Abstract
Purpose:
Adult T-cell leukemia (ATL) is usually CD25+ and rapidly fatal. Anti-CD25 recombinant immunotoxin LMB-2 had phase I activity limited by immunogenicity and rapid growth. To prevent antidrug antibodies and leukemic progression between cycles, a phase II trial was performed with LMB-2 after cyclophosphamide and fludarabine.
Experimental Design:
ATL patients received cyclophosphamide and fludarabine days 1 to 3 and 2 weeks later began up to 6 cycles at 3-week intervals of cyclophosphamide and fludarabine days 1 to 3 followed by LMB-2 30–40 μg/kg i.v. days 3, 5, and 7. Three different dose levels of cyclophosphamide and fludarabine were used, 20+200 (n = 3), 25+250 (n = 12), and 30+300 mg/m2 (n = 2).
Results:
Of 17 patients enrolled and treated with fludarabine and cyclophosphamide for cycle-1, 15 received subsequent cycle (s) containing LMB-2 and were therefore evaluable for response. Lack of antibody formation permitted retreatment in most patients. Of 10 evaluable leukemic patients receiving 25+250 or 30+300 mg/m2 of fludarabine and cyclophosphamide, 6 (60%) achieved complete remission (CR) and 2 (20%) partial remission (PR), and all 5 with >25% leukemic cells achieved CR. No responses were achieved in 5 with lymphomatous ATL or lower fludarabine and cyclophosphamide doses. Median CR duration for the 6 CRs was 40 weeks. One is without detectable ATL at 47 months. Toxicity was mostly attributable to fludarabine and cyclophosphamide. Capillary leak from LMB-2 was non-dose limiting. One patient in CR died of a preexisting infection.
Conclusions:
LMB-2, administered with fludarabine and cyclophosphamide to prevent antidrug antibodies and rapid intercycle progression, is highly effective in achieving CR in leukemia ATL. Fludarabine and cyclophosphamide dose/schedule is important for safety and efficacy in this high-risk population.
Introduction
Adult T-cell leukemia is an aggressive CD4+/CD25+ T-cell lymphoproliferative disorder caused by human T-cell lymphotropic virus type I (HTLV-I; refs. 1, 2), with clusters of cases in southwestern Japan, the Caribbean basin, northeastern South America, central Africa, and the southeastern United States (3). It is estimated that 15 to 20 million people are infected with HTLV-1 worldwide (4). Seroprevalence rates are up to 10% in southwestern Japan, and up to 6% in the Caribbean basin, including Jamaica and Trinidad. Those infected have a cumulative lifetime risk of 1 to 5 percent for developing ATL (3, 5). Median survival from diagnosis was reported to be approximately 6, 10, and 24 months for acute, lymphoma, and chronic types, respectively, and longer for smoldering type (6). Treatment of aggressive (acute and lymphomatous) ATL includes multiagent cytotoxic and myelosuppressive chemotherapy, including VCAP-AMP-VECP or high-intensity (biweekly) CHOP (CHOP-14), with or without stem cell transplantation (7–9). Unfortunately, despite the complete remission (CR) rates of 40% and 25% for VCAP-AMP-VECP and CHOP-14, respectively, 3-year survival rate was only 24% and 13% and toxicity was high, with grade 4 neutropenia in 98% versus 83%. Thus, treatment options for aggressive ATL remain clearly suboptimal.
The HTLV-1 viral genome encodes the 42-kDa Tax transactivating transcription factor that activates the HTLV-I long terminal repeat (LTR), the expression of viral genes, and the transcription of cellular genes encoding multiple growth factors and their receptors, including IL2 receptor α (IL2Rα), also called CD25 (10). CD25 has low affinity for IL2 (11), and is expressed on ATL cells freshly obtained from patients at levels of 1,600 to 21,000 (median 8,800) sites/cells (12). To target CD25 on ATL, the anti-CD25 monoclonal antibody (mAb) anti-Tac was developed (13, 14), and in murine or humanized form displayed antitumor activity in patients with this disease (15–17). To direct a cytotoxic toxin to ATL cells via CD25, the variable domains of anti-Tac were fused together with a peptide linker and then connected to a truncated form of Pseudomonas exotoxin (18). The resulting recombinant immunotoxin anti-Tac(Fv)-PE40 and its slightly shorter derivative anti-Tac(Fv)-PE38 (called LMB-2) were selectively cytotoxic toward CD25+ malignant cells, including ATL-derived cell lines, and patient samples (19–23). In a phase I trial of LMB-2 in patients with hematologic malignancies, 2 patients with ATL were included (24), both of whom had rapid reductions of circulating malignant cells, but only one achieved partial response and outcome was compromised by both immunogenicity and rapid regrowth of ATL.
To address both immunogenicity and rapid regrowth after response of LMB-2 in ATL, we used fludarabine and cyclophosphamide with LMB-2. The choice of fludarabine and cyclophosphamide as the induction chemotherapy was based on the association of fludarabine with a lower incidence of human anti-mouse antibody (HAMA) after the mAb tositumomab (25), the utility of cyclophosphamide in the treatment of ATL, and the ability of fludarabine and cyclophosphamide to decrease T-cell augmentation (26, 27), which may be important for humoral immunity to LMB-2. We had also reported synergy when a nucleoside analogue, namely gemcitabine, was combined with LMB-2 in targeting murine xenografts displaying human CD25 (28). Patients were pretreated with fludarabine and cyclophosphamide alone, and after 2 weeks were treated with cycles of fludarabine and cyclophosphamide immediately preceding LMB-2. Because of the activity seen on this ongoing trial, we now report early promising results of safety, immunogenicity, and response to fludarabine and cyclophosphamide/LMB-2 in patients at different dose levels of fludarabine and cyclophosphamide.
Patients and Methods
Eligibility
LMB-2 and fludarabine and cyclophosphamide were administered by a phase II protocol approved by the Institutional review board of the NCI (Bethesda, MD). All patients received treatment at the NIH Clinical Center (Bethesda, MD). Patients required a diagnosis of HTLV-1–associated ATL and CD25 positivity. Acute, lymphomatous, and chronic subtypes are eligible, as well as smoldering ATL patients with symptomatic skin lesions. Patients required prior treatment unless they were ineligible for or refused other treatments. Baseline-neutralizing antibodies could not neutralize >75% of the activity of 200 ng/mL of LMB-2 (24). Performance status required ECOG 0–2, neutrophil count ≥ 1,000/μL, and platelets >50,000/μL. Exclusions were similar to those published (24) and included chemotherapy (except hydroxyurea) within 3 weeks.
Study design
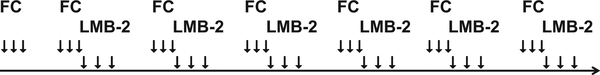
The trial was designed with fludarabine and cyclophosphamide at a fixed dose level of 25+250 mg/m2 on days 1, 2, and 3 of each cycle, and a dose escalation of LMB-2 from 30 to 40 μg/kg on days 3, 5, and 7 (QOD × 3) if 3 evaluable patients tolerated 30 μg/kg QOD × 3 without dose-limiting toxicity (DLT). Because of lack of toxicity and presence of anti-drug antibodies, the dose level of fludarabine and cyclophosphamide was raised by amendment with the 8th patient to 30 + 300 mg/m2 but due to thrombocytopenia in patient CF09 returned to 25 + 250 mg/m2. To explore whether a lower dose of fludarabine and cyclophosphamide might also be associated with major responses, 20 + 200 mg/m2 was used for 3 patients (Table 2). The infusion times for fludarabine and cyclophosphamide were 30 and 60 minutes, respectively, each in 100 mL 0.9% saline, and fludarabine and cyclophosphamide was administered on days 1, 2, and 3 of each cycle, with cycle 1 containing only fludarabine and cyclophosphamide, and cycles 2 and 7 containing LMB-2 on days 3, 5, and 7. As shown in Fig. 1, cycle 2 began 2 weeks after day 1 of cycle 1, and subsequent cycles were 3 weeks apart.
Table 2.
Results of LMB-2 preceded by fludarabine and cyclophosphamide
| Fludarabine | Cyclophosphamide | LMB-2a (μg/kg) d3, 5, 7 | Total cycles given | Best response | Response duration (wk) |
Time (wk) to |
LMB-2 immunogenicity | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | (mg/m2) d1, 2, 3 | CR | PR | CR | PR | |||||
| CF01 | 25 | 250 | N/A | 1 | NE | NE | ||||
| CF02 | 25 | 250 | 30 | 3 | SD | N | ||||
| CF03 | 25 | 250 | 30 | 5 | CR | 15 | 30 | 4.7 | 4.7 | Y |
| CF04 | 25 | 250 | 30 | 3 | SD | N | ||||
| CF05 | 25 | 250 | 40 | 5 | PR | 96 | 14.0 | Y | ||
| CF06 | 25 | 250 | 40 | 2 | PD | N | ||||
| CF07 | 25 | 250 | 40 | 3 | SD | N | ||||
| CF08b | 30 | 300 | 40 | 4 | CR | 62 | 65 | 5.1 | 1.9 | Y |
| CF09 | 30 | 300 | 40 | 3 | PR | 8 | 1.7 | N | ||
| CF10 | 25 | 250 | 40 | 7 | CR | 203+ | 207+ | 4.7 | 0.6 | N |
| CF11 | 25 | 250 | 40 | 2 | PD | N | ||||
| CF12c | 25 | 250 | 40 | 7 | CR | 71 | 74 | 5.3 | 1.6 | N |
| CF13 | 25 | 250 | 40 | 7 | CR | 19 | 108 | 10.6 | 1.7 | Y |
| CF14d | 25 | 250 | 40 | 5 | CR | 12 | 15 | 4.4 | 1.7 | N |
| CF15 | 20 | 200 | N/A | 1 | NE | NE | ||||
| CF16 | 20 | 200 | 40 | 3 | SD | N | ||||
| CF17 | 20 | 200 | 40 | 2 | PD | NE | ||||
LMB-2 began with cycle 2.
CF08 received fludarabine and cyclophosphamide but no LMB-2 for cycle 4.
CF12 received cyclophosphamide 200 mg/m2 for cycle 3 and no fludarabine and cyclophosphamide thereafter.
CF14 received no fludarabine and cyclophosphamide after cycle 2.
Figure 1.
Schema for the fludarabine and cyclophosphamide (FC)/LMB-2 trial. Cycle 1 contained only fludarabine and cyclophosphamide on days 1, 2, and 3. Cycles 2–7, which began 2 weeks after cycle 1, contained fludarabine and cyclophosphamide on days 1, 2, and 3, LMB-2 on days 3, 5 and 7, and were 3 weeks apart.
Statistical trial design
The trial was designed using a Simon optimal two-stage design (29) to rule out a 35% response rate and target a 60% response rate. With α= 0.10 and β= 0.10 (the probabilities of accepting a poor treatment and rejecting a beneficial treatment, respectively), the trial was to have a first stage of 16 evaluable patients and if 7 or more patients would have response duration of 8 weeks or longer, then accrual would continue to a second stage. At the end of the second stage, 13 or more patients with responses of 8 weeks or longer out of a total of 27 patients would be considered promising. In this trial, the response endpoint for the first stage was met after achievement of response in the 13th patient, so this report includes early results from the trial for those initial 13 patients as well as 4 subsequently enrolled.
Drug administration
LMB-2, as previously reported (24), was given by intravenous infusion over 30 minutes. Per protocol, the LMB-2 dose level was 30 μg/kg every other day for 3 doses (QOD × 3) for the first 3 evaluable patients, and then subsequently 40 μg/kg QOD × 3. Hydration with 500 mL of 5% dextrose containing 0.45% saline was administered prior to and after fludarabine and cyclophosphamide, 1 liter of the same fluid before and after LMB-2, but only 1 liter between fludarabine and cyclophosphamide and LMB-2 on day 3. Oral premedications to prevent allergic reaction of LMB-2 were as previously reported (24).
Response evaluation
CR criteria included resolution of radiographic measurable disease to short axis ≤1.5 cm if >1.5 at baseline, or <1 cm if 1.1–1.5 cm at baseline, normalization of markers of response including LDH, regression in spleen size to nonpalpable if enlarged at baseline, negative bone marrow histology, and negative flow cytometry of blood for ATL cells. PET scans were used as a research tool but not to determine response. Partial response (PR) required a ≥50% reduction in circulating ATL count, ≥50% reduction in measurable lesions, and no growing or new lesions. Circulating ATL counts below 100 cells/mm3 by flow cytometry were not considered high enough to prevent consideration of PR by other criteria. Progressive disease was defined as a ≥50% increase in tumor size or doubling of the circulating ATL count.
Assays
Neutralizing antibody and pharmacokinetic assays were performed as previously described (24). Plasma levels of LMB-2 were determined by testing dilutions of posttreatment plasma for cytotoxicity toward SP2/Tac and comparing with a standard cytotoxicity curve using purified LMB-2 (24). The soluble CD25 assay was performed either using the Human CD25/IL2 R alpha ELISA Kit from R&D Systems, or a lab ELISA assay with comparable results. For the latter, Nunc Maxi sorb plates (Sigma-Aldrich) were coated with daclizumab (humanized anti-Tac), 0.1 μg/100 μL/well, washed with TPBS (PBS containing 0.05% Tween 20 (Sigma-Aldrich)], blocked with 300 μL/well of 1% BSA in PBS, washed with TPBS, incubated with patient serum diluted at least 1:10 with PBS, washed with TPBS, incubated with murine mAb 7g7 in PBS, washed with TPBS, incubated with biotinylated goat anti-mouse mAb (Jackson ImmunoResearch), washed with TPBS, incubated with Avidine–HRP conjugate (Biosource) diluted 1:2,500 with PBS containing 1% BSA and 0.05% Tween 20, washed with TPBS followed by PBS, incubated 15 minutes with TMB-peroxide substrate (Sigma-Aldrich), stopped with 2N H2SO4 and read at 450 nm.
Statistical analyses
Duration of PR and CR were determined by the Kaplan–Meier method, beginning at the date the PR or CR was identified. Progression-free survival (PFS) was determined by the Kaplan–Meier method beginning at the on-study date and continuing until progression or last follow-up without progression. A log-rank test was used to determine the statistical significance of the difference between two Kaplan–Meier curves. Pharmacokinetic parameters were compared between two groups indicated using an exact Wilcoxon rank sum test, separately for cycle 2 and cycle 3. For these exploratory comparisons, results are presented without formal correction for multiple comparisons, but in the context of the large number of tests performed with varying degrees of independence and dependence, P < 0.005 could be considered a statistically significant difference while 0.005 < P <0.05 would be considered a strong trend. Comparison of the fraction of patients with respect to development of immunogenicity was done using the Fisher exact test. All P values are two tailed except where indicated.
Results
Patient characteristics
The characteristics of the patients are listed in Table 1. The 17 patients enrolled included 6 males and 11 females. Ages ranged from 22 to 69 (median 37). Four patients had lymphoma type disease with <1% malignant cells in the blood, while the other patients met criteria for acute leukemic ATL based on hypercalcemia and/or high LDH. Despite high LDH prior to enrollment, disease activity in one of the patients (CF05) was more consistent with smoldering ATL with symptomatic skin lesions. Only 1 patient was treatment naïve, 8 had prior CHOP, 2 had prior EPOCH with rituximab and siplizumab (EPOCH-RS), 3 had prior alemtuzumab with either EPOCH or CHOP, and one had ESHAP. Three patients had hydroxyurea, given to decrease rapidly progressive leukemic ATL and hypercalcemia prior to enrollment. While patients were restricted from prior chemotherapy or steroids within 3 weeks of enrollment, hydroxyurea could be used up until the day before enrollment providing it was not increased during the week prior to enrollment. As patients CF10, CF13, and CF17 refused standard chemotherapy and were ineligible for other protocols, they were eligible without further prior therapy. The 4 patients with lymphomatous ATL had solid masses 1.9 to 9 cm in maximal diameter. The other 13 patients had 80–213,000 (median 5604) ATL cells/mm3 in the peripheral blood, comprising 1.02% to 95.6% (median 39%) of the circulating white blood cells. These levels were measured on or several days prior to the first dose of fludarabine and cyclophosphamide, except for patient CF09, who on the day of enrollment had <1% ATL cells because the white blood cell count contained 52% eosinophils due to ATL-associated eosinophilia. This patient had hypercalcemia, high LDH, and no lymphomatous masses consistent with acute ATL, and had >1% ATL cells in the blood 7.5 months prior to enrollment just before EPOCH-RS (Table 1). Seven (41%) of the 17 patients had hypercalcemia and all had high LDH consistent with acute or lymphomatous ATL. Extravascular sites included bone, lung, skin lesions and subcutaneous nodules, pelvis, muscle, lymph node, and enlarged spleen. Nodal or tumor masses, present in 10 patients, ranged from 1.7 to 9 cm (median 2.4 cm). Splenomegaly was present in 5 patients with a maximum spleen diameter of 15 to 20 cm (median 17.5 cm).
Table 1.
Patient characteristics
| Patient | Age | Sex | Type | Prior treatment | ATL cells/mm3 | ATL cells (%) | High Ca++ | High LDH | Extravascular sites | Max tumor size |
|---|---|---|---|---|---|---|---|---|---|---|
| CF01 | 28 | M | Acute | CHOP | 450 | 6.7 | Y | Y | Bone, lung, skin | <1 cm |
| CF02 | 51 | F | Lymphoma | EPOCH-C | 0 | 0.0 | N | Y | Thigh (skin) | 9 cm |
| CF03 | 31 | F | Acute | CHOP | 408 | 11.8 | Y | Y | Pelvis | 5.6 cm |
| CF04 | 34 | M | Acute | C, ESHAP, PTX, Gem | 687 | 5.1 | N | Y | Muscle | <1 cm |
| CF05 | 55 | M | Acute | Medi507, Ontak, HAT | 80 | 1.02 | N | Y | Skin | <1 cm |
| CF06 | 43 | F | Lymphoma | CHOP | 0 | 0.0 | N | Y | LN | 1.9 cm |
| CF07 | 29 | F | Acute | CHOP, C | 246 | 12.5 | N | Y | LN | 2 cm |
| CF08 | 27 | M | Acute | CHOP, C | 5,604 | 48.1 | Y | Y | Spleen, LN | 20, 1.8 cm |
| CF09 | 69 | F | Acute | EPOCH-RS | 206 | 1.3 | Y | Y | Subcutaneous | <1 cm |
| CF10 | 53 | F | Acute | None | 8,216 | 63.1 | N | Y | None | <1 cm |
| CF11 | 37 | F | Lymphoma | EPOCH-RS | 1 | 0.1 | N | Y | Subcutaneous | 5.8 cm |
| CF12 | 45 | F | Acute | CHOP | 13,153 | 49.8 | N | Y | Spleen, LN | 18.5, 1.7 cm |
| CF13 | 27 | F | Acute | Hydroxyurea | 210,000 | 92.2 | Y | Y | Spleen | 17.5 cm |
| CF14 | 45 | F | Acute | CHOP, Hydroxyurea | 24,112 | 59.5 | Y | Y | Spleen | 17 cm |
| CF15 | 35 | F | Acute | CHOP | 7,737 | 39.0 | N | Y | Spleen, LN | 15, 2.5 cm |
| CF16 | 22 | M | Lymphoma | LSG-15, radiation | 0 | 0.0 | N | Y | Bone, subcutaneous | 6 cm |
| CF17 | 48 | M | Acute | Hydroxyurea | 213,000 | 95.6 | Y | Y | LN | 2.2 cm |
NOTE: Prior treatments included cyclophosphamide, adriamycin, vincristine and prednisone (CHOP), these 4 agents with etoposide (EPOCH) and campath (C or alemtuzumab, together EPOCH-C), etoposide, methylprednisolone, cytarabine, and cisplatin (ESHAP), pralatrexate (PTX), gemcitabine (Gem), Siplizumab (Medi507), denileukin diftitox (Ontak), daclizumab or humanized anti-Tac (HAT), and EPOCH with rituximab and siplizumab (EPOCH-RS). The LSG-15 regimen includes prednisone, adriamycin, carmustine, etoposide, carboplatin, and vinorelbine. High Ca++ is a corrected calcium > 2.74, and high LDH is > 400 u/L. Extravascular sites include lymph nodes (LN) and the maximum size is listed, respectively, with the maximum spleen diameter.
Response and dose levels
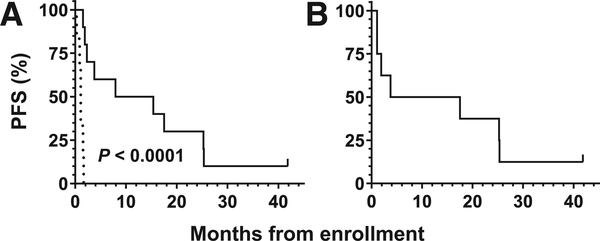
To determine whether fludarabine and cyclophosphamide chemotherapy would be associated with major response to LMB-2, patients received fludarabine and cyclophosphamide at 3 dose levels, 20 and 200, 25 and 250, and 30 and 300 mg/m2, respectively, and LMB-2 at 2 different dose levels, 30 and 40 μg/kg QOD × 3. As shown in Table 2, 2 of 17 patients were none-valuable for LMB-2 response due to inability to receive the second cycle, which was the first cycle containing LMB-2, in CF01 due to withdrawing and in CF15 due to progressing prior to cycle 2. Of the remaining 15 patients evaluable for LMB-2 response, there were 6 CRs and 2 PRs. All 8 major responses were in the 10 evaluable leukemic (nonlymphomatous) patients receiving at least 25 and 250 mg/m2 of fludarabine and cyclophosphamide. In these 10 patients, the median PFS was 11.6 versus 1.1 months in the other 6 patients (P < 0.0001, Fig. 2A). In the 8 patients treated with 25 and 250 mg/m2 of fludarabine and cyclophosphamide and LMB-2 40 μg/kg × 3, median PFS was 10.6 months (Fig. 2B). The duration of CR ranged from 12 weeks to still responding at 203weeks (median 40.4). The patient with ongoing CR (CF10) originally presented with leukemic disease and both Cryptococcal meningitis and pulmonary abscess, requiring liposomal amphotericin and ventricular–peritoneal shunt. The patient returned to part-time work after cycle 5 and currently works full time. The duration of PR ranged from 8 weeks to still responding at 207 weeks (median 70). Among those with a PR, the time to PR was 0.6–14 (median 1.8) weeks, and among those with CR, the time to CR was 4.4–10.6 (median 4.9) weeks. Thus, the majority of patients who responded did so prior to the second cycle. As the durations of the first and subsequent cycles were 2 and 3 weeks, respectively (Fig. 1), the majority of CRs were achieved prior to cycle 3, that is, as a result of the first cycle containing LMB-2. When comparing the soluble CD25 levels (ng/mL) between responders (n = 8) and nonresponders (n = 8), the median (range) pretreatment levels were 32 (3.2–190) and 13 (3.7–127), respectively (P = 0.57), while the median nadir/posttreatment levels were 1.1 (undetectable–6.0) and 29 (5.2–319), respectively (P = 0.0006). By protocol, patients with CR before cycle 2, that is, due to fludarabine and cyclophosphamide alone, would not be able to continue, but no patients had CR by that point. Thus, CR appeared facilitated by fludarabine and cyclophosphamide, but likely required at least the second cycle that contained LMB-2.
Figure 2.
PFS to fludarabine and cyclophosphamide /LMB-2. In A, 6 patients with lymphoma or those receiving fludarabine and cyclophosphamide at 20 + 200 mg/m2 experienced a median PFS of 1.1 months versus 11.6 months in 10 patients with leukemia and 25 + 250 or 30 + 300 mg/m2 of fludarabine and cyclophosphamide (P < 0.0001). B, 8 patients treated with fludarabine and cyclophosphamide 25 + 250 mg/m2 and LMB-2 40 μg/kg had 10.6 month median PFS. Patient CF01 withdrew before cycle 2 and was nonevaluable for PFS.
Neutralizing antibodies
To determine whether pretreatment with fludarabine and cyclophosphamide was associated with lack of neutralizing antibodies to LMB-2, we assessed antidrug antibodies by cytotoxicity assay prior to and after each cycle. To determine whether a serum sample contained neutralizing antibodies, the serum was incubated with LMB-2 at 37°C for 15 minutes, and then diluted with cell culture media and tested for cytotoxicity against CD25+ cells. On the basis of previous results where 29 (60.4%) of 48 non-CLL patients historically produced antibodies neutralizing >25% of 1,000 ng/mL of LMB-2 when treated with it as a single agent, our goal was to avoid >25% neutralization of 1,000/mL. Patients with >75% neutralization of LMB-2 1,000 ng/mL could not receive additional cycles of LMB-2 as antitumor response was felt unlikely at this higher level of neutralization. CLL patients were not included in the historical control group because of their decreased ability to make antidrug antibodies to recombinant immunotoxins (24, 30). As shown in Table 2, 4 (29%) of 14 evaluable patients made high levels of neutralizing antibodies, and those patients received a total of 4, 5, 5, and 7 cycles. This rate of antidrug antibodies was substantially lower than that of our historical control group rate of 29 of 48 (60.4%, one-tailed P = 0.036, two-tailed P = 0.066), and thus was consistent with an effect of fludarabine and cyclophosphamide on immunogenicity. There was no evidence of less immunogenicity at higher doses of fludarabine and cyclophosphamide, with one of 2 patients at the highest dose level having neutralizing antibodies (Table 2), but the numbers of patients above and below 25 + 250 mg/m2 were few. To determine whether reductions of normal T and B cells were associated with immunogenicity of LMB-2, these cells were quantified by flow cytometry before and after the first cycle. Normal T cells were decreased by 27% to 96% (median 67%), and normal B-cells by 17% to 100% (median 96%), but the percent decreases were not associated with whether patients made high levels of neutralizing antibodies to LMB-2. Thus, fludarabine and cyclophosphamide was effective in decreasing normal T- and B-cells prior to exposure to LMB-2, and this decrease may have helped delay or prevent immunogenicity, but the amount of T- or B-cell reduction did not correlate with immunogenicity.
Table 4.
Pharmacokinetics of LMB-2 in ATL
| Dose (μg/kg) | Time point | n | Peak (ng/mL) | Cmax (ng/mL) | t1/2 (min) | AUC (μg-min/mL) | Vd (L) | Clearance (mL/min) | |
|---|---|---|---|---|---|---|---|---|---|
| 30 | C2 D1 | 3 | Range | 189–329 | 212–379 | 91–370 | 50–113 | 5.3–11.3 | 21–40 |
| Median | 303 | 356 | 104 | 54 | 5.6 | 37 | |||
| 30 | C2 D5 | 3 | Range | 204–306 | 88–182 | 208–581 | 66–152 | 8.9–22.1 | 16–30 |
| Median | 302 | 103 | 433 | 66 | 13.4 | 30 | |||
| 30 | C3–4 D1 | 4 | Range | 265–566 | 251–428 | 144–332 | 67–155 | 4.7–71.4 | 17–274 |
| Median | 374 | 346 | 176 | 90 | 32.4 | 143 | |||
| 30 | C3–4 D5 | 4 | Range | 354–916 | 229–582 | 136–411 | 105–214 | 3.6–8.4 | 10–18 |
| Median | 581 | 458 | 286 | 159 | 5.9 | 15 | |||
| 40 | C2 D1 | 12 | Range | 205–1,072 | 97–1,062 | 154–549 | 130–265 | 3.3–313 | 10.9–191 |
| Median | 727 | 243 | 365 | 167 | 73.6 | 115 | |||
| 40 | C2 D5 | 12 | Range | 166–932 | 119–1,629 | 173–530 | 111–406 | 2.2–193 | 5–223 |
| Median | 580 | 256 | 361 | 171 | 32.6 | 72 | |||
| 40 | C3–7 D1 | 23 | Range | 201–1,566 | 83–1,577 | 69–541 | 14–433 | 2.4–253 | 9–1,274 |
| Median | 609 | 479 | 178 | 147 | 20.0 | 69 | |||
| 40 | C3–7 D5 | 23 | Range | 453–1,905 | 242–1,677 | 70–509 | 50–565 | 2.3–73 | 0.2–355 |
| Median | 610 | 469 | 220 | 163 | 10.6 | 26 |
NOTE: Cycles of LMB-2 given but not evaluable due to neutralizing antibodies include cycle 5 for patients CF03 and CF05, and cycle 7 for patient CF13.
Discontinuation of therapy
As shown in Table 2, only 3 patients completed all 7 cycles. The most common reason for discontinuation was progressive disease (PD), which occurred before the first cycle of LMB-2 in 1 patient (CF15), after the first cycle of LMB-2 (cycle 2) in 3 patients (CF06, CF11, and CF17), and after cycle 3 in 5 patients (CF02, CF04, CF07, CF09, and CF16). Three patients stopped due to neutralizing antibodies (CF03, CF05, and CF08). One patient had grade 5 toxicity after cycle 5 (CF14), and one voluntarily withdrew before receiving LMB-2 (CF01). Thus, the most common cause of early discontinuation was not toxicity but rather progression in those not achieving CR early.
Safety of fludarabine and cyclophosphamide and LMB-2 in ATL
To determine toxicity of fludarabine and cyclophosphamide and LMB-2 in ATL, patients were monitored closely for adverse events due either to chemotherapy or LMB-2. Shown in Table 3 are adverse events attributed at least possibly to fludarabine and cyclophosphamide or LMB-2, including events of all grades occurring in at least 2 patients, and all grade ≥3 events. The most common events were fludarabine and cyclophosphamide related, including neutropenia, nausea/vomiting, and lymphopenia/leucopenia, thrombocytopenia, and anemia, encountered in 59% to 82% of the patients, and 35% to 71% experienced these toxicities at grade ≥3 level. Low CD4 count was attributed to fludarabine and cyclophosphamide and not to LMB-2, due to the low number of CD4+/CD25+ normal lymphocytes and their rapid renewal (31). The reduction of CD4+ normal T cells was an intended effect of fludarabine and cyclophosphamide to reduce immunogenicity. Fever was observed as a result of LMB-2, and, like neutropenic fever, was partially related to fludarabine and cyclophosphamide. Transaminases elevations, usually AST and less commonly ALT, were LMB-2–related, usually < grade 3, and never dose limiting per protocol, consistent with previous clinical testing (24). Evidence of capillary leak syndrome (CLS) with LMB-2 included hypoalbuminemia, hypotension, proteinuria, weight gain, and edema. Grade ≥3 infections were reported in 3 patients, including 2 cases of reversible pneumonia. One patient with prior CHOP and hydroxyurea and preexisting infection with vancomycin-resistant enterococcus (VRE), pneumocystis, and cytomegalovirus, had grade 4 pneumonia with Stenotrophomonas maltophilia during cycles 2 and 3, and grade 5 (fatal) VRE sepsis after cycle 5. As shown in Table 3, the fludarabine and cyclophosphamide-related hematologic toxicities appear somewhat less common at the lowest dose of fludarabine and cyclophosphamide, but the numbers of patients treated above or below 25 + 250 mg/m2 were too small for formal comparison. Thus, severe infections were encountered in a minority of these already immunosuppressed patients (32), and interfered with outcome particularly when infection was present at baseline.
Table 3.
Toxicity of LMB-2/fludarabine and cyclophosphamide in patients with ATL
| Toxicity in >1 patient | Fludarabine and cyclophosphamide dose levels (mg/m2; all grade 3–5 toxicity) |
Fludarabine and cyclophosphamide dose levels (mg/m2) |
|||||
|---|---|---|---|---|---|---|---|
| All grades | 20 + 200 | 25 + 250 | 30 + 300 | 20 + 200 | 25 + 250 | 30 + 300 | |
| Patients treated | n= 3 | n= 12 | n= 2 | n = 3 | n= 12 | n= 2 | |
| Neutropenia | 2 (67%) | 10 (83%) | 2 (100%) | Neutropenia | 1 (33%) | 9 (75%) | 2 (100%) |
| Nausea/vomiting/anorexia | 2 (67%) | 10 (83%) | 2 (100%) | Leukopenia/lymphopenia | 1 (33%) | 9 (75%) | 2 (100%) |
| Fever/chills | 1 (33%) | 10 (83%) | 1 (50%) | Anemia | 0 (0%) | 8 (67%) | 0 (0%) |
| Leukopenia/lymphopenia | 1 (33%) | 9 (75%) | 2 (100%) | Transaminases | 1 (33%) | 4 (33%) | 0 (0%) |
| Transaminases | 3 (100%) | 8 (67%) | 1 (50%) | Thrombocytopenia | 0 (0%) | 5 (42%) | 1 (50%) |
| Hypotension/tachycardia | 1 (33%) | 8 (67%) | 2 (100%) | Fever/chills | 0 (0%) | 3 (25%) | 1 (50%) |
| Thrombocytopenia | 1 (33%) | 8 (67%) | 2 (100%) | Pneumonitis | 0 (0%) | 3 (25%) | 0 (0%) |
| Anemia | 0 (0%) | 9 (75%) | 1 (50%) | Low CD4 count | 1 (33%) | 1 (8%) | 1 (50%) |
| Myalgia/headache | 2 (67%) | 7 (58%) | 2 (100%) | Hypotension/tachycardia | 0 (0%) | 2 (17%) | 0 (0%) |
| Hypoalbuminemia | 2 (67%) | 6 (50%) | 1 (50%) | Rectal hemorrhage | 0 (0%) | 1 (8%) | 0 (0%) |
| Hematuria | 1 (33%) | 5 (42%) | 1 (50%) | Bilirubin | 0 (0%) | 1 (8%) | 0 (0%) |
| Proteinuria | 0 (0%) | 7 (58%) | 0 (0%) | Dysuria | 0 (0%) | 1 (8%) | 0 (0%) |
| Fatigue/dizziness | 1 (33%) | 4 (33%) | 2 (100%) | Bladder infection | 0 (0%) | 1 (8%) | 0 (0%) |
| Edema | 0 (0%) | 6 (50%) | 0 (0%) | Hypoxia | 0 (0%) | 1 (8%) | 0 (0%) |
| Abdominal pain | 0 (0%) | 5 (42%) | 0 (0%) | Proteinuria | 0 (0%) | 1 (8%) | 0 (0%) |
| Diarrhea | 1 (33%) | 3 (25%) | 0 (0%) | Sepsis | 0 (0%) | 1 (8%)a | 0 (0%) |
| CPK | 0 (0%) | 4 (33%) | 0 (0%) | ||||
| Mucositis | 0 (0%) | 3 (25%) | 1 (50%) | ||||
| Hypomagnesemia | 0 (0%) | 3 (25%) | 0 (0%) | ||||
| Bilirubin | 1 (33%) | 2 (17%) | 0 (0%) | ||||
| Alkaline phosphatase/GGT | 0 (0%) | 3 (25%) | 0 (0%) | ||||
| Pneumonitis | 0 (0%) | 3 (25%) | 0 (0%) | ||||
| Low CD4 count | 1 (33%) | 1 (8%) | 1 (50%) | ||||
| Lipase | 0 (0%) | 3 (25%) | 0 (0%) | ||||
| Bladder infection | 0 (0%) | 2 (17%) | 0 (0%) | ||||
| Dyspnea | 0 (0%) | 2 (17%) | 0 (0%) | ||||
| Prothrombin time | 1 (33%) | 1 (8%) | 0 (0%) | ||||
| Pruritus | 1 (33%) | 0 (0%) | 1 (50%) | ||||
Grade 5 event.
Pharmacokinetics
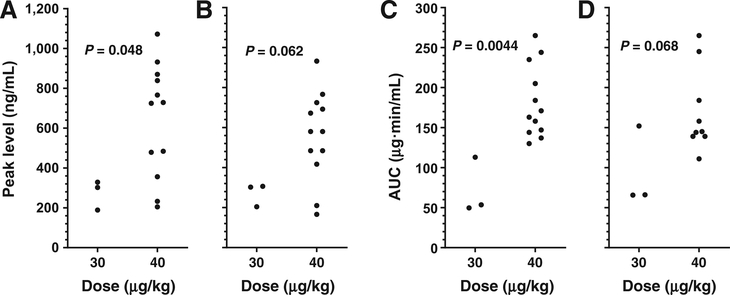
To determine the plasma levels of active LMB-2 that are available to bind to and kill the ATL cells, a cytotoxicity assay was performed in which dilutions of plasma were incubated with the CD25+ cell line SP2/Tac, and the cytotoxicity compared with that of purified LMB-2 on a standard curve (24). Plasma samples were generally taken for doses 1 and 3 (days 1 and 5) of each cycle, just after the end of infusion and then 1, 2, 3, 4, 10, and 24 hours later. Pharmacokinetic parameters were calculated from best fit of mono- or biexponential decay curves based on Akaike’s rule (24, 33). As shown in Table 4, peak plasma levels were 189–329 ng/mL (median 303 ng/mL) after the first dose of 30 μg/kg, versus 205–1,072 ng/mL (median 727 ng/mL) after the first dose of 40 μg/kg. As shown in Fig. 3, both peak levels and AUCs were higher at 40 than at 30 μg/kg QOD × 3, with the significance of the difference greater after the first (day 1) than after the third (day 5) dose.
Figure 3.
Pharmacokinetics of LMB-2 in patients treated with fludarabine and cyclophosphamide/LMB-2. Peak levels are shown in A and B after the first and third doses, respectively. AUCs are shown in C and D after the first and third doses, respectively. All results are from cycle 2, the first cycle containing LMB-2.
Discussion
To determine whether chemotherapy pretreatment could facilitate the efficacy of anti-CD25 recombinant immunotoxin LMB-2 in ATL by preventing both antidrug antibodies and rapid progression between cycles, patients with ATL received cycles of fludarabine and cyclophosphamide prior to LMB-2. We found that fludarabine and cyclophosphamide/LMB-2 was highly effective in inducing CR, particularly in ATL patients with leukemia rather than lymphoma, and in patients receiving at least 25 and 250 mg/m2 of fludarabine and cyclophosphamide, respectively. The endpoint of reducing the immunogenicity of LMB-2 to below the 60% incidence noted historically in non-CLL was reached at this point in the trial with a 29% rate of immunogenicity (one-tailed P = 0.035; two-tailed P = 0.066). The first-stage response endpoint of at least 7 responses out of up to 16 evaluable was also met. One patient remains in CR without minimal residual ATL for nearly 4 years. Additional patients with leukemic ATL on the second stage of this trial will receive fludarabine and cyclophosphamide at 25 and 250 mg/m2 and LMB-2 at 40 μg/kg QOD × 3; this combination was associated with a PFS of 10.6 months in leukemic ATL (Fig. 2B) and this LMB-2 dose was without DLT. No advantage was observed with a higher or lower dose level of fludarabine and cyclophosphamide.
Established and investigational treatments for ATL
Effective treatment of acute and lymphomatous ATL, and even less aggressive subtypes, including chronic ATL, has remained suboptimal at best. The most recommended first-line treatment for aggressive ATL is the multiagent sequential chemotherapy regimen VCAP–AMP–VECP, composed of vincristine, cyclophosphamide, doxorubicin, prednisolone (VCAP), doxorubicin, ranimustine, prednisolone (AMP), vindesine, etoposide, carboplatin, and prednisolone (VECP; refs. 7–9). A randomized trial showed that 3-year overall survival after first-line VCAP–AMP–VECP was higher than that of CHOP-14 (24% vs. 13%), but more toxic (8). Patients who can undergo allogeneic stem cell transplantation have better outcomes than those who cannot (34, 35). For relapsed ATL, which most of our patients had, there is no effective standard therapy (7). Options recently under clinical testing include the anti-CCR4 mAb mogamulizumab, brentuximab vedotin, and lenalidomide, bortezomib, forodesine, pralatrexate, panobinostat, alisertib, alemtuzumab, interferon, retroviral agents, and denileukin diftitox (7, 36). Clinical trials of denileukin diftitox, containing IL2 and truncated diphtheria toxin, have not been reported for ATL, and evidence of clinical activity is limited to several case reports, one of which required aggressive chemotherapy with hyper-CVAD (37, 38).
Fludarabine and cyclophosphamide/LMB-2 compared with primary chemotherapy
It is difficult to compare the results of fludarabine and cyclophosphamide/LMB-2 in this small study of mostly relapsed/refractory patients to those of first-line chemotherapy. As LMB-2 was without significant myelosuppressive toxicities, the incidence of grade 4 neutropenia and thrombocytopenia were 41% and 35%, respectively, compared with 98% and 74% reported for the VCAP–AMP–VECP regimen. Improved safety of fludarabine and cyclophosphamide might be obtained by longer delays for patients with fludarabine and cyclophosphamide–related toxicity. It is possible that fludarabine and cyclophosphamide decreased the ability of LMB-2 to cause CLS, as CLS-related events seemed milder and more infrequent than on the phase I single-agent trial. Of the 10 patients with nonlymphomatous ATL receiving LMB-2 with at least 25 and 250 mg/m2 of fludarabine and cyclophosphamide, the median OS was 18.5 months, and OS was 42, 53, and 56 months in 3 patients, 2 of whom are still alive. Thus, fludarabine and cyclophosphamide/LMB-2 containing 40 μg/kg QOD × 3 of LMB-2 and 25 and 250 mg/m2 of fludarabine and cyclophosphamide has activity and safety profile appropriate for further clinical testing in patients with ATL, particularly those with relapsed disease and limited alternatives. This protocol could be attempted as a bridge to allogeneic transplantation, which might improve the outcome in patients who completely respond but then relapse. However, that was not tested in this trial, and the 2 patients who went to allogeneic transplantation were either fully relapsed from CR (CF03) or had not responded to fludarabine and cyclophosphamide/LMB-2 (CF16).
Response to both fludarabine and cyclophosphamide and LMB-2
The fludarabine and cyclophosphamide regimen was chosen not only to prevent immunogenicity, but also for its potential cytotoxic effect against ATL. As fludarabine and cyclophosphamide was not possible to model in animals due to its pharmacokinetics in mice, we studied the pyrimidine analogue gemcitabine in CD25+ tumor bearing mice. We found that a single dose of gemcitabine was sufficient to decrease the intratumoral sCD25 in the mice, which prior to treatment was several orders of magnitude higher than the level of serum sCD25 (28). This antitumor activity of gemcitabine was associated with synergism when combined with LMB-2 (28). We have recently reported that targeted antigen shedding, while potentially helpful to the delivery of antimesothelin recombinant immunotoxin SS1P to tumor cells, may prevent delivery of LMB-2 to CD25+ tumor cells (39). Thus, depletion of intratumoral sCD25 by chemotherapy may allow LMB-2 to reach tumor cells in vivo, and allow complete remissions to occur. Chemotherapy might not only cause better delivery of LMB-2 to ATL tumor masses by reducing intratumoral sCD25, but also by decreasing circulating tumor cells and plasma sCD25, allowing longer exposure to higher plasma levels of LMB-2. We did not see complete remissions of ATL by fludarabine and cyclophosphamide alone after cycle 1, which would have made patients ineligible to begin LMB-2 with cycle 2. In fact, we often saw evidence of tumor progression prior to beginning cycle 2. Thus, while we cannot rule out that fludarabine and cyclophosphamide alone for repeated cycles could have achieved CRs, we believe this is unlikely due to the consistent presence of disease prior to LMB-2 and the known rapidity of progression of ATL between treatments. One unanswered question is whether fludarabine and cyclophosphamide is necessary for every cycle of LMB-2. During design of the protocol, fludarabine and cyclophosphamide was felt to be necessary on every cycle to prevent antidrug antibody formation to repeated doses of LMB-2. However, several patients, including CF12 and CF14, received multiple cycles of LMB-2 without fludarabine and cyclophosphamide due to its toxicity on prior cycles, without resulting in antidrug antibodies. Thus, it is possible that some patients might be able to receive repeated doses LMB-2 without antibodies after just a few cycles of fludarabine and cyclophosphamide.
Chemotherapy to reduce the immunogenicity of truncated pseudomonas exotoxin
We have reported high immunogenicity of the same truncated form of pseudomonas exotoxin (PE38), fused to an antimesothelin Fv. The resulting recombinant immunotoxin SS1P, either by continuous infusion or bolus dosing, had limited clinical activity at least partly due to inability to deliver multiple cycles (40, 41). To prevent immunogenicity of SS1P in mesothelioma and in potentially other solid tumors, it was administered combined with pentostatin and cyclophosphamide, which markedly delayed the onset of neutralizing antibodies (42). This led to major tumor regressions in several patients despite lack of response to prior chemotherapy. The pentostatin was particularly successful in lowering normal B and T cells without prolonged neutropenia or other dose-limiting myelosuppression. An important difference between the mesothelioma and ATL trials is that while chemotherapy was given to reduce antidrug antibodies in both, in the ATL trial it also was given to increase antitumor activity. Prevention of immunogenicity with purine analogues, including pentostatin and fludarabine, may be of use in the future for highly cytotoxic recombinant toxins, which may be limited by immunogenicity.
Translational Relevance.
Recombinant immunotoxins have shown clinical activity as single agents, but even patients with hematologic malignancies can make neutralizing antibodies to the bacterial toxin portion, limiting the number of treatments that may be given. One strategy to prevent antidrug antibodies and improve response is to coadminister chemotherapy, which would blunt the humoral immune response, and also reduce tumor burden. We used the highly aggressive adult T-cell leukemia (ATL) as a model for this approach and added fludarabine and cyclophosphamide chemotherapy to recombinant immunotoxin LMB-2. While LMB-2 alone previously resulted in transient responses, antidrug antibodies developed and disease rapidly progressed. In contrast, LMB-2 with fludarabine and cyclophosphamide produced durable partial and complete remissions. We believe that the approach of combining recombinant immunotoxin with chemotherapy, recently reported for mesothelioma, will prove effective in hematologic and other tumors.
Acknowledgments
The authors thank the research staff for handling patient issues, particularly Sonya Duke, Barbara Debrah, Lesley Matthews, Rita Mincemoyer, Natasha Kormanik, and Elizabeth Maestri. The authors also thank Dr. David Waters, Laura Wisch, Timothy McNickle, Inger Margulies, and Hong Zhou for technical assistance and Drs. John Janik and John Morris for referrals and helpful discussions.
Grant Support
This work was supported by the intramural research program, NIH, NCI. The trial was sponsored by the Cancer Therapy Evaluation Program, NCI.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Uchiyama T, Yodoi J, Sagawa K, Takatsuki K, Uchino H. Adult T-cell leukemia: clinical and hematologic features of 16 cases. Blood 1977;50:481–92. [PubMed] [Google Scholar]
- 2.Broder S, Bunn PA, Jaffe ES, Blattner W, Gallo RC, Wong-Staal F, et al. NIH conference. T-cell lymphoproliferative syndrome associated with human T-cell leukemia/lymphoma virus. Ann Intern Med 1984;100:543–57. [DOI] [PubMed] [Google Scholar]
- 3.Proietti FA, Carneiro-Proietti AB, Catalan-Soares BC, Murphy EL. Global epidemiology of HTLV-I infection and associated diseases. Oncogene 2005;24:6058–68. [DOI] [PubMed] [Google Scholar]
- 4.Satake M, Yamada Y, Atogami S, Yamaguchi K. The incidence of adult T-cell leukemia/lymphoma among human T-lymphotropic virus type 1 carriers in Japan. Leuk Lymphoma 2015;56:1806–12. [DOI] [PubMed] [Google Scholar]
- 5.Murphy EL, Hanchard B, Figueroa JP, Gibbs WN, Lofters WS, Campbell M, et al. Modelling the risk of adult T-cell leukemia/lymphoma in persons infected with human T-lymphotropic virus type I. Int J Cancer 1989;43: 250–3. [DOI] [PubMed] [Google Scholar]
- 6.Shimoyama M Diagnostic criteria and classification of clinical subtypes of adult T-cell leukaemia-lymphoma. A report from the Lymphoma Study Group (1984–87) Br J Haematol 1991;79:428–37. [DOI] [PubMed] [Google Scholar]
- 7.Ishitsuka K, Tamura K. Human T-cell leukaemia virus type I and adult T-cell leukaemia-lymphoma. Lancet Oncol 2014;15:e517–26. [DOI] [PubMed] [Google Scholar]
- 8.Tsukasaki K, Utsunomiya A, Fukuda H, Shibata T, Fukushima T, Takatsuka Y, et al. VCAP-AMP-VECP compared with biweekly CHOP for adult T-cell leukemia-lymphoma: Japan Clinical Oncology Group Study JCOG9801. J Clin Oncol 2007;25:5458–64. [DOI] [PubMed] [Google Scholar]
- 9.Tsukasaki K, Hermine O, Bazarbachi A, Ratner L, Ramos JC, Harrington W, et al. Definition, prognostic factors, treatment, and response criteria of adult T-cell leukemia-lymphoma: a proposal from an international consensus meeting. J Clin Oncol 2009;27:453–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeang KT, Boros I, Brady J, Radonovich M, Khoury G. Characterization of cellular factors that interact with the human T-cell leukemia virus type I p40x-responsive 21-base-pair sequence. J Virol 1988;62: 4499–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taniguchi T, Minami Y. The IL2/IL-2 receptor system: a current overview. Cell 1993;73:5–8. [DOI] [PubMed] [Google Scholar]
- 12.Kodaka T, Uchiyama T, Ishikawa T, Kamio M, Onishi R, Itoh K, et al. Interleukin-2 receptor b-chain (p70–75) expressed on leukemic cells from adult T cell leukemia patients. Jpn. J. Cancer Res 1990;81:902–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waldmann TA, Greene WC, Sarin PS, Saxinger C, Blayney DW, Blattner WA, et al. Functional and phenotypic comparison of human T cell leukemia/lymphoma virus positive adult T cell leukemia with human T cell leukemia/lymphoma virus negative Sézary leukemia and their distinction using anti-Tac. Monoclonal antibody identifying the human receptor for T cell growth factor. J Clin Invest 1984;73:1711–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waldmann TA, Longo DL, Leonard WJ, Depper JM, Thompson CB, Kronke M, et al. Interleukin 2 receptor (Tac antigen) expression in HTLV-1-associated adult T-cell leukemia. Cancer Res 1985;45:4559s–62s. [PubMed] [Google Scholar]
- 15.Waldmann TA, Goldman CK, Bongiovanni KF, Sharrow SO, Davey MP, Cease KB, et al. Therapy of patients with human T-cell lymphotrophic virus I-induced adult T-cell leukemia with anti-Tac, a monoclonal antibody to the receptor for interleukin-2. Blood 1988;72:1805–16. [PubMed] [Google Scholar]
- 16.Waldmann TA, White JD, Carrasquillo JA, Reynolds JC, Paik CH, Gansow OA, et al. Radioimmunotherapy of interleukin-2R alpha-expressing adult T-cell leukemia with Yttrium-90-labeled anti-Tac [see comments]. Blood 1995;86:4063–75. [PubMed] [Google Scholar]
- 17.Berkowitz JL, Janik JE, Stewart DM, Jaffe ES, Stetler-Stevenson M, Shih JH,et al. Safety, efficacy, and pharmacokinetics/pharmacodynamics of daclizumab (anti-CD25) in patients with adult T-cell leukemia/lymphoma. Clin Immunol 2014;155:176–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chaudhary VK, Queen C, Junghans RP, Waldmann TA, FitzGerald DJ,Pastan I. A recombinant immunotoxin consisting of two antibody variable domains fused to Pseudomonas exotoxin. Nature 1989;339: 394–7. [DOI] [PubMed] [Google Scholar]
- 19.Kreitman RJ, Chaudhary VK, Waldmann T, Willingham MC, FitzGerald DJ, Pastan I. The recombinant immunotoxin anti-Tac(Fv)-Pseuodomonas exotoxin 40 is cytotoxic toward peripheral blood malignant cells from patients with adult T-cell leukemia. Proc Natl Acad Sci. U S A 1990; 87:8291–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kreitman RJ, Chaudhary VK, Waldmann TA, Hanchard B, Cranston B, FitzGerald DJP, et al. Cytotoxic activities of recombinant immunotoxins composed of Pseudomonas toxin or diphtheria toxin toward lymphocytes from patients with adult T-cell leukemia. Leukemia 1993;7: 553–62. [PubMed] [Google Scholar]
- 21.Kreitman RJ, Pastan I. Targeting Pseudomonas exotoxin to hematologic malignancies. Semin Cancer Biol 1995;6:297–306. [DOI] [PubMed] [Google Scholar]
- 22.Kreitman RJ, Batra JK, Seetharam S, Chaudhary VK, FitzGerald DJ, Pastan I. Single-chain immunotoxin fusions between anti-Tac and Pseudomonas exotoxin: relative importance of the two toxin disulfide bonds. Bioconjug Chem 1993;4:112–20. [DOI] [PubMed] [Google Scholar]
- 23.Saito T, Kreitman RJ, Hanada S-i, Makino T, Utsunomiya A, Sumizawa T, et al. Cytotoxicity of recombinant Fab and Fv immunotoxins on adult T-cell leukemia lymph node and blood cells in the presence of soluble interleukin-2 receptor. Cancer Res 1994;54:1059–64. [PubMed] [Google Scholar]
- 24.Kreitman RJ, Wilson WH, White JD, Stetler-Stevenson M, Jaffe ES, Waldmann TA, et al. Phase I trial of recombinant immunotoxin Anti-Tac(Fv)-PE38 (LMB-2) in patients with hematologic malignancies. J Clin Oncol 2000;18:1614–36. [DOI] [PubMed] [Google Scholar]
- 25.Leonard JP, Coleman M, Kostakoglu L, Chadburn A, Cesarman E, Furman RR, et al. Abbreviated chemotherapy with fludarabine followed by tositumomab and iodine I 131 tositumomab for untreated follicular lymphoma. J Clin Oncol 2005;23:5696–704. [DOI] [PubMed] [Google Scholar]
- 26.Bishop MR, Steinberg SM, Gress RE, Hardy NM, Marchigiani D, KastenSportes C, et al. Targeted pretransplant host lymphocyte depletion prior to T-cell depleted reduced-intensity allogeneic stem cell transplantation. Br J Haematol 2004;126:837–43. [DOI] [PubMed] [Google Scholar]
- 27.Bishop MR, Fowler DH, Marchigiani D, Castro K, KastenSportes C, Steinberg SM, et al. Allogeneic lymphocytes induce tumor regression of advanced metastatic breast cancer. J Clin Oncol 2004;22:3886–92. [DOI] [PubMed] [Google Scholar]
- 28.Singh R, Zhang Y, Pastan I, Kreitman RJ. Synergistic antitumor activity of anti-CD25 recombinant immunotoxin LMB-2 with chemotherapy. Clin Cancer Res 2011;18:152–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simon R Optimal two-stage designs for phase II clinical trials. Control Clin Trials 1989;10:1–10. [DOI] [PubMed] [Google Scholar]
- 30.Kreitman RJ, Squires DR, Stetler-Stevenson M, Noel P, Fitzgerald DJ, Wilson WH, et al. Phase I trial of recombinant immunotoxin RFB4 (dsFv)-PE38 (BL22) in patients with B-cell malignancies. J Clin Oncol 2005;23:6719–29. [DOI] [PubMed] [Google Scholar]
- 31.Attia P, Powell DJ, Maker AV, Kreitman RJ, Pastan I, Rosenberg SA. Selective elimination of human regulatory T lymphocytes in vitro with the recombinant immunotoxin, LMB-2. J Immunother 2006;29:208–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White JD, Zaknoen SL, Kasten-Sportes C, Top LE, Navarro-Roman L, Nelson DL, et al. Infectious complications and immunodeficiency in patients with human T-cell lymphotropic virus I-associated adult T-cell leukemia/lymphoma. Cancer 1995;75:1598–607. [DOI] [PubMed] [Google Scholar]
- 33.Akaike H A new look at the statistical model identification. IEEE Transactions on Automatic Control 1974;19:716–23. [Google Scholar]
- 34.Kawada H, Yoshimitsu M, Nakamura D, Arai A, Hayashida M, Kamada Y, et al. A retrospective analysis of treatment outcomes in adult T cell leukemia/lymphoma patients with aggressive disease treated with or without allogeneic stem cell transplantation: A single-center experience. Biol Blood Marrow Transplant 2015;21:696–700. [DOI] [PubMed] [Google Scholar]
- 35.Bazarbachi A, Cwynarski K, Boumendil A, Finel H, Fields P, Raj K, et al. Outcome of patients with HTLV-1-associated adult T-cell leukemia/lymphoma after SCT: a retrospective study by the EBMT LWP. Bone Marrow Transplant 2014;49:1266–8. [DOI] [PubMed] [Google Scholar]
- 36.Tsukasaki K, Tobinai K. Human T-cell lymphotropic virus type I-associated adult T-cell leukemia-lymphoma: new directions in clinical research. Clin Cancer Res 2014;20:5217–25. [DOI] [PubMed] [Google Scholar]
- 37.Di Venuti G, Nawgiri R, Foss F. Denileukin diftitox and hyper-CVAD in the treatment of human T-cell lymphotropic virus 1-associated acute T-cell leukemia/lymphoma. Clin Lymphoma 2003;4:176–8. [DOI] [PubMed] [Google Scholar]
- 38.Manoukian G, Hagemeister F. Denileukin diftitox: a novel immunotoxin. Expert Opin Biol Ther 2009;9:1445–51. [DOI] [PubMed] [Google Scholar]
- 39.Pak Y, Pastan I, Kreitman RJ, Lee B. Effect of antigen shedding on targeted delivery of immunotoxins in solid tumors from a mathematical model. PLoS ONE 2014;9:e110716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hassan R, Bullock S, Premkumar A, Kreitman RJ, Kindler H, Willingham M, et al. Phase I study of SS1P, a recombinant anti-mesothelin immunotoxin given as a bolus I.V. infusion to patients with mesothelin-expressing mesothelioma, ovarian, and pancreatic cancers. Clin Cancer Res 2007; 13:5144–9. [DOI] [PubMed] [Google Scholar]
- 41.Kreitman RJ, Hassan R, FitzGerald DJ, Pastan I. Phase I Trial of Continuous Infusion Anti-Mesothelin Recombinant Immunotoxin SS1P. Clin Cancer Res 2009;15:5274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hassan R, Miller AC, Sharon E, Thomas A, Reynolds JC, Ling A, et al. Major cancer regressions in mesothelioma after treatment with an anti-mesothelin immunotoxin and immune suppression. Sci Transl Med 2013;5:208ra147. [DOI] [PMC free article] [PubMed] [Google Scholar]