Abstract
Background: To better understand health habits in older nurses versus the general population, we sought to determine whether the demographics, health care utilization, and Medicare spending by the Nurses' Health Study (NHS) participants enrolled in Medicare and a matched sample of Medicare beneficiaries meaningfully differed.
Materials and Methods: Analytic cohorts included a random 20% sample of Medicare beneficiaries continuously enrolled in fee for service (FFS) Medicare that were propensity matched to the NHS participants continuously enrolled in FFS Medicare in a single year (2012). Matching was based upon preselected demographic factors and health status, using a nearest-neighbor matching algorithm to obtain a 1:1 match without replacement. Healthcare utilization and spending were compared between the two groups; we also stratified findings by number of chronic comorbidities.
Results: Similar rates of utilization of primary care and most outpatient services. However, NHS participants had slightly higher rates of cancer screening, specialist care, and inpatient surgery were observed. When stratified by comorbidity status, the largest differences in utilization and spending were found in women with no comorbidity.
Conclusions: The modest differences in observed healthcare utilization and spending suggest that older healthcare professionals may access care in fairly similar ways to the general population, and that health status may be a more important determinant of utilization and spending than health profession in older age groups.
Keywords: administrative claims data, generalizability studies, linkage studies, healthcare spending, healthcare utilization, Nurses' Health Study
Introduction
The Nurses' Health Study (NHS) was initiated in 1976 to prospectively examine factors that influence women's health, including cancers.1–3 Registered nurses were selected for several reasons, notably the reliability of their contact for follow-up questioning, and their ability to provide complete and accurate information about health. The first questionnaires were mailed to female, registered married nurses between the ages of 30 and 55 years living in 1 of 11 United States states.4
As the study participants aged over time, most subsequently enrolled in Medicare, now permitting linkage of their epidemiologic data with administrative claims to study how behaviors and events are related to healthcare utilization and health outcomes. Moreover, these combined data sources could uniquely provide insight into health and healthcare utilization of an aging cohort of current and former nurses, whose former experiences as direct providers of care and as participants of the medical decision-making team may influence their utilization later in life. In addition, the NHS has 40 years of longitudinal information on self-reported health and health-related characteristics that could be useful to investigate late life health status and treatments that is not otherwise possible for the general population.
We questioned whether there would be differences in baseline demographics and health status between the NHS participants and the general population and (after adjusting for these identifiable sources of bias) whether nurses used and spent on healthcare differently than a similarly aged sample of the general population. Any findings would inform our ability to generalize the unique longitudinal data of an NHS–Medicare linkage to non-nurse populations. For example, prior studies on NHS participants' health status have shown that while nurses have a lower mean body mass index and less prevalent smoking histories, their incidence of breast cancer appears similar to that of the general population.5 To answer this question, we compared NHS participants' demographics, and their use of healthcare as derived from Medicare claims data to a randomly selected and propensity-matched sample of similarly aged women in the Medicare fee for service (FFS) population.
Materials and Methods
Our investigation of healthcare utilization for women participating in the NHS cohort who were aged 65 years or older in 2012 began with the linkage of two data sources: Medicare FFS claims data and the NHS cohort data. A comparison cohort consisted of American women from the general population, drawn from a 20% national sample of Medicare beneficiaries. This study was approved by Institutional Review Boards at Brigham and Women's Hospital and Dartmouth College.
Data sources
Nurses' Health Study
The NHS is based at Brigham and Women's Hospital in Boston, MA in the Channing Division of Network Medicine. The initial cohort was identified in 1976, when 121,700 female, registered nurses, aged 30–55 years living in 1 of 11 states, returned a mailed questionnaire to collect health and lifestyle information. The nurses have since migrated to all 50 states. Follow-up is conducted every 2 years via mailed questionnaires, spanning 40 years to date. Follow-up rates through this period remain in excess of 90%.
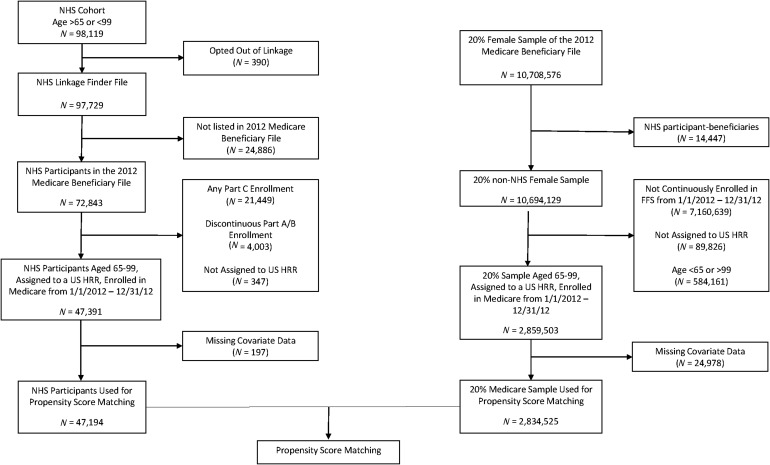
Medicare linkage
The construction of the NHS–Medicare linked cohort is summarized in Figure 1. As of January 1, 2012, 97,729 active NHS participants were alive and 65 years or older, therefore eligible for Medicare. In August 2013, NHS participants were notified of the planned Medicare linkage and were given the option to “opt-out” of this research; 390 (0.4%) women opted out. Of NHS participants, 47,391 were assigned to a United States hospital referral region (HRR) and enrolled in FFS Medicare Parts A or B for the entirety of 2012. After excluding women with missing covariate data, 47,194 NHS participants comprised the cohort for which a matched sample of Medicare beneficiaries was drawn. We compared these two groups of NHS participants and found that between the 25,452 women ineligible for the linkage and those who were eligible for linkage, there were few meaningful differences in measured demographics and employment, aside from geographic dispersion. A greater proportion of the FFS NHS participants (25%) reside in the Southern United States census region as opposed 15% of the non FFS participants (Supplementary Table S1; Supplementary Data are available online at www.liebertpub.com/jwh).
FIG. 1.
Construction of the analytic cohort.
Medicare 20% random sample
The comparator Medicare cohort of women was derived from a random 20% sample of all Medicare beneficiaries in the United States. For this study, we restricted our analysis to the 10,708,576 female Medicare beneficiaries and removed 14,447 NHS participants from this initial sample. After aligning their ages to the NHS participants (e.g., women between 65 and 99 years old), assigning them to a United States HRR, and ensuring they were enrolled for 12 continuous months, or until death, of Part A and B FFS coverage in the Medicare Beneficiary Summary file the final cohort used for propensity matching consisted of 2,834,525 women (Fig. 1).
Outcome measures
We characterized healthcare utilization for preventive, outpatient and inpatient services using 2012 inpatient (Medicare Provider Analysis and Review file [MedPAR]), professional service claims (Physician/Supplier Part B file) and outpatient files. We also report on overall Medicare spending in 2012.
Preventive testing
Preventive tests included the mean annual per capita utilization for common diagnostic tests for cancer and osteoporosis screening. We specifically determined use of mammography, colonoscopy, sigmoidoscopy, barium enema, fecal occult blood testing, and dual-energy x-ray absorptiometry (DEXA) bone densitometry. Though unique procedural codes exist for screening versus diagnostic intent for some of the tests (e.g., mammography), we could not be certain regarding the intent of the testing performed for all tests. Therefore, we report the proportions of women who underwent at least one examination by type regardless of diagnostic intent.
Outpatient services
Outpatient physician services as derived from Part B data included emergency room visits not leading to hospitalization and other ambulatory care visits by primary care and specialty providers. These along with inpatient services are reported as rates per 1,000 women.
Inpatient services
Medicare Part A data were used to determine inpatient utilization on the basis of discharges for medical conditions, surgical conditions, and ambulatory care sensitive conditions.
Medicare spending
Medicare spending was assessed in three categories: (1) All inpatient facility spending, which was obtained from the MedPAR file, (2) Part B professional services spending, which was derived from Carrier file, and (3) total spending. Total spending was derived from the MedPAR file, Carrier file, home health, hospice, durable medical equipment, and other facility claims data files. Spending was then standardized to adjust for regional differences in Medicare reimbursement due to cost of living, disproportionate share, graduate medical education, and hospital payments.6
Matching factors
Since we were primarily interested in understanding healthcare utilization in nurses versus the general population, independent of demographic factors that we know influence healthcare utilization (i.e., age, race/ethnicity, geographic location, etc.), we matched NHS participants and our general population sample according to several characteristics. From the Medicare Beneficiary Summary file, beneficiaries' age, race/ethnicity, Medicare–Medicaid dual eligibility, mortality status, and ZIP code of residence were extracted for analysis. ZIP codes were used to obtain 2012 United States Census Tract median household income and to identify HRR, which are geographically defined health care markets.7,8 In addition, since health status obviously influences health care utilization, each woman's number of chronic conditions was assessed using the Elixhauser comorbidity score, a validated aggregate measure of an individual's chronic comorbid illness based on claims data diagnosis codes annually updated by the Agency for Healthcare Research and Qualty.9–11 These variables were then included in the statistical propensity-matching model described below, and these were also used to stratify participants by comorbid illness to understand whether underlying health status influenced results.
Statistical analysis
Descriptive analysis of differences between NHS and the 20% Medicare sample of women were compared using either two-sided t-tests (for continuous variables) or chi-squared tests (for categorical variables). Given expected and observed imbalances in factors such as socioeconomics and demographics between the nurses and the general population, propensity score matching was then used to balance observable factors between the study populations. Scores were estimated by using logistic regression to determine the likelihood that a woman would have participated in the NHS, based upon the covariates listed above.
Propensity score matching was performed using a nearest-neighbor matching algorithm to obtain a 1:1 match without replacement between NHS participants and the general 20% sample of women from the Medicare population. The match was done using an optimal caliper equal to 0.2 times the standard deviation of the logit of the propensity scores to match the logit of the propensity scores.12 A 100% match was obtained. Finally, the balance in the observable confounders between the NHS participants and the matched cohort from the 20% sample was verified by calculating the standardized difference of means for each factor in the two groups, both before and after matching. A standardized difference greater than or equal to 0.10 is considered large enough for cohorts to be unbalanced for that factor.12
After the match and initial analysis, the match was assessed using sensitivity analyses by eliminating first the use of HRR then substituting individual disease flags for the Elixhauser composite score. Neither sensitivity analysis improved the fit, so both the HRR and Elixhauser score were used in the regression and propensity matching model. After propensity score matching was complete, outcomes of interest for the NHS and the 20% Medicare sample of women were again compared using either two-sided t-tests (for continuous variables) or chi-squared tests (for categorical variables). Since we planned further analyses stratified by Elixhauser score (to explore healthcare utilization according to health status), we confirmed that within the individual strata of Elixhauser score (reflected by Elixhauser scores of 0, 1–2 and 3+), propensity matching did not introduce statistical imbalances in demographics of NHS versus the general population. Therefore, we were able to examine resource utilization by comorbidity subgroups of none, few, or several chronic conditions. Analyses were conducted using Stata v14.1 (College Station, TX) and SAS v9.4 (Cary, NC).
Results
Participant characteristics
As of January 1, 2012, 47,194 of the NHS participants had a corresponding record in the Medicare Beneficiary Summary File (Fig. 1). Before matching based upon known covariates, the NHS participants and Medicare beneficiaries were similar in age and comorbid disease burden, though the nurses differed from the Medicare beneficiaries on distributions of race, socioeconomic status, and geographic distribution (Table 1). Roughly one quarter of NHS participants and Medicare beneficiaries had no comorbid illness, and another quarter had a single diagnosis. For women (including both NHS participants and the Medicare beneficiaries) with three or more diagnoses, the average number of diagnoses was 4.5. There were no significant differences in the two groups of womens' count of comorbidities before or after propensity score matching. Before matching, there were more Caucasians among the NHS sample, NHS participants lived in zip codes of higher median income and more NHS participants lived in the Northeast. A smaller proportion of NHS participants had diabetes than the general population of medicare beneficiaries (14.8% vs. 19.4%).
Table 1.
Characteristics of the Nurses' Health Study Participant and Medicare Control Cohorts, Before and After Propensity Score Matching
| Covariate | NHS participants | Medicare controls (before matching) | Medicare controls (after matching) | Std. differencea(after matching) |
|---|---|---|---|---|
| N | 47,194 | 2,834,525 | 47,194 | |
| Age as of January 1, 2012, mean (std) | 76.6 (6.8) | 76.1 (8.1) | 76.5 (7.5) | 0.02 |
| Race, N (%) | ||||
| White | 46,036 (97.6) | 2,457,989 (86.7) | 46,242 (98.0) | −0.03 |
| Black | 696 (1.5) | 218,150 (7.7) | 588 (1.3) | 0.03 |
| Other | 438 (0.9) | 111,084 (3.9) | 345 (0.7) | 0.02 |
| Hispanic | 24 (0.1) | 47,302 (1.7) | 19 (0.0) | 0.01 |
| Socioeconomic status | ||||
| Dual eligible, N (%) | 1,187 (2.5) | 490,890 (17.3) | 948 (2.0) | 0.04 |
| Median income,b mean (std) | $66,374 ($24,724) | $57,438 ($23,030) | $66,264 ($25,302) | 0.01 |
| Census region, N (%) | ||||
| Northeast | 22,517 (47.7) | 552,404 (19.5) | 22,118 (46.9) | 0.02 |
| South | 11,832 (25.1) | 1,085,094 (38.3) | 12,253 (26.0) | −0.02 |
| Midwest | 7,044 (14.9) | 695,434 (24.5) | 7,106 (15.1) | 0.00 |
| West | 5,801 (12.3) | 501,593 (17.7) | 5,717 (12.1) | 0.00 |
| Health status | ||||
| Elixhauser comorbidity count = 0, N (%) | 11,962 (25.4) | 780,034 (27.5) | 12,637 (26.8) | −0.03 |
| Elixhauser comorbidity count = 1–2, N (%) | 21,211 (44.9) | 1,174,156 (41.4) | 21,977 (46.6) | −0.03 |
| Elixhauser comorbidity count ≥3, N (%) | 14,021 (29.7) | 880,335 (31.1) | 12,580 (26.7) | 0.07 |
| Overall Elixhauser comorbidity count, mean (std) | 1.98 (2.1) | 2.00 (2.1) | 1.79 (1.8) | 0.05 |
| Comorbidity count if Elixhauser count ≥3 mean (std) | 4.51 (1.9) | 4.52 (1.8) | 4.22 (1.6) | 0.09 |
Demographic and health status data before and after propensity score matching are displayed above.
Standardized difference after propensity score matching is calculated as the standardized difference of means between the two groups. Absolute values greater than or equal to 0.10 were interpreted as a statistically significant difference between the two cohorts.
Median income is derived from patient zip code, not individual level data.
NHS, Nurses' Health Study.
Utilization of health services
Preventive testing
Overall, we found fairly similar utilization of health screening among nurses and the general population (Table 2). The greatest absolute difference in testing, nearly 10%, was observed for mammography: 53% of NHS participants had a mammogram in 2012, compared with 44% of matched Medicare beneficiaries. Bone densitometry was also slightly more frequent in the NHS cohort (3% higher than the matched Medicare beneficiaries). When we examined mammography and densitometry prevalence by strata of chronic condition count, we found that the differences in mammography between the nurses and the general population became less pronounced as the comorbidity count increased. For women without any comorbid conditions, the mammography rate was 13.7% higher than the matched Medicare beneficiaries. For women with three or more comorbid conditions, this rate was 7.3% higher (Supplementary Fig. S1A). A similar trend was observed with densitometry (Supplementary Fig. S1B).
Table 2.
2012 Utilization of Healthcare Resources by Nurses' Health Study Participants and Matched Medicare Beneficiaries
| Utilization category | NHS participants (N = 47,194) | Matched Medicare cohort (N = 47,194) | p-Value | Total difference in utilizationa(95% CI) | Relative differencebin utilization (%) |
|---|---|---|---|---|---|
| Preventive testing (percentage of women undergoing a test in 2012) | |||||
| Mammogram | 53.2 (52.8–53.7) | 43.8 (43.3–44.2) | <0.01 | 9.5 (8.8–10.1) | 22 |
| Colonoscopy | 7.8 (7.5–8.0) | 7.0 (6.8–7.2) | <0.01 | 0.8 (0.4–1.1) | 11 |
| Flexible sigmoidoscopy | 0.4 (0.3–0.5) | 0.4 (0.3–0.4) | 0.43 | 0.0 (0.0–0.1) | 9 |
| Barium enema | 0.2 (0.2–0.3) | 0.2 (0.2–0.3) | 0.89 | 0.0 (−0.1 to 0.1) | −2 |
| Fecal occult blood testing | 1.8 (1.7–1.9) | 1.6 (1.5–1.8) | 0.10 | 0.1 (0.0–0.3) | 8 |
| DEXA bone densitometry | 17.3 (16.9–17.6) | 14.7 (14.4–15.0) | <0.01 | 2.6 (2.1–3.0) | 17 |
| Outpatient service rates (per capita) | |||||
| ER visitsc | 1.1 (1.1–1.1) | 1.1 (1.1–1.1) | <0.01 | −0.02 (−0.03 to 0.01) | −2 |
| Primary care E/Md visits | 3.8 (3.8–3.9) | 3.9 (3.8–3.9) | 0.16 | 0.0 (−0.1 to 0.0) | −1 |
| Specialty care E/M visits | 5.6 (5.5–5.6) | 4.9 (4.8–4.9) | <0.01 | 0.7 (0.6–0.8) | 14 |
| Total E/M visits | 9.4 (9.3–9.5) | 8.7 (8.7–8.8) | <0.01 | 0.7 (0.6–0.8) | 7 |
| Inpatient service rates (per 1,000) | |||||
| Medical discharges | 191 (186–197) | 175 (169–180) | <0.01 | 17 (9–24) | 10 |
| Surgical discharges | 89 (87–92) | 72 (70–75) | <0.01 | 17 (13–21) | 24 |
| Total discharges | 281 (274–288) | 247 (241–253) | <0.01 | 34 (25–43) | 14 |
The total difference in utilization is calculated as follows: (Utilization by NHS participants) – (Utilization by matched Medicare cohort). Negative numbers indicate less utilization by NHS participants than Medicare controls.
Relative difference in utilization is calculated: (Total difference in utilization)/(Utilization by NHS participants). Negative numbers indicate less utilization by NHS participants than Medicare controls.
ER visits not leading to inpatient admission.
Evaluation and management.
CI, confidence interval; DEXA, dual-energy x-ray absorptiometry; E/M, evaluation and management; ER, emergency room.
Outpatient services
There were modest differences in use of the outpatient service rates of NHS participants and the matched Medicare beneficiaries. Both groups visited primary care physicians about four times in 2012 and required emergency care once (Table 2). In sum, NHS participants ended up visiting, on average, one more physician in 2012 than matched Medicare beneficiaries (10.4/year for NHS participants vs. 9.3 for Medicare beneficiaries). This was due to, on average, one extra NHS participant visit with a medical specialist. This difference was observed across all three strata of comorbidity counts (Supplementary Fig. S2).
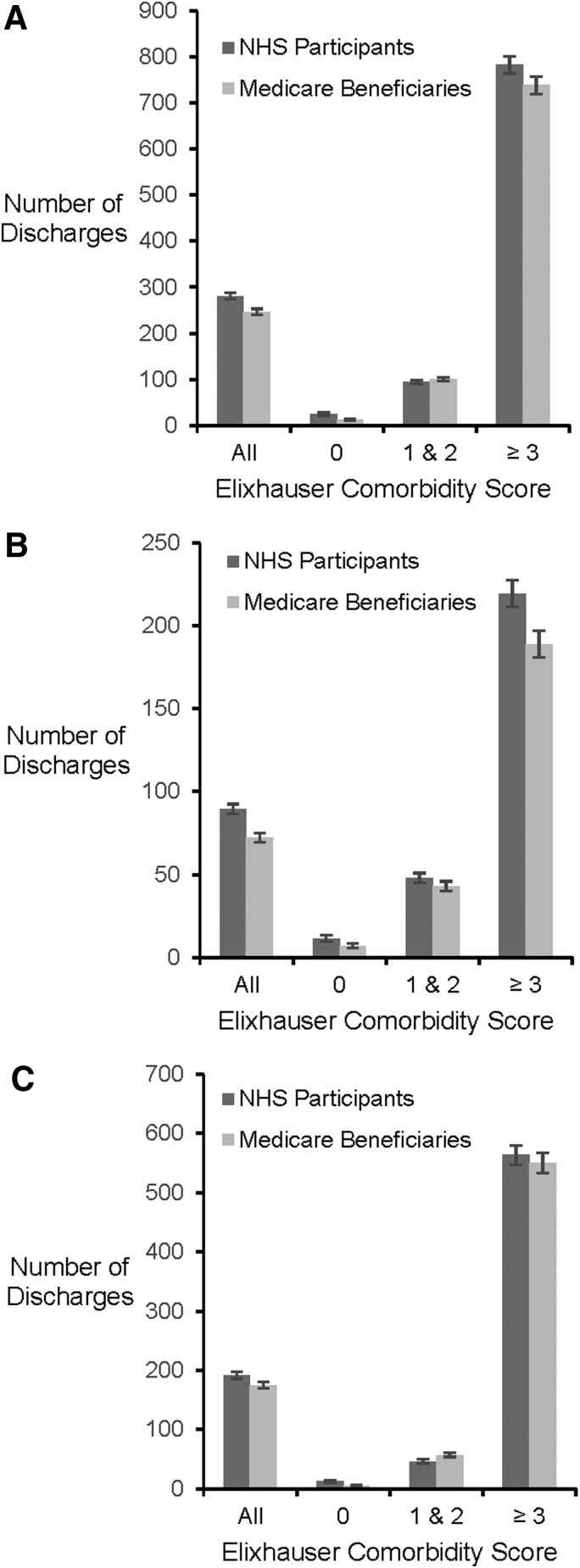
Inpatient services
Overall inpatient rates were higher among NHS participants (Table 2). In 2012, there were 281 discharges per 1,000 NHS participants, compared with 247 discharges among the same number of matched Medicare beneficiaries (Fig. 2A). When these differences were examined according to chronic condition subgroups, the most pronounced difference was observed for surgical admissions for women with at least three comorbidities (Fig. 2B). There were 219 surgical discharges per 1,000 NHS participants in this group, compared with 189 discharges for the matched Medicare beneficiaries, a difference of 30 discharges per 1,000 women. Less frequent inpatient utilization for medical diagnoses was observed among the NHS participants with 1–2 chronic comorbid conditions (Fig. 2C), a difference of 11 per 1,000 women.
FIG. 2.
(A) Inpatient discharges by NHS participants and matched Medicare controls in 2012. Inpatient discharges depicted as the total number of inpatient discharges (both medical and surgical) per 1,000 women. Data are stratified by chronic comorbidity count. (B) Surgical discharges by NHS participants and matched Medicare controls in 2012. Surgical discharges per 1,000 women. Data are stratified by chronic comorbidity count. (C) Medical discharges by NHS participants and matched Medicare controls in 2012. Medical condition discharges per 1,000 women. Data are stratified by chronic comorbidity count. NHS, Nurses' Health Study.
Medicare spending
Greater utilization of healthcare services among NHS participants translated into higher spending (Table 3). The mean total spending per NHS participant in 2012 was $10,138 compared with $8,904 among matched Medicare beneficiaries. The marginal spending by the NHS participants was largely derived from hospital-based and professional services, which ranged between 12% and 18% more than the general population.
Table 3.
2012 Spending by Nurses' Health Study Participants and Matched Medicare Beneficiaries
| Spending category | NHS participants (N = 47,194) | Matched Medicare cohort, = (N = 47,194) | p-Value | Total difference in spendinga(95% CI) | Relative differencebin spending (%) |
|---|---|---|---|---|---|
| Mean standardized Medicare spending (95% CI) | |||||
| Total | $10,138 ($9,970–$10,306) | $8,904 ($8,751–$9,057) | <0.01 | $1,234 ($1,006–$1,461) | 14 |
| Inpatient hospital | $3,889 ($3,776–$4,001) | $3,344 ($3,239– $3,449) | <0.01 | $545 ($391–$699) | 16 |
| Outpatient hospital | $1,344 ($1,308–$1,381) | $1,142 ($1,113–$1,172) | <0.01 | $202 ($155–$249) | 18 |
| Professional services | $3,901 ($3,848–$3,954) | $3,469 ($3,423–$3,514) | <0.01 | $432 ($363–$502) | 12 |
| Durable medical equipment | $204 ($190–$219) | $193 ($176–$210) | 0.31 | $12 (−$11 to $34) | 6 |
| Hospice | $333 ($302–$364) | $287 ($257–$317) | 0.03 | $46 ($3–$89) | 16 |
| Home health Agency | $467 ($450–$484) | $470 ($453–$486) | 0.80 | −$3 (−$27 to $21) | −1 |
| Part B professional services (95% CI) | |||||
| E/M visits | $1,416 ($1,401–$1,432) | $1,299 ($1,285–$1,313) | <0.01 | $117 ($97–$138) | 9 |
| Procedures | $1,120 ($1,102–$1,138) | $988 ($970–$1,007) | <0.01 | $132 ($106–$157) | 13 |
| Laboratory tests | $380 ($375–$386) | $349 ($344–$354) | <0.01 | $31 ($24–$38) | 9 |
| Imaging studies | $358 ($353–$362) | $328 ($324–$333) | <0.01 | $29 ($23–$36) | 9 |
| Durable medical Equipment | $628 ($592–$661) | $504 ($477–$530) | <0.01 | $123 ($80–$166) | 24 |
Data are displayed as the excess in spending of NHS participants above matched Medicare controls, both overall and according to Elixhauser health status.
The difference in spending is calculated: (Spending by NHS participants) − (Spending by matched Medicare cohort). Negative numbers indicate less spending by NHS participants than Medicare controls.
Relative difference in spending is calculated as: (Total difference in spending/spending by NHS participants). Negative numbers indicate lower spending by NHS participants than Medicare controls.
To determine the degree to which comorbidity counts influenced differences in spending, the women were stratified accordingly, as above with utilization (Supplementary Table S2). In the nurses and the matched Medicare beneficiaries, spending was higher as the number of chronic comorbid conditions increased. In general, the greatest proportionate differences in spending comparing NHS and general population beneficiaries was in the group with no comorbidities, although this did not equate to a substantial absolute difference. For example, total spending among NHS participants without any comorbidities was $2,915 compared with $2,259 (p < 0.01) among matched Medicare beneficiaries (a relative difference of 29%).
In contrast, overall spending and the differences in spending between NHS participants and matched Medicare beneficiaries with at least three comorbidities was higher in absolute terms, while relative differences were no greater than 10%. For example, spending among NHS participants with at least three comorbid conditions was $22,704, compared with the $21,200 spent (p < 0.01) by matched Medicare beneficiaries (a relative difference of 7.1%).
Discussion
We compared healthcare utilization and spending among 47,194 NHS participants, propensity matched to the same number of Medicare FFS female beneficiaries. Before matching, the nurses were less racially diverse and lived in higher income areas, which was characteristic of the nursing profession in the 1970s when the cohort was established. Propensity score matching mitigated the observed differences in race, income, and geographic region. Both before and after matching, the overall count of the women's chronic conditions remained similar.
We found that, in general, the utilization and spending patterns were fairly similar between the two groups. However, for certain services, such as preventive testing, specialty care, and inpatient surgery, there was a pattern of greater utilization and spending among the NHS participants compared with the general Medicare sample. This pattern was most pronounced among women with no medical comorbidities and the magnitude of the difference decreased as the comorbidity count increased.
Our findings partially confirm those of a 2011 report released by Thomson Reuters, which demonstrated that 1.1 million U.S. hospital workers were costlier than 17.8 million health plan members from various nonhealth care industries.13,14 While the reasons for the observed utilization and spending differences are uncertain, possible mechanisms may stem directly from nurses' training and occupational experience. These factors may combine to heighten nurses' awareness of symptoms and lower threshold to seek diagnosis and/or treatment, especially when they are healthier. Furthermore, it is likely that increased health literacy and access improves completion of preventative services. A nurse's estimated median income of nearly $70,000 per year15 may also enable higher utilization and spending, as healthcare spending is known to directly correlate with income.16 While we used propensity score matching to address socioeconomic imbalances, our correction was imputed from geographic area, not individual income, so income differences may still partially confound the comparisons of nurses to the general population.
We also found that the relative differences in utilization and spending between nurses and other beneficiaries were mostly focused on the healthiest women with no comorbidities, and that once health began to deteriorate care patterns among women with higher levels of comorbidity became more similar. One potential explanation for this finding is that discretionary use of healthcare services may be more sensitive to differences in knowledge, access, or income. Such discretionary healthcare spending dominates total healthcare spending when there are few other essential services required, and decreases when most of the healthcare dollar is spent on essential—as opposed to elective or preventive—care. Ultimately, however, this explanation remains a conjecture as we cannot know whether specific conditions or situations accounted for the patterns we observed.
Study limitations warrant consideration. First, our findings were derived from nurses and Medicare beneficiaries enrolled in FFS Medicare. Women under the age of 65, those not enrolled in FFS, or those enrolled in Medicare Advantage (Part C) plans were excluded and thus we cannot generalize our findings to these groups. Second, the health status of the nurses and that of the Medicare cohort was estimated from claims data. Other health measures such as health-related quality of life or smoking history cannot be reflected in these data. Third, our findings support an association between being a nurse and utilization without the explicit finding of a causal link. In other words, the observed differences in healthcare utilization are associated with, though not necessarily due to occupational exposures encountered among nursing professionals. Finally, since we were interested in evaluating how health professionals utilize healthcare, rather than in evaluating how socioeconomic status or race/ethnicity may influence spending, we used propensity matching to reduce such differences between the nurse and general population groups. However, propensity matching is an imperfect means to eliminate potential sources of bias, as it can only be performed on identified variables. Thus some of the differences we found in healthcare utilization and spending might be explained by socioeconomic status and other unmeasured variables rather than by being a nurse.
Conclusions
These linked data provide health care utilization and spending details for nearly 50,000 participants in the NHS. While the demographics of the nurses differed from female Medicare beneficiaries of similar age, propensity score matching mitigated the observed differences in demographics without affecting the observed baseline similarities counts of chronic comorbid conditions. After accounting for these differences, the resultant healthcare utilization and spending was slightly higher for elective and preventive services among NHS participants, and the higher utilization among nurses compared with Medicare beneficiaries was most pronounced among women without medical comorbidities. Future research will seek to understand specific factors that underlie these differences.
Supplementary Material
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Colditz GA, Manson JE, Hankinson SE. The nurses' health study: 20-Year contribution to the understanding of health among women. J Womens Health 1997;6:49–62 [DOI] [PubMed] [Google Scholar]
- 2. Morabia A. 120,000 Nurses who shook public health. Am J Public Health 2016;106:1528–1529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bao Y, Bertoia ML, Lenart EB, et al. Origin, methods, and evolution of the three nurses' health studies. Am J Public Health 2016;106:1573–1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Belanger CF, Hennekens CH, Rosner B, Speizer FE. The nurses' health study. Am J Nurs 1978;78:1039–1040 [PubMed] [Google Scholar]
- 5. Colditz GA, Hankinson SE. The nurses' health study: Lifestyle and health among women. Nat Rev Cancer 2005;5:388–396 [DOI] [PubMed] [Google Scholar]
- 6. Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don't drive regional Medicare spending variations. Health Aff (Millwood) 2010;29:537–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Aff (Millwood) 2002;Suppl Web Exclusives:W96–W114 [DOI] [PubMed] [Google Scholar]
- 8. The Dartmouth Atlas of Health Care. Research methods, 2017. Available at: www.dartmouthatlas.org/tools/faq/researchmethods.aspx Accessed March16, 2017
- 9. Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res 2008;8:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Menendez ME, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res 2014;472:2878–2886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care 2012;50:1109–1118 [DOI] [PubMed] [Google Scholar]
- 12. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009;28:3083–3107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Thomson Reuters. Sicker and Costlier: Healthcare utilization of US hospital employees, 2011. Available at: www.chime.org/CHA/assets/File/advocacy/employee-health/toolkits/H_PAY_EMP_1108_10237_HHE_Report_WEB.pdf Accessed March10, 2017
- 14. Sherman D. Hospital workers outspend others on medical care., 2011. Available at: www.reuters.com/article/us-workers-outspend-idUSTRE78B45020110912 Accessed March10, 2017
- 15. Bureau of Labor Statistics, U.S. Department of Labor. Occupational outlook handbook, 2016–2017 edition, registered nurses. Available at: https://bls.gov/ooh/healthcare/registered-nurses.htm Accessed January06, 2017
- 16. Bureau of Labor Statistics, U.S. Department of Labor. A look at healthcare spending, employment, pay, benefits, and prices, 2016. Available at: https://bls.gov/spotlight/2016/a-look-at-healthcare-spending-employment-pay-benefits-and-prices/pdf/a-look-at-healthcare-spending-employment-pay-benefits-and-prices.pdf Accessed December30, 2016
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.