Abstract
Background and objectives
Fine particulate matter (PM2.5, particulate matter with an aerodynamic diameter less than or equal to 2.5 μm) has multiple adverse effects on human health, especially on the respiratory and circulatory system. The purpose of this study was to evaluate the short-term effect of PM2.5 on the mortality risk of non-accidental and circulatory diseases, and to explore the potential effect modification by sex, education and death location.
Methods
We collected daily mortality counts of Changchun (China) residents, daily meteorology and air pollution data, from January 1, 2014, to January 1, 2017. We focused on the elderly (≥65 years old) population who died from non-accidental causes and circulatory diseases, and stratified them by sex, education, and death location. A generalized additive Poisson regression model (GAM) was used to analyse the impact of air pollutants on mortality. We fit single pollutant models to examine PM2.5 effects with different lag structures of single-day (distributed lag:lag0-lag3) and multi-day (moving average lag: lag01-lag03). To test the sensitivity of the model, a multi-pollutant model was established when the PM2.5 effect was strongest.
Results
In the single pollutant models, an increment of PM2.5 by 10 μg/m3 at lag0-3 was associated with a 0.385% (95% CI: 0.069% to 0.702%) increase in daily non-accidental mortality and a 0.442% (95% CI: 0.038% to 0.848%) increase in daily circulatory disease mortality. NO2 (lag1) and O3 (lag0, lag1, lag2, lag01,lag02, lag03) were associated with daily non-accidental death and NO2 (lag1, lag3, lag03) and O3 (lag0, lag1, lag01,lag02, lag03) were associated with daily circulatory disease mortality. In the co-pollutant models, the risk estimates for PM2.5 changed slightly. The excess mortality risk of non-accidental and circulatory diseases was higher for women, people with low education, and died outside hospital.
Conclusions
We found that short-term exposure to PM2.5 increased the mortality risk of non-accidental and circulatory diseases among the elderly in Changchun. Women, people with low education and died outside hospital are more susceptible to PM2.5. NO2 and O3 were also associated with an increase in mortality from non-accidental and circulatory diseases and the O3 is a high effect.
1.Introduction
Ambient air pollution (AAP), which has a substantial impact on human health, has become a global public health risk[1]. Data from the World Health Organization (WHO) show that 98% of cities in the world's low- and middle-income countries experience high levels of air pollution[2]. Fine particulate matter (PM2.5, particulate matter with an aerodynamic diameter less than or equal to 2.5 μm) is a principal air pollutant [3]. PM2.5 is a mixture of various compounds that can enter major organ systems through the lungs, and it has multiple adverse effects on human health, especially on the respiratory and circulatory systems[4–8]. Numerous epidemiologic studies have reported the short-term effects of PM2.5[9–12]. However, short-term effects varied by exposure levels, air pollutant, population characteristics, and geographic location[13].
The WHO air quality guidelines (AQGs) set an annual mean of 10 μg/m3 and a 24-hour mean of 25 μg/m3 for PM2.5, and the risks of short-term and long-term mortality can be significantly reduced at below-mean concentrations[14]. Globally, the population-weighted average concentration of PM2.5 continues to increase, and 87% of people worldwide were exposed to PM2.5 levels greater than 10 μg/m3 in 2013[15].
In China, PM2.5 pollution is more severe. Only 4% of Chinese people live in areas that meet the WHO AQGs[15]. In 2013, 760,000 people in China died from exposure to PM2.5[16]. As the capital city of Jilin Province (China), Changchun is the largest automobile industrial city in China and the birthplace of China's automobile, film, optical, bio-pharmaceutical, and track bus industries. In 2017, the total area was 20,565 square kilometres, with a total registered population of 7.489 million and an urban population of 4.383 million. The energy source of Changchun mainly consists of coal, making it a soot polluted city. In recent years, with the increase in car ownership, there is a trend towards mixed pollution. Due to the long heating period, the air pollution in Changchun is more serious in the winter. No study on the relationship between short-term exposure to PM2.5 and mortality risk has been conducted in Changchun. Since the elderly are more vulnerable to air pollution[17,18], we therefore conducted a time-series study of the elderly in Changchun to evaluate the short-term effect of PM2.5 on non-accidental and circulatory disease mortality, and explored the potential effect modification by sex, education and death location.
2. Materials and methods
2.1. Data
2.1.1. Mortality data
Daily mortality data for residents in Changchun from January 1, 2014, to January 1, 2017, was obtained from the Jilin Provincial Center for Disease Control and Prevention. The anonymous records included age, sex, date of death, and the underlying cause of death. The underlying causes of death are classified by the International Classification of Diseases (ICD-10), in which non-accidental mortality are A00-R99 and circulatory system diseases are I00~I99. To determine the daily death toll, we selected all the elderly (≥65 years old) who ‘died of non-accidental causes and those who died of circulatory diseases and stratified them by sex, education and death location.
2.1.2. Air pollution and meteorology data
Daily air pollution data were obtained from ten national environmental monitoring stations in Changchun, including PM2.5, particulate matter with an aerodynamic diameter of equal or less than 10 μm (PM10), sulphur dioxide (SO2), nitrogen dioxide (NO2) and ozone (O3) (average concentration over 8 hours). Each indicator has at least 27 daily averages per month (at least 25 daily averages in February), and at least 324 daily averages per year. Daily meteorology data were obtained from the Changchun meteorological bureau, including average relative humidity and mean temperature. The annual data loss rate is less than 5%, and each index has at least 347 daily mean values per year. Audits of the validity, accuracy, normalization of the data, and of data quality can be used for analysis.
2.2. Statistical analysis
Spearman's rank correlation test was used to evaluate the correlation between air pollutants and meteorological conditions. The generalized additive Poisson regression model (GAM) was used to analyse the impact of air pollutants on the mortality of people. We applied smoothing spline functions to control the effects of confounding factors such as daily mean temperature, relative humidity, secular trend and seasonality on population mortality. The day of the week (DOW) was included in the multiple regression model as a dummy variable. The basic model was as follows:
where:
-
--
E(Yi) is the expected daily death toll;
-
--
s(.) is the smoothing spline function for nonlinear variables;
-
--
β is the regression coefficient;
-
--
ν is the degree of freedom. The degree of freedom was selected according to minimum Akaike information criterion (AIC). We applied the following degrees of freedom (df): 7/year for the time trend and 3 for mean temperature and average relative humidity;
-
--
dow is the day of the week;
-
--
α is the intercept
We fit single pollutant models to examine PM2.5 effects with different lag structures of single-day (distributed lag: lag0-lag3) and multi-day (moving average lag: lag01-lag03). In single-day models, lag0 and lag1 for example correspond to the pollution concentration on the day and the day before. In multi-day lag models, lag03 for example corresponds to a 4-day moving average pollutant concentration of the current and previous 3 days. To test the sensitivity of the model, a multi-pollutant model was established when the PM2.5 effect was strongest. Considering that there may be collinearity among air pollutants, other pollutants (PM10, SO2, NO2, O3) are entered in the multi- pollutant model step-by-step. The excess risk (ER) was used to evaluate the increased death risk of non-accidental and circulatory diseases with each increase of 10μg/m3 of air pollutants (ER = (RR-1)×100%; RR, relative risk). We also stratified the association of daily mortality with PM2.5 by sex, education, and death location (died in hospital versus outside of hospital).
SPSS(Version 17.0; IBM Corp, Armonk, New York, USA) was used for descriptive analysis and Spearman correlation analysis, and R software (version 3.5.0; http://www.r-project.org) was used for time series analysis, with test degree α = 0.05.
3. Results
3.1. Descriptive statistics
From January 2014 to January 2017, a total of 46,780 non-accidental deaths were reported among the elderly (≥65 years old) in Changchun, of which 26,498 died of circulatory diseases. The mean daily deaths from non-accidental and circulatory diseases were 32.0 and 18.1, respectively. The daily average temperature was 7.0°C, and the daily average relative humidity was 60.1%. The daily mean concentration of PM2.5 was 55.9 μg/m3, with a Standard deviation (SD) of 49.5 μg/m3. For the other air pollutants, the daily mean concentrations of PM10, SO2, NO2 and O3 were 93.3 μg/m3, 30.7 μg/m3, 40.8 μg/m3 and 89.1 μg/m3, respectively (Table 1).
Table 1. Descriptive statistics.
| Index | Mean | Standard deviation | 25% quartile | Median | 75% quartile | Range |
|---|---|---|---|---|---|---|
| Pollution concentration | ||||||
| PM2.5 (μg/m3) | 55.9 | 49.5 | 25.0 | 41.0 | 71.0 | 481.0 |
| PM10 (μg/m3) | 93.3 | 66.2 | 53.0 | 77.0 | 114.0 | 12.0 |
| SO2 (μg/m3) | 30.7 | 28.9 | 8.0 | 16.0 | 48.0 | 148.0 |
| NO2 (μg/m3) | 40.8 | 14.0 | 30.0 | 39.0 | 48.0 | 98.0 |
| O3 (μg/m3) | 89.1 | 38.1 | 58.0 | 82.0 | 113.0 | 212.0 |
| Meteorology measures | ||||||
| Mean temperature (°C) | 7.0 | 13.8 | -5.8 | 9.2 | 19.5 | 52.6 |
| Average relative humidity (%) | 60.1 | 16.8 | 48.0 | 61.0 | 73.0 | 86.0 |
| Daily non-accidental death counts1 | ||||||
| Total | 32.0 | 6.5 | 27.0 | 32.0 | 36.0 | 39.0 |
| Women | 15.2 | 4.3 | 12.0 | 15.0 | 18.0 | 26.0 |
| Men | 16.8 | 4.4 | 14.0 | 17.0 | 20.0 | 28.0 |
| Junior high school and below | 24.1 | 5.6 | 20.0 | 24.0 | 28.0 | 35.0 |
| High school degree or above | 8.0 | 3.1 | 6.0 | 8.0 | 10.0 | 26.0 |
| Died in the hospital | 15.8 | 4.3 | 13.0 | 15.0 | 19.0 | 28.0 |
| Died outside the hospital | 16.2 | 4.5 | 13.0 | 16.0 | 19.0 | 28.0 |
| Daily circulatory diseases death counts2 (I00-I99) | ||||||
| Total | 18.1 | 4.7 | 15.0 | 18.0 | 21.0 | 33.0 |
| Women | 9.0 | 3.3 | 7.0 | 9.0 | 11.0 | 21.0 |
| Men | 9.1 | 3.1 | 7.0 | 9.0 | 11.0 | 21.0 |
| Junior high school and below | 14.2 | 4.2 | 11.0 | 14.0 | 17.0 | 29.0 |
| High school degree or above | 3.9 | 2.2 | 2.0 | 4.0 | 5.0 | 16.0 |
| Died in the hospital | 6.7 | 2.7 | 5.0 | 6.0 | 9.0 | 17.0 |
| Died outside the hospital | 11.4 | 3.7 | 9.0 | 11.0 | 14.0 | 24.0 |
1 people who died of all-nonaccidental causes
2 people who died of circulatory diseases.
3.2. Spearman correlation between air pollutants and weather conditions
PM2.5 was positively correlated with PM10 (r = 0.83), SO2 (r = 0.52) and NO2 (r = 0.72). O3, mean temperature and relative humidity were negatively correlated with PM2.5 (Table 2).
Table 2. Spearman correlation between air pollutants and weather conditions.
| Index | PM2.5 | PM10 | SO2 | NO2 | O3 | CO |
|---|---|---|---|---|---|---|
| PM2.5 | - | - | - | - | - | - |
| PM10 | 0.83** | - | - | - | - | - |
| SO2 | 0.52** | 0.37** | - | - | - | - |
| NO2 | 0.72** | 0.57** | 0.49** | - | - | - |
| O3 | -0.17** | -0.03* | -0.50** | -0.11** | - | - |
| Mean temperature | -0.34** | -0.21** | -0.81** | -0.25** | 0.70** | - |
| Average relative humidity | -0.02** | -0.22** | -0.05** | -0.09** | -0.23** | 0.09* |
*P<0.05
**P<0.01.
3.3. Single pollutant model
Table 3 shows the excess mortality risk of non-accidental and circulatory diseases for the elderly due to PM2.5 for each 10 μg/m3 increase on different lag days in single pollutant models. PM2.5 was associated with daily non-accidental mortality on lag1 and lag2 days, and the largest risk estimates were found with lag03; PM2.5 was associated with daily circulatory disease mortality on lag1, the largest risk estimates were also found with lag03.
Table 3. Association between 10 μg/m3 increase in PM2.5 and increase in deaths by lags.
| Lag days | ER of daily non-accidental death count (%) | ER of daily circulatory diseases death count (%) |
|---|---|---|
| lag0 | 0.21 (-0.02, 0.44) | 0.27 (-0.03, 0.57) |
| lag1 | 0.33 (0.10, 0.57)* | 0.38 (0.08, 0.68)* |
| lag2 | 0.23 (0.01, 0.46)* | 0.16 (-0.13, 0.45) |
| lag3 | 0.05 (-0.18, 0.28) | 0.14 (-0.15, 0.43) |
| lag01 | 0.35 (0.09, 0.62)* | 0.42 (0.08, 0.76)* |
| lag02 | 0.42 (0.12, 0.71)* | 0.44 (0.06, 0.81)* |
| lag03 | 0.39 (0.07, 0.70)* | 0.442 (0.04, 0.85)* |
*P<0.05
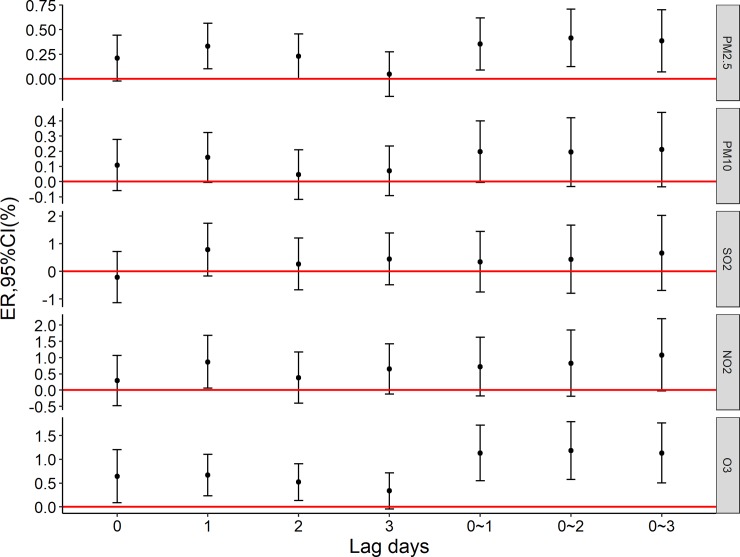
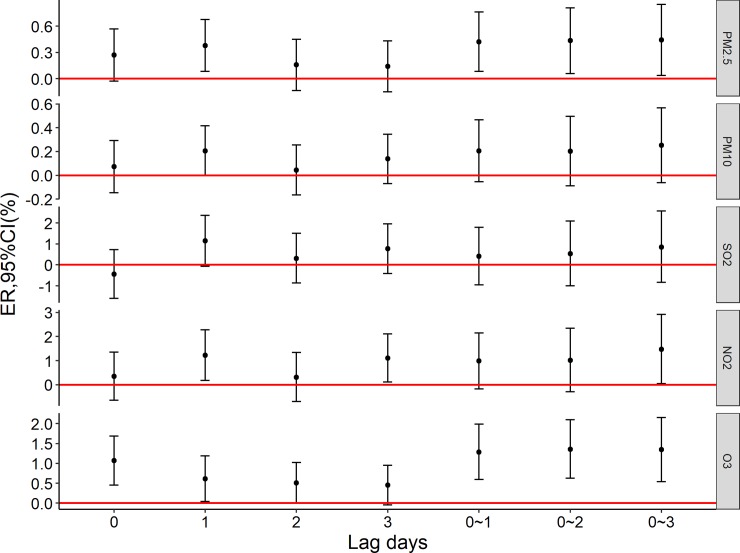
Fig 1 shows the excess mortality risk to the elderly population caused by per 10 μg/m3 increase in air pollutions. NO2 (lag1) and O3 (lag0, lag1, lag2, lag01,lag02, lag03) were associated with daily non-accidental death; Fig 2 shows the excess mortality risk to the elderly who die of circulatory diseases caused by per 10 μg/m3 increase in air pollution. NO2 (lag1, lag3, lag03) and O3 (lag0, lag1, lag01,lag02, lag03) were associated with daily circulatory disease mortality.
Fig 1. The excess mortality risk of non-accidental death per 10 μg/m3 increase in air pollutants.
Fig 2. The excess mortality risk of Circulatory diseases death per 10 μg/m3 increase in air pollutants.
3.4. Co-pollutant model
In the single pollutant models, an increment of PM2.5 by 10 μg/m3 at lag0-3 was associated with a 0.386% (95% CI: 0.07% to 0.70%) increase in daily non-accidental mortality and a 0.44% (95% CI: 0.04% to 0.85%) increase in daily circulatory disease mortality; NO2 was associated with increased daily circulatory disease mortality, and O3 was associated with increased daily non-accidental mortality and daily circulatory disease mortality. In the co-pollutant models, the risk estimates for PM2.5 changed slightly (Table 4).
Table 4. Association between a 10 μg/m3 increase in PM2.5 (lag 03 day) and an increase in deaths using the co-pollutant model.
| Pollutant model | ER of daily non-accidental death count (%) | ER of daily circulatory diseases death count (%) |
|---|---|---|
| Single pollutant model | ||
| PM2.5 | 0.36 (0.07, 0.70)* | 0.44 (0.04, 0.85)* |
| PM10 | 0.21 (-0.03, 0.46) | 0.25 (-0.06, 0.57) |
| SO2 | 0.65 (-0.96, 2.02) | 0.85 (-0.84, 2.57) |
| NO2 | 1.08 (-0.03, 2.20) | 1.48 (0.05, 2.92)* |
| O3 | 1.13 (0.50, 1.77)* | 1.34 (0.54, 2.15)* |
| Co-pollutant model | ||
| PM2.5+PM10 | 0.63 (-0.03, 1.30) | 0.68 (-0.18, 1.54) |
| PM2.5+SO2 | 0.39 (0.04, 0.73)* | 0.43 (-0.01, 0.86) |
| PM2.5+NO2 | 0.33 (-0.08, 0.75) | 0.30 (-0.23, 0.83) |
| PM2.5+O3 | 0.24 (-0.09, 0.57) | 0.28 (-0.14, 0.70) |
| PM2.5+PM10+SO2 | 0.64 (-0.06, 1.34) | 0.66 (-0.24, 1.56) |
| PM2.5+PM10+NO2 | 0.58 (-0.16, 1.33) | 0.50 (-0.46, 1.47) |
| PM2.5+PM10+O3 | 0.62 (-0.05, 1.28) | 0.65 (-0.20, 1.51) |
| PM2.5+SO2+NO2 | 0.33 (-0.08, 0.75) | 0.30 (-0.23, 0.83) |
| PM2.5+SO2+O3 | 0.22 (-0.14, 0.57) | 0.23 (-0.23, 0.68) |
| PM2.5+NO2+O3 | 0.18 (-0.24, 0.60) | 0.11 (-0.43, 0.66) |
*P<0.05
3.5. Subgroup analysis
The excess mortality risk of non-accidental and circulatory diseases was higher for women, people with low education and died outside hospital than it was for men, poeple with high education and died in hospital (Table 5).
Table 5. Association between a 10 μg/m3 increase in PM2.5 (lag 03 day) and an increase in deaths using the single pollutant model, according to sex, education and death location.
| Index | ER of daily non-accidental death count (%) | ER of daily circulatory diseases death count (%) |
|---|---|---|
| Sex | ||
| Women | 0.52 (0.10, 0.94)* | 0.65 (0.11, 1.19)* |
| Men | 0.38 (-0.04, 0.80) | 0.40 (-0.16, 0.96) |
| Education | ||
| Junior high school and below | 0.45 (0.09, 0.82)* | 0.54 (0.08, 0.99)* |
| High school degree or above | 0.24 (-0.36, 0.84) | 0.21 (-0.61, 1.04) |
| Death location | ||
| In the hospital | 0.24 (-0.36, 0.84) | 0.12 (-0.56, 0.79) |
| Outside the hospital | 0.52 (0.10, 0.95)* | 0.65 (0.15,1.15)* |
4. Discussion
Our study analysed the short-term effects of PM2.5 on the elderly in Changchun. This study is the first study to examine the relationship between PM2.5 and population mortality in Jilin Province. We found that PM2.5 was associated with an increase in mortality from non-accidental and circulatory diseases. There appears to be a greater impact of PM2.5 on mortality from non-accidental and circulatory diseases on women, poeple with low education and died outside hospital. NO2 and O3 were also associated with an increase in mortality from non-accidental and circulatory diseases. The effect of O3 is higher than other pollutants.
The estimated effects in our study of PM2.5 on non-accidental mortality risk were lower than effects observed in a worldwide meta-analysis of a 1.04% (0.52%-1.56%) per 10 μg/m3 increase in PM2.5[19]. This discrepancy could be due to differences in population composition, geographical location and PM2.5 sources. However, compared with studies of Chinese populations, the estimated effects in our study are higher. For example, a recent Chinese multicity study found that the risk of non-accidental death increased by 0.22% for every 10 μg/m3 increase in PM2.5 (lag01)[20]. In another study, mortality risks for non-accidental deaths increased by 0.25% at lag days 0–1 for every 10 μg/m3 increase in PM2.5[21]. The larger effect estimates observed in our study may be due to the age of the subject. We studied the elderly and the elderly make up a high-risk group[22,23]. The short-term association of PM2.5 with mortality from circulatory diseases was consistent with previous epidemiological studies[17]. PM2.5 may reduce cardiac parasympathetic input leading to decreased heart rate variability (HRV)[24,25]. Additionally, the direct translocation of PM2.5 into the circulatory system can lead to an acute cardiovascular response[26–28].
For the metric of mortality from non-accidental and circulatory diseases, women, people with low education and died outside hospital were found to have increased susceptibility to PM2.5. Previous studies on the gender-specific health effects of air pollution are lacking, and the patterns are not conclusive. For example, Franklin et al. studied over 1.3 million deaths in 27 US communities and found that women were more susceptible than men to the mortality effects of PM2.5[29]. Hong et al. also found that elderly woman were more susceptible than elderly men to the mortality effects of PM10[30]. Similarly, a statement from the American Heart Association (AHA) concluded that particulate matter exposure may contribute to higher cardiovascular mortality in women[31]. There are some reasons that may explain the increased vulnerability of women. Inhaled particles could deposit regionally in women.[32]; women have fewer red blood cells than men, so women are more vulnerable to the toxic effects of air pollution[33]; in addition, the high reactivity of the airway to oxidants, hormonal status, smoking rates, and even a relatively low socioeconomic status are also possible causes[34]. However, the exact reasons for the gender-specific effects of air pollution on health are unclear and deserve further investigation.
Our study found that the impact on non-accidental and circulatory disease mortality from PM2.5 is higher for those at a lower education level than for those with a higher education level, which is consistent with previous observations on individual education level[35]. In epidemiological studies, education has been used as a surrogate indicator of socioeconomic status (SES)[36]. It is well known that SES can affect health indicators such as mortality[37]. People with a lower SES are more likely to be exposed to air pollutants and are more likely to suffer from diseases linked to air pollution that confer a greater risk of dying[38–40]. People of a lower SES may also receive inferior medical treatment and less health care, making them more susceptible to the effects of air pollution[18]. In addition, people with a lower SES may have more limited access to fish, fresh fruits and vegetables, resulting in a reduced intake of protective fatty acids and vitamins[41].
Our results showed that the impact of PM2.5 on mortality from non-accidental and circulatory diseases appears to be greater among people that die outside of a hospital. People outside hospital are less likely to acquire knowledge about PM2.5 prevention and have more exposure risks. In addition, it is more difficult for people outside hospital to receive timely treatment to alleviate a condition in the event of an outbreak.
Changchun is located in northeast China and has significant seasonal differences. Although the annual average concentration of gaseous pollutants such as SO2, NO2 and O3 is not high, both SO2 and NO2 maintain relatively high levels during heating periods in the winter, while O3 is relatively high in the summer, which exposes residents to persistent hazards from different air pollutants in different seasons. Our results showed that NO2 and O3 can increase the risk of non-accidental death in the elderly, and there was also a lag effect. Previous studies have also reached the same conclusion[42]. With co-pollutant adjustment in multi-pollutant models, the effect of PM2.5 on mortality changed slightly. This result suggests that our model is relatively stable.
The findings support public policy-related activities focused on the reduction of PM2.5 levels and the improvement of target daily PM2.5 standards. The estimation of the short-term mortality risk due to short-term exposure to PM2.5 can also help in planning appropriate medical interventions. Some limitations exist in our study: (1) Our study was based in a single city, Changchun, and generalizations need to be made in conjunction with other evidence. (2) Although it is considered reasonable to use the ambient pollutant concentration of PM2.5 to represent individual exposure[43], there may be errors in the PM2.5 exposure of different subgroups[44]. Further studies of the relationship between PM2.5 and mortality are needed.
5. Conclusions
We found that short-term exposure to PM2.5 increased the mortality risk of non-accidental and circulatory diseases among the elderly in Changchun. Women, people with low education and died outside hospital are more susceptible to PM2.5. NO2 and O3 were also associated with an increase in mortality from non-accidental and circulatory diseases and the O3 is a high effect.
Supporting information
(XLSX)
Data Availability
The survey was implemented by Jilin Center for Disease Control and Prevention in Jilin Province in 2014-2017. The national health and health commission of China requires that data from national projects remain confidential in order to protect patient privacy. If the data needs to be accessed please contact the department of environmental and health hazards prevention and control, jilin provincial center for disease control and prevention (E-mail: jlcdchjs@163.com).
Funding Statement
China's central government subsidizes projects to monitor the impact of local air pollution on people's health; Key scientific research project of Jilin Provincial Health and Family Planning Commission in 2015 (2015Z03).
References
- 1.Ren M, Fang X (2017) Concentration-Response Relationship between PM2.5 and Daily Respiratory Deaths in China: A Systematic Review and Metaregression Analysis of Time-Series Studies. 2017: 5806185 10.1155/2017/5806185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li P, Xin J, Wang Y, Li G, Pan X, Wang S, et al. (2015) Association between particulate matter and its chemical constituents of urban air pollution and daily mortality or morbidity in Beijing City. Environ Sci Pollut Res Int 22: 358–368. 10.1007/s11356-014-3301-1 [DOI] [PubMed] [Google Scholar]
- 3.(1973) Electric heating versus oil heating in the service territory of Long Island Lighting Company. II. An analysis of air pollution effects associated with electric heating and oil-fired on site heating.
- 4.Kim KH, Kabir E, Kabir S (2015) A review on the human health impact of airborne particulate matter. Environment International 74: 136–143. 10.1016/j.envint.2014.10.005 [DOI] [PubMed] [Google Scholar]
- 5.Evangelia S, Massimo S, Sophia R, Bart O, Christophe D, Ester A, et al. (2013) Associations between Fine and Coarse Particles and Mortality in Mediterranean Cities: Results from the MED-PARTICLES Project. Environmental Health Perspectives 121: 932–938. 10.1289/ehp.1206124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lepeule J, Laden F, Dockery D, Schwartz J (2012) Chronic exposure to fine particles and mortality: an extended follow-up of the Harvard Six Cities study from 1974 to 2009. Environ Health Perspect 120: 965–970. 10.1289/ehp.1104660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y, et al. (2009) Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res Rep Health Eff Inst: 5–114; discussion 115–136. [PubMed] [Google Scholar]
- 8.Kloog I, Nordio F, Zanobetti A, Coull BA, Koutrakis P, Schwartz JD. (2014) Short term effects of particle exposure on hospital admissions in the Mid-Atlantic states: a population estimate. PLoS One 9: e88578 10.1371/journal.pone.0088578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kloog I, Ridgway B, Koutrakis P, Coull BA, Schwartz JD (2013) Long- and short-term exposure to PM2.5 and mortality: using novel exposure models. Epidemiology 24: 555–561. 10.1097/EDE.0b013e318294beaa [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janssen NA, Fischer P, Marra M, Ameling C, Cassee FR (2013) Short-term effects of PM2.5, PM10 and PM2.5–10 on daily mortality in The Netherlands. Sci Total Environ 463–464: 20–26. 10.1016/j.scitotenv.2013.05.062 [DOI] [PubMed] [Google Scholar]
- 11.Apte JS, Marshall JD, Cohen AJ, Brauer M (2015) Addressing Global Mortality from Ambient PM2.5. Environ Sci Technol 49: 8057–8066. 10.1021/acs.est.5b01236 [DOI] [PubMed] [Google Scholar]
- 12.Baxter LK, Duvall RM, Sacks J (2013) Examining the effects of air pollution composition on within region differences in PM2.5 mortality risk estimates. J Expo Sci Environ Epidemiol 23: 457–465. 10.1038/jes.2012.114 [DOI] [PubMed] [Google Scholar]
- 13.Petronella SA, Conboy-Ellis K (2003) Asthma epidemiology: risk factors, case finding, and the role of asthma coalitions. Nurs Clin North Am 38: 725–735. [DOI] [PubMed] [Google Scholar]
- 14.Organization WH (2007) Air quality guidelines: Global update 2005. Particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Indian Journal of Medical Research 4: 492–493. [Google Scholar]
- 15.Brauer M, Freedman G, Frostad J, van Donkelaar A, Martin RV, Dentener F, et al. (2016) Ambient Air Pollution Exposure Estimation for the Global Burden of Disease 2013. Environ Sci Technol 50: 79–88. 10.1021/acs.est.5b03709 [DOI] [PubMed] [Google Scholar]
- 16.Song Y, Wang X, Maher BA, Li F, Xu C, Liu X, et al. (2016) The spatial-temporal characteristics and health impacts of ambient fine particulate matter in China. Journal of Cleaner Production 112: 1312–1318. [Google Scholar]
- 17.Liang H, Qiu H, Tian L (2018) Short-term effects of fine particulate matter on acute myocardial infraction mortality and years of life lost: A time series study in Hong Kong. Sci Total Environ 615: 558–563. 10.1016/j.scitotenv.2017.09.266 [DOI] [PubMed] [Google Scholar]
- 18.Yang C, Peng X, Huang W, Chen R, Xu Z, Chen B, et al. (2012) A time-stratified case-crossover study of fine particulate matter air pollution and mortality in Guangzhou, China. Int Arch Occup Environ Health 85: 579–585. 10.1007/s00420-011-0707-7 [DOI] [PubMed] [Google Scholar]
- 19.Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA (2015) Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Journal of Exposure Science & Environmental Epidemiology 25: 208–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen R, Yin P, Meng X, Liu C, Wang L, Xu X, et al. (2017) Fine Particulate Air Pollution and Daily Mortality. A Nationwide Analysis in 272 Chinese Cities. Am J Respir Crit Care Med 196: 73–81. 10.1164/rccm.201609-1862OC [DOI] [PubMed] [Google Scholar]
- 21.Li T, Yan M, Sun Q, Anderson GB (2018) Mortality risks from a spectrum of causes associated with wide-ranging exposure to fine particulate matter: A case-crossover study in Beijing, China. Environ Int 111: 52–59. 10.1016/j.envint.2017.10.023 [DOI] [PubMed] [Google Scholar]
- 22.Cox LA Jr., Popken DA, Ricci PF (2013) Warmer is healthier: effects on mortality rates of changes in average fine particulate matter (PM2.5) concentrations and temperatures in 100 U.S. cities. Regul Toxicol Pharmacol 66: 336–346. 10.1016/j.yrtph.2013.05.006 [DOI] [PubMed] [Google Scholar]
- 23.Wang Y, Shi L, Lee M, Liu P, Di Q, Zanobetti A, et al. (2017) Long-term Exposure to PM2.5 and Mortality Among Older Adults in the Southeastern US. Epidemiology 28: 207–214. 10.1097/EDE.0000000000000614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Devlin RB, Ghio AJ, Kehrl H, Sanders G, Cascio W (2003) Elderly humans exposed to concentrated air pollution particles have decreased heart rate variability. Eur Respir J Suppl 40: 76s–80s. [DOI] [PubMed] [Google Scholar]
- 25.Gong H Jr., Linn WS, Terrell SL, Clark KW, Geller MD, Anderson KR, et al. (2004) Altered heart-rate variability in asthmatic and healthy volunteers exposed to concentrated ambient coarse particles. Inhal Toxicol 16: 335–343. 10.1080/08958370490439470 [DOI] [PubMed] [Google Scholar]
- 26.Fiordelisi A, Piscitelli P, Trimarco B, Coscioni E, Iaccarino G, Sorriento D. (2017) The mechanisms of air pollution and particulate matter in cardiovascular diseases. 22: 337–347. 10.1007/s10741-017-9606-7 [DOI] [PubMed] [Google Scholar]
- 27.Niu J, Liberda EN, Qu S, Guo X, Li X, Zhang J, et al. (2013) The role of metal components in the cardiovascular effects of PM2.5. PLoS One 8: e83782 10.1371/journal.pone.0083782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zuo L, Youtz DJ, Wold LE (2011) Particulate matter exposure exacerbates high glucose-induced cardiomyocyte dysfunction through ROS generation. PLoS One 6: e23116 10.1371/journal.pone.0023116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franklin M, Zeka A, Schwartz J (2007) Association between PM2.5 and all-cause and specific-cause mortality in 27 US communities. Journal of Exposure Science & Environmental Epidemiology 17: 279. [DOI] [PubMed] [Google Scholar]
- 30.Hong YC, Lee JT, Kim H, Ha EH, Schwartz J, Christiani DC. (2002) Effects of air pollutants on acute stroke mortality. Environ Health Perspect 110: 187–191. 10.1289/ehp.02110187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. (2010) Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 121: 2331–2378. 10.1161/CIR.0b013e3181dbece1 [DOI] [PubMed] [Google Scholar]
- 32.Kim CS, Hu SC (1998) Regional deposition of inhaled particles in human lungs: comparison between men and women. J Appl Physiol (1985) 84: 1834–1844. 10.1152/jappl.1998.84.6.1834 [DOI] [PubMed] [Google Scholar]
- 33.Sorensen M, Daneshvar B, Hansen M, Dragsted LO, Hertel O, Knudsen L, et al. (2003) Personal PM2.5 exposure and markers of oxidative stress in blood. Environ Health Perspect 111: 161–166. 10.1289/ehp.111-1241344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clougherty JE (2010) A growing role for gender analysis in air pollution epidemiology. Environ Health Perspect 118: 167–176. 10.1289/ehp.0900994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kan H, London SJ, Chen G, Zhang Y, Song G, et al. (2008) Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The Public Health and Air Pollution in Asia (PAPA) Study. Environ Health Perspect 116: 1183–1188. 10.1289/ehp.10851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zeka A, Zanobetti A, Schwartz J (2006) Individual-level modifiers of the effects of particulate matter on daily mortality. Am J Epidemiol 163: 849–859. 10.1093/aje/kwj116 [DOI] [PubMed] [Google Scholar]
- 37.Wilkinson RG (1997) Socioeconomic inequalities in morbidity and mortality in western Europe. Lancet 350: 516–517; author reply 517–518. [DOI] [PubMed] [Google Scholar]
- 38.Sexton K, Gong H Jr., Bailar JC 3rd, Ford JG, Gold DR, Lambert WE, et al. (1993) Air pollution health risks: do class and race matter? Toxicol Ind Health 9: 843–878. [DOI] [PubMed] [Google Scholar]
- 39.Rotko T, Kousa A, Alm S, Jantunen M (2001) Exposures to nitrogen dioxide in EXPOLIS-Helsinki: microenvironment, behavioral and sociodemographic factors. J Expo Anal Environ Epidemiol 11: 216–223. 10.1038/sj.jea.7500162 [DOI] [PubMed] [Google Scholar]
- 40.Pellizzari ED, Perritt RL, Clayton CA (1999) National human exposure assessment survey (NHEXAS): exploratory survey of exposure among population subgroups in EPA Region V. J Expo Anal Environ Epidemiol 9: 49–55. [DOI] [PubMed] [Google Scholar]
- 41.Romieu I, Téllez-Rojo MM, Lazo M, Manzano-Patiño A, Cortez-Lugo M, Julien P, et al. (2005) Omega-3 fatty acid prevents heart rate variability reductions associated with particulate matter. American Journal of Respiratory & Critical Care Medicine 172: 1534. [DOI] [PubMed] [Google Scholar]
- 42.Chen R, Pan G, Zhang Y, Xu Q, Zeng G, Xu X, et al. (2011) Ambient carbon monoxide and daily mortality in three Chinese cities: the China Air Pollution and Health Effects Study (CAPES). Sci Total Environ 409: 4923–4928. 10.1016/j.scitotenv.2011.08.029 [DOI] [PubMed] [Google Scholar]
- 43.Schwartz J, Sarnat JA, Coull BA, Wilson WE (2007) Effects of exposure measurement error on particle matter epidemiology: a simulation using data from a panel study in Baltimore, MD. J Expo Sci Environ Epidemiol 17 Suppl 2: S2–10. [DOI] [PubMed] [Google Scholar]
- 44.Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. (2000) Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect 108: 419–426. 10.1289/ehp.00108419 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
The survey was implemented by Jilin Center for Disease Control and Prevention in Jilin Province in 2014-2017. The national health and health commission of China requires that data from national projects remain confidential in order to protect patient privacy. If the data needs to be accessed please contact the department of environmental and health hazards prevention and control, jilin provincial center for disease control and prevention (E-mail: jlcdchjs@163.com).