (13.2%) | 95 (19.9%) |
| Difficulty concentrating | 96 (11.9%) | 28 (11.8%) | 6 (6.8%) | 62 (13.0%) |
| Tension | 210 (26.1%) | 54 (22.8%) | 25 (27.5%) | 131 (27.5%) |
| Unhappy with living situation | 165 (21.5%) | 37 (16.2%) | 12 (14.5%) | 116 (25.4%) |
| Unhappy with life | 166 (21.8%) | 24 (15.0%) | 5 (6.1%) | 127 (28.0%) |
| Unhappy with relationships | 172 (22.5%) | 37 (16.2%) | 11 (12.4%) | 124 (27.3%) |
| Unhappy with leisure activities | 187 (24.2%) | 36 (15.6%) | 17 (20.5%) | 134 (29.1%) |
| Marijuana use | 176 (21.8%) | 22 (9.3%) | 15 (16.5%) | 134 (29.1%) |
| Other drug use | 145 (18.0%) | 27 (11.4%) | 8 (8.8%) | 110 (23.0%) |
Note. DrInC=Drinker Inventory of Consequences; PFI=Psychosocial Functioning Inventory.
Latent Profiles of Three Year Outcomes
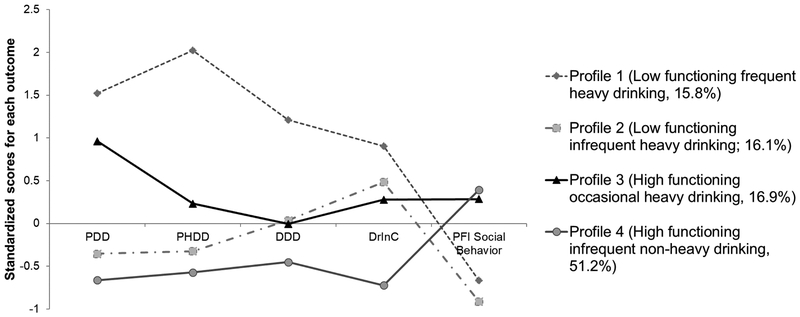
Latent profile models with two through nine profiles were estimated and a four-profile model was retained as the optimal solution in validation and replication sub-samples. The data were then combined and re-estimated with the total sample. Consistent with the validation and replication sub-samples, in the combined sample the three profile model was rejected in favor of a four profile model (LRT=554.61, p=0.03) and the five profile model did not fit significantly better than the four profile model (LRT=463.97, p=0.15). The BIC and aBIC continued to decrease with each additional profile. The classification precision of the four-profile model was excellent (entropy=0.92). The profiles were also substantively meaningful. See Figure 1 for standardized scores (mean=0, SD=1) on the continuous outcomes and Figure 2 for probability of endorsing binary outcomes by profile.
Figure 1.
Standardized Mean Scores (Sample Mean = 0 and Standard Deviation = 1) on each of the Continuous Outcome Indicators by Latent Profiles
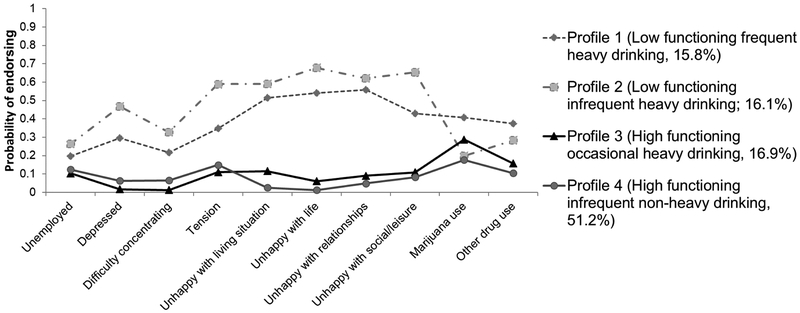
Figure 2.
Probability of Endorsing each of the Binary Outcome Indicators by Latent Profiles.
Profile 1 (15.8% of the total sample), “low functioning frequent heavy drinking,” reported PDD=84.5%, PHDD=79.2%, DDD=11.2, and DrInC=56.1, below average PFI social behavior (see Figure 1), and a higher likelihood of endorsing unemployment, other drug use, psychiatric symptoms, and life dissatisfaction (see Figure 2). Profile 2 (16.1% of the total sample), “low functioning infrequent heavy drinking,” reported PDD=16.4%, PHDD=9.7%, DDD=4.8, and DrInC=43.7, below average PFI social behavior, and the highest likelihood of endorsing unemployment, psychiatric symptoms, and life dissatisfaction. Approximately 20% of those in Profile 2 endorsed other drug use. Profile 3 (16.9% of the total sample), “high functioning occasional heavy drinking,” reported PDD=67.9%, PHDD=25.5%, DDD=5.9, and DrInC=32.5, above average PFI social behavior, and a low probability of endorsing unemployment, other drug use, psychiatric symptoms, and life dissatisfaction. Profile 4 (51.2% of the sample), “high functioning infrequent non-heavy drinking,” reported PDD=6.9%, PHDD=2.8%, DDD=2.1, and DrInC=15.7, above average PFI social behavior, and a low probability endorsing unemployment, other drug use, psychiatric symptoms, and life dissatisfaction.
The high functioning infrequent non-heavy drinking profile (Profile 4) and the low functioning infrequent heavy drinking profile (Profile 2) both included a large number of abstainers. Among individuals most likely classified in Profile 4, 48.9% were abstinent from alcohol and 44.8% were abstinent from alcohol and other drugs. Among individuals most likely classified in Profile 2, 26.9% were abstinent from alcohol and 19.2% were abstinent from alcohol and drugs. No individuals in Profile 1 and Profile 3 were abstinent from alcohol.
Change in Functioning from Baseline by Latent Profiles
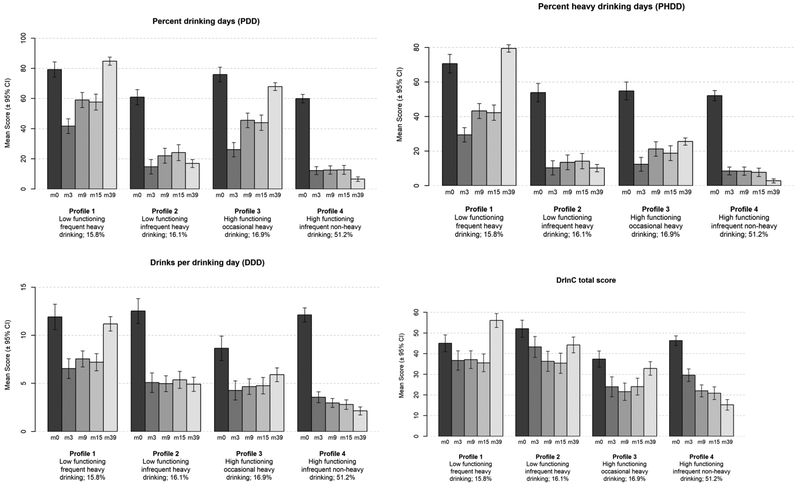
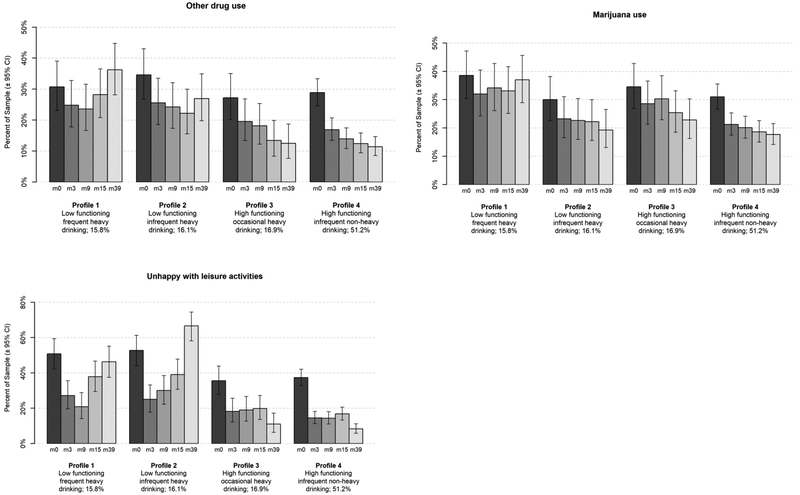
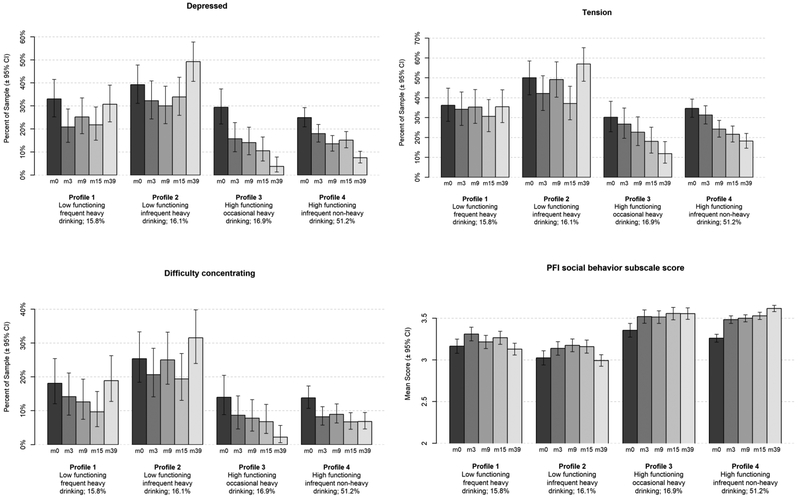
To determine whether the profiles at three years following treatment were indicative of change from baseline on outcomes we examined average functioning (means and 95% confidence intervals) from baseline (month 0) through the three year (month 39) follow-up by latent profile membership. As seen in Figure 3, individuals in Profiles 3 and 4 had lower drinking intensity over time than individuals in Profile 1, and individuals in Profile 2 and 4 reported less drinking frequency over time than individuals in Profiles 1 and 3. Figures 4 and 5 show that individuals in the high functioning profiles (Profiles 3 and 4) showed the greatest recovery of functioning through the three-year follow-up. Individuals in the low functioning profiles (Profiles 1 and 2) had less initial improvement and deterioration of functioning over time.
Figure 3.
Change in Consumption Outcomes and Drinking Consequences over Time at Baseline (m0), End of Treatment (m3), and 9- (m9), 15- (m15), and 39- (m39) months following Treatment by Latent Profiles
Figure 4.
Change in Drug Use Outcomes and Satisfaction with Leisure Activities over Time at Baseline (m0), End of Treatment (m3), and 9- (m9), 15- (m15), and 39- (m39) months following Treatment by Latent Profiles
Figure 5.
Change in Mental Health Symptoms (ASI) and Social Functioning (PFI) over Time at Baseline (m0), End of Treatment (m3), and 9- (m9), 15- (m15), and 39- (m39) months following Treatment by Latent Profiles
Correlates of Latent Profiles
Next, we examined the associations between patient characteristics and latent profiles using model-based multinomial logistic regression. In these models, all covariates were included as predictors of latent profile membership with one profile as the reference profile. For descriptive purposes, the means (standard deviations) for continuous covariates and frequency of endorsing binary covariates at three years following treatment by the four latent profiles (using the highest probability of profile membership) are provided in Table 2. Multinomial logistic regression parameters for patient characteristics predicting odds of membership in each of the latent profiles (rows; odds ratios and 95% confidence intervals (CI)) versus the reference profile (columns)) are provided in Table 3.
Table 2.
Frequencies and Means (Standard Deviation) for Demographic and Risk Covariates by Latent Profiles
| Baseline Covariates (sample size out of n=806 in 3 year follow-up sample) |
Profile 1: Low Functioning Frequent Heavy Drinking |
Profile 2: Low Functioning Infrequent Heavy Drinking |
Profile 3: High Functioning Occasional Heavy Drinking |
Profile 4: High Functioning Infrequent Non-Heavy Drinking |
|---|---|---|---|---|
| Sex % Male (n=806) | 76% | 69% | 74% | 71% |
| Marital status % Married (n=804) | 41% | 43% | 46% | 43% |
| Race % White (n=806) | 84% | 80% | 85% | 76% |
| Age (n=806) | 38.80 (9.67) | 37.97 (10.12) | 40.63 (11.25) | 37.99 (10.95) |
| Social support for drinking (IPA, n=787) | 6.30 (1.05) | 6.29 (0.99) | 6.40 (1.05) | 6.12 (1.10) |
| Alcohol dependence (ADS, n=799) | 15.23 (6.84) | 16.35 (6.88) | 12.28 (6.21) | 15.03 (7.53) |
| End of Treatment Covariates | ||||
| Low risk drinking or abstinence (n=771) | 29% | 47% | 41% | 60% |
| Coping (PCQ, n=776) | 2.94 (0.61) | 3.25 (0.51) | 2.86 (0.67) | 3.17 (0.64) |
| One Year Post-Treatment Covariates | ||||
| Psychiatric severity (ASI, n=771) | 0.13 (0.19) | 0.19 (0.20) | 0.07 (0.13) | 0.09 (0.15) |
| Depression (BDI, n=746) | 10.40 (7.78) | 10.83 (8.32) | 5.78 (5.58) | 5.11 (6.90) |
| Anger (STAX, n=754) | 27.89 (6.90) | 29.18 (6.98) | 24.47 (5.59) | 24.16 (6.08) |
| Purpose in life (PIL, n=754) | 97.05 (16.35) | 96.23 (17.40) | 108.27 (14.52) | 107.85 (17.66) |
| Three Years Post-Treatment Covariates | ||||
| Social support from family (SSQ, n=775) | 8.02 (2.23) | 7.49 (2.12) | 8.52 (1.87) | 8.67 (1.79) |
| Social support friends (SSQ, n=758) | 7.19 (1.99) | 6.77 (1.92) | 7.40 (2.02) | 7.74 (1.82) |
| AA involvement (AAI, n=776) | 1.30 (1.70) | 2.14 (2.07) | 1.35 (1.70) | 2.24 (2.30) |
| Self-efficacy (AASE, n=786) | 2.49 (0.72) | 3.12 (0.96) | 3.08 (0.79) | 3.86 (1.04) |
| Cigarettes/day (n=784) | 14.62 (14.46) | 12.74 (15.13) | 11.90 (14.31) | 10.96 (12.28) |
Note. IPA=Important People and Activities; ADS=Alcohol Dependence Scale; PCQ=Process of Change Questionnaire; ASI=Addiction Severity Index; BDI=Beck Depression Inventory; STAX=State Trait Anger Expession Inventory; PIL=Purpose in Life Test; SSQ=Social Support Questionnaire; AAI=Alcoholics’ Anonymous Involvement Scale; AASE=Alcohol Abstinence Self-Efficacy Scale. The BDI, STAX, and PIL were not administered at the 3-year post-treatment assessment time point.
Table 3.
Odds Ratios (95% Confidence Intervals) for Covariate Effects in Multinomial Logistic Regressions with Patient Characteristics predicting Odds of Membership in each Profile (Rows) versus the Reference Group (Columns)
| Covariate – Time Period Assessed | Profile 1: Low Functioning Frequent Heavy Drinking (Reference) |
Profile 2: Low Functioning Infrequent Heavy Drinking (Reference) |
Profile 3: High Functioning Occasional Heavy Drinking (Reference) |
Profile 4: High Functioning Infrequent Non-Heavy Drinking (Reference) |
|---|---|---|---|---|
| Sex, male =1 – Baseline | ||||
| Versus Profile 1 | -- | 1.26 (0.64, 2.48) | 1.37 (0.68, 2.79) | 1.77 (0.92, 3.41) |
| Versus Profile 2 | 0.80 (0.40, 1.57) | -- | 1.09 (0.54, 2.21) | 1.41 (0.73, 2.71) |
| Versus Profile 3 | 0.73 (0.36, 1.48) | 0.91 (0.45, 1.85) | -- | 1.29 (0.70, 2.38) |
| Versus Profile 4 | 0.57 (0.30, 1.08) | 0.71 (0.37, 1.36) | 0.78 (0.42, 1.42) | -- |
| Treatment contrast, CBT =1 – Baseline | ||||
| Versus Profile 1 | -- | 0.98 (0.50, 1.91) | 1.13 (0.57, 2.26) | 1.53 (0.77, 3.04) |
| Versus Profile 2 | 1.02 (0.52, 2.00) | -- | 1.16 (0.57, 2.35) | 1.57 (0.81, 3.02) |
| Versus Profile 3 | 0.88 (0.44, 1.76) | 0.86 (0.42, 1.76) | -- | 1.35 (0.72, 2.52) |
| Versus Profile 4 | 0.65 (0.33, 1.30) | 0.64 (0.33, 1.23) | 0.74 (0.40, 1.38) | -- |
| Treatment contrast, MET =1 – Baseline | ||||
| Versus Profile 1 | -- | 0.86 (0.43, 1.73) | 1.72 (0.84, 3.50) | 1.47 (0.75, 2.88) |
| Versus Profile 2 | 1.16 (0.58, 2.35) | -- | 2.00 (0.94, 4.24) | 1.71 (0.87, 3.36) |
| Versus Profile 3 | 0.58 (0.29, 1.18) | 0.50 (0.24, 1.06) | -- | 0.09 (0.05, 1.64) |
| Versus Profile 4 | 0.68 (0.35, 1.32) | 0.58 (0.30, 1.14) | 1.17 (0.62, 2.22) | -- |
| Marital status, married =1 – Baseline | ||||
| Versus Profile 1 | -- | 0.90 (0.50, 1.63) | 0.76 (0.42, 1.36) | 0.84 (0.47, 1.50) |
| Versus Profile 2 | 1.11 (0.62, 2.00) | -- | 0.84 (0.45. 1.55) | 0.93 (0.53, 1.64) |
| Versus Profile 3 | 1.32 (0.73, 2.38) | 1.19 (0.65, 2.20) | -- | 1.11 (0.07, 1.88) |
| Versus Profile 4 | 1.19 (0.67, 2.14) | 1.08 (0.61, 1.90) | 0.90 (0.53, 1.53) | -- |
| Race, Non-Hispanic White =1 – Baseline | ||||
| Versus Profile 1 | -- | 1.28 (0.58, 2.83) | 0.75 (0.32, 1.79) | 1.81 (0.83, 3.98) |
| Versus Profile 2 | 0.78 (0.35, 1.73) | -- | 0.59 (0.24, 1.46) | 1.42 (0.68, 2.96) |
| Versus Profile 3 | 1.33 (0.56, 3.15) | 1.70 (0.68, 4.20) | -- | 2.41 (1.09, 5.31)* |
| Versus Profile 4 | 0.55 (0.25, 1.21) | 0.70 (0.35, 1.42) | 0.42 (0.19, 0.91)* | -- |
| Age – Baseline | ||||
| Versus Profile 1 | -- | 1.01 (0.98, 1.04) | 1.00 (0.97, 1.03) | 1.03 (1.001, 1.06)* |
| Versus Profile 2 | 0.99 (0.96, 1.02) | -- | 0.99 (0.96, 1.02) | 1.02 (0.99, 1.05) |
| Versus Profile 3 | 1.00 (0.97, 1.03) | 1.01 (0.98, 1.04) | -- | 1.03 (1.00, 1.06) |
| Versus Profile 4 | 0.97 (0.94, 0.999)* | 0.98 (0.95, 1.01) | 0.97 (0.94, 1.00) | -- |
| Alcohol dependence severity (ADS) – Baseline | ||||
| Versus Profile 1 | -- | 1.00 (0.96, 1.04) | 1.04 (0.99, 1.09) | 0.98 (0.94, 1.02) |
| Versus Profile 2 | 1.00 (0.96, 1.04) | -- | 1.04 (0.99, 1.09) | 0.98 (0.94, 1.02) |
| Versus Profile 3 | 0.96 (0.92, 1.01) | 0.96 (0.92, 1.01) | -- | 0.94 (0.90, 0.98)** |
| Versus Profile 4 | 1.02 (0.98, 1.07) | 1.02 (0.98, 1.07) | 1.06 (1.02, 1.11)** | -- |
| Social support for drinking (IPA) – Baseline | ||||
| Versus Profile 1 | -- | 1.05 (0.81, 1.36) | 0.98 (0.74, 1.28) | 1.31 (1.003, 1.71)* |
| Versus Profile 2 | 0.96 (0.74, 1.24) | -- | 0.93 (0.69, 1.25) | 1.25 (0.95, 1.64) |
| Versus Profile 3 | 1.03 (0.78, 1.35) | 1.07 (0.80, 1.44) | -- | 1.34 (1.03, 1.75)* |
| Versus Profile 4 | 0.76 (0.59, 0.99)* | 0.80 (0.61, 1.05) | 0.74 (0.57, 0.97)* | -- |
| Low risk drinking or abstinence – Treatment | ||||
| Versus Profile 1 | -- | 0.43 (0.23, 0.80)** | 0.80 (0.42, 1.51) | 0.31 (0.16, 0.56)*** |
| Versus Profile 2 | 2.32 (1.25, 4.29)** | -- | 1.86 (0.97, 3.58) | 0.71 (0.38, 1.31) |
| Versus Profile 3 | 1.26 (0.66, 2.36) | 0.54 (0.28, 1.04) | -- | 0.38 (0.22, 0.67)** |
| Versus Profile 4 | 3.28 (1.78, 6.03)*** | 1.41 (0.77, 2.60) | 2.62 (1.50, 4.59)** | -- |
| Coping (PCQ) – End of Treatment | ||||
| Versus Profile 1 | -- | 0.42 (0.25, 0.71)** | 1.22 (0.75, 1.99) | 0.66 (0.39, 1.10) |
| Versus Profile 2 | 2.38 (1.41, 3.99)** | -- | 2.89 (1.65, 5.07)*** | 1.56 (0.92, 2.63) |
| Versus Profile 3 | 0.82 (0.50, 1.34) | 0.35 (0.20, 0.06)*** | -- | 0.54 (0.32, 0.90)* |
| Versus Profile 4 | 1.53 (0.91, 2.55) | 0.64 (0.38, 1.08) | 1.86 (1.13, 3.04)* | -- |
| Psychiatric severity (ASI) – 1 year | ||||
| Versus Profile 1 | -- | 0.78 (0.65, 0.93)** | 1.03 (0.82, 1.28) | 1.03 (0.81, 1.31) |
| Versus Profile 2 | 1.29 (1.07, 1.55)** | -- | 1.32 (1.06, 1.66)* | 1.33 (1.03, 1.71)* |
| Versus Profile 3 | 0.97 (0.78, 1.21) | 0.77 (0.60. 0.95)* | -- | 1.00 (0.78, 1.29) |
| Versus Profile 4 | 0.97 (0.77, 1.23) | 0.75 (0.59, 0.96)* | 1.00 (0.78, 1.27) | -- |
| Depression (BDI) – 1 year | ||||
| Versus Profile 1 | -- | 1.04 (0.98, 1.09) | 1.03 (0.97, 1.10) | 1.07 (1.004, 1.14)* |
| Versus Profile 2 | 0.96 (0.91, 1.02) | -- | 0.99 (0.93, 1.06) | 1.03 (0.96, 1.11) |
| Versus Profile 3 | 0.97 (0.91, 1.03) | 1.01 (0.94, 1.08) | -- | 1.04 (0.97, 1.11) |
| Versus Profile 4 | 0.93 (0.87, 0.996)* | 0.97 (0.91, 1.04) | 0.96 (0.90, 1.03) | -- |
| Anger (STAX) – 1 year | ||||
| Versus Profile 1 | -- | 0.99 (0.94, 1.04) | 1.06 (1.01, 1.12)* | 1.08 (1.03, 1.14)* |
| Versus Profile 2 | 1.01 (0.96, 1.06) | -- | 1.07 (1.01, 1.13)* | 1.09 (1.04, 1.15)** |
| Versus Profile 3 | 0.94 (0.89, 0.99)* | 0.93 (0.88, 0.99)* | -- | 1.02 (0.97, 1.07) |
| Versus Profile 4 | 0.92 (0.88, 0.97)* | 0.92 (0.87, 0.96)** | 0.98 (0.94. 1.03) | -- |
| Purpose in Life (PIL) – 1 year | ||||
| Versus Profile 1 | -- | 1.01 (0.99, 1.03) | 0.98 (0.95, 0.997)* | 0.99 (0.97, 1.01) |
| Versus Profile 2 | 0.99 (0.97, 1.01) | -- | 0.97 (0.94, 0.99)** | 0.98 (0.96, 1.01) |
| Versus Profile 3 | 1.03 (1.003, 1.05)* | 1.04 (1.01, 1.06)** | -- | 1.02 (0.99, 1.04) |
| Versus Profile 4 | 1.01 (0.99, 1.03) | 1.02 (0.99, 1.04) | 0.99 (0.96, 1.01) | -- |
| Social support from family (SSQ) – 3 years | ||||
| Versus Profile 1 | -- | 1.11 (0.96, 1.29) | 0.95 (0.81, 1.11) | 0.84 (0.80, 0.996)* |
| Versus Profile 2 | 0.90 (0.77, 1.04) | -- | 0.85 (0.72, 1.00) | 0.75 (0.64, 0.88)*** |
| Versus Profile 3 | 1.06 (0.90, 1.24) | 1.17 (1.00, 1.38) | -- | 0.88 (0.74, 1.05) |
| Versus Profile 4 | 1.19 (1.004, 1.42)* | 1.33 (1.14, 1.55)*** | 1.13 (0.96, 1.34) | -- |
| Social support from friends (SSQ) – 3 years | ||||
| Versus Profile 1 | -- | 1.11 (0.93, 1.31) | 1.00 (0.84, 1.19) | 0.86 (0.73, 1.03) |
| Versus Profile 2 | 0.90 (0.76, 1.07) | -- | 0.90 (0.76, 1.07) | 0.78 (0.66, 0.92)** |
| Versus Profile 3 | 1.00 (0.84, 1.18) | 1.11 (0.93, 1.31) | -- | 0.86 (0.73, 1.01) |
| Versus Profile 4 | 1.16 (0.98, 1.37) | 1.28 (1.09, 1.51)** | 1.16 (0.99, 1.36) | -- |
| AA involvement (AAI) – 3 years | ||||
| Versus Profile 1 | -- | 0.83 (0.70, 0.97)* | 0.86 (0.72, 1.04) | 0.75 (0.62, 0.89)** |
| Versus Profile 2 | 1.21 (1.03, 1.43)* | -- | 1.04 (0.89, 1.23) | 0.90 (0.78, 1.04) |
| Versus Profile 3 | 1.16 (0.96, 1.40) | 0.96 (0.81, 1.13) | -- | 0.87 (0.85, 0.998)* |
| Versus Profile 4 | 1.34 (1.12, 1.60)** | 1.11 (0.96, 1.28) | 1.16 (1.002, 1.33)* | -- |
| Self-efficacy (AASE) – 3 years | ||||
| Versus Profile 1 | -- | 0.41 (0.29, 0.57)*** | 0.55 (0.40, 0.74)*** | 0.20 (0.14, 0.29)*** |
| Versus Profile 2 | 2.46 (1.75, 3.46)*** | -- | 1.34 (0.98, 1.83) | 0.50 (0.36, 0.69)*** |
| Versus Profile 3 | 1.83 (1.35, 2.49)*** | 0.75 (0.55, 1.02) | -- | 0.37 (0.28, 0.49)*** |
| Versus Profile 4 | 4.94 (3.43, 7.11)*** | 2.01 (1.46, 2.77)*** | 2.69 (2.04, 3.55)*** | -- |
| Cigarettes per day – 3 years | ||||
| Versus Profile 1 | -- | 1.02 (1.002, 1.05)* | 1.01 (0.99, 1.03) | 1.03 (1.008, 1.05)** |
| Versus Profile 2 | 0.98 (0.96, 0.998)* | -- | 0.99 (0.97, 1.01) | 1.01 (0.99, 1.03) |
| Versus Profile 3 | 0.99 (0.97, 1.01) | 1.01 (0.99, 1.03) | -- | 1.02 (1.00, 1.04) |
| Versus Profile 4 | 097 (0.95, 0.99)** | 0.99 (0.97, 1.01) | 0.98 (0.96, 1.00) | -- |
Note.
p<.05;
p<.01;
p<.001. All covariates listed in Table 2 were included in the models. IPA=Important People and Activities; ADS=Alcohol Dependence Scale; PCQ=Process of Change Questionnaire; ASI=Addiction Severity Index; BDI=Beck Depression Inventory; STAX=State Trait Anger Expression Inventory; PIL=Purpose in Life Test; SSQ=Social Support Questionnaire; AAI=Alcoholics’ Anonymous Involvement Scale; AASE=Alcohol Abstinence Self-Efficacy Scale. The BDI, STAX, and PIL were not administered at the 3-year post-treatment assessment time point.
Of the demographic measures and treatment conditions, only age and race were significantly associated with profile membership. Individuals who were non-Hispanic white had a 2.41 (95% CI 1.09, 5.31) greater odds of membership in Profile 3 (“high functioning occasional heavy drinking”), as compared to Profile 4 (“high functioning infrequent non-heavy drinking”). Younger age predicted a significantly greater probability of membership in Profile 4, as compared to Profile 1 (“low functioning frequent heavy drinking”).
Greater abstinence self-efficacy was associated with a significantly higher probability of being in all other profiles versus Profile 1 (“low functioning frequent heavy drinking” Table 3, column 2). More AA involvement and smoking fewer cigarettes per day were associated with a significantly higher probability of being in the infrequent drinking profiles (Profile 2 and 4) versus Profile 1. Lower anger at 1-year follow-up predicted a significantly higher probability of being in the high functioning profiles (Profiles 3 and 4) versus Profile 1. Similarly, greater purpose in life at 1-year follow-up predicted a significantly higher probability of being in Profile 3 “high functioning occasional heavy drinking,” as compared to Profile 1. Lower depression, less social support, and achieving low risk drinking or abstinence during treatment predicted a significantly greater probability of membership in Profile 4 “high functioning infrequent non-heavy drinking,” as compared to Profile 1.
Lower psychiatric severity at 1-year follow-up predicted a significantly higher probability of being in all other profiles versus Profile 2 (“low functioning infrequent heavy drinking”; Table 3, column 3). Not achieving abstinence or low risk drinking during treatment and lower coping scores at the end of treatment predicted a higher probability of being in the low functioning heavy drinking profile (Profile 1), as compared to Profile 2. Lower anger at 1-year follow-up predicted a significantly higher probability of being in the high functioning profiles (Profiles 3 and 4) versus Profile 2. Greater purpose in life at 1-year follow-up predicted a significantly higher probability of being in Profile 3 “high functioning occasional heavy drinking,” as compared to Profile 2. Greater social support from family and friends at 3-year follow-up predicted a higher probability of membership in Profile 4 “high functioning infrequent non-heavy drinking,” as compared to Profile 2.
Table 3, columns 4 and 5, provide covariate effects with the “high functioning occasional heavy drinking” profile (Profile 3) and “high functioning infrequent non-heavy drinking” profile (Profile 4) as reference profiles, respectively. Greater alcohol dependence severity and lower social support for drinking at baseline, achieving abstinence or low risk drinking during treatment, and greater abstinence self-efficacy and AA involvement at 3-year follow-up predicted a higher probability of membership in Profile 4, as compared to Profile 3.
Discussion
When examining recovery from AUD as a multidimensional construct reflective of functioning and a range of alcohol consumption indicators, we found support for four distinct profiles. Individuals could be differentiated based on functioning and levels of drinking. Just over half of the sample fit into a profile of infrequent non-heavy drinking with high functioning (51.2%), and the remainder of the sample was split between profiles that included: frequent heavy drinking/low functioning (15.8%), infrequent heavy drinking/low functioning (16.1%), and occasional heavy drinking/high functioning (16.9%). Approximately 49% of the high functioning infrequent heavy drinking profile and 27% of the low functioning infrequent heavy drinking profile reported abstinence. The high functioning profiles were characterized by greater social functioning, less unemployment, lower probability of endorsing depression and anxiety symptoms, less cognitive difficulty, and greater satisfaction with life, relationships, living situation, and social/leisure activities than the low functioning profiles.
Our results suggest that knowing an individual is engaging in some heavy drinking or knowing that an individual is abstinent provides incomplete information about patient functioning. Consistent with our prior work [48] we found success in those who failed to achieve the no heavy drinking definition (e.g., exceeding 4/5 drinks per day for women/men), given that approximately one-third of those in the current study who engaged in some heavy drinking (Profile 3) were functioning well and the other two-thirds (Profiles 1 and 2) were functioning poorly. Similarly, achieving infrequent drinking or abstinence also did not guarantee higher functioning. Approximately 75% of those who achieved infrequent drinking were high functioning (Profile 4), whereas 25% of those who achieved infrequent drinking had very poor functioning (Profile 2). Approximately 20% of those in Profile 2 engaged in other drug use, which could have also impacted functioning.
Beyond portraying a broader representation of AUD recovery, this work also helped clarify factors that may contribute to both consumption and functional outcomes. At baseline, greater social support for drinking differentiated heavier drinking from less frequent drinking, and lower alcohol dependence severity at baseline predicted high functioning heavy drinking. Better mental health, including fewer psychiatric symptoms, less depression and anger, greater purpose in life, and social support from family and friends were associated with higher functioning at three years following treatment.
Limitations and Future Directions
The current study was limited by the available data in the outpatient sample of Project MATCH. As such, the covariates were assessed at varying time periods. Project MATCH provided a relatively comprehensive assessment of psychological and social functioning, but measures of physical health were not available. Future research that incorporates measures of physical health functioning would provide more information about recovery of functioning [49]. Similarly, reliance on self-report prevented us from ascertaining the perspectives of family, friends, employers, and providers with respect to functioning status (e.g., individuals who were engaging in heavy drinking may not be regarded as “high functioning” among family members).
Using latent profile analysis to identify the profiles is both a limitation and a strength. The identified profiles are probabilistic, and there is always some misclassification of individuals in latent profile analysis. However, using a probabilistic approach also eliminated the need to create cutoffs (e.g., no heavy drinking days; [50,51]) and the validation-replication approach provides greater confidence in the profile solution. Finally, recovery is perhaps better conceptualized as a process of change [52], whereas the current study examined outcomes at a single point in time. Replication in a new sample and consideration of additional covariates, especially cognitive functioning/executive control, medical health and chronic pain, and misuse of prescription drugs are important future directions for this work.
Consensus statements have suggested broad definitions of recovery [1,4,9,52]. The present study supports and extends these previous studies by calling into question how recovery from AUD is conceptualized. Acknowledgment of client heterogeneity was an essential element that guided the primary aims of Project MATCH [22]. Specifically, because of client heterogeneity, the research team hypothesized that certain clients would respond more favorably to certain treatments. It may also be time for the field to acknowledge the heterogeneity in how individuals recover from an AUD. Using any single indicator as a benchmark to define success in recovery, such as abstinence, makes an implicit assumption that recovery is an easily defined construct and that alcohol use is directly and uniquely connected with psychosocial functioning. AUD is a complex syndrome with diverse presentation; we should expect recovery from AUD to be similarly complex. The importance of taking a broad perspective in defining AUD outcomes based on multiple areas of life functioning, has been advocated for decades [52]. The results from the current study provide empirical support for a broader definition of recovery based on functioning and a range of alcohol use, including some heavy drinking.
Acknowledgments
Preparation of this manuscript was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism (R01 AA022328, R01 AA025539, 2K05 AA016928, K01 AA024796, K01 AA023233, and T32 AA018108). The authors declare no conflicts of interest.
Contributor Information
Katie Witkiewitz, University of New Mexico.
Adam D. Wilson, University of New Mexico
Matthew R. Pearson, University of New Mexico
Kevin S. Montes, University of New Mexico
Megan Kirouac, University of New Mexico.
Corey R. Roos, University of New Mexico
Kevin A. Hallgren, University of Washington
Stephen A. Maisto, Syracuse University
References
- 1.Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. J Subst Abuse Treat 2007;33(3):221–8. [DOI] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Adminitsration. SAMHSA working definition of recovery: 10 guiding principles of recovery Rockville, MD: Department of Health and Human Services; 2011. [Google Scholar]
- 3.White WL. Addiction recovery: Its definition and conceptual boundaries. J Subst Abuse Treat 2007;33(3):229–41. [DOI] [PubMed] [Google Scholar]
- 4.Kaskutas LA, Borkman TJ, Laudet A, Ritter LA, Witbrodt J, Subbaraman MS, et al. Elements that define recovery: the experiential perspective. J Stud Alcohol Drugs 2014;75(6):999–1010. A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neale J, Vitoratou S, Finch E, Lennon P, Mitcheson L, Panebianco D, et al. Development and validation of SURE: A patient reported outcome measure for recovery from drug and alcohol dependence. Drug Alcohol Depend 2016;165:159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirouac M, Witkiewitz K. Identifying “Hitting Bottom” Among Individuals with Alcohol Problems: Development and Evaluation of the Noteworthy Aspects of Drinking Important to Recovery (NADIR). Subst Use Misuse 2017; 52(12):1602–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tucker JA, Simpson CA. The recovery spectrum: from self-change to seeking treatment. Alcohol Res Heal 2011;33(4):371–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Moos RH, Moos BS. Protective resources and long-term recovery from alcohol use disorders. Drug Alcohol Depend 2007;86(1):46–54. [DOI] [PubMed] [Google Scholar]
- 9.Neale J, Finch E, Marsden J, Mitcheson L, Rose D, Strang J, et al. How should we measure addiction recovery? Analysis of service provider perspectives using online Delphi groups. Drugs Educ Prev Policy 2014;21(4):310–23. [Google Scholar]
- 10.Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction 2005;100(3):281–92. [DOI] [PubMed] [Google Scholar]
- 11.Kelly JF, Stout RL, Greene MC, Slaymaker V. Young adults, social networks, and addiction recovery: post treatment changes in social ties and their role as a mediator of 12-step participation. PLoS One 2014;9(6):e100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roos CR, Witkiewitz K. Adding tools to the toolbox: The role of coping repertoire in alcohol treatment. J Consult Clin Psychol 2016;84(7):599–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Mechanisms of behavior change in alcoholics anonymous: does Alcoholics Anonymous lead to better alcohol use outcomes by reducing depression symptoms? Addiction 2010;105(4):626–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kelly JF, Stout RL, Tonigan JS, Magill M, Pagano ME. Negative affect, relapse, and Alcoholics Anonymous (AA): does AA work by reducing anger? J Stud Alcohol Drugs 2010;71(3):434–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roos CR, Kirouac M, Pearson MR, Fink BC, Witkiewitz K. Examining temptation to drink from an existential perspective: Associations among temptation, purpose in life, and drinking outcomes. Psychol Addict Behav 2015;29(3):716–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Spirituality in recovery: a lagged mediational analysis of alcoholics anonymous’ principal theoretical mechanism of behavior change. Alcohol Clin Exp Res 2011;35(3):454–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Connors GJ, Tonigan JS, Miller WR, MATCH Research Group. A longitudinal model of intake symptomatology, AA participation and outcome: retrospective study of the project MATCH outpatient and aftercare samples. J Stud Alcohol 2001;62(6):817–25. [DOI] [PubMed] [Google Scholar]
- 18.Maisto SA, McKay JR, O’Farrell TJ. Twelve-month abstinence from alcohol and long-term drinking and marital outcomes in men with severe alcohol problems. J Stud Alcohol 1998;59(5):591–8. [DOI] [PubMed] [Google Scholar]
- 19.Dawson DA, Goldstein RB, Ruan WJ, Grant BF. Correlates of Recovery from Alcohol Dependence: A Prospective Study Over a 3-Year Follow-Up Interval. Alcohol Clin Exp Res 2012;36(7):1268–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neale J, Nettleton S, Pickering L. What is the role of harm reduction when drug users say they want abstinence? Int J Drug Policy 2011;22(3):189–93. [DOI] [PubMed] [Google Scholar]
- 21.Laudet AB, White WL. Recovery Capital as Prospective Predictor of Sustained Recovery, Life Satisfaction, and Stress Among Former Poly-Substance Users. Subst Use Misuse 2008;43(1):27–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol 1997;58(1):7–29. [PubMed] [Google Scholar]
- 23.Kadden RM, Carroll KM, Donovan DM, Cooney NL, Monti PM, Abrams D, et al. Cognitive-behavioral coping skills therapy manual Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 24.Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivation enhancement therapy manual Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1994. [Google Scholar]
- 25.Nowinski J, Baker S, Carroll KM. Twelve step facilitation therapy manual Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 26.Miller WR. Form 90: A structured assessment interview for drinking and related behaviors Project MA. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1996. [Google Scholar]
- 27.Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC) Project MA. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 28.Feragne MA, Longabaugh R, Stevenson JF. The Psychosocial Functioning Inventory. Eval Health Prof 1983;6(1):25–48. [DOI] [PubMed] [Google Scholar]
- 29.McLellan a T, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat 1992;9(3):199–213. [DOI] [PubMed] [Google Scholar]
- 30.Mäkelä K Studies of the reliability and validity of the Addiction Severity Index. Addiction 2004;99(4):398–410. [DOI] [PubMed] [Google Scholar]
- 31.Moos RH, Moos BS. Sixteen-year changes and stable remission among treated and untreated individuals with alcohol use disorders. Drug Alcohol Depend 2005;80(3):337–47. [DOI] [PubMed] [Google Scholar]
- 32.Witkiewitz K, Pearson MR, Hallgren KA, Maisto SA, Roos CR, Kirouac M, et al. Who achieves low risk drinking during alcohol treatment? An analysis of patients in three alcohol clinical trials. Addiction 2017;112(12):2112–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tonigan JS, Rynes KN, McCrady BS. Spirituality as a change mechanism in 12-step programs: a replication, extension, and refinement. Subst Use Misuse 2013;48(12):1161–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maisto SA, Clifford PR, Stout RL, Davis CM. Drinking in the year after treatment as a predictor of three-year drinking outcomes. J Stud Alcohol 2006;67(6):823–32. [DOI] [PubMed] [Google Scholar]
- 35.Skinner HA, Horn JL. Alcohol Dependence Scale (ADS) user’s guide. Toronto: Addiction Research Foundation; 1984. [Google Scholar]
- 36.Clifford PR, Longabaugh R. Manual for the Administration of the Important People and Activities Instrument Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1991. [Google Scholar]
- 37.Prochaska JO, Velicer WF, DiClemente CC, Fava J. Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol 1988;56(4):520–8. [DOI] [PubMed] [Google Scholar]
- 38.DiClemente CC, Carroll KM, Connors GJ, Kadden RM. Process assessment in treatment matching research. J Stud Alcohol Suppl 1994;12:156–62. [DOI] [PubMed] [Google Scholar]
- 39.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71. [DOI] [PubMed] [Google Scholar]
- 40.Spielberger CD. Manual for the State-Trait Anger Expression Scale Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- 41.Crumbaugh JC, Maholik LT. An experimental study in existentialism: The psychometric approach to Frankl’s concept of noogenic neurosis. J Clin Psychol 1964;20:200–7. [DOI] [PubMed] [Google Scholar]
- 42.DiClemente CC, Carbonari JP, Montgomery RP, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. J Stud Alcohol 1994;55(2):141–8. [DOI] [PubMed] [Google Scholar]
- 43.Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. Am J Community Psychol 1983;11(1):1–24. A [DOI] [PubMed] [Google Scholar]
- 44.Rice C, Longabaugh R. Measuring general social support in alcoholic patients: Short forms for perceived social support. Psychol Addict Behav 1996. [;10(2):104–14. [Google Scholar]
- 45.Tonigan JS, Connors GJ, Miller WR. Alcoholics Anonymous Involvement (AAI) scale: Reliability and norms. Psychol Addict Behav 1996;10(2):75–80. A [Google Scholar]
- 46.Muthén LK, Muthén BO. Mplus users guide (Version 8). 2017; [Google Scholar]
- 47.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Model 2007;14(4):535–69. [Google Scholar]
- 48.Wilson AD, Bravo AJ, Pearson MR, Witkiewitz K. Finding success in failure: using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction 2016. ;111(12):2145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, Bierut LJ, Grucza RA. Alcohol Consumption, Heavy Drinking, and Mortality: Rethinking the J-Shaped Curve. Alcohol Clin Exp Res 2014;38(2):471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maisto SA, Roos CR, Hallgren KA, Moskal D, Wilson AD, Witkiewitz K. Do Alcohol Relapse Episodes During Treatment Predict Long-Term Outcomes? Investigating the Validity of Existing Definitions of Alcohol Use Disorder Relapse. Alcohol Clin Exp Res 2016;40(10):2180–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pearson MR, Kirouac M, Witkiewitz K. Questioning the validity of the 4+/5+ binge or heavy drinking criterion in college and clinical populations. Addiction 2016. ;111(10):1720–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moos RH, Finney JW. The expanding scope of alcoholism treatment evaluation. Am Psychol 1983;38(10):1036. [DOI] [PubMed] [Google Scholar]