Abstract
Context:
Little is known about the hopes patients with advanced (incurable) cancer have for their treatment.
Objectives:
To describe the treatment hopes of advanced cancer patients, factors associated with expressing specific hopes, and the persons with whom hopes are discussed.
Methods:
We surveyed 265 advanced cancer patients in the USA about their hopes for treatment at baseline and after three months. We developed a taxonomy of hopes for treatment, which two investigators used to independently code patient responses. We explored associations between hopes for cure and patient covariates.
Results:
We developed 8 categories of hopes. We were able to apply these codes reliably, and 95% of the patient’s responses fit at least one hope category. The hope categories in order of descending baseline prevalence were: quality of life, life extension, tumor stabilization, remission, milestone, unqualified cure, control not otherwise specified (NOS), and cure tempered by realism. Most patients reported discussing hopes with partners, family/friends, and oncologists; a minority reported discussing hopes with nurses, primary care physicians (PCPs), clergy, or support groups. In logistic regression analysis, unqualified hopes for cure were more likely in younger patients and in those who did not endorse discussing their hopes with primary care physicians.
Conclusion:
Advanced cancer patients harbor a range of treatment hopes. These hopes often are not discussed with key members of the healthcare team. Younger age and lack of discussion of hopes with PCPs may lead to less realistic hopes for cure.
Keywords: Hope, advanced cancer, goals, end-of-life care, communication, palliative care
INTRODUCTION
Among patients confronting serious illness such as advanced cancer, hope takes on multiple forms.1–5 In general, hope is the wish for – or belief in the possibility of – a better future. A hope can also be a desire that a decision or intervention might produce a specific outcome. According to Coulehan, hopes differ from expectations in that hopes are always positive, and may be improbable.2
Physicians of advanced cancer patients are faced with the challenge of maintaining or improving a patient’s well-being in the face of an incurable illness. One way they may address this is to help patients establish or prioritize more concrete and realistic goals,2 such as decreasing nausea, going on a vacation, or making financial arrangements. When hopes are misaligned with what is medically realistic (e.g. when patients with incurable disease hope for a cure), patients may avoid advanced directive discussions,6 choose inappropriately aggressive care,7 and endure excessive psychological distress.3,8 It is important for physicians to understand their patient’s hopes for treatment to facilitate informed patient-centered decision making.
Previous studies have investigated advanced cancer patients’ treatment goals using both closed- and open-ended questions.9–17 However, these studies have been limited by small sample sizes,9,11,15 including patients with serious illnesses other than advanced cancer,11 including only a small subset of cancer types,9,12,13 including only patients who expected to be offered palliative chemotherapy,16 or using cross-sectional study designs.9,10
In the current study, we asked patients with advanced cancer what they were “hoping for from their cancer treatment” at two points in time to address our research questions. First, among patients with advanced cancer, what are patients’ hopes for treatment and how prevalent are these hopes? Specifically, how often do patients with advanced cancer say that they hope their treatment will lead to cure? Second, with whom do patients with advanced cancer discuss their hopes? Third, what demographic, clinical, and contextual factors are associated with hopes for unqualified cure?
METHODS
Overview
Our analysis was based on survey data from the Values and Options in Cancer Care (VOICE) cluster randomized clinical trial (RCT), which measured the effect of oncologist communication training and patient coaching on communication between oncologists and adult patients with advanced non-hematologic cancer. In the current study, we reviewed survey responses regarding patients’ hopes for treatment from baseline assessment (n=265) and three months after study entry (n=216). The oncologist was the unit of randomization and we used stratified randomization to balance the number of breast cancer specialists across arms. Details of the parent study have been published previously.18,19
Clinician and Patient Recruitment
Medical oncologists were recruited from participating community-based clinics, hospitals, and academic medical centers in Sacramento, California and Rochester, New York. Research assistants reviewed clinic rosters of participating physicians to recruit patients who were 21 years or older, English speaking, and diagnosed with either stage IV non-hematologic cancer or stage III cancer and whose oncologist “would not be surprised” if the patient died within the next year. Among cancer patients, a “no” response to this “surprise question” has been associated with a seven times greater one-year mortality.20 Patients who were hospitalized or enrolled in hospice were ineligible.
Elicitation and Coding of “Hopes for Treatment”
At baseline, most surveys were administered in person and a few by telephone. At follow-up, surveys were administered in person when feasible but by telephone for patients who were not scheduled for follow up appointments during the data collection window. Telephone surveys were completed by the same research personnel whom the patients had previously met at study entry. The focus of this study was the open-ended survey question: “What are you hoping for at this time in your cancer treatment?” This question was not further qualified, but patients answered in the context of ongoing care by their medical oncologist. Patients were allowed time to formulate hopes in their own words, which were then transcribed verbatim.
A three-person coding team (CC, JD, and RK) reviewed verbatim survey responses to the question regarding hopes. Using inductive reasoning, the team developed a taxonomy and codebook based on the first 25 patient responses from the baseline survey. The codebook included category names, operational definitions, instructions for code application, and illustrative quotes; these are summarized in Table 2. Many patients expressed multiple hopes for treatment, so the number of hopes expressed at each time point exceeded the number of patients.
Table 2.
Categories of Hopes for Treatment Including Frequency, Definitions, and Examples
| Category | Baseline | 3 months | Definition | Examples |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Unqualified cure | 33 (12) | 17 (8) | To be permanently free of disease | “To be cured. So I can enjoy my life with no worries” |
| Cure tempered by realism | 14 (5) | 3 (1) | To wish to be free of disease, but realizing this is unrealistic | “A cure...I would love, but I know that is not possible” |
| Quality of life | 110 (42) | 78 (36) | To continue or improve well-being, including physical, emotional, and social functioning | “Walk strongly and feel normal when I get up” |
| Milestone | 36 (14) | 8 (4) | To survive long enough to experience a specific life event, phase of life, or significant accomplishment | “See [my] grandchildren, daughter was just married” |
| Life extension | 84 (32) | 57 (26) | To sustain life beyond what could be anticipated in the absence of treatment | “Extend my life as long as possible” |
| Tumor stabilization | 68 (26) | 66 (31) | To shrink, slow, or maintain, the tumor short of remission | “Stabilize the spread of cancer. Keep it in check” |
| Remission | 54 (20) | 34 (16) | To achieve temporary disappearance of clinically detectable cancer | “Knocking the hell out of cancer…put it in remission” |
| Control NOS | 25 (9) | 26 (12) | To achieve control that cannot readily be classified as relating to life extension, remission, or stabilization | “Show improvement from the treatment” |
a At baseline, n=265 patients, they expressed 424 hopes total. At 3 months, n=216 patients, they expressed 289 hopes total. As some patients voiced more than one hope, the percentages of patients expressing each hope at each timepoint add up to more than 100%
Following codebook development, CC and JD independently coded the remaining 240 baseline responses and all 216 of the three-month responses with good reliability. The mean (95% confidence interval) of the category specific kappa values, was 0.76 (0.71, 0.81) at baseline and 0.84 (0.79, 0.88)) at three months. After all the responses were coded, CC and JD sought to reconcile their disagreements; based on the codebook RK adjudicated 18 discrepancies at baseline and seven discrepancies at three months.
Other Survey Measures
In addition to the open-ended question discussed previously, patients were asked to rate on a 5-point Likert scale how thoroughly they had discussed their hopes with their: 1) spouse or partner, 2) other family members or friends, 3) oncologist, 4) primary care physician, 5) nurse, 6) clergy, or 7) a support group. We dichotomized patients’ responses for how thoroughly they had discussed their hopes with confidants in which not at all or a little bit was considered “not substantive” and somewhat, quite a bit, or very much was considered “substantive.”
Patient-Level Covariates
We created a series of patient-level variables, dichotomized for ease of interpretation. Demographic variables included age, gender, race, education, income, relationship status, and religion. We also noted whether patients were diagnosed with “aggressive” cancers, determined prospectively in consultation with two oncologists, and including lung, gastrointestinal cancers (except colon), and genitourinary cancers (except prostate). We also constructed indicator variables for study site and trial arm.
Statistical Analysis
Analyses were conducted using STATA (Version 14.2, College Station, TX). We estimated the prevalence of the hope categories at both time points and used Pearson’s chi-square test to identify statistically significant associations between patient variables and 1) hopes for unqualified cure, and 2) hopes for quality of life (defining statistical significance as a two-tailed p-value<0.05). We chose to focus on these two hope categories because we hypothesized that they may be related to a life-extending versus palliative orientation near the end of life. We used mixed-effects multiple logistic regression to assess the independent association between selected patient-level variables with these two categories of hopes, adjusting for study site, study arm, and physician breast cancer subspecialty to account for the stratified randomized design. Due to the need for parsimony,21 and the lack of prior knowledge regarding predictors of hopes, we entered into the multiple logistic regression only those candidate covariates that were statistically significant in bivariate analysis. To account for the clustering of patients within physicians, we specified physician-level random intercepts.
RESULTS
Participant Characteristics
Most patients in the study identified as white, Christian, and had at least some college education (Table 1). Half had cancers classified as aggressive.
Table 1.
Characteristics of Participants (N=265)
| N | % (mean) | |
|---|---|---|
| Patient age | 265 | 64.3 (SD=11.4) |
| Gender | ||
| Male | 119 | 45 |
| Female | 146 | 55 |
| Race | ||
| Non-white | 30 | 11 |
| White | 235 | 89 |
| Patient education | ||
| HS or less | 73 | 28 |
| Some college or more | 192 | 72 |
| Income | ||
| $50,000 or less | 123 | 54 |
| $Over $50,000 | 106 | 46 |
| Relationship status | ||
| Committed/Married | 176 | 66 |
| Separated/Widowed/Never | 89 | 34 |
| Married | ||
| Patient religion | ||
| Christianity | 191 | 72 |
| Other/ No Religion | 74 | 28 |
| Cancer typea | ||
| Aggressive | 133 | 50 |
| Non-aggressive | 132 | 50 |
| Location | ||
| Sacramento, California | 94 | 35 |
| Rochester, New York | 171 | 65 |
Aggressive tumors were prospectively determined by two oncologists and included lung, GI cancers (except colon), and GU cancers (except prostate) while less aggressive cancers included breast, prostate and colon
Categories of Hopes for Treatment
Of the 265 patients who responded to baseline surveys, 45 patients died and 4 dropped out of the study in the intervening three months; survey responses at three months were available from 216 patients. Using the taxonomy described in the Methods, our team identified eight categories of hopes into which 95% of patients’ responses could be categorized at both baseline and three months: 1) unqualified cure, 2) cure tempered by realism (in which the patient hopes for cure but acknowledges this is unrealistic), 3) quality of life, 4) milestone, 5) life extension, 6) tumor stabilization, 7) remission, and 8) control NOS. The distribution of hopes by category at each time, category definitions, and examples are shown in Table 2.
Patients expressed an average of 1.6 (SD=0.77) hopes for treatment at baseline and 1.3 (SD=0.66) hopes at three months. At both time points, the most frequently expressed hope was for improved or maintained quality of life, while patients infrequently expressed unqualified hopes for cure and cure tempered by realism.
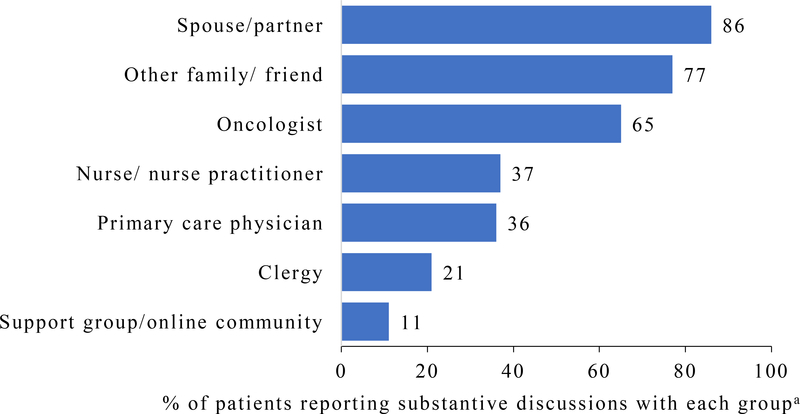
Discussions of Hopes with Members of Care Team
As shown in Figure 1, most patients reported having substantive discussions about their hopes for treatment with spouses/partners, other family or friends, or oncologists. A minority reported having substantive discussions with nurses or nurse practitioners, primary care physicians, clergy, or members of support groups or online communities.
Figure 1.
Frequency of Hopes Discussion with Members of Care Team at Baseline
a Hope discussion quality was rated by patients on a 5-point scale and dichotomized for analysis. “Not substantive” included those who responded they discussed hopes not at all or a little bit, whereas “substantive” included those who responded they discussed hopes somewhat, quite a bit, or very much
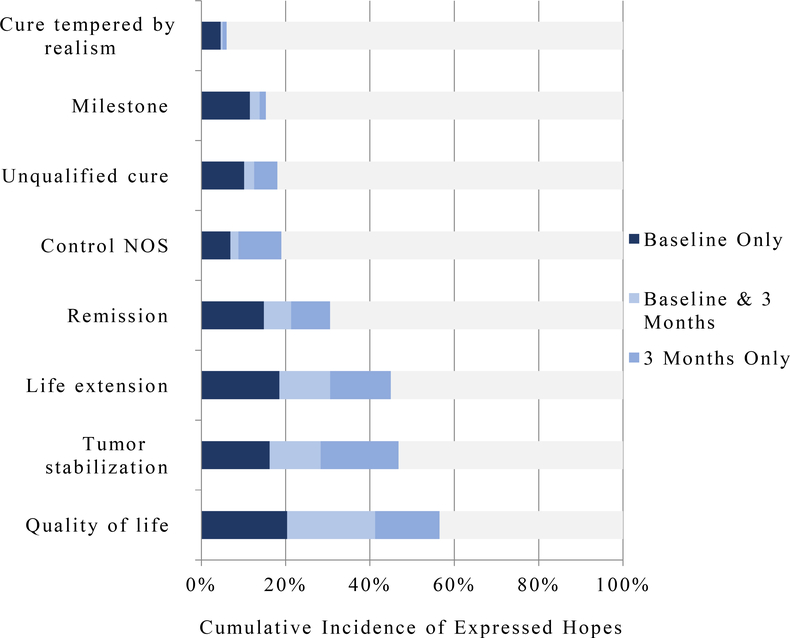
Individual Changes, Timepoint Prevalence and Cumulative Incidence of Hopes
Among the 216 patients who provided responses at both baseline and three months, 185 (86%) expressed at least one change in the categories of hopes they expressed from baseline to three months. The largest change in the prevalence of hope types from baseline to three-months (Figure 2) were in hopes for milestone (from 14% at baseline to 3% at three months) and hopes for cure tempered by realism (5% to 1%). However, the most common at both baseline and three months were hopes for quality of life (41% vs 36%).
Figure 2.
Prevalence and Cumulative Incidence of Hopes (n=216)
Associations with Hopes for Unqualified Cure and Quality of Life
In bivariate analysis, we identified two patient variables that were significantly associated with hopes for cure (Supplemental Table 1). Patients in the youngest quartile (< 57 years) were statistically significantly more likely to express hopes for cure than patients age 58 or greater. Additionally, patients who did not substantively discuss hopes with their primary care physician were more likely to express unqualified hopes for cure. Only one variable, study site, was found to have a significant association with hopes for quality of life (Supplemental Table 2). Patients from Rochester, New York were more likely than patients in Sacramento, California to express hopes for quality of life (47% vs 32%, p=0.02).
In the multiple logistic regression (Table 3), the adjusted odds of expressing hopes for an unqualified cure were higher in patients younger than 57 years old and patients who did not discuss hopes with primary care physicians. Physician effects (as measured by the betweenphysician variance component) were not significantly different from 0.
Table 3.
Adjusted Associations between Baseline Characteristics and Hopes for Unqualified Cure
| Variable | Adjusted Odds Ratio (95% CI)a | P Value |
|---|---|---|
| Age | ||
| <57 years | 3.92 (1.63–9.40) | 0.002 |
| ≥58 years | 1.0 (ref) | |
| Hope Discussions with Primary Care | ||
| Physiciansb | 3.21 (1.13–9.14) | 0.029 |
| Not Substantive | 1.0 (ref) | |
| Substantive | ||
From multiple logistic regression model that adjusted for listed variables as well as site, study arm, and breast cancer subspecialty among the 38 physician clusters. Unmeasured physician factors (as measured by the estimated variance component for the distribution of physician random effects) were not significant.
Hope discussion quality was rated by patients on a 5-point scale and dichotomized for analysis. “Not substantive” included those who responded they discussed hopes not at all or a little bit, whereas “substantive” included those who responded they discussed hopes somewhat, quite a bit, or very much
DISCUSSION
In this longitudinal study of a clinically diverse sample of patients with advanced cancer, investigators reliably classified patient’s responses to an open-ended question about their hopes for treatment into 8 categories. While the presence of specific hope categories often changed in individual participants over three months, the relative prevalence of these categories did not change substantially. We also found that while the majority of patients discuss their hopes with spouses, family and friends, and oncologists, a minority are discussing them other individuals who could have important roles in health and well-being including primary care physicians, nurses, clergy and support groups.
The eight categories in our study expand upon the six treatment goals found in the structured literature review by Kaldjian et al.17 In both our study and the literature review,17 the two most common hopes were for good quality of life and life extension. These two treatment goals are consistent with the aims of both palliative cancer-directed therapy and of palliative care more generally,22 and therefore could be construed as realistic in this setting of advanced cancer.23,24 In contrast, a small, but a non-trivial minority of patients in our study harbored hopes for cure from their treatments, which were arguably unrealistic hopes given that patients were recruited based on limited life expectancy and the incurability of their cancers.
Patients were less likely to hope for cure if they reported discussing their hopes with primary care physicians. In contrast, patients who discussed hopes with oncologists were just as likely to hope for cure as patients who did not discuss hopes with oncologists. While we cannot assume causation from these associations, primary care physicians may play a role in helping patients reframe what is important and realistic. These practitioners may also be less likely to stoke hopes for cure than oncologists, as they are not directly vested in cancer-directed treatment. In some studies, oncologists have been observed to skirt discussions of prognosis to focus on treatment options,25 a process of mutual avoidance that some have termed “collusion.” This process of avoidance may be well intentioned to protect patients from despair, leaving important topics unexplored. Alternatively, patients with more unrealistic expectations may be less likely to seek, remember, or seriously consider counsel from a primary care physician. It is also possible that cancer patients who have a trusting relationship with their primary care physicians may differ from their counterparts in other ways that affect hopes.
Unsurprisingly, we also found that younger patients are more likely to hope for a cure. Older patients may be more likely to accept grim prognoses both because the potential losses are less grievous (fewer years of productive life are being lost) and because they are less likely to have dependent children. Another study has shown that advanced cancer patients with dependent children were more likely to prefer aggressive treatments over palliative care and less likely to engage in advanced care planning,10 perhaps driven by higher levels of psychological distress at the thought of leaving dependent children behind.
We found that many individuals expressed different hopes at baseline and three months, however at the population level, hopes for quality of life remained most common while hopes for cure remained a sizable minority. The concept of evolving goals in individuals was discussed by Sachs et al. in reference to patients with dementia.26 As suggested by Epstein et al. values and preferences evolve as the disease progresses and treatment options change,27 but preferences may also be related to other life events unrelated to the disease. For example, some of the patients who no longer reported hoping to reach a milestone (e.g. a grandchild’s birth), may have either reached this milestone or changed their priorities.
The primary strength of this study is that we used open-ended questions to allow participants to freely express their hopes at two points in time. However, there are several threats to internal validity including that the survey interviews were brief, and our data on the extent of discussions with PCPs and other care team members were subject to recall bias. Additionally, our results may not be generalizable to the entire population of advanced cancer patients because patients were recruited from only two geographic areas, and the sample was predominately white, Christian, and well-educated. While concerns have been raised about the validity of the “surprise” question, especially in non-cancer populations,28 we applied this question only to patients with stage III cancer (stage IV were automatically eligible), and the median survival in our study was 16 months,18 indicating that the target population of patients was successfully recruited.
We found that patients with advanced cancer have a wide range of hopes that are often not discussed with members of the healthcare team or other confidants. While maintenance of quality of life was the most commonly expressed hope, a sizable minority of patients hoped for an unqualified cure despite the poor prognosis of their cancers. By asking about hopes for treatment, physicians and other care team members can provide empathetic education and guidance to help patient establish realistic goals for treatment. Future studies may consider how advanced cancer patients’ hopes for treatment affect medical decisions and how oncologists, primary care physicians, and other members of the patient’s support system can tackle the challenge of helping patients more realistically understand their illness and treatment options while maintaining their well-being.
Supplementary Material
DISCLOSURES AND ACKNOWLEDGEMENTS
Funding: This work was supported by the National Cancer Institute (R01 CA140419–05; co– principal investigators: Drs. Epstein and Kravitz). Dr. Duberstein is supported by a grant from the National Cancer Institute (R01CA168387).
Footnotes
Disclosure/Conflicts of Interest: All authors have nothing to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Wiles R, Cott C, Gibson BE. Hope, expectations and recovery from illness: a narrative synthesis of qualitative research. Journal of advanced nursing. 2008;64(6):564–573. [DOI] [PubMed] [Google Scholar]
- 2.Coulehan J Deep hope: a song without words. Theoretical medicine and bioethics. 2011;32(3):143–160. [DOI] [PubMed] [Google Scholar]
- 3.Gum A, Snyder CR. Coping with terminal illness: the role of hopeful thinking. Journal of palliative medicine. 2002;5(6):883–894. [DOI] [PubMed] [Google Scholar]
- 4.Stephenson C The concept of hope revisited for nursing. Journal of advanced nursing. 1991;16(12):1456–1461. [DOI] [PubMed] [Google Scholar]
- 5.Kylma J, Vehvilainen-Julkunen K. Hope in nursing research: a meta-analysis of the ontological and epistemological foundations of research on hope. Journal of advanced nursing. 1997;25(2):364–371. [DOI] [PubMed] [Google Scholar]
- 6.Lamont EB, Siegler M. Paradoxes in cancer patients’ advance care planning. Journal of palliative medicine. 2000;3(1):27–35. [DOI] [PubMed] [Google Scholar]
- 7.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. Jama. 1998;279(21):1709–1714. [DOI] [PubMed] [Google Scholar]
- 8.Nilsson ME, Maciejewski PK, Zhang B, et al. Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer. 2009;115(2):399–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rand KL, Banno DA, Shea AM, Cripe LD. Life and treatment goals of patients with advanced, incurable cancer. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2016;24(7):2953–2962. [DOI] [PubMed] [Google Scholar]
- 10.Hitz F, Ribi K, Li Q, Klingbiel D, Cerny T, Koeberle D. Predictors of satisfaction with treatment decision, decision-making preferences, and main treatment goals in patients with advanced cancer. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2013;21(11):3085–3093. [DOI] [PubMed] [Google Scholar]
- 11.Haberle TH, Shinkunas LA, Erekson ZD, Kaldjian LC. Goals of care among hospitalized patients: a validation study. The American journal of hospice & palliative care. 2011;28(5):335–341. [DOI] [PubMed] [Google Scholar]
- 12.Patil V, Joshi A, Noronha V, et al. Expectations and preferences for palliative chemotherapy in head and neck cancers patients. Oral oncology. 2016;63:10–15. [DOI] [PubMed] [Google Scholar]
- 13.Soylu C, Babacan T, Sever AR, Altundag K. Patients’ understanding of treatment goals and disease course and their relationship with optimism, hope, and quality of life: a preliminary study among advanced breast cancer outpatients before receiving palliative treatment. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2016;24(8):3481–3488. [DOI] [PubMed] [Google Scholar]
- 14.Craft PS, Burns CM, Smith WT, Broom DH. Knowledge of treatment intent among patients with advanced cancer: a longitudinal study. European journal of cancer care. 2005;14(5):417–425. [DOI] [PubMed] [Google Scholar]
- 15.Sanatani M, Schreier G, Stitt L. Level and direction of hope in cancer patients: an exploratory longitudinal study. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2008;16(5):493–499. [DOI] [PubMed] [Google Scholar]
- 16.Koedoot CG, de Haan RJ, Stiggelbout AM, et al. Palliative chemotherapy or best supportive care? A prospective study explaining patients’ treatment preference and choice. British journal of cancer. 2003;89(12):2219–2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaldjian LC, Curtis AE, Shinkunas LA, Cannon KT. Goals of care toward the end of life: a structured literature review. The American journal of hospice & palliative care. 2008;25(6):501–511. [DOI] [PubMed] [Google Scholar]
- 18.Epstein RM, Duberstein PR, Fenton JJ, et al. Effect of a Patient-Centered Communication Intervention on Oncologist-Patient Communication, Quality of Life, and Health Care Utilization in Advanced Cancer: The VOICE Randomized Clinical Trial. JAMA Oncol. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoerger M, Epstein RM, Winters PC, et al. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC cancer. 2013;13:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. Journal of palliative medicine. 2010;13(7):837–840. [DOI] [PubMed] [Google Scholar]
- 21.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. Journal of clinical epidemiology. 1996;49(12):1373–1379. [DOI] [PubMed] [Google Scholar]
- 22.Temel JS, Greer JA, Muzikansky A, et al. Early Palliative Care for Patients with Metastatic Non– Small-Cell Lung Cancer. New England Journal of Medicine. 2010;363(8):733–742. [DOI] [PubMed] [Google Scholar]
- 23.American Cancer Society. Treating Advanced Cancer. 2016; https://www.cancer.org/treatment/understanding-your-diagnosis/advancedcancer/treatment.html. Accessed August 5, 2018.
- 24.World Health Organization. Cancer Diagnosis and Treatment. 2018; http://www.who.int/cancer/treatment/en/. Accessed August 5, 2018.
- 25.The AM, Hak T, Koeter G, van Der Wal G. Collusion in doctor-patient communication about imminent death: an ethnographic study. BMJ (Clinical research ed). 2000;321(7273):1376–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sachs GA. Dementia and the goals of care. Journal of the American Geriatrics Society. 1998;46(6):782–783. [DOI] [PubMed] [Google Scholar]
- 27.Epstein RM, Peters E. Beyond information: exploring patients’ preferences. Jama. 2009;302(2):195–197. [DOI] [PubMed] [Google Scholar]
- 28.Downar J, Goldman R, Pinto R, Englesakis M, Adhikari NKJ. The “surprise question” for predicting death in seriously ill patients: a systematic review and meta-analysis. Canadian Medical Association Journal. 2017;189(13):E484–E493. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.