Abstract
Objectives
The objective of this Health Technology Assessment was to evaluate effectiveness, complications and cost-effectiveness of surgical or non-surgical treatment for proximal, diaphyseal or distal fractures of the humerus in elderly patients. Secondary objectives were to evaluate the intervention costs per treatment of proximal humerus fractures (PHF) and to investigate treatment traditions of PHF in Sweden.
Methods and findings
The assessment contains a systematic review of clinical and health economic studies comparing treatment options for humerus fractures in elderly patients. The results regarding the effectiveness of treatments are summarized in meta-analyses. The assessment also includes a cost analysis for treatment options and an analysis of registry data of PHF. For hemiarthroplasty (HA) and non-operative treatment, there was no clinically important difference for moderately displaced PHF at one-year follow-up regarding patient rated outcomes, (standardized mean difference [SMD]) -0.17 (95% CI: -0.56; 0.23). The intervention cost for HA was at least USD 5500 higher than non-surgical treatment. The trend in Sweden is that surgical treatment of PHF is increasing. When functional outcome of percutaneous fixation/plate fixation/prosthesis surgery and non-surgical treatment was compared for PHF there were no clinically relevant differences, SMD -0.05 (95% CI: -0.26; 0.15). There was not enough data for interpretation of quality of life or complications. Evidence was scarce regarding comparisons of different surgical options for humerus fracture treatment. The cost of plate fixation of a PHF was at least USD 3900 higher than non-surgical treatment, costs for complications excluded. In Sweden the incidence of plate fixation of PHF increased between 2005 and 2011.
Conclusions
There is moderate/low certainty of evidence that surgical treatment of moderately displaced PHF in elderly patients has not been proven to be superior to less costly non-surgical treatment options. Further research of humerus fractures is likely to have an important impact.
Introduction
Treatment of humerus fractures in the elderly remains a therapeutic challenge. These injuries are among the most common fractures [1] and cause large expenses for the individual and for society, due to their high frequency, the surgical complexity, and risk of poor outcome. There are indications that the incidence of osteoporosis related proximal humerus fractures (PHF) is increasing [2, 3], with an incidence of 10,5/10,000 in people aged 60 or older in a Scandinavian population [3].
Although non-surgical treatment is a reasonable treatment option for the majority of humerus fractures [4–6], there is an increasing interest in surgical intervention [7, 8]. New technical possibilities for fracture fixation in the elderly were evident after the introduction of angle stable implants at the turn of the 21st century [9]. The use of shoulder arthroplasties as fracture treatment has undergone a rapid development during the 21st century [10]. Only few comparing studies have been performed investigating effectiveness and complications after fracture surgery, and the need for prospective randomized trials has been advocated [11]. New surgical methods for humerus fracture care have been introduced and widespread before they have been scientifically evaluated [10]. There are no evidence-based treatment recommendations, thus permitting large local variation in treatment preferences [7, 10–12]. Moreover, societal costs are increasing for osteoporosis fracture health care [13], and there is reason to believe that more sophisticated surgical methods for treatment of humerus fractures will add more expenses in the future. However, to the best of our knowledge, health economic assessments of humerus fractures are largely lacking.
Heath Technology Assessment (HTA) is a scientific methodology used to gather and summarize scientific data to influence policy and clinical decision making on the use of health technologies. In this context, the primary aim of this HTA analysis was to assess the literature describing the effectiveness, complications and the cost-effectiveness of treatment options for humerus fractures in a population with a mean age above 60 years. Other aims were to evaluate the intervention costs for treatments of proximal humerus fractures and to investigate the Swedish national incidence rates of PHF and their treatment during the period 2005–2013.
Materials and methods
The present HTA analysis includes a systematic literature review of clinical and health economic studies comparing treatment options for fractures of any part of the humerus. The results regarding the effectiveness of the treatments are summarized in meta-analyses. In addition, the assessment contains a cost analysis for different treatment options commonly used for PHF care. Lastly, this HTA report includes an analysis of registry data providing information on the incidence and treatment traditions concerning PHF during the period 2005–2013. The present work was conducted and funded within the framework for the Swedish Agency for Health Technology Assessment and Assessment of Social Services, SBU (http://www.sbu.se/en), a Swedish public agency conducting health technology assessments. The process during which this HTA analysis was performed, has continuously been reviewed by an internal group for quality control of the Swedish Agency for Health Technology Assessment and Assessment of Social Services. After completion, its accuracy was audited by an external council of medical experts.
Systematic review and meta-analysis
Protocol and registration
The systematic literature review was based upon studies investigating benefits and possible risks of different methods for treating humeral fractures in a study population with mean age of at least 60 years. Methods of analysis and inclusion criteria for the project were specified in advance, as a part of the internal process at SBU. No protocol has been published.
Eligibility criteria
The criteria for eligibility were outlined according to the PICOS model (Population, Intervention, Comparator, Outcome and Study design) and included the following characteristics:
| Population | The mean age of the study population 60 years or above. All study participants were treated for a fracture of any part of the humerus. Studies on cadavers were excluded. |
| Interventions | Any operative or non-operative fracture treatment. |
| Comparator | Any comparator (e.g., any alternative treatment, operative or non-operative). |
| Outcome and measures | Functional outcomes, adverse effects/complications, quality of life (QoL), cost-effectiveness and costs. Any validated measure was acceptable. |
| Study design | Randomized controlled trial (RCT), non-randomized controlled (Non-R) studies and comparative registry studies. |
| Setting | Any setting. |
| Language | Studies published in English or in the Scandinavian languages. |
| Publication type | Studies published in peer-reviewed journals. |
Information sources. Studies were identified by searching electronic databases and by scanning the reference lists of studies meeting the eligibility criteria, and of relevant systematic reviews. The electronic databases PubMed, EMBASE, Cochrane Library, and Scopus were searched from January 1990 to December 2016.
Search strategy
Electronic searches were conducted using a combination of medical subject headings (MeSH) and relevant text word terms related to fractures of the upper extremity, old age, interventions and study type. (For detailed information about the search strategies, see S1 Appendix.)
Study selection
Six reviewers, all expert senior scientists, independently screened the titles and abstracts for eligibility. Each abstract was screened by two reviewers. The abstracts were screened and rated using the online available scanning tool Rayyan [14]. All publications of potential relevance according to the inclusion criteria were retrieved in full text. Eligibility for inclusion was independently assessed by two reviewers. Disagreements were resolved by consensus. Reference lists of studies meeting the eligibility criteria and of relevant systematic reviews were screened for additional relevant studies. (For detailed information about the included studies, see S2 Appendix, excluded studies, see S3 Appendix.)
Risk of bias in individual studies
To determine the internal validity of the eligible trials, a pair of reviewers independently assessed the risk of bias according to the SBU checklist [15]. The SBU checklist for the inclusion of studies, which has been described in detail previously [16] “is based on the CONSORT statement and discloses risk of bias related to six main aspects: selection; treatment (including blinding); measurement; attrition; reporting; and conflicts of interest [17]. The checklist was used to reveal shortcomings of the studies. The reviewers thereafter assessed the extent to which the internal validity of the results could have been affected by these shortcomings. A rating of low, moderate or high risk of bias was given to each category of items. Based on the severity of the combined threats to internal validity, an overall rating of risk of bias was then given to each study.” For the health economic studies, a specific check-list for within trial cost-effectiveness studies was used [18]. Only studies with a low or moderate overall risk of bias were included in the synthesis.
Data items
The following information was extracted from the included trials: (1) Type of injury, study design, time to follow-up, period when the study was performed (yrs.); (2) Number of participants, mean age and sex; (3) treatment, drop-out rate, side-effects; (4) type of comparator, drop-out rate, side-effects (5) outcome and measures; (6) risk of bias.
Data collection process
Data was extracted from each included study and inserted into a table by one reviewer. A second reviewer audited the data extraction. Any disagreements were resolved by discussion. Functional outcome was reported by validated assessment instruments, e.g. Disabilities of the Arm, Shoulder, and Hand (DASH) [19] and Constant and Murley Score (Constant score) [20]. Quality of life was presented if reported by validated quality of life instruments, such as EuroQoL 5 Dimensions (EQ-5D) [21, 22] and 15-Dimensional (15-D) [23]. Minimal clinically important differences (MCID) scores for different outcomes (Table 1) were used to reflect the clinical importance of the measured differences between the treatments. Complications were defined as major if they demanded surgical treatment or produced permanent serious disability. All other complications were defined as minor. Each complication was presumed to occur in one individual, even if some patients inevitably may have been affected by two or more complications, thus overestimating the number of patients with complications. Any statistically significant difference in complications was considered clinically important.
Table 1. Outcome measurements used in this HTA analysis regarding fractures of the proximal humerus, with corresponding minimal clinically important differences (MCID).
Statistical methods
The software Comprehensive Meta-Analysis (CMA), Version 3.3, software (Biostat NJ, USA) was used for the meta-analyses. Random effect models were applied, due to the substantial heterogeneity that was expected regarding populations, interventions, comparators and outcome measures across studies. The principal summary measures were mean difference (MD) with 95% CI for the final follow-up assessment. The summary measure standardized mean difference (SMD, Cohen’s d), based on the groups’ sample sizes, means and standard deviations were used when summaries of measures were not possible to be presented as MD. In case of only one RCT forming the results, Non-R studies and registry studies were also used to illustrate the differences between treatment options. For analysis of complications, meta-analysis was performed through calculation of Risk Difference (RD), presented as percentages. All results are presented for one year follow up, or longer follow-up times when data was available. Inconsistencies and heterogeneity disclosed by the meta-analyses were considered when the certainty of evidence across studies was assessed.
Assessing certainty of evidence across studies using GRADE
The international system GRADE [32] was used to assess the certainty of evidence for efficacy, effectiveness and complications across studies according to the following four levels, as described in detail previously [33]:
High–We are very confident that the true effect lies close to that of the estimate of the effect. This level is illustrated in Tables 2, 3, and 4 (⊕⊕⊕⊕).
Table 2. Certainty of evidence for surgical vs. non-surgical treatment options of proximal humerus fractures in the elderly.
N/A = Not Applicable.
| Intervention | Outcome measure | Comparator (C) | NRCT+Cohort/Trials [Reference(s)] | Results | Certainty of evidence (GRADE) | Comment |
|---|---|---|---|---|---|---|
| Surgical vs. non-surgical methods—proximal humerus fractures | ||||||
| Hemiarthroplasty (HA) | Function | Sling | 101/ 2 RCTs/[52, 56] | No clinically important difference | (⊕⊕❍❍) | -2 indirectness |
| SMD -0.17 (-0.56; 0.23) | ||||||
| Hemiarthroplasty (HA) | Quality of life | Sling | 54/1 RCTs/[52] | N/A | (⊕❍❍❍) | Single study |
| Hemiarthroplasty (HA) | Complications- minor | Sling | No study | N/A- minor | (⊕❍❍❍) | |
| Hemiarthroplasty (HA) | Complications- major | Sling | 101/ 2 RCTs/[52, 56] | N/A- major | (⊕❍❍❍) | -1 risk of bias |
| -2 indirectness | ||||||
| Different types of internal fixation | Function | Sling | 373+231/4 RCTs and 3 cohorts/[50, 51, 55, 57–60] | No clinically important difference) | (⊕⊕⊕❍) | -1 indirectness |
| SMD -0.05 (-0.26; 0.15 | ||||||
| Different types of internal fixation | Quality of life | Sling | 277/3 RCTs/[50, 51, 55] | No clinically important difference | (⊕⊕❍❍) | -1 risk of bias |
| MD -0.01 (-0.06; 0.05) | -1 indirectness | |||||
| Different types of internal fixation | Complications-minor | Sling | 44+129/2 RCTs and 1 cohort/[55, 57, 58] | N/A | (⊕⊕❍❍) | -1 risk of bias |
| -2 indirectness | ||||||
| Different types of internal fixation | Complications -major | Sling | 373+129/ 4 RCTs and 1 cohort/[50, 51, 55, 57, 58] | No clinically important difference regarding major complications | (⊕⊕❍❍) | -1 risk of bias |
| RD 0.07 (-0.06; 0,20) | -1 inconsistency | |||||
Table 3. Certainty of evidence for surgical treatment options of proximal humerus fractures in the elderly.
N/A = Not Applicable.
| Intervention | Outcome (measure) | Comparator (C) | NRCT+Cohort/Trials [Reference(s)] | Results | Certainty of evidence (GRADE) | Comment |
|---|---|---|---|---|---|---|
| Surgical vs. surgical methods—proximal humerus fractures | ||||||
| Plates with monoaxial locking screws | Function | Plates with polyaxial locking screws | 56+76/1 RCT and 1 cohorts/ [65, 66] | - | (⊕❍❍❍) | N/A |
| Plates with monoaxial locking screws | Quality of life | Plates with polyaxial locking screws | - | - | (⊕❍❍❍) | No study |
| Plates with monoaxial locking screws | Complications | Plates with polyaxial locking screws | 56+76/1 RCT and 1 cohorts/ [65, 66] | - | (⊕❍❍❍) | N/A |
| Plates with enhanced support | Function | Plates without enhanced support | 122/ 2 RCTs/ [53, 67] | - | (⊕❍❍❍) | N/A |
| Plates with enhanced support | Quality of life | Plates without enhanced support | - | - | (⊕❍❍❍) | No study |
| Plates with enhanced support | Complications | Plates without enhanced support | 122/ 2 RCTs + 1 cohort/ [53, 67, 68] | - | (⊕❍❍❍) | N/A |
| Different kinds of internal fixation | Function | Prosthesis | 60+104 /1 RCT and 2 cohorts/[54, 69, 70] | - | (⊕❍❍❍) | |
| Different kinds of internal fixation | Quality of life | Prosthesis | 44/ 1 cohort/[69] | - | (⊕❍❍❍) | |
| Different kinds of internal fixation | Complications | Prosthesis | 60+104 /1 RCT and 2 cohorts/[54, 69, 70] | - | (⊕❍❍❍) | |
| Plate fixation | Function | Intramedullary nail | 65+193/1 RCT and 2 cohorts/[71–73] | No clinically important difference MDRCT, -3.8 (95% CI: -11.85 to 4.25) MDcohorts: 4.51 (95% CI: -0.99 to 10.1) | (⊕⊕❍❍) | Single study |
| Plate fixation | Quality of life | Intramedullary nail | 41/1 cohort/[73] | - | (⊕❍❍❍) | Single study |
| Plate fixation | Complications | Intramedullary nail | 65+328/1 RCT and 3 cohorts/[71–74] | - | (⊕❍❍❍) | -1 indirectness |
| -2 inconsistency | ||||||
| Reverse shoulder arthroplasty (RSA) | Function | Hemiarthroplasty (HA) | 61+448/1 RCT and 3 cohort/[61–64] | Statistically significant difference RSA>HA | (⊕⊕❍❍) | -1 risk of bias |
| MDRCT 6.9 (95% CI: 3.0 to 10.8) | -1 indirectness | |||||
| Reverse shoulder arthroplasty (RSA) | Quality of life | Hemiarthroplasty (HA) | - | - | (⊕❍❍❍) | No study |
| Reverse shoulder arthroplasty (RSA) | ComplicationsMinor and major | Hemiarthroplasty (HA) | Minor: 62+80/1 RCT and 2 cohorts /[61–63] Major: 368/ 1 cohort/[64] | - | (⊕❍❍❍) | -2 indirectness-1 inconsistency |
| Different kinds of fixation of the tubercles during arthroplasty | Function | Different kinds of fixation of the tubercles during arthroplasty | 35+54/1 RCT and 1 cohort/[75, 76] | - | (⊕❍❍❍) | -1 risk of bias |
| -1 indirectness -1 inconsistency | ||||||
| Different kinds of fixation of the tubercles during arthroplasty | Quality of life | Different kinds of fixation of the tubercles during arthroplasty | - | - | (⊕❍❍❍) | No study |
| Different kinds of fixation of the tubercles during arthroplasty | Complications | Different kinds of fixation of the tubercles during arthroplasty | 35/1 RCT/[75] | - | (⊕❍❍❍) | Single study |
| Straight intramedullary nail | Function | Curved intramedullary nail | 52/1 RCT/[77] | - | (⊕❍❍❍) | Single study |
| Straight intramedullary nail | Quality of life | Curved intramedullary nail | - | - | (⊕❍❍❍) | No study |
| Straight intramedullary nail | Complications | Curved intramedullary nail | 52/1 RCT/[77] | - | (⊕❍❍❍) | Single study |
Table 4. Certainty of evidence for comparisons of non-surgical treatment options of proximal humerus fractures in the elderly.
| Intervention | Outcome measure | Comparator (C) | NRCT+Cohort/Trials [Reference(s)] | Results | Certainty of evidence (GRADE) | Comment |
|---|---|---|---|---|---|---|
| Surgical vs. surgical methods- proximal humerus fractures | ||||||
| Early mobilization after hemiarthroplasty (HA) | Function | Late mobilization after hemiarthroplasty (HA) | 49/1 RCT/ [78] | - | (⊕❍❍❍) | One study |
| Early mobilization after hemiarthroplasty (HA) | Quality of life | Late mobilization after hemiarthroplasty (HA) | - | (⊕❍❍❍) | No study | |
| Early mobilization after hemiarthroplasty (HA) | Complications | Late mobilization after hemiarthroplasty (HA) | 49/1 RCT/ [78] | - | (⊕❍❍❍) | One study |
Moderate–We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. This level is illustrated in Tables 2, 3 and 4 (⊕⊕⊕❍).
Low–Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. This level is illustrated in Tables 2, 3 and 4 (⊕⊕❍❍).
Very low–We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of the effect. This level is illustrated in Tables 2, 3 and 4 (⊕❍❍❍).
The GRADE system postulates that scientific evidence based on data from RCTs is assessed as high certainty. The level of confidence for either study type may then be downgraded due to several circumstances noted in each particular study, such as risk of bias, inconsistency, indirectness, imprecision and publication bias. There was no upgrading in confidence based on large magnitude of effect or dose response. The rating of certainty of evidence in our literature review was decided through consensus among the authors supported by GRADE guidelines.
Cost analysis
Direct costs of the primary treatment opportunity in primary or inpatient care for the different treatments for PHF care in a Swedish setting were estimated using a bottom up approach [34]. In this approach, the resources necessary to provide each treatment are first identified and then valued using unit costs for each unit of resources. Four different operative treatments as well as a non-operative alternative were included in the analysis: Plate fixation, Intramedullary (IM) nail fixation, Hemiarthroplasty (HA), Reverse shoulder arthroplasty (RSA)) and non-operative treatment with a sling.
The cost analysis included the cost for staff, operating theatre rental costs (including overhead costs), costs for medical technical equipment, costs for orthopedic implants, and costs for consumables. For a detailed description, see S5 Appendix. Calculations were performed only for costs related to the primary treatment opportunity in inpatient care, i.e. no calculations were performed regarding for example out-patient clinic follow-ups, or societal costs. Short- or long-term complications were not included in the analysis due to lack of published data. All resources needed for each treatment method were identified by expert senior scientists in the research group. Time in operating theatre for each type of surgical intervention was estimated from previous publications [35–38]. Time consumption for non-surgical interventions, pre- and post-operative care, hospital inpatient duration and utilization of staff involved in different stages of the different treatments, were estimated by expert senior scientists in the research group based on clinical experience and reported data from three large Swedish general hospitals’ computerized operation planning systems. The time for pre-and post-operative care in the perioperative intensive care ward was estimated to be equally long for all surgical treatments, see detailed description in S5 Appendix.
The material costs (consumables and implants) were estimated by collecting data from the economic departments of three general hospitals in Sweden (The Sahlgrenska University hospital, Gothenburg, Skåne University hospital, Malmö, and the hospital Södersjukhuset, Stockholm). The cost for material was valued using a conservative approach by always using the product with the lowest procured price. The units and unit costs derived from these sources are presented in S5 Appendix. All costs were converted to US dollars in 2016 using the method recommended by The Cochrane and Campbell Economic Methods Group, i.e. with PPPs (purchasing power parity) via The CCEMG–EPPI-Centre Cost Converter (v.1.5 last update: 29 April 2016) http://eppi.ioe.ac.uk/costconversion/ (IMF-PPP).
Registry analysis
All Swedish health-care providers supply mandatory registration of all out- and in-patient care given in Sweden. Registered data is collected in the Swedish National Patient Registry kept by the National Board of Health and Welfare (https://www.socialstyrelsen.se/english). For the purpose of the present study, in- and outpatient clinic data was ordered for the period 2005–2013 with a selection of all individuals above the age of 50 with a reported International Classification of Disease edition 10 (ICD-10) code [39] for a PHF. Individuals were counted only once to avoid overestimation of incidences. If a Nordic code for surgical procedures (NOMESCO) code [40] for surgical intervention of PHF occurred in the registry within 30 days of the date of a PHF code, the fracture was considered to have been treated surgically. All other fractures were considered to have been treated non-operatively. Incidences were calculated as the number of events divided by the size of the target population according to Statistics Sweden (http://www.scb.se/en/). The data was connected to the Swedish Causes of Death Registry (http://www.socialstyrelsen.se/register/dodsorsaksregistret) to calculate the risk of death after proximal humerus injury. All handling of data and calculations of registry data were performed in SPSS (version 23; IBM, NY, USA).
Ethics
No ethical permit was collected for this literature review. All patient data was collected from published data. All registry data used in this study was unidentified and approved by the National Board of Health and Welfare in Sweden.
Results
Systematic review and meta-analysis
Eligible studies
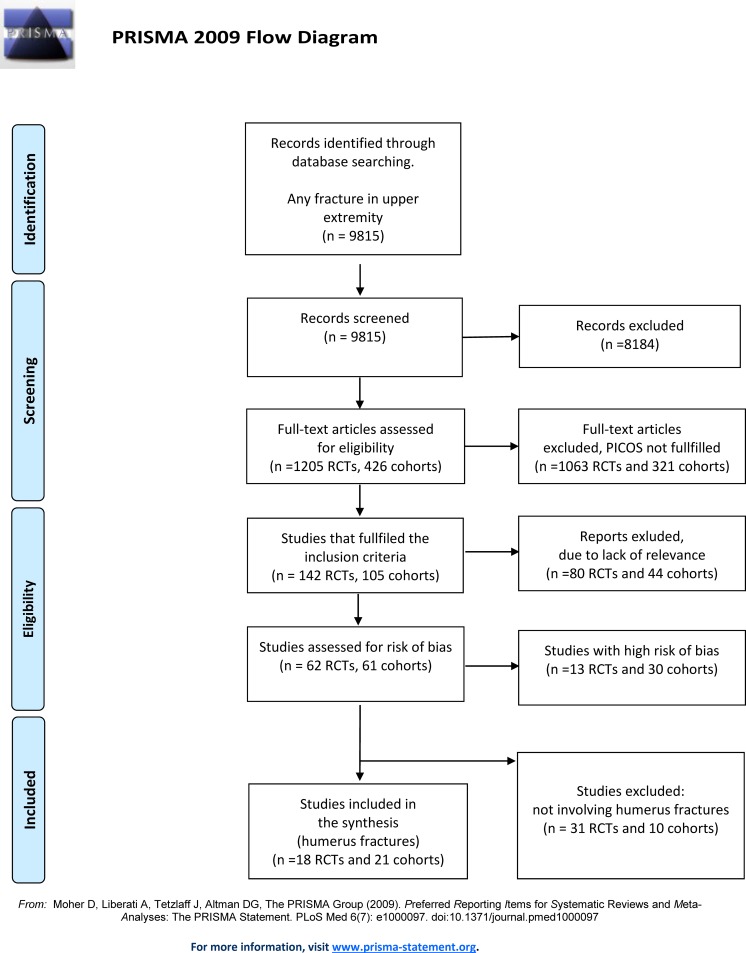
The literature search of studies investigating the effectiveness of treatments for the upper extremity yielded a total of 9815 citations: after review of the abstracts, 8184 were discarded. The full text of a total of 1205 RCTs and 426 cohort studies citations was examined. 1063 RCTs and 321 cohort studies were excluded since the studies did not meet the inclusion criteria, thus leaving 142 RCTs and 105 cohorts to be evaluated for relevance. Out of these, 80 RCTs and 44 cohort studies were deemed as not relevant, leaving 62 relevant RCTs and 61 relevant cohort studies. After the assessment of risk of bias, 13 RCTs and 30 cohorts were considered to be of high risk of bias, leaving 49 RCTs and 31 cohort studies with low/moderate risk of bias (see S2 Appendix for included studies and S3 Appendix for excluded studies). Studies investigating the forearm (radius and ulna) were finally discarded, leaving 18 RCTs and 21 Non-R studies regarding humerus fractures for analysis (Fig 1).
Fig 1. PRISMA flow-chart.
The search for health economic studies regarding fracture treatment in the upper extremity yielded a total of 569 potentially relevant citations. Out of these, 118 were read in full text and nine of these were judged to be relevant studies of treatments for humerus fractures. Six of these studies focused only on resource use or costs [41–46] and only three remaining studies were full cost-utility analyses (CUA) [47–49] (see S2 Appendix for included studies and S3 Appendix for excluded studies).
Risk of bias in individual studies
All included studies were deemed to have moderate or low risk of bias based on the methodological assessment performed by authors CE, CMN, LZ, PN, POJ and LEO (the latter mentioned in the Acknowledgement section). Included studies and their risk of bias are presented in S6 Appendix. All studies presented data with a mean age of study participants that cohered to the inclusion criteria of this meta-analysis. However, some studies included only elderly patients whereas other studies included all ages but with a mean age of participants that met the inclusion criteria for this meta-analysis, S6 Appendix. Differences in age distribution among studies may have introduced bias. Fracture severity was not always described in full detail and represents a risk of bias. Most studies regarding proximal humerus fractures presented included fractures by the Neer classification as listed in S6 Appendix. Exclusion criteria however, differed between studies and may introduce a risk of bias. Olerud and Handoll for example [50–52], excluded patients due to indication for mandatory surgical treatment. This definition however, was not explained in full detail. Only Chen and Liu [53, 54] defined the level of mineral bone density as an inclusion criterion, a detail which maybe would have been appropriate for all patient populations to avoid bias. Most results were collected from the 1-year follow-up, but some results were collected from a later follow-up point (S6 Appendix) which may represent a risk of bias. In studies comparing surgery and non-operative treatment, blinding was not possible to achieve. No study described a double-blind allocation and assessment.
Comparison of non-surgical and surgical treatment–Proximal humerus fractures
Study characteristics
Nine trials, six RCTs (474 participants) and three Non-R studies (231 participants) were included that compared non-surgical and surgical treatment of PHF in the elderly. The subjects were predominantly female. All nine studies were conducted in Europe. The treatment methods under study were HA or plate fixation compared with non-surgical treatment (sling: body bandage). No study included fractures demanding imperative surgical treatment.
Hemiarthroplasty (HA) vs. non-surgical treatment
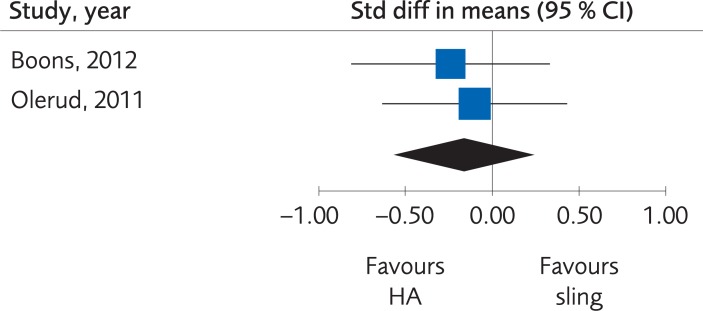
Results. Two RCTs compared HA with sling immobilization regarding the functional outcome results as measured by Disabilities of the Arm, Shoulder and Hand (DASH) Score and Constant score. There was no clinically important difference, at one-year follow-up, SMD -0.17; 95% CI: -0.56 to 0.23 (Fig 2). Due to the low number of trials, the certainty of evidence was rated as low.
Fig 2. Meta-analysis of randomized controlled trials comparing hemiarthroplasty (HA) with sling immobilization: results of functional outcome, in elderly patients with proximal humerus fractures at one-year follow-up.
Operative vs. non-operative treatment
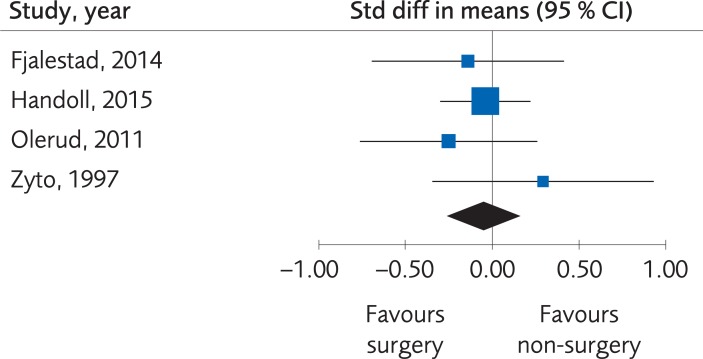
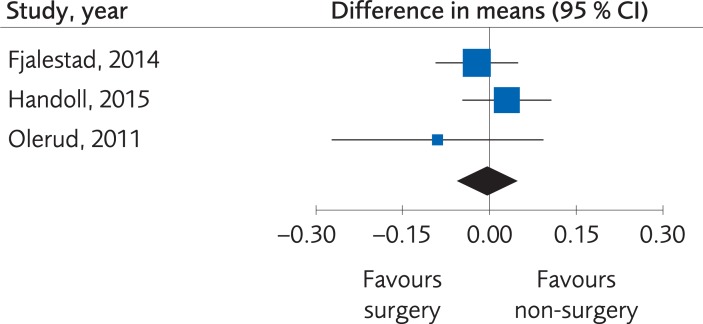
Results. Four RCTs (373 subjects) and three Non-R studies (231 subjects) compared functional outcomes (DASH Score, Constant score or Oxford shoulder score (OSS)) between different methods for surgical intervention (percutaneous fixation, plate fixation, nail or arthroplasty) and sling immobilization. There were no clinically important differences regarding the functional outcome, SMD -0.05; 95% CI: -0.26 to 0.15, Fig 3, at one-year follow-up, and the evidence was rated as being of moderate quality due to the limited number of participants. Quality of life was measured in three of these studies, using the EQ-5D in two [50, 51] and 15-D in the one by Fjalestad et al., 2014 [55]. There were no clinically important differences regarding quality of life, MD -0.01; 95% CI: -0.06 to 0.05, Fig 4, but because of the limited number of participants the certainty of evidence was rated as low quality. Table 2.
Fig 3. Meta-analysis of randomized controlled trials comparing different methods for internal fixation with treatment with a sling: results of functional outcome, in elderly patients with proximal humerus fractures at one-year follow-up.
Fig 4. Meta-analysis of randomized controlled trials comparing different methods for internal fixation with treatment with a sling: results of quality of life, in elderly patients with proximal humerus fractures at one-year follow-up.
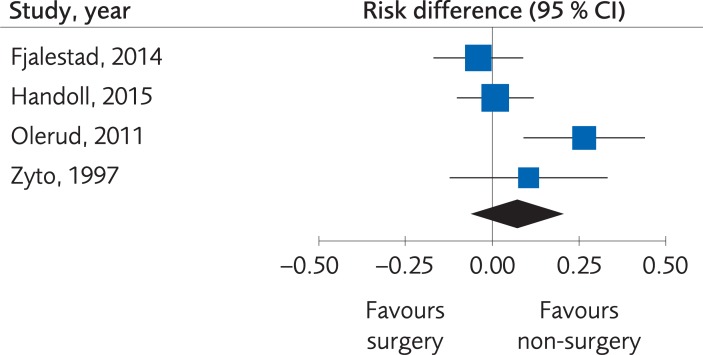
Minor complications were reported by two RCTs and one Non-R study, but the number of events was too small to determine differences (15 events for operative treatment and 4 events for the non-operative treatment). Major complications were reported in in four RCTs and one Non-R study, but the certainty of evidence was rated as low quality, since there was a risk of bias and inconsistency. No clinically important differences were found, RD 0.07; 95% CI: -0.06 to 0.20, Fig 5.
Fig 5. Meta-analysis of randomized controlled trials comparing different methods for internal fixation with treatment with a sling: results of major complications, in elderly patients with proximal humerus fractures at one-year follow-up.
Comparison of different options for surgical treatment–Proximal humerus fractures
Study characteristics
Twenty-five trials, nine RCTs (572 participants) and sixteen Non-R studies (1 663 participants) were included that compared different surgical treatment options in elderly patients with PHF. The subjects were predominantly female. Out of these studies, fifteen were conducted in Europe, seven in Asia, one in USA, one in South America and one in Oceania. The treatment methods analyzed were surgical treatments with different kinds of internal fixation with plates, different kinds of plates with or without medial support, different kinds of internal fixation compared to prosthesis, plate fixation compared to intramedullary nail, RSA compared to HA, different kinds of fixation of the tubercles during arthroplasty and different kinds of intramedullary nails.
Comparison of plates, nails and prostheses
Results. When different kinds of plate fixation with or without angle-stable screws, plate fixation with or without screws supporting the fracture medially, internal fixation and arthroplasty were compared, there were not enough data to present results regarding differences in clinical result, quality of life or complications. The certainty of evidence was rated as very low (Table 3).
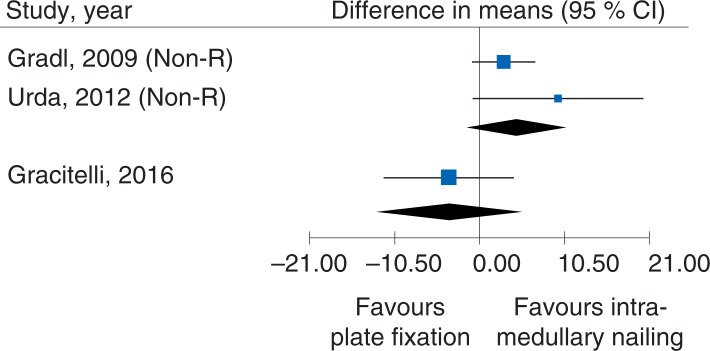
One RCT (65 participants) (using DASH as outcome) and two Non-R studies (193 participants) (using Constant score as outcome) compared plate fixation with intramedullary nailing. No clinically important differences were seen, MDRCT, -3.8 (95% CI: -11.85 to 4.25) and MDcohorts: 4.51 (95% CI: -0.99 to 10.1), Fig 6. The certainty of evidence was rated as low, due to the low number of trials and participants, and indirectness (lack of generalizability between the study designs). Analysis of quality of life and complications also failed due to too few observations.
Fig 6. Meta-analysis of a randomized controlled trial and two Non-R studies comparing different methods for plate fixation with intramedullary nailing: results of functional outcomes, in elderly patients with proximal humerus fractures at one-year follow-up.
The study of Konrad et al., 2012 could not be illustrated in the meta-analysis, since only boxplot was presented.
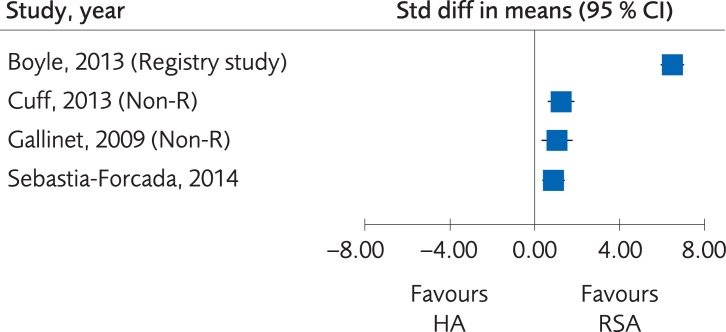
Comparison of hemiarthroplasty vs. Reverse shoulder arthroplasty
Results. One RCT, two Non-R studies and one registry study compared RSA with HA regarding functional outcome (OSS, DASH or American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES)). The combined results [61–63, 64] showed a statistically significant difference in favor of RSA, MDRCT 6.9 (95% CI: 3.0 to 10.8), Fig 7, but this difference is not clinically significant. The certainty of evidence, however, was rated as very low due to the Non-R studies included and limitations in study design (Table 3).
Fig 7. Meta-analysis of a randomized controlled trial and two Non-R studies and one registry study comparing hemiarthroplasty (HA) with reverse shoulder arthroplasty (RSA): Results of functional outcome, in elderly patients with proximal humerus fractures at one to five-year follow-up.
Comparison of different non-surgical treatments–Proximal humerus fractures
Study characteristics
One RCT (49 participants) was included that compared different non-surgical regimens. The subjects were predominantly female, and the study was conducted in Europe. The treatment methods analyzed were early and late immobilization after HA.
Results. The study did not provide enough data for determination of differences regarding functional outcome and complications. Quality of life was not evaluated, and certainty of evidence was rated as very low (Table 4).
Comparison of different options for surgical treatment–Diaphyseal humerus fractures
Study characteristics
Only one Non-R study (511 participants) was identified that compared different surgical treatments options in elderly with midshaft humerus fractures. The subjects were predominantly female, and the study was conducted in the USA.
Results. The study compared plate fixation and nailing regarding complications for elderly with humeral shaft fractures [79]. Due to only one study with a low number of participants, the certainty of evidence was rated as very low quality. No studies corresponding to our inclusion criteria evaluated plate fixation versus nailing for elderly with humeral shaft fractures regarding clinical function or quality of life. The certainty of evidence was rated as very low.
Comparison of different options for surgical treatment–Distal humerus fractures (supracondylar fractures)
Study characteristics
One controlled randomized study (40 participants) and one Non-R study (32 participants) compared different surgical treatments options in elderly with distal humerus fractures. The subjects were predominantly female, and the studies were conducted in Europe and Canada.
Results. One RCT compared plate fixation with total elbow arthroplasty regarding clinical function and complications, for displaced intra-articular distal humeral fractures in elderly patients [80]. The certainty of evidence was rated as very low. No studies corresponding to the project's criteria evaluated ORIF versus total elbow arthroplasty for elderly with distal humerus fractures regarding quality of life. The certainty of evidence was rated as very low.
One Non-R study compared early versus delayed total elbow replacement for distal humeral fractures in the elderly, regarding clinical function and complications [81]. The certainty of evidence was rated as very low quality. No studies corresponding to our project's inclusion criteria evaluated early versus delayed treatment of total elbow arthroplasty for elderly with distal humerus fractures regarding quality of life. The certainty of evidence was rated as very low.
Health economic studies
Three economic evaluations were identified that evaluated treatments of PHF [47–49]. All three studies were assessed to have moderate quality, but the study by Nwachukwu and colleagues [48] showed low transferability to Swedish conditions. No studies investigated diaphyseal or distal fractures of the humerus.
Two of the cost-utility analyses compared surgical to non-surgical treatment for humerus fractures. The PROHFER study, by Corbacho et al., 2016 [47] showed that surgical treatment was more expensive and yielded worse outcome as measured by the EQ-5D (although not statistically significant result) when compared to non-surgical treatment. At a willingness to pay per QALY of GBP 30,000, their estimations showed a probability of only 23% that surgical treatment would be a cost-effective alternative compared to the non-surgical treatment. In contrast, Fjalestad et al., 2010 [49] reported initially higher costs for surgical treatment compared to non-surgical treatment but these differences evened out when a longer-term analysis was performed due to a larger number of out-patient visits for the non-operatively treated group after hospital dismissal. In addition, Fjalestad et al., 2010 [49] showed a small but not statistically significant difference in QALYs in favor of surgery (0.009 QALYs, 95% CI -0.025 to 0.042). Thus, the authors concluded that surgery was both less costly and more effective from a health care perspective. Nevertheless, the costs for surgery increased when including production losses in the analysis. In this scenario, the cost per QALY increased to approximately EURO 231,000 which corresponds to USD 340,000.
Cost analysis
Intervention costs for treatment of PHF are shown in Table 5. The intervention costs ranged from USD 40 for treatment with immobilization in a sling, to USD 7 728 for surgical treatment with RSA, which was the most expensive treatment method. The treatment cost for IM nail fixation was slightly lower than for plate fixation due to a shorter operation time. The higher costs associated with HA and RSA are explained by higher implant costs, longer operation time and longer inpatient care. Surgery with HA and RSA was estimated to 120 minutes [52, 64], while the operation time for plate fixation and IM nail fixation was estimated to 100 and 60 minutes respectively [43, 51, 66, 73, 74, 82–85]. The time in inpatient care was estimated to be two days for plate fixation and IM nail fixation, and three days for HA and RSA.
Table 5. Intervention costs per treatment of proximal humerus fractures in a Swedish setting.
Estimation performed within the context of a HTA analysis performed by the Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU).
| Intervention cost (USD 2016) | |||||
|---|---|---|---|---|---|
| Resources | Sling | Plate fixation | Intramedullary (IM) nail fixation | Hemiarthroplasty (HA) | Reverse shoulder arthroplasty (RSA) |
| Material (consumables and implants) | 2 | 489 | 489 | 1363 | 3518 |
| Time in the operating theatre including fixed equipment + overhead costs |
890 | 762 | 953 | 953 | |
| Orthopaedic surgeon | 24 | 286 | 191 | 333 | 333 |
| Assisting orthopaedic surgeon | 238 | 143 | 286 | 286 | |
| Anaesthesist | 155 | 155 | 155 | 155 | |
| Anaesthetic nurse | 318 | 272 | 340 | 340 | |
| Surgical nurse | 318 | 272 | 340 | 340 | |
| Operation assistant | 222 | 191 | 238 | 238 | |
| Out-patient clinic nurse | 14 | 0 | 0 | 0 | 0 |
| Inpatient care due to operation | 0 | 1043 | 1043 | 1565 | 1565 |
| Total | 40 | 3959 | 3518 | 5573 | 7728 |
Registry analysis
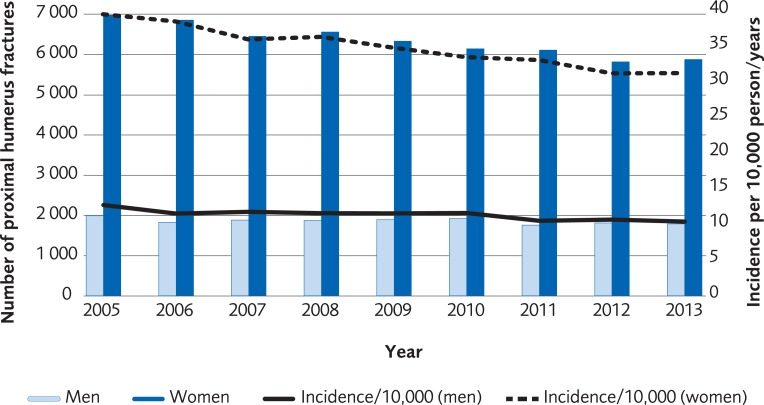
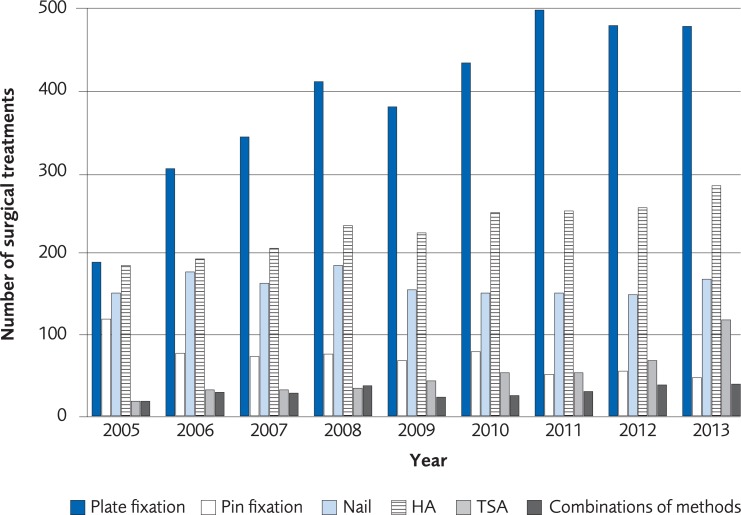
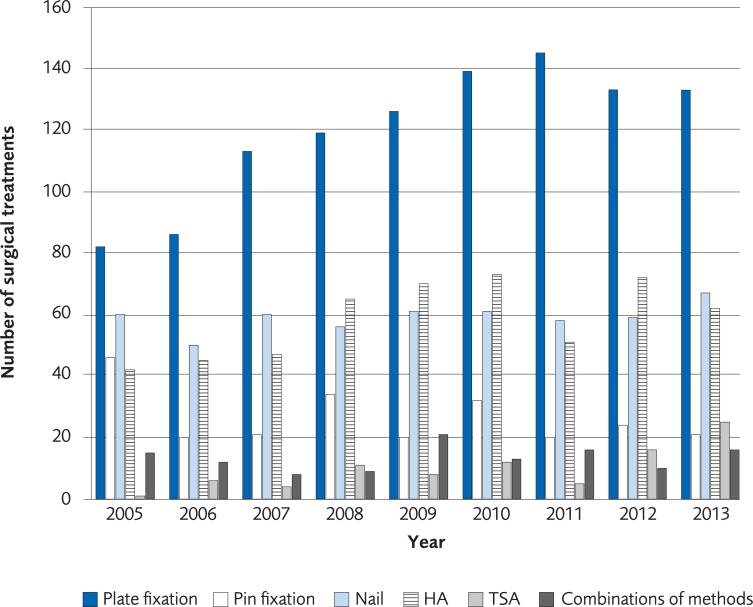
The analysis was performed on registry data from 57,075 women and 16,774 men over the age of 50 recorded in the Swedish National Patient Registry with a PHF during the period 2005 to 2013. The incidence of a PHF in patients over 50 years old was 33/10,000-person years among women in 2005 and 31/10,000-person years in 2013. The incidence of a PHF in men in the same age group was 12/10,000-person years in 2005 and 10/10,000 in 2013 (Fig 8). The proportion of patients undergoing surgical treatment increased by 5.5% for women and 2.5% for men during 2005–2013. The most common method for surgical treatment in 2005 was plate fixation and its use increased until 2011 (Fig 9, for women, Fig 10 for men). The number of total shoulder arthroplasty (TSA) increased between 2011 and 2013 from 58 to 143, which represents an increase of 147%. Risk of death within 30 days from the PHF was 2.1%.
Fig 8. Incidence per 10,000 person-years of proximal humerus fractures in the Swedish population ≥50 years old, between 2005 and 2013 according to registry data from the Swedish Board of National Health and Welfare.
Fig 9. The most common surgical treatments of proximal humerus fracture in women, ≥50 years old, between 2005 to 2013 in Sweden according to registry data from the Swedish Board of National Health and Welfare.
Fig 10. The most common surgical treatments of proximal humerus fracture in men, ≥50 years old, between 2005 to 2013 in Sweden according to registry data from the Swedish Board of National Health and Welfare.
Discussion
The present HTA analysis presents the current literature on treatment of humeral fractures including RCTs and cohort studies performed on patient over 60 years of age. The main finding is that there was no proven benefit with surgical intervention of moderately displaced PHF compared to non-operative treatment with immobilization in a sling. Moreover, the health economic evaluation showed that surgical treatment of a proximal humeral fracture was considerably more expensive (USD 3478 to USD 7688) than non-operative treatment. Many areas under investigation in this HTA analysis lacks sufficient scientific data to express any certitude regarding efficacy, effectiveness, complications and cost-effectiveness.
Our findings regarding functional outcome after PHF are supported by a review published by Launonen et al., 2015 [4]. They found no benefit of surgical treatment in patients over 60 years of age, with 3- or 4-parts PHF as compared to non-surgical treatment. Launonen and colleagues found more complications in the group of surgically treated patients than in the non-operative group. Equal findings regarding functional outcome and complications were reported in a systematic review by Beks et al., 2018 [86]. According to definitions used in our literature review, we consider the available evidence too scarce to draw any qualified conclusions regarding comparisons of complications after operative or non-operative treatment of PHF. In contrast to Launonen and Beks, we also included studies regarding diaphyseal and distal humerus fractures in our literature search. Other authors support our opinion that there is a lack of scientific data regarding treatment of diaphyseal and distal humeral fractures, especially in elderly patients [87–89].
In accordance with our finding, Sabharwal et al., 2016 [90] and Beks et al., 2018 [86] concluded in their reviews that there was no overall benefit of surgical treatment of proximal humeral fractures. These reviews used Constant score as the most important outcome measure, as opposed to our study where we used DASH as the preferred primary outcome. A sub group analysis of different fracture patterns was performed in the study by Sabharwal., 2016 [90], indicating higher quality of life for patients with 4-part fractures, i.e. more complex fractures, when treated operatively. Interestingly, fractures of high complexity have been excluded from clinical trials, e.g. Olerud et al., 2011 [51, 52] and Handoll et al., 2015 [50], with the explanation that the indication for surgery was absolute. Moreover, the definitions of inclusion criteria regarding fracture types and degrees of displacement vary widely between studies. In some studies, radiographic inclusion criteria were not clearly described. One should refrain from generalizing findings from studies investigating moderately displaced fractures to populations suffering from complex fracture patterns. We support Sabharwal et al., 2016 [90] in their opinion that future studies must be very strict and clear when defining and describing inclusion criteria regarding fracture classification and degree of displacement.
In the present systematic review, the majority of data was collected from follow-up at one year. There is a paucity of adequate publications of short- mid and long-term follow-ups and more studies must be performed to discern potential differences on different time horizons. According to Handoll et al., 2017 [91], who reported no differences in reoperation rates between the 2-year and 5-year follow-up of their multicenter study comparing surgery and non-surgical treatment, there is reason to believe that no more than 2 years is necessary for final follow-up. In their study they presented slight improvement as measured by the OSS, equally large in both groups, between the 2- and 5 years follow-up, although the improvement was statistically but not clinically significant [91].
There is a lack of studies regarding the cost-effectiveness of treatment of humeral fractures. The few studies that have been published [47–49] have had short time perspectives and showed conflicting results. This highlights the need for more well-designed cost-effectiveness studies. The costs to be included in such an analysis may differ from country to country and between patient populations. In the age group studied in this report, prolonged hospital stays, temporary stays in home for the elderly, and home care should be included in a cost-effectiveness analysis, whereas in a younger population sick-leave and rehabilitation costs may be of larger importance. Long term analysis is important in future studies, since an initially more expensive treatment method may be less expensive in the long run if out-patient care visits and complications can be avoided [49]. It appears conflicting, that the incidence of expensive fracture surgery for PHF is increasing despite the lack of scientific evidence of its effectiveness. Surgical treatment that is not cost-effective should not be performed. A retrospective analysis of current surgical practice in a British setting, confirmed our findings that surgical treatment was more expensive than non-operative treatment [92]. They stated that extensive resources could be saved if non-operative treatment was chosen instead. However, future studies on both clinical effectiveness and cost effectiveness are needed to clarify the relationship between costs and effects of treatment methods used for humerus fractures.
The proportion of operative treatments for PHF in the elderly has showed an increasing trend in Sweden over the last years, as demonstrated by our data retrieved from the Swedish National Patient Registry. Similar trends have been observed in the USA. Bell et al., 2011 [7] presented data from 1999 to 2005 with rising surgery rates of PHF [7]. Rosas et al., 2016 [93] also reported similar findings and their study supports our findings of a rising incidence of total shoulder arthroplasty following PHF. Another confirmation of our findings of patterns of surgery trends can be found in the publication from Khatib et al., 2014 [94] who presented data on the same age group as we did.
A registry-based study from Sumrein et al., 2017 [8] reported a steeply rising incidence of PHF in Sweden between 2001–2012. This is contrary to our findings of a slightly decreasing incidence of PHF 2005–2013. Sumrein et al., 2017 used registry data from the Swedish National Patient registry, as in our systematic review, and included all patients over 18 years of age. Data was used from the out- and inpatient registry, and data was presented for separate age groups individually. The difference in results compared to our study may be explained that the out-patient registry started in 2001 and data from the first few years of registrations may not have been complete. Missing data during 2001–2005 may have been misinterpreted as increasing incidence. A different age stratification between our and Sumrein’s studies may also be an explanation for differences in findings. The Swedish Patient registry has a good validity regarding in-patient care [95] but to the best of our knowledge, the out-patient registry has not been validated regarding ICD10 codes for humerus fractures. Validation studies of any registry are important to confirm accuracy of findings.
This systematic review shows that there is very low certainty of evidence for treatment options for diaphyseal or distal fractures of the humerus in elderly patients. The absence of conclusive evidence should not be interpreted as evidence of lack of effectiveness. Rather, it means that further research is very likely to have an important impact.
Limitations
Some limitations of our systematic review should be noted. Despite the large number of publications on the treatment of humeral fractures, few of them meet the scientific standards to be included in our review. The low number of included trials–in combination with the heterogeneous interventions, comparators, and populations–made statistical tests of publication bias unreliable. We also solely had to rely on the information available in the included reports. Some reports did not, for instance, clearly indicate the severity of the fracture, the quality of the bone, when the surgery was performed in relation to the day of the fracture, or the number of individuals included in the analyses at one-year follow-up. In such situations, we assumed that all randomized participants were included, which might not always have been the case. Whether different modalities of non-operative treatment, including physiotherapy, could have influenced the outcome cannot be determined. We only reported outcomes at one-year follow-up, due to low number of included trials that reported on shorter times.
Evaluation of radiologic outcome was not performed in this systematic review and we have not included radiologic malunion in the presentation of complications in our report. On the other hand, we believe that a clinically significant malunion is likely to have been expressed as poor outcome. Other authors have also refrained from analyzing radiographic data of humerus fractures [4, 50, 90].
The registry data used for the analysis of surgical practice in Sweden has limitations since the fracture code (ICD10) does not allow specification of fracture severity and the procedural code e.g. does not discriminate between different types of arthroplasties. Detailed validation studies of the Swedish National Patient Registry have not been performed for fracture diagnoses and treatments.
An obvious strength with our study is its size and its coverage, it is methodologically sound and robust, and the production of all results have continuously been reviewed by expertise from the Swedish Agency for Health Technology Assessment and Assessment of Social Services, SBU. Another strength is that diaphyseal and distal humeral fractures also have been included in this systematic review.
Conclusions
Despite the limitations and the relatively few studies included, we conclude that surgical treatment of moderately displaced fractures of the proximal humerus in the elderly yields no clear benefit compared to the less costly non-surgical treatment option.
Based on these data one should have a restrictive attitude to surgical treatment of PHF. However, each patient should be treated individually rather than on a statistical basis and consideration has to be taken to fracture pattern and specific needs of the patient. For fractures of the distal parts of the humerus, too few studies have been published to draw meaningful conclusions in this context.
In future research, one should focus on methodologically well-conducted prospective comparative studies to evaluate the rate of functional recovery and outcomes associated with treatment methods, for humerus fractures, in which the population is clearly described regarding age, sex, bone quality and severity of the fracture. To contribute to higher quality of evidence, the studies need to have sufficiently number of individuals included, long follow-up (more than a year) and use validated measurement methods. Future studies should also report aspects of quality of life with validated instruments and include cost-effectiveness analyses.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
Karin Stenström accepts responsibility for the integrity and validity of the data collected and analysed. This systematic review was funded by and carried out within the framework of a public agency, the Swedish Agency for Health Technology Assessment and Assessment of Social Services. We would like to thank Anna Edling for diligent assistance with the figures and Lars-Eric Olsson (LEO) for valuable cooperation.
Data Availability
Most relevant data are within the paper and its Supporting Information files. Additional data is available at www.sbu.se/262e (see Appendices).
Funding Statement
This study was funded by and conducted within the framework of the Swedish Agency for Health Technology Assessment and Assessment of Social Services, SBU (www.sbu.se/en), a public Agency conducting health technology assessments. The study design, data collection and analyses were completed within this framework.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37(8):691–7. Epub 2006/07/04. 10.1016/j.injury.2006.04.130 . [DOI] [PubMed] [Google Scholar]
- 2.Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis care & research. 2012;64(3):407–14. Epub 2011/12/14. 10.1002/acr.21563 . [DOI] [PubMed] [Google Scholar]
- 3.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clinical orthopaedics and related research. 2006;442:87–92. Epub 2006/01/06. . [DOI] [PubMed] [Google Scholar]
- 4.Launonen AP, Lepola V, Flinkkila T, Laitinen M, Paavola M, Malmivaara A. Treatment of proximal humerus fractures in the elderly: a systemic review of 409 patients. Acta orthopaedica. 2015;86(3):280–5. Epub 2015/01/13. 10.3109/17453674.2014.999299 ; PubMed Central PMCID: PMCPMC4443467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. The Journal of bone and joint surgery American volume. 2000;82(4):478–86. Epub 2000/04/13. . [DOI] [PubMed] [Google Scholar]
- 6.Papasoulis E, Drosos GI, Ververidis AN, Verettas DA. Functional bracing of humeral shaft fractures. A review of clinical studies. Injury. 2010;41(7):e21–7. Epub 2009/06/16. 10.1016/j.injury.2009.05.004 . [DOI] [PubMed] [Google Scholar]
- 7.Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. The Journal of bone and joint surgery American volume. 2011;93(2):121–31. Epub 2011/01/21. 10.2106/JBJS.I.01505 ; PubMed Central PMCID: PMCPMC3016042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sumrein BO, Huttunen TT, Launonen AP, Berg HE, Fellander-Tsai L, Mattila VM. Proximal humeral fractures in Sweden-a registry-based study. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2017;28(3):901–7. Epub 2016/10/28. 10.1007/s00198-016-3808-z . [DOI] [PubMed] [Google Scholar]
- 9.Bjorkenheim JM, Pajarinen J, Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate: a retrospective evaluation of 72 patients followed for a minimum of 1 year. Acta orthopaedica Scandinavica. 2004;75(6):741–5. Epub 2005/03/15. . [DOI] [PubMed] [Google Scholar]
- 10.Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. Reverse shoulder arthroplasty versus hemiarthroplasty for treatment of proximal humerus fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2015;24(10):1560–6. Epub 2015/05/11. 10.1016/j.jse.2015.03.018 . [DOI] [PubMed] [Google Scholar]
- 11.Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. The Cochrane database of systematic reviews. 2015;(11):Cd000434. Epub 2015/11/13. 10.1002/14651858.CD000434.pub4 . [DOI] [PubMed] [Google Scholar]
- 12.Guy P, Slobogean GP, McCormack RG. Treatment preferences for displaced three- and four-part proximal humerus fractures. Journal of orthopaedic trauma. 2010;24(4):250–4. Epub 2010/03/26. 10.1097/BOT.0b013e3181bdc46a . [DOI] [PubMed] [Google Scholar]
- 13.Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Archives of osteoporosis. 2013;8:136 Epub 2013/10/12. 10.1007/s11657-013-0136-1 ; PubMed Central PMCID: PMCPMC3880487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elmagarmid A, Fedorowicz Z, Hammady H, Ilyas I, Khabsa M, Ouzzani M. Rayyan: a systematic reviews web app for exploring and filtering searches for eligible studies for Cochrane Reviews. Evidence-Informed Publich Health: Opportunities and Challenges Abstracts of the 22nd Cochrane Colloquium; 2014 21–26 Sep Evidence-Informed Publich Health: Opportunities and Challenges. Abstracts of the 22nd Cochrane Colloquium;: Hyderabad, India: John Wiley & Sons; 2014. [Google Scholar]
- 15.SBU, Swedish Agency for Health Technology Assessment and Assesment of Social Services. Checklist for Assessing the Risk of Bias [Preliminary version] 2017. Available from: www.sbu.se.http://www.sbu.se/contentassets/76adf07e270c48efaf67e3b560b7c59c/eng_metodboken.pdf.
- 16.Jonsson U, Bertilsson G, Allard P, Gyllensvard H, Soderlund A, Tham A, et al. Psychological Treatment of Depression in People Aged 65 Years and Over: A Systematic Review of Efficacy, Safety, and Cost-Effectiveness. PloS one. 2016;11(8):e0160859 Epub 2016/08/19. 10.1371/journal.pone.0160859 ; PubMed Central PMCID: PMCPMC4990289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. Jama. 1996;276(8):637–9. Epub 1996/08/28. . [DOI] [PubMed] [Google Scholar]
- 18.SBU, Swedish Agency for Health Technology Assessment and Assesment of Social Services. Checklist for Assessing the Quality of Health Economic Modelling Studies [Version 2017:1] 2017. Available from: www.sbu.se.
- 19.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602–8. 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L . [DOI] [PubMed] [Google Scholar]
- 20.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical orthopaedics and related research. 1987;(214):160–4. . [PubMed] [Google Scholar]
- 21.Olerud P, Tidermark J, Ponzer S, Ahrengart L, Bergstrom G. Responsiveness of the EQ-5D in patients with proximal humeral fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2011;20(8):1200–6. 10.1016/j.jse.2011.06.010 . [DOI] [PubMed] [Google Scholar]
- 22.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72. . [DOI] [PubMed] [Google Scholar]
- 23.Sintonen H. The 15D-measure of health-related quality of life. I. Reliability, validity and sensitivity of its health state descriptive system. National Centre for Health Program Evaluation, Working Paper 41. Melbourne: 1994.
- 24.Christiansen DH, Frost P, Falla D, Haahr JP, Frich LH, Svendsen SW. Responsiveness and Minimal Clinically Important Change: A Comparison Between 2 Shoulder Outcome Measures. The Journal of orthopaedic and sports physical therapy. 2015;45(8):620–5. 10.2519/jospt.2015.5760 . [DOI] [PubMed] [Google Scholar]
- 25.Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aarimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2013;22(12):1650–5. 10.1016/j.jse.2013.05.002 . [DOI] [PubMed] [Google Scholar]
- 26.Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14(6):1523–32. . [DOI] [PubMed] [Google Scholar]
- 27.Coretti S, Ruggeri M, McNamee P. The minimum clinically important difference for EQ-5D index: a critical review. Expert review of pharmacoeconomics & outcomes research. 2014;14(2):221–33. 10.1586/14737167.2014.894462 . [DOI] [PubMed] [Google Scholar]
- 28.The DASH Outcome Measure: http://www.dash.iwh.on.ca/faq. In.
- 29.Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis care & research. 2011;63 Suppl 11:S174–88. Epub 2012/05/25. 10.1002/acr.20630 . [DOI] [PubMed] [Google Scholar]
- 30.Kim JK, Park ES. Comparative responsiveness and minimal clinically important differences for idiopathic ulnar impaction syndrome. Clinical orthopaedics and related research. 2013;471(5):1406–11. Epub 2013/02/14. 10.1007/s11999-013-2843-8 ; PubMed Central PMCID: PMCPMC3613518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.St-Pierre C, Desmeules F, Dionne CE, Fremont P, MacDermid JC, Roy JS. Psychometric properties of self-reported questionnaires for the evaluation of symptoms and functional limitations in individuals with rotator cuff disorders: a systematic review. Disability and rehabilitation. 2016;38(2):103–22. Epub 2015/03/25. 10.3109/09638288.2015.1027004 . [DOI] [PubMed] [Google Scholar]
- 32.Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of clinical epidemiology. 2011;64(4):401–6. Epub 2011/01/07. 10.1016/j.jclinepi.2010.07.015 . [DOI] [PubMed] [Google Scholar]
- 33.Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, et al. The GRADE Working Group clarifies the construct of certainty of evidence. Journal of clinical epidemiology. 2017;87:4–13. Epub 2017/05/23. 10.1016/j.jclinepi.2017.05.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Negrini D, Kettle A, Sheppard L, Mills GH, Edbrooke DL. The cost of a hospital ward in Europe: is there a methodology available to accurately measure the costs? Journal of health organization and management. 2004;18(2–3):195–206. Epub 2004/09/16. 10.1108/14777260410548437 . [DOI] [PubMed] [Google Scholar]
- 35.Costa ML, Achten J, Caroline P, Parsons NR, Rangan A, Tubeuf S, et al. UK DRAFFT: A randomised controlled triaof percutaneous fixation with kirschner wires versus volar locking-plate fixation in the treatment of adult patients with a dorsally displaced fracture of the distal radius. Health Technology Assessment. 2015;19:17 FULL TEXT LINK 10.3310/hta19170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Navarro CM, Pettersson HJ, Enocson A. Complications after distal radius fracture surgery: results from a Swedish nationwide registry study. Journal of orthopaedic trauma. 2015;29(2):e36–42. Epub 2014/07/23. 10.1097/BOT.0000000000000199 . [DOI] [PubMed] [Google Scholar]
- 37.Pritchett JW. External fixation or closed medullary pinning for unstable Colles fractures? Journal of Bone and Joint Surgery—Series B. 1995;77(2):267–9. ; PubMed Central PMCID: PMC7706344. [PubMed] [Google Scholar]
- 38.Schonnemann JO, Hansen TB, Soballe K. Randomised study of non-bridging external fixation compared with intramedullary fixation of unstable distal radial fractures. Journal of plastic surgery and hand surgery. 2011;45(4–5):232–7. Epub 2011/12/14. 10.3109/2000656X.2011.613243 . [DOI] [PubMed] [Google Scholar]
- 39.Klassifikation av sjukdomar och hälsoproblem 1997, Swedish version of International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). www.socialstyrelsen.se.
- 40.Klassifikation av kirurgiska åtgärder 1997. Swedish version of NOMESCO, Classification of Surgical Procedures Version 1.9. www.socialstyrelsen.se
- 41.Chalmers PN, Slikker W, Mall NA, Gupta AK, Rahman Z, Enriquez D, et al. Reverse total shoulder arthroplasty for acute proximal humeral fracture: comparison to open reduction-internal fixation and hemiarthroplasty. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2014;23(2):197–204. Epub 2013/10/01. 10.1016/j.jse.2013.07.044 . [DOI] [PubMed] [Google Scholar]
- 42.Dean BJF, Jones LD, Palmer AJR, Macnair RD, Brewer PE, Jayadev C, et al. A review of current surgical practice in the operative treatment of proximal humeral fractures: Does the profher trial demonstrate a need for change? Bone JtRes. 2016;5(5):178–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Handschin AE, Cardell M, Contaldo C, Trentz O, Wanner GA. Functional results of angular-stable plate fixation in displaced proximal humeral fractures. Injury. 2008;39(3):306–13. Epub 2008/02/05. 10.1016/j.injury.2007.10.011 . [DOI] [PubMed] [Google Scholar]
- 44.Manoli A, Capriccioso CE, Konda SR, Egol KA, Author A, Nyu hospital for joint diseases US, et al. Total shoulder arthroplasty for proximal humerus fracture is associated with increased hospital charges despite a shorter length of stay. Orthopaedics and Traumatology: Surgery and Research. 2016;102(1):19–24. PubMed PMID: 20160104132 FULL TEXT LINK 10.1016/j.otsr.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 45.Sabharwal S, Carter AW, Rashid A, Darzi A, Reilly P, Gupte CM. Cost analysis of the surgical treatment of fractures of the proximal humerus: an evaluation of the determinants of cost and comparison of the institutional cost of treatment with the national tariff. The bone & joint journal. 2016;98-b(2):249–59. Epub 2016/02/07. 10.1302/0301-620x.98b2.36255 . [DOI] [PubMed] [Google Scholar]
- 46.Solomon JA, Joseph SM, Shishani Y, Victoroff BN, Wilber JH, Gobezie R, et al. Cost Analysis of Hemiarthroplasty Versus Reverse Shoulder Arthroplasty for Fractures. Orthopedics. 2016:1–6. Epub 2016/06/21. 10.3928/01477447-20160610-03 . [DOI] [PubMed] [Google Scholar]
- 47.Corbacho B, Duarte A, Keding A, Handoll H, Chuang LH, Torgerson D, et al. Cost effectiveness of surgical versus nonsurgical treatment of adults with displaced fractures of the proximal humerus: Economic evaluation alongside the profher trial. Bone and Joint Journal. 2016;98B(2):152–9. PubMed PMID: 20160156676; PubMed Central PMCID: PMC26850418. [DOI] [PubMed] [Google Scholar]
- 48.Nwachukwu BU, Schairer WW, McCormick F, Dines DM, Craig EV, Gulotta LV, et al. Arthroplasty for the surgical management of complex proximal humerus fractures in the elderly: A cost-utility analysis. Journal of Shoulder and Elbow Surgery. 2016;25(5):704–13. PubMed PMID: 20160224309 FULL TEXT LINK 10.1016/j.jse.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 49.Fjalestad T, Hole MO, Jorgensen JJ, Stromsoe K, Kristiansen IS. Health and cost consequences of surgical versus conservative treatment for a comminuted proximal humeral fracture in elderly patients. Injury. 2010;41(6):599–605. Epub 2009/12/01. 10.1016/j.injury.2009.10.056 . [DOI] [PubMed] [Google Scholar]
- 50.Handoll H, Brealey S, Rangan A, Keding A, Corbacho B, Jefferson L, et al. The ProFHer (PROximal fracture of the humerus: Evaluation by randomisation) trial–A pragmatic multicentre randomized controlled trial evaluating the clinical effectiveness and cost-effectiveness of surgical compared with non-surgical treatment for proximal fracture of the humerus in adults. Health Technology Assessment. 2015;19(24):1–279. 10.3310/hta19240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2011;20(5):747–55. Epub 2011/03/26. 10.1016/j.jse.2010.12.018 . [DOI] [PubMed] [Google Scholar]
- 52.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2011;20(7):1025–33. Epub 2011/07/26. 10.1016/j.jse.2011.04.016 . [DOI] [PubMed] [Google Scholar]
- 53.Liu ZZ, Zhang GM, Ge T. Use of a proximal humeral internal locking system enhanced by injectable graft for minimally invasive treatment of osteoporotic proximal humeral fractures in elderly patients. Orthopaedic surgery. 2011;3(4):253–8. Epub 2011/10/25. 10.1111/j.1757-7861.2011.00150.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen H, Ji X, Gao Y, Zhang L, Zhang Q, Liang X, et al. Comparison of intramedullary fibular allograft with locking compression plate versus shoulder hemi-arthroplasty for repair of osteoporotic four-part proximal humerus fracture: Consecutive, prospective, controlled, and comparative study. Orthopaedics & traumatology, surgery & research: OTSR. 2016;102(3):287–92. Epub 2016/03/08. 10.1016/j.otsr.2015.12.021 . [DOI] [PubMed] [Google Scholar]
- 55.Fjalestad T, Hole MO. Displaced proximal humeral fractures: operative versus non-operative treatment—a 2-year extension of a randomized controlled trial. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie. 2014;24(7):1067–73. Epub 2014/01/15. 10.1007/s00590-013-1403-y . [DOI] [PubMed] [Google Scholar]
- 56.Boons HW, Goosen JH, van Grinsven S, van Susante JL, van Loon CJ. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clinical orthopaedics and related research. 2012;470(12):3483–91. Epub 2012/08/17. 10.1007/s11999-012-2531-0 ; PubMed Central PMCID: PMCPmc3492647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. The Journal of bone and joint surgery British volume. 1997;79(3):412–7. Epub 1997/05/01. . [DOI] [PubMed] [Google Scholar]
- 58.Hauschild O, Konrad G, Audige L, de Boer P, Lambert SM, Hertel R, et al. Operative versus non-operative treatment for two-part surgical neck fractures of the proximal humerus. Archives of orthopaedic and trauma surgery. 2013;133(10):1385–93. Epub 2013/07/04. 10.1007/s00402-013-1798-2 . [DOI] [PubMed] [Google Scholar]
- 59.Innocenti M, Carulli C, Civinini R, Matassi F, Tani M, Muncibi F, et al. Displaced fragility fractures of proximal humerus in elderly patients affected by severe comorbidities: Percutaneous fixation and conservative treatment. Aging clinical and experimental research. 2013;25(4):447–52. PubMed PMID: 2013683729; PubMed Central PMCID: PMC23760947. 10.1007/s40520-013-0063-4 [DOI] [PubMed] [Google Scholar]
- 60.Schai P, Imhoff A, Preiss S. Comminuted humeral head fractures: a multicenter analysis. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 1995;4(5):319–30. Epub 1995/09/01. . [DOI] [PubMed] [Google Scholar]
- 61.Sebastia-Forcada E, Cebrian-Gomez R, Lizaur-Utrilla A, Gil-Guillen V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2014. Epub 2014/08/05. 10.1016/j.jse.2014.06.035 . [DOI] [PubMed] [Google Scholar]
- 62.Cuff DJ, Pupello DR. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. The Journal of bone and joint surgery American volume. 2013;95(22):2050–5. Epub 2013/11/22. 10.2106/JBJS.L.01637 . [DOI] [PubMed] [Google Scholar]
- 63.Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthopaedics & traumatology, surgery & research: OTSR. 2009;95(1):48–55. Epub 2009/03/03. 10.1016/j.otsr.2008.09.002 . [DOI] [PubMed] [Google Scholar]
- 64.Boyle MJ, Youn SM, Frampton CM, Ball CM. Functional outcomes of reverse shoulder arthroplasty compared with hemiarthroplasty for acute proximal humeral fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2013;22(1):32–7. Epub 2012/06/02. 10.1016/j.jse.2012.03.006 . [DOI] [PubMed] [Google Scholar]
- 65.Shi HF, Xiong J, Chen YX, Wang JF, Wang SF, Chen ZJ, et al. Management of proximal humeral fractures in elderly patients with uni- or polyaxial locking osteosynthesis system. Archives of orthopaedic and trauma surgery. 2011;131(4):541–7. Epub 2010/10/22. 10.1007/s00402-010-1199-8 . [DOI] [PubMed] [Google Scholar]
- 66.Voigt C, Geisler A, Hepp P, Schulz AP, Lill H. Are polyaxially locked screws advantageous in the plate osteosynthesis of proximal humeral fractures in the elderly? A prospective randomized clinical observational study. Journal of orthopaedic trauma. 2011;25(10):596–602. Epub 2011/06/15. 10.1097/BOT.0b013e318206eb46 . [DOI] [PubMed] [Google Scholar]
- 67.Zhang L, Zheng J, Wang W, Lin G, Huang Y, Zheng J, et al. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. International orthopaedics. 2011;35(11):1655–61. Epub 2011/03/10. 10.1007/s00264-011-1227-5 ; PubMed Central PMCID: PMCPmc3193968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Peng CH, Wu WT, Yu TC, Chen LC, Hsu SH, Kwong ST, et al. Surgical treatment for proximal humeral fracture in elderly patients with emphasis on the use of intramedullary strut allografts. Tzu Chi Medical Journal. 2012;24(3):131–5. 10.1016/j.tcmj.2012.08.010 [Google Scholar]
- 69.Spross C, Platz A, Erschbamer M, Lattmann T, Dietrich M. Surgical treatment of Neer Group VI proximal humeral fractures: retrospective comparison of PHILOS(R) and hemiarthroplasty. Clinical orthopaedics and related research. 2012;470(7):2035–42. Epub 2011/12/14. 10.1007/s11999-011-2207-1 ; PubMed Central PMCID: PMCPmc3369075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ortmaier R, Mattiassich G, Pumberger M, Hitzl W, Moroder P, Auffarth A, et al. Comparison between reverse shoulder arthroplasty and Humerusblock in three- and four-part proximal humerus fractures in elderly patients. International orthopaedics. 2015;39(2):335–42. Epub 2014/07/21. 10.1007/s00264-014-2433-8 . [DOI] [PubMed] [Google Scholar]
- 71.Gracitelli ME, Malavolta EA, Assuncao JH, Kojima KE, Dos Reis PR, Silva JS, et al. Locking intramedullary nails compared with locking plates for two- and three-part proximal humeral surgical neck fractures: a randomized controlled trial. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2016;25(5):695–703. Epub 2016/04/18. 10.1016/j.jse.2016.02.003 . [DOI] [PubMed] [Google Scholar]
- 72.Gradl G, Dietze A, Kaab M, Hopfenmuller W, Mittlmeier T. Is locking nailing of humeral head fractures superior to locking plate fixation? Clinical orthopaedics and related research. 2009;467(11):2986–93. Epub 2009/06/16. 10.1007/s11999-009-0916-5 ; PubMed Central PMCID: PMCPmc2758984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Urda A, Gonzalez A, Colino A, Lopiz Y, Garcia-Fernandez C, Marco F. Management of displaced surgical neck fractures of the humerus: health related quality of life, functional and radiographic results. Injury. 2012;43 Suppl 2:S12–9. Epub 2013/05/03. 10.1016/s0020-1383(13)70174-8 . [DOI] [PubMed] [Google Scholar]
- 74.Konrad G, Audige L, Lambert S, Hertel R, Sudkamp NP. Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures. Clinical orthopaedics and related research. 2012;470(2):602–9. Epub 2011/09/01. 10.1007/s11999-011-2056-y ; PubMed Central PMCID: PMCPmc3254759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fialka C, Stampfl P, Arbes S, Reuter P, Oberleitner G, Vecsei V. Primary hemiarthroplasty in four-part fractures of the proximal humerus: randomized trial of two different implant systems. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2008;17(2):210–5. Epub 2007/10/13. 10.1016/j.jse.2007.07.002 . [DOI] [PubMed] [Google Scholar]
- 76.Dietz SO, Broos P, Nijs S, Author A, Centre f, Musculoskeletal Surgery UMCJ, et al. Suture fixation versus cable cerclage of the tuberosities in shoulder arthroplasty-clinical and radiologic results. Archives of orthopaedic and trauma surgery. 2012;132(6):793–800. PubMed PMID: 2012475172; PubMed Central PMCID: PMC22323058. 10.1007/s00402-012-1470-2 [DOI] [PubMed] [Google Scholar]
- 77.Lopiz Y, Garcia-Coiradas J, Garcia-Fernandez C, Marco F. Proximal humerus nailing: a randomized clinical trial between curvilinear and straight nails. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2014;23(3):369–76. Epub 2013/12/03. 10.1016/j.jse.2013.08.023 . [DOI] [PubMed] [Google Scholar]
- 78.Agorastides I, Sinopidis C, El Meligy M, Yin Q, Brownson P, Frostick SP. Early versus late mobilization after hemiarthroplasty for proximal humeral fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2007;16(3 Suppl):S33–8. Epub 2006/12/19. 10.1016/j.jse.2006.07.004 . [DOI] [PubMed] [Google Scholar]
- 79.Chen F, Wang Z, Bhattacharyya T. Outcomes of nails versus plates for humeral shaft fractures: a Medicare cohort study. Journal of orthopaedic trauma. 2013;27(2):68–72. Epub 2013/01/25. 10.1097/BOT.0b013e31824a3e66 ; PubMed Central PMCID: PMCPmc3399046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McKee MD, Veillette CJ, Hall JA, Schemitsch EH, Wild LM, McCormack R, et al. A multicenter, prospective, randomized, controlled trial of open reduction—internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2009;18(1):3–12. Epub 2008/10/01. 10.1016/j.jse.2008.06.005 . [DOI] [PubMed] [Google Scholar]
- 81.Prasad N, Dent C. Outcome of total elbow replacement for distal humeral fractures in the elderly: a comparison of primary surgery and surgery after failed internal fixation or conservative treatment. The Journal of bone and joint surgery British volume. 2008;90(3):343–8. Epub 2008/03/04. 10.1302/0301-620X.90B3.18971 . [DOI] [PubMed] [Google Scholar]
- 82.Konrad G, Hirschmuller A, Audige L, Lambert S, Hertel R, Sudkamp NP. Comparison of two different locking plates for two-, three- and four-part proximal humeral fractures—results of an international multicentre study. International orthopaedics. 2012;36(5):1051–8. Epub 2011/12/01. 10.1007/s00264-011-1410-8 ; PubMed Central PMCID: PMCPmc3337113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ortmaier R, Filzmaier V, Hitzl W, Bogner R, Neubauer T, Resch H, et al. Comparison between minimally invasive, percutaneous osteosynthesis and locking plate osteosynthesis in 3-and 4-part proximal humerus fractures. BMC musculoskeletal disorders. 2015;16:297 Epub 2015/10/16. 10.1186/s12891-015-0770-4 ; PubMed Central PMCID: PMCPMC4607011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lin J. Effectiveness of locked nailing for displaced three-part proximal humeral fractures. The Journal of trauma. 2006;61(2):363–74. Epub 2006/08/19. 10.1097/01.ta.0000224148.73016.30 . [DOI] [PubMed] [Google Scholar]
- 85.Kazakos K, Lyras DN, Galanis V, Verettas D, Psillakis I, Chatzipappas C, et al. Internal fixation of proximal humerus fractures using the Polarus intramedullary nail. Archives of orthopaedic and trauma surgery. 2007;127(7):503–8. Epub 2007/07/11. 10.1007/s00402-007-0390-z . [DOI] [PubMed] [Google Scholar]
- 86.Beks RB, Ochen Y, Frima H, Smeeing DPJ, van der Meijden O, Timmers TK, et al. Operative versus nonoperative treatment of proximal humeral fractures: a systematic review, meta-analysis, and comparison of observational studies and randomized controlled trials. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2018. Epub 2018/05/08. 10.1016/j.jse.2018.03.009 . [DOI] [PubMed] [Google Scholar]
- 87.Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. The Cochrane database of systematic reviews. 2011;(6):Cd005959 Epub 2011/06/17. 10.1002/14651858.CD005959.pub2 . [DOI] [PubMed] [Google Scholar]
- 88.Gosler MW, Testroote M, Morrenhof JW, Janzing HM. Surgical versus non-surgical interventions for treating humeral shaft fractures in adults. The Cochrane database of systematic reviews. 2012;1:Cd008832 Epub 2012/01/20. 10.1002/14651858.CD008832.pub2 . [DOI] [PubMed] [Google Scholar]
- 89.Harding P, Rasekaba T, Smirneos L, Holland AE. Early mobilisation for elbow fractures in adults. The Cochrane database of systematic reviews. 2011;(6):Cd008130 Epub 2011/06/17. 10.1002/14651858.CD008130.pub2 . [DOI] [PubMed] [Google Scholar]
- 90.Sabharwal S, Patel NK, Griffiths D, Athanasiou T, Gupte CM, Reilly P. Trials based on specific fracture configuration and surgical procedures likely to be more relevant for decision making in the management of fractures of the proximal humerus: Findings of a meta-analysis. Bone & joint research. 2016;5(10):470–80. Epub 2016/10/21. 10.1302/2046-3758.510.2000638 ; PubMed Central PMCID: PMCPMC5086838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Handoll HH, Keding A, Corbacho B, Brealey SD, Hewitt C, Rangan A. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. The bone & joint journal. 2017;99-b(3):383–92. Epub 2017/03/03. 10.1302/0301-620x.99b3.bjj-2016-1028 ; PubMed Central PMCID: PMCPMC5404240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dean BJ, Jones LD, Palmer AJ, Macnair RD, Brewer PE, Jayadev C, et al. A review of current surgical practice in the operative treatment of proximal humeral fractures: Does the PROFHER trial demonstrate a need for change? Bone & joint research. 2016;5(5):178–84. Epub 2016/05/15. 10.1302/2046-3758.55.2000596 ; PubMed Central PMCID: PMCPMC4921043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rosas S, Law TY, Kurowicki J, Formaini N, Kalandiak SP, Levy JC. Trends in surgical management of proximal humeral fractures in the Medicare population: a nationwide study of records from 2009 to 2012. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2016;25(4):608–13. Epub 2015/10/18. 10.1016/j.jse.2015.08.011 . [DOI] [PubMed] [Google Scholar]
- 94.Khatib O, Onyekwelu I, Zuckerman JD. The incidence of proximal humeral fractures in New York State from 1990 through 2010 with an emphasis on operative management in patients aged 65 years or older. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al. ]. 2014;23(9):1356–62. Epub 2014/04/15. 10.1016/j.jse.2013.12.034 . [DOI] [PubMed] [Google Scholar]
- 95.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC public health. 2011;11:450 Epub 2011/06/11. 10.1186/1471-2458-11-450 ; PubMed Central PMCID: PMCPMC3142234. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
Most relevant data are within the paper and its Supporting Information files. Additional data is available at www.sbu.se/262e (see Appendices).