In this study, we report results of a novel international airway registry of endotracheal intubation in the NICU and DR settings.
Abstract
BACKGROUND AND OBJECTIVES:
Neonatal tracheal intubation is a critical but potentially dangerous procedure. We sought to characterize intubation practice and outcomes in the NICU and delivery room (DR) settings and to identify potentially modifiable factors to improve neonatal intubation safety.
METHODS:
We developed the National Emergency Airway Registry for Neonates and collected standardized data for patients, providers, practices, and outcomes of neonatal intubation. Safety outcomes included adverse tracheal intubation–associated events (TIAEs) and severe oxygen desaturation (≥20% decline in oxygen saturation). We examined the relationship between intubation characteristics and adverse events with univariable tests and multivariable logistic regression.
RESULTS:
We captured 2009 NICU intubations and 598 DR intubations from 10 centers. Pediatric residents attempted 15% of NICU and 2% of DR intubations. In the NICU, the first attempt success rate was 49%, adverse TIAE rate was 18%, and severe desaturation rate was 48%. In the DR, 46% of intubations were successful on the first attempt, with 17% TIAE rate and 31% severe desaturation rate. Site-specific TIAE rates ranged from 9% to 50% (P < .001), and severe desaturation rates ranged from 29% to 69% (P = .001). Practices independently associated with reduced TIAEs in the NICU included video laryngoscope (adjusted odds ratio 0.46, 95% confidence interval 0.28–0.73) and paralytic premedication (adjusted odds ratio 0.38, 95% confidence interval 0.25–0.57).
CONCLUSIONS:
We implemented a novel multisite neonatal intubation registry and identified potentially modifiable factors associated with adverse events. Our results will inform future interventional studies to improve neonatal intubation safety.
What’s Known on This Subject:
Endotracheal intubation is a critical skill in neonatology but is less frequently performed than in previous years because of changes in neonatal practice. Little is known about the current practice and safety outcomes of neonatal intubation in the academic setting.
What This Study Adds:
Pediatric residents rarely perform neonatal intubation. Only half of first intubation attempts are successful, and adverse events and severe oxygen desaturation are common. Paralytic premedication and video laryngoscopy are associated with decreased adverse events in the NICU.
Neonatal tracheal intubation (TI) is a life-saving but potentially dangerous procedure.1 The authors of studies of pediatric patients demonstrate that adverse events are common during TI,2–4 but adverse events have not been comprehensively characterized in the NICU and delivery room (DR) settings. Many studies of neonatal TI practice and outcomes were single-site studies, had a relatively small number of infants enrolled, or were published >10 years ago.5–12 These studies may not generalize well or reflect current practice. Neonatal TI is less commonly performed in the current era because of changes in the management of infants born through meconium-stained amniotic fluid13 and more emphasis on noninvasive respiratory support for preterm infants.14 In addition, neonatal intubation practice has evolved in part because of recommendations for preprocedural medication for nonemergent intubation15,16 and the availability of video laryngoscopes for neonates.17
We sought to characterize the process and safety of neonatal TI across a wide spectrum of NICU settings. We established the National Emergency Airway Registry for Neonates (NEAR4NEOS), which was adapted from the National Emergency Airway Registry (NEAR)18 and the National Emergency Airway Registry for Children (NEAR4KIDS).2 Our objectives with this study were to characterize the current landscape of TI practice and outcomes in the NICU and DR settings and to identify potentially modifiable factors to improve the safety of TI in the neonatal population.
Methods
Settings
This study was conducted across 10 academic neonatal centers in North America, Europe, and Asia (Supplemental Table 7).
Design
NEAR4NEOS was based on the foundation of the NEAR4KIDS.2 We modified the NEAR4KIDS operational definitions and data collection form for the neonatal population, with extensive input from neonatologists and respiratory therapists from the initial NEAR4NEOS participating sites. Academic neonatal centers volunteered to collect and contribute patient, provider, practice, and outcome data for all intubations performed in the NICU and DR settings. Each site developed a compliance plan to ensure data were captured from >90% of all intubation encounters. This plan was reviewed and approved by 2 NEAR4NEOS compliance officers.
Staff at each participating site were trained in the NEAR4NEOS operational definitions, and local teams completed data collection forms at the time of each intubation. The data from each intubation were then entered into a secure research electronic data capture electronic data capture tool hosted at the Children’s Hospital of Philadelphia, a secure, Web-based application designed to support data capture for research studies.19 At all participating centers, this project was either granted institutional review board approval or deemed a quality improvement initiative exempt from institutional review board oversight.
Definitions and Outcome Measures
We used the same airway operational definitions as the NEAR and NEAR4KIDS registries.2,18 Briefly, an encounter is an episode of airway management. A course is 1 method for the intubation, including the device, approach (nasal or oral), and use of premedications. An attempt is defined as an airway maneuver that starts with the insertion of the device (ie, laryngoscope) into the patient’s mouth and ends when the device is removed. There can be many attempts by multiple providers within a given course as long as all attempts are made by using the same method (ie, the same airway device, approach, and medication regimen). If these variables are changed after failed attempts, this represents the start of a new course. To focus on the initial approach to neonatal TI, only the first course of each intubation encounter was included in this analysis.
Patient demographics recorded included weight at the time of intubation, gestational age at birth, and postnatal age at the time of intubation. We also collected information about underlying patient diagnoses and indications for intubation; >1 diagnosis and indication could be recorded for a given TI encounter. Airway devices included conventional laryngoscopes and video laryngoscopes. If a video laryngoscope was used, the device was coded as video laryngoscope, irrespective of whether the provider performed the intubation with a direct or indirect view. Premedications were classified as “sedative and/or narcotic” (including opiates, benzodiazepines, and barbiturates) and “paralytic” (including depolarizing or nondepolarizing neuromuscular blockade).
Successful airway management was defined as endotracheal tube placement in the trachea, confirmed by chest rise, auscultation, second independent laryngoscopy, carbon dioxide (Co2) detection, and/or chest radiograph. First-attempt success was defined as successful intubation on the first attempt by the first airway provider. Success within 2 attempts was reported when the same airway provider performed the first and second attempts. Overall course success was defined as successful intubation by any provider on any attempt within that course.
Adverse tracheal intubation–associated events (TIAEs) were categorized as nonsevere (esophageal intubation with immediate recognition, dysrhythmia [including any duration of heart rate <60 beats per minute without chest compressions performed], mainstem bronchial intubation, gum or dental trauma, emesis without aspiration, pain and/or agitation requiring additional medications causing a delay in intubation, epistaxis, and lip trauma) and severe (cardiac arrest, esophageal intubation with delayed recognition, hypotension requiring therapy, cardiac compressions <1 minute, laryngospasm, pneumothorax and/or pneumomediastinum, and direct airway injury). Esophageal intubation with delayed recognition was defined as placement of the endotracheal tube into the esophagus or hypopharynx with a lapse of time and clinical deterioration (such as desaturation) before the misplaced tube was removed.
Oxygen desaturations were captured separately from adverse TIAEs. We recorded the highest pulse oxygen saturation (Spo2) measurement immediately before the first intubation attempt and the lowest measured Spo2 during the intubation. Severe oxygen desaturations were defined as ≥20% decrease in oxygen saturation from the highest level achieved immediately before the first attempt and were only reported for intubations for which a preintubation Spo2 level was recorded.
Statistical Analysis
Using Stata 14.0 (Stata Corp, College Station, TX), we generated summary statistics for patient characteristics and intubation practice and outcome measures. These characteristics are presented separately for the NICU and DR settings because neonatal TI practice and outcomes may vary between these distinct environments. We graphically presented site-level variance in adverse events (severe desaturations and adverse TIAEs) for TIs in the NICU setting and assessed for differences in adverse events among hospitals using χ2 test.
For intubations in the NICU setting, we examined the association between patient, practice, and provider characteristics and outcomes of TIAEs and severe desaturations using χ2 test or Fisher’s exact test for categorical variables and the Wilcoxon rank test for nonparametric variables. Factors that were significant in univariable analysis (P < .05) were included in logistic regression models for each outcome (adverse TIAEs and severe desaturations). A P value <.05 was considered statistically significant.
Using similar methods, we examined the association between intubation characteristics and TIAEs and severe desaturations in the DR setting, excluding practice characteristics that were not routinely used across multiple sites. Because fewer practice characteristics were examined, we did not perform multivariable analyses for intubations in the DR.
Results
We collected data on 2607 intubation encounters in 10 centers from October 1, 2014, through March 31, 2017 (Table 1). Of these, 2009 TIs occurred in the NICU setting, and 598 took place in the DR. Patient demographics are shown in Table 1. The most common underlying diagnosis in both settings was acute respiratory failure, and the most common indications for intubation were oxygen failure, ventilation failure, and surfactant administration.
TABLE 1.
Patient Characteristics
| Characteristic | NICU Intubations (N = 2009) | DR Intubations (N = 598) |
|---|---|---|
| Dosing wt, g, median (IQR) | 1800 (980–3000) | 1549 (790–2900) |
| Gestational age at birth, wk, median (IQR) | 28 (25–35) | 30 (26–37) |
| Postnatal age, d, median (IQR) | 13 (1–49) | N/A |
| Diagnosisa, n (%) | ||
| Acute respiratory failure | 1174 (58) | 411 (69) |
| Chronic respiratory failure | 478 (24) | N/A |
| Congenital anomaly requiring surgery | 195 (10) | 142 (24) |
| Congenital heart disease | 143 (7) | 60 (10) |
| Neurologic impairment | 146 (7) | 11 (2) |
| Sepsis | 134 (7) | 10 (2) |
| Airway and/or craniofacial anomaly | 130 (6) | 17 (3) |
| Indicationa, n (%) | ||
| Ventilation failure | 759 (38) | 87 (15) |
| Oxygen failure | 629 (31) | 121 (20) |
| Frequent apnea and bradycardia events | 397 (20) | 28 (5) |
| Surfactant administration | 363 (18) | 168 (28) |
| Reintubation after unplanned extubation | 252 (13) | 4 (1) |
| Procedure | 214 (11) | 3 (1) |
| Upper airway obstruction | 110 (5) | 4 (1) |
| Unstable hemodynamics | 40 (2) | 12 (2) |
| DR, clinical indication | N/A | 367 (61) |
| DR, routine practice for diagnosis | N/A | 119 (20) |
IQR, interquartile range; N/A, not applicable.
More than 1 diagnosis and indication could be reported per patient. Diagnoses and indications occurring in <1% of population are not reported.
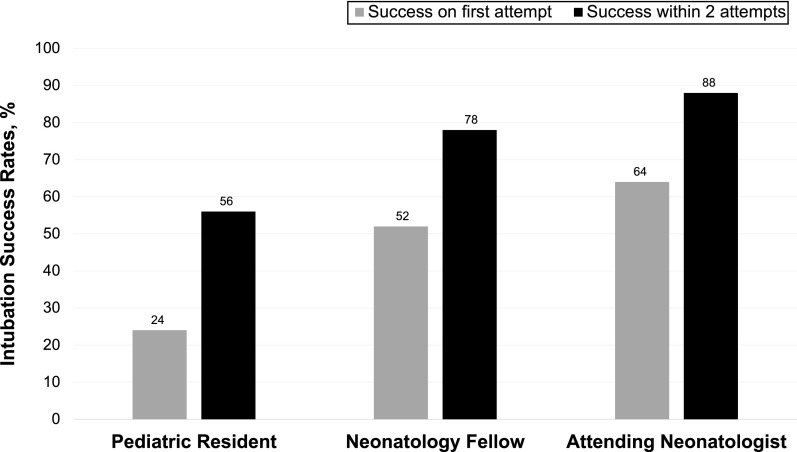
The training level of the first airway provider was significantly associated with first attempt intubation success (P < .001) and success within 2 intubation attempts (P < .001) (Fig 1). In the NICU setting, the most common first airway providers were advanced practice practitioners (38%), neonatal fellows (30%), and pediatric residents (15%) (Table 2). A conventional laryngoscope was used in 79% of TIs, and 36% of TIs were performed without any sedation or paralysis premedication. The first intubation attempt was successful in 49% of NICU intubations (Table 3). In the DR, neonatal fellows were the most common airway providers (49%) followed by advanced practice practitioners (36%) (Table 2). Pediatric residents were the first airway provider in only 2% of DR TIs. A conventional laryngoscope was used in 88% of TIs, and 86% of intubations were performed without any premedication. In the DR, 46% of intubations were successfully performed on the first attempt (Table 3).
FIGURE 1.
Neonatal intubation success by provider level. Neonatal intubation success rates on the first attempt and within 2 attempts for the same provider, based on training level of physician providers, are shown. Provider level was significantly associated with first attempt success (P < .001) and success within 2 attempts for the first airway provider (P < .001).
TABLE 2.
Provider and Practice Characteristics of Intubations
| Characteristic | NICU Intubations (N = 2009) | DR Intubations (N = 598) |
|---|---|---|
| First provider, n (%) | ||
| Neontatal fellow | 609 (30) | 295 (49) |
| Advanced practice provider (NP, PA, hospitalist) | 766 (38) | 213 (36) |
| Pediatric resident | 299 (15) | 10 (2) |
| Attending neonatologist | 140 (7) | 29 (5) |
| Respiratory therapist | 44 (2) | 3 (1) |
| Other | 151 (8) | 48 (8) |
| First device used, n (%) | ||
| Conventional laryngoscope | 1583 (79) | 527 (88) |
| Video laryngoscope | 415 (21) | 68 (11) |
| Othera | 11 (1) | 3 (1) |
| Premedications, n (%) | ||
| Sedation plus paralysis | 936 (47) | 61 (10) |
| No sedation or paralysis | 725 (36) | 514 (86) |
| Sedation only | 348 (17) | 23 (4) |
| Approach, n (%) | ||
| Oral | 1876 (93) | 592 (99) |
| Nasal | 121 (6) | 6 (1) |
| Other | 12 (1) | 0 |
IQR, interquartile range; NP, nurse practitioner; PA, physician assistant.
Other devices: laryngeal mask airway, fiber optic flexible bronchoscopy.
TABLE 3.
Intubation Outcomes in the NICU and DR Setting
| Outcome | NICU Intubations (N = 2009) | DR Intubations (N = 598) |
|---|---|---|
| First attempt success | 987 (49%) | 278 (46%) |
| Course success | 1920 (96%) | 567 (95%) |
| No. attempts (if course successful), median (IQR) | 1 (1–3) | 2 (1–2) |
| Any TIAE | 361 (18%) | 103 (17%) |
| Severe TIAE | 87 (4%) | 27 (5%) |
| Severe oxygen desaturationa | 938 (48%) | 134 (31%) |
IQR, interquartile range.
Reported for 1950 NICU encounters and 426 DR encounters with documented preintubation Spo2.
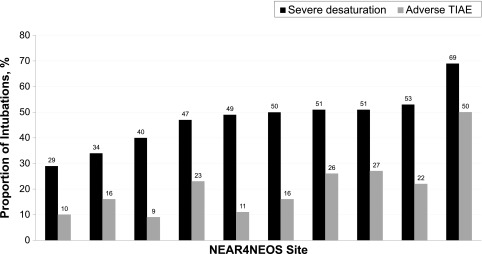
Severe oxygen desaturations were common, occurring in 938 of 1950 (48%) NICU TIs and 134 of 426 (31%) DR intubations with a recorded preintubation Spo2. At least 1 adverse TIAE occurred in 18% of NICU TIs and 17% of DR TIs (Table 3). The most common nonsevere adverse TIAEs in both settings were esophageal intubation with immediate recognition, dysrhythmia, and mainstem bronchial intubation (Table 4). Severe TIAEs were reported in 4% of NICU TIs and 5% of DR TIs. The most common severe TIAEs were esophageal intubation with delayed recognition, cardiac compressions lasting <1 minute, and laryngospasm (Table 4). Center-level adverse event rates during NICU TIs are shown in Fig 2. There was statistically significant variability in the occurrence of adverse events across centers. Severe oxygen desaturation rates ranged from 29% to 69% of TIs (P = .001), whereas adverse TIAE rates ranged from 9% to 50% (P < .001).
TABLE 4.
Number of Types of Observed Adverse TIAEs
| TIAE | NICU Intubations (N = 2009) | DR Intubations (N = 598) |
|---|---|---|
| Severe TIAE, n (%) | ||
| Esophageal intubation, delayed recognition | 20 (1) | 7 (1) |
| Cardiac compressions <1 min | 16 (1) | 8 (1) |
| Laryngospasm | 14 (1) | 1 (<1) |
| Cardiac arrest, patient survived | 8 (<1) | 1 (<1) |
| Emesis with aspiration | 8 (<1) | 0 |
| Pneumothorax and/or pneumomediastinum | 6 (<1) | 2 (<1) |
| Direct airway injury | 5 (<1) | 2 (<1) |
| Hypotension requiring intervention | 3 (<1) | 1 (<1) |
| Cardiac arrest, patient died | 2 (<1) | 2 (<1) |
| Nonsevere TIAE, n (%) | ||
| Esophageal intubation, immediate recognition | 187 (9) | 73 (12) |
| Dysrthythmiaa | 78 (4) | 16 (3) |
| Mainstem intubation | 35 (2) | 4 (1) |
| Gum or dental trauma | 18 (1) | 4 (1) |
| Emesis without aspiration | 20 (1) | 0 |
| Pain and/or agitation requiring additional medication and causing delay in intubation | 11 (1) | 0 |
| Epistaxis | 4 (<1) | 1 (<1) |
| Lip trauma | 3 (<1) | 3 (1) |
Includes heart rate <60 beats per minute without chest compressions.
FIGURE 2.
Site-specific adverse events during intubation in the NICU. Sites are rank-ordered according to severe oxygen desaturation rate. Severe oxygen desaturation rates ranged from 29% to 69% (P = .001), and adverse TIAE rates ranged from 9% to 50% (P < .001).
Results from the univariable analysis of characteristics associated with adverse TIAEs and severe desaturations in the NICU are shown in Table 5. Of note, the proportion of infants with an airway and/or craniofacial anomaly did not significantly differ between infants with and without TIAEs or severe oxygen desaturations (data not shown). Factors associated with adverse TIAEs and severe oxygen desaturations in the DR are presented in Table 6. Because premedication and video laryngoscopy were routinely used in the DR at only 1 participating site, these factors were not examined.
TABLE 5.
Univariable Analysis of Patient, Provider, and Practice Characteristics and Adverse Events During Intubations Performed in the NICU
| Factor | TIAEs | Severe Desaturations | ||||
|---|---|---|---|---|---|---|
| Any TIAE (n = 361) | No TIAE (n = 1648) | P | Severe Desaturation (n = 938) | No Severe Desaturation (n = 1012) | P | |
| Patient current wt, g, median (IQR) | 1300 (782–2595) | 1940 (1000–3100) | <.001 | 1600 (900–3000) | 1925 (1034–3050) | .01 |
| Gestational age at birth, wk, median (IQR) | 27 (25–32) | 29 (25–35) | <.001 | 28 (25–34) | 30 (26–36) | <.001 |
| Patient postnatal age, d, median (IQR) | 13 (1–42) | 13 (1–50) | .35 | 20 (2–56) | 6 (1–44) | <.001 |
| Indication, n (%) | ||||||
| Ventilation failure | 134 (37) | 625 (38) | .78 | 358 (38) | 390 (39) | .87 |
| Oxygen failure | 114 (32) | 515 (31) | .90 | 307 (33) | 311 (31) | .34 |
| Frequent apnea and bradycardia events | 95 (26) | 302 (18) | .001 | 206 (22) | 176 (17) | .01 |
| Surfactant administration | 70 (19) | 293 (18) | .47 | 142 (15) | 209 (21) | .002 |
| Reintubation after unplanned extubation | 48 (13) | 204 (12) | .63 | 129 (14) | 115 (11) | .11 |
| Upper airway obstruction | 26 (7) | 84 (5) | .11 | 59 (6) | 48 (5) | .13 |
| Procedure | 17 (5) | 197 (12) | <.001 | 87 (9) | 120 (12) | .06 |
| Unstable hemodynamics | 14 (4) | 26 (2) | .005 | 19 (2) | 18 (2) | .69 |
| First providera | ||||||
| Pediatric resident | 60 of 187 (32%) | 239 of 861 (28%) | .47 | 169 of 509 (33%) | 126 of 513 (25%) | .003 |
| NICU fellow | 102 of 187 (55%) | 507 of 861 (59%) | 269 of 509 (53%) | 323 of 513 (63%) | ||
| NICU attending | 25 of 187 (13%) | 115 of 861 (13%) | 71 of 509 (14%) | 64 of 513 (12%) | ||
| Video laryngoscopeb | 26 of 192 (14%) | 387 of 990 (39%) | <.001 | 192 of 573 (34%) | 214 of 593 (36%) | .36 |
| Sedative premedication | 198 (55%) | 1086 (66%) | <.001 | 634 (68%) | 632 (62%) | .02 |
| Paralytic premedicationc | 95 of 341 (28%) | 850 of 1589 (53%) | <.001 | 430 of 904 (48%) | 503 of 969 (52%) | .06 |
| No. attempts, median (IQR) | 3 (2–4) | 1 (1–2) | <.001 | 2 (1–3) | 1 (1–2) | <.001 |
IQR, interquartile range.
First provider analysis only includes intubations with resident, fellow, or attending providers.
Video laryngoscope analysis only includes sites that report any video laryngoscope use.
Analysis of paralytic medication only includes sites that reported any paralytic use.
TABLE 6.
Univariable Analysis of Patient, Provider, and Practice Characteristics and Adverse Events During Intubations Performed in the DR
| Factor | TIAE | Severe Desaturations | ||||
|---|---|---|---|---|---|---|
| Any TIAE (n = 103) | No TIAE (n = 495) | P | Severe Desaturation (n = 134) | No Severe Desaturation (n = 292) | P | |
| Patient current wt, g, median (IQR) | 1040 (680–2700) | 1630 (820–3000) | .001 | 1060 (700–2155) | 1610 (800–3000) | .001 |
| Gestational age at birth, wk, median (IQR) | 27 (25–36) | 31 (26–37) | .002 | 28 (25–34) | 31 (26–37) | <.001 |
| Indicationa, n (%) | ||||||
| DR, clinical indication | 74 (72) | 293 (59) | .02 | 90 (67) | 173 (59) | .12 |
| DR, routine practice for diagnosis | 15 (15) | 104 (21) | .14 | 13 (10) | 57 (20) | .01 |
| Surfactant administration | 33 (32) | 135 (27) | .33 | 55 (41) | 87 (30) | .02 |
| Oxygen failure | 21 (20) | 100 (20) | .97 | 34 (25) | 60 (21) | .27 |
| Ventilation failure | 13 (13) | 74 (15) | .54 | 21 (16) | 46 (16) | .98 |
| Frequent apnea and bradycardia events | 6 (6) | 22 (4) | .55 | 11 (8) | 12 (4) | .08 |
| Unstable hemodynamics | 4 (4) | 8 (2) | .14 | 2 (1) | 1 (<1) | .23 |
| First providerb | ||||||
| Pediatric resident | 2 of 58 (3%) | 8 of 276 (3%) | .82 | 3 of 65 (5%) | 6 of 163 (4%) | .84 |
| NICU fellow | 52 of 58 (90%) | 243 of 276 (88%) | 57 of 65 (88%) | 141 of 163 (87%) | ||
| NICU attending | 4 of 58 (7%) | 25 of 276 (9%) | 5 of 65 (8%) | 16 of 163 (10%) | ||
| No. attempts, median (IQR) | 2 (2–3) | 1 (1–2) | <.001 | 2 (1–3) | 1 (1–2) | <.001 |
IQR, interquartile range.
Only indications occurring in >1% of population presented.
First provider analysis only includes intubations with resident, fellow, or attending providers.
In multivariable analysis, characteristics that were independently associated with adverse TIAEs in the NICU were procedural indication of unstable hemodynamics (adjusted odds ratio [aOR] 3.85, 95% confidence interval [CI] 1.59–9.35) and increased number of intubation attempts (aOR 1.87, 95% CI 1.63–2.14). Factors associated with lower odds of adverse events included use of video laryngoscope (aOR 0.46, 95% CI 0.28–0.73) and paralytic premedication (aOR 0.38, 95% CI 0.25–0.57) (Supplemental Table 8). In a multivariable analysis, factors independently associated with severe desaturations in the NICU included sedative premedication (aOR 1.49, 95% CI 1.09–2.04), attending level provider (compared with neonatal fellow; aOR 1.99, 95% CI 1.29–3.07), and number of attempts (aOR 2.10, 95% CI 1.81–2.43) (Supplemental Table 9).
Discussion
This is the first multicenter report from a novel NEAR4NEOS airway registry. We successfully developed and implemented this registry to characterize the patients, providers, practices, and outcomes of neonatal intubation across 10 NICUs in an international setting. In this multisite study of academic centers, pediatric residents were rarely involved in neonatal TI in either the NICU or DR setting. At least 95% of initial TI courses across the NICU and DR were successful, but ≥1 adverse TIAE occurred in 18% of NICU and 17% of DR TIs. In addition, almost half of NICU TIs were complicated by severe oxygen desaturations. In an exploratory analysis, we identified modifiable factors that were independently associated with adverse TIAEs and severe oxygen desaturations during intubations in the NICU.
Despite the fact that all of the participating sites have a pediatric residency program, neonatal fellows and advanced practice providers were the first airway providers for the majority of neonatal TIs in both the NICU and DR setting. Residents were the first airway provider in only 15% of NICU TIs, which is comparable with resident participation rates of 15% to 38% documented in other contemporary reports.10,11,20,21 Surprisingly, pediatric residents attempted just 2% of DR TIs in our study, which is far lower than resident participation rates in DR intubations reported in previous studies.6,8,22
Many authors have observed a decline in opportunities for residents to intubate in both the neonatal and pediatric population.10,23,24 In a single-site study, Leone et al7 found that the mean number of intubation attempts throughout training per resident declined from 38 to 12 over an 8-year period ending in 2002. One explanation for this decline is resident duty hour limitations and an increased reliance on nontrainee practitioners, such as hospitalists and nurse practitioners, to staff NICUs.25,26 In addition, neonatal TI is less commonly performed because of significant practice changes over the last decade. Intubation and tracheal aspiration are no longer recommended for infants born through meconium-stained amniotic fluid,13 and noninvasive respiratory support is now prioritized for preterm infants.14 Given these changes, it is unlikely that most pediatric residents will acquire enough procedural exposure to become competent in neonatal intubation during their residency training.27 Therefore, it may be prudent for some programs to preferentially offer neonatal intubation opportunities to trainees who will need this skill in their future practice, such as pediatric residents who will be responsible for attending DR resuscitations after graduation and neonatal fellows who have not reached procedural competence.
Similar to other studies, we found that increasing training level among physician providers was associated with both increased first attempt success rates and success within 2 attempts for the first airway provider. To date, little has been published about attending neonatologists’ intubation performance. Haubner et al20 reported attending intubation success rates of 50% on the first attempt and 72% overall (number of attempts not quantified). However, attending physicians attempted only 22 intubations in that cohort, making it difficult to generate broad conclusions from those data. We found higher success rates for attending physicians in our study; attending neonatologists successfully performed 64% of intubations on the first attempt and 88% within 2 attempts.
At least 1 TIAE occurred in 18% (NICU) and 17% (DR) of TIs, with a severe TIAE rate of 5% (NICU) and 6% (DR) during intubation. These results are similar to those reported from multiple PICUs in NEAR4KIDS, where TIAES occurred in 20% and severe TIAEs occurred in 6% of pediatric TIs.2 Few previous studies have contained comprehensive reports on adverse events during neonatal TI. Using NEAR4KIDS operational definitions, Foglia et al11 found that TIAEs occurred in 22% of 701 intubations in a single level 4 NICU. Using different definitions, Hatch et al12 reported an adverse event rate of 39% in a single-site study of 162 infants. By using standardized operational definitions, an airway registry such as NEAR4NEOS will potentially make it easier to compare adverse events across studies in the future.
Consistent with the NEAR and NEAR4KIDS definitions,2,18 we collected oxygen saturation data separately from adverse TIAEs. We recorded both preintubation and lowest Spo2 values, which allowed us to define oxygen desaturation as a change from preintubation baseline, rather than using a preset Spo2 threshold. Severe oxygen desaturations occurred in almost half of NICU intubations and in one-third of DR intubations. Other authors have documented oxygen desaturation rates of 41% to 51% during neonatal TI.8,11 In a study of 5 academic NICUs, Haubner et al20 reported that physiologic instability, including oxygen desaturation, was the most common reason for unsuccessful intubation attempts. Oxygen desaturation therefore represents a target for quality improvement during neonatal intubation.
The NEAR4NEOS registry provides an opportunity for participating sites to benchmark TI safety outcomes across institutions. Similar to the NEAR4KIDS registry,4 we observed important variation in adverse TIAE rates among NEAR4NEOS sites. This variation may result from differences in patient characteristics between centers, but there may be differences in site-level practices that are associated with safety of neonatal intubation. This information will likely provide learning opportunities among participating sites in the future.
In multivariable analyses of NICU intubations, we found that video laryngoscopy and paralytic premedication were independently associated with reduced odds of adverse TIAEs but not severe desaturations. Similar to a single site report by Foglia et al,11 use of sedative premedication, captured separately from paralytic premedication, was not protective against TIAEs in the current study. In addition, we found that sedative premedication was independently associated with an increase in the odds of severe oxygen desaturation. These results suggest that paralytic use, when appropriate, is an important component of a procedural premedication regimen to improve the safety of neonatal intubation.
The authors of 2 recent randomized trials demonstrated that using video laryngoscopy to teach intubation improves neonatal TI success rates among pediatric trainees, but neither trial contained comprehensive reports on adverse events.28,29 In our study, esophageal intubation with immediate recognition was the most common adverse TIAE. We can speculate that video laryngoscopy may reduce esophageal intubation by allowing senior providers to use the video display to monitor and guide inexperienced providers through laryngoscopy and endotracheal tube insertion. Identification of these modifiable factors will inform future interventional projects aimed at reducing adverse TIAEs during neonatal TI.
We acknowledge limitations to our study. Intubation success and adverse event outcomes were all collected via self-report. We undertook extensive training at each site before initiating data collection, but it is possible that reporting bias exists. In addition, we did not collect data on the duration of intubation attempts, which may vary significantly across sites and may also be an important contributor to oxygen desaturations and adverse events. We only collected data on adverse events that took place during the immediate airway management period. Other authors have reported an association between increased number of intubation attempts and adverse neurologic outcomes.30,31 An additional modification has been made in the NEAR4NEOS database to track longer-term patient outcomes of neonatal intubation. Analyses of factors associated with TIAEs and severe desaturations were confined to NICU intubations. Some practice measures that are protective against TIAEs (such as paralytic premedication) may not be appropriate for use during DR intubation. Last, all of the participating NEAR4NEOS sites to date are academic centers; study results may not reflect practice and outcomes of neonatal TI in community-based NICUs.
Conclusions
We developed and implemented a large multisite registry of prospectively collected data on patient, provider, practice, and outcome characteristics of neonatal TI. Resident participation during neonatal TI, particularly in the DR, was lower than previously reported and may reflect a decreasing trend in this skill acquisition. Across all participants, the first intubation was successful in less than half of intubations in both the NICU and DR settings. We characterized the incidence of adverse TIAEs and severe desaturations during neonatal TI and identified potentially modifiable factors to reduce these events during NICU intubations. These findings will inform future educational and interventional studies to improve the success and safety of neonatal intubation.
Glossary
- aOR
adjusted odds ratio
- CI
confidence interval
- DR
delivery room
- NEAR
National Emergency Airway Registry
- NEAR4KIDS
National Emergency Airway Registry for Children
- NEAR4NEOS
National Emergency Airway Registry for Neonates
- Spo2
pulse oxygen saturation
- TI
tracheal intubation
- TIAE
tracheal intubation–associated event
Footnotes
Dr Foglia conceptualized and designed the study, analyzed the data, drafted the initial manuscript, and reviewed and revised the manuscript; Drs Ades, Sawyer, Glass, Singh, Jung, Quek, Johnston, Barry, Zenge, and Ms Napolitano conceptualized and designed the study, coordinated and supervised data collection, interpreted the data, and critically reviewed and revised the manuscript; Drs Kim, DeMeo, Moussa, Nadkarni, and Nishisaki conceptualized the study, designed the study collection instruments, interpreted the data, and critically reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Foglia is supported by a Eunice Kennedy Shriver National Institute of Child Health and Human Development Career Development Award K23HD084727. Dr Nishisaki and Ms Napolitano are supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development grants 1R21HD089151, AHRQ R18HS02264, and R18HS024511. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Sawyer T, Foglia E, Hatch LD, et al. Improving neonatal intubation safety: a journey of a thousand miles. J Neonatal Perinatal Med. 2017;10(2):125–131 [DOI] [PubMed] [Google Scholar]
- 2.Nishisaki A, Turner DA, Brown CA III, Walls RM, Nadkarni VM; National Emergency Airway Registry for Children (NEAR4KIDS); Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network . A National Emergency Airway Registry for Children: landscape of tracheal intubation in 15 PICUs. Crit Care Med. 2013;41(3):874–885 [DOI] [PubMed] [Google Scholar]
- 3.Sanders RC Jr, Giuliano JS Jr, Sullivan JE, et al. ; National Emergency Airway Registry for Children Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network . Level of trainee and tracheal intubation outcomes. Pediatrics. 2013;131(3). Available at: www.pediatrics.org/cgi/content/full/131/3/e821 [DOI] [PubMed] [Google Scholar]
- 4.Nett S, Emeriaud G, Jarvis JD, Montgomery V, Nadkarni VM, Nishisaki A; NEAR4KIDS Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network . Site-level variance for adverse tracheal intubation-associated events across 15 North American PICUs: a report from the National Emergency Airway Registry for Children*. Pediatr Crit Care Med. 2014;15(4):306–313 [DOI] [PubMed] [Google Scholar]
- 5.Falck AJ, Escobedo MB, Baillargeon JG, Villard LG, Gunkel JH. Proficiency of pediatric residents in performing neonatal endotracheal intubation. Pediatrics. 2003;112(6 pt 1):1242–1247 [DOI] [PubMed] [Google Scholar]
- 6.Lane B, Finer N, Rich W. Duration of intubation attempts during neonatal resuscitation. J Pediatr. 2004;145(1):67–70 [DOI] [PubMed] [Google Scholar]
- 7.Leone TA, Rich W, Finer NN. Neonatal intubation: success of pediatric trainees. J Pediatr. 2005;146(5):638–641 [DOI] [PubMed] [Google Scholar]
- 8.O’Donnell CPF, Kamlin COF, Davis PG, Morley CJ. Endotracheal intubation attempts during neonatal resuscitation: success rates, duration, and adverse effects. Pediatrics. 2006;117(1). Available at: www.pediatrics.org/cgi/content/full/117/1/e16 [DOI] [PubMed] [Google Scholar]
- 9.Bismilla Z, Finan E, McNamara PJ, LeBlanc V, Jefferies A, Whyte H. Failure of pediatric and neonatal trainees to meet Canadian Neonatal Resuscitation Program standards for neonatal intubation. J Perinatol. 2010;30(3):182–187 [DOI] [PubMed] [Google Scholar]
- 10.Downes KJ, Narendran V, Meinzen-Derr J, McClanahan S, Akinbi HT. The lost art of intubation: assessing opportunities for residents to perform neonatal intubation. J Perinatol. 2012;32(12):927–932 [DOI] [PubMed] [Google Scholar]
- 11.Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108(1):23–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hatch LD, Grubb PH, Lea AS, et al. Endotracheal intubation in neonates: a prospective study of adverse safety events in 162 infants. J Pediatr. 2016;168:62–66.e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wyckoff MH, Aziz K, Escobedo MB, et al. Part 13: neonatal resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 suppl 2):S543–S560 [DOI] [PubMed] [Google Scholar]
- 14.Committee on Fetus and Newborn; American Academy of Pediatrics . Respiratory support in preterm infants at birth. Pediatrics. 2014;133(1):171–174 [DOI] [PubMed] [Google Scholar]
- 15.Kumar P, Denson SE, Mancuso TJ; Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine . Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics. 2010;125(3):608–615 [DOI] [PubMed] [Google Scholar]
- 16.Barrington K. Premedication for endotracheal intubation in the newborn infant. Paediatr Child Health. 2011;16(3):159–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balaban O, Tobias JD. Videolaryngoscopy in neonates, infants, and children. Pediatr Crit Care Med. 2017;18(5):477–485 [DOI] [PubMed] [Google Scholar]
- 18.Walls RM, Brown CA III, Bair AE, Pallin DJ; NEAR II Investigators . Emergency airway management: a multi-center report of 8937 emergency department intubations. J Emerg Med. 2011;41(4):347–354 [DOI] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haubner LY, Barry JS, Johnston LC, et al. Neonatal intubation performance: room for improvement in tertiary neonatal intensive care units. Resuscitation. 2013;84(10):1359–1364 [DOI] [PubMed] [Google Scholar]
- 21.Hatch LD, Grubb PH, Lea AS, et al. Interventions to improve patient safety during intubation in the neonatal intensive care unit. Pediatrics. 2016;138(4):e20160069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kamlin COF, O’Connell LAF, Morley CJ, et al. A randomized trial of stylets for intubating newborn infants. Pediatrics. 2013;131(1). Available at: www.pediatrics.org/cgi/content/full/131/1/e198 [DOI] [PubMed] [Google Scholar]
- 23.Gozzo YF, Cummings CL, Chapman RL, Bizzarro MJ, Mercurio MR. Who is performing medical procedures in the neonatal intensive care unit? J Perinatol. 2011;31(3):206–211 [DOI] [PubMed] [Google Scholar]
- 24.Gabrani A, Kojima T, Sanders RC Jr, et al. ; National Emergency Airway Registry for Children (NEAR4KIDS) Collaborators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) . Downward trend in pediatric resident laryngoscopy participation in PICUs. Pediatr Crit Care Med. 2018;19(5):e242–e250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee HC, Rhee CJ, Sectish TC, Hintz SR. Changes in attendance at deliveries by pediatric residents 2000 to 2005. Am J Perinatol. 2009;26(2):129–134 [DOI] [PubMed] [Google Scholar]
- 26.Freed GL, Dunham KM, Moran LM, Spera L; Research Advisory Committee of the American Board of Pediatrics . Resident work hour changes in children’s hospitals: impact on staffing patterns and workforce needs. Pediatrics. 2012;130(4):700–704 [DOI] [PubMed] [Google Scholar]
- 27.DeMeo SD, Katakam L, Goldberg RN, Tanaka D. Predicting neonatal intubation competency in trainees. Pediatrics. 2015;135(5). Available at: www.pediatrics.org/cgi/content/full/135/5/e1229 [DOI] [PubMed] [Google Scholar]
- 28.O’Shea JE, Thio M, Kamlin CO, et al. Videolaryngoscopy to teach neonatal intubation: a randomized trial. Pediatrics. 2015;136(5):912–919 [DOI] [PubMed] [Google Scholar]
- 29.Moussa A, Luangxay Y, Tremblay S, et al. Videolaryngoscope for teaching neonatal endotracheal intubation: a randomized controlled trial. Pediatrics. 2016;137(3):e20152156. [DOI] [PubMed] [Google Scholar]
- 30.Wallenstein MB, Birnie KL, Arain YH, et al. Failed endotracheal intubation and adverse outcomes among extremely low birth weight infants. J Perinatol. 2016;36(2):112–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sauer CW, Kong JY, Vaucher YE, et al. Intubation attempts increase the risk for severe intraventricular hemorrhage in preterm infants-a retrospective cohort study. J Pediatr. 2016;177:108–113 [DOI] [PubMed] [Google Scholar]