Abstract
Background
The development of molecular techniques to estimate the risk of breast cancer recurrence has been a significant addition to the suite of tools available to pathologists and breast oncologists. It has previously been shown that immunohistochemistry can provide a surrogate measure of tumor recurrence risk, effectively providing a less expensive and more rapid estimate of risk without the need for send-out. However, concordance between gene expression-based and immunohistochemistry-based approaches has been modest, making it difficult to determine when one approach can serve as an adequate substitute for the other. We investigated whether immunohistochemistry-based methods can be augmented to provide a useful therapeutic indicator of risk.
Methods
We studied whether the Oncotype DX breast cancer recurrence score can be predicted from routinely acquired immunohistochemistry of breast tumor histology. We examined the effects of two modifications to conventional scoring measures based on ER, PR, Ki-67, and Her2 expression. First, we tested a mathematical transformation that produces a more diagnostic-relevant representation of the staining attributes of these markers. Second, we considered the expression of BCL-2, a complex involved in regulating apoptosis, as an additional prognostic marker.
Results
We found that the mathematical transformation improved concordance rates over the conventional scoring model. By establishing a measure of prediction certainty, we discovered that the difference in concordance between methods was even greater among the most certain cases in the sample, demonstrating the utility of an accompanying measure of prediction certainty. Including BCL-2 expression in the scoring model increased the number of breast cancer cases in the cohort that were considered high certainty, effectively expanding the applicability of this technique to a greater proportion of patients.
Conclusions
Our results demonstrate an improvement in concordance between immunohistochemistry-based and gene expression-based methods to predict breast cancer recurrence risk following two simple modifications to the conventional scoring model.
Keywords: Digital pathology, Prognostic markers, Computer-assisted diagnosis, Staining
Background
A number of prognostic factors have been described with a significant relationship to likelihood of breast cancer recurrence, and commonly include patient age [1, 2], tumor size [3], lymph node status [4], and histologic grade [5], but also include biomarkers as assessed by immunohistochemistry (IHC) including Her2 status [6], patterns of hormone receptor expression (ER and PR) [7, 8], and expression of proliferative marker Ki-67 [9, 10]. Gene expression analysis has also been used to successfully predict recurrence likelihood [11], with one such test (Oncotype DX, Genomic Health, Redwood City, CA) having been added to NCCN guidelines for treatment [12]. This test provides a recurrence score (RS) which estimates the likelihood of recurrence according to a 21-gene assay. Importantly, RS has also been shown to successfully predict chemotherapy benefit [13], and has extensively been shown to alter treatment recommendations when considered alongside other diagnostic factors [14–20].
Despite the clear clinical utility of this approach, it remains costly and inaccessible to many patients, leading several groups to evaluate alternative methods as a surrogate for the Oncotype DX test. Turner, et al. suggested that limiting the use of the test based on routine histologic examination could reduce send out by up to 23%, resulting in significant cost savings [21]. More recently, Gage, et al. argued that a 44% reduction in send out could be achieved based on traditional variables used in sign out [22]. In addition to economic considerations, another focus has been to provide accurate predictions from immediately available data. Flanagan, et al. described one of the most compelling methods, using histologic factors combined with routinely acquired protein expression data from IHC to predict RS [23]. This approach provided an estimate of recurrence likelihood using data immediately available following routine processing of the tissue. In a subsequent study, this group offered three modifications to the original formulation with similar predictive success [24]; one such modification, the Magee Score #3, generated a prediction of RS strictly from ER, PR, Ki-67, and Her2 status. An advantage to this modification is that it is entirely quantitative and reproducible, and does not depend on pathologist grading or interpretation which has been shown to exhibit considerable inter-observer variability [25]. Furthermore, with the advent of whole-slide imaging and its association with modern informatics approaches, a score based entirely on image analysis of IHC has the potential to be generated in a completely automated fashion.
Although the Magee Score #3 is an attractive alternative to the Oncotype DX test, it achieved only 54.4% overall concordance in their study. Improved concordance between this IHC-based approach and RS is needed to inspire confidence in the performance of this technique. We explored whether two modifications to this approach could be used to improve concordance and produce a viable IHC-based algorithm with clinical potential. First, we examined the impact on concordance by applying a diagnostically-relevant data transformation. Second, we explored whether the expression of BCL-2 as part of a complete breast panel can improve the estimation of RS. BCL-2 expression has previously been shown to be associated with a decreased risk of recurrence [26, 27] and a higher relapse-free survival rate [28–32]. We hypothesized that the prognostic information provided by BCL-2 accompanied by an optimized mathematical treatment of these variables can be harnessed to improve RS estimation.
Methods
Case selection
One hundred and fifty-eight breast cancer cases between 2010 and 2017 were identified retrospectively from the Drexel University College of Medicine breast cancer databank that met the following criteria:
a diagnosis of primary invasive breast carcinoma was rendered on the original pathology report;
Oncotype DX recurrence scores were available in the original pathology report;
a breast panel that included expression of ER, PR, Ki-67, Her2, and BCL-2, had been performed on the same block using IHC;
slides were scanned using whole-slide imaging and staining was assessed quantitatively using computational image analysis;
ER percent positive staining was at least 1%;
Her2 was considered negative or equivocal by image analysis and confirmed manually.
Case data were obtained by an honest broker and delivered to the investigators in a deidentified fashion. This study was considered exempt by the Drexel University College of Medicine Institutional Review Board under Category 4.
Histologic processing
All breast specimens had ischemic and fixation times within CAP/ASCO guidelines. Biopsy cases were processed in a standard fashion after fixation in neutral buffered formalin. Lumpectomy specimens were entirely submitted after fixation in neutral buffered formalin and inking all surfaces to maintain orientation. A specimen map was used as a worksheet to document lesional tissue and distance to margins. After review of all carcinoma slides, the most representative slide was used to perform the invasive breast panel consisting of ER, PR, Ki-67, Her2, and BCL-2. Immunohistochemical stains for ER (SP1, RM, Ventana, Benchmark Ultra), PR (1E2, RM, Ventana, Benchmark Ultra), Ki-67 (30–9, RM, Ventana, Benchmark Ultra), Her2 (4B5, RM, Ventana, Benchmark Ultra), and BCL-2 (124, MM, Ventana, Benchmark Ultra) antibodies were performed on formalin-fixed paraffin-embedded sections. The antibody conditions for ER, PR, Ki-67, Her2, and BCL-2 were as follows: 8.1 pH antigen retrieval using CC1 reagent for 36–64 min, followed by primary antibody incubation for 16–44 min, and then staining with the Ultra Ultraview Universal DAB Detection Kit.
Image analysis
High resolution whole-slide images were acquired at either 20x or 40x magnification using the Aperio Scanscope XT (Leica Microsystems, Wetzlar, Germany). Eight regions of interest were manually selected by a pathologist for scoring, and the average score was derived using one of three semi-automated algorithms provided by the Aperio software. The nuclear staining algorithm was applied to ER, PR, and Ki-67 slides and was used to compute the percentage of positively stained cells, as well as an H-score indicating staining intensity, consistent with CAP/ASCO guidelines [33]. The membrane algorithm was applied to Her2 slides and generated a Her2 score consistent with CAP/ASCO guidelines [34]. The cytoplasmic algorithm was applied to BCL-2 slides and produced an H-score based on cytoplasmic staining intensity. Importantly, these scores were obtained at the time of diagnosis and were not influenced by the purposes of this study. Original Her2 scores that were reported using previous CAP/ASCO guidelines [35] were recomputed to meet current standards, but this did not require the image analysis portion to be modified.
Regression model
We performed linear regression to derive a set of coefficients (and a constant term) that, in combination with selected IHC data, could be used to predict RS. To compute concordance, we embedded this model within a 10-fold cross-validation framework to ensure that the test sample was not used to generate the coefficients. To further ensure that the model was not susceptible to overfitting, we repeated the cross-validation 10,000 times, randomly selecting training and test data groups (folds) at each iteration. The results that we report are accompanied by a standard deviation which represents the iteration-to-iteration variability of the value under test. Generally, we observed only a small difference in the model’s coefficients between iterations.
Logistic transformation
Using Eq. 1, we applied a logistic transformation to the percent positive nuclear staining metric, x, to generate a diagnostically-relevant score, y, between zero and one:
| 1 |
The value, k, was selected so that y is approximately half its maximum at the diagnostic threshold, Tx (Eq. 2).
| 2 |
This relationship holds true only for small values of Tx (i.e. when e-k approaches zero). For example, when Tx is 0.14, y is equal to 0.500 when x is 0.14 and 0.999 when x is 1. We selected values of Tx based on previous reports of diagnostic criteria that were successful in stratifying patients using ER [36], PR [37], and Ki-67 [9, 10, 38] (10, 10, and 14%, respectively).
Analysis of concordance
We measured concordance between the IHC-based score we generated and RS by comparing the categorical interpretations of both scores. We judged the certainty, η, of the categorical prediction by measuring the difference between the score and its closest categorical threshold (Eq. 3).
| 3 |
We used a threshold of 18 to distinguish the low from intermediate group and a threshold of 31 to distinguish the intermediate from high group, consistent with thresholds established for the Oncotype DX test [11].
Relationship between H-score and percent positive cells
We used H-score to describe the staining attributes of ER and PR in a subset of analyses. We observed that H-score, in contrast to the logistic score described above, maintained a linear relationship with the percent positive metric. To demonstrate the relationship between H-score and the percent positive metric, we performed simulations by randomly assigning a staining intensity of 0, 1+, 2+, or 3+ to a set of 104 model cells. We measured the H-score and computed the corresponding percent positive staining for the model cells, repeating this process 105 times.
Results
The conventional scoring model is highly reproducible
We performed a retrospective analysis of 158 cases (103 resections, 55 core needle biopsies) of invasive breast carcinoma. As shown in Table 1, relative proportions of histologic grade in this sample were consistent with previous reports [39, 40]. Furthermore, the relative proportions of histologic grade were roughly equivalent across both biopsies and resections, confirming that a bias did not exist as a function of sampling procedure. Cases with histologic grade of 3 also had higher Oncotype DX recurrence scores (RS) than cases with a grade of 2 (p < < 0.01, Mann-Whitney U test), as demonstrated previously [41–45]. The proportions of PR-positive and Ki-67-positive cases present in this ER-positive and Her2-negative/equivocal sample were also found to be within an expected range [46, 47] (Table 2).
Table 1.
Case details by histologic grade
| Histologic grade | ||||
|---|---|---|---|---|
| Total | I | II | III | |
| Number of cases | 158 | 34 | 86 | 38 |
| Resection | 103 | 20 | 58 | 25 |
| Biopsy | 55 | 14 | 28 | 13 |
| Median patient age | 57 ± 8 | 57.5 ± 6 | 56.5 ± 7 | 56.5 ± 9 |
| Tumor size (cm) | 1.6 ± 0.6 | 1.5 ± 0.7 | 1.6 ± 0.7 | 1.5 ± 0.4 |
| Oncotype DX RS | 15 ± 4.5 | 14 ± 3 | 14 ± 4 | 23.5 ± 6.5 |
The number of cases in our cohort are divided by histologic grade and presented according to relevant clinicopathological variables, including RS. Ranges represent quartiles
Table 2.
Immunohistochemistry attributes of the data set
| Negative or Not overexpressed | Low positive or Equivocal | Positive or Overexpressed | |
|---|---|---|---|
| ER | 0 (0.0%) | 2 (1.3%) | 156 (98.7%) |
| PR | 14 (8.9%) | 12 (7.6%) | 132 (83.5%) |
| Ki-67 | 34 (21.5%) | 46 (29.1%) | 78 (49.4%) |
| Her2 | 134 (84.8%) | 24 (15.2%) | 0 (0%) |
The relative proportions of ER, PR, Ki-67, and Her2 categories are shown as the number (and corresponding percentage) of cases
We developed an equation using linear regression to predict breast cancer recurrence by estimating RS from ER, PR, Ki-67, and Her2 expression determined using IHC. We categorized IHC scores using a threshold of 18 to distinguish between “low” and “intermediate” risk of recurrence and 31 to distinguish between “intermediate” and “high” risk of recurrence, the same thresholds used for RS categorization [13]. We measured the concordance between RS and the categorical predictions of IHC using the H-scores of ER and PR, the percent positive staining for Ki-67, and Her2 category (overexpressed, not overexpressed, equivocal), following previous methods [23, 24, 48, 49]. We found that IHC and RS shared the same category in 63.4% of cases. In comparison, we used the coefficients from the Magee Score #3 [24] which was based on the same variables, and found similar overall performance to our eq. (59.5%), a rate that exceeded the performance reported by the authors when applied to their cohort of 248 cases (54.4%). We also compared the coefficients of both equations and found that they were similar (Table 3, first and second columns) except that Her2 status was more strongly weighted in the equation derived from our cohort, likely due to the difference in the Her2 scoring standard applied. Nevertheless, these results demonstrate a high degree of reproducibility of the conventional scoring model on the data set presented here and confirm its ability to predict RS.
Table 3.
Contribution to IHC score
| Conventional model | Revised model | |||
|---|---|---|---|---|
| Magee Score #3 coefficients | Linear regression coefficients | Linear regression coefficients | Standardized weight | |
| ER | −0.022 | −0.025 | −26.75 | 2.28 |
| PR | −0.029 | −0.040 | −10.83 | 3.59 |
| Ki-67 | 0.186 | 0.196 | 11.64 | 3.15 |
| Her2 | 1.47a | 7.97a | 9.14 | 2.06 |
| BCL-2 | – | – | −7.39 | 2.17 |
a Her2 score was defined differently in our calculation of Her2 score, reflecting the change in Her2 recommendations from Hammond, et al., 2013
The relative contributions of each marker to the IHC-based scores are presented using metrics that examine the weighting of each quantity in the equations. The conventional model refers to the model based on the technique described in Klein, et al. using ER and PR H-score, Ki-67% positive cells, and Her2 score. The conventional model uses a variable weight based on the categorical interpretation of Her2; for clarity, only the coefficient that is applied to a Her2 score of 2 is shown. The equation’s coefficients derived from the Klein data set are shown in the first column and the coefficients that we derived from our cohort are shown in the second column. Notably, BCL-2 is excluded from this analysis because it was not a variable included in the authors’ formulation of the equation. The coefficients from the revised model, which includes BCL-2 as a prognostic variable, ER/PR percent positive cells as a replacement for H-score, and follows the logistic transformation applied to ER, PR, and Ki-67, and a linear treatment of the Her2 score, are shown in the third column. The standardized weights of the markers, defined as the product of the coefficients and the standard deviations of the values in our cohort, are shown in the fourth column
Transformation of staining attributes improve concordance
CAP/ASCO guidelines specify that ER and PR expression as determined by IHC should be reported according to the percentage of positively stained cells to guide diagnostic interpretation and treatment decision making [33]. Likewise, Her2 expression is reported according to a score which measures the relative proportions of 3+, 2+, 1+, and unstained cells based on membrane staining intensity [34]. Treatment decision making critically relies on the categorical interpretation of these quantities [50–55], but it is difficult to reconcile the clinical utility of categorical data with the linear treatment of a continuous variable. For instance, a tumor is considered to exhibit ER immunoreactivity if the percentage of positively stained cells exceeds 1% [33]. This implies that the binary categorization of this quantity into “positive” and “negative”, which has a profound effect on its diagnostic and therapeutic interpretation, largely ignores differences in expression levels over the vast majority of its range. Therefore, using a continuous scalar quantity such as percent positive cells or H-score to characterize ER expression is not consistent with the diagnostic interpretation of ER.
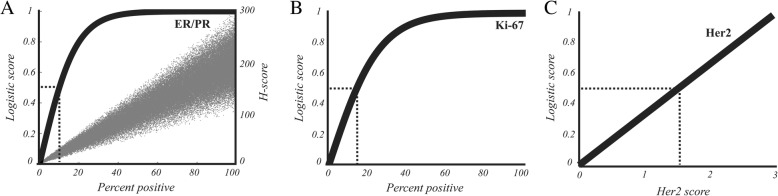
We developed a scoring model in which we applied a logistic transformation to the percent positive metric to produce a value that is consistent with the diagnostic interpretation of ER, PR, and Ki-67. This transformation produced a diagnostically-relevant score whose relationship to percent positivity is shown in Fig. 1, in contrast with the H-score (Fig. 1a, gray points) which maintained a linear relationship with percent positivity. Likewise, we removed the tripartite categorization of Her2 score to better reflect the prognostic interpretation of Her2 status, given that Her2 scores of 1 have been shown to predict a significantly higher incidence of recurrence than scores of 0 [56] despite both being assigned to the same “not overexpressed” category that is largely used to determine eligibility for Her2-specific treatment. After applying these transformations, we again computed predictive scores using cross-validation. We found that 64.6% of cases were assigned by IHC to the same category as the corresponding RS, a modest improvement over the 63.6% concordance rate achieved by not using logistic transformation.
Fig. 1.
Transformation of staining attributes. a The ER and PR percent positive cells metric was transformed to a diagnostic score using logistic transformation. As indicated by the dotted lines, the curve is half maximum at the diagnostic cut-off of 10%, producing a score of 0.5. Gray points indicate the relationship between H-score and percent positive cells using simulations. b The logistic transformation is applied to the Ki-67% positive cells metric using a diagnostic cut-off of 14% to produce a diagnostic score. c Her2 score is transformed to a diagnostic score by dividing its value by 3, maintaining a linear relationship
BCL-2 improves classification performance
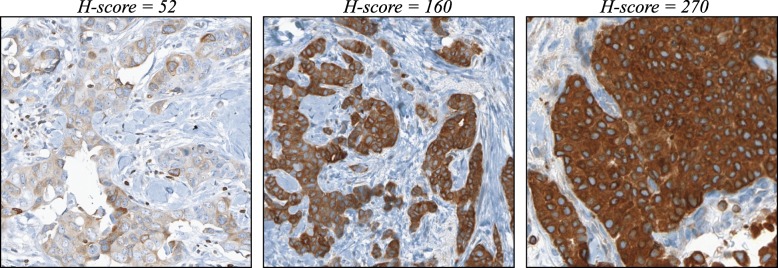
Low BCL-2 expression in breast cancer has been associated with increased likelihood of recurrence [26, 27] and generally carries a less favorable prognosis [28–32]. We augmented the IHC-based methods by adding BCL-2 expression as an additional prognostic variable. Since there is not an established threshold for stratifying recurrence risk for BCL-2, we elected to use the H-score to quantify BCL-2 staining (Fig. 2) instead of applying the logistic transform with an arbitrary threshold. In Fig. 3, the distribution of IHC-based scores using ER, PR, Ki-67, Her2, and BCL-2 is shown in relation to the corresponding RS. We again categorized IHC-based scores into “low”, “intermediate”, and “high” risk groups. Using these criteria, blue points represent scores that were classified by IHC as low risk; likewise, green points and red points represent scores in the intermediate and high risk categories, respectively. We found that the addition of BCL-2 further improved the concordance rate to 68.2% (Fig. 4, rightmost bar).
Fig. 2.
Representative examples of BCL-2 staining.We selected representative images from three cases that exhibited low (left panel), intermediate (center panel), and high (right panel) intensity staining for BCL-2. The corresponding H-scores are shown
Fig. 3.
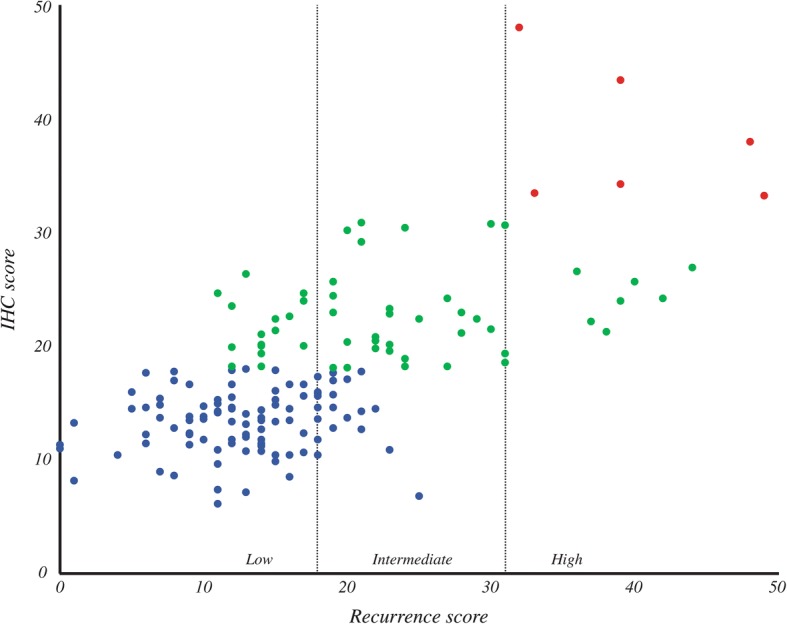
Estimation of RS from IHC. The RS for each sample is represented on the x-axis. The IHC scores generated by linear regression, following data transformation and the addition of BCL-2, are represented on the y-axis. Dotted lines represent the categorical boundaries that distinguish low, intermediate, and high risks of recurrence. The category to which each sample is assigned based on IHC score is indicated by color; blue = low, green = intermediate, red = high
Fig. 4.
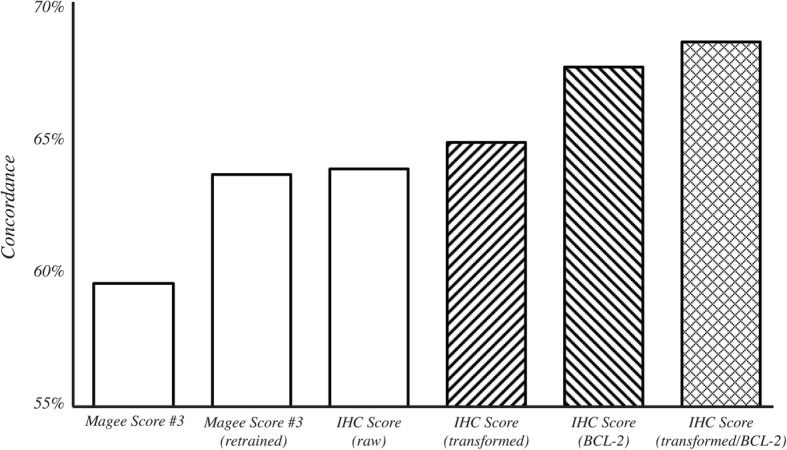
Concordance of IHC-based methods with RS. Concordance rates were computed on 158 cases using cross-validation for each of the following methods tested (starting with the left-most bar): Magee Score #3 with the coefficients and variables described in Klein, et al. [24]; Magee Score #3 with coefficients recomputed based on our cohort; IHC Score using ER, PR, and Ki-67% positive staining, and Her2 score; IHC Score using the logistic transformation applied to ER, PR, and Ki-67; IHC Score after inclusion of BCL-2 H-score; IHC Score using both the logistic transformation and the inclusion of BCL-2 H-score
To further demonstrate the impact of these modifications on concordance rate, we sorted the IHC score as a function of prediction certainty. We hypothesized that scores close to 18 or 31 have a higher likelihood of misclassification due to their proximity to the categorical boundaries. We developed a measure of certainty based on the difference between the score and its closest threshold. We found that the most certain predictions were indeed more likely to be concordant with RS. However, cases with IHC scores close to 18 were always either low or intermediate according to RS and cases with IHC scores close to 31 were always either intermediate or high. We did not observe any cases that were classified into the low category by IHC and the high category by RS, or vice versa. As shown in Fig. 5, the likelihood of concordant classification increased when only the most certain cases were considered, achieving a concordance of nearly 90% for the most certain 20% of the cohort.
Fig. 5.
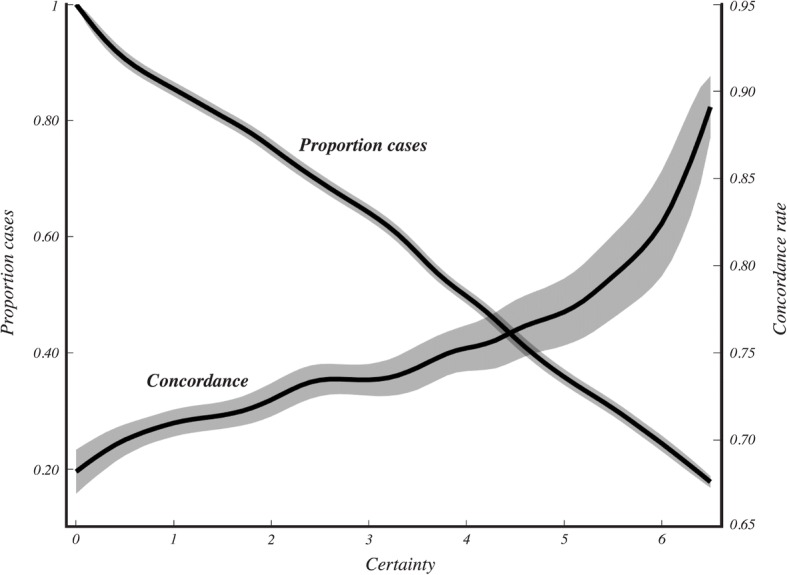
Cumulative concordance rate scales with certainty. Concordance rates were computed based only on the samples with certainty values greater than the value indicated on the x-axis. The proportion of cases used to compute the concordance value is shown on the y-axis to the left, where 1 indicates that all 158 samples were used. Standard deviation of the rates based on 10,000 iterations are represented by the shaded regions
Individual contribution of markers to the prediction of RS
We compared the independent contributions of each marker to the concordance rate of the algorithm. When markers were individually used to predict RS, we found that they were poor predictors alone. When we evaluated the performance of the algorithm when trained with only two markers at a time, we found that PR and BCL-2 together produced the highest number of high-certainty scores (> 3), achieving an overall concordance rate of 63.7%. We found that the most successful trio of markers was PR, BCL-2, and Ki-67, expanding the number of high-certainty predictions and achieving an overall concordance rate of 65.3%.
We developed an alternative measure of the individual contributions of each marker by examining the equation’s coefficients. We found that the standardized weights of the coefficients were similar to the rank order observed originally, except that Ki-67 had a much higher standardized weight than BCL-2 (Table 3, fourth column). The disparity between the results of the two methods indicates that BCL-2 and PR likely share a complementary role that is not revealed when all the markers are present.
IHC score to predict chemotherapy benefit
These results, taken together with those that have examined chemotherapy benefit as a function of RS [13, 16, 20, 57–59], suggest that patients with a sufficiently low IHC score are unlikely to benefit from chemotherapy. Recent evidence from the TAILORx trial suggests that a subset of patients with RS scores in the intermediate range are also unlikely to benefit from chemotherapy [60]. Figure 3 shows that of the 98 cases with IHC scores in the “low” group, only 21 (21.4%) equaled or exceeded an RS of 18 that would put them into the intermediate category. Furthermore, these 21 discordant cases had a mean RS of 19.6, suggesting that they predominantly resided on the low end of the intermediate range. Only 3 of the 98 cases classified by our technique as belonging to the “low” group had an RS greater than 21. Therefore, very few of the patients misclassified by the IHC score are likely to benefit from chemotherapy. We replotted the data in Fig. 3 and expressed the results in terms of estimated chemotherapy benefit (Fig. 6). The results support our contention that patients with tumors that were classified into the “low” category using IHC were unlikely to exhibit a chemotherapy benefit. Based on these results, we suggest that patients with an IHC score less than 18 do not benefit from additional molecular testing to confirm that they are unlikely to benefit from chemotherapy. In our cohort, this cutoff would reduce send-out by 62%.
Fig. 6.
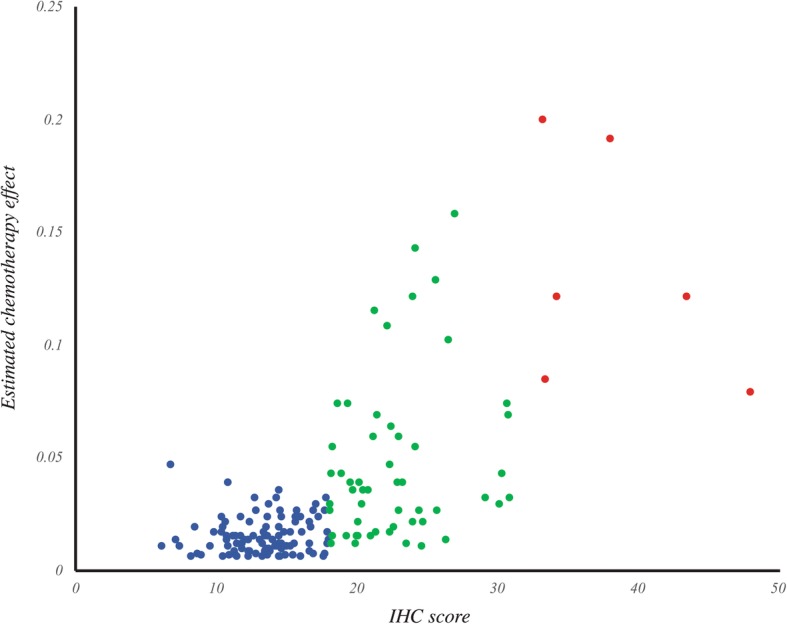
Prediction of chemotherapy effect from IHC. Chemotherapy effect was calculated from RS and plotted against IHC score for each case. Chemotherapy effect was estimated from the model presented by Paik, et al. [13] by subtracting the 10-year likelihood of recurrence at a given RS for patients treated with Tamoxifen + chemotherapy from those treated with Tamoxifen alone. The category to which each sample is assigned based on IHC score is indicated by color; blue = low, green = intermediate, red = high
Discussion
The results that we describe demonstrate a quantitative approach to estimating the likelihood of breast cancer recurrence from routinely acquired protein expression data. This technique offers the ability to immediately stratify patients following IHC processing of excised tissue. The IHC score is based strictly on the results of image analysis of tissue and does not require other information that may not be available at the time of biopsy, for example. It also does not necessarily require whole-slide imaging; it can be used with any semi-quantitative method for estimating staining and therefore is accessible to underprivileged areas, offering a key advantage over some molecular approaches. However, when combined with whole-slide imaging, it may offer the potential to be robust in the presence of tumor heterogeneity by enabling the analysis to be performed with spatial precision. This not only provides a check that can confirm the reliability of the molecular interpretation of the result, but can also help guide microdissection to improve sampling for molecular send out.
The two main innovations over existing IHC-based approaches are the addition of BCL-2 to the panel and a logistic transformation pre-processing step to transform conventionally reported values into a more diagnostically-relevant score. Together, these additions improved the concordance rate from 59.5% using the Magee Score #3 to 68.2%. Importantly, the results demonstrate that the logistic transformation step eliminates the need to use H-score to quantify ER and PR expression, which may not always be accessible. Furthermore, the IHC score can also be accompanied by a measure of certainty that describes the likelihood of the score belonging to a particular category. After converting a given score’s certainty value to a likelihood measure (Fig. 4), a sample reporting of the results may take the form:
IHC score: 11.6
A score of 11.6 indicates an 89% chance of belonging to the low recurrence likelihood group and an 11% chance of belonging to the intermediate recurrence likelihood group.
Refining the certainty and prediction accuracy measures on which these interpretations are based would be aided by testing this technique on additional data sets.
BCL-2 as a predictive marker
Our analysis of the individual contributions of each marker to the predictive success of the IHC score suggests that all the markers we used in this study provide unique information that aids in the prediction of RS. However, the results also indicate that only two markers (PR and BCL-2) are needed to provide approximately the same performance as conventional IHC measures for recurrence likelihood. This result illustrates the complementary contributions of PR and BCL-2 in predicting recurrence, and perhaps de-emphasizes the importance of ER, Ki-67, and Her2 in this role. Although ER, Ki-67, and Her2 are routinely analyzed in invasive breast cancer cases, the results also suggest that quantitative image analysis can likely be sequestered to just PR and BCL-2 slides in underprivileged areas for the purpose of predicting breast cancer recurrence.
Conclusions
We suggest that conventional methods for estimation of the Oncotype DX breast recurrence score can be augmented by the addition of BCL-2, by the mathematical transformation of ER, PR, and Ki-67, or by the combination of both approaches. The results indicate that this modification improves concordance between IHC- and gene-expression-based methods, and can be extended to predict chemotherapy effect.
Acknowledgements
We would like to thank Sharon Cavone for her histology expertise.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IHC
Immunohistochemistry
- RS
Recurrence score
Authors’ contributions
MZ made substantial contributions to conception and design; acquired, analyzed, and interpreted the data; and drafted the manuscript. RH made substantial contributions to conception and design; and contributed to the preparation of the manuscript. NP made substantial contributions to conception and design; and contributed to the preparation of the manuscript. FG made substantial contributions to conception and design; and contributed to the preparation of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethics approval and the consent to participate were considered exempt by the Institutional Review Board at Drexel University under category 4.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mark D. Zarella, Phone: (215) 762-8657, Email: mark.zarella@drexelmed.edu
Rebecca C. Heintzelman, Email: rebecca.heintzelman@ctca-hope.com
Nikolay K. Popnikolov, Email: nikolay.popnikolov@drexelmed.edu
Fernando U. Garcia, Email: fernando.garcia@ctca-hope.com
References
- 1.Liedtke C, Hess KR, Karn T, Rody A, Kiesel L, Hortobagyi GN, Pusztai L, Gonzalez-Angulo AM. The prognostic impact of age in patients with triple-negative breast cancer. Breast Cancer Res Treat. 2013;138(2):591–599. doi: 10.1007/s10549-013-2461-x. [DOI] [PubMed] [Google Scholar]
- 2.Nixon AJ, Neuberg D, Hayes DF, Gelman R, Connolly JL, Schnitt S, Abner A, Recht A, Vicini F, Harris JR. Relationship of patient age to pathologic features of the tumor and prognosis for patients with stage I or II breast cancer. J Clin Oncol. 1994;12(5):888–894. doi: 10.1200/JCO.1994.12.5.888. [DOI] [PubMed] [Google Scholar]
- 3.Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer. 1989;63(1):181–187. doi: 10.1002/1097-0142(19890101)63:1<181::aid-cncr2820630129>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 4.Cianfrocca M, Goldstein LJ. Prognostic and predictive factors in early-stage breast cancer. Oncologist. 2004;9(6):606–616. doi: 10.1634/theoncologist.9-6-606. [DOI] [PubMed] [Google Scholar]
- 5.Le Doussal V, Tubiana-Hulin M, Friedman S, Hacene K, Spyratos F, Brunet M. Prognostic value of histologic grade nuclear components of Scarff-Bloom-Richardson (SBR). An improved score modification based on a multivariate analysis of 1262 invasive ductal breast carcinomas. Cancer. 1989;64(9):1914–1921. doi: 10.1002/1097-0142(19891101)64:9<1914::aid-cncr2820640926>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 6.Gamucci T, Vaccaro A, Ciancola F, Pizzuti L, Sperduti I, Moscetti L, Longo F, Fabbri MA, Giampaolo MA, Mentuccia L, et al. Recurrence risk in small, node-negative, early breast cancer: a multicenter retrospective analysis. J Cancer Res Clin Oncol. 2013;139(5):853–860. doi: 10.1007/s00432-013-1388-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colleoni M, Sun Z, Price KN, Karlsson P, Forbes JF, Thurlimann B, Gianni L, Castiglione M, Gelber RD, Coates AS, et al. Annual Hazard rates of recurrence for breast Cancer during 24 years of follow-up: results from the international breast Cancer study group trials I to V. J Clin Oncol. 2016;34(9):927–935. doi: 10.1200/JCO.2015.62.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng L, Swartz MD, Zhao H, Kapadia AS, Lai D, Rowan PJ, Buchholz TA, Giordano SH. Hazard of recurrence among women after primary breast cancer treatment--a 10-year follow-up using data from SEER-Medicare. Cancer Epidemiol Biomark Prev. 2012;21(5):800–809. doi: 10.1158/1055-9965.EPI-11-1089. [DOI] [PubMed] [Google Scholar]
- 9.Criscitiello C, Disalvatore D, De Laurentiis M, Gelao L, Fumagalli L, Locatelli M, Bagnardi V, Rotmensz N, Esposito A, Minchella I, et al. High Ki-67 score is indicative of a greater benefit from adjuvant chemotherapy when added to endocrine therapy in luminal B HER2 negative and node-positive breast cancer. Breast. 2014;23(1):69–75. doi: 10.1016/j.breast.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 10.de Azambuja E, Cardoso F, de Castro G, Jr, Colozza M, Mano MS, Durbecq V, Sotiriou C, Larsimont D, Piccart-Gebhart MJ, Paesmans M. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer. 2007;96(10):1504–1513. doi: 10.1038/sj.bjc.6603756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351(27):2817–2826. doi: 10.1056/NEJMoa041588. [DOI] [PubMed] [Google Scholar]
- 12.Trosman JR, Van Bebber SL, Phillips KA. Coverage policy development for personalized medicine: private payer perspectives on developing policy for the 21-gene assay. J Oncol Pract. 2010;6(5):238–242. doi: 10.1200/JOP.000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, Cronin M, Baehner FL, Watson D, Bryant J, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726–3734. doi: 10.1200/JCO.2005.04.7985. [DOI] [PubMed] [Google Scholar]
- 14.Fried G, Moskovitz M. Treatment decisions in estrogen receptor-positive early breast cancer patients with intermediate oncotype DX recurrence score results. Springerplus. 2014;3:71. doi: 10.1186/2193-1801-3-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joh JE, Esposito NN, Kiluk JV, Laronga C, Lee MC, Loftus L, Soliman H, Boughey JC, Reynolds C, Lawton TJ, et al. The effect of Oncotype DX recurrence score on treatment recommendations for patients with estrogen receptor-positive early stage breast cancer and correlation with estimation of recurrence risk by breast cancer specialists. Oncologist. 2011;16(11):1520–1526. doi: 10.1634/theoncologist.2011-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loncaster J, Armstrong A, Howell S, Wilson G, Welch R, Chittalia A, Valentine WJ, Bundred NJ. Impact of Oncotype DX breast recurrence score testing on adjuvant chemotherapy use in early breast cancer: real world experience in greater Manchester, UK. Eur J Surg Oncol. 2017;43(5):931–7. [DOI] [PubMed]
- 17.Malo TL, Lipkus I, Wilson T, Han HS, Acs G, Vadaparampil ST. Treatment choices based on OncotypeDx in the breast oncology care setting. J Cancer Epidemiol. 2012;2012:941495. doi: 10.1155/2012/941495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen MT, Stessin A, Nagar H, D'Alfonso TM, Chen Z, Cigler T, Hayes MK, Shin SJ. Impact of oncotype DX recurrence score in the management of breast cancer cases. Clinical Breast Cancer. 2014;14(3):182–190. doi: 10.1016/j.clbc.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Ozmen V, Atasoy A, Gokmen E, Ozdogan M, Guler N, Uras C, Ok E, Demircan O, Isikkdogan A, Cabioglu N, et al. Correlations between Oncotype DX recurrence score and classic risk factors in early breast Cancer: results of a prospective multicenter study in Turkey. J Breast Health (2013) 2016;12(3):107–111. doi: 10.5152/tjbh.2016.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneider JG, Khalil DN. Why does Oncotype DX recurrence score reduce adjuvant chemotherapy use? Breast Cancer Res Treat. 2012;134(3):1125–1132. doi: 10.1007/s10549-012-2134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner BM, Skinner KA, Tang P, Jackson MC, Soukiazian N, Shayne M, Huston A, Ling M, Hicks DG. Use of modified Magee equations and histologic criteria to predict the Oncotype DX recurrence score. Mod Pathol. 2015;28(7):921–931. doi: 10.1038/modpathol.2015.50. [DOI] [PubMed] [Google Scholar]
- 22.Gage MM, Mylander WC, Rosman M, Fujii T, Le Du F, Raghavendra A, Sinha AK, Espinosa Fernandez JR, James A, Ueno NT, et al. Combined pathologic-genomic algorithm for early-stage breast cancer improves cost-effective use of the 21-gene recurrence score assay. Ann Oncol. 2018;29(5):1280–1285. doi: 10.1093/annonc/mdy074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flanagan MB, Dabbs DJ, Brufsky AM, Beriwal S, Bhargava R. Histopathologic variables predict Oncotype DX recurrence score. Mod Pathol. 2008;21(10):1255–1261. doi: 10.1038/modpathol.2008.54. [DOI] [PubMed] [Google Scholar]
- 24.Klein ME, Dabbs DJ, Shuai Y, Brufsky AM, Jankowitz R, Puhalla SL, Bhargava R. Prediction of the Oncotype DX recurrence score: use of pathology-generated equations derived by linear regression analysis. Mod Pathol. 2013;26(5):658–664. doi: 10.1038/modpathol.2013.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dalton LW, Pinder SE, Elston CE, Ellis IO, Page DL, Dupont WD, Blamey RW. Histologic grading of breast cancer: linkage of patient outcome with level of pathologist agreement. Mod Pathol. 2000;13(7):730–735. doi: 10.1038/modpathol.3880126. [DOI] [PubMed] [Google Scholar]
- 26.Hurlimann J, Larrinaga B, Vala DL. Bcl-2 protein in invasive ductal breast carcinomas. Virchows Arch. 1995;426(2):163–168. doi: 10.1007/BF00192638. [DOI] [PubMed] [Google Scholar]
- 27.Yang Q, Moran MS, Haffty BG. Bcl-2 expression predicts local relapse for early-stage breast cancer receiving conserving surgery and radiotherapy. Breast Cancer Res Treat. 2009;115(2):343–348. doi: 10.1007/s10549-008-0068-4. [DOI] [PubMed] [Google Scholar]
- 28.Bilalovic N, Vranic S, Hasanagic S, Basic H, Tatarevic A, Beslija S, Selak I. The Bcl-2 protein: a prognostic indicator strongly related to ER and PR in breast cancer. Bosn J Basic Med Sci. 2004;4(4):5–12. doi: 10.17305/bjbms.2004.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lipponen P, Pietilainen T, Kosma VM, Aaltomaa S, Eskelinen M, Syrjanen K. Apoptosis suppressing protein bcl-2 is expressed in well-differentiated breast carcinomas with favourable prognosis. J Pathol. 1995;177(1):49–55. doi: 10.1002/path.1711770109. [DOI] [PubMed] [Google Scholar]
- 30.Kobayashi S, Iwase H, Ito Y, Yamashita H, Iwata H, Yamashita T, Ito K, Toyama T, Nakamura T, Masaoka A. Clinical significance of bcl-2 gene expression in human breast cancer tissues. Breast Cancer Res Treat. 1997;42(2):173–181. doi: 10.1023/a:1005760013810. [DOI] [PubMed] [Google Scholar]
- 31.Charpin C, Garcia S, Bonnier P, Martini F, Andrac L, Horschowski N, Lavaut MN, Allasia C. bcl-2 automated and quantitative immunocytochemical assays in breast carcinomas: correlation with 10-year follow-up. J Clin Oncol. 1998;16(6):2025–2031. doi: 10.1200/JCO.1998.16.6.2025. [DOI] [PubMed] [Google Scholar]
- 32.Lee KH, Im SA, Oh DY, Lee SH, Chie EK, Han W, Kim DW, Kim TY, Park IA, Noh DY, et al. Prognostic significance of bcl-2 expression in stage III breast cancer patients who had received doxorubicin and cyclophosphamide followed by paclitaxel as adjuvant chemotherapy. BMC Cancer. 2007;7:63. doi: 10.1186/1471-2407-7-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hammond M, Hayes D, Wolff A, Mangu P, Temin S. American society of clinical oncology/college of american pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract. 2010;6(4):195–197. doi: 10.1200/JOP.777003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Arch Pathol Lab Med. 2014;138(2):241–256. doi: 10.5858/arpa.2013-0953-SA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolff A, Hammond M, Schwartz J, Hagerty K, Allred D, Cote R, Dowsett M, Fitzgibbons P, Hanna W, Langer A. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med. 2007;131(1):18–43. doi: 10.5858/2007-131-18-ASOCCO. [DOI] [PubMed] [Google Scholar]
- 36.Deyarmin B, Kane J, Valente A, van Laar R, Gallagher C, Shriver C, Ellsworth R. Effect of ASCO/CAP guidelines for determining ER status on molecular subtype. Ann Surg Oncol. 2013;20(1):87–93. doi: 10.1245/s10434-012-2588-8. [DOI] [PubMed] [Google Scholar]
- 37.Braun L, Mietzsch F, Seibold P, Schneeweiss A, Schirmacher P, Chang-Claude J, Peter Sinn H, Aulmann S. Intrinsic breast cancer subtypes defined by estrogen receptor signalling-prognostic relevance of progesterone receptor loss. Mod Pathol. 2013;26(9):1161–1171. doi: 10.1038/modpathol.2013.60. [DOI] [PubMed] [Google Scholar]
- 38.Cheang M, Chia S, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard P, Parker J. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101(10):736–750. doi: 10.1093/jnci/djp082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwartz AM, Henson DE, Chen D, Rajamarthandan S. Histologic grade remains a prognostic factor for breast cancer regardless of the number of positive lymph nodes and tumor size: a study of 161 708 cases of breast cancer from the SEER program. Arch Pathol Lab Med. 2014;138(8):1048–1052. doi: 10.5858/arpa.2013-0435-OA. [DOI] [PubMed] [Google Scholar]
- 40.Albrektsen G, Heuch I, Thoresen SO. Histological type and grade of breast cancer tumors by parity, age at birth, and time since birth: a register-based study in Norway. BMC Cancer. 2010;10:226. doi: 10.1186/1471-2407-10-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hanna MG, Bleiweiss IJ, Nayak A, Jaffer S. Correlation of Oncotype DX recurrence score with Histomorphology and immunohistochemistry in over 500 patients. Int J Breast Cancer. 2017;2017:1257078. doi: 10.1155/2017/1257078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Orucevic A, Bell JL, McNabb AP, Heidel RE. Oncotype DX breast cancer recurrence score can be predicted with a novel nomogram using clinicopathologic data. Breast Cancer Res Treat. 2017;163(1):51–61. [DOI] [PMC free article] [PubMed]
- 43.Eaton AA, Pesce CE, Murphy JO, Stempel MM, Patil SM, Brogi E, Hudis CA, El-Tamer M. Estimating the OncotypeDX score: validation of an inexpensive estimation tool. Breast Cancer Res Treat. 2017;161(3):435–441. doi: 10.1007/s10549-016-4069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bomeisl PE, Thompson CL, Harris LN, Gilmore HL. Comparison of Oncotype DX recurrence score by histologic types of breast carcinoma. Arch Pathol Lab Med. 2015;139(12):1546–1549. doi: 10.5858/arpa.2014-0557-OA. [DOI] [PubMed] [Google Scholar]
- 45.Mattes MD, Mann JM, Ashamalla H, Tejwani A. Routine histopathologic characteristics can predict oncotype DX(TM) recurrence score in subsets of breast cancer patients. Cancer Investig. 2013;31(9):604–606. doi: 10.3109/07357907.2013.849725. [DOI] [PubMed] [Google Scholar]
- 46.Kurbel S, Dmitrovic B, Marjanovic K, Vrbanec D, Juretic A. Distribution of Ki-67 values within HER2 & ER/PgR expression variants of ductal breast cancers as a potential link between IHC features and breast cancer biology. BMC Cancer. 2017;17(1):231. doi: 10.1186/s12885-017-3212-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hodi Z, Chakrabarti J, Lee AH, Ronan JE, Elston CW, Cheung KL, Robertson JF, Ellis IO. The reliability of assessment of oestrogen receptor expression on needle core biopsy specimens of invasive carcinomas of the breast. J Clin Pathol. 2007;60(3):299–302. doi: 10.1136/jcp.2006.036665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tang P, Wang J, Hicks DG, Wang X, Schiffhauer L, McMahon L, Yang Q, Shayne M, Huston A, Skinner KA, et al. A lower Allred score for progesterone receptor is strongly associated with a higher recurrence score of 21-gene assay in breast cancer. Cancer Investig. 2010;28(9):978–982. doi: 10.3109/07357907.2010.496754. [DOI] [PubMed] [Google Scholar]
- 49.Gage MM, Rosman M, Mylander WC, Giblin E, Kim HS, Cope L, Umbricht C, Wolff AC, Tafra L. A validated model for identifying patients unlikely to benefit from the 21-gene recurrence score assay. Clin Breast Cancer. 2015;15(6):467–472. doi: 10.1016/j.clbc.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jinno H, Matsuda S, Hayashida T, Takahashi M, Hirose S, Ikeda T, Kitagawa Y. Differential pathological response to preoperative chemotherapy across breast cancer intrinsic subtypes. Chemotherapy. 2012;58(5):364–370. doi: 10.1159/000343663. [DOI] [PubMed] [Google Scholar]
- 51.Fountzilas G, Dafni U, Bobos M, Batistatou A, Kotoula V, Trihia H, Malamou-Mitsi V, Miliaras S, Chrisafi S, Papadopoulos S, et al. Differential response of immunohistochemically defined breast cancer subtypes to anthracycline-based adjuvant chemotherapy with or without paclitaxel. PLoS One. 2012;7(6):e37946. doi: 10.1371/journal.pone.0037946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sanchez-Munoz A, Garcia-Tapiador AM, Martinez-Ortega E, Duenas-Garcia R, Jaen-Morago A, Ortega-Granados AL, Fernandez-Navarro M, de la Torre-Cabrera C, Duenas B, Rueda AI, et al. Tumour molecular subtyping according to hormone receptors and HER2 status defines different pathological complete response to neoadjuvant chemotherapy in patients with locally advanced breast cancer. Clin Transl Oncol. 2008;10(10):646–653. doi: 10.1007/s12094-008-0265-y. [DOI] [PubMed] [Google Scholar]
- 53.Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE, Jr, Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman PA, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353(16):1673–1684. doi: 10.1056/NEJMoa052122. [DOI] [PubMed] [Google Scholar]
- 54.Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, Gianni L, Baselga J, Bell R, Jackisch C, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005;353(16):1659–1672. doi: 10.1056/NEJMoa052306. [DOI] [PubMed] [Google Scholar]
- 55.Early Breast Cancer Trialists’ Collaborative G Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–1717. doi: 10.1016/S0140-6736(05)66544-0. [DOI] [PubMed] [Google Scholar]
- 56.Gilcrease MZ, Woodward WA, Nicolas MM, Corley LJ, Fuller GN, Esteva FJ, Tucker SL, Buchholz TA. Even low-level HER2 expression may be associated with worse outcome in node-positive breast cancer. Am J Surg Pathol. 2009;33(5):759–767. doi: 10.1097/PAS.0b013e31819437f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Soran A, Bhargava R, Johnson R, Ahrendt G, Bonaventura M, Diego E, McAuliffe PF, Serrano M, Menekse E, Sezgin E, et al. The impact of Oncotype DX(R) recurrence score of paraffin-embedded core biopsy tissues in predicting response to neoadjuvant chemotherapy in women with breast cancer. Breast Dis. 2016;36(2–3):65–71. doi: 10.3233/BD-150199. [DOI] [PubMed] [Google Scholar]
- 58.Jahn B, Rochau U, Kurzthaler C, Hubalek M, Miksad R, Sroczynski G, Paulden M, Kluibenschadl M, Krahn M, Siebert U. Cost effectiveness of personalized treatment in women with early breast cancer: the application of OncotypeDX and adjuvant! Online to guide adjuvant chemotherapy in Austria. Springerplus. 2015;4:752. doi: 10.1186/s40064-015-1440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen C, Dhanda R, Tseng WY, Forsyth M, Patt DA. Evaluating use characteristics for the oncotype dx 21-gene recurrence score and concordance with chemotherapy use in early-stage breast cancer. J Oncol Pract. 2013;9(4):182–187. doi: 10.1200/JOP.2012.000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE, Jr, Dees EC, Goetz MP, Olson JA, Jr, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast Cancer. N Engl J Med. 2018;379(2):111–121. doi: 10.1056/NEJMoa1804710. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.