Abstract
Background:
This paper concerns public health crises today—the problem of opioid prescription access and related abuse. Inspired by Case and Deaton’s seminal work on increasing mortality among white Americans with lower education, this paper explores the relationship between opioid prescribing and local economic factors.
Objective:
We examined the association between county-level socioeconomic factors (median household income, unemployment rate, Gini index) and opioid prescribing.
Subjects:
We used the complete 2014 Medicare enrollment and part D drug prescription data from the Center for Medicare and Medicaid Services to study opioid prescriptions of disabled Medicare beneficiaries without record of cancer treatment, palliative care, or end-of-life care.
Measures and Research Design:
We summarized the demographic and geographic variation, and investigated how the local economic environment, measured by county median household income, unemployment rate, Gini index, and urban-rural classification correlated with various measures of individual opioid prescriptions. Measures included number of filled opioid prescriptions, total days’ supply, average morphine milligram equivalent (MME)/day, and annual total MME dosage. To assess the robustness of the results, we controlled for individual and other county characteristics, used multiple estimation methods including linear least squares, logistic regression, and Tobit regression.
Results and Conclusions:
Lower county median household income, higher unemployment rates, and less income inequality were consistently associated with more and higher MME opioid prescriptions among disabled Medicare beneficiaries. Geographically, we found that the urban-rural divide was not gradual and that beneficiaries in large central metro counties were less likely to have an opioid prescription than those living in other areas.
Keywords: opioid prescriptions, local economic conditions, disabled medicare beneficiaries
The rapid increase in opioid prescribing has taken a substantial toll in terms of cost,1–3 health,1,4,5 and lives6–8 despite scarce clinical evidence of their effectiveness in treating chronic, noncancer pain.9–11 The rising use of prescription opioids has played a key role in the ongoing opioid overdose epidemic.12–15
High numbers of working-class middle-aged people are unemployed or disabled,16 and prescription opioid overdose mortality has increased in recent years for adults (ages 25–64 y).17 Mounting evidence suggests that prescription opioid misuse among the under-65 Social Security Disability Insurance (SSDI) population may be a serious and growing health and social problem.2,18 Understanding factors related to opioid prescribing is thus particularly pressing for this population. A high percentage (45%) of Medicare-enrolled SSDI beneficiaries take prescription opioids.18 Opioids are prescribed far more frequently and at higher dosages for disabled adults in the United States compared with the general population.2 Further, there is an associated cost with this high prescribing: in 2006, Medicare spent $1.8 billion on prescription opioids for Medicare enrollees under age 65, which far exceeded the $637 million spent on enrollees aged 65 and over.2
Legislation,19 clinical guidelines,10,20 and policy initiatives have been proposed to address the epidemic, but a better understanding of the social determinants associated with opioid prescribing may improve their effectiveness.20 A gap in the literature exists such that large geographic variations in opioid prescribing and related mortality are un-accounted for,8,21 and small-scale studies have shown conflicting observations.22 Evidence exists that individual and local economic conditions are highly correlated with health behaviors, health care quality, and outcomes,23 in general. It is unknown to what extent the local economic environment is a risk factor for high-risk opioid prescribing among the under-65 disabled population. In this paper, we summarize the demographic and geographic patterns of opioid prescriptions, explore the predictive power of county median household income, unemployment rate, income inequality (measured in terms of the Gini coefficient), and urban-rural classification, and discuss the significance of the findings.
METHODS
Study Population
With access to the complete files of the 2014 Medicare claims data from the Centers for Medicare & Medicaid Services (CMS), we studied outpatient prescribing of the under-65 year old disabled population who were enrolled in Medicare part D for at least 12 months, and who entered the program through the SSDI program for the medically disabled. In 2014, 56 million people from 50 states and the District of Columbia were in the Medicare program. Almost 9 million individuals (8.6 million) who became eligible for Medicare through the disability program were under the age of 65. Among the 8.6 million, 12-month drug prescription data were available for the 5.9 million who were enrolled in Medicare part D. These beneficiaries were either in fee-for-service programs, which covered 4.2 million continuously for 12 months in 2014, or managed care programs (1.7 million had 12-months managed care coverage). CMS does not collect data on medical claims for the latter cases, so they are excluded from our analysis. We followed the standard approach in previous studies18,24 and excluded people with records of cancer treatments, end stage renal disease, hospice care. We also dropped those with unknown race/ethnicity. These exclusions brought the study population to 3,493,551.
Measures of Opioid Use
The Medicare part D Prescription Drug event file has detailed information on all prescriptions filled in 2014. We used the National Drug Code classification system to identify opioid prescriptions for our study population (refills included). Opioids were identified from the Centers for Disease Control and Prevention’s (CDC) compilation of opioid formulations.25 We dropped a prescription whenever its days’ supply exceeded 365 days and quantity dispensed exceeded 1000, and excluded the drugs with generic drug name “buprenorphine,” “buprenorphine hydrochloride,” and “buprenorphine hydrochloride/naloxone hydrochloride” because buprenorphine is a commonly prescribed medication for treating opioid dependence. We used a standard measure for the strength of a given amount of opioids that can be compared across specific brands and formulations of drugs by converting the dosage of the drug to its morphine milligram equivalent (MME).
We developed multiple measures of opioid prescribing for each individual in our cohort. These measures allowed us to examine overall prescribing and specific thresholds of use that may be inappropriate. We measured opioid prescribing by the number of opioid prescriptions, total days’ supply, average MME/day, and annual total MME opioid dosage. We calculated average MME/day by dividing annual total MME of the enrollee by the number of days covered by his or her opioid prescription. If 2 prescriptions overlapped on a date, we counted a single day.
Covariates
Beneficiaries’ demographic information was retrieved from the Medicare Beneficiary Summary file. This file contains information on age, sex, race/ethnicity, state of residence, and county of residence (Table 1). There is also a proxy for income level: part D cost share information (low-income subsidy status) (Table 1).
TABLE 1.
Characteristics of Disabled Medicare Part D Beneficiaries Aged 65 or Below in Fee-for-Service Programs, 2014
| Characteristics | No. Beneficiaries (%) | Mean |
|---|---|---|
| Sex | ||
| Male | 1,752,132 (50.2) | |
| Female | 1,741,419 (49.8) | |
| Age (y) | ||
| 15–24 | 58,737 (1.7) | |
| 25–34 | 355,065 (10.2) | |
| 35–44 | 582,285 (16.7) | |
| 45–54 | 1,044,685 (29.9) | |
| 55–64 | 1,452,779 (41.6) | |
| Race/ethnicity | ||
| Non-Hispanic white | 2,520,886 (72.2) | |
| Non-Hispanic black | 706,345 (20.2) | |
| Hispanic | 145,747 (4.2) | |
| Asian | 43,572 (1.3) | |
| American Native | 38,050 (1.1) | |
| Other | 38,951 (1.1) | |
| County median household income | 51,560 | |
| County Gini index | 0.455 | |
| County unemployment rate | 6.5% | |
| Low-income subsidy status* | ||
| Status 1 | 485,474 (13.9) | |
| Status 2 | 1,440,327 (41.2) | |
| Status 3 | 737,875 (21.1) | |
| Status 4 | 223,648 (6.4) | |
| Status 5 | 6580 (0.2) | |
| Status 6 | 19,143 (0.5) | |
| Status 7 | 16,063 (0.5) | |
| Status 8 | 10,250 (0.3) | |
| Status 9 | 554,191 (15.9) | |
| Selected health conditions | ||
| Myocardial infarction | 130,920 (3.8) | |
| CHF | 227,599 (6.5) | |
| Peripheral vascular disease | 197,878 (5.7) | |
| Cerebrovascular disease | 281,567 (8.1) | |
| COPD | 933,179 (26.7) | |
| Dementia | 25,663 (0.7) | |
| Paralysis | 73,791 (2.1) | |
| Diabetes | 971,802 (27.8) | |
| Diabetes with sequelae | 283,004 (8.1) | |
| Chronic renal failure | 226,134 (6.4) | |
| Various cirrhodites | 59,021 (1.7) | |
| Moderate-severe liver disease | 26,822 (0.8) | |
| Ulcers | 53,874 (1.5) | |
| Rheumatoid arthritis | 157,047 (4.5) | |
| AIDS | 68,488 (1.9) | |
| Depression | 731,662 (20.9) | |
| Serious mental illness | 650,109 (18.6) | |
| Alcohol abuse | 76,350 (2.2) | |
| Urban-rural classification | ||
| Large central metro | 729,133 (20.9) | |
| Large fringe metro | 672,267 (19.2) | |
| Medium metro | 761,298 (21.8) | |
| Small metro | 453,637 (12.9) | |
| Micropolitan | 506,575 (14.5) | |
| Noncore | 370,641 (10.6) | |
| Total | 3,493,551 | |
Detailed definitions are in the supplement (Supplemental Digital Content 1, http://links.lww.com/MLR/B493).
AIDS indicates acquired immune deficiency syndrome; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease.
We assessed 3 indicators of local economic conditions at the county level: median household income, unemployment rate, and Gini index (a measure of a community’s income distribution on a 0–1 scale, where 0 equals perfect equality and 1 denotes maximal inequality). We obtained county median household income for 2014 and Gini index from the US Census Bureau’s American Community Survey, 2010–2014,26 and unemployment rate (2014 annual averages) from the US Bureau of Labor Statistics.27 We took the natural logarithm of median household income to measure percentage changes. The variables included are popular measures for overall affluence, employment availability, and economic inequality, which are 3 critical dimensions of the local economy.
As for geographic variation, we used state dummy variables to control for between-state variations in policies and other characteristics, and controlled for within-state factors by including urban-rural classifications. For example, rural hospitals are known to have recruitment difficulties.23 We adopted the latest 2013 Urban-Rural Classification Scheme for Counties of the National Center for Health Statistics (NCHS),28 which designates four metropolitan (urban) categories and 2 nonmetropolitan (rural) ones, and distinctively separates counties in the largest metropolitan areas into 2 groups called large central metro (roughly for inner cities) and large fringe metro.
We included 15 comorbid conditions, such as heart disease, AIDS, and diabetes, which are used in calculating the Charlson Comorbidity Index (cancer is not among the 15 because we excluded cancer patients).29 We also constructed indicators for diagnoses of depression, serious mental illness, and alcohol abuse (Supplemental Digital Content 1, http://links.lww.com/MLR/B493).
Data Analysis
We first conducted preliminary analyses of the influence of age, sex, race/ethnicity, and urban-rural categories (Table 2) by calculating, for each subgroup, the proportions of beneficiaries with at least 1 prescription, with at least 6 prescriptions, with an average MME/day dosage ≥ 50 mg (a threshold for careful assessment according to the latest CDC guideline10), and with an average MME/day ≥ 90 mg (a threshold to avoid or carefully justify increasing dosage beyond) (Table 2).
TABLE 2.
Opioid Prescriptions by Sex, Age, Race/Ethnicity, and Metro/Nonmetro Classification Among Disabled Medicare Part D Beneficiaries Aged 65 or Below in Fee-for-Service Programs, 2014
| No. Beneficiaries | Opioid Users (%) | Long-term Opioid User (%) | ≥ 50 MME Daily Dosage (%) | ≥ 90 MME Daily Dosage (%) | |
|---|---|---|---|---|---|
| Male | 1,752,132 | 42 | 23 | 14 | 7 |
| Age 15–24 | 34,964 | 17 | 3 | 3 | 1 |
| Age 25–34 | 197,393 | 27 | 9 | 7 | 3 |
| Age 35–44 | 297,000 | 38 | 19 | 12 | 6 |
| Age 45–54 | 531,031 | 46 | 27 | 16 | 9 |
| Age 55–64 | 691,744 | 47 | 27 | 16 | 8 |
| Female | 1,741,419 | 56 | 32 | 16 | 8 |
| Age 15–24 | 23,773 | 29 | 5 | 5 | 1 |
| Age 25–34 | 157,672 | 43 | 16 | 10 | 4 |
| Age 35–44 | 285,285 | 53 | 28 | 16 | 8 |
| Age 45–54 | 513,654 | 59 | 36 | 19 | 10 |
| Age 55–64 | 761,035 | 59 | 34 | 17 | 8 |
| Non-Hispanic white | 2,520,886 | 51 | 30 | 17 | 9 |
| Non-Hispanic black | 706,345 | 47 | 23 | 11 | 5 |
| Hispanic | 145,747 | 40 | 16 | 9 | 4 |
| Asian | 43,572 | 27 | 9 | 5 | 2 |
| American Native | 38,050 | 53 | 31 | 16 | 8 |
| Other | 38,951 | 37 | 18 | 11 | 6 |
| Large central metro | 729,133 | 43 | 22 | 13 | 7 |
| Large fringe metro | 672,267 | 47 | 26 | 16 | 9 |
| Medium metro | 761,298 | 49 | 27 | 16 | 8 |
| Small metro | 453,637 | 51 | 29 | 15 | 8 |
| Micropolitan | 506,575 | 53 | 31 | 16 | 8 |
| Noncore | 370,641 | 56 | 34 | 16 | 8 |
| Total | 3,493,551 | 51 | 27 | 15 | 8 |
MME indicates morphine milligram equivalent.
To mitigate problems involving small samples (ie, 35 counties had <10 beneficiaries in the study population), we used “commuting zones” which are groupings of counties based on commuting patterns in the 1990 US Census30 and mapped in Figure 1. The aggregation of counties also facilitates comparisons with closely related literature.22 In our regression analyses, the dependent variables correspond to different characteristics of opioid prescriptions. They include the indicators of ever prescribing (dummy variable that takes the value of 1 if the individual had at least 1 opioid prescription on record and 0 otherwise), having long-term opioid prescriptions (at least 6 prescriptions in 2014), total days’ supply (number of days of prescription opioid medication assuming full compliance), average MME/day, and total MME.
FIGURE 1.
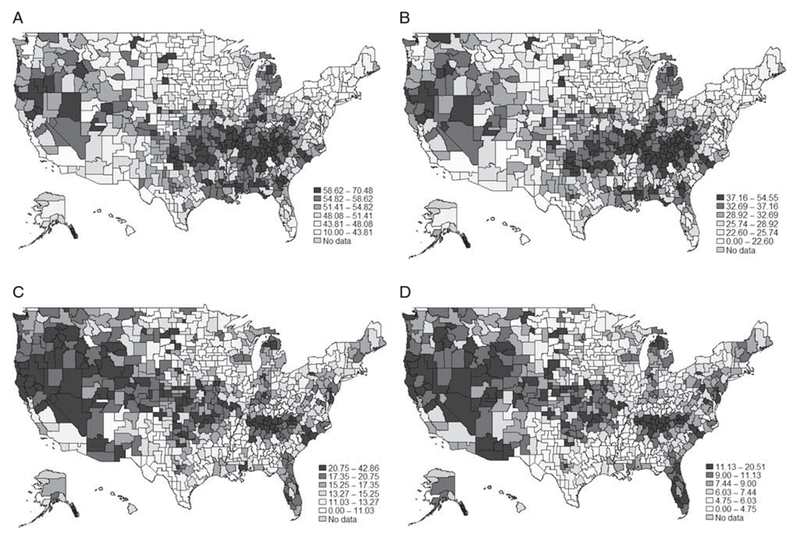
Geographical variations in opioid prescriptions among Medicare part D beneficiaries aged 65 or below in fee-for-service programs, by commuting zones in 2014. A, Percentage with an opioid prescription. B, Percentage with long-term opioid prescription. C, Percentage of opioid prescriptions ≥ 50 daily MME. D, Percentage of opioid prescriptions ≥ 90 daily MME. MME indicates morphine milligram equivalent.
Multilevel linear least square (LLS) estimation is the main regression method, with the state fixed effects controlled. We studied the effects of 3 economic variables separately (Table 3 and Sections 1–3 of the Supplement, Supplemental Digital Content 1, http://links.lww.com/MLR/B493) and also let them enter regressions jointly (Table 4 and Section 4 of the Supplement, Supplemental Digital Content 1, http://links.lww.com/MLR/B493). Regressions controlled for aforementioned covariates plus age squared as a common practice in economics literature.31
TABLE 3.
Linear Least Square Regressions of Opioid Prescriptions on Each Local Economic Condition Separately Among Medicare Part D Disabled Beneficiaries Aged 65 or Below in Fee-for-Service Programs, 2014
| Coefficients of the Regression | Opioid User | Long-term Opioid User | Total Days of Usage | Log Mean Daily MME | Log Total MME |
|---|---|---|---|---|---|
| Log median household income† | −0.0532 (0.0000)*** | −0.0433 (0.0000)*** | −16.0250 (0.0000)*** | −0.1181 (0.0030)*** | −0.4570 (0.0000)*** |
| Unemployment rate | 0.4331 (0.0000)*** | 0.3401 (0.0080)*** | 139.9007 (0.0010)*** | 0.8300 (0.0670)* | 3.8887 (0.0010)*** |
| Gini index | −0.3957 (0.0000)*** | −0.3118 (0.0000)*** | −91.8825 (0.0000)*** | −1.6716 (0.0000)*** | −3.6182 (0.0000)*** |
There are 3,493,551 observations for each regression. All models controlled for age, age squared, sex, race/ethnicity, medical condition, state dummies, rural-urban dummies, and individual income status (proxied by cost share information). Reference group for the urban-rural classification is large central metro.
Below each estimated coefficient, its P-value is calculated based on robust SEs clustered by county.
P < 0.1.
P < 0.05.
P < 0.01.
The natural logarithm of median household income.
TABLE 4.
Linear Least Square Regressions of Opioid Prescriptions on All Local Economic Conditions Jointly Among Medicare Part D Disabled Beneficiaries Aged 65 or Below in Fee-for-Service Programs, 2014
| Coefficients of the Regression | Opioid User | Long-term Opioid User | Total Days of Usage | Log Mean Daily MME | Log Total MME |
|---|---|---|---|---|---|
| Log median household income† | −0.0639 (0.0000)*** | −0.0530 (0.0000)*** | −17.4243 (0.0000)*** | −0.1822 (0.0000)*** | −0.5405 (0.0000)*** |
| Unemployment rate | 0.0797 (0.4570) | 0.0430 (0.7560) | 40.2352 (0.3860) | −0.0604 (0.8960) | 0.9652 (0.4120) |
| Gini index | −0.4795 (0.0000)*** | −0.3793 (0.0000)*** | −115.8516 (0.0000)*** | −1.8898 (0.0000)*** | −4.3441 (0.0000)*** |
| Large fringe metro | 0.0210 (0.0010)*** | 0.0177 (0.0050)*** | 5.4735 (0.0070)*** | 0.0816 (0.0020)*** | 0.1921 (0.0020)*** |
| Medium metro | 0.0222 (0.0000)*** | 0.0139 (0.0290)** | 3.8287 (0.0580)* | 0.0803 (0.0030)*** | 0.1738 (0.0050)*** |
| Small metro | 0.0268 (0.0000)*** | 0.0157 (0.0220)** | 3.8240 (0.0850)* | 0.0789 (0.0060)*** | 0.1842 (0.0060)*** |
| Micropolitan | 0.0262 (0.0000)*** | 0.0193 (0.0050)*** | 5.1081 (0.0210)** | 0.0773 (0.0060)*** | 0.1984 (0.0030)*** |
| Noncore | 0.0376 (0.0000)*** | 0.0342 (0.0000)*** | 8.9669 (0.0000)*** | 0.1170 (0.0000)*** | 0.3248 (0.0000)*** |
There are 3,493,551 observations for each regression. All models controlled for age, age squared, sex, race/ethnicity, medical condition, state dummies, rural-urban dummies, and individual income status (proxied by cost share information). Reference group for the urban-rural classification is large central metro.
Below each estimated coefficient, its P-value is calculated based on robust SEs clustered by county.
P < 0.1.
P < 0.05.
P < 0.01.
The natural logarithm of median household income.
In addition to, main regressions, we ran various sensitivity tests. We reported simple correlations of outcome variables and economic statistics (Section 5 of the Supplement, Supplemental Digital Content 1, http://links.lww.com/MLR/B493). We ran logistic regressions for the models with ever prescribing and long-term prescribing as the outcome variables; we applied a Tobit model with lower bound 0 and upper bound 365 for total days’ supply; we applied Tobit models with lower bound 0 for log mean MME/day and log total MME (Section 6 of the Supplement, Supplemental Digital Content 1, http://links.lww.com/MLR/B493).
There are concerns that depression, serious mental illness, and alcohol abuse may be partially endogenous. We thus explore the consequence of excluding these controls in regressions (Section 7 of the Supplement, Supplemental Digital Content 1, http://links.lww.com/MLR/B493).
We used STATA MP 14.0 and SAS Enterprise Guide 7.1.
RESULTS
Descriptive
Our study population, which are individuals under age 65 with at least 12 consecutive months of Medicare A, B, and D fee-for-service and with no active cancer diagnosis or hospice, numbering 3,493,551, accounted for 16,288,923 opioid prescriptions in 2014 (Table 2). The median quantity dispenses is 90. The mean quantity dispensed is 86. Half (49%; n = 1,712,741) of these beneficiaries filled opioid prescriptions at least once. The average number of opioid prescriptions among this population was 4.7. The average days they were on an opioid prescription was 81 days.
In total 27% were prescribed opioids long term (at least 6 prescriptions; Table 2). Fifteen percent were prescribed an average MME/day of at least 50 mg, and 8% were prescribed at least 90 mg.
Sex, Age, Race/Ethnicity, and Metro/Nonmetro Variation
Table 2 shows characteristics of opioid prescriptions for different demographic groups. There was greater opioid prescribing among female beneficiaries compared with their male counterparts in almost all age groups for each of the 4 prescription opioid measures. There was greater opioid prescribing among older beneficiaries (ages 55–64 y; male individuals = 47%, female individuals 59%) than younger beneficiaries for each sex (ages 15–24 y; male individuals = 17%, female individuals 29%).
Non-Hispanic white and Native American beneficiaries were more likely to have been prescribed opioids long term (30% and 31%, respectively) compared with non-Hispanic black beneficiaries (24%), and were more likely to have been prescribed a high daily MME dosage (≥ 90 MME, 9% and 8%, respectively) than African Americans (5%). Asian beneficiaries were least likely to be long-term opioid users or be prescribed daily equivalents of at least 90 MME (9% and 2%, respectively).
Using the NCHS urban-rural classification scheme, we discovered that a greater distinction exists between large central metro counties and the other 5 types of counties than between urban counties and rural counties. A smaller proportion of people living in large central metro areas had opioid prescriptions (43%) or were prescribed long-term opioid therapy (22%) compared with people living in small metro areas (51% and 29%, respectively). Beneficiaries living in large central metro counties also were less likely to be prescribed a high daily MME dosages (13% for ≥ 50 MME and 7% for ≥ 90 MME) compared with beneficiaries living in other areas: for example, the corresponding percentages are 16% and 9% for people living in large fringe metro areas.
Geographical Variation
Four maps (Fig. 1) show the geographical variations of opioid prescribing based on commuting zones. They similarly identify the South, Southwest, and Midwest as regions of more intensive opioid prescribing, which closely overlaps with regions of economic hardship.32
This is confirmed by a strong negative correlation between various measures of opioid prescribing and county median household income, and a strong positive correlation between those measures and county unemployment rate (Section 5 of the Supplement, Supplemental Digital Content 1, http://links.lww.com/MLR/B493). Our regression analysis below, which controls for covariates, validates the association between local economic conditions and opioid prescribing.
Influence of Local Economic Conditions on Opioid Prescriptions: Separate Regressions
Estimated coefficients of median household income, unemployment rate, Gini index from separate multilevel LLS regressions are reported in Table 3. They are all statistically significant at the 1% level, except for 1 case of P-value equaling 0.0670.
Signs of coefficients are coherent for different measures of opioid prescription. Among them, a 1% growth in median household income is associated with a decrease of total MME dosage by 0.46%, a 1% increase in unemployment rate is associated with an increase of total MME by 3.89%, and a 0.01 increase in Gini index is associated with a 3.62% reduction of total MME.
Influence of Local Economic Conditions on Opioid Prescriptions: Joint Regressions
Coefficients of median household income, unemployment rate, Gini index, and urban-rural classification from joint multilevel LLS regressions are reported in Table 4. The results are comparable with those with 3 economic statistics included separately, but the unemployment rate becomes statistically insignificant for all 5 regressions. One potential interpretation is that the information about the unemployment rate is less important when we know the other 2 measures.
After controlling for the 3 local economic statistics and other covariates, the finding for the urban-rural divide is similar to those contained in descriptive statistics (Table 2), so the descriptive urban-rural divide cannot be explained by differences in those 3 indicators of local economy. Large central metro areas were different from the rest of categories. Large fringe metro counties were similar to rural counties. For example, all other things remaining equal, people who live in large fringe metro would likely have 5.47 days more opioid usage compared with people who live in large central metro, and people who live in micropolitan have 5.10 more days.
Sensitivity Analysis
Simple correlations between economic indicators and measures of opioid prescription are reported in Section 5 of the Supplement (Supplemental Digital Content 1, http://links.lww.com/MLR/B493). All signs accord with those from separate LLS regressions.
Logistic and Tobit regressions, which handle the issues of binary or censored dependent variables but rely heavily on distributional assumptions, are reported in Section 6 of the Supplement (Supplemental Digital Content 1, http://links.lww.com/MLR/B493). Results are qualitatively the same as Table 4.
To guard against potential biases explained earlier, we excluded depression, serious mental illness, and alcohol abuse from regressions, which are reported in Section 7 of the Supplement (Supplemental Digital Content 1, http://links.lww.com/MLR/B493). The qualitative results are intact.
DISCUSSION
Our study showed a strong association between 3 county-level economic estimates (median household income, the Gini index, and the unemployment rate) and receipt of prescription opioids among disabled nonelderly Medicare beneficiaries. The metro/nonmetro pattern of opioid prescribing was different from that of other health indicators such as smoking, cerebrovascular disease, and mortality which follow different patterns, suggesting a distinctive mechanism for the emergence of the problem, which justifies future research.28 The results stand in contrast with related studies21,33 of smaller scales which found neighborhoods with high income inequality but lower poverty rates are the highest risk area.
The negative association between opioid prescribing and income inequality was unexpected. Theories34 predict more marginalized individuals, such as disabled Medicare beneficiaries living in a county with high income inequality, to be more susceptible to pain-related conditions. There seems to be a connection between our results and a finding that life expectancy for bottom income quartile individuals was positively correlated with Gini index (r = 0.20, P = 0.11).22 It is difficult to explain this unexpected association, but there are a number of possibilities. For example, more homogenous regions might be more susceptible to social contagions that spread harmful behaviors. Alternatively, low inequality may be associated with other characteristics—like the absence of a dynamic economy and hence a lack of job opportunities not captured by other controlled variables. Moreover, provider behavior, such as opioid prescribing, might vary in different environments and this may affect quality of care.35 Other mechanisms that can contribute to the identified associations also have deep socioeconomic roots.
Some caution is necessary in interpreting the results. First, the study population is large, but its unrepresentativeness cautions against making generalizations to other groups and thus justifies further investigation using other sources of data. The analyses are limited to a dataset on persons on disability Medicare coverage. Some beneficiaries had to pay a small amount for Medicare part D coverage, raising a potential selection problem. Second, quantity prescribed may not equal quantity consumed, so our results might overestimate potential risk. Third, pharmacy claims represent filled prescriptions reimbursed and do not capture prescriptions paid for with cash, resulting in an underestimate of opioids consumed. Fourth, there could be some regional variation because certain regions may have greater percentage of certain health conditions, for example back pain, because of the predomination occupations in that region.24
Although appropriately treating the health conditions of individuals is a necessary first step in reducing prescription opioid misuse, abuse, and overdose, the current study suggests an interdisciplinary approach could be beneficial for addressing the opioid epidemic. A solely medical approach may be less effective than a comprehensive one that incorporates socioeconomic policies such as poverty alleviation. Vulnerable persons in disadvantaged communities may be exposed to higher risk drug regimens, which are responsible for rising all-cause mortality among middle aged Caucasians Americans.7 Socioeconomic interventions may be important to consider as they can influence a range of individual health factors as well as health systems factors. Prevention strategies might include developing and implementing interventions that target critical factors, or directing existing interventions geographically to have the greatest impact (eg, targeting academic detailing on clinical guidelines in nonmetro areas).
In addition, monitoring local economic conditions may be helpful for identifying attributes of areas with potentially risky prescribing practices. For instance, if we know an industry cluster is collapsing due to advancements in robotics, policy makers can introduce preventative measures in view of high future risks of local opioid epidemic.
CONCLUSIONS
Our study of disabled, nonelderly Medicare part D beneficiaries in 2014 evidenced widespread prescribing of opioids (50% of the Medicaid-part-D disabled population received a prescription opioid compared with 10% of the general population). There was substantial demographic and geographic variation in measures of opioid prescribing. People at greatest risk for potentially harmful use live in communities outside inner cities with lower median household incomes, higher unemployment rates, and a lower Gini index. To identify the reasons for the association of opioid prescribing and local economic conditions, a multipronged approach (involving medical, behavioral health, and socioeconomic disciplines) would be needed.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Mick Ballesteros, PhD (CDC), Curtis Florence, PhD (CDC), Tamara Haegerich, PhD (CDC), Karin Mack, PhD (CDC), and Rita Noonan, PhD (CDC) who provided helpful comments, but were not compensated. This work was done when Zhou was at CDC and Yu was at Emory University.
Footnotes
The opinions and conclusions are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC), Health Care Cost Institute, and Stanford University.
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website, www.lww-medicalcare.com.
REFERENCES
- 1.Florence CS, Zhou C, Luo F, et al. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54:901–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou C, Florence CS, Dowell D. Payments for opioids shifted substantially to public and private insurers while consumer spending declined, 1999–2012. Health Aff. 2016;35:824–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart WF, Ricci JA, Chee E, et al. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290:2443–2454. [DOI] [PubMed] [Google Scholar]
- 4.Carman WJ, Su S, Cook SF, et al. Coronary heart disease outcomes among chronic opioid and cyclooxygenase-2 users compared with a general population cohort. Pharmacoepidemiol Drug Saf. 2011;20:754–762. [DOI] [PubMed] [Google Scholar]
- 5.Li L, Setoguchi S, Cabral H, et al. Opioid use for noncancer pain and risk of myocardial infarction amongst adults. J Intern Med. 2013;273:511–526. [DOI] [PubMed] [Google Scholar]
- 6.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300:2613–2620. [DOI] [PubMed] [Google Scholar]
- 7.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci USA. 2015;112:15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60:1487. [PubMed] [Google Scholar]
- 9.Daubresse M, Chang HY, Yu Y, et al. Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000–2010. Med Care. 2013;51:870–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315:1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nicholas MK, Molloy AR, Brooker C. Using opioids with persisting noncancer pain: a biopsychosocial perspective. Clin J Pain. 2006;22:137–146. [DOI] [PubMed] [Google Scholar]
- 12.Cicero TJ, Ellis MS, Surratt HL. Effect of abuse-deterrent formulation of OxyContin. N Engl J Med. 2012;367:187–189. [DOI] [PubMed] [Google Scholar]
- 13.Apfelbaum JL, Ashburn MA, Connis RT. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116:248–273. [DOI] [PubMed] [Google Scholar]
- 14.Miech R, Johnston L, O’Malley PM, et al. Prescription opioids in adolescence and future opioid misuse. Pediatrics. 2015;136:1169–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edlund MJ, Martin BC, Russo JE, et al. The role of opioid rrescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription. Clin J Pain. 2014;30:557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bureau of Labor Statistics. Persons with a disability: barriers to employment, types of assistance, and other labor-related issues. May 2012. Available at: www.bls.gov/news.release/dissup.toc.htm. Accessed September 18, 2017
- 17.Chen LH, Hedegaard H, Warner M. Drug-poisoning deaths involving opioid analgesics: United States, 1999-2011. NCHS Data Brief. 2014;166:1–8. [PubMed] [Google Scholar]
- 18.Meara E, Horwitz JR, Powell W, et al. State legal restrictions and prescription-opioid use among disabled adults. N Engl J Med. 2016;375:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams AR, Bisaga A. From AIDS to opioids—how to combat an epidemic. N Engl J Med. 2016;375:813–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10:113. e122–130.e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.King NB, Fraser V, Boikos C, et al. Determinants of increased opioid-related mortality in the United States and Canada, 1990–2013: a systematic review. Am J Public Health. 2014;104:e32–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001-2014. JAMA. 2016;315:1750–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roth AE. On the allocation of residents to rural hospitals: a general property of two-sided matching markets. Econometrica. 1986;54:425–427. [Google Scholar]
- 24.Morden NE, Munson JC, Colla CH, et al. Prescription opioid use among disabled Medicare beneficiaries: intensity, trends and regional variation. Med care. 2014;52:852–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC; CDC compilation of opioid analgesic formulations with morphine milligram equivalent conversion factors, 2014 version. Available at: www.pdmpassist.org/pdf/BJA_performance_measure_aid_MME_conversion.pdf. Accessed September 18, 2017. [Google Scholar]
- 26.US Census Bureau. Income and Poverty in the United States. 2014. Available at: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-252.pdf. Accessed September 18, 2017.
- 27.Bureau of Labor Statistics. Labor force statistics from the current population survey. 2017. Available at: www.bls.gov/cps/cpsaat01.htm. Accessed September 18, 2017.
- 28.CDC. 2013. NCHS urban-rural classification scheme for counties. Available at: www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf. Accessed September 18, 2017.
- 29.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 30.Tolbert CM, Sizer M. US commuting zones and labor market areas: a 1990 update. Washington, DC: Economic Research Service, Rural Economy Division; 1996. [Google Scholar]
- 31.Filoso V Regression anatomy, revealed. Stata J. 2013;13:92–106. [Google Scholar]
- 32.Autor DH, Dorn D, Hanson GH. The China syndrome: local labor market effects of import competition in the United States. Am Econ Rev. 2013;103:2121–2168. [Google Scholar]
- 33.Cerdá M, Ransome Y, Keyes KM, et al. Prescription opioid mortality trends in New York City, 1990-2006: examining the emergence of an epidemic. Drug Alcohol Depend. 2013;132:53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kondo N, Sembajwe G, Kawachi I, et al. Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. BMJ. 2009;339:b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13:988–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


