Abstract
Hypertensive emergency is a clinical entity with potentially serious health implications and high healthcare utilization. There is a lack of nationally representative data on incidence, causes, and predictors of 30-day readmission after hospitalization for hypertensive emergency. We used the 2013–2014 Nationwide Readmissions Database to identify index hospitalizations for hypertensive emergency. Primary outcome was all-cause unplanned 30-day readmission. Multivariable hierarchical logistic regression was used to identify independent predictors of readmission. There were 166,531 index hospitalizations for hypertensive emergency representative of 355,627 (standard error 9,401) hospitalizations nationwide in 2013–2014. Mean age was 66.0 (standard error 0.14) years and 53.7% were women. The overall incidence of unplanned 30-day readmissions was 17.8%. The most common causes of readmission were heart failure (14.2%), hypertension with complications (10.2%), sepsis (5.9%), acute kidney injury (5.1%), and cerebrovascular accident (5.1%). Non-cardiovascular causes accounted for 57.9% of readmissions. We found age<65 years (odds ratio 1.21, 95% CI 1.17–1.25, p<0.001), female sex (odds ratio 1.09, 95% 1.07–1.12, p<0.001), comorbid disease burden, substance use disorders, and socioeconomic risk factors to be significant predictors of readmission. One out of six patients hospitalized for hypertensive emergency had an unplanned 30-day readmission. Heart failure, uncontrolled hypertension, and stroke were among the most frequent causes of readmission, however over half of all readmissions were due to non-cardiovascular causes.
Keywords: blood pressure, cardiovascular disease, hospital readmissions, hypertension, outcomes research
Introduction
Hypertension affects nearly half of all US adults and is responsible for substantial burden of morbidity, mortality, and financial costs on the healthcare system. 1 The 2017 American College of Cardiology / American Heart Association High Blood Pressure guidelines are expected to increase the awareness of hypertension in the US, especially among young adults.2 Hypertensive emergency is a complication of uncontrolled hypertension and is defined as acute severe hypertension with evidence of target end organ damage.3 Approximately 1–2% of adults with hypertension will develop hypertensive emergency in their lifetime and the incidence of hypertensive emergency has increased over the last decade.4,5 There is a paucity of data on 30-day readmission rates after hospitalization for hypertensive emergency. In this study using a national administrative database, we evaluated the incidence, causes and predictors of 30-day readmissions after hospitalization for hypertensive emergency.
Methods
Data Source
Data used in this study as well as methods to analyze these data are published annually by the Agency for Healthcare Research and Quality. Datasets, analytic methods, and study materials used in the study will not be made available to other researchers by the study authors but can be obtained from the Healthcare Cost and Utilization Project database catalogue. We used the 2013–2014 Nationwide Readmissions Database (NRD), which is a part of the Healthcare Cost and Utilization Project from the Agency for Healthcare Research and Quality.6,7 The NRD is an all-payer national database of inpatient hospital stays that can be used to generate nationally representative estimates of readmission rates in the US.8 The NRD is composed of discharges included in the State Inpatient Databases (SID) of participating states. Twenty-one states participated in the 2013 NRD and 22 states in the 2014 NRD. Approximately 85% of all discharges from SIDs of participating states have been included in the 2013–2014 NRD.6,7 There are approximately 15 million unweighted yearly discharges representative of approximately 35 million discharges nationwide. Individual patients can be tracked across hospitalizations by a patient linkage variable. The study was exempt from Institutional Review Board approval from the primary institution because the study utilized a publicly available database containing de-identified patient level data.
Identification of cases
Hypertensive emergency hospitalizations were defined as records with primary or secondary diagnosis codes for acute hypertension and at least one additional diagnosis code for end-organ damage (Table 1) (Figure 1). This approach for identification of hypertensive emergency is similar to a prior study using an administrative database.4
Table 1:
Diagnosis codes used to define the study population
| Variables used to define the study population | ICD-9 codes used |
|---|---|
| Codes for acute hypertension | |
| Primary malignant hypertension | 401.0 |
| Secondary malignant hypertension | 405.01 and 405.09 |
| Malignant hypertensive heart or kidney disease | 402.00, 402.01, 403.00, 403.01, 404.00, 404.01, 404.02, 404.03 |
| Codes for end-organ damage | |
| Retinal hemorrhage | 362.81 |
| Papilledema with increase intracranial pressure | 377.01 |
| Acute on unspecified (not chronic) heart failure | 428.0, 428.1, 428.20, 428.21, 428.23, 428.30, 428.31, 428.33, 428.40, 428.41, 428.43, 428.9 |
| Acute myocardial infarction | 410.x, 410.xx |
| Ruptured aortic aneurysm or aortic dissection | 414.12, 443.21, 443.22, 443.23, 443.24, 443.29, 441.x |
| Subarachnoid hemorrhage | 430.x |
| Intracerebral hemorrhage | 431.x |
| Hypertensive encephalopathy | 437.2 |
| Non-traumatic extradural hemorrhage | 432.x |
| Cerebral thrombosis | 434.x |
| Transient cerebral ischemia | 435.x |
| Other cerebrovascular disease | 436.x |
Figure 1:
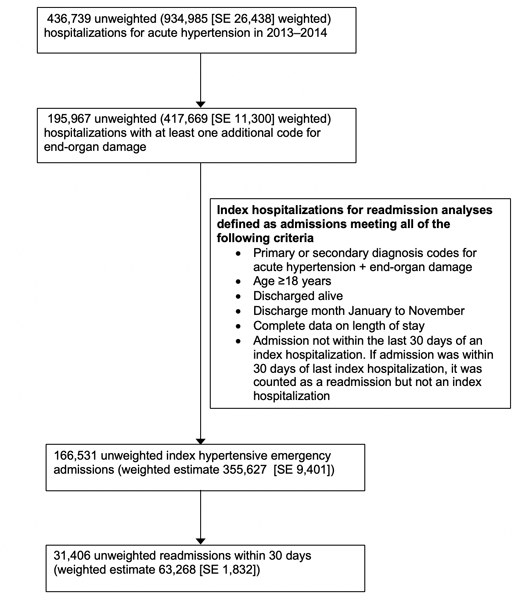
Selection of index hospitalizations for hypertensive emergency in the 2013–2014 Nationwide Readmissions Database. SE stands for standard error.
Outcome measures
Primary outcome was unplanned all-cause 30-day readmission. Causes of readmission were ascertained using Clinical Classification Software codes in the primary diagnosis field. The cause of readmission was designated as cardiovascular if ICD-9 codes for the principal diagnosis of readmission fell within the range 390–459 (Diseases of the circulatory system).
Sensitivity Analysis
We performed a sensitivity analysis to ascertain whether our results were sensitive to a more restrictive definition of hypertensive emergency. This subsample for sensitivity analysis was defined as index admissions with a primary or a secondary diagnosis code of acute hypertension with an additional primary or secondary diagnosis code of acute heart failure, hypertensive encephalopathy, or papilledema. All other criteria used to define the subsample for sensitivity analysis were identical to that used for the full study sample. Using this subsample of index admissions, we ascertained incidence, causes, and predictors of unplanned all-cause 30-day readmission, similar to the primary analysis.
Statistical Analysis
We used survey analysis techniques to account for data clustering and stratification. Differences in continuous variables were tested using linear regression while differences in categorical variables were tested using logistic regression. Univariable and multivariable hierarchical logistic regression models were used to identify independent predictors of readmission. We included a hospital-level random intercept to account for within hospital correlation in 30-day readmission risk. Hierarchical models were unweighted as per the recommendations of the Agency for Healthcare Research and Quality for conducting hierarchical modeling using Healthcare Cost and Utilization Project data.9 Improvement in model fit from the null model was tested by a change in Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) compared with the null model. Lower values of AIC and BIC for the full model are supportive of an improvement in model fit compared with the null model. A p-value of ≤0.05 was considered significant. All analyses were conducted using Stata MP 15.1 (Stata Corp, College Station, TX).
Results
Baseline characteristics and outcomes of index hospitalization
There were 195,967 unweighted hospitalizations for hypertensive emergency representative of 417,669 (standard error [SE] 11,300) hospitalizations nationally. Of these, 3.8% died during the initial hospitalization. Using the criteria outlined in Figure 1, we identified 355,627 [SE 9,401] weighted index hospitalizations for hypertensive emergency.
Mean age was 66.0 (SE 0.14) years and 53.7% were women. Common comorbidities included diabetes mellitus (DM) without complications (31.8%), heart failure (HF) (34.4%), and chronic kidney disease (CKD) (34.6%). The most common forms of end-organ involvement were acute heart failure (63.2%) and acute ischemic stroke or transient ischemic attack (22.2%). Most patients were covered under Medicare (64.1%), while 11.6% were covered under Medicaid, and 14.2% by private insurance. Most hospitalizations occurred at hospitals classified as large (62.6%) and metropolitan teaching hospitals (52.8%). Mean length of stay was 7 days and mean cost was $16,623 (Table 2).
Table 2:
Baseline patient and hospital characteristics. SE stands for standard error.
| Baseline characteristics for all index admissions | |
|---|---|
| Demographics | Mean (SE) or Percent for continuous and categorical variables respectively |
| Age, years mean (SE) |
66.0 (0.14) |
| Females | 53.7% |
| Median income for patient’s ZIP code | |
| First quartile | 40.2% |
| Second quartile | 27.4% |
| Third quartile | 19.2% |
| Fourth quartile | 13.1% |
| Primary payer | |
| Medicare | 64.1% |
| Medicaid | 11.6% |
| Private insurance | 14.2% |
| Self-pay | 6.8% |
| No charge | 0.9% |
| Other | 2.5% |
| Hospital characteristics | |
| Bed size | |
| Small | 11.8% |
| Medium | 25.7% |
| Large | 62.6% |
| Teaching status | |
| Metropolitan nonteaching | 36.8% |
| Metropolitan teaching | 52.8% |
| Nonmetropolitan hospital | 10.4% |
| Hospital control | |
| Government, nonfederal | 11.1% |
| Private, not-for-profit | 68.4% |
| Private, investor-owned | 20.6% |
| Comorbidities | |
| Diabetes mellitus without complications | 31.8% |
| Diabetes mellitus with complications | 13.5% |
| Heart failure | 34.4% |
| Chronic kidney disease | 34.6% |
| CKD stage 1 | 0.2% |
| CKD stage 2 | 1.8% |
| CKD stage 3 | 13.5% |
| CKD stage 4 | 6.4% |
| CKD stage 5 | 11.6% |
| CKD, not otherwise specified | 8.5% |
| End-stage renal disease | 12.7% |
| Valvular heart disease | 6.5% |
| Obesity | 22.0% |
| Peripheral vascular disease | 13.5% |
| Chronic lung disease | 24.6% |
| Pulmonary circulation disease | 4.5% |
| Chronic liver disease | 2.3% |
| Coagulopathy | 5.4% |
| Drug abuse | 5.2% |
| Alcohol abuse | 4.7% |
| Charlson comorbidity index Mean (SE) |
3.22 (0.01) |
| End-organ involvement | |
| Acute or unspecified heart failure | 63.2% |
| Acute myocardial infarction | 12.6% |
| Ruptured aortic aneurysm or dissection | 4.3% |
| Hypertensive encephalopathy | 5.4% |
| Subarachnoid, intracerebral or nontraumatic extradural hemorrhage | 5.8% |
| Cerebral thrombosis, transient cerebral ischemia, other cerebrovascular disease | 22.2% |
| Papilledema with increased intracranial pressure | 0.01% |
| Retinal hemorrhage | 0.1% |
| Index hospitalization outcomes | |
| Length of stay in days Mean (SE) |
7.0 (0.06) |
| Cost of index hospitalization in 2018 US dollars Mean (SE) |
16,623 (185) |
| Disposition | |
| Routine | 56.4% |
| Transfer to short-term hospital | 1.3% |
| Transfer to skilled nursing facility or intermediate care facility | 21.7% |
| Home healthcare | 19.1% |
| Discharge against medical advice | 1.5% |
Incidence, causes and predictors of 30-day readmission
Overall incidence of readmission was 17.8%. Of the patients who were readmitted, 42.1% had a cardiovascular cause of readmission. The 5 most common causes of readmission were HF (14.3%), hypertension with complications (10.5%), sepsis (5.9%), acute kidney injury (5%), and stroke (4.9%) (Figure 2). A complete list of the 15 most common principal diagnoses accounting for 67% readmissions is presented in Supplemental Table S1. Noncardiovascular causes accounted for 57.9% of all readmissions. Of the total 30-day readmissions, 36.1% of readmissions occurred within a week of discharge (Figure 3). A quarter of readmissions were to a different hospital than the index admission. We found several independent predictors of readmission including age<65, female sex, comorbidity burden, primary payer, substance use disorders, socioeconomic status, prolonged hospital stay, and discharge disposition (Table 3). Differences in Akaike Information Criterion (–7404.3) and Bayesian Information Criterion (–7013.5) for the full model compared with the null model indicated very strong support for the full model. Likelihood ratio test showed significant improvement in model fit for the full model compared with the null model (p<0.001) (Table 3).
Figure 2:
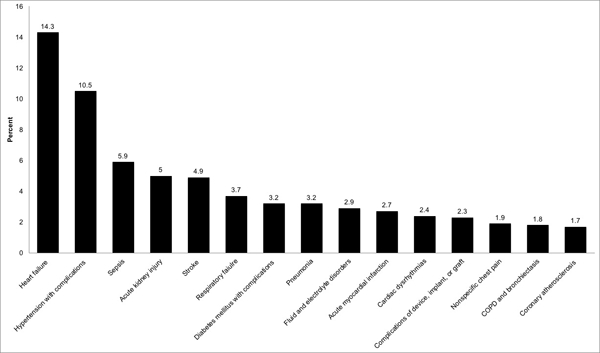
The fifteen most common principal diagnoses associated with 30-day readmissions.
Figure 3:
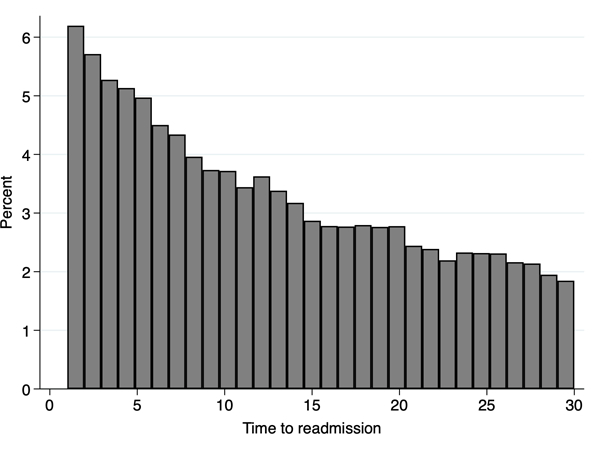
Distribution of time-to-readmission among patients who were readmitted within 30 days of discharge. Of the patients who were readmitted, 36.1% were readmitted within 7 days, and 61.1% were readmitted within 14 days.
Table 3:
Results of univariable and multivariable hierarchical logistic regression models for all-cause 30-day readmission
| Covariates | Unadjusted OR (95% CI) | p-value | Adjusted OR (95% CI)* | p-value |
|---|---|---|---|---|
| Age<65 years | 1.02 (1.00–1.05) | 0.10 | 1.21 (1.17–1.25) | <0.001 |
| Female sex | 1.10 (1.07–1.13) | <0.001 | 1.09 (1.07–1.12) | <0.001 |
| Primary payer | ||||
| Medicare | Reference | Reference | ||
| Medicaid | 1.15 (1.11–1.20) | <0.001 | 1.05 (1.002–1.10) | 0.04 |
| Private insurance | 0.54 (0.52–0.56) | <0.001 | 0.63 (0.60–0.66) | <0.001 |
| Self-pay | 0.51 (0.48–0.55) | <0.001 | 0.61 (0.57–0.66) | <0.001 |
| No charge | 0.50 (0.42–0.59) | <0.001 | 0.61 (0.51–0.72) | <0.001 |
| Other | 0.66 (0.60–0.72) | <0.001 | 0.71 (0.65–0.78) | <0.001 |
| Missing | 0.53 (0.35–0.81) | <0.001 | 0.57 (0.37–0.86) | 0.008 |
| Income quartile of patient’s ZIP code | ||||
| First | Reference | Reference | ||
| Second | 0.92 (0.89–0.95) | <0.001 | 0.97 (0.94–1.00) | 0.06 |
| Third | 0.88 (0.85–0.91) | <0.001 | 0.95 (0.91–0.99) | 0.007 |
| Fourth | 0.83 (0.79–0.87) | <0.001 | 0.93 (0.89–0.97) | 0.002 |
| Missing | 0.87 (0.78–0.97) | 0.01 | 0.94 (0.84–1.04) | 0.23 |
| Hospital characteristics | ||||
| Hospital bedsize | ||||
| Small | Reference | Reference | ||
| Medium | 1.09 (1.02 – 1.15) | 0.007 | 1.05 (0.99–1.11) | 0.08 |
| Large | 1.11 (1.05–1.17) | <0.001 | 1.07 (1.01–1.12) | 0.02 |
| Teaching status | ||||
| Metropolitan nonteaching | Reference | Reference | ||
| Metropolitan teaching | 0.97 (0.93–1.00) | 0.07 | 0.98 (0.95–1.02) | 0.36 |
| Nonmetropolitan hospital | 0.89 (0.84–0.95) | <0.001 | 0.94 (0.88–1.00) | 0.054 |
| Hospital control | ||||
| Government, nonfederal | Reference | Reference | ||
| Private, not-for-profit | 1.04 (0.98–1.10) | 0.19 | 1.01 (0.96–1.06) | 0.78 |
| Private, investor-owned | 1.14 (1.07–1.22) | <0.001 | 1.10 (1.03–1.16) | 0.003 |
| Comorbidities | ||||
| DM with complications | 1.64 (1.59–1.70) | <0.001 | 1.20 (1.16–1.24) | <0.001 |
| Chronic kidney disease | 1.85 (1.81–1.90) | <0.001 | 1.20 (1.16–1.24) | <0.001 |
| End-stage renal disease | 2.21 (2.14–2.29) | <0.001 | 1.46 (1.41–1.52) | <0.001 |
| Valvular heart disease | 1.11 (1.05–1.16) | <0.001 | 1.03 (0.98–1.09) | 0.29 |
| Obesity | 0.89 (0.86–0.91) | <0.001 | 0.86 (0.83–0.89) | <0.001 |
| Peripheral vascular disease | 1.28 (1.24–1.33) | <0.001 | 1.10 (1.06–1.15) | <0.001 |
| Chronic lung disease | 1.44 (1.40–1.48) | <0.001 | 1.19 (1.16–1.23) | <0.001 |
| Pulmonary circulation disease | 1.37 (1.30–1.45) | <0.001 | 1.09 (1.03–1.16) | 0.003 |
| Chronic liver disease | 1.63 (1.52–1.75) | <0.001 | 1.27 (1.18–1.37) | <0.001 |
| Coagulopathy | 1.24 (1.18–1.31) | <0.001 | 1.02 (0.97–1.08) | 0.41 |
| Drug abuse | 1.37 (1.30–1.44) | <0.001 | 1.32 (1.25–1.40) | <0.001 |
| Charlson comorbidity index >3 | 1.93 (1.88–1.98) | <0.001 | 1.25 (1.21–1.29) | <0.001 |
| End-organ involvement | ||||
| Acute or unspecified heart failure | 1.92 (1.87–1.98) | <0.001 | 1.37 (1.32–1.42) | <0.001 |
| Acute myocardial infarction | 0.95 (0.91–0.98) | 0.004 | 1.00 (0.96–1.04) | 0.87 |
| Stroke or transient ischemic attack | 0.54 (0.52–0.56) | <0.001 | 0.76 (0.73–0.80) | <0.001 |
| Length of stay > median | 1.44 (1.40–1.47) | <0.001 | 1.25 (1.22–1.29) | <0.001 |
| Disposition | ||||
| Routine | Reference | Reference | ||
| Transfer to short-term hospital | 1.48 (1.33–1.64) | <0.001 | 1.60 (1.44–1.78) | <0.001 |
| Transfer to skilled nursing facility or intermediate care facility | 1.35 (1.31–1.39) | <0.001 | 1.29 (1.24–1.33) | <0.001 |
| Home healthcare | 1.36 (1.32–1.41) | <0.001 | 1.24 (1.20–1.28) | <0.001 |
| Discharge against medical advice | 2.44 (2.24–2.66) | <0.001 | 2.20 (2.01–2.40) | <0.001 |
| Unknown | 0.31 (0.16–0.61) | <0.001 | 0.34 (0.17–0.68) | 0.002 |
*AIC for full model – AIC for null model= –7404.3, BIC for full model – BIC for null model= –7013.5. Differences in AIC and BIC for full model versus null model indicate very strong support for the full model. Likelihood ratio test showed a statistically significant improvement in model fit (p<0.001) for the full model compared with the null model.
AIC: Akaike Information Criterion, BIC: Bayesian Information Criterion
Sensitivity Analysis
A total of 110,158 index admissions representative of 235,069 (SE 6,266) index admissions nationwide were hospitalized with hypertensive emergency based on the more restrictive case definition, constituting 66.1% of the full study cohort. Mean age was 65.9 (SE 0.15) years and 55% were women. Overall incidence of unplanned all-cause 30-day readmission was 20.1%. The most common causes of readmission were heart failure (17.3%), hypertension with complications (11.1%), sepsis (5.7%), acute kidney injury (5.3%), and respiratory failure (4.2%) (Supplemental Figure S1). Noncardiovascular causes accounted for 57.9% of the readmissions. Predictors of readmission were consistent with the primary analysis (Supplemental Table S2).
Discussion
We found several potentially clinically relevant findings in this study. Patients hospitalized with hypertensive emergency have a high 30-day readmission rate of 18%. HF, uncontrolled hypertension, and stroke are the most common cardiovascular causes of readmission but more than half of all readmissions are for non-cardiovascular causes. Nearly two-thirds of all 30-day readmissions occur within 2 weeks of hospital discharge. Age<65 years, female sex, comorbidities such as DM, CKD, substance use disorder, and socioeconomic risk factors are significant predictors of 30-day readmission.
Consistent with our study findings, prior studies have demonstrated substantial readmission burden among patients hospitalized with severe hypertension. In a multicenter cross-sectional study, Gore et al. studied the 90-day readmission rates after acute severe hypertension and found a 90-day readmission rate of 35%.10 Insurance status and comorbidities such as HF, CKD, and substance abuse were significant predictors of readmission. In our study, age<65 was associated with higher odds of 30-day readmission. Similar age trends in 30-day readmission were observed among all hospitalized patients in a recent study using the NRD, where age≥65 years was associated with significantly lower adjusted odds of readmission compared with age 45 years.11 Potential explanations may include higher rates of medication nonadherence and substance use disorders in younger patients12 and positive spillover effects of readmission reduction strategies implemented by hospitals to avoid penalties under the Centers for Medicare and Medicaid Services (CMS) Hospital Readmission Reduction Program (HRRP). The latter may have an ancillary benefit of reducing readmissions for non-target conditions in older patients.13
More than half the readmissions were non-cardiovascular in nature. This is consistent with the readmission patterns noted for other chronic cardiovascular conditions such as HF and myocardial infarction (MI). 14,15 Comprehensive readmission reduction strategies, including focus on socioeconomics, healthcare access, and transitions in care may improve short-term readmission rates. Future studies are needed to determine if early outpatient follow-up, self-monitoring of blood pressure and blood pressure control to guideline-recommended targets may lessen this readmission burden. This is particularly relevant since early follow-up has been shown to be associated with fewer all-cause 30-day readmissions in patients with HF.16
Our study findings have important clinical and health policy implications. In this study, we observed that the 30-day readmission rates for hypertensive emergency are comparable to that reported for other common cardiovascular conditions such as HF and acute MI.14,15 This is particularly relevant since unlike HF and MI, hypertensive emergency is not targeted under the current CMS HRRP to incentivize hospitals to reduce 30-day readmission rates. Furthermore, with the increasing incidence and decreasing mortality rates for hypertensive emergency4,5, its readmission burden would be expected to increase. Targeting and lessening the burden of readmissions in patients with severe hypertension may impact overall excess healthcare expenditures in this population.17 Future studies are needed to determine what proportion of 30-day readmissions among patients with hypertensive emergency is preventable.
Our study is subject to certain limitations. First, the NRD is an administrative databases and identification of cases was based on a combination of ICD-9 codes. Therefore, the study may be susceptible to changes in coding practices and miscoding. However, we used a robust definition of hypertensive emergency that has previously been used for identification of hypertensive emergency in administrative datasets.4 Moreover, our findings were insensitive to a more restrictive case definition of hypertensive emergency which limited the inclusion criteria to a relatively homogeneous subsample of the main study cohort. Second, follow-up of individual patients in the NRD is based on a patient linkage variable. Therefore, records with missing or unverified linkage numbers are excluded from the NRD. Third, residual measured or unmeasured confounding may have influenced some of these findings. Fourth, granular patient-level data such as blood pressure measurements, drugs used to treat hypertensive emergency, and medication adherence and timeliness of follow-up visits after discharge were not available in the NRD database. Therefore, we were unable to ascertain the readmission risk associated with these potentially modifiable factors, which may be targeted in the early post-discharge period to prevent unplanned 30-day readmissions. Lastly, follow-up in the NRD in limited to calendar year of admission, therefore readmission analysis was limited to the year of admission.
Perspectives
In conclusion, we found that hypertensive emergency hospitalizations were associated with a high burden (~15–20%) of 30-day readmissions. Although these readmissions are commonly for HF, uncontrolled hypertension, and stroke, more than half are related to non-cardiovascular etiologies. Future studies should evaluate strategies to minimize the burden of 30-day readmission after hospitalization for hypertensive emergency.
Supplementary Material
Novelty and significance
What is new?
We determined incidence, causes and predictors of 30-day readmissions after hospitalization for hypertensive emergency.
What is relevant?
Hospitalizations for hypertensive emergency are associated with a 30-day readmission rate of 18%, comparable to target conditions included in the Centers for Medicare and Medicaid Services Hospital Readmission Reduction Program. Younger age, female sex, comorbidity burden, and socioeconomic factors are important predictors of readmission.
Summary
Hospitalizations for hypertensive emergency are associated with a substantial burden of 30-day readmission. A majority of these readmissions are related to non-cardiovascular conditions. We found multiple predictors of readmission that could help inform readmission reduction strategies.
Footnotes
Sources of funding: NONE
Disclosures
Dr. Muthiah Vaduganathan is supported by the NHLBI T32 postdoctoral training grant (T32HL007604) and serves on advisory boards for Bayer AG and Baxter Healthcare.
Dr. Deepak L. Bhatt discloses the following relationships - Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, TobeSoft; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic, Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, Eisai, Ethicon, Forest Laboratories, Idorsia, Ironwood, Ischemix, Lilly, Medtronic, PhaseBio, Pfizer, Regeneron, Roche, Sanofi Aventis, Synaptic, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Biotronik, Boston Scientific, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Merck, Novo Nordisk, PLx Pharma, Takeda.
References
- 1.Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT, Whelton PK. Potential US Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline. Circulation. 2018;137:109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaduganathan M, Pareek M, Qamar A, Pandey A, Olsen MH, Bhatt DL. Baseline Blood Pressure, the 2017 ACC/AHA High Blood Pressure Guidelines, and Long-Term Cardiovascular Risk in SPRINT. Am J Med. 2018; 131(8):956–960 [DOI] [PubMed] [Google Scholar]
- 3.Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest. 2000;118:214–227. [DOI] [PubMed] [Google Scholar]
- 4.Janke AT, McNaughton CD, Brody AM, Welch RD, Levy PD. Trends in the Incidence of Hypertensive Emergencies in US Emergency Departments From 2006 to 2013. J Am Heart Assoc. 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah M, Patil S, Patel B, Arora S, Patel N, Garg L, Agrawal S, Jacobs L, Steigerwalt SP, Martinez MW. Trends in Hospitalization for Hypertensive Emergency, and Relationship of End-Organ Damage With In-Hospital Mortality. Am J Hypertens. 2017;30:700–706. [DOI] [PubMed] [Google Scholar]
- 6.Introduction To The HCUP Nationwide Readmissions Database (NRD) 2013 [Internet]. hcup-us.ahrq.gov. [cited 2018 Mar 21];Available from: https://www.hcup-us.ahrq.gov/db/nation/nrd/NRD_Introduction_2013.jsp
- 7.Introduction To The HCUP Nationwide Readmissions Database (NRD) 2014 [Internet]. hcup-us.ahrq.gov. [cited 2018 Mar 21];Available from: https://www.hcup-us.ahrq.gov/db/nation/nrd/NRD_Introduction_2010-2014.jsp
- 8.Calculating NRD variances [Internet]. hcup-us.ahrq.gov. [cited 2017 May 17];Available from: https://www.hcup-us.ahrq.gov/reports/methods/2017-01.pdf
- 9.HCUP Methods Series: Hierarchical Modeling using HCUP Data [Internet]. hcup-us.ahrq.gov. [cited 2018 Mar 26];Available from: https://www.hcup-us.ahrq.gov/reports/methods/2007_01.pdf
- 10.Gore JM, Peterson E, Amin A, Anderson FA, Dasta JF, Levy PD, O’Neil BJ, Sung GY, Varon J, Wyman A, Granger CB, STAT Investigators. Predictors of 90-day readmission among patients with acute severe hypertension. The cross-sectional observational Studying the Treatment of Acute hyperTension (STAT) study. Am Heart J. 2010;160:521–527.e1. [DOI] [PubMed] [Google Scholar]
- 11.Berry JG, Gay JC, Maddox KJ, Coleman EA, Bucholz EM, O’Neill MR, Blaine K, Hall M. Age trends in 30 day hospital readmissions: US national retrospective analysis. BMJ. 2018;360:k497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta P, Patel P, Strauch B, Lai FY, Akbarov A, Maresova V, White CMJ, Petrak O, Gulsin GS, Patel V, Rosa J, Cole R, Zelinka T, Holaj R, Kinnell A, Smith PR, Thompson JR, Squire I, Widimsky JJ, Samani NJ, Williams B, Tomaszewski M. Risk Factors for Nonadherence to Antihypertensive Treatment. Hypertension. 2017;69:1113–1120. [DOI] [PubMed] [Google Scholar]
- 13.Demiralp B, He F, Koenig L. Further Evidence on the System-Wide Effects of the Hospital Readmissions Reduction Program. Health Serv Res. 2017; 53(3):1478–1497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bergethon KE, Ju C, DeVore AD, Hardy NC, Fonarow GC, Yancy CW, Heidenreich PA, Bhatt DL, Peterson ED, Hernandez AF. Trends in 30-Day Readmission Rates for Patients Hospitalized With Heart Failure: Findings From the Get With The Guidelines-Heart Failure Registry. Circ Heart Fail. 2016;9:e002594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khera R, Jain S, Pandey A, Agusala V, Kumbhani DJ, Das SR, Berry JD, de Lemos JA, Girotra S. Comparison of Readmission Rates After Acute Myocardial Infarction in 3 Patient Age Groups (18 to 44, 45 to 64, and ≥65 Years) in the United States. Am J Cardiol. 2017;120:1761–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. [DOI] [PubMed] [Google Scholar]
- 17.Kirkland EB, Heincelman M, Bishu KG, Schumann SO, Schreiner A, Axon RN, Mauldin PD, Moran WP. Trends in Healthcare Expenditures Among US Adults With Hypertension: National Estimates, 2003–2014. J Am Heart Assoc. 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


