Abstract
The search for the etiologic agent for Kaposi sarcoma (KS) led to the discovery of Kaposi sarcoma associated herpesvirus (KSHV) in 1994. KSHV, also called human herpesvirus-8 (HHV-8) has since been shown to be the etiologic agent for several other tumors and diseases, including primary effusion lymphoma (PEL), an extracavitary variant of PEL, KSHV-associated diffuse large B-cell lymphoma, a form of multicentric Castleman disease (MCD), and KSHV inflammatory cytokine syndrome (KICS). KSHV encodes several genes that interfere with innate and specific immunity, thwart apoptosis, enhance cell proliferation and cytokine production, and promote angiogenesis, and these play important roles in the disease pathogenesis. HIV is an important co-factor in KS pathogenesis, and widespread use of antiretroviral therapy has reduced KS incidence. However, KS remains the second most frequent tumor arising in HIV-infected patients in the United States and is particularly common in sub-Saharan Africa. KSHV prevalence varies substantially in different populations. KSHV is secreted in saliva, and public health measures to reduce its spread may help reduce the incidence of KSHV-associated diseases. While there have been advances in the treatment of KS, KSHV-MCD, and PEL, improved therapies are needed, especially those that are appropriate for KS in resource-poor regions.
Introduction
A report of Kaposi sarcoma (KS) in young gay men in New York and San Francisco in 1981 was one of the first harbingers of AIDS[1]. KS was first described in 1872 by Moritz Kaposi as a relatively indolent angioproliferative tumor in elderly men[2]. Several epidemiological subtypes of KS were subsequently differentiated: classic KS (in Mediterranean and Eastern European regions); more aggressive endemic KS (in Africa); and transplantation-associated KS[3, 4]. Prior to the AIDS epidemic, KS was rare in the United States. The AIDS epidemic changed that[1, 5]. Before development of effective antiretroviral therapy (ART), this new form, called AIDS-associated or epidemic KS, developed in up to 30% of AIDS patients[6, 7]. Unlike classic KS, AIDS-associated KS was often disseminated, rapidly progressive, and frequently fatal.
AIDS-associated KS was noted to develop in men who have sex with men (MSM), but less often in other HIV risk groups, suggesting a second infectious etiology[8]. In 1994, using representational difference analysis, Yuan Chang and Patrick Moore identified a novel gamma-herpesvirus in an AIDS-associated KS tumor. This virus, most closely related to Epstein-Barr virus (EBV), was called Kaposi sarcoma-associated herpesvirus (KSHV)[9]. Further studies revealed that KSHV, also called human herpesvirus-8 (HHV-8), is the etiologic agent of all epidemiologic subtypes of KS[4, 10]. A key finding supporting this conclusion was that detection of KSHV in the peripheral blood mononuclear cells (PBMC) preceded the development of KS[11]. Also, the prevalence of KSHV in various populations was found to parallel the incidence of KS[4].
Soon after its discovery, researchers identified two additional diseases caused by KSHV (Table 1). One was primary effusion lymphoma (PEL)[12], an aggressive B cell lymphoma usually arising in body cavities. Body cavity lymphomas had been observed before, but only after the association with KSHV was a distinct lymphoma subtype recognized[12, 13]. The other was a plasmablastic form of multicentric Castleman disease (KSHV-MCD)[14]. These conditions develop primarily in HIV-infected patients, but may also occur in HIV-uninfected persons. Nomenclature for KSHV-associated lymphomas has evolved to include an extracavitary variant of PEL and KSHV-associated diffuse large B-cell lymphoma[15]. Additionally, a KSHV inflammatory cytokine syndrome (KICS) has been proposed[16, 17]. Finally, primary infection with KSHV, while often silent, may sometimes be associated with fever, lymphadenopathy, rash or diarrhea[18]. Importantly, patients co-infected with KSHV and HIV often develop more than one KSHV-associated disease. Thus, clinicians seeing a patient with one of these disorders should keep a high index of suspicion for others, as additional diagnoses may have treatment implications.
Table 1.
Conditions caused by KSHV infection
| Disease | Implicated Cell Type | Evidence of KSHV Lytic Replication |
|---|---|---|
| Kaposi sarcoma (KS) | Spindle cell, endothelial origin | Rare cells. KSHV usually not detected in blood |
| KSHV-associated multicentric Castleman disease (KSHV-MCD) | Plasmablast | ~15–20% infected plasmablasts express lytic genes. Elevated KSHV viral load |
| Primary effusion lymphoma (PEL), including extracavitary variant | B-cell | Some cells produce vIL-6, elevated KSHV viral load |
| Large cell lymphoma developing in the context of KSHV-MCD | B-cell | Unknown. Clinical presentation may overlap with PEL |
| KSHV inflammatory cytokine syndrome (KICS) | Unknown; May occur in setting of KS or PEL | Circulating vIL-6 and elevated KSHV viral load in blood |
| Primary infection – silent or associated with fever, fatigue, lymphadenopathy, rash, and diarrhea | Unknown; may involve both B-cells and endothelial cells | Detectable KSHV viral load reported. |
Epidemiology and Transmission of KSHV
Unlike most other herpesviruses, KSHV prevalence varies widely among different populations[4] (Table 2). In general, KSHV is highly prevalent in sub-Saharan Africa, is of intermediate prevalence in the Mediterranean and parts of Latin and South America, and is of low prevalence in the general population in northern Europe, North America, and most of Asia. However, there are substantial differences in seroprevalence within these regions. Also, the prevalence in MSM is much higher in many areas, and is approximately 14–26% % in the U.S. among HIV-uninfected men, and even higher (up to 58%) in HIV-infected MSM[19]. Four major subtypes (A–D) have been defined based on variability of the ORF-K1 gene. Geographic distribution of these subtypes suggest that KSHV is an ancient virus[20]. Interestingly, extremely high seroprevalence has noted among some relatively isolated populations, including certain Amerindian groups in the Amazon as well as in ethnic groups in Xinjang, China (Table 2). Immunosuppression is an important cofactor for the development of KS and other KSHV-related diseases. Before the use of ART, 50% or more of HIV-infected patients with detectable KSHV were found to develop KS[11]. By contrast, KS develops in relatively infrequently in KSHV-infected patients without immunodeficiency[21, 22].
Table 2.
Geographical estimates of KSHV seroprevalence
| Geographic Region | KSHV seroprevalence |
|---|---|
| HIV Uninfected General Population | |
| Africa | |
| Uganda[156] | 69%(mothers) 15% (children) |
| Cameroon[157] | 82% |
| Nigeria[158] | 24% (adults) |
| Tanzania[158] | 45% (adults) |
| South Africa[64] | 11% |
| Europe and Mediterranean | |
| England [159] | <5% blood donors |
| Sicily, Italy[160] | 9% general |
| Central Italy[161] | 20% |
| Spain[162] | 4% |
| Israel [163] | 10% |
| Asia | |
| Japan [164] | 5% |
| Korea[162] | 5% |
| Thailand[162] | 8–10% |
| China [165, 166] | Varies widely in different regions, from <6% to >18% in Xinjiang region |
| Americas | |
| Argentina[162] | 6% |
| Brazilian Amazon[167] | 65% (ages 0–9) and 92% in Mapuera Indians 10% (ages 0–9) and 50% (>35 years) in non-Mapuera Indians |
| Colombia[162] | 13% |
| Costa Rica[162] | 10% |
| United States[168] | 4% |
| HIV Infected | |
| Cameroon[157] | 84% HIV |
| Johannesburg, South Africa[169] | 48% |
| United States[170, 171] | 38%–58%% |
| Peru [172] | 67% |
| Australia [173] | 52% |
| Men Who Have Sex with Men (not HIV infected) | |
| Shanghai China[174] | 23% |
| Japan[164] | 12% |
| Peru[172] | 27% |
| United States[170, 175] | 14–26%% |
| Sicily [176] | 16% |
| Eastern China [177] | 3% |
| Australia [173] | 11% |
KSHV transmission varies in different populations. KSHV may be secreted in saliva, and this is believed to be a principal means of spread[19]. KSHV viral load (VL) is substantially lower in semen, and this is not believed to be an important means of transmission[23]. An important portal of entry is the mouth; in sub-Saharan Africa, infection often occurs during childhood and is believed to be mediated by close contact and perhaps specific practices, such as food pre-mastication[24, 25]. KSHV can be detected in the circulating B cells of otherwise healthy infected individuals [26] and may rarely be spread by blood transfusion in sub-Saharan Africa[27]. However, even in areas with high seroprevalence, the risk of spread by transfusion is less than 3%[28]Transfusion practices used in the United States, such as the washing of red blood cells, substantially reduce this risk. KSHV may also be spread through solid organ transplantation[29], which can be associated with KSHV-associated malignancies post-transplant in the setting of immunosuppression. In MSM, there continues to be a high rate of KSHV transmission even when safer sex practices are utilized[19, 30]. Important routes of spread among MSM are believed to be is the use of saliva as a lubricant during anal sex, oral-anal sex, and deep oral kissing[30, 31]. The mouth has a number of anti-viral defenses which are lacking in the anus; thus small tears in anal tissue may be a particularly vulnerable entry point.
KSHV is a necessary cause of KSHV-associated malignancies. If spread could be halted, this would prevent the subsequent development of KSHV-associated tumors. Unlike other herpesviruses, transmission of KSHV is relatively inefficient, and it should theoretically be feasible to develop an effective vaccine. However, to date there has been little economic incentive for this. Even without a vaccine, it may be possible to reduce the spread of KSHV through public health measures. There is currently almost no knowledge about KSHV among MSM, and advice to not use saliva as a lubricant in anal sex is a potential behavioral intervention to reduce transmission in this population. Also, increased education about other routes of KSHV transmission may help lead to a decrease in new infections. Additional research on these issues is needed to inform future public health policy.
KSHV Biology and Disease Pathogenesis
KSHV is a large double-stranded DNA virus[32, 33]. It can infect several cell types, including B-cells, monocytes and endothelial cells. Like other herpesviruses, KSHV has latent and lytic replication programs. During latency, few genes are expressed, including those encoded by ORFK12 (kaposin), ORF71 (vFLIP), ORF72 (v-cyclin), ORF73 (latency-associated nuclear antigen[LANA]), ORFK10.5 (vIRF3) and several viral microRNAs (miRNAs)[32, 33]. Lytic replication involves expression of all genes, production and release of progeny virions, and death of infected cells. The switch to lytic replication is mediated by replication and transcription activator (RTA), encoded by ORF50[34]. A variety of physiologic signals can activate RTA, including hypoxia[35], oxidative stress[36], certain cytokines [37], as well as certain chemicals, such as sodium butyrate and 12-O-tetradecanoylphorbol-13-acetate (TPA).
KSHV encodes genes that can thwart innate cellular defenses, such as apoptosis or cell cycle arrest; subvert immunologic antiviral defenses; and promote proliferation of infected cells[32, 33]. Some KSHV genes mimic human genes with angiogenic and inflammatory properties[38, 39]. While the evolutionary pressure for these genes is to promote KSHV survival, they can also lead to the development of KSHV-related tumors and proliferative diseases, which are unintended consequences.
A few KSHV-encoded genes warrant specific mention. A viral interleukin-6 (vIL-6) induces the JAK/STAT pathway leading to increased expression of VEGF and angiogenesis[40, 41]. vIL-6 also promotes cell proliferation and contributes to the symptomatology of KSHV-MCD[42]. LANA inhibits p53, decreasing apoptosis of KSHV-infected cells[43]. KSHV-encoded interferon response factors (vIRFs) promote immune evasion by downregulation of MHC proteins[44, 45]. In addition, KSHV-encoded K3 and K5 ubiquinate surface MHC-1 and further contribute to downregulation, making infected cells invisible to effector T-cells[46, 47]. Several KSHV genes upregulate human IL-6, including v-FLIP, kaposin B, and ORF4[48]. KSHV v-FLIP activates NF-κB[49] which contributes to the pathogenesis of PEL, KS, and KSHV-MCD[49–51].
KSHV is somewhat unusual among oncogenic viruses in that several lytic genes play an important role in tumor pathogenesis. In KS and PEL, only a small percentage of infected cells express lytic genes[52, 53]. Even so, these genes are quite important in disease pathogenesis. In particular, there is evidence that a viral G-protein-coupled receptor (vGPCR), encoded by ORF74, plays a key role in KS[54–56]. In KSHV-MCD, KSHV-infected plasmablasts are the key cells driving the disease process. Many of these plasmablasts express vIL-6, and a substantial subset also express other lytic genes[53, 57–59]. It is unclear why different diseases develop in different KSHV-infected patients. One possibility is that differences in KSHV-encoded microRNA may contribute to different disease manifestations[60].
Kaposi Sarcoma (KS)
During the early AIDS epidemic, a substantial percentage of AIDS patients developed KS and it was an important cause of morbidity and mortality[61]. Soon after the introduction of the first anti-retroviral drugs, its incidence decreased, and it fell further after the development of combination ART (cART)[62]. Even so, it remains the second commonest tumor in HIV patients, with approximately 900 cases per year in the US in recent years, including cases in patients on long term cART[63]. Furthermore, KSHV prevalence is high in sub-Saharan Africa[64, 65], and both HIV-unrelated and HIV-associated KS are common in these regions. In some countries in sub-Saharan Africa, KS is the most common tumor in men[66]. Multiple factors will contribute to future epidemiologic trends, but given that aging is a risk for classic KS, it is possible that KS will become more common as the HIV-infected population ages.
Pathophysiology
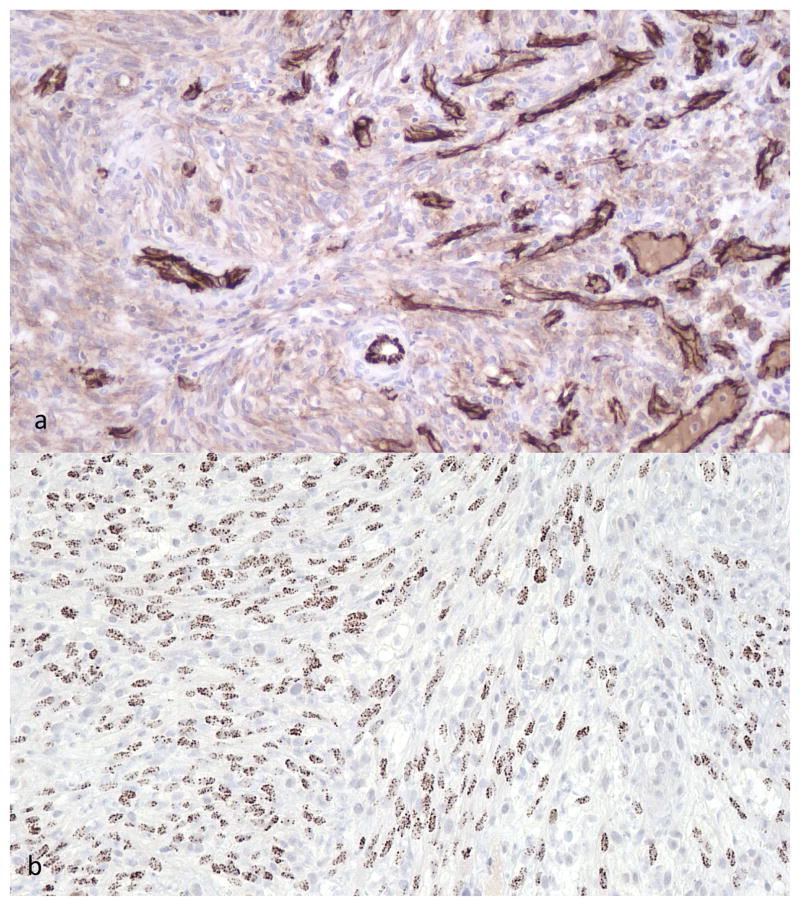
KS is a multicentric hyperproliferative disease that most often presents with violaceous skin lesions. Microscopically, lesions consist of spindle-shaped tumor cells, often accompanied by fibrosis, inflammatory infiltrates, vascular slits, and hemosiderin. Immunohistochemical staining for CD31 is positive, and staining of spindle cells for KSHV LANA is sensitive and specific[12, 67–72] (Figure 1). Extravasated red blood cells give lesions a purplish hue. There is evidence that early in the course of KS, tumors are multiclonal[73, 74]. However, more advanced disease has been reported to be oligoclonal or monoclonal[73, 75], and the clonality of KS is still an area of uncertainty.
Figure 1.
Cutaneous Kaposi sarcoma, 200x magnification. a) spindle cell tumor with abnormal blood vessels highlighted by CD31 immunohistochemistry, b) KS spindle cells with nuclear staining of KSHV encoded latency encoded nuclear antigen (LANA).
The cell of origin of KS is a KSHV-infected vascular or lymphatic endothelial cell[76, 77]. Several KSHV genes are implicated in KS pathogenesis. As noted above, expression of KSHV vGPCR, a lytic gene, in a small subset of cells appears to play a key role[55, 56]. This constitutively active receptor leads to production of factors such as vascular epithelial growth factor (VEGF), IL-6, interleukin-8 (IL-8), and tumor necrosis factor-alpha (TNF-α), which in turn promote KS through autocrine and paracrine activities. Cutaneous KS appears most frequently in the feet, which have poor oxygenation, especially in elderly men who develop classic KS. Hypoxia can induce RTA and other KSHV lytic genes, which may explain this association[35, 78, 79]. Interestingly, KSHV in turn enhance cellular levels of hypoxia inducible factors (HIFs) which mediate the cellular response to hypoxia, and this seems to be important in KSHV biology[80, 81].
KS Evaluation, Staging, and Treatment
Besides skin, KS can also develop in other locations, including oral mucosa, gastrointestinal tract, lymph nodes, and lung[82]. Skin lesions range from small patches to nodules. Diagnosis is made by biopsy. Pulmonary KS may be detected on chest X-ray or computerized tomography (Figure 2). In a patient with established KS, pulmonary disease is usually established by bronchoscopy with visualization of typical lesions and exclusion of other infectious etiologies. Biopsy of endobronchial lesion is generally avoided due to a risk of bleeding. KS may present anywhere along the gastrointestinal track. While bulky disease may be symptomatic, gastrointestinal disease is often first detected through evaluation of occult blood loss and/or microcytic anemia. Workup with upper endoscopy and colonoscopy should be reserved for patients with symptoms or fecal blood loss.
Figure 2.
Clinical manifestations of Kaposi sarcoma (KS). a) lower extremity KS with ulceration, b) inner thigh nodules, c) oral KS, d) lower extremity KS with tumor associated edema, e) pulmonary KS with associated effusion on computerized tomography.
Because KS is a multicentric disease, neither standard sarcoma staging nor the term metastases are useful. Patients are assessed on the extent of tumor (T), the status of the immune system (I) and the presence of systemic illness (S); for each parameter, a subscript of 0 is used to connote good risk and a subscript 1 poor risk[83]. For tumor burden, patients with tumor-associated edema or ulceration, extensive oral KS, gastrointestinal KS, or KS in other non-nodal viscera are considered poor risk (T1), while patients with disease confined to the skin, lymph nodes, and non-nodular oral disease confined to the palate are considered good risk (T0). (Table 3). The original staging criteria developed before availability of cART defined I1 as a CD4+ T-cell count <200 cells/uL. With cART, a CD4+ T-cell counts of <100 or <150 cells/uL appear to be better prognostic thresholds[84–86]. Some investigators advocate eliminating I in KS staging, thus stratifying patients as poor risk (T1S1) or good risk (T1S0, T0S1, or T0S0). Pulmonary KS is associated with a particularly high risk of death[86]. In clinical studies, response to therapy is usually evaluated by KS-specific criteria[83].
Table 3.
Kaposi Sarcoma Staging (ACTG Staging System)
| Tumor (T) | T0: Tumor limited to skin and/or nodes and/or minimal oral disease |
| T1: Tumor associated edema or ulceration, Extensive oral KS, Gastrointestinal KS, or Visceral KS (other than non-nodal viscera) | |
| Immune System (I) | I0: CD4+ T-cell count ≥150μL |
| I1: CD4+ T-cell count <150μL | |
| Systemic Illness (S) | S0: No prior OI, thrush or B symptoms* |
| S1: Prior OI, thrush, B symptoms, Karnofsky performance status <70%, or other HIV-related illnesses |
For each risk factor the subscripts “0” and “1” represent good risk and poor risk respectively. In the era of effective antiretroviral therapy, T1S1 represents the poor risk patients and T0S0, T0S1, or T1So represent good risk patients.
B symptoms are characterized by fever, night sweats and ≥ 10% of body weight loss.
ACTG: AIDS Clinical Trials Group; KS: Kaposi sarcoma; OI: opportunistic infection.
Patients with AIDS-related KS should be administered cART. Up to 80% of patients may have regression with cART alone; remissions are most likely in patients who are ART-naïve, have limited disease, and achieve optimal HIV control[85, 87]. The median time to response varies from about 3 to 9 months. Substantial responses to cART are rare in patients with poor prognosis (T1S1) disease[85, 88]. Some HIV-infected patients who are started on cART will develop KS or have an exacerbation of their existing KS that may be a manifestation of immune reconstitution inflammatory syndrome (IRIS)[89, 90]. There are no controlled trials to assess the optimal care of such patients, although systemic therapy for KS seems appropriate. While steroids are utilized in patients with other manifestations of IRIS, they can substantially exacerbate KS[91] and should be avoided when possible.
In vitro studies have shown that certain HIV protease inhibitors may have activity against KS, through anti-angiogenesis activity or other mechanisms, and nelfinavir has been reported to inhibit KSHV replication[92, 93]. Several early clinical studies failed to find any advantage of protease-inhibitor containing cART regimens in preventing or treating KS[94, 95]. However, a more recent study that controlled for time on a given cART regimen found a reduction of KS in HIV-infected patients receiving boosted protease inhibitors (but not nelfinavir) after two years of treatment[96], and this an area for future study.
Patients with a few small but problematic lesions can be treated with local therapy (topical 9-cis-retinoic acid, cryotherapy, radiation therapy, or intralesional injections, or surgical resection), but results are often unsatisfactory and these approaches are now rarely used[16, 97, 98]. There are no hard criteria for systemic KS therapy, and the decision should be individualized. Systemic KS therapy is usually administered to patients with widespread T1 disease, extensive cutaneous KS, symptomatic or life-threatening visceral KS, ulcerating KS, KS associated with edema, or tumor related pain. Also, systemic therapy is justified in patients that fail to respond to cART, those with social withdrawal from KS, or when a rapid response is desired. For patients hospitalized with symptomatic KS, urgent therapy is often indicated, and may even need to be started in the intensive care unit. The most commonly used Food and Drug Administration (FDA)-approved systemic therapy is liposomal doxorubicin (Doxil)[99, 100]. Other approved agents include liposomal daunorubicin (DaunoXome) and paclitaxel[101, 102]. Interferon-alpha has activity[103], but is poorly tolerated and is rarely used. Other chemotherapeutic agents with some activity include vincristine, vinblastine, doxorubicin, and bleomycin, but these have relatively less activity and greater toxicity. They are rarely used in the U.S.[16], but are still used in low-resource settings[85].
A more detailed description of KS treatment is beyond the scope of this article, and the reader is referred to other reviews[16, 98]. However, a few key points are worth mentioning. Specific KS therapy should only be instituted if there is a pathological diagnosis. Other than obtaining a biopsy for diagnosis, the only role for surgery is to remove a lesion that is anatomically problematic (e.g. one blocking an airway). Also, while long-term remissions can be attained, KS is not considered a tumor that can be “cured”, and the goal of therapy is acceptable palliation. This may require long-term therapy, sometimes intermittently. A good strategy is to continue a specific therapy until a remission or response plateau is achieved, and then taper or stop. There is no evidence that KS develops resistance to any therapeutic agent, and previously effective agents can often be reused in case of regrowth. Given that KSHV is a herpesvirus, patients are sometimes given antiherpes drugs. However, while cidofovir and ganciclovir are active against KSHV in the lab, prospective studies have shown no clinical activity in patients with established KS[104, 105]. Finally, corticosteroids can dramatically exacerbate KS[91] and should be avoided when possible.
Approximately 30% of KS patients have inadequate responses to standard chemotherapy. Others need prolonged treatment; however long-term use of chemotherapeutic agents is associated with cumulative toxicities, including cytopenias, cardiomyopathy, and neuropathy. In particular; patients receiving a cumulative dose of more than 450 mg/m2 of doxorubicin can develop irreversible cardiac toxicity. Although liposomal formulations may be less cardiotoxic, caution with cumulative dosing, including monitoring of cardiac ejection fraction, is advised. There is therefore a substantial unmet need for novel anti-KS agents, especially those suitable for resource-poor regions. Rapamycin is effective in renal transplantation recipients with KS[106], and a recent study showed that it had some activity in AIDS-KS but also substantial pharmacologic interactions with antiretroviral drugs with strong CYP3A4 inhibitory activity[107]. Other targeted agents demonstrating some activity in early phase trials include imatinib (tyrosine kinase inhibitor of BCR-ABL), interleukin-12, COL-3 (matrix metalloproteinase inhibitor), bevacizumab (anti-vascular growth factor inhibitor), and thalidomide[108–113]. More recently, pomalidomide was shown to be tolerable and lead to a 73% response rate, with activity in both AIDS-KS and HIV-unassociated KS[112]. A larger study is now in the planning stage to assess toxicity and activity and feasibility of administration of pomalidomide in sub-Saharan Africa. A second study is evaluating safety and efficacy of pomalidomide in combination with liposomal doxorubicin in patients with more advanced KS (NCT02659930).
Primary Effusion Lymphoma (PEL)
PEL is a rare B-cell malignancy that usually presents as an effusion in the pleura, peritoneum, or pericardium in HIV-infected patients. It may also present as non-cavitary solid disease in lymph nodes, skin, or organs[12, 114]. Diagnosis requires demonstration of KSHV in the tumor cells; in about 80% of cases, they are co-infected with EBV. In most cells, only latent KSHV genes are expressed; however, a minority express vIL-6 or other lytic genes[53]. Pathological examination usually shows expression of CD45, CD138, CD30, CD38 and HLA-DR with lack of B-cell markers such as CD20, CD19 and immunoglobulins[115]. Abnormal phenotypes including tumors with T-cell markers have been described[116]. PEL tumor cells have clonal immunoglobulin gene rearrangements. There is provocative recent evidence that PEL may arise from KSHV-infected mesothelial cells which differentiate into “B1-like” tumor cells[117].
Although originally described in patients with advanced AIDS, recent data shows PEL may occur at higher CD4+ T-cell counts, with a median of 204 cells/μL noted in one recent cohort [118]. Patients often present with fevers, malaise, and other inflammatory symptoms. In addition, they often present with a syndrome of hypoalbuminemia, thrombocytopenia, anemia, elevated IL-6, and elevated KSHV viral load that is relatively unique amongst HIV-associated lymphomas[119]. Clinicians should be vigilant for PEL in any HIV-infected patient with an effusion, especially if they have inflammatory symptoms or other KSHV-associated diseases. Historically, median survival was less than 6 months[120]. Nonetheless, PEL should be approached with curative intent. Combination therapy with a CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone)-based regimen and cART is commonly used as first line therapy, and may lead to long-term remissions in approximately 40% of patients[118]. Our group reported similar overall survival in 19 HIV-infected PEL patients treated with modified DA-EPOCH (etoposide, doxorubicin, vincristine, cyclophosphamide) based regimen and cART[121]. Interestingly, elevations in inflammatory cytokines, ferritin, and serum IgE, but not usual parameters of lymphoma prognosis, were predictive of a poor outcomes[121]. We are currently initiating a prospective trial of lenalidomide, which counters KSHV vFLIP upregulation of IRF4, an important survival pathway in PEL[50, 122, 123] and KSHV-induced MHC-1 downregulation[124], in combination with EPOCH and rituximab (NCT02911142).
Multicentric Castleman Disease
The term Castleman disease is used to describe a number of related lymphoproliferative disorders that vary based on anatomic distribution (unicentric vs. multicentric) and pathology[125]. KSHV is the cause of a distinct subset of multicentric Castleman disease (KSHV-MCD) that usually develops in HIV-infected patients[14, 126]. It is clinically characterized by inflammatory symptoms, including fevers, night sweats, weight loss, cachexia, edema, and effusions[125, 127]. KSHV-MCD patients characteristically have lymphadenopathy and splenomegaly, and commonly also have respiratory, dermatologic, respiratory, and neurologic symptoms. Laboratory abnormalities include anemia, thrombocytopenia, hyponatremia, decreased albumin, elevated C-reactive protein, and elevated KSHV-viral load as measured in both plasma and circulating mononuclear cells[59, 125–128]. The course is characterized by intermittent flares and is usually fatal if not treated[129]. Patients with untreated KSHV-MCD are at high risk of developing large B cell lymphoma[130–132]. The clinical presentation of KSHV-MCD is similar in HIV-uninfected patients[133].
Pathophysiology and Evaluation
Diagnosis of KSHV-MCD requires biopsy of an affected lymph node and demonstration of KSHV-infected plasmablasts (identified by LANA staining), usually in lymph nodes or spleen. KSHV-MCD lymph nodes have regressed germinal centers with vascularized core (sometimes a “lollypop” sign) and mantle zone expansion with KSHV infected plasmablastic cells[132]. A substantial proportion of these plasmablasts express vIL-6, and a subset of these show lytic activation[53, 134]. Interestingly, while plasmablasts are polyclonal, they are monotypic and express IgM and lambda[132]. Inflammatory symptoms result from production of a variety of cytokines and factors, especially IL-6, IL-10, and vIL-6[57, 59, 135]. Nearly all patients have elevated IL-6 levels during flares, while a substantial subset have elevated vIL-6[42, 59]. vIL-6 plays a critical role and helps induce IL-6 production[58]. Direct activation of KSHV vIL-6 by X-box binding protein type 1 (XBP-1) in infected plasmablasts can upregulate vIL-6 without the need for full lytic induction of KSHV[134]. There is evidence that KSHV v-FLIP plays an important additional role in KSHV-MCD pathogenesis[136]. There is also evidence that certain KSHV microRNA sequences may be associated with an increased risk of KSHV-MCD [60]. Interestingly, a cytokine excess syndrome similar to KSHV-MCD and associated with increased IL-6 has been observed in cancer patients treated with chimeric antigen receptor (CAR) T-cells[137].
18F-fluorodeoxyglucose positron emission tomography (PET) of patients with KSHV-MCD often shows hypermetabolic symmetrical lymphadenopathy and splenomegaly and may be useful in selecting lymph nodes for biopsy and excluding concurrent lymphoma. The diagnosis of KSHV-MCD is often missed, and physicians should be vigilant for this condition in patients with KS and symptoms or characteristic laboratory abnormalities. C-reactive protein is elevated during flares and can be used as a rough screening test along with evaluation of KSHV viral load. Patients with KSHV-MCD can deteriorate quickly due to sepsis-like syndromes, which are often mistakenly believed to be bacterial in origin.
KSHV-MCD is considered a rare disorder. However, it is almost certainly underreported. Improved diagnostic coding of Castleman disease may improve future epidemiologic studies. Unlike KS, KSHV-MCD often arises in patients with relatively preserved CD4+ T-cell counts, and there is evidence that its incidence may be increasing since the introduction of cART[138]. Interestingly, KSHV-MCD may be associated with defects in invariant natural killer T-cells (iNKT)[139]. There are few cases reported in sub-Saharan Africa, despite the very high prevalence of KSHV and HIV co-infection. We have seen several African immigrants with KSHV-MCD in our studies in the NIH Clinical Center[59, 140, 141], suggesting that many cases are missed in Africa. This may be changing, and a recent case series of KSHV-MCD was reported from Malawi[142]. Given our improved understanding of KSHV-MCD, it is quite possible that some patients with fevers and inflammatory symptoms in the AIDS epidemic had KSHV-MCD.
Treatment of KSHV-MCD
Without treatment, KSHV-MCD is generally lethal. Before specific therapies were developed, observed overall survival was two years or less[125, 127]. However, there have been substantial advances, and long-term remissions and survival can be attained in most cases[16, 143]. Rituximab (monoclonal antibody targeting CD20 antigen), alone or in combination with other agents, has dramatically improved outcomes, as demonstrated in three prospective studies and several cohort studies [133, 141, 144–148]. Rituximab as a single agent[145, 146] leads to resolution of MCD symptoms in excess of 90%. The high rate of success along with a safe toxicity profile led to the recommendation of rituximab as a first line treatment option. Relapse-free survival after rituximab-based therapy is 70–80%, and maintenance therapy does not appear to be required[147]. However, rituximab may have limitations in patients with low CD4+ T-cell counts, severe symptoms, organ dysfunction, and patients with coexisting KS, as rituximab can lead to worsening of KS[145, 146, 149, 150]. Patients with KSHV-MCD flares can be extremely sick with a sepsis-like appearance and require treatment in an intensive care unit, where they may quickly respond when appropriately treated. The addition of cytotoxic chemotherapy to rituximab has been recommended for patients with advanced KSHV-MCD manifested by a poor performance status (Eastern Cooperative Oncology Group performance status ≥2), organ dysfunction, hemophagocytcic syndrome or severe hemolytic anemia, and either concurrent liposomal doxorubicin or etoposide has been used in this setting. Our group has studied the combination of rituximab and liposomal doxorubicin in patients with KSHV-MCD and KS or with severe KSHV-MCD[141]; the rationale was that in the latter group, the liposomal doxorubicin may provide additional killing of the KSHV-MCD plasmablasts. We observed major clinical and biochemical responses in 94% and 88% of patients respectively and on overall 3-year survival of 81%[141]. Also, while one patient developed KS, 5 of 6 patients with concomitant KS had improvement.
Another prospectively studied approach is virus-activated cytotoxic therapy using high dose zidovudine plus valganciclovir (a pro-drug of ganciclovir). This is based on in vitro observations that the KSHV lytic genes ORF21 and ORF36 can phosphorylate ganciclovir, leading to a toxic moiety and that ORF21, another lytic gene, can similarly phosphorylate zidovudine[151–153]. A substantial subset of KSHV-MCD plasmablasts express lytic genes, and based on this, our group evaluated high dose AZT and valganciclovir in MCD patients. The combination yielded major clinical responses in 86% of patients, with major biochemical responses in 50%[140]. There are some limitations to this approach, including inadequate activity in patients with advanced disease, dose limiting cytotoxicity requiring intermittent dosing, and high pill burden. However, combined with maintenance therapy or treatment of relapses, the overall survival was 86% at 12 months or beyond[140].
In addition to the KSHV-MCD specific treatments listed above, HIV-infected patients should receive cART. Glucocorticosteroids can be useful during flares[16]; however, patients should be weaned as soon as possible because of their inadequacy in controlling KSHV-MCD in the long term and their potential to worsen KS. Because of the role of IL-6 in KSHV-MCD, there has been an interest in exploring the use of monoclonal antibodies targeting IL-6 signaling, such as tocilizumab or siltuximab in KSHV-MCD. However, given the importance of other cytokines[59], such as vIL-6, it is not evident that they would be sufficient, and their use is discouraged outside the setting of a clinical trial. We are currently evaluating tocilizumab alone or in combination with virus activated cytotoxic therapy (NCT01441063).
KSHV Inflammatory Cytokine Syndrome (KICS)
Several years ago, our group observed that occasional patients with KSHV infection had a symptom profile that resembled KSHV-MCD but did not have KSHV-MCD. In a retrospective analysis, we identified six such patients[42]. In none were we able to make a pathologic diagnosis of KSHV-MCD or identify another condition to account for the findings. Four had KS, but the other 2 did not have any tumors. There are several mechanisms by which KSHV can increase cytokine production, and we hypothesized that the symptoms in these patients resulted from direct or indirect cytokine activation by KSHV. Further study showed that these patients had elevated vIL-6, human IL-6, IL-10, and other cytokines and factors, as well as a high KSHV viral load[42]. We have proposed the term Kaposi sarcoma herpesvirus inflammatory syndrome (KICS) to describe these patients and developed a prospective case definition (Table 4)[17, 154]. We subsequently initiated a prospective study, and recently reported the first 10 patients[17]. Interestingly, all 10 patients had KS, and 2 also had PEL; this may reflect our referral pattern, as the patients were all initially referred for other KSHV malignancies. PET scans showed increased uptake by the tumors, but not the generalized lymph node uptake seen in KSHV-MCD[17]. KS did not respond to standard therapy in many of these patients, and overall they fared poorly; in total, 9 of our16 patients with KICS died, often from progressive KSHV-related tumors. Since our original publication, other investigators have reported similar cases[155]. Many questions remain, such as the source of the cytokine production. It is also unclear how to best treat this condition. We have been treating the underlying tumors, and in addition, exploring approaches developed for KSHV-MCD: high dose zidovudine plus valganciclovir, or liposomal doxorubicin plus pomalidomide.
Table 4.
Working Case Definition of KSHV Inflammatory cytokine syndrome (KICS)
| 1. Clinical, Laboratory and Radiographic Abnormalities |
|
| 2. Laboratory Evidence of Systemic Inflammation |
| High C-reactive protein (>3g/dL) |
| 3. Laboratory Evidence of KSHV Lytic Activity |
| High KSHV viral load in PBMC (>100 copies/106 cells) |
| 4. No Evidence of KSHV-Associated Multicentric Castleman Disease |
| Requires biopsy of lymph nodes, spleen or bone marrow to rule out KSHV-MCD |
| Definition of KICS requires at least two clinical, laboratory or radiographic manifestations drawn from at least two categories (a, b and c) AND each of the criteria in 2, 3 and 4. |
Table adapted from Polizzotto et al. Front Microbiol 2012[154]
The nomenclature is not standardized. There are several clinical differences between KICS patients and those with KSHV-MCD, and we restrict the term KSHV-MCD to those patients with the appropriate pathologic findings, and consider other patients with IL-6 related inflammatory symptoms and elevated KSHV viral load to have KICS, even if they have a concurrent malignancy. In patients with PEL and KICS, one could argue that KICS is a severe manifestation of “B symptoms”, however, given the common viral etiology with KSHV-MCD, severity of symptoms, and cytokine profile that can also be observed in certain patients with KS or even without KSHV malignancy, we find the term KICS useful for considering these patients as a group. This is an area of active investigation that may lead to an improved understanding of disease pathogenesis in these high-risk patients, and modified classification of KSHV-MCD and KICS may be warranted in the future.
Conclusion
The discovery of KSHV and its identification as the cause of KS[9, 10] opened the door to a number of lines of inquiry and new insights. It is now appreciated that KSHV can cause several diseases, several of which had not been previously recognized. We have come a long way to understanding the biology of KSHV and disease pathogenesis, and are starting to develop therapeutic approaches targeting specific pathways. Even so, there is much more work to be done. Transmission rates of KSHV continue to be high in certain populations, and we do not have a vaccine or even a clear understanding of the modes of transmission. Efforts to better understand how KSHV is spread and the ways that this can be reduced through education and public health strategies are needed. There are also many unanswered questions regarding KSHV biology and the ways in which this virus induces disease. While therapy has improved for KS and KSHV-MCD, the prognosis for PEL and high risk KS remains poor, and there remains a need for improved and less toxic therapies. Finally, it should be stressed that recognized and unrecognized KSHV-related diseases continue to be a major public health problem in sub-Saharan Africa, and there is an urgent need for improved prevention, diagnosis, and therapy that can be utilized in resource-poor areas.
Acknowledgments
This research was supported by the Intramural Research Program of the NIH, National Cancer Institute. We thank Dr. Sun from the NCI Laboratory of Pathology for pathology images.
Footnotes
Role of Authors
The primary drafting of the manuscript was undertaken primarily by Drs. PG and RY; all authors contributed to the writing, edited the manuscript, and approved the final version.
Disclosure: This work was supported by the Intramural Research Program of the NIH, National Cancer Institute.
Conflict of Interest Statement
Research of the authors is supported in part by a CRADA between the National Cancer Institute and Celgene Corp. Also, TSU and RY are co-inventors on a patent application related to the treatment of KSHV-associated diseases with pomalidomide, and the spouse of RY is a co-inventor on a patent related to the measurement of KSHV vIL-6. These inventions were all made as part of their duties as employees of the US Government, and the patents are or will be assigned to U.S. Department of Health and Human Services. The government may convey a portion of the royalties it receives from licensure of its patents to its employee inventors. Finally, RY and TSU have recently conducted clinical research using drugs supplied to the NCI by Merck and Co., Hoffman LaRoche, and Bayer Healthcare.
References
- 1.Centers for Disease C. Kaposi’s sarcoma and Pneumocystis pneumonia among homosexual men--New York City and California. MMWR Morbidity and mortality weekly report. 1981;30(25):305–308. [PubMed] [Google Scholar]
- 2.Kaposi M. Idiopathisches multiples Pigmentsarkom der Haut. Archiv Für Dermatologie Und Syphillis. 1872;4:265–273. [Google Scholar]
- 3.Franceschi S, Geddes M. Epidemiology of classic Kaposi’s sarcoma, with special reference to Mediterranean population. Tumori. 1995;81(5):308–314. doi: 10.1177/030089169508100502. [DOI] [PubMed] [Google Scholar]
- 4.Gao S-J, Kingsley L, Zheng ML, Zheng W, Parravicini C, Zeigler J, et al. KSHV antibodies among Americans, Italians, and Ugandans with and without Kaposi’s sarcoma. Nature Med. 1996;2(8):925–928. doi: 10.1038/nm0896-925. [DOI] [PubMed] [Google Scholar]
- 5.Hymes KB, Cheung T, Greene JB, Prose NS, Marcus A, Ballard H, et al. Kaposi’s sarcoma in homosexual men-a report of eight cases. Lancet. 1981;2(8247):598–600. doi: 10.1016/s0140-6736(81)92740-9. [DOI] [PubMed] [Google Scholar]
- 6.Rabkin CS, Biggar RJ, Horm JW. Increasing incidence of cancers associated with the human immunodeficiency virus epidemic. Int J Cancer. 1991;47:692–696. doi: 10.1002/ijc.2910470511. [DOI] [PubMed] [Google Scholar]
- 7.Safai B, Johnson KG, Myskowski PL, Koziner B, Yang SY, Cunningham-Rundles S, et al. The natural history of Kaposi’s sarcoma in the acquired immunodeficiency syndrome. Annals of internal medicine. 1985;103(5):744–750. doi: 10.7326/0003-4819-103-5-744. [DOI] [PubMed] [Google Scholar]
- 8.Beral V, Peterman TA, Berkelman RL, Jaffe HW. Kaposi’s sarcoma among persons with AIDS: a sexually transmitted infection? Lancet. 1990;335(8682):123–128. doi: 10.1016/0140-6736(90)90001-l. [DOI] [PubMed] [Google Scholar]
- 9.Chang Y, Cesarman E, Pessin MS, Lee F, Culpepper J, Knowles DM, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science. 1994;266(5192):1865–1869. doi: 10.1126/science.7997879. [DOI] [PubMed] [Google Scholar]
- 10.Moore PS, Chang Y. Detection of herpesvirus-like DNA sequences in Kaposi’s sarcoma in patients with and without HIV infection. N Engl J Med. 1995;332(18):1181–1185. doi: 10.1056/NEJM199505043321801. [DOI] [PubMed] [Google Scholar]
- 11.Whitby D, Howard MR, Tenant-Flowers M, Brink NS, Copas A, Boshoff C, et al. Detection of Kaposi sarcoma associated herpesvirus in peripheral blood of HIV-infected individuals and progression to Kaposi’s sarcoma. Lancet. 1995;346(8978):799–802. doi: 10.1016/s0140-6736(95)91619-9. [DOI] [PubMed] [Google Scholar]
- 12.Cesarman E, Chang Y, Moore PS, Said JW, Knowles DM. Kaposi’s sarcoma-associated herpesvirus-like DNA sequences in AIDS-related body-cavity-based lymphomas. The New England journal of medicine. 1995;332(18):1186–1191. doi: 10.1056/NEJM199505043321802. [DOI] [PubMed] [Google Scholar]
- 13.Nador RG, Cesarman E, Chadburn A, Dawson DB, Ansari MQ, Sald J, et al. Primary effusion lymphoma: a distinct clinicopathologic entity associated with the Kaposi’s sarcoma-associated herpes virus. Blood. 1996;88(2):645–656. [PubMed] [Google Scholar]
- 14.Soulier J, Grollet L, Oksenhendler E, Cacoub P, Cazals-Hatem D, Babinet P, et al. Kaposi’s sarcoma-associated herpesvirus-like DNA sequences in multicentric Castleman’s disease. Blood. 1995;86(4):1276–1280. [PubMed] [Google Scholar]
- 15.Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–2390. doi: 10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goncalves PH, Ziegelbauer J, Uldrick TS, Yarchoan R. Kaposi sarcoma herpesvirus-associated cancers and related diseases. Curr Opin HIV AIDS. 2017;12(1):47–56. doi: 10.1097/COH.0000000000000330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Polizzotto MN, Uldrick TS, Wyvill KM, Aleman K, Marshall V, Wang V, et al. Clinical Features and Outcomes of Patients With Symptomatic Kaposi Sarcoma Herpesvirus (KSHV)-associated Inflammation: Prospective Characterization of KSHV Inflammatory Cytokine Syndrome (KICS) Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2016;62(6):730–738. doi: 10.1093/cid/civ996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang QJ, Jenkins FJ, Jacobson LP, Kingsley LA, Day RD, Zhang ZW, et al. Primary human herpesvirus 8 infection generates a broadly specific CD8(+) T-cell response to viral lytic cycle proteins. Blood. 2001;97(8):2366–2373. doi: 10.1182/blood.v97.8.2366. [DOI] [PubMed] [Google Scholar]
- 19.Pauk J, Huang ML, Brodie SJ, Wald A, Koelle DM, Schacker T, et al. Mucosal shedding of human herpesvirus 8 in men. The New England journal of medicine. 2000;343(19):1369–1377. doi: 10.1056/NEJM200011093431904. [DOI] [PubMed] [Google Scholar]
- 20.Zong JC, Ciufo DM, Alcendor DJ, Wan X, Nicholas J, Browning PJ, et al. High-level variability in the ORF-K1 membrane protein gene at the left end of the Kaposi’s sarcoma-associated herpesvirus genome defines four major virus subtypes and multiple variants or clades in different human populations. Journal of virology. 1999;73(5):4156–4170. doi: 10.1128/jvi.73.5.4156-4170.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhutani M, Polizzotto MN, Uldrick TS, Yarchoan R. Kaposi sarcoma-associated herpesvirus-associated malignancies: epidemiology, pathogenesis, and advances in treatment. Seminars in oncology. 2015;42(2):223–246. doi: 10.1053/j.seminoncol.2014.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gallo RC. The enigmas of Kaposi’s sarcoma. Science. 1998;282(5395):1837–1839. doi: 10.1126/science.282.5395.1837. [DOI] [PubMed] [Google Scholar]
- 23.Monini P, de Lellis L, Fabris M, Rigolin F, Cassai E. Kaposi’s sarcoma-associated herpesvirus DNA sequences in prostate tissue and human semen. The New England journal of medicine. 1996;334(18):1168–1172. doi: 10.1056/NEJM199605023341805. [DOI] [PubMed] [Google Scholar]
- 24.Crabtree KL, Wojcicki JM, Minhas V, Smith DR, Kankasa C, Mitchell CD, et al. Risk factors for early childhood infection of human herpesvirus-8 in Zambian children: the role of early childhood feeding practices. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2014;23(2):300–308. doi: 10.1158/1055-9965.EPI-13-0730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borges JD, Souza VA, Giambartolomei C, Dudbridge F, Freire WS, Gregorio SA, et al. Transmission of human herpesvirus type 8 infection within families in american indigenous populations from the Brazilian Amazon. The Journal of infectious diseases. 2012;205(12):1869–1876. doi: 10.1093/infdis/jis278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blackbourn DJ, Ambroziak J, Lennette E, Adams M, Ramachandran B, Levy JA. Infectious human herpesvirus 8 in a healthy North American blood donor. Lancet. 1997;349(9052):609–611. doi: 10.1016/S0140-6736(96)10004-0. [DOI] [PubMed] [Google Scholar]
- 27.Mbulaiteye SM, Biggar RJ, Bakaki PM, Pfeiffer RM, Whitby D, Owor AM, et al. Human herpesvirus 8 infection and transfusion history in children with sickle-cell disease in Uganda. J Natl Cancer Inst. 2003;95(17):1330–1335. doi: 10.1093/jnci/djg039. [DOI] [PubMed] [Google Scholar]
- 28.Hladik W, Dollard SC, Mermin J, Fowlkes AL, Downing R, Amin MM, et al. Transmission of human herpesvirus 8 by blood transfusion. The New England journal of medicine. 2006;355(13):1331–1338. doi: 10.1056/NEJMoa055009. [DOI] [PubMed] [Google Scholar]
- 29.Barozzi P, Luppi M, Facchetti F, Mecucci C, Alu M, Sarid R, et al. Post-transplant Kaposi sarcoma originates from the seeding of donor-derived progenitors. Nature medicine. 2003;9(5):554–561. doi: 10.1038/nm862. [DOI] [PubMed] [Google Scholar]
- 30.Martin JN, Ganem DE, Osmond DH, Page-Shafer KA, Macrae D, Kedes DH. Sexual transmission and the natural history of human herpesvirus 8 infection. The New England journal of medicine. 1998;338(14):948–954. doi: 10.1056/NEJM199804023381403. [DOI] [PubMed] [Google Scholar]
- 31.Butler LM, Osmond DH, Jones AG, Martin JN. Use of saliva as a lubricant in anal sexual practices among homosexual men. Journal of acquired immune deficiency syndromes. 2009;50(2):162–167. doi: 10.1097/QAI.0b013e31819388a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dittmer DP, Damania B. Kaposi sarcoma-associated herpesvirus: immunobiology, oncogenesis, and therapy. J Clin Invest. 2016;126(9):3165–3175. doi: 10.1172/JCI84418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schulz TF, Cesarman E. Kaposi Sarcoma-associated Herpesvirus: mechanisms of oncogenesis. Curr Opin Virol. 2015;14:116–128. doi: 10.1016/j.coviro.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 34.Sun R, Lin SF, Gradoville L, Yuan Y, Zhu F, Miller G. A viral gene that activates lytic cycle expression of Kaposi’s sarcoma-associated herpesvirus. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(18):10866–10871. doi: 10.1073/pnas.95.18.10866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis DA, Rinderknecht AS, Zoeteweij JP, Aoki Y, Read-Connole EL, Tosato G, et al. Hypoxia induces lytic replication of Kaposi sarcoma-associated herpesvirus. Blood. 2001;97(10):3244–3250. doi: 10.1182/blood.v97.10.3244. [DOI] [PubMed] [Google Scholar]
- 36.Li X, Feng J, Sun R. Oxidative stress induces reactivation of Kaposi’s sarcoma-associated herpesvirus and death of primary effusion lymphoma cells. Journal of virology. 2011;85(2):715–724. doi: 10.1128/JVI.01742-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chang J, Renne R, Dittmer D, Ganem D. Inflammatory cytokines and the reactivation of Kaposi’s sarcoma-associated herpesvirus lytic replication. Virology. 2000;266(1):17–25. doi: 10.1006/viro.1999.0077. [DOI] [PubMed] [Google Scholar]
- 38.Moore PS, Boshoff C, Weiss RA, Chang Y. Molecular mimicry of human cytokine and cytokine response pathway genes by KSHV. Science. 1996;274(5293):1739–1744. doi: 10.1126/science.274.5293.1739. [DOI] [PubMed] [Google Scholar]
- 39.Boshoff C, Endo Y, Collins PD, Takeuchi Y, Reeves JD, Schweickart VL, et al. Angiogenic and HIV-inhibitory functions of KSHV-encoded chemokines. Science. 1997;278(5336):290–294. doi: 10.1126/science.278.5336.290. [DOI] [PubMed] [Google Scholar]
- 40.Aoki Y, Jones KD, Tosato G. Kaposi’s sarcoma-associated herpesvirus-encoded interleukin-6. J Hematother Stem Cell Res. 2000;9(2):137–145. doi: 10.1089/152581600319351. [DOI] [PubMed] [Google Scholar]
- 41.Liu C, Okruzhnov Y, Li H, Nicholas J. Human herpesvirus 8 (HHV-8)-encoded cytokines induce expression of and autocrine signaling by vascular endothelial growth factor (VEGF) in HHV-8-infected primary-effusion lymphoma cell lines and mediate VEGF-independent antiapoptotic effects. Journal of virology. 2001;75(22):10933–10940. doi: 10.1128/JVI.75.22.10933-10940.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Uldrick TS, Wang V, O’Mahony D, Aleman K, Wyvill KM, Marshall V, et al. An interleukin-6-related systemic inflammatory syndrome in patients co-infected with Kaposi sarcoma-associated herpesvirus and HIV but without Multicentric Castleman disease. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2010;51(3):350–358. doi: 10.1086/654798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Friborg J, Jr, Kong W, Hottiger MO, Nabel GJ. p53 inhibition by the LANA protein of KSHV protects against cell death. Nature. 1999;402(6764):889–894. doi: 10.1038/47266. [DOI] [PubMed] [Google Scholar]
- 44.Lagos D, Trotter MW, Vart RJ, Wang HW, Matthews NC, Hansen A, et al. Kaposi sarcoma herpesvirus-encoded vFLIP and vIRF1 regulate antigen presentation in lymphatic endothelial cells. Blood. 2007;109(4):1550–1558. doi: 10.1182/blood-2006-05-024034. [DOI] [PubMed] [Google Scholar]
- 45.Schmidt K, Wies E, Neipel F. Kaposi’s sarcoma-associated herpesvirus viral interferon regulatory factor 3 inhibits gamma interferon and major histocompatibility complex class II expression. Journal of virology. 2011;85(9):4530–4537. doi: 10.1128/JVI.02123-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ishido S, Wang C, Lee BS, Cohen GB, Jung JU. Downregulation of major histocompatibility complex class I molecules by Kaposi’s sarcoma-associated herpesvirus K3 and K5 proteins. Journal of virology. 2000;74(11):5300–5309. doi: 10.1128/jvi.74.11.5300-5309.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haque M, Ueda K, Nakano K, Hirata Y, Parravicini C, Corbellino M, et al. Major histocompatibility complex class I molecules are down-regulated at the cell surface by the K5 protein encoded by Kaposi’s sarcoma-associated herpesvirus/human herpesvirus-8. The Journal of general virology. 2001;82(Pt 5):1175–1180. doi: 10.1099/0022-1317-82-5-1175. [DOI] [PubMed] [Google Scholar]
- 48.An J, Sun Y, Sun R, Rettig MB. Kaposi’s sarcoma-associated herpesvirus encoded vFLIP induces cellular IL-6 expression: the role of the NF-kappaB and JNK/AP1 pathways. Oncogene. 2003;22(22):3371–3385. doi: 10.1038/sj.onc.1206407. [DOI] [PubMed] [Google Scholar]
- 49.Grossmann C, Podgrabinska S, Skobe M, Ganem D. Activation of NF-kappaB by the latent vFLIP gene of Kaposi’s sarcoma-associated herpesvirus is required for the spindle shape of virus-infected endothelial cells and contributes to their proinflammatory phenotype. Journal of virology. 2006;80(14):7179–7185. doi: 10.1128/JVI.01603-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Forero A, Moore PS, Sarkar SN. Role of IRF4 in IFN-stimulated gene induction and maintenance of Kaposi sarcoma-associated herpesvirus latency in primary effusion lymphoma cells. Journal of immunology. 2013;191(3):1476–1485. doi: 10.4049/jimmunol.1202514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Keller SA, Schattner EJ, Cesarman E. Inhibition of NF-kappaB induces apoptosis of KSHV-infected primary effusion lymphoma cells. Blood. 2000;96(7):2537–2542. [PubMed] [Google Scholar]
- 52.Staskus KA, Zhong W, Gebhard K, Herndier B, Wang H, Renne R, et al. Kaposi’s sarcoma-associated herpesvirus gene expression in endothelial (spindle) tumor cells. Journal of virology. 1997;71(1):715–719. doi: 10.1128/jvi.71.1.715-719.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parravicini C, Chandran B, Corbellino M, Berti E, Paulli M, Moore PS, et al. Differential viral protein expression in Kaposi’s sarcoma-associated herpesvirus-infected diseases: Kaposi’s sarcoma, primary effusion lymphoma, and multicentric Castleman’s disease. The American journal of pathology. 2000;156(3):743–749. doi: 10.1016/S0002-9440(10)64940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sodhi A, Montaner S, Gutkind JS. Does dysregulated expression of a deregulated viral GPCR trigger Kaposi’s sarcomagenesis? FASEB J. 2004;18(3):422–427. doi: 10.1096/fj.03-1035hyp. [DOI] [PubMed] [Google Scholar]
- 55.Grisotto MG, Garin A, Martin AP, Jensen KK, Chan P, Sealfon SC, et al. The human herpesvirus 8 chemokine receptor vGPCR triggers autonomous proliferation of endothelial cells. J Clin Invest. 2006;116(5):1264–1273. doi: 10.1172/JCI26666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Montaner S, Sodhi A, Ramsdell AK, Martin D, Hu J, Sawai ET, et al. The Kaposi’s sarcoma-associated herpesvirus G protein-coupled receptor as a therapeutic target for the treatment of Kaposi’s sarcoma. Cancer research. 2006;66(1):168–174. doi: 10.1158/0008-5472.CAN-05-1026. [DOI] [PubMed] [Google Scholar]
- 57.Oksenhendler E, Carcelain G, Aoki Y, Boulanger E, Maillard A, Clauvel JP, et al. High levels of human herpesvirus 8 viral load, human interleukin-6, interleukin-10, and C reactive protein correlate with exacerbation of multicentric castleman disease in HIV-infected patients. Blood. 2000;96(6):2069–2073. [PubMed] [Google Scholar]
- 58.Suthaus J, Stuhlmann-Laeisz C, Tompkins VS, Rosean TR, Klapper W, Tosato G, et al. HHV-8-encoded viral IL-6 collaborates with mouse IL-6 in the development of multicentric Castleman disease in mice. Blood. 2012;119(22):5173–5181. doi: 10.1182/blood-2011-09-377705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Polizzotto MN, Uldrick TS, Wang V, Aleman K, Wyvill KM, Marshall V, et al. Human and viral interleukin-6 and other cytokines in Kaposi sarcoma herpesvirus-associated multicentric Castleman disease. Blood. 2013;122(26):4189–4198. doi: 10.1182/blood-2013-08-519959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ray A, Marshall V, Uldrick T, Leighty R, Labo N, Wyvill K, et al. Sequence analysis of Kaposi sarcoma-associated herpesvirus (KSHV) microRNAs in patients with multicentric Castleman disease and KSHV-associated inflammatory cytokine syndrome. The Journal of infectious diseases. 2012;205(11):1665–1676. doi: 10.1093/infdis/jis249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McKenzie R, Travis WD, Dolan SA, Pittaluga S, Feuerstein IM, Shelhamer J, et al. The causes of death in patients with human immunodeficiency virus infection: a clinical and pathologic study with emphasis on the role of pulmonary diseases. Medicine (Baltimore) 1991;70(5):326–343. doi: 10.1097/00005792-199109000-00004. [DOI] [PubMed] [Google Scholar]
- 62.Engels EA, Pfeiffer RM, Goedert JJ, Virgo P, McNeel TS, Scoppa SM, et al. Trends in cancer risk among people with AIDS in the United States 1980–2002. Aids. 2006;20(12):1645–1654. doi: 10.1097/01.aids.0000238411.75324.59. [DOI] [PubMed] [Google Scholar]
- 63.Robbins HA, Pfeiffer RM, Shiels MS, Li J, Hall HI, Engels EA. Excess cancers among HIV-infected people in the United States. J Natl Cancer Inst. 2015;107(4) doi: 10.1093/jnci/dju503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dollard SC, Butler LM, Jones AM, Mermin JH, Chidzonga M, Chipato T, et al. Substantial regional differences in human herpesvirus 8 seroprevalence in sub-Saharan Africa: insights on the origin of the “Kaposi’s sarcoma belt”. International journal of cancer. 2010;127(10):2395–2401. doi: 10.1002/ijc.25235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rohner E, Wyss N, Heg Z, Faralli Z, Mbulaiteye SM, Novak U, et al. HIV and human herpesvirus 8 co-infection across the globe: Systematic review and meta-analysis. International journal of cancer. 2016;138(1):45–54. doi: 10.1002/ijc.29687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wabinga HR, Nambooze S, Amulen PM, Okello C, Mbus L, Parkin DM. Trends in the incidence of cancer in Kampala, Uganda 1991–2010. International journal of cancer. 2014;135(2):432–439. doi: 10.1002/ijc.28661. [DOI] [PubMed] [Google Scholar]
- 67.Dupin N, Fisher C, Kellam P, Ariad S, Tulliez M, Franck N, et al. Distribution of human herpesvirus-8 latently infected cells in Kaposi’s sarcoma, multicentric Castleman’s disease, and primary effusion lymphoma. Proceedings of the National Academy of Sciences of the United States of America. 1999;96(8):4546–4551. doi: 10.1073/pnas.96.8.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Said JW, Shintaku IP, Asou H, deVos S, Baker J, Hanson G, et al. Herpesvirus 8 inclusions in primary effusion lymphoma: report of a unique case with T-cell phenotype. Archives of pathology & laboratory medicine. 1999;123(3):257–260. doi: 10.5858/1999-123-0257-HIIPEL. [DOI] [PubMed] [Google Scholar]
- 69.Hsi ED, Foreman KE, Duggan J, Alkan S, Kauffman CA, Aronow HD, et al. Molecular and pathologic characterization of an AIDS-related body cavity-based lymphoma, including ultrastructural demonstration of human herpesvirus-8: a case report. The American journal of surgical pathology. 1998;22(4):493–499. doi: 10.1097/00000478-199804000-00016. [DOI] [PubMed] [Google Scholar]
- 70.Wakely PE, Jr, Menezes G, Nuovo GJ. Primary effusion lymphoma: cytopathologic diagnosis using in situ molecular genetic analysis for human herpesvirus 8. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2002;15(9):944–950. doi: 10.1038/modpathol.3880635. [DOI] [PubMed] [Google Scholar]
- 71.Patel RM, Goldblum JR, Hsi ED. Immunohistochemical detection of human herpes virus-8 latent nuclear antigen-1 is useful in the diagnosis of Kaposi sarcoma. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2004;17(4):456–460. doi: 10.1038/modpathol.3800061. [DOI] [PubMed] [Google Scholar]
- 72.Pantanowitz L, Grayson W, Simonart T, Dezube BJ. Pathology of Kaposi’s sarcoma. J HIV Ther. 2009;14(2):41–47. [PubMed] [Google Scholar]
- 73.Gill P, Tsai Y, Rao AP, Jones P. Clonality in Kaposi’s sarcoma. The New England journal of medicine. 1997;337(8):570–571. doi: 10.1056/NEJM199708213370813. discussion 571–572. [DOI] [PubMed] [Google Scholar]
- 74.Gill PS, Tsai YC, Rao AP, Spruck CH, 3rd, Zheng T, Harrington WA, Jr, et al. Evidence for multiclonality in multicentric Kaposi’s sarcoma. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(14):8257–8261. doi: 10.1073/pnas.95.14.8257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rabkin CS, Janz S, Lash A, Coleman AE, Musaba E, Liotta L, et al. Monoclonal origin of multicentric Kaposi’s sarcoma lesions. The New England journal of medicine. 1997;336(14):988–993. doi: 10.1056/NEJM199704033361403. [DOI] [PubMed] [Google Scholar]
- 76.Cancian L, Hansen A, Boshoff C. Cellular origin of Kaposi’s sarcoma and Kaposi’s sarcoma-associated herpesvirus-induced cell reprogramming. Trends Cell Biol. 2013;23(9):421–432. doi: 10.1016/j.tcb.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 77.Wang HW, Trotter MW, Lagos D, Bourboulia D, Henderson S, Makinen T, et al. Kaposi sarcoma herpesvirus-induced cellular reprogramming contributes to the lymphatic endothelial gene expression in Kaposi sarcoma. Nat Genet. 2004;36(7):687–693. doi: 10.1038/ng1384. [DOI] [PubMed] [Google Scholar]
- 78.Haque M, Davis DA, Wang V, Widmer I, Yarchoan R. Kaposi’s sarcoma-associated herpesvirus (human herpesvirus 8) contains hypoxia response elements: relevance to lytic induction by hypoxia. Journal of virology. 2003;77(12):6761–6768. doi: 10.1128/JVI.77.12.6761-6768.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cai Q, Lan K, Verma SC, Si H, Lin D, Robertson ES. Kaposi’s sarcoma-associated herpesvirus latent protein LANA interacts with HIF-1 alpha to upregulate RTA expression during hypoxia: Latency control under low oxygen conditions. Journal of virology. 2006;80(16):7965–7975. doi: 10.1128/JVI.00689-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Carroll PA, Kenerson HL, Yeung RS, Lagunoff M. Latent Kaposi’s sarcoma-associated herpesvirus infection of endothelial cells activates hypoxia-induced factors. Journal of virology. 2006;80(21):10802–10812. doi: 10.1128/JVI.00673-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Viollet C, Davis DA, Tekeste SS, Reczko M, Ziegelbauer JM, Pezzella F, et al. RNA Sequencing Reveals that Kaposi Sarcoma-Associated Herpesvirus Infection Mimics Hypoxia Gene Expression Signature. PLoS pathogens. 2017;13(1):e1006143. doi: 10.1371/journal.ppat.1006143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Antman K, Chang Y. Kaposi’s sarcoma. New Engl J Med. 2000;342(14):1027–1038. doi: 10.1056/NEJM200004063421407. [DOI] [PubMed] [Google Scholar]
- 83.Krown SE, Metroka C, Wernz JC. Kaposi’s sarcoma in the acquired immune deficiency syndrome: a proposal for uniform evaluation, response, and staging criteria. AIDS Clinical Trials Group Oncology Committee. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1989;7(9):1201–1207. doi: 10.1200/JCO.1989.7.9.1201. [DOI] [PubMed] [Google Scholar]
- 84.Krown SE, Testa MA, Huang J. AIDS-related Kaposi’s sarcoma: prospective validation of the AIDS Clinical Trials Group staging classification. AIDS Clinical Trials Group Oncology Committee. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1997;15(9):3085–3092. doi: 10.1200/JCO.1997.15.9.3085. [DOI] [PubMed] [Google Scholar]
- 85.Mosam A, Shaik F, Uldrick TS, Esterhuizen T, Friedland GH, Scadden DT, et al. A randomized controlled trial of highly active antiretroviral therapy versus highly active antiretroviral therapy and chemotherapy in therapy-naive patients with HIV-associated Kaposi sarcoma in South Africa. Journal of acquired immune deficiency syndromes. 2012;60(2):150–157. doi: 10.1097/QAI.0b013e318251aedd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nasti G, Talamini R, Antinori A, Martellotta F, Jacchetti G, Chiodo F, et al. AIDS-related Kaposi’s Sarcoma: evaluation of potential new prognostic factors and assessment of the AIDS Clinical Trial Group Staging System in the Haart Era--the Italian Cooperative Group on AIDS and Tumors and the Italian Cohort of Patients Naive From Antiretrovirals. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2003;21(15):2876–2882. doi: 10.1200/JCO.2003.10.162. [DOI] [PubMed] [Google Scholar]
- 87.Bower M, Weir J, Francis N, Newsom-Davis T, Powles S, Crook T, et al. The effect of HAART in 254 consecutive patients with AIDS-related Kaposi’s sarcoma. Aids. 2009;23(13):1701–1706. doi: 10.1097/QAD.0b013e32832d080d. [DOI] [PubMed] [Google Scholar]
- 88.Krown SE. Highly active antiretroviral therapy in AIDS-associated Kaposi’s sarcoma: implications for the design of therapeutic trials in patients with advanced, symptomatic Kaposi’s sarcoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2004;22(3):399–402. doi: 10.1200/JCO.2004.08.064. [DOI] [PubMed] [Google Scholar]
- 89.Levy JA, Ziegler JL. Acquired immunodeficiency syndrome is an opportunistic infection and Kaposi’s sarcoma results from secondary immune stimulation. Lancet. 1983;2(8341):78–81. doi: 10.1016/s0140-6736(83)90062-4. [DOI] [PubMed] [Google Scholar]
- 90.Letang E, Lewis JJ, Bower M, Mosam A, Borok M, Campbell TB, et al. Immune reconstitution inflammatory syndrome associated with Kaposi sarcoma: higher incidence and mortality in Africa than in the UK. Aids. 2013;27(10):1603–1613. doi: 10.1097/QAD.0b013e328360a5a1. [DOI] [PubMed] [Google Scholar]
- 91.Gill PS, Loureiro C, Bernstein-Singer M, Rarick MU, Sattler F, Levine AM. Clinical effect of glucocorticoids on Kaposi sarcoma related to the acquired immunodeficiency syndrome (AIDS) Annals of internal medicine. 1989;110(11):937–940. doi: 10.7326/0003-4819-110-11-937. [DOI] [PubMed] [Google Scholar]
- 92.Gantt S, Carlsson J, Ikoma M, Gachelet E, Gray M, Geballe AP, et al. The HIV protease inhibitor nelfinavir inhibits Kaposi’s sarcoma-associated herpesvirus replication in vitro. Antimicrobial agents and chemotherapy. 2011;55(6):2696–2703. doi: 10.1128/AAC.01295-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sgadari C, Barillari G, Toschi E, Carlei D, Bacigalupo I, Baccarini S, et al. HIV protease inhibitors are potent anti-angiogenic molecules and promote regression of Kaposi sarcoma. Nature medicine. 2002;8(3):225–232. doi: 10.1038/nm0302-225. [DOI] [PubMed] [Google Scholar]
- 94.Martinez V, Caumes E, Gambotti L, Ittah H, Morini JP, Deleuze J, et al. Remission from Kaposi’s sarcoma on HAART is associated with suppression of HIV replication and is independent of protease inhibitor therapy. Br J Cancer. 2006;94(7):1000–1006. doi: 10.1038/sj.bjc.6603056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Portsmouth S, Stebbing J, Gill J, Mandalia S, Bower M, Nelson M, et al. A comparison of regimens based on non-nucleoside reverse transcriptase inhibitors or protease inhibitors in preventing Kaposi’s sarcoma. Aids. 2003;17(11):F17–22. doi: 10.1097/00002030-200307250-00001. [DOI] [PubMed] [Google Scholar]
- 96.Kowalkowski MA, Kramer JR, Richardson PR, Suteria I, Chiao EY. Use of boosted protease inhibitors reduces Kaposi sarcoma incidence among male veterans with HIV infection. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2015;60(9):1405–1414. doi: 10.1093/cid/civ012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Walmsley S, Northfelt DW, Melosky B, Conant M, Friedman-Kien AE, Wagner B. Treatment of AIDS-related cutaneous Kaposi’s sarcoma with topical alitretinoin (9-cis-retinoic acid) gel. Panretin Gel North American Study Group. Journal of acquired immune deficiency syndromes. 1999;22(3):235–246. doi: 10.1097/00126334-199911010-00004. [DOI] [PubMed] [Google Scholar]
- 98.Yarchoan R, Uldrick TS, Polizzotto MN, Little RF. HIV-associated malignancies. In: DeVita VTJ, Lawrence TS, Rosenberg SA, editors. Cancer: Principals and Practice of Oncology. Philadelphia, PA: Wolters Kluwer Health; 2015. pp. 1780–1793. [Google Scholar]
- 99.Cooley T, Henry D, Tonda M, Sun S, O’Connell M, Rackoff W. A randomized, double-blind study of pegylated liposomal doxorubicin for the treatment of AIDS-related Kaposi’s sarcoma. The oncologist. 2007;12(1):114–123. doi: 10.1634/theoncologist.12-1-114. [DOI] [PubMed] [Google Scholar]
- 100.Northfelt DW, Dezube BJ, Thommes JA, Miller BJ, Fischl MA, Friedman-Kien A, et al. Pegylated-liposomal doxorubicin versus doxorubicin, bleomycin, and vincristine in the treatment of AIDS-related Kaposi’s sarcoma: results of a randomized phase III clinical trial. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1998;16(7):2445–2451. doi: 10.1200/JCO.1998.16.7.2445. [DOI] [PubMed] [Google Scholar]
- 101.Cianfrocca M, Lee S, Von Roenn J, Tulpule A, Dezube BJ, Aboulafia DM, et al. Randomized trial of paclitaxel versus pegylated liposomal doxorubicin for advanced human immunodeficiency virus-associated Kaposi sarcoma: evidence of symptom palliation from chemotherapy. Cancer. 2010;116(16):3969–3977. doi: 10.1002/cncr.25362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Welles L, Saville MW, Lietzau J, Pluda JM, Wyvill KM, Feuerstein I, et al. Phase II trial with dose titration of paclitaxel for the therapy of human immunodeficiency virus-associated Kaposi’s sarcoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1998;16(3):1112–1121. doi: 10.1200/JCO.1998.16.3.1112. [DOI] [PubMed] [Google Scholar]
- 103.Krown SE, Real FX, Cunningham-Rundles S, Myskowski PL, Koziner B, Fein S, et al. Preliminary observations on the effect of recombinant leukocyte A interferon in homosexual men with Kaposi’s sarcoma. N Engl J Med. 1983;308:1071–1076. doi: 10.1056/NEJM198305053081806. [DOI] [PubMed] [Google Scholar]
- 104.Little RF, Merced-Galindez F, Staskus K, Whitby D, Aoki Y, Humphrey R, et al. A pilot study of cidofovir in patients with Kaposi’s sarcoma. J Infect Dis. 2003;187:149–153. doi: 10.1086/346159. [DOI] [PubMed] [Google Scholar]
- 105.Krown SE, Dittmer DP, Cesarman E. Pilot study of oral valganciclovir therapy in patients with classic Kaposi sarcoma. The Journal of infectious diseases. 2011;203(8):1082–1086. doi: 10.1093/infdis/jiq177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Stallone G, Schena A, Infante B, Di Paolo S, Loverre A, Maggio G, et al. Sirolimus for Kaposi’s sarcoma in renal-transplant recipients. The New England journal of medicine. 2005;352(13):1317–1323. doi: 10.1056/NEJMoa042831. [DOI] [PubMed] [Google Scholar]
- 107.Krown SE, Roy D, Lee JY, Dezube BJ, Reid EG, Venkataramanan R, et al. Rapamycin with antiretroviral therapy in AIDS-associated Kaposi sarcoma: an AIDS Malignancy Consortium study. Journal of acquired immune deficiency syndromes. 2012;59(5):447–454. doi: 10.1097/QAI.0b013e31823e7884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cianfrocca M, Cooley TP, Lee JY, Rudek MA, Scadden DT, Ratner L, et al. Matrix metalloproteinase inhibitor COL-3 in the treatment of AIDS-related Kaposi’s sarcoma: a phase I AIDS malignancy consortium study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2002;20(1):153–159. doi: 10.1200/JCO.2002.20.1.153. [DOI] [PubMed] [Google Scholar]
- 109.Koon HB, Bubley GJ, Pantanowitz L, Masiello D, Smith B, Crosby K, et al. Imatinib-induced regression of AIDS-related Kaposi’s sarcoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2005;23(5):982–989. doi: 10.1200/JCO.2005.06.079. [DOI] [PubMed] [Google Scholar]
- 110.Little RF, Pluda JM, Wyvill KM, Rodriguez-Chavez IR, Tosato G, Catanzaro AT, et al. Activity of subcutaneous interleukin-12 in AIDS-related Kaposi sarcoma. Blood. 2006;107(12):4650–4657. doi: 10.1182/blood-2005-11-4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Little RF, Wyvill KM, Pluda JM, Welles L, Marshall V, Figg WD, et al. Activity of thalidomide in AIDS-related Kaposi’s sarcoma. J Clin Oncol. 2000;18(3):2593–2602. doi: 10.1200/JCO.2000.18.13.2593. [DOI] [PubMed] [Google Scholar]
- 112.Polizzotto MN, Uldrick TS, Wyvill KM, Aleman K, Peer CJ, Bevans M, et al. Pomalidomide for Symptomatic Kaposi’s Sarcoma in People With and Without HIV Infection: A Phase I/II Study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016;34(34):4125–4131. doi: 10.1200/JCO.2016.69.3812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Uldrick TS, Wyvill KM, Kumar P, O’Mahony D, Bernstein W, Aleman K, et al. Phase II study of bevacizumab in patients with HIV-associated Kaposi’s sarcoma receiving antiretroviral therapy. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012;30(13):1476–1483. doi: 10.1200/JCO.2011.39.6853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chadburn A, Hyjek E, Mathew S, Cesarman E, Said J, Knowles DM. KSHV-positive solid lymphomas represent an extra-cavitary variant of primary effusion lymphoma. The American journal of surgical pathology. 2004;28(11):1401–1416. doi: 10.1097/01.pas.0000138177.10829.5c. [DOI] [PubMed] [Google Scholar]
- 115.Gaidano G, Gloghini A, Gattei V, Rossi MF, Cilia AM, Godeas C, et al. Association of Kaposi’s sarcoma-associated herpesvirus-positive primary effusion lymphoma with expression of the CD138/syndecan-1 antigen. Blood. 1997;90(12):4894–4900. [PubMed] [Google Scholar]
- 116.Dong HY, Wang W, Uldrick TS, Gangi M. Human herpesvirus 8- and Epstein-Barr virus-associated solitary B cell lymphoma with a T cell immunophenotype. Leuk Lymphoma. 2013;54(7):1560–1563. doi: 10.3109/10428194.2012.747680. [DOI] [PubMed] [Google Scholar]
- 117.Sanchez-Martin D, Uldrick TS, Kwak H, O’hnuki H, Polizzotto MN, Annunziata CM, et al. Evidence for a mesothelial origin of body cavity effusion lymphomas. JNCI. 2017 doi: 10.1093/jnci/djx016. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Guillet S, Gerard L, Meignin V, Agbalika F, Cuccini W, Denis B, et al. Classic and extracavitary primary effusion lymphoma in 51 HIV-infected patients from a single institution. American journal of hematology. 2016;91(2):233–237. doi: 10.1002/ajh.24251. [DOI] [PubMed] [Google Scholar]
- 119.Uldrick TS, Polizzotto MN, Filie A, Aleman K, Wyvill KM, Little RF, et al. Clinical, Immunologic, and Virologic Findings in Kaposi Sarcoma Herpesvirus (KSHV)-Associated Lymphomas Suggest KSHV-Associated Inflammatory Syndromes Contribute to Symptoms and Disease Pathogenesis. In. 54th American Society of Hematology Annual Meeting; Atlanta, GA. 2012. [Google Scholar]
- 120.Boulanger E, Daniel MT, Agbalika F, Oksenhendler E. Combined chemotherapy including high-dose methotrexate in KSHV/HHV8-associated primary effusion lymphoma. American journal of hematology. 2003;73(3):143–148. doi: 10.1002/ajh.10341. [DOI] [PubMed] [Google Scholar]
- 121.Uldrick TSBM, Polizzotto M, Aleman K, Wyvill K, Goncalves P, et al. Inflammatory cytokines, hyperferritinemia and IgE are prognostic in patients with KSHV-associated lymphomas treated with curative intent therapy. In. American Society of Hematology. 2014:3001. [Google Scholar]
- 122.Carbone A, Gloghini A, Cozzi MR, Capello D, Steffan A, Monini P, et al. Expression of MUM1/IRF4 selectively clusters with primary effusion lymphoma among lymphomatous effusions: implications for disease histogenesis and pathogenesis. British journal of haematology. 2000;111(1):247–257. doi: 10.1046/j.1365-2141.2000.02329.x. [DOI] [PubMed] [Google Scholar]
- 123.Gopalakrishnan R, Matta H, Tolani B, Triche T, Jr, Chaudhary PM. Immunomodulatory drugs target IKZF1-IRF4-MYC axis in primary effusion lymphoma in a cereblon-dependent manner and display synergistic cytotoxicity with BRD4 inhibitors. Oncogene. 2016;35(14):1797–1810. doi: 10.1038/onc.2015.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Davis DA, Anagho HA, Mishra SK, Carey RF, Takamatsu Y, Maeda K, et al. Lenalidomide and pomalidomide inhibit KSHV-induced downregulation of MHC class I expression in primary effusion lymphoma cells. 15th International Conference on Malignancies in AIDS and Other Acquired Immunodeficiencies; Bethesda, MD: National Cancer Institute; 2015. [Google Scholar]
- 125.Waterston A, Bower M. Fifty years of multicentric Castleman’s disease. Acta Oncol. 2004;43(8):698–704. doi: 10.1080/02841860410002752. [DOI] [PubMed] [Google Scholar]
- 126.Uldrick TS, Polizzotto MN, Yarchoan R. Recent advances in Kaposi sarcoma herpesvirus-associated multicentric Castleman disease. Curr Opin Oncol. 2012;24(5):495–505. doi: 10.1097/CCO.0b013e328355e0f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Oksenhendler E, Duarte M, Soulier J, Cacoub P, Welker Y, Cadranel J, et al. Multicentric Castleman’s disease in HIV infection: a clinical and pathological study of 20 patients. Aids. 1996;10(1):61–67. [PubMed] [Google Scholar]
- 128.Oksenhendler E, Boutboul D, Beldjord K, Meignin V, de Labarthe A, Fieschi C, et al. Human herpesvirus 8+ polyclonal IgMlambda B-cell lymphocytosis mimicking plasmablastic leukemia/lymphoma in HIV-infected patients. Eur J Haematol. 2013;91(6):497–503. doi: 10.1111/ejh.12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bower M, Newsom-Davis T, Naresh K, Merchant S, Lee B, Gazzard B, et al. Clinical Features and Outcome in HIV-Associated Multicentric Castleman’s Disease. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29(18):2481–2486. doi: 10.1200/JCO.2010.34.1909. [DOI] [PubMed] [Google Scholar]
- 130.Oksenhendler E, Boulanger E, Galicier L, Du MQ, Dupin N, Diss TC, et al. High incidence of Kaposi sarcoma-associated herpesvirus-related non-Hodgkin lymphoma in patients with HIV infection and multicentric Castleman disease. Blood. 2002;99(7):2331–2336. doi: 10.1182/blood.v99.7.2331. [DOI] [PubMed] [Google Scholar]
- 131.Gerard L, Michot JM, Burcheri S, Fieschi C, Longuet P, Delcey V, et al. Rituximab decreases the risk of lymphoma in patients with HIV-associated multicentric Castleman disease. Blood. 2012;119(10):2228–2233. doi: 10.1182/blood-2011-08-376012. [DOI] [PubMed] [Google Scholar]
- 132.Cronin DM, Warnke RA. Castleman disease: an update on classification and the spectrum of associated lesions. Adv Anat Pathol. 2009;16(4):236–246. doi: 10.1097/PAP.0b013e3181a9d4d3. [DOI] [PubMed] [Google Scholar]
- 133.Dossier A, Meignin V, Fieschi C, Boutboul D, Oksenhendler E, Galicier L. Human herpesvirus 8-related Castleman disease in the absence of HIV infection. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2013;56(6):833–842. doi: 10.1093/cid/cis1009. [DOI] [PubMed] [Google Scholar]
- 134.Hu D, Wang V, Yang M, Abdullah S, Davis DA, Uldrick TS, et al. Induction of Kaposi’s Sarcoma-Associated Herpesvirus-Encoded Viral Interleukin-6 by X-Box Binding Protein 1. Journal of virology. 2015;90(1):368–378. doi: 10.1128/JVI.01192-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Aoki Y, Tosato G, Fonville TW, Pittaluga S. Serum viral interleukin-6 in AIDS-related multicentric Castleman disease. Blood. 2001;97(8):2526–2527. doi: 10.1182/blood.v97.8.2526. [DOI] [PubMed] [Google Scholar]
- 136.Ballon G, Chen K, Perez R, Tam W, Cesarman E. Kaposi sarcoma herpesvirus (KSHV) vFLIP oncoprotein induces B cell transdifferentiation and tumorigenesis in mice. J Clin Invest. 2011;121(3):1141–1153. doi: 10.1172/JCI44417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chen F, Teachey DT, Pequignot E, Frey N, Porter D, Maude SL, et al. Measuring IL-6 and sIL-6R in serum from patients treated with tocilizumab and/or siltuximab following CAR T cell therapy. J Immunol Methods. 2016;434:1–8. doi: 10.1016/j.jim.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Powles T, Stebbing J, Bazeos A, Hatzimichael E, Mandalia S, Nelson M, et al. The role of immune suppression and HHV-8 in the increasing incidence of HIV-associated multicentric Castleman’s disease. Ann Oncol. 2009;20(4):775–779. doi: 10.1093/annonc/mdn697. [DOI] [PubMed] [Google Scholar]
- 139.Sbihi Z, Dossier A, Boutboul D, Galicier L, Parizot C, Emarre A, et al. iNKT and memory B cells alterations in HHV-8 multicentric Castleman disease. Blood. 2016 doi: 10.1182/blood-2016-06-719716. [DOI] [PubMed] [Google Scholar]
- 140.Uldrick TS, Polizzotto MN, Aleman K, O’Mahony D, Wyvill KM, Wang V, et al. High-dose zidovudine plus valganciclovir for Kaposi sarcoma herpesvirus-associated multicentric Castleman disease: a pilot study of virus-activated cytotoxic therapy. Blood. 2011;117(26):6977–6986. doi: 10.1182/blood-2010-11-317610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Uldrick TS, Polizzotto MN, Aleman K, Wyvill KM, Marshall V, Whitby D, et al. Rituximab plus liposomal doxorubicin in HIV-infected patients with KSHV-associated multicentric Castleman disease. Blood. 2014;124(24):3544–3552. doi: 10.1182/blood-2014-07-586800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gopal S, Liomba NG, Montgomery ND, Moses A, Kaimila B, Nyasosela R, et al. Characteristics and survival for HIV-associated multicentric Castleman disease in Malawi. J Int AIDS Soc. 2015;18:20122. doi: 10.7448/IAS.18.1.20122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bower M. How I treat HIV-associated multicentric Castleman disease. Blood. 2010;116(22):4415–4421. doi: 10.1182/blood-2010-07-290213. [DOI] [PubMed] [Google Scholar]
- 144.Marcelin AG, Aaron L, Mateus C, Gyan E, Gorin I, Viard JP, et al. Rituximab therapy for HIV-associated Castleman disease. Blood. 2003;102(8):2786–2788. doi: 10.1182/blood-2003-03-0951. [DOI] [PubMed] [Google Scholar]
- 145.Gerard L, Berezne A, Galicier L, Meignin V, Obadia M, De Castro N, et al. Prospective study of rituximab in chemotherapy-dependent human immunodeficiency virus associated multicentric Castleman’s disease: ANRS 117 CastlemaB Trial. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25(22):3350–3356. doi: 10.1200/JCO.2007.10.6732. [DOI] [PubMed] [Google Scholar]
- 146.Bower M, Powles T, Williams S, Davis TN, Atkins M, Montoto S, et al. Brief communication: rituximab in HIV-associated multicentric Castleman disease. Annals of internal medicine. 2007;147(12):836–839. doi: 10.7326/0003-4819-147-12-200712180-00003. [DOI] [PubMed] [Google Scholar]
- 147.Dalla Pria A, Pinato D, Roe J, Naresh K, Nelson M, Bower M. Relapse of multicentric Castleman’s disease following Rituximab based therapy in HIV-positive patients. Blood. 2017 doi: 10.1182/blood-2016-10-747477. [DOI] [PubMed] [Google Scholar]
- 148.Hoffmann C, Schmid H, Muller M, Teutsch C, van Lunzen J, Esser S, et al. Improved outcome with rituximab in patients with HIV-associated multicentric Castleman disease. Blood. 2011;118(13):3499–3503. doi: 10.1182/blood-2011-02-333633. [DOI] [PubMed] [Google Scholar]
- 149.Pantanowitz L, Fruh K, Marconi S, Moses AV, Dezube BJ. Pathology of rituximab-induced Kaposi sarcoma flare. BMC clinical pathology. 2008;8:7. doi: 10.1186/1472-6890-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Clifford KS, Demierre MF. Progression of classic Kaposi’s sarcoma with rituximab. Journal of the American Academy of Dermatology. 2005;53(1):155–157. doi: 10.1016/j.jaad.2004.12.048. [DOI] [PubMed] [Google Scholar]
- 151.Cannon JS, Hamzeh F, Moore S, Nicholas J, Ambinder RF. Human herpesvirus 8-encoded thymidine kinase and phosphotransferase homologues confer sensitivity to ganciclovir. Journal of virology. 1999;73(6):4786–4793. doi: 10.1128/jvi.73.6.4786-4793.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Gustafson EA, Schinazi RF, Fingeroth JD. Human herpesvirus 8 open reading frame 21 is a thymidine and thymidylate kinase of narrow substrate specificity that efficiently phosphorylates zidovudine but not ganciclovir. Journal of virology. 2000;74(2):684–692. doi: 10.1128/jvi.74.2.684-692.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Davis DA, Singer KE, Reynolds IP, Haque M, Yarchoan R. Hypoxia enhances the phosphorylation and cytotoxicity of ganciclovir and zidovudine in Kaposi’s sarcoma-associated herpesvirus infected cells. Cancer research. 2007;67(14):7003–7010. doi: 10.1158/0008-5472.CAN-07-0939. [DOI] [PubMed] [Google Scholar]
- 154.Polizzotto MN, Uldrick TS, Hu D, Yarchoan R. Clinical Manifestations of Kaposi Sarcoma Herpesvirus Lytic Activation: Multicentric Castleman Disease (KSHV-MCD) and the KSHV Inflammatory Cytokine Syndrome. Frontiers in microbiology. 2012;3:73. doi: 10.3389/fmicb.2012.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tamburro KM, Yang D, Poisson J, Fedoriw Y, Roy D, Lucas A, et al. Vironome of Kaposi sarcoma associated herpesvirus-inflammatory cytokine syndrome in an AIDS patient reveals co-infection of human herpesvirus 8 and human herpesvirus 6A. Virology. 2012;433(1):220–225. doi: 10.1016/j.virol.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Nalwoga A, Cose S, Wakeham K, Miley W, Ndibazza J, Drakeley C, et al. Association between malaria exposure and Kaposi’s sarcoma-associated herpes virus seropositivity in Uganda. Trop Med Int Health. 2015;20(5):665–672. doi: 10.1111/tmi.12464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Stolka K, Ndom P, Hemingway-Foday J, Iriondo-Perez J, Miley W, Labo N, et al. Risk factors for Kaposi’s sarcoma among HIV-positive individuals in a case control study in Cameroon. Cancer Epidemiol. 2014;38(2):137–143. doi: 10.1016/j.canep.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Pfeiffer RM, Wheeler WA, Mbisa G, Whitby D, Goedert JJ, de The G, et al. Geographic heterogeneity of prevalence of the human herpesvirus 8 in sub-Saharan Africa: clues about etiology. Ann Epidemiol. 2010;20(12):958–963. doi: 10.1016/j.annepidem.2010.07.098. [DOI] [PubMed] [Google Scholar]
- 159.Simpson GR, Schulz TF, Whitby D, Cook PM, Boshoff C, Rainbow L, et al. Prevalence of Kaposi’s sarcoma associated herpesvirus infection measured by antibodies to recombinant capsid protein and latent immunofluorescence antigen. Lancet. 1996;348(9035):1133–1138. doi: 10.1016/S0140-6736(96)07560-5. [DOI] [PubMed] [Google Scholar]
- 160.Pelser C, Vitale F, Whitby D, Graubard BI, Messina A, Gafa L, et al. Socio-economic and other correlates of Kaposi sarcoma-associated herpesvirus seroprevalence among older adults in Sicily. J Med Virol. 2009;81(11):1938–1944. doi: 10.1002/jmv.21589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Valdarchi C, Serraino D, Cordiali Fei P, Castilletti C, Trento E, Farchi F, et al. Demographic indicators and risk of infection with human herpesvirus type 8 in Central Italy. Infection. 2007;35(1):22–25. doi: 10.1007/s15010-007-5123-2. [DOI] [PubMed] [Google Scholar]
- 162.de Sanjose S, Mbisa G, Perez-Alvarez S, Benavente Y, Sukvirach S, Hieu NT, et al. Geographic variation in the prevalence of Kaposi sarcoma-associated herpesvirus and risk factors for transmission. The Journal of infectious diseases. 2009;199(10):1449–1456. doi: 10.1086/598523. [DOI] [PubMed] [Google Scholar]
- 163.Davidovici B, Karakis I, Bourboulia D, Ariad S, Zong J, Benharroch D, et al. Seroepidemiology and molecular epidemiology of Kaposi’s sarcoma-associated herpesvirus among Jewish population groups in Israel. J Natl Cancer Inst. 2001;93(3):194–202. doi: 10.1093/jnci/93.3.194. [DOI] [PubMed] [Google Scholar]
- 164.Katano H, Yokomaku Y, Fukumoto H, Kanno T, Nakayama T, Shingae A, et al. Seroprevalence of Kaposi’s sarcoma-associated herpesvirus among men who have sex with men in Japan. J Med Virol. 2013;85(6):1046–1052. doi: 10.1002/jmv.23558. [DOI] [PubMed] [Google Scholar]
- 165.Fu B, Sun F, Li B, Yang L, Zeng Y, Sun X, et al. Seroprevalence of Kaposi’s sarcoma-associated herpesvirus and risk factors in Xinjiang, China. J Med Virol. 2009;81(8):1422–1431. doi: 10.1002/jmv.21550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Zhang T, Shao X, Chen Y, Zhang T, Minhas V, Wood C, et al. Human herpesvirus 8 seroprevalence, China. Emerg Infect Dis. 2012;18(1):150–152. doi: 10.3201/eid1801.102070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Nascimento MC, Sumita LM, Souza VU, Weiss HA, Oliveira J, Mascheretti M, et al. Seroprevalence of Kaposi sarcoma-associated herpesvirus and other serologic markers in the Brazilian Amazon. Emerg Infect Dis. 2009;15(4):663–667. doi: 10.3201/eid1504.081488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Pellett PE, Wright DJ, Engels EA, Ablashi DV, Dollard SC, Forghani B, et al. Multicenter comparison of serologic assays and estimation of human herpesvirus 8 seroprevalence among US blood donors. Transfusion. 2003;43(9):1260–1268. doi: 10.1046/j.1537-2995.2003.00490.x. [DOI] [PubMed] [Google Scholar]
- 169.Maskew M, Macphail AP, Whitby D, Egger M, Wallis CL, Fox MP. Prevalence and predictors of kaposi sarcoma herpes virus seropositivity: a cross-sectional analysis of HIV-infected adults initiating ART in Johannesburg, South Africa. Infect Agent Cancer. 2011;6:22. doi: 10.1186/1750-9378-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Osmond DH, Buchbinder S, Cheng A, Graves A, Vittinghoff E, Cossen CK, et al. Prevalence of Kaposi sarcoma-associated herpesvirus infection in homosexual men at beginning of and during the HIV epidemic. JAMA. 2002;287(2):221–225. doi: 10.1001/jama.287.2.221. [DOI] [PubMed] [Google Scholar]
- 171.Labo N, Miley W, Benson CA, Campbell TB, Whitby D. Epidemiology of Kaposi’s sarcoma-associated herpesvirus in HIV-1-infected US persons in the era of combination antiretroviral therapy. Aids. 2015;29(10):1217–1225. doi: 10.1097/QAD.0000000000000682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Guanira JV, Casper C, Lama JR, Morrow R, Montano SM, Caballero P, et al. Prevalence and correlates of human herpesvirus 8 infection among Peruvian men who have sex with men. Journal of acquired immune deficiency syndromes. 2008;49(5):557–562. doi: 10.1097/QAI.0b013e31818d5bf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Grulich AE, Cunningham P, Munier ML, Prestage G, Amin J, Ringland C, et al. Sexual behaviour and human herpesvirus 8 infection in homosexual men in Australia. Sex Health. 2005;2(1):13–18. doi: 10.1071/sh04029. [DOI] [PubMed] [Google Scholar]
- 174.Liu Z, Fang Q, Zuo J, Wang J, Chen Y, Minhas V, et al. High seroprevalence of human herpesvirus 8 and herpes simplex virus 2 infections in men who have sex with men in Shanghai, China. J Med Virol. 2017;89(5):887–894. doi: 10.1002/jmv.24718. [DOI] [PubMed] [Google Scholar]
- 175.Casper C, Carrell D, Miller KG, Judson FD, Meier AS, Pauk JS, et al. HIV serodiscordant sex partners and the prevalence of human herpesvirus 8 infection among HIV negative men who have sex with men: baseline data from the EXPLORE Study. Sex Transm Infect. 2006;82(3):229–235. doi: 10.1136/sti.2005.016568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Di Benedetto MA, Di Piazza F, Amodio E, Taormina S, Romano N, Firenze A. Prevalence of sexually transmitted infections and enteric protozoa among homosexual men in western Sicily (south Italy) J Prev Med Hyg. 2012;53(4):181–185. [PubMed] [Google Scholar]
- 177.Zhang T, Lin H, Minhas V, Zhu W, Wood C, He N. Prevalence and correlates of Kaposi’s sarcoma-associated herpesvirus infection in a sample of men who have sex with men in Eastern China. Epidemiol Infect. 2013;141(9):1823–1830. doi: 10.1017/S0950268812002361. [DOI] [PMC free article] [PubMed] [Google Scholar]