Summary
Objective
Minimizing program dropout is essential for weight‐loss success, but factors that influence dropout among commercial programs are unclear. This study's objective was to determine factors associated with early dropout in a commercial weight‐loss program.
Methods
A retrospective analysis of a remotely delivered, employer‐based commercial program from 2013 to 2016 was conducted. The dependent variable was ‘early dropout’, defined as enrollees who disengaged from telephone coaching by month 2's end. Independent variables included demographics, program website engagement and early weight change. Multivariate logistic regression analyses were used to assess for differences in early dropout by several factors, adjusted for employer clustering.
Results
Of the 5,274 participants, 26.8% dropped out early. Having ≥1 chronic condition (odds ratio [OR] 1.41, p < 0.001) and ‘weight‐loss failure’ defined as ≥0% weight change at month 1's end (OR 1.86, p < 0.001) had significantly increased odds of early dropout. Increasing age by 10‐year intervals (OR 0.90, p = 0.002) and ‘meeting the website login goal’ defined as ≥90 logins in 3 months (OR 0.13, p < 0.001) significantly decreased the odds of early dropout.
Conclusions
Presence of comorbidities, less online engagement and weight‐loss failure were associated with early dropout in a commercial program. Strategies to prevent dropout among high‐risk participants, such as increased support or program tailoring, should be developed and tested.
Keywords: Commercial weight‐loss program, dropout
Introduction
In randomized controlled trials (RCTs), behavioural weight‐loss programs have been designed and tested to address obesity and reduce comorbidities. For example, 35% of participants in the Diabetes Prevention Program trial sustained the 7% weight loss goal and reduced their risk of developing diabetes mellitus at the final study visit 3 years later 1. In general, greater weight loss has been associated with greater participation in and continued engagement with the intervention/study staff in clinical trials 2, 3, 4. This association also appears true for web‐based weight‐loss interventions, as a systematic review found evidence to suggest that greater usage of the program website was associated with greater weight loss 5. Minimizing program dropout has been deemed essential for success; however, there is a need to better understand the factors that influence attrition 6.
A 2011 systematic review on factors related to dropout concluded that younger participants and participants with lower educational status were more likely to drop out of trials with in‐person weight‐loss interventions 2. Most studies did not find an association between baseline weight and dropout; however, participants with greater/unrealistic weight‐loss expectations and less initial weight loss were more likely to drop out. Similar findings were reported in a 2014 systematic review of lifestyle modification programs 7. A 2010 systematic review of web‐based weight management interventions attempted to synthesize whether components of web‐based interventions were associated with attrition; however, few published studies reported these outcomes 5. Program‐level factors that influenced dropout among in‐person weight‐loss interventions included greater travel distance, financial difficulties and the requirement to pay for treatment 2. In hospital/clinic‐based programs, dropout occurs frequently within the first few months and has been associated with various factors including younger age, male sex, non‐Hispanic Black race, hypertension and greater travel distance 3, 8, 9.
Commercial weight‐loss programs are popular among individuals looking to lose weight 10, 11, and recent guidelines suggest that clinicians consider referring patients to commercial programs with demonstrated weight loss efficacy 12. A 2015 systematic review found that few commercial programs demonstrated significantly greater long‐term weight losses than comparators in RCTs, and this review found that attrition varied across included trials (e.g. range 18–46% within Weight Watchers RCTs at 12 months; 4–13% within Jenny Craig RCTs at 12 months) 13. Similarly, an RCT of the commercial smartphone application (app), My Fitness Pal, demonstrated a precipitous drop in usage over the 6‐month study 14. Overall, factors contributing to this varying degree of dropout are unclear. Attrition is also a challenge for commercial programs outside the trial setting, as individuals frequently drop out within a few months 15, 16, 17. An analysis of over 60,000 Jenny Craig clients found that 27% drop out at 4 weeks and 58% by 13 weeks 16. A prior study of the online commercial program, The Biggest Loser Club, found that non‐usage attrition occurred commonly 18. Evidence providing reasons for the high degree of dropout among commercial program participants outside the clinical trial setting is limited. Given that individuals usually self‐refer and/or pay out‐of‐pocket for commercial programs, different factors might contribute to participant dropout than those factors identified among participants of trials testing behavioural interventions or hospital/clinic‐based programs 2.
The study objective was to determine the participant characteristics, program website engagement and weight‐loss factors associated with early dropout in a remotely delivered, employer‐based commercial weight‐loss program among participants outside a clinical trial setting. The study hypothesis was that dropout would be greater among participants with younger age, greater baseline body mass index (BMI), more chronic medical conditions, fewer website logins and smaller early weight loss. Understanding factors associated with commercial program dropout might (1) aid clinicians in identifying patients at high risk for dropout who they refer to these programs and then taking action to support these individuals and (2) help commercial programs consider modifications to their strategy to promote attendance and completion, as individuals are unlikely to attain weight loss without continued participation.
Methods
Description of commercial program
The study used data available from Innergy®, which is an employer‐based commercial weight‐loss program that combines telephone coaching with web‐based support. Innergy® was adapted from a remotely delivered behavioural weight‐loss intervention previously shown to be effective in an RCT – Practice‐based Opportunities for Weight Reduction (POWER) at Johns Hopkins 19. In the first 3 months, participants have weekly calls with their coach, and then calls decrease in occurrence after that point (once a month during months 4–12 and every 6–8 weeks in months 13–24). The coaches provide support and promote behaviour change using motivational interviewing techniques – coaching is considered the key feature of this program. Web‐based components include educational modules and self‐monitoring of weight, food intake and physical activity. The program promotes the use of the DASH Eating Plan 20 as the dietary strategy and recommends 30–60 min of moderate intensity aerobic exercise 5–7 d per week. During the program, participants were encouraged to track their weight, food and physical activity daily through the website, and this website was used by coaches to communicate electronically with participants as well as document telephone encounters.
To enrol, participants had to be affiliated with an organization who had contracted to offer Innergy® to their eligible beneficiaries. Generally, eligible beneficiaries included employees, spouses and dependents with obesity. Organizations covered a portion of the costs for beneficiaries to participate (six covered all program costs and three covered some of the program costs), and this benefit was promoted via targeting of eligible individuals and/or internal mass media campaigns where individuals were directed to the online registration site. Of the nine organizations, three were for‐profit companies and six were non‐profit entities. Given these differences by organization, analyses were adjusted for clustering by organization/employer to account for these effects.
Study design and data source
The study was a retrospective analysis of de‐identified data from participants in Innergy® (data from 2/2013 to 10/2016) from two sources – baseline survey and website tracking data. As a part of the online registration, participants answered questions regarding their demographics and health status, which was the baseline survey. Throughout the program, the website tracked usage, and data were entered by both participants and coaches.
The Johns Hopkins Institutional Review Board declared this project not human subjects research. To be included in this analysis, participants had to complete program enrolment by 30 June 2016 (completed registration, at least one coach call and recorded at least two weights) so that all had the opportunity to reach the 3‐month time point in the program based on their enrolment date (255 right censored as they had less than 3 months of enrolment) (Figure S1).
Variables
The dependent variable was ‘early dropout’, which was defined as participants who disengaged from the telephone coaching program by the end of month 2. Dropout could occur in two ways: participants who (1) did not complete more than two coach calls by the end of month 2 (‘non‐usage attrition’ as failed to participate) or (2) purposely exited by the end of month 2 (‘purposeful dropout’).
The independent variables included several individual‐level, program website engagement and weight‐loss factors. Individuals right‐censored at the 3‐month time point did not contribute data for any 3‐month independent variables described in the next discussion. Individual‐level factors included baseline age, gender, weight, BMI (calculated from self‐reported weight and height), smoking status, number of chronic conditions and self‐reported chronic conditions (i.e. hypertension, dyslipidaemia, dysglycaemia, sleep apnoea, depression, osteoarthritis and asthma). Program website engagement included the number of website logins during months 1–3, as well as approximating participants as ‘meeting the website login goal’ if they logged into the website at least 90 times during the first 3 months, as the program recommends that participants login at least daily (i.e. daily logins would total at least 90 over a 3‐month or approximately 90‐d period). Several weight‐loss outcomes were examined including ‘weight loss failure’ (defined as weight change ≥0% at the end of the first month), as well as per cent weight change at months 1 and 3. For individuals with missing weight data at the 3‐month time point due to failure to track their weight, both a last‐observation‐carried‐forward approach and a baseline‐observation‐carried‐forward approach were employed to address the missing values. A modified completers' approach was also employed, which included individuals that had at least one weight value reported in month 3. No missing weight data existed for month 1. As weight change is self‐reported and prone to data entry errors by the participants, extreme weight change values were excluded from weight analyses (>15% change at month 1; >30% change at month 3 [of note, n for these groups included in the Table 1 footnotes]).
Table 1.
Baseline individual‐level characteristics, program website engagement factors and early weight change among those without and with early dropout
| Not early dropout | Early dropout | p‐value* | |
|---|---|---|---|
| n = 3,861 | n = 1,413 | ||
| Individual‐level characteristics | |||
| Mean age in years (SD) | 48.6 (10.4) | 47.5 (10.5) | <0.001 |
| Women, % | 75.9 | 76.8 | 0.49 |
| Mean weight in kg (SD) | 105.6 (21.4) | 106.1 (21.2) | 0.49 |
| Mean BMI in kg m−2 (SD) | 37.4 (6.7) | 37.6 (6.5) | 0.41 |
| % Current smokers | 3.3 | 6.3 | <0.001 |
| # chronic conditions, % | |||
| 0 | 45.0 | 33.1 | <0.001 |
| 1–2 | 36.9 | 41.8 | |
| 3–4 | 15.4 | 21.2 | |
| ≥5 | 2.6 | 3.8 | |
| ≥1 chronic condition, % | 55.0 | 66.9 | <0.001 |
| Specific chronic conditions†, % | |||
| Hypertension | 28.6 | 34.4 | <0.001 |
| Dyslipidaemia† | 29.0 | 34.9 | <0.001 |
| Dysglycaemia† | 13.2 | 18.5 | <0.001 |
| Sleep apnoea | 15.2 | 20.2 | <0.001 |
| Depression | 13.0 | 20.1 | <0.001 |
| Osteoarthritis | 9.8 | 10.8 | 0.29 |
| Asthma | 9.5 | 12.5 | 0.002 |
| Program website engagement factors | |||
| Median # logins during M1–3 (IQR) | 59 (27,124) | 15 (7,32) | <0.001 |
| Median # logins in M1 (IQR) | 28 (13,56) | 10 (5,20) | <0.001 |
| Median # logins in M2 (IQR) | 16 (5,39) | 1 (0,5) | <0.001 |
| Median # logins in M3 (IQR) | 9 (2,28) | 0 (0,1) | <0.001 |
| Met login goal (≥90 over 3 months), % | 34.9 | 5.4 | <0.001 |
| Early weight change‡ | |||
| Weight loss failure, % | 20.4 | 38.2 | <0.001 |
| Mean M1 weight change (SD) | −1.7% (2.0) | −0.8% (1.9) | <0.001 |
| Mean M3 weight change, mC (SD) | −3.7% (3.5) | −1.6% (3.0) | <0.001 |
| Mean M3 weight change, LOCF (SD) | −3.3% (3.4) | −1.1% (2.5) | <0.001 |
| Mean M3 weight change, BOCF (SD) | −3.0% (3.4) | −0.4% (1.7) | <0.001 |
Bivariate analyses comparing ‘not early dropout’ and ‘early dropout’ groups conducted using t‐tests, Chi2 tests and Wilcoxon rank‐sum tests, as appropriate. Given the multiple comparison testing, we defined a statistically significant p‐value as p < 0.002 per Bonferroni correction (signified by bold text).
We identified a participant as having dyslipidaemia if he or she endorsed high cholesterol and/or low high‐density lipoprotein and as having dysglyceamia if he or she endorsed having prediabetes and/or diabetes.
Weight change analyses excluded individuals with extreme change values, which we defined as >15% change at M1 (n = 28) and >30% change at M3 (n = 10 for mC, n = 22 for LOCF and n = 10 for BOCF). All participants had a weight reported in M1, so there were no missing weight data. At M3, 1,755 individuals had missing weight entry. Therefore, we report the results of the mC analysis (i.e. those that had at least one weight value reported in M3), as well as LOCF or BOCF approaches to handle missing data. Therefore, the samples included in the weight analyses were M1 = 5,246, M3 mC = 3,509, M3 LOCF = 5,252 and M3 BOCF = 5,264.
BMI, body mass index; BOCF, baseline observation carried forward; IQR, interquartile range; LOCF, last observation carried forward; M1, month 1; M2, month 2; M3, month 3; mC, modified completers.
Analyses
Descriptive analyses of all variables were conducted, as well as bivariate analyses using t‐tests, Chi2 tests and Wilcoxon rank‐sum tests, as appropriate, to examine for differences in early dropout status by individual‐level, program website engagement and weight‐change factors. Given the multiple comparison testing, a Bonferroni corrected p‐value was used to define statistical significance (p < 0.002) for these bivariates analyses. Multivariate logistic regression was used, adjusted for clustering by organization/employer, to examine the association between early dropout and all statistically significant factors identified in bivariate analyses, specifically weight loss failure, age scaled by 10‐year intervals, smoking status, ≥1 chronic condition and meeting the website login goal. Based on these results, adjusted predicted probabilities were calculated for early dropout for weight loss failure, smoking status, ≥1 chronic condition and meeting the website login goal. Finally, multivariate logistic regression was conducted assessing the association between early dropout and per cent weight change at month 3, adjusted for age, smoking status, ≥1 chronic condition, meeting the website login goal and clustering by organization/employer.
Results
The analysis included 5,274 participants. The mean age was 48.3 years (SD 10.4), 76.1% were women and mean BMI was 37.4 kg m−2 (SD 6.6). Overall, 26.8% (n = 1,413) met the definition of early dropout. For those meeting this definition, 31.5% were purposeful dropouts (n = 445), whereas 68.5% met criteria for non‐usage attrition (n = 968).
Regarding individual‐level factors, participants with early dropout were more likely to be younger, current smokers and have more chronic conditions in bivariate analyses (Table 1). Individuals with hypertension, dyslipidaemia, dysglycaemia, sleep apnoea and depression were significantly more likely to drop out early (Table 1). With respect to program website engagement factors, participants who dropped out early had significantly fewer website logins compared with those without early dropout in bivariate analyses (Table 1). Participants with early dropout fell far short of achieving the website login goal compared with participants who did not drop out early (34.9% vs. 5.4%, p < 0.001). Regarding weight‐loss factors, dropouts were significantly more likely to experience weight loss failure (38.2% vs. 20.4%, p < 0.001) and had significantly less weight loss at months 1 and 3 compared with those who did not drop out in bivariate analyses, regardless of method used to handle missing data (Table 1).
In the multivariate model, all statistically significant factors in bivariate analyses remained significant (Figure 1). Specifically, weight‐loss failure (odds ratio [OR] 1.86, 95% confidence interval [CI] 1.67–2.08, p < 0.001), smoking status (OR 1.77, 95% CI 1.21–2.57, p = 0.003) and ≥1 chronic condition (OR 1.41, 95% CI 1.33–1.49, p < 0.001) significantly increased the odds of early dropout. In contrast, increasing age by 10‐year intervals (OR 0.90, 95% CI 0.85–0.96, p = 0.002) and meeting the website login goal (OR 0.13, 95% CI 0.08–0.19, p < 0.001) significantly decreased the odds of early dropout. With respect to month 3 weight change, the odds of early dropout significantly increased as mean per cent weight change increased (modified completers' approach: OR 1.17, 95% CI 1.14–1.21, p < 0.001; last‐observation‐carried‐forward approach: OR 1.22, 95% CI 1.18–1.25, p < 0.001; baseline‐observation‐carried‐forward approach: OR 1.42, 95% CI 1.35–1.49, p < 0.001).
Figure 1.
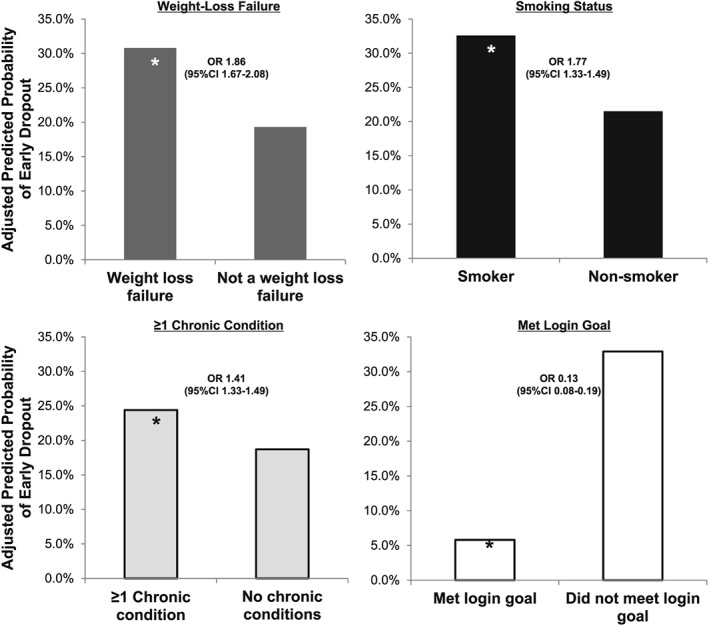
Adjusted predicted probability of early dropout by several factors. Factors presented are weight‐loss failure, smoking status, presence of chronic conditions and meeting the website login goal. Weight‐loss failure defined as weight change ≥0% at the end of the first month. Meeting the website login goal defined as logging into the website at least 90 times during the first 3 months. Early dropout defined as participants who disengaged from the telephone coaching program by the end of month 2 by either failing to complete more than two coach calls or purposely exiting the program. Predicted probabilities calculated from the result of logistic regression model that includes all factors listed as well as adjustment for age and clustering by organization/employer. ‘*’ indicates a statistically significant difference from the comparator. CI, confidence interval; OR, odds ratio.
Discussion
In this study, several individual‐level, program website engagement and weight‐change factors were significantly associated with early dropout in an employer‐based commercial weight‐loss program. Individual‐level factors associated with early dropout included younger age and greater number of chronic conditions. Current smoking status was statistically significant, although the between‐group difference is unlikely to be clinically significant. Regarding program website engagement, participants with early dropout had significantly fewer logins compared with those who did not drop out early. Those who experienced weight‐loss failure were significantly more likely to drop out early, and similarly, participants with early dropout had less weight loss at months 1 and 3. These results address an important evidence gap, as there have been few studies specifically examining factors that influence dropout in commercial weight‐loss programs.
Several individual‐level factors were significantly associated with early dropout. Similar to previous findings among clinical trials 2, this study confirms that participants in commercial programs who drop out early were more likely to be younger. A prior study of another online commercial program found that increasing age decreased risk of non‐usage attrition at 12 weeks 18, which also supports the idea that younger participants are more likely to drop out or disengage. Importantly, this study found that individuals with a greater number of chronic conditions were more likely to drop out early, and this finding held true for nearly every chronic condition evaluated. The only two conditions that did not meet the criteria for statistical significance were the presence of osteoarthritis and asthma. Most prior studies assessing comorbidities and dropout focus only on a single disease, such as type 2 diabetes, osteoarthritis or cardiovascular disease, rather than total burden of chronic conditions. Previous literature has been inconsistent regarding chronic conditions individually among clinical trial participants, and similarly, results have been mixed regarding the association between disease burden and attrition with in‐person weight‐loss interventions 2. Participants with a greater number of chronic conditions may struggle prioritizing the demands of their condition(s) with those of the weight‐loss program and might also require healthcare provider intervention (e.g. medication dose adjustment with weight loss or expertise around health condition). Future studies should investigate strategies that might reduce dropout particularly among participants with chronic conditions – potential approaches that could be employed might include increased coaching support, specially trained coaches to work with these patients or specific tailoring of call content and website content that addresses health needs related to their conditions.
Regarding program website engagement, individuals who dropped out early had significantly fewer website logins during the first 3 months and more often did not meet the target number of logins in this period. These results are generally consistent with previous literature among in‐person weight‐loss interventions, which has linked program attendance with dropout in clinical trials 2. A prior systematic review of web‐based weight management interventions identified only one study that explored the association between online logins and attrition 5. This study found a significant association between lower initial number of website logins and dropout by 12 months 21. An RCT of My Fitness Pal showed that app use declined over time – 97% of participants logged in during the first month, while only 35% logged in during month 6 14. While the reasons for the low login rates across studies are unknown, these differences could hypothetically occur by educational level or computer skill level. Unfortunately, these attributes are not available in the data for this study, and therefore, future studies should consider exploring how these factors may influence program engagement and early dropout. In addition, these participants may have never fully engaged in the program for some reason regardless of ability – e.g. a low login frequency might be a hallmark that an individual is not motivated or ready to commit to the behavioural changes needed to lose weight 22. Exploring reasons why individuals might not engage should also be explored, as factors such as readiness, motivation, time constraints or dissatisfaction with the coach/website could also contribute. In the study of My Fitness Pal, interviews and surveys with participants revealed that they stopped using the app because they found it to be tedious, difficult to use or they were too stressed/busy 14. Future studies should consider establishing a strategy, a priori, to conduct similar qualitative and/or quantitative investigations with dropouts and non‐users to better understand why they did not continue to engage. Regardless of the reason, given the striking difference between groups in logins during the first month, commercial programs that utilize a web‐based component could consider also tracking logins during this period as a marker of ‘high risk’ for early dropout. This marker could then be a target for coaching strategies that promote continued participation in the program, such as increased frequency of shorter calls, calls outside regular business hours and on weekends or a simplified website interface.
Considering weight loss factors, this study found that early dropout was associated with worse weight‐loss outcomes. These findings are consistent with previous research among clinical trial participants – lower early weight loss has been associated with dropout 2. This study is the first analysis that assesses the relationship between weight‐loss factors and dropout in a remotely delivered commercial program. The concept of ‘weight‐loss failure’, defined as weight change ≥0% at the end of the first month, could also be a marker, which commercial programs could monitor and then target for intervention. Strategies to address weight‐loss failure in the commercial setting might include specially trained coaches who are highly skilled in motivational interviewing to work with these patients to resolve ambivalence and elicit the behaviour changes needed to lose weight; however, such approaches need to be designed and rigorously tested to ensure that they are effective.
The 2013 adult weight management guidelines from the American Heart Association/American College of Cardiology/The Obesity Society suggest that clinicians consider referring patients to commercial weight‐loss programs with demonstrated weight loss efficacy 12. A recent systematic review has identified the few commercial programs that have this evidence 13, which may aid clinicians in counselling patients regarding which of these programs to consider. The results of this current study complement the prior review by providing clinicians an understanding of factors associated with early dropout from a commercial program. When clinicians refer to a commercial program, this study's results may aid in identifying their patients at high risk for dropout – younger and greater number of chronic conditions. Clinicians might consider close follow‐up with these patients to monitor for program disengagement and then help promote retention by addressing barriers or challenges facing the patient. Patients with multiple chronic conditions may require particular attention from the clinician when participating in these programs as they may struggle prioritizing the demands of their condition(s) with those of the weight‐loss program, require medication dose adjustment with weight loss or need expertise regarding their health condition. Clinicians will likely need to help these patients balance the demands of chronic disease self‐management with activities of the commercial program.
The concept of ‘dropout’ lacks a standard definition in the scientific literature 6. A range of terms have been used to refer to dropout or related concepts (e.g. attrition, withdrawal, non‐completers, interrupted treatment, non‐adherence and non‐compliance) 2, 6, 23. In general, the concept has been studied for over half a century in various settings including inpatient, addiction treatment and pharmacotherapy studies 24, 25. Research has also focused on dropout in weight‐loss studies 2, 5, 8, 9, 15, 16, 17, 18, and the term ‘early dropout’ in weight‐loss studies has ranged between 1 and 4 months 26, 27, 28. In this study, ‘early dropout’ was defined as participants who disengaged from the telephone coaching program by the end of month 2 (~8 weeks), which was selected given the potential to identify markers that suggest a high risk of dropout early in a participants' experience. Theoretically, these markers may be more useful for interventions that aim to improve retention and result in greater weight losses and improvements in comorbidities.
This study has several limitations. First, the study relies upon self‐reported data, which is subject to bias. For example, self‐reported weight is often under‐reported, especially in overweight women, which comprise a majority of the study population 29. Another study found that underestimation of web‐based self‐reported weight increased over time and was associated with less weight loss among individuals 30. Second, while this study was able to investigate individual‐level and program website engagement factors in relation to early dropout, previous research has demonstrated relationships between several variables that are unavailable in the data such as greater body dissatisfaction, greater number of past dieting attempts, lower physical activity levels, poorer mental health, lower self‐efficacy and less social support 2. The data did not include participant education or race, which have also been differentially associated with dropout 2, nor did the data include individual‐level behavioural factors (e.g. emotional eating and skipping meals) that have been associated with increased the risk of non‐usage attrition in an online commercial weight‐loss program 18. Finally, the findings of this study may not be generalizable to all commercial weight‐loss programs, as there may be differences between employer‐based and traditional commercial weight‐loss programs, as organizations/employers may offset some or all of the costs of the program to their employees. This study also did not examine whether any attributes of the employer/organization influenced dropout such as employment sector (e.g. manufacturing, health care and business).
In conclusion, several factors significantly associated with early dropout in an employer‐based commercial weight‐loss program, including younger age, greater number of chronic conditions, fewer website logins and weight‐loss failure. Future research is needed to confirm the association of these factors with early dropout in other commercial programs, as well as to design and test strategies that promote retention among participants at high risk for early dropout. Possible strategies to promote retention should address the challenges related to the identified risk factors. For example, increased support or tailoring to address the health needs might be appropriate to improve retention among individuals with chronic conditions. Individuals with low website logins may not be ready to commit to the behavioural changes needed to lose weight; therefore, programs might consider specially training coaches who are highly skilled in motivational interviewing to work with these patients to resolve ambivalence and elicit the behaviour changes needed to lose weight. Ultimately, understanding the factors associated with early dropout might be used to tailor programs to encourage retention and weight loss success.
Funding
The analyses presented in this manuscript were funded as part of an agreement between Johns Hopkins University and Sharecare, Inc to critically evaluate their employer‐based commercial weight‐loss program, Innergy®. A report of the results was provided to Sharecare, Inc for their internal use. Sharecare, Inc did not have a direct role in study design, data management, analysis or manuscript drafting. They had the opportunity to view the manuscript in advance of submission for review and comment to determine whether any confidential information was included and, if identified, removed.
Conflict of Interest Statement
Sharecare, Inc has commercialized a weight‐loss program called Innergy®, which it purchased from Healthways. Under an agreement with Sharecare, Inc, Johns Hopkins faculty monitor the Innergy® program's content and process (staffing, training and counselling) and outcomes (engagement and weight loss) to ensure consistency with the corresponding arm of the POWER Trial 19. Johns Hopkins receives fees for these services, and faculty members who participate in the consulting services receive a portion of these fees. Johns Hopkins receives royalty on sales of the Innergy program. The authors have no other potential conflict of interest relevant to this article to report. The authors wish to acknowledge and thank the members of the external oversight board.
Supporting information
Figure S1 . Selection of Study Sample. Figure displays process for selection of participants included in the analytic sample.
Alexander, E. , Tseng, E. , Durkin, N. , Jerome, G. J. , Dalcin, A. , Appel, L. J. , Clark, J. M. , and Gudzune, K. A. (2018) Factors associated with early dropout in an employer‐based commercial weight‐loss program. Obesity Science & Practice, 4: 545–553. 10.1002/osp4.304.
References
- 1. The Diabetes Prevention Program Research . Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obesity Research 2004; 12: 1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moroshko I, Brennan L, O'Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obesity Reviews 2011; 12: 912–934. [DOI] [PubMed] [Google Scholar]
- 3. Honas JJ, Early JL, Frederickson DD, O'Brien MS. Predictors of attrition in a large clinic‐based weight‐loss program. Obesity Research 2003; 11: 888–894. [DOI] [PubMed] [Google Scholar]
- 4. Fontaine KR, Cheskin LJ. Self‐efficacy, attendance, and weight loss in obesity treatment. Addictive Behaviors 1997; 22: 567–570. [DOI] [PubMed] [Google Scholar]
- 5. Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web‐based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta‐analysis. Obesity Reviews 2010; 11: 306–321. [DOI] [PubMed] [Google Scholar]
- 6. Miller BM, Brennan L. Measuring and reporting attrition from obesity treatment programs: a call to action! Obesity Research & Clinical Practice 2015; 9: 187–202. [DOI] [PubMed] [Google Scholar]
- 7. Leung AWY, Chan RSM, Sea MMM, Woo J. An overview of factors associated with adherence to lifestyle modification programs for weight management in adults. International Journal of Environmental Research and Public Health 2017; 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Spring B, Sohn MW, Locatelli SM, Hadi S, Kahwati L, Weaver FM. Individual, facility, and program factors affecting retention in a national weight management program. BMC Public Health 2014; 14: 363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jiandani D, Wharton S, Rotondi MA, Ardern CI, Kuk JL. Predictors of early attrition and successful weight loss in patients attending an obesity management program. BMC Obesity 2016; 3: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Levy AS, Heaton AW. Weight control practices of U.S. adults trying to lose weight. Annals of Internal Medicine 1993; 119: 661–666. [DOI] [PubMed] [Google Scholar]
- 11. Kruger J, Galuska DA, Serdula MK, Jones DA. Attempting to lose weight: specific practices among U.S. adults. American Journal of Preventive Medicine 2004; 26: 402–406. [DOI] [PubMed] [Google Scholar]
- 12. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology 2014; 63: 2985–3023. [DOI] [PubMed] [Google Scholar]
- 13. Gudzune KA, Roshi RS, Mehta AK, et al. Efficacy of commercial weight‐loss programs: an updated systematic review. Annals of Internal Medicine 2015; 162: 501–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Laing BY, Mangione CM, Tseng CH, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: a randomized, controlled trial. Annals of Internal Medicine 2014; 161: S5–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Finley CE, Barlow CE, Greenway FL, Rock CL, Rolls BJ, Blair SN. Retention rates and weight loss in a commercial weight loss program. International Journal of Obesity 2006; 31: 292–298. [DOI] [PubMed] [Google Scholar]
- 16. Volkmar FR, Stunkard AJ, Woolston J, Bailey RA. High attrition rates in commercial weight reduction programs. Archives of Internal Medicine 1981; 141: 426–428. [PubMed] [Google Scholar]
- 17. Mitchell C, Stuart RB. Effect of self‐efficacy on dropout from obesity treatment. Journal of Consulting and Clinical Psychology 1984; 52: 1100–1101. [DOI] [PubMed] [Google Scholar]
- 18. Neve MJ, Collins CE, Morgan PJ. Dropout, nonusage attrition, and pretreatment predictors of nonusage attrition in a commercial web‐based weight loss program. Journal of Medical Internet Research 2010; 12: e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight‐loss interventions in clinical practice. The New England Journal of Medicine 2011; 365: 1959–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. The New England Journal of Medicine 1997; 336: 1117–1124. [DOI] [PubMed] [Google Scholar]
- 21. Tate DF, Jackvony EH, Wing RR. Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. Journal of the American Medical Association 2003; 289: 1833–1836. [DOI] [PubMed] [Google Scholar]
- 22. Tsai AG, Fabricatore AN, Wadden TA, et al. Readiness redefined: a behavioral task during screening predicted 1‐year weight loss in the Look AHEAD study. Obesity (Silver Spring) 2014; 22: 1016–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Grave RD, Suppini A, Calugi S, Marchesini G. Factors associated with attrition in weight loss programs. International Journal of Behavioral Consultation and Therapy 2006; 2: 341–353. [Google Scholar]
- 24. Brandt LW. Studies of “dropout” patients in psychotherapy: a review of findings. Psychotherapy: Theory, Research & Practice. 1965; 2: 6–12. [Google Scholar]
- 25. Baekeland F, Lundwall L. Dropping out of treatment: a critical review. Psychological Bulletin 1975; 82: 738–783. [DOI] [PubMed] [Google Scholar]
- 26. Pekarik G, Blodgett C, Evans RG, Wierzbicki M. Variables related to continuance in a behavioral weight loss program. Addictive Behaviors 1984; 9: 413–416. [DOI] [PubMed] [Google Scholar]
- 27. Bennett GA, Jones SE. Dropping out of treatment for obesity. Journal of Psychosomatic Research 1986; 30: 567–573. [DOI] [PubMed] [Google Scholar]
- 28. Michelini I, Falchi AG, Muggia C, et al. Early dropout predictive factors in obesity treatment. Nutrition Research and Practice 2014; 8: 94–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rowland ML. Self‐reported weight and height. The American Journal of Clinical Nutrition 1990; 52: 1125–1133. [DOI] [PubMed] [Google Scholar]
- 30. Jerome GJ, Dalcin A, Coughlin JW, et al. Longitudinal accuracy of web‐based self‐reported weights: results from the Hopkins POWER trial. Journal of Medical Internet Research 2014; 16: e173. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 . Selection of Study Sample. Figure displays process for selection of participants included in the analytic sample.


