Abstract
Background and Objectives:
The use of laparoscopy in the trauma setting is gaining momentum, with more therapeutic procedures being performed. We evaluated the use of laparoscopic splenectomy among trauma patients with data from the National Trauma Database. We compared outcomes for trauma patients undergoing laparoscopic (LS) versus open splenectomy (OS).
Methods:
From the National Trauma Database (2007 to 2015), we identified all patients who underwent a total splenectomy. Patients who had other abdominal operations were excluded. All patients were categorized into 1 of 2 groups: LS or OS. Outcomes of in-hospital mortality, postoperative length of stay, and incidence of major complications between the 2 groups were compared. Bivariate parametric and nonparametric analyses were performed. Patients were then matched on baseline demographic and injury characteristics by using propensity score matching techniques, and we compared differences by using regression analysis.
Results:
A total of 25,408 patients underwent OS and 113 patients underwent LS (0.44%). Patients were significantly different at baseline, with the LS group being less severely injured. Bivariate analysis revealed no difference in length of stay (9 vs 8 days, P = .62), incidence of major complications (10% vs 15%, P = .24), or mortality (6% vs 11%, P = .23). LS was performed in 29.2% of patients beyond 24 hours from presentation compared with 9.5% in the OS (P < .001). Adjusted multivariate analysis showed no overall difference in outcomes.
Conclusion:
LS for trauma is increasingly being used at many centers throughout the United States. The procedure is safe, with outcomes similar to those of OS in selected trauma patients.
Keywords: Laparoscopic surgery, Laparoscopic splenectomy, Open splenectomy
INTRODUCTION
Laparoscopic surgery is the standard of care for a variety of elective surgical procedures such as laparoscopic cholecystectomy, but its adoption in the trauma setting has been slow. Exploratory laparotomy has been the standard of care, with laparoscopy reserved only for selected cases in which a diagnosis of abdominal penetration is questionable. In 1995, the first therapeutic laparoscopic procedure in a trauma patient was reported, which involved the repair of a diaphragmatic injury.1 In the past decade, there has been an increased use of both diagnostic and therapeutic laparoscopic techniques in the trauma setting. There have been reports of repairs of injuries to the stomach, intestine, liver, spleen, and diaphragm.2–5 The imminent goal in trauma patients often includes the most expeditious way to diagnose and treat life-threatening conditions; many believe this can be best achieved through laparotomy with full exploration of the abdomen. Yet, often, trauma patients are stable enough to avoid a laparotomy in favor of a laparoscopic approach.
Laparoscopic splenectomy (LS), first described in 1991, is often the preferred approach in an elective setting.6 Its use in trauma, however, was reported in only some case reports and small series. Therapeutic laparoscopy, especially splenectomy in a trauma setting, is controversial. The purposes of this study were to describe the national trends in LS in trauma patients and to compare the outcomes for trauma patients undergoing LS with those of patients undergoing open splenectomy (OS).
METHODS
The National Trauma Database (NTDB) was queried for all the patients who underwent splenectomy between 2007 and 2015. The NTDB is the largest trauma registry in the United States (US) and has data from >750 trauma centers across the nation with >6 million records. All patients who underwent isolated total splenectomy with no other major operative procedure were included in the analysis. International Classification of Diseases, Ninth Revision (ICD-9) procedure code 41.5 for total splenectomy was used to identify patients. Patients who underwent other major operative intervention as well as those with missing outcome information were excluded from analysis.
The following patient characteristics were collected: age, sex, insurance status, and date of admission. Injury characteristics included Injury Severity Score (ISS), mechanism of injury, body region involved, and grade of splenic injury. Facility characteristics included trauma level and size. Outcome variables of interest were in-hospital mortality, length of hospital stay (LOS) and any major complications during the hospital stay.
Patients were divided into 2 major group according to the surgical intervention; LS and OS. Due to the absence of an ICD-9 code for LS, all patients who underwent diagnostic laparoscopy, with total splenectomy without laparotomy or any other major operative intervention, were classified as having undergone total LS.
Descriptive analysis was performed for the qualitative variables. Bivariate comparison was performed for the baseline characteristics and outcomes using the χ2 and t tests where appropriate. Outcome variables included in-hospital mortality, LOS, and the occurrence of any major complication. Major complications included surgical site infections, sepsis, venous thromboembolism, myocardial infarction, pneumonia, cerebrovascular accident, reintubation, acute renal failure, acute respiratory distress syndrome, and cardiac arrest.
Propensity score matching techniques were used to match patients in the LS with those with the OS group. The outcomes of the subset of matched patients were compared using logistic regression for mortality, complications, and prolonged LOS (defined as longer than the 75th percentile).
We also performed subset analysis on patients with isolated abdominal injuries. These were patients with an Abbreviated Injury Scale of <3 for all body regions other than “abdomen.” All analysis was performed by using STATA v 13.
The study was approved by the institutional review board at Howard University. The NTDB is a publicly available deidentified data set and therefore was exempt from full ethical review.
RESULTS
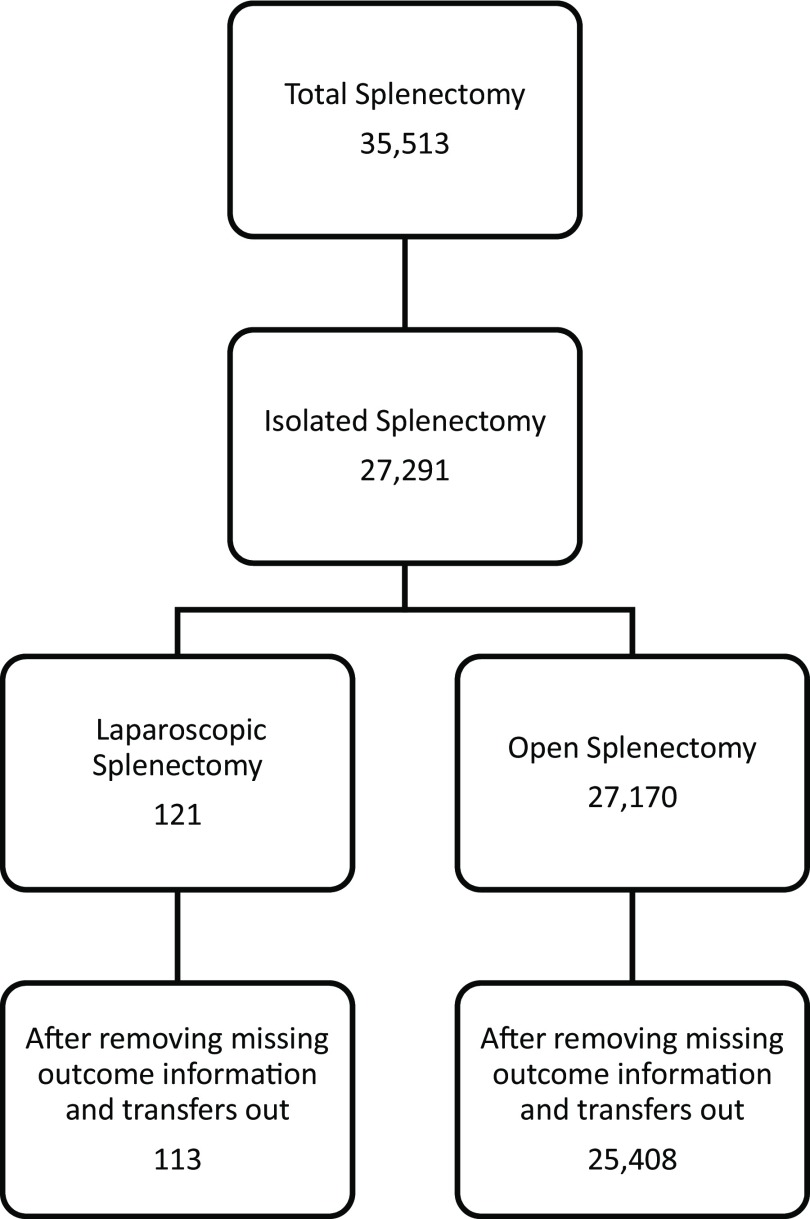
A total of 35,513 patients underwent total splenectomy during the period 2007–2015, in which 27,291 patients underwent isolated splenectomy. Of these 27,291 patients with isolated splenectomy, 121 patients underwent LS and 27,170 patients underwent OS. After adjustment for missing outcome information, there were 113 (0.44%) patients who underwent LS and 25,408 who underwent OS and were compared for the purpose of this study (Figure 1).
Figure 1.
Patients for analysis.
The mean age for the LS group was 44 years old, and the mean age for the OS group was 39 years old (P = .01). Males underwent LS 70% of the time versus undergoing OS 71% of the time (P = .83). Insurance status was not significantly associated with either intervention with 81% of patients in LS being insured compared with 78% in the OS group (P = .44). Type of injury (blunt vs penetrating) was not significantly associated with either group with 10% in the LS group and 12% in the OS group having penetrating injury (P = .59). A higher ISS (>25) was associated with a greater proportion of OS patients (P < .001). Presenting vital signs consistent with hypotension (systolic blood pressure <90), was associated more with OS group at 20% compared to 13% in LS group (p = 0.04). Glasgow Coma Scale (GCS) score was not statistically significant, but a trend was noticed with higher GCS score (12–15) being associated with a greater proportion of LS patients (P = .076) (Table 1).
Table 1.
Baseline Characteristics of Trauma Patients
| Variable | Overall | LS | OS | P Value |
|---|---|---|---|---|
| Total number of patients | 25,521 | 113 | 25,408 | |
| Mean Age (in Years) | 39 (20) | 44 (25) | 39 (20) | 0.01 |
| Male Gender | 18,065 (71%) | 79 (70%) | 17,986 (71%) | 0.83 |
| Race | 0.29 | |||
| White | 18,124 (74%) | 80 (78%) | 18,044 (74%) | |
| Black | 2,913 (12%) | 9 (9%) | 2,904 (12%) | |
| Hispanic | 1,960 (8%) | 11 (11%) | 1,949 (8%) | |
| Other | 1,506 (6%) | 3 (3%) | 1,503 (6%) | |
| Insured | 16,923 (77%) | 81 (81%) | 16,842 (78%) | 0.44 |
| Penetrating | 2,939 (12%) | 11 (10%) | 2,928 (12%) | 0.59 |
| Mechanism | 0.11 | |||
| MVC | 14,963 (66%) | 57 (60%) | 14,906 (66%) | |
| Stab | 847 (4%) | 6 (6%) | 841 (4%) | |
| GSW | 2,092 (9%) | 5 (5%) | 2,087 (9%) | |
| Pedestrian | 998 (4%) | 7 (7%) | 991 (4%) | |
| Fall | 3,346 (15%) | 20 (21%) | 3,326 (15%) | |
| Mean ISS | 27 (14) | 22 (13) | 27 (14) | <0.001 |
| ISS Categories | <0.001 | |||
| 0–8 | 873 (3%) | 11 (10%) | 862 (3%) | |
| 9–15 | 3,344 (13%) | 25 (22%) | 3,319 (13%) | |
| 16–24 | 6,092 (24%) | 31 (28%) | 6,061 (24%) | |
| 25–75 | 14,936 (59%) | 45 (40%) | 14,891 (59%) | |
| Hypotensive | 5,047 (20%) | 14 (13%) | 5,033 (20%) | 0.04 |
| GCS | 0.076 | |||
| 3–5 | 5,130 (21%) | 16 (14.7%) | 5,114 (21%) | |
| 6–8 | 717 (3%) | 0% | 717 (3%) | |
| 9–11 | 655 (3%) | 2 (1.8%) | 653 (3%) | |
| 12–15 | 18,150 (74%) | 91 (83.5%) | 18,059 (74%) | |
| Level of Trauma Center | 0.64 | |||
| 1 | 16,593 (66%) | 79 (71%) | 16,514 (66%) | |
| 2 | 7,163 (29%) | 28 (25%) | 7,135 (29%) | |
| 3 | 891 (4%) | 5 (4%) | 886 (4%) |
Bold emphasis represents significant p values.
Multivariate analysis predicting a patient undergoing LS after adjustment for demographics and injury variables was also performed. An ISS <25, along with systolic BP >140 mm Hg were found to be independent predictors for LS (Table 2).
Table 2.
Independent Predictors for Laparoscopic Splenectomy
| Laparoscopic Splenectomy | OR | P-Value | 95% CI | |
|---|---|---|---|---|
| ISS (compared to ISS 1–8) | ||||
| 9–15 | 0.80 | 0.642 | 0.32 | 2.02 |
| 16–24 | 0.54 | 0.183 | 0.22 | 1.34 |
| 25–75 | 0.35 | 0.022 | 0.14 | 0.86 |
| Systolic BP | ||||
| 1–89 | 0.39 | 0.012 | 0.18 | 0.81 |
| 90–140 | 0.53 | 0.011 | 0.32 | 0.86 |
| 141–300 | 1.00 | (Collinearity) | ||
Bold emphasis represents significant p values.
Although a greater proportion of the OS group had in-hospital mortality (18%) compared with the LS group (14.2%), this was not statistically significant (P = .3). The median postoperative LOS was also similar between the 2 groups at 9 days for LS and 8 days for OS (P = .62). In-hospital morbidity was 19.5% in the LS group and 24% in the OS group (P = .25). On propensity score matching, the odds ratio (OR) with 95% confidence interval (CI) was 1.15 (95% CI = 0.65–0.62) for in-hospital mortality, 1.14 (95% CI = 0.7–1.86) for LOS, and 0.99 (CI = 0.6–1.6) for morbidity between the 2 groups and not statistically significant (Table 3).
Table 3.
Comparison of Outcomes between Patients Undergoing LS vs OS
| Outcome | LS | OS | Unadjusted P-Value | Adjusted Analysis |
|
|---|---|---|---|---|---|
| OR | 95% CI | ||||
| In Hospital Mortality | 14.2% | 18% | 0.3 | 1.15 | 0.65−2 |
| Median Post op LOS (Days) | 9 | 8 | 0.62 | 1.14 | 0.7−1.86 |
| Major Complications | 19.5% | 24% | 0.25 | 0.99 | 0.6−1.6 |
On subset analysis of patients with isolated abdominal injuries, the LS group had 52 patients and the OS group had 10,538 patients. Of these patients, the LS group had 6% in hospital mortality compared with 11% in the OS group (P = .23). Median postoperative length of stay was similar in the LS group (8 days) compared with the OS group (7 days) (P = .56). A lower rate of major complications was seen in the LS group (10%) compared with the OS group (15%) (P = .24). On propensity score matching, the ORs (with 95% CIs) were 0.89 for in-hospital mortality (0.21–3.76), 0.69 for LOS (0.21–2.25), and 0.71 for morbidity (0.25–2.00) between the 2 groups and were not significant (Table 4).
Table 4.
Outcomes of Patients with Isolated Abdominal Injuries Undergoing LS vs OS
| Isolated Abdominal Injuries |
Adjusted Analysis |
||||
|---|---|---|---|---|---|
| Outcome | LS | OS | P-Value | OR | 95% CI |
| Number of patients | 52 | 10,538 | |||
| In Hospital Mortality | 6% | 11% | 0.23 | 0.89 | 0.21−3.76 |
| Median Post-op LOS (Days) | 8 | 7 | 0.56 | 0.69 | 0.21−2.25 |
| Major Complications | 10% | 15% | 0.24 | 0.71 | 0.25−2 |
Patients with higher grades of splenic injury were more likely to have a procedure performed within the first 24 hours compared with patients with lower grades (P < .001). OS and LS were performed within the first 6 hours in 82.8% and 59.3% of all splenic trauma cases, respectively. LS was performed in 29.2% of patients past 24 hours compared with 9.5% in the OS group (P < .001). In patients with grade V splenic injuries, 88.5% of patients underwent surgery within the first 6 hours, compared with 6.2% beyond 24 hours (Table 5).
Table 5.
Time to Splenectomy (Hours) in Relation to Grade of Injury and type of Procedure Received
| 0–6H | 6–24H | >24H | |
|---|---|---|---|
| Grade of injury (P < 0.001) | |||
| I–II | 4281 (80.5%) | 469 (8.8%) | 571 (10.7%) |
| III | 446 (78%) | 57 (10%) | 69 (12%) |
| IV | 6118 (81.7%) | 597 (8%) | 770 (10.3%) |
| V | 5922 (88.5%) | 353 (5.3%) | 416 (6.2%) |
| Type of procedure (P < 0.001) | |||
| Open | 21033 (82.8%) | 1951 (7.7%) | 2424 (9.6%) |
| Laparoscopic | 67 (59.3%) | 13 (11.5%) | 33 (29.2%) |
DISCUSSION
The introduction of laparoscopy has revolutionized surgery. It offers many well-documented advantages over open procedures including, but not limited to, decreased postoperative pain, decreased postoperative LOS, minimal blood loss,7 and earlier return to normal function.8 Laparoscopy also offers better exposure, especially of foregut organs such as the spleen, liver, and diaphragm, and similarly allows inspection of the pelvic organs that may not be easily amenable to inspection via open surgery.9 Its use in the trauma setting, however, has been slow. Historically, there were reports of missed injuries possibly due to inability to fully visualize all regions of the abdomen. But, with increased expertise and improvement in laparoscopic equipment and imaging, data have shown that laparoscopic intervention, in the appropriate hand, is very sensitive, specific, and highly accurate.10 Current figures demonstrate an incidence of missed injury of less then 1%, in concordance with an open abdominal exploration, and as a result, it has become more widely embraced in trauma.10 In penetrating diaphragmatic injuries, laparoscopic repair is the preferred option for stable patients.11
The literature on LS in a trauma setting is limited, but there are published reports that demonstrate successful management of trauma patients via LS. Huscher et al12 published a case series on LS, and further reports by Kaul,13 Dissanaike,14 and Basso et al15 all highlighted the successful use of LS when managing patients with a high grade IV or V splenic injuries. Nasr et al16 reported a series of 4 stable patients undergoing delayed LS for blunt trauma with favorable outcomes. Recently, Huang et al17 published a report regarding 11 trauma patients managed via LS and noted similar postoperative courses compared with OS patients.
Various LS approaches have been described in the literature with success. One such approach is the right side down semilateral approach, which is the preferred approach; however, the anterior approach has been used when there was concomitant abdominal viscera injury. The semilateral approach was associated with a superior exposure to the splenic hilum, in which rapid hemostasis can be achieved by stapling across the hilum, thus preventing excessive blood loss.18 Despite this, LS remains a challenging procedure. While it has emerged as the gold standard in elective splenectomies,19 the limited use in the acute setting of trauma implies that LS has perhaps not been as widely embraced by surgeons who are not as comfortable in advanced laparoscopic procedures.
The main reason cited for selecting open intervention in the trauma setting as opposed to laparoscopic surgery was the lack of laparoscopic expertise.20 Current surgery training has seen an increase in the number of laparoscopic procedures being performed, numerous laparoscopic simulators being introduced, and a mandatory laparoscopic curriculum that trainees have to pass before graduating. All of these measures will allow graduates to be more comfortable and facile at laparoscopy compared with their previous peers. However, caution should be maintained when confronted with an injury beyond one's expertise, and subsequent conversion to open procedure should ensue, if necessary, to appropriately deal with the injury.
In this study, there were >27,000 isolated splenectomies that were performed in the US during the period 2007–2015, with the majority being OS. Overall, 0.44% of all the patients who received isolated splenectomy underwent LS. A higher GCS score and systolic BP >140 mm Hg were associated with a greater proportion of LS, whereas a higher ISS score, lower GCS score, and hypotension (systolic BP <90 mmHg) was associated with a greater proportion of OS (Table 2). A 14.2% mortality rate was seen in the LS group, which was comparable to the 18% mortality rate seen in the OS group (Table 3). The mortality rate obtained is reflective of the overall injury burden incurred by the patient and is not attributed to the surgical intervention. There was no statistical difference in mortality between OS and LS. Heuer et al21 studied >13,000 trauma patients, of whom 46.5% underwent splenectomy. The overall in-hospital mortality for their splenectomy patients was 24.8%, which was accounted for by the higher ISS score. Isolated splenic injury patients had a 6% mortality rate in the LS group compared with 10% in the OS group, which was not statistically significant (Table 4). The mortality rates were similar to those from Hamlat et al,22 who looked at >33,000 trauma patients with splenic injuries, of whom 26.2% underwent a splenectomy with a 6.1% in-hospital mortality rate in patients (range 2.1%–9.2%).
Although this study does demonstrate that LS is not inferior to OS, as the 3 major outcomes were not different statistically once matched, an emphasis must be placed on careful selection of patients for LS. Hemodynamically unstable patients should not undergo LS, and OS should remain the intervention of choice for such patients. In a hemodynamically stable patient, nonoperative management has been used for low-grade injuries (grade I–II), whereas surgery is used for higher-grade injuries (grade III-V). With conservative management, the overall nonoperative failure rate varies between 2% and 52%.23 In this retrospective data set, we were unable to elucidate the clinical factors prompting the decision to perform surgery; however, prior reports showed that factors that lead to failure of nonoperative management include age older than 55 years, ISS >25, hemoperitoneum >300 mL, rupture of subcapsular hematoma or intraparenchymal pseudoaneurysms, active contrast extravasation on computed tomography, and delayed bleeding from remodeling.24,25
Failure of nonoperative management was considered in patients who were operated on after 24 hours (Table 5). Overall, 83.6% of the patients underwent splenectomy within the first 6 hours, 7.4% at 6 to 24 hours, and 9.1% of the patients underwent surgical intervention after 24 hours. LS was performed in 29.2% after 24 hours compared with 9.5% of the OS (P < .001). A higher percentage of LS procedures seen after 24 hours may be due to the lesser grade of splenic injury, and a stable patient compared with a higher grade with unstable patient in OS group resulting in earlier surgery. A trend toward earlier splenectomy was associated with a higher grade of splenic injury.
To the best of our knowledge, this study is the largest analysis comparing LS with OS in trauma patients. LS for trauma is being performed at centers across the US, but at a rate of 0.44%. LS is a safe procedure in the trauma setting in a select group of stable patients with adequately trained providers. As surgeons become more experienced and comfortable in laparoscopic techniques, the use of LS in trauma patients is expected to rise. From the results of this study, we advocate that in a hemodynamically stable trauma patient with splenic injury, LS should be entertained by surgeons with the appropriate skills.
We recognize that this study has several limitations. As a retrospective analysis of prospectively collected registry data, our data are limited by the coding of individual trauma centers. Our exclusion criteria ensured that the laparoscopic group contained only LS patients; however, in doing so, it is possible that we likely failed to identify some LS patients who were not coded as such due to the lack of ICD-9 codes for LS. Because of the nature of our data set, we were also unable to assess transfusion needs, postoperative complications such as pain, functional status, bowel recovery, as well as long-term complications such as incisional hernias. Further studies should be performed on a larger scale that analyze the adjusted comparisons between open and laparoscopic approaches to splenectomy in the trauma setting.
CONCLUSION
LS in trauma is a feasible and safe option in expert hands. It has similar outcomes to OS when performed in properly selected patients. Larger studies are needed for better comparison of outcomes.
Contributor Information
Adeel Ahmed Shamim, Department of Surgery, Howard University Hospital, Washington, DC, USA..
Syed Nabeel Zafar, Department of Surgery, University of Maryland, Baltimore, Maryland, USA..
Wasay Nizam, Department of Surgery, Howard University Hospital, Washington, DC, USA..
Ahmad Zeineddin, Department of Surgery, Howard University Hospital, Washington, DC, USA..
Gezzer Ortega, Department of Surgery, Howard University Hospital, Washington, DC, USA..
Terrence Malcolm Fullum, Minimally Invasive Surgery, Department of Surgery, Howard University Hospital, Washington, DC USA..
Daniel Dinh Tran, Minimally Invasive Surgery, Department of Surgery, Howard University Hospital, Washington, DC USA..
References:
- 1. Smith RS, Fry WR, Morabito DJ, et al. Therapeutic laparoscopy in trauma. Am J Surg. 1995;170:632–636; discussion 636–637. [DOI] [PubMed] [Google Scholar]
- 2. Testini M, Girardi A, Isernia RM, et al. Emergency surgery due to diaphragmatic hernia: case series and review. World J Emerg Surg. 2017;12:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Spinelli P, Di Felice G, Pizzetti P, et al. Laparoscopic repair of full-thickness stomach injury. Surg Endosc. 1991;5:156–157. [DOI] [PubMed] [Google Scholar]
- 4. Lachachi F, Moumouni I, Atmani H, et al. Laparoscopic repair of small bowel injury in penetrating abdominal trauma. J Laparoendosc Adv Surg Tech. 2002;12:387–389. [DOI] [PubMed] [Google Scholar]
- 5. Pilgrim CH, Usatoff V. Role of laparoscopy in blunt liver trauma. ANZ J Surg. 2006;76:403–406. [DOI] [PubMed] [Google Scholar]
- 6. Delaitre B, Maignien B. Splenectomy by the laparoscopic approach. Report of a case. Presse Med. 1991;20:2263. [PubMed] [Google Scholar]
- 7. Yong F, Chen W, Lan P, et al. Applications of laparoscopic technique in spleen surgery. Eur Rev Med Pharmacol Sci. 2014;18:1713–1716. [PubMed] [Google Scholar]
- 8. Nyilas A, Paszt A, Simonka Z, et al. Comparison of laparoscopic and open splenectomy. Magy Seb. 2013;66:14–20. [DOI] [PubMed] [Google Scholar]
- 9. El-Bendary YB, Al-Adawi J, Al-Qadhi H. The use of laparoscopy in the management of trauma patients: brief review. Sultan Qaboos Univ Med J. 2016;16:e9–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zafar SN, Onwugbufor MT, Hughes K, et al. Laparoscopic surgery for trauma: the realm of therapeutic management. Am J Surg. 2015;209:627–632. [DOI] [PubMed] [Google Scholar]
- 11. Tserng TL, Gatmaitan MB. Laparoscopic approach to the management of penetrating traumatic diaphragmatic injury. Trauma Case Rep. 2017;10:4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huscher CG, Mingoli A, Sgarzini G, et al. Laparoscopic treatment of blunt splenic injuries: initial experience with 11 patients. Surg Endosc. 2006;20:1423–1426. [DOI] [PubMed] [Google Scholar]
- 13. Kaul A. Laparoscopic splenectomy for a blunt trauma splenic injury in a stable patient. JCR. 2015;5:187–191. [Google Scholar]
- 14. Dissanaike S, Frezza EE. Laparoscopic splenectomy in blunt trauma. J Soc Laparoendosc Surg. 2006;10:499–503. [PMC free article] [PubMed] [Google Scholar]
- 15. Basso N, Silecchia G, Raparelli L, et al. Laparoscopic splenectomy for ruptured spleen: lessons learned from a case. J Laparoendosc Adv Surg Tech A. 2003;13:109–112. [DOI] [PubMed] [Google Scholar]
- 16. Nasr WI, Collins CL, Kelly JJ. Feasibility of laparoscopic splenectomy in stable blunt trauma: a case series. J Trauma. 2004;57:887–889. [DOI] [PubMed] [Google Scholar]
- 17. Huang GS, Chance EA, Hileman BM, et al. Laparoscopic splenectomy in hemodynamically stable blunt trauma. J Soc Laparoendosc Surg. 2017;21(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Podevin G, Victor A, De Napoli S, et al. Laparoscopic splenectomy: comparison between anterior and lateral approaches. J Laparoendosc Adv Surg Tech A. 2011;21:865–868. [DOI] [PubMed] [Google Scholar]
- 19. Somasundaram S, Massey L, Gooch D, et al. Laparoscopic splenectomy is emerging ‘gold standard’ treatment even for massive spleens. Ann R Coll Surg Engl. 2015;97:345–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. O'Malley E, Boyle E, O'Callaghan A, et al. Role of laparoscopy in penetrating abdominal trauma: a systematic review. World J Surg. 2013;37:113–122. [DOI] [PubMed] [Google Scholar]
- 21. Heuer M, Taeger G, Kaiser GM, et al. No further incidence of sepsis after splenectomy for severe trauma: a multi-institutional experience of the trauma registry of the DGU with 1,630 patients. Eur J Med Res. 2010;15:258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hamlat CA, Arbabi S, Koepsell TD, et al. National variation in outcomes and costs for splenic injury and the impact of trauma systems: a population-based cohort study. Ann Surg. 2012;255:165–170. [DOI] [PubMed] [Google Scholar]
- 23. Velmahos GC, Chan LS, Kamel E, et al. Nonoperative management of splenic injuries: have we gone too far? Arch Surg. 2000;135:674–679; discussion 679–681. [DOI] [PubMed] [Google Scholar]
- 24. McIntyre LK, Schiff M, Jurkovich GJ. Failure of nonoperative management of splenic injuries: causes and consequences. Arch Surg. 2005;140:563–568; discussion 568–569. [DOI] [PubMed] [Google Scholar]
- 25. Stassen NA, Bhullar I, Cheng JD, et al. Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(suppl 4):S294–S300. [DOI] [PubMed] [Google Scholar]