Abstract
Schistosomiasis is a neglected parasitosis caused by Schistosoma spp. Praziquantel is used for the chemoprophylaxis and treatment of this disease. Although this monotherapy is effective, the risk of resistance and its low efficiency against immature worms compromises its effectiveness. Therefore, it is necessary to develop new schistosomicide drugs. However, the development of new drugs is a long and expensive process. The repositioning of approved drugs has been proposed as a quick, cheap, and effective alternative to solve this problem. This study employs chemogenomic analysis with use of bioinformatics tools to search, identify, and analyze data on approved drugs with the potential to inhibit Schistosoma mansoni energy metabolism enzymes. The TDR Targets Database, Gene DB, Protein, DrugBank, Therapeutic Targets Database (TTD), Promiscuous, and PubMed databases were used. Fifty-nine target proteins were identified, of which 18 had one or more approved drugs. The results identified 20 potential drugs for schistosomiasis treatment; all approved for use in humans.
Introduction
Schistosomiasis is a neglected parasitic illness caused by Schistosoma trematodes, mainly caused by three species of medical importance: S. mansoni, S. haematobium, and S. japonicum. In 2016, transmission of this illness was recorded in 78 countries, with about 206 million people requiring preventive chemotherapy. However, approximately 88 million people received treatment in 52 countries with a high or moderate prevalence of this parasitosis [1].
For schistosomiasis treatment and chemophylaxis, the World Health Organization (WHO) recommends the use of the drug praziquantel (PZQ) [2], because it is an anthelmintic that is effective in a single oral dose, mild adverse reactions (include abdominal pain, diarrhea, dizziness, sleepiness and headache) and has a relatively low cost [3,4]. The exact mechanism of action of the PZQ has not yet established, although has been suggested that the drug PZQ acts as an antagonist of calcium ion channels (Ca2+) that induce the influx of Ca2+ and an indirect evidence that a possible target for PZQ action is the interaction between beta subunits and pore-forming alpha(1) subunits in schistosomes [4,5]. Although this drug is effective, the appearance of strains resistant to PZQ, as well as its low effectiveness against immature worms, make research and new drug development extremely necessary [6–8].
For this reason, the investigation of target molecules that act in the metabolism of Schistosoma spp. and have potential to interact with compound candidates for anti-schistosomiasis therapy is necessary [9,10]. This strategy focuses on energy metabolism enzymes, as they are considered interesting targets for inhibitor development because they reduce energy production capacity, consequently contributing to the death and elimination of the parasite. Mitochondria and glycolytic pathways are the main sites of energy production, both in the larval and adult stages of this parasite. In the mitochondria occurs the Krebs cycle and oxidative phosphorylation. In the glycolytic route the sequential degradation of the glucose occurs, obtaining lactic acid as product [11]. Some enzymes have been reported as potential targets to therapeutic use, Mefloquine inhibits Enolase [12] and Artemether is an inhibitor of Calcium-transporting ATPase (SmSERCA) [13].
Conventional research and development strategies for novel drugs are considered high-cost (estimated at millions of dollars), time-consuming (between 10–17 years), and risky. The serious side-effects and diminished efficacy in humans that can occur during clinical trials are common factors leading to a compound not being approved for commercialization [14,15]. Moreover, pharmaceutical industries are not interested in investing in the development and production of new drugs for treating Neglected Tropical Diseases (NTDs), because they offer a low profit return [16].
To overcome these difficulties, the repositioning of approved drugs is proposed, which offers an excellent cost-benefit ratio by diminishing the time (between 3–12 years) and money spent compared to the time and cost of developing new compounds. This strategy consists of identifying new therapeutic indications for already approved drugs to treat other illnesses and/or those with already discovered targets [10,15,17–21]. In silico analysis, guided by databases that provide information about potential off-target drug interactions, allows the prediction of side effects and the identification of compounds that are candidates for repositioning [21–26]. Using this strategy, the probability of success increases during in vitro and in vivo tests, the risk of failure is reduced, and the experimentation on animals is rationalized [17,27].
In this study, the following open access databases were used: TDR Targets Database, Gene DB, Protein, Therapeutic Targets Database (TTD), DrugBank, Promiscuous, and PubMed. These databases complement each other to provide information on the profiles of hundreds of molecular targets and approved drugs, including data about pharmacology, toxicity, pharmacogenomics, and clinical screenings. Using this information, the identification of S. mansoni energy metabolism-inhibiting enzymes was possible, to enable the in silico repositioning of approved drugs for use in anti-schistosomiasis therapy.
Materials and methods
The methodology utilized is an adaptation of the methodology used by Bispo et al. [28] and Silva et al. [29].
Identification of Schistosoma mansoni energy metabolism targets
The initial target screening was performed using the TDR Targets Database version 5.0 (Fig 1A) (http://tdrtargets.org/) [30]. On the initial page, the “Targets” option was selected. Next, in the “Select pathogen species of interest” field, the Schistosoma mansoni option was selected as the species of interest. The filters field contained the following information: Name/Annotation, Features, Structures, Expression, Antigenicity, Phylogenetic distribution, Essentiality, Validation data, Druggability, Assayability, and Bibliographic references. The number of filters was limited to increase the chances of getting results. For this reason, the only expanded filter was “Name/Annotation,” and in the “Energy metabolism” option was selected in the “KEGG high-level pathway” field. Finally, the “Search” option was selected. The database returned a table containing the identity (ID) of each gene of interest.
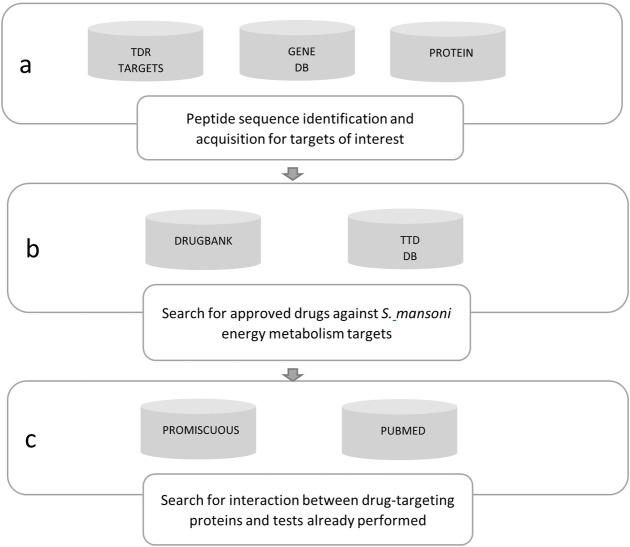
Fig 1. Research pipeline used to identify potential anti-schistosomiasis drugs.
a) TDR Targets Database supplied the S. mansoni energy metabolism target identity; Gene DB and Protein were used to obtain each target's peptide sequence. b) DrugBank and TTD were used to search for approved drugs. c) Promiscuous was used to identify the interactions between the drug-target protein and possible side effects of the interaction; PubMed was used to acquire articles on in vitro and/or in vivo tests with the identified drugs.
After the genes of interest list was produced, the ID of each gene was used to obtain the targets’ peptide sequences form the Gene DB version 2.5 database (Fig 1A) (http://www.genedb.org/) [31]. On the initial Gene DB page, each gene id was inserted into the “Name/Product” field and, right after, “S. mansoni” was selected in the “All organism” field, and the search was executed. The Protein database (http://www.ncbi.nlm.nih.gov/protein/) was employed when the gene of interest did not appear in the Gene DB search results. On the initial Protein page, the gene ids were inserted in the “Gene name” field, followed by Schistosoma mansoni in the “Organism” field. The gene ids and their respective peptides were tabulated in an Excel spreadsheet.
Peptide sequences were obtained from the DrugBank (http://www.drugbank.ca/) and TTD (http://bidd.nus.edu.sg/group/cjttd/) databases, and this provided basic information about hypothetical drug targets and their corresponding inhibitors.
Search for approved drugs for the selected targets: General strategy in DrugBank and TTD
DrugBank version 4.0 (Fig 1B) stores information on drugs and their targets. This database contains approximately 8,000 compounds, including 1,700 Food and Drug Administration (FDA)-approved drugs and 6,000 experimental drugs [32].
Another database utilized was the TTD update 2016 (Fig 1B) that provides information on drug targets, such as sequence, function, and three-dimensional structure. At the time of the search, TTD contained 2,589 targets and around 31,614 drugs, of which 2,071 were approved and 7,291 were in the clinical trial phase [33].
In these two databases, the general strategy was based on the principle of target similarity, where each S. mansoni energy metabolism target was compared with other targets that already have approved drugs for treatment. All homologous drug targets with an expectation value (E-value) less than 1 × 10−5 obtained from the databases were input into a table as potential targets.
Specific commands for the DrugBank database
On the initial DrugBank page, in the “Search” option, “Target Sequences” was selected. Then, we inserted the protein sequence for consultation. The BLAST parameters offered by the database were maintained and in the "drug types" filter, the option "approved” was marked.
Specific commands for the Therapeutic Targets Database
In the initial TTD page, the “Target Similarity” option was selected and the peptide sequence was introduced into the “Input your protein sequence in FASTA format” field, and the “Search” function was executed. All the results with an E-value less than 1 × 10−5 were considered for analysis.
Criteria for the compilation of expected targets
From the results obtained regarding potential drug targets, we select those that interacted with compounds approved for clinical use in human beings. The following parameters were introduced in the table for targets with positive outcomes: “Name(s) of homologous target(s)” (Drug Bank and TTD), “Target ID(s)" (DrugBank and TTD), “Pharmacological indication” (DrugBank), and “Drug approval phase” (DrugBank and TTD) (Table 1).
Table 1. Identified targets and their function in S. mansoni energy metabolism.
| Number | Target(s) | ID(s)a | Function |
|---|---|---|---|
| 02 | Cytochrome—C oxidase |
Smp_128610 Smp_144000 |
Reduction of O2 to H2O is supplemented by the extrusion of four protons in the intramitochondrial compartment |
| 01 | Glutamate synthase | Smp_128380.2 | Chemical reactions and pathways that result in glutamate formation, anion of 2-amino pentatonic acid |
| 01 | Alcohol dehydrogenase | Smp_044440 | Involved in the oxidation process of ethanol for conversion into acetyl-CoA |
| 03 | ATP Synthase |
Smp_029390 Smp_082120 Smp_038100 |
Involved in the transport of protons connected to ATP synthesis |
| 01 | NADH-ubiquinone oxidoreductase | Smp_038870.1 | Acts as an NADPH oxireductor |
| 01 | Aminomethyltransferase | Smp_128980 | Acts on glycine decarboxylation through the cleavage system |
| 01 | Succinate dehydrogenase | Smp_061230 | Involved in the tricarboxylic acid cycle |
| 02 | Glutaminase |
Smp_147040 Smp_091460 |
Involved in the glutamine metabolic process |
aID–Target identity
Search for interaction between drugs identified with other protein targets and the possible side effects of this relationship
Promiscuous version 3.0 (http://bioinformatics.charite.de/promiscuous/) contains information on 25,000 drugs, 1,100 different side effects, and 12,000 protein targets. Moreover, this database makes information available on protein-protein and drug-protein interactions [34].
Promiscuous offers different search strategies to the user: drug name, target by interest, and metabolic pathway. In the present study, the search strategy chosen was to use the drug name. On the initial page, the “Drugs” option was selected, and each drug name was inserted into the "Drug name" field. Subsequently, the code of each drug was inserted into the PubChem field, found at https://pubchem.ncbi.nlm.nih.go [35], and the “Only with targets” option was selected. Information on the interaction between the drug and protein target and the eventual side effects were separately included in a table (Table 2).
Table 2. The new associations between Schistosoma mansoni energy metabolism targets and drugs identified in the present study.
| Drug name | Drug category | Drug toxicity | IDa and S. mansoni target name | E-valueb |
|---|---|---|---|---|
| (DB00730) Thiabendazole | Anthelmintic | High dosage may be associated with transient vision and psychological disturbances. The oral LD50 is 3.6 g/kg, 3.1 g/kg, and 3.8 g/kg in mice, rats, and rabbits, respectively | (Smp_061230) Succinate dehydrogenase | 4.68425e-121 |
| (DB00518) Albendazole | Anthelmintic | Overdose symptoms include increased liver enzymes, headaches, hair loss, low white blood cell count (neutropenia), fever, and itching | (Smp_061230) Succinate dehydrogenase | 2.31889e-25 |
| (DB01213) Fomepizole | Antidote | Headaches, nausea, and dizziness | (Smp_044440) Alcohol dehydrogenase | 5.95631e-125 |
| (DB01189) Desflurane | Anesthetic | Unavailable | (Smp_082120) ATP synthase delta chain, mitochondrial | 2.72872e-44 |
| (DB00753) Isoflurane | Anesthetic | LC50 = 15300 ppm/3 hours (inhalation per rat) | (Smp_082120) ATP synthase delta chain, mitochondrial | 2.72872e-44 |
| (DB00630) Alendronate |
Anti-hypokalemic | Damages the esophagus not only because of the medicine's toxicity but non-specific irritation secondary to contact between the pill and the esophageal mucosa, similar to other "esophagitis pill" cases | (Smp_038100) ATP synthase beta-subunit | 1.35936e-21 |
| (DB01119) Diazoxide | Antihypertensive | LD50 orally: 980 mg/kg for rats and 444 mg/kg for mice | (Smp_091460) Glutamine synthetase 1, 2 (glutamate ammonia ligase) (gs) | 3.91448e-180 |
aID–Target identity
bE-value–Expectation value
After obtaining results of interactions between drugs and protein targets and their side effects, the “Show interactive network” option was selected, with the objective of integrating the results in graphs on the interactive network and representing the relationship between cited compounds. The search result was saved in the export network to XGMML section, and the archive was exported to Cytoscape software version 2.0 (http://cytoscape.org/), making it possible to visualize the interaction networks [36].
List of drugs already tested against Schistosoma spp.
Lastly, the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed) was used to verify if the identified drugs had already been tested against Schistosoma spp. The definition of “test” in this study included in vitro and/or in vivo tests against the three species of medical importance: S. mansoni, S. haematobium, and S. japonicum. Drugs were classified as “not tested” when no related publication could be found. In those cases, one of the following search terms was introduced into PubMed: (“drug name” [MeSH Terms] OR “drug name” [All Fields]) AND (“Schistosomiasis” [MeSH Terms] OR “Schistosomiasis” [All Fields]) and (2) (“drug name” [MeSH Terms] OR “drug name” [All Fields]) AND (“Schistosomiasis” [MeSH Terms] OR “Schistosomiasis” [All Fields]).
Results
Development of a predicted target list
In the TDR Targets Database, 59 genes were identified that encode S. mansoni energy metabolism enzymes. All the products of these genes were considered as potential therapeutic targets.
Identification of targets and drugs with potential for anti-schistosomiasis therapy
The DrugBank and TTD databases returned 11 and one targets, respectively, with approved drugs against them. The protein targets and their respective functions are presented in Table 1.
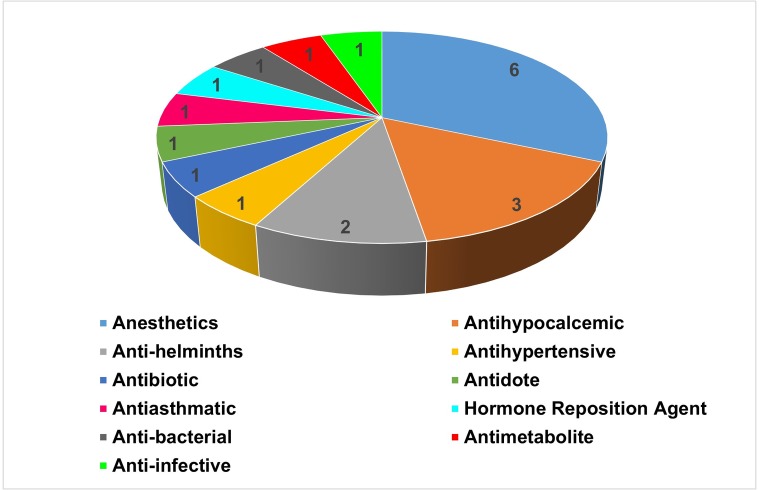
For each of the targets, the DrugBank and TTD databases returned one or more drugs. Twenty drugs were identified, 19 in the DrugBank and one in the TTD. These drugs and their original indications are presented in Fig 2.
Fig 2. Original principal drug indications with potential anti-schistosomiasis activity.
Of the ten targets, eight had high chemotherapeutic potential because of their very low E-values. Five targets that interact with seven high potential anti-schistosomiasis drugs were selected. Detailed information on these compounds is presented in Table 2.
Identification of interaction network between drug(s), target(s) protein(s), and side effect(s)
In this analysis, drugs identified as having therapeutic potential against schistosomiasis were considered if they had a low cost, were approved for use in humans, and possessed few side effects. Interactions of drugs identified with other targets were investigated using the Promiscuous database to meet this last criterion. Each of the drugs was subjected to analysis, and 18 of them presented interactions with different molecules. In this study, only the interaction networks of drugs with high anti-schistosomiasis potential were detailed (Table 2).
Thiabendazole
Thiabendazole shows interaction potential with the targets cytochrome P450 1A2 (CP1A2_HUMAN) and cytochrome P450 1A1 (CP1A1_HUMAN). Interactions and side effects are presented in S1 Fig.
Albendazole
Albendazole shows interaction potential with the targets cytochrome P450 3A4 (CP3A4_HUMAN), cytochrome P450 1A2 (CP1A2_HUMAN), and cytochrome P450 1A1 (CP1A1_HUMAN). Interactions and side effects are shown in S2 Fig.
Fomepizole
Fomepizole shows interaction potential with the targets alcohol dehydrogenase 1A (ADH1A_HUMAN), alcohol dehydrogenase 1B (ADH1B_HUMAN), Alcohol dehydrogenase 1C (ADH1G_HUMAN), catalase (CATA_HUMAN), cytochrome P450 2A6 (CP2A6_HUMAN), and cytochrome P450 2E1 (CP2E1_HUMAN). Interactions and side effects are shown in S3 Fig.
Desflurane
Desflurane presents interaction potential with targets Glutamate receptor 1 (GRIA1_HUMAN), Glycine receptor alpha-1 subunit (GLRA1_HUMAN), ATP delta synthase subunit, mitochondrial (ATPD_HUMAN), gamma-aminobutyric acid receptor alpha-1 subunit (GBRA1_HUMAN), potassium voltage-gated channel subfamily A member 1 (KCNA1_HUMAN), and ATPase for calcium transport type 2C member 1 (AT2C1_HUMAN). Interactions and side effects are shown in S4 Fig.
Isoflurane
Isoflurane presents interaction potential with targets ATPase member 2C of calcium transport type 1 (AT2C1_HUMAN), ATP delta synthase subunit (ATPD_HUMAN), calmodulin (CALM_HUMAN), cytochrome P450 2E1 (CP2E1_HUMAN), cytochrome P450 2B6 (CP2B6_HUMAN), gamma-aminobutyric acid receptor alpha-1 subunit (GBRA1_HUMAN), Glycine alpha-1 receptor subunit (GLRA1_HUMAN), Glutamate 3 receptor (GRIA3_HUMAN), Glutamate 1 receptor (GRIA1_HUMAN), NADH-ubiquinone oxidoreductase (NU1M_HUMAN), and potassium voltage-gated channel for subfamily 1 member 1 (KCNA1_HUMAN). Interactions and side effects are shown in S5 Fig.
Alendronate
Alendronate presents interaction potential with the Tyrosine phosphatase type 4 (PTN4_HUMAN) and farnesyl pyrophosphate synthase targets (FPPS_HUMAN). Interactions and side effects are shown in S6 Fig.
Diazoxide
Diazoxide demonstrates interaction potential with targets ATP-binding cassette subfamily C member 8 (ABCC8_HUMAN), ATPase transport of sodium/potassium alpha 1 subunit (AT1A1_HUMAN), ATP-sensitive inward rectifier potassium channel 11 (IRK11_HUMAN), calcium-activated potassium channel subunit alpha-1 (KCMA1_HUMAN), sulfonylurea receptor (Q59GM5_HUMAN), carbonic anhydrase 1 (CAH1_HUMAN), carbonic anhydrase 2 (CAH2_HUMAN), carbonic anhydrase 4 (CAH4_HUMAN), and solute carrier family 12 member 3 (S12A3_HUMAN). Interactions and side effects are shown in S7 Fig.
Discussion
Drugs already tested against Schistosoma spp. metabolism
Two drugs identified using this strategy were already tested as anti-schistosomiasis agents: thiabendazole and albendazole.
Thiabendazole is indicated for the treatment of parasitic illnesses caused by Ascaris lumbricoides, Strongyloides stercoralis, Necator americanus, Ancylostoma duodenale, Ancylostoma braziliense, Trichuris trichiura, Toxocara canis, Toxocara cati, and Enterobius vermicularis. Thiabendazole acts as an inhibitor of the flavoprotein subunit of fumarate reductase in these organisms, which catalyzes the oxidation of succinate to fumarate during the Krebs cycle (Drug Bank Data). Here, it is suggested that this drug exhibits potential as a succinate dehydrogenase inhibitor (Table 2), as it interferes with the transfer of electrons from succinate to ubiquinone (Smp_061230) (Gene DB Data).
Albendazole is an anthelmintic used to treat parasitic illnesses caused by Taenia solium and Echinococcus granulosus. This drug acts as a beta tubulin inhibitor and interferes with microtubule polymerization and assembly. As a consequence of cytoplasmic microtubule loss, a reduction in glucose absorption by the parasites in larval and adult stages occurs, resulting in reduced ATP synthesis. Moreover, albendazole acts as a fumarate reductase inhibitor, a flavoprotein subunit present in the metabolism of Shewanella oneidensis, interfering with the catalysis of the reduction of fumarate (Drug Bank Data). In silico analysis demonstrated that albendazole inhibits succinate dehydrogenase (Smp_061230) (Table 2).
To evaluate in vivo anti-schistosomiasis activity of thiabendazole and albendazole in mice infected with S. mansoni, 100 mg/kg/day and 500 mg/kg/day doses were used, respectively. In this assessment, it was found that albendazole treatment showed no effect on the number of dead adult specimens and/or the elimination of eggs from this parasite. In contrast, treatment using thiabendazole significantly increased the mortality of adult worms [37].
Drugs not already tested against Schistosoma spp
The study's main purpose was to identify new anti-schistosomiasis drugs using an in silico repositioning strategy with drugs approved for treating other diseases. The following is a discussion of each of the drugs identified in the present study and their potential effects on S. mansoni energy metabolism.
Fomepizole is indicated for treating methanol poisoning or used when the ingestion of ethylene glycol is suspected [38]. This drug acts as an inhibitor of alcohol dehydrogenase 1B, present in human metabolism [39]. In this target, fomepizole inhibits the oxidation of ethanol to acetaldehyde (DrugBank data). In the present study, fomepizole was identified as having the capacity to inhibit (Smp_044440) alcohol dehydrogenase (Table 2), as both cited targets present similar functions. Results obtained from the Promiscuous database reveal that fomepizole also inhibits catalase (CATA_HUMAN), which degrades hydrogen peroxide; cytochrome P450 2A6 (CP2A6_HUMAN), which functions as a component in the metabolic activation of the B1 aflatoxin; and cytochrome P450 2E1 (CP2E1_HUMAN), which inactivates a series of drugs and xenobiotics and also bioactivates many xenobiotic substrates in their hepatotoxic or carcinogenic forms (S3 Fig) (Promiscuous data).
Desflurane is used as an inhalation agent for inducing and maintaining general anesthesia (DrugBank data). This drug inhibits the mitochondrial ATP synthase subunit delta target, in human metabolism. This inhibitor interferes with the synthesis of ATP from ADP in the presence of an electrochemical gradient [40]. In vitro analysis verified that desflurane presents antiplatelet activity, interfering with the induction of platelet and leukocyte aggregation, through inhibiting the stimulation of P-selectin synthesis, which carries out the function of heterophilic cell adhesion [41]. Desflurane was identified as presenting potential to inhibit mitochondrial ATP synthase delta chain (Smp_082120) (Table 2), by interfering with the proton transport through a membrane, generating an electrochemical gradient that contributes to ATP synthesis (Gene DB Data). Moreover, desflurane presents potential target interaction with Glutamate 1 receptor (GRIA1_HUMAN), which regulates glutamate release; Glycine subunit alpha-1 receptor (GLRA1_HUMAN), which regulates glycine release; NADH-ubiquinone oxidoreductase (NU1M_HUMAN), which transfers NADH electrons to the respiratory chain; ATP synthase delta mitochondrial subunit (ATPD_HUMAN), which produces ATP from ADP in the presence of; a proton gradient; gamma-aminobutyric acid subunit alpha-1 receptor (GBRA1_HUMAN), which functions in regulating histamine release; potassium voltage-gated channel subfamily A member 1 (KCNA1_HUMAN), which functions in transmembrane potassium transport; and ATPase of calcium transport type 2C member 1 (AT2C1_HUMAN), an ATP hydrolysis catalyst that is also involved in calcium transport (S4 Fig) (Promiscuous data).
Isoflurane is also used for inducing and maintaining general anesthesia. This drug acts as an inhibitor of the mitochondrial ATP synthase subunit delta target, in human metabolism. This inhibitor interferes with the production of ATP from ADP in the presence of a proton gradient (DrugBank data). In vivo analysis verified that isoflurane presents potential as an antidepressant, inhibiting the glycogen synthase kinase 3β target, interfering with the regulatory functions of hormonal homeostasis and Wnt signaling (pathway associated with cell proliferation) [42]. This study identified that isoflurane can inhibit mitochondrial ATP synthase subunit delta (Smp_082120) (Table 2), as both targets mentioned have similar functions.
Even though desflurane and isoflurane offer anesthetic pharmacological activity, it is possible to make them usable for clinical trials against S. mansoni, using molecular remodeling.
Alendronate is indicated for treatment of Paget’s disease and osteoporosis. This drug acts as an inhibitor of the ATPase type IV subunit A target, interfering in proton transport through a rotation mechanism. Alendronate exhibits toxicity evidenced by esophageal mucosa damage (DrugBank data). In this study, alendronate was identified as having the capacity to inhibit ATP synthase subunit beta (Smp_038100), interfering with the function of proton transport connected to ATP synthesis (Table 2) (Gene DB data). Furthermore, alendronate presents interaction potential with the Tyrosine phosphatase type 4 target (PTN4_HUMAN), which has roles in the junctions between the membrane and the cytoskeleton and with the farnesyl pyrophosphate synthase target (FPPS_HUMAN), through the function of the biosynthesis of isoprenoids that catalyze the formation of farnesyl diphosphate (S6 Fig) (Promiscuous data).
Conclusions
This study presents an in silico repositioning strategy to identify new drugs for treating intestinal schistosomiasis based on the principle of target similarity to identify drugs approved for clinical use in humans. Twenty drugs were identified, eight of which have high schistosomicide potential. The action of the drugs was compared among the targets using databases that presented interaction analysis of the drug with other targets. Using this methodology, it was possible to confirm the drug-protein target interaction, as well as the interaction with other targets that may or may not have roles in energy metabolism. Furthermore, information was obtained on possible side effects of the identified drugs. However, it is important to emphasize that there are no guarantees that the identified compounds will act on S. mansoni energy metabolism targets. Therefore, the authors of this study are carrying out in vitro tests to confirm the effect of the thiabendazole on energy metabolism target. In our results, we found that this drug acts against Succinate Dehydrogenase (SDH), an essential enzyme for Krebs cycle. SDH has been investigated as drug target in fungi and human cancers [43–45]. In fungi, SDH inhibitors has been used in agriculture since the 1960s. In last years, several SDH inhibitors has been validated in silico, in vitro and in vivo evaluations [43–47]. Here, we are suggested that SDH of the S. mansoni is an important target for therapeutic of the schistosomiasis.
Supporting information
(CP1A2_HUMAN): Cytochrome P450 1A2 (CP1A1_HUMAN): Cytochrome P450 1A1.
(PDF)
(CP3A4_HUMAN): Cytochrome P450 3A4, (CP1A2_HUMAN): Cytochrome P450 1A2, (CP1A1_HUMAN): Cytochrome P450 1A1.
(PDF)
(ADH1A_HUMAN): Alcohol dehydrogenase 1A, (ADH1B_HUMAN): Alcohol dehydrogenase 1B, (ADH1G_HUMAN): Alcohol dehydrogenase 1C, (CATA_HUMAN): Catalase, (CP2A6_HUMAN): Cytochrome P450 2A6, (CP2E1_HUMAN): Cytochrome P450 2E1.
(PDF)
(GRIA1_HUMAN): Glutamate receptor 1, (GLRA1_HUMAN): Glycine receptor alpha-1 subunit, (ATPD_HUMAN): ATP delta synthase subunit, mitochondrial, (GBRA1_HUMAN): Gamma-aminobutyric acid receptor alpha-1 subunit, (AT2C1_HUMAN): ATPase for calcium transport type 2C member 1, (KCNA1_HUMAN): Potassium voltage-gated channel subfamily A member 1, (NU1M_HUMAN): NADH-ubiquinone oxidoreductase.
(PDF)
(GLRA1_HUMAN): Glycine alpha-1 receptor subunit, (CP2B6_HUMAN): Cytochrome P450 2B6, (CALM HUMAN): Calmodulin, (GRIA3_HUMAN): Glutamate 3 receptor, (GRIA1_HUMAN): Glutamate 1 receptor, (NU1M_HUMAN): NADH-ubiquinone oxidoreductase, (AT2C1_HUMAN): ATPase for calcium transport type 2C member 1, (ATPD_HUMAN): ATP delta synthase subunit, mitochondrial, (CP2E1_HUMAN): Cytochrome P450 2E1, (KCNA1_HUMAN): Potassium voltage-gated channel for subfamily 1 member 1, (GBRA1_HUMAN): Gamma-aminobutyric acid receptor alpha-1 subunit.
(PDF)
(PTN4_HUMAN): Tyrosine phosphatase type 4, (FPPS_HUMAN): Farnesyl pyrophosphate synthase.
(PDF)
(ABCC8_HUMAN): ATP-binding cassette subfamily C member 8, (AT1A1_HUMAN): ATPase transport of sodium/potassium alpha 1 subunit, (IRK11_HUMAN): ATP-sensitive inward rectifier potassium channel 11, (KCMA1_HUMAN): Calcium-activated potassium channel subunit alpha-1, (Q59GM5_HUMAN): Sulfonylurea receptor, (CAH1_HUMAN): carbonic anhydrase 1, (CAH2_HUMAN): carbonic anhydrase 2, (CAH4_HUMAN): carbonic anhydrase 4, (S12A3_HUMAN): solute carrier family 12 member 3.
(PDF)
Acknowledgments
This work was supported by the Instituto Federal de Educação, Ciência e Tecnologia Goiano/GO.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported by the Brazilian National Council for Scientific and Technological Development (CNPq/MS/DECIT n. 37/2014. Projeto 470298/2014-6 to CBB). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Schistosomiasis and soil- transmitted helminthiases: number of people treated in 2016. Wkly Epidemiol Rec. 2017;92: 749–760. [PubMed] [Google Scholar]
- 2.World Health Organization. Preventive chemotherapy for helminth diseases: progress report, 2014. Wkly Epidemiol Rec. 2016; 89–104. [PubMed] [Google Scholar]
- 3.Chai J. Praziquantel Treatment in Trematode and Cestode Infections: An Update. Infect Chemother. 2013;45: 32–43. 10.3947/ic.2013.45.1.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doenhoff MJ, Cioli D, Utzinger J. Praziquantel: mechanisms of action, resistance and new derivatives for schistosomiasis. Curr Opin Infect Dis. LWW; 2008;21: 659–667. 10.1097/QCO.0b013e328318978f [DOI] [PubMed] [Google Scholar]
- 5.Silva-Moraes V, Couto FFB, Vasconcelos MM, Araújo N, Coelho PMZ, Katz N, et al. Antischistosomal activity of a calcium channel antagonist on schistosomula and adult Schistosoma mansoni worms. Mem Inst Oswaldo Cruz. 2013;108: 600–604. 10.1590/0074-0276108052013011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cupit PM, Cunningham C. What is the mechanism of action of praziquantel and how might resistance strike? Future Med Chem. 2015;7: 701–705. 10.4155/fmc.15.11 [DOI] [PubMed] [Google Scholar]
- 7.Greenberg RM. New approaches for understanding mechanisms of drug resistance in schistosomes. Parasitology. 2013;140: 1534–1546. 10.1017/S0031182013000231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kasinathan RS, Morgan WM, Greenberg RM. Schistosoma mansoni express higher levels of multidrug resistance-associated protein 1 (SmMRP1) in juvenile worms and in response to praziquantel. Mol Biochem Parasitol. Elsevier B.V.; 2010;173: 25–31. 10.1016/j.molbiopara.2010.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panic G, Vargas M, Scandale I, Keiser J. Activity profile of an FDA-approved compound library against Schistosoma mansoni. PLoS Negl Trop Dis. Public Library of Science; 2015;9: e0003962 10.1371/journal.pntd.0003962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Panic G, Duthaler U, Speich B, Keiser J. Repurposing drugs for the treatment and control of helminth infections. Int J Parasitol Drugs drug Resist. 2014;4: 185–200. 10.1016/j.ijpddr.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.You H, Stephenson RJ, Gobert GN, McManus DP. Revisiting glucose uptake and metabolism in schistosomes: New molecular insights for improved schistosomiasis therapies. Front Genet. 2014;5: 1–8. 10.3389/fgene.2014.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manneck T, Keiser J, Müller J. Mefloquine interferes with glycolysis in schistosomula of Schistosoma mansoni via inhibition of enolase. Parasitology. 2012; 497–505. 10.1017/S0031182011002204 [DOI] [PubMed] [Google Scholar]
- 13.Lepore R, Simeoni S, Raimondo D, Caroli A, Tramontano A, Via A. Identification of the Schistosoma mansoni molecular target for the antimalarial drug artemether. J Chem Inf Model. 2011; 3005–3016. 10.1021/ci2001764 [DOI] [PubMed] [Google Scholar]
- 14.Kaitin K. Deconstructing the drug development process: the new face of innovation. Clin Pharmacol Ther. 2010;3: 1–6. 10.1038/clpt.2009.293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khanna I. Drug discovery in pharmaceutical industry: Productivity challenges and trends. Drug Discovery Today. 2012. 10.1016/j.drudis.2012.05.007 [DOI] [PubMed] [Google Scholar]
- 16.Ioset JR, Chang S. Drugs for Neglected Diseases initiative model of drug development for neglected diseases: Current status and future challenges. Future Med Chem. 2011; 10.4155/fmc.11.102 [DOI] [PubMed] [Google Scholar]
- 17.Sleigh SH, Barton CL. Repurposing Strategies for Therapeutics. Pharmaceut Med. 2010;24: 151–159. 10.1007/BF03256811 [DOI] [Google Scholar]
- 18.Ekins S, Williams AJ, Krasowski MD, Freundlich JS. In silico repositioning of approved drugs for rare and neglected diseases. Drug Discov Today. 2011;16: 298–310. 10.1016/j.drudis.2011.02.016 [DOI] [PubMed] [Google Scholar]
- 19.Lee H, Bae T, Lee J-H, Kim D, Oh Y, Jang Y, et al. Rational drug repositioning guided by an integrated pharmacological network of protein, disease and drug. BMC Syst Biol. BMC Systems Biology; 2012;6: 80 10.1186/1752-0509-6-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andrews KT, Fisher G, Skinner-Adams TS. Drug repurposing and human parasitic protozoan diseases. Int J Parasitol Drugs Drug Resist. 2014;4: 95–111. 10.1016/j.ijpddr.2014.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oprea TI, Overington JP. Computational and Practical Aspects of Drug Repositioning. Drug repurposing, rescue, repositioning. 2015;0: 1–8. 10.1089/drrr.2014.0009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Padhy BM, Gupta YK. Drug repositioning: Re-investigating existing drugs for new therapeutic indications. J Postgrad Med. 2011;57: 153–159. 10.4103/0022-3859.81870 [DOI] [PubMed] [Google Scholar]
- 23.Wishart DS, Knox C, Guo AC, Shrivastava S, Hassanali M, Stothard P, et al. DrugBank: a comprehensive resource for in silico drug discovery and exploration. Nucleic Acids Res. 2006;34: D668–D672. 10.1093/nar/gkj067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wishart DS, Knox C, Guo AC, Cheng D, Shrivastava S, Tzur D, et al. DrugBank: a knowledgebase for drugs, drug actions and drug targets. Nucleic Acids Res. 2008;36: D901–D906. 10.1093/nar/gkm958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ma DL, Chan DSH, Leung CH. Drug repositioning by structure-based virtual screening. Chem Soc Rev. 2013;42: 2130–2141. 10.1039/c2cs35357a [DOI] [PubMed] [Google Scholar]
- 26.Liu Z, Fang H, Reagan K, Xu X, Mendrick DL, Slikker W, et al. In silico drug repositioning-what we need to know. Drug Discov Today. Elsevier Ltd; 2013;18: 110–115. 10.1016/j.drudis.2012.08.005 [DOI] [PubMed] [Google Scholar]
- 27.Pelkonen O, Turpeinen M, Raunio H. In Vivo-In Vitro-In Silico Pharmacokinetic Modelling in Drug Development. 2011;50: 483–491. 10.2165/11592400-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 28.Bispo NANA, Culleton R, Silva LALA, Cravo P. A Systematic In Silico Search for Target Similarity Identifies Several Approved Drugs with Potential Activity against the Plasmodium falciparum Apicoplast. PLoS One. 2013;8: e59288 10.1371/journal.pone.0059288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silva LA, Vinaud MC, Castro AM, Cravo PVL, Bezerra JCB. In silico search of energy metabolism inhibitors for alternative leishmaniasis treatments. Biomed Res Int. 2015;2015. 10.1155/2015/965725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crowther GJ, Shanmugam D, Carmona SJ, Doyle MA, Hertz-Fowler C, Berriman M, et al. Identification of attractive drug targets in neglected- disease pathogens using an in Silico approach. PLoS Negl Trop Dis. 2010;4 10.1371/journal.pntd.0000804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Logan-Klumpler FJ, De Silva N, Boehme U, Rogers MB, Velarde G, McQuillan JA, et al. GeneDB-an annotation database for pathogens. Nucleic Acids Res. Oxford University Press; 2012;40: D98–108. 10.1093/nar/gkr1032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Law V, Knox C, Djoumbou Y, Jewison T, Guo AC, Liu Y, et al. DrugBank 4.0: shedding new light on drug metabolism. Nucleic Acids Res. 2014;42: D1091–7. 10.1093/nar/gkt1068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang H, Qin C, Li YH, Tao L, Zhou J, Yu CY, et al. Therapeutic target database update 2016: Enriched resource for bench to clinical drug target and targeted pathway information. Nucleic Acids Res. 2016;44 10.1093/nar/gkv1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.von Eichborn J, Murgueitio MS, Dunkel M, Koerner S, Bourne PE, Preissner R. PROMISCUOUS: a database for network-based drug-repositioning. Nucleic Acids Res. 2011;39: D1060–6. 10.1093/nar/gkq1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim S, Thiessen PA, Bolton EE, Chen J, Fu G, Gindulyte A, et al. PubChem substance and compound databases. Nucleic Acids Res. 2016;44: D1202–D1213. 10.1093/nar/gkv951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shannon P, Markiel A, Owen Ozier 2, Baliga NS, Wang JT, Ramage D, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003; 2498–2504. 10.1101/gr.1239303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.PANCERA CF, ALVES AL, PASCHOALOTTI MA, CHIEFFI PP. Effect of wide spectrum anti-helminthic drugs upon Schistosoma mansoni experimentally infected mice. Rev Inst Med Trop Sao Paulo. Instituto de Medicina Tropical de São Paulo; 1997;39: 159–164. 10.1590/S0036-46651997000300007 [DOI] [PubMed] [Google Scholar]
- 38.Beatty L, Green R, Magee K, Zed P. A systematic review of ethanol and fomepizole use in toxic alcohol ingestions. Emerg Med Int. 2013;2013: 638057 10.1155/2013/638057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ye B, Ji C-Y, Zhao Y, Li W, Feng J, Zhang X. Single nucleotide polymorphism at alcohol dehydrogenase-1B is associated with risk of esophageal squamous cell carcinoma. Cancer Cell Int. 2014;14: 12 10.1186/1475-2867-14-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pravdic D, Hirata N, Baber L, Sedlic F, Bosnjak ZJ, Bienengraeber M. Complex I and ATP synthase mediate membrane depolarization and matrix acidification by isoflurane in mitochondria. Eur J Pharmacol. 2012;690: 149–157. 10.1016/j.ejphar.2012.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Horn NA, De Rossi L, Robitzsch T, Hecker KE, Hutschenreuter G, Rossaint R. The effects of sevoflurane and desflurane in vitro on platelet-leukocyte adhesion in whole blood. Anaesthesia. 2003;58: 312–319. 10.1046/j.1365-2044.2003.03076.x [DOI] [PubMed] [Google Scholar]
- 42.Antila H, Ryazantseva M, Popova D, Sipila P, Guirado R, Kohtala S, et al. Isoflurane produces antidepressant effects and induces TrkB signaling in rodents. Sci Rep. 2017; 1–12. 10.1038/s41598-016-0028-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang H, Huwaimel B, Verma K, Miller J, Germain TM, Kinarivala N, et al. Synthesis and Antineoplastic Evaluation of Mitochondrial Complex II (Succinate Dehydrogenase) Inhibitors Derived from Atpenin A5. ChemMedChem. NIH Public Access; 2017;12: 1033–1044. 10.1002/cmdc.201700196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hou YP, Chen YL, Qu XP, Wang JX, Zhou MG. Effects of a novel SDHI fungicide pyraziflumid on the biology of the plant pathogenic fungi Bipolaris maydis. Pestic Biochem Physiol. 2018;149: 20–25. 10.1016/j.pestbp.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 45.Hou YP, Chen YL, Wu LY, Wang JX, Chen CJ, Zhou MG. Baseline sensitivity of Bipolaris maydis to the novel succinate dehydrogenase inhibitor benzovindiflupyr and its efficacy. Pestic Biochem Physiol. 2018;149: 81–88. 10.1016/j.pestbp.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 46.Yao TT, Fang SW, Li ZS, Xiao DX, Cheng JL, Ying HZ, et al. Discovery of Novel Succinate Dehydrogenase Inhibitors by the Integration of in Silico Library Design and Pharmacophore Mapping. J Agric Food Chem. 2017;65: 3204–3211. 10.1021/acs.jafc.7b00249 [DOI] [PubMed] [Google Scholar]
- 47.Lv XH, Ren ZL, Liu P, Li BX, Li QS, Chu MJ, et al. Design, synthesis and biological evaluation of novel nicotinamide derivatives bearing a substituted pyrazole moiety as potential SDH inhibitors. Pest Manag Sci. 2017;73: 1585–1592. 10.1002/ps.4488 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(CP1A2_HUMAN): Cytochrome P450 1A2 (CP1A1_HUMAN): Cytochrome P450 1A1.
(PDF)
(CP3A4_HUMAN): Cytochrome P450 3A4, (CP1A2_HUMAN): Cytochrome P450 1A2, (CP1A1_HUMAN): Cytochrome P450 1A1.
(PDF)
(ADH1A_HUMAN): Alcohol dehydrogenase 1A, (ADH1B_HUMAN): Alcohol dehydrogenase 1B, (ADH1G_HUMAN): Alcohol dehydrogenase 1C, (CATA_HUMAN): Catalase, (CP2A6_HUMAN): Cytochrome P450 2A6, (CP2E1_HUMAN): Cytochrome P450 2E1.
(PDF)
(GRIA1_HUMAN): Glutamate receptor 1, (GLRA1_HUMAN): Glycine receptor alpha-1 subunit, (ATPD_HUMAN): ATP delta synthase subunit, mitochondrial, (GBRA1_HUMAN): Gamma-aminobutyric acid receptor alpha-1 subunit, (AT2C1_HUMAN): ATPase for calcium transport type 2C member 1, (KCNA1_HUMAN): Potassium voltage-gated channel subfamily A member 1, (NU1M_HUMAN): NADH-ubiquinone oxidoreductase.
(PDF)
(GLRA1_HUMAN): Glycine alpha-1 receptor subunit, (CP2B6_HUMAN): Cytochrome P450 2B6, (CALM HUMAN): Calmodulin, (GRIA3_HUMAN): Glutamate 3 receptor, (GRIA1_HUMAN): Glutamate 1 receptor, (NU1M_HUMAN): NADH-ubiquinone oxidoreductase, (AT2C1_HUMAN): ATPase for calcium transport type 2C member 1, (ATPD_HUMAN): ATP delta synthase subunit, mitochondrial, (CP2E1_HUMAN): Cytochrome P450 2E1, (KCNA1_HUMAN): Potassium voltage-gated channel for subfamily 1 member 1, (GBRA1_HUMAN): Gamma-aminobutyric acid receptor alpha-1 subunit.
(PDF)
(PTN4_HUMAN): Tyrosine phosphatase type 4, (FPPS_HUMAN): Farnesyl pyrophosphate synthase.
(PDF)
(ABCC8_HUMAN): ATP-binding cassette subfamily C member 8, (AT1A1_HUMAN): ATPase transport of sodium/potassium alpha 1 subunit, (IRK11_HUMAN): ATP-sensitive inward rectifier potassium channel 11, (KCMA1_HUMAN): Calcium-activated potassium channel subunit alpha-1, (Q59GM5_HUMAN): Sulfonylurea receptor, (CAH1_HUMAN): carbonic anhydrase 1, (CAH2_HUMAN): carbonic anhydrase 2, (CAH4_HUMAN): carbonic anhydrase 4, (S12A3_HUMAN): solute carrier family 12 member 3.
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.