Legislation to raise uptake of HPV vaccination among adolescents was not associated with increases in risky sexual behavior in this quasi-experimental study.
Abstract
BACKGROUND:
Despite preventive health benefits of the human papillomavirus (HPV) vaccination, uptake in the United States remains low. Twenty-four states have enacted legislation regarding HPV vaccination and education. One reason these policies have been controversial is because of concerns that they encourage risky adolescent sexual behaviors. Our aim in this study is to determine if state HPV legislation is associated with changes in adolescent sexual behaviors.
METHODS:
This is a difference-in-difference study in which we use data on adolescent sexual behaviors from the school-based state Youth Risk Behavior Surveillance System from 2001 to 2015. Sexual behaviors included ever having sexual intercourse in the last 3 months and condom use during last sexual intercourse. We compared changes in sexual behaviors among high school students before and after HPV legislation to changes among high school students in states without legislation.
RESULTS:
A total of 715 338 participants reported ever having sexual intercourse in the last 3 months, and 217 077 sexually active participants reported recent condom use. We found no substantive or statistically significant associations between HPV legislation and adolescent sexual behaviors. Recent sexual intercourse decreased by 0.90 percentage points (P = .21), and recent condom use increased by 0.96 percentage points (P = .32) among adolescents in states that enacted legislation compared with states that did not. Results were robust to a number of sensitivity analyses.
CONCLUSIONS:
Implementation of HPV legislation was not associated with changes in adolescent sexual behaviors in the United States. Concern that legislation will increase risky adolescent sexual behaviors should not be used when deciding to pass HPV legislation.
What’s Known on This Subject:
Despite preventive health benefits of human papillomavirus vaccination, uptake in the United States remains low. Twenty-four states have enacted legislation to raise vaccine uptake via financial incentives and school-based education. However, 1 concern is that these policies may encourage risky sexual behaviors.
What This Study Adds:
Enacting legislation regarding human papillomavirus was not associated with changes in recent sexual intercourse or condom use during last sexual intercourse in United States adolescents.
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States.1 Persistent infection with a high-risk strain can lead to serious health problems including cervical, anal, penile, vaginal, vulvar, and oropharyngeal cancers as well as genital warts in both men and women.2 Currently, there are 3 US Food and Drug Administration–approved HPV vaccines, for which multiple doses are recommended.3–5 The Centers for Disease Control and Prevention has recommended routine HPV vaccination for girls ages 11 to 12 since 2006 and for boys ages 11 to 12 since 2009, with catch-up vaccination for older adolescents and young adults.6,7 However, despite the availability of the vaccines, uptake remains low, with only 49.5% of girls and 37.5% of boys having up-to-date HPV vaccinations in 2016.8
Many reasons for the low uptake of the HPV vaccine have been proposed, including high costs and poor access, difficulty completing the multidose regimen, safety and health concerns, and worries that the vaccine will promote unsafe sexual activity among adolescents.9–12 Currently, 23 states and the District of Columbia have successfully passed legislation regarding HPV to help improve HPV vaccination coverage.13 These policies vary in terms of leniency and include requiring schools to provide information about HPV vaccination to students, subsidizing costs and incentivizing insurers to cover the vaccine, and mandating vaccination (Supplemental Table 4).13 Further adoption of these policies has been hampered by a number of concerns.13,14 One concern is that encouraging adoption of the HPV vaccination may encourage risky sexual behaviors among adolescents, and it may be seen as conflicting with abstinence only sexual education.14–17 Consequently, many states have had to defer vaccination mandates and instead pass related legislation focusing on HPV education or cost.17,18 Although in recent research no changes in sexually transmitted infections among privately insured individuals receiving the HPV vaccine have been found, the broader impacts of policies to increase vaccine uptake on sexual behaviors in the general adolescent population have not been examined.19 Rigorous evidence in this domain will be critical as policymakers continue to grapple with strategies to raise vaccination rates.
In this study, we examined the impact of state-level legislation aiming to raise awareness and uptake of HPV vaccination on adolescent sexual behaviors. We used a quasi-experimental difference-in-difference approach to assess how the policy is associated with the number of sexual partners and condom use during last sexual intercourse.20
Methods
Data on the outcomes of adolescent sexual behaviors were collected from the 2001 to 2015 state Youth Risk Behavior Surveillance System (YRBSS).21 The state YRBSS is a large, state-representative, biannual, school-based survey of ninth- to 12th-grade students from the United States. Underrepresented minorities were purposely oversampled at each stage of the 3-stage sampling procedure.22 The state YRBSS survey collected information from students in 25 states without HPV legislation and 16 states with HPV legislation (Supplemental Table 4). States could choose when they wanted to publicly report their results, so the coverage of states differed each year during our study period.
The YRBSS asked students to report if they ever had sexual intercourse in the last 3 months and if they used a condom the last time they had sexual intercourse. Ever having sexual intercourse during the last 3 months was a binary yes or no variable (0 for people who never had sex or did not have sex in the last 3 months, 1 for people who had sex during the last 3 months). Condom use during last sexual intercourse was a binary yes or no variable that was conditional on ever having had sex in the last 3 months. As a secondary outcome, we looked at the number of sexual partners during the last 3 months as a continuous variable from 0 (people who never had sex or did not have sex in last 3 months) to 6 (6 or more partners in the last 3 months).
The main exposure was whether respondents’ state of residence had legislation aiming to raise HPV vaccination rates in place during the year of the interview. Information on the type of policy and year of passage was obtained from the National Conference of State Legislatures (Supplemental Table 4).13 The exposure was then further categorized by the type of legislation that was passed: vaccination mandates, HPV education (in schools, for parents, general awareness, research funds), and vaccine cost and accessibility (cost of vaccine, insurance coverage, prescription requirements).
We used difference-in-difference models to study the association of the legislation with adolescent sexual behaviors.20 We compared changes in sexual behavior for adolescents living in states that passed HPV legislation before and after policy implementation against the same changes in states that did not pass legislation. In our model, we adjusted for respondent age, sex, race, and grade. To adjust for potential confounders for the association between the states with legislation and adolescent sexual health behaviors, we added state-year factors to the model, including state-specific linear time trends. In our models, we include state effects that account for any fixed differences between states (such as political, educational, or teen-aged pregnancy differences) and also include year effects that account for any trends in the risky teenager sexual behaviors over time that are similar across all states. As a secondary analysis, we also adjusted for rates of unemployment, teen-aged pregnancies, and sexually transmitted diseases among teenagers ages 15 to 19 as well as the Children’s Health Insurance Program (CHIP) and the Medicaid program of the states, the majority political party of the state legislature, and the political party of the governor. CHIP and Medicaid were included in case any changes to health care coverage for adolescents or vaccinations occurred around the same time that legislation was passed and could be acting as a confounder for the relationship between legislation and adolescent sexual behaviors. We estimated models, defining the exposure as passage of any policy as well as passage of specific types of legislation, including mandates, legislation about vaccine cost or access, and legislation about education. Because of the small number of states with mandates and the timing of the mandates, we were not able to examine the effect of the mandates separately and instead, they are only included in the any policy analysis.
Although our main outcomes were binary variables, we used ordinary least squares regression to estimate our models. This is because there are well-known biases in limited dependent variable estimators in fixed effect models.23 For all models, we corrected SEs for clustering at the state level to account for serial correlation in the outcome.24 Survey weights were used when examining the descriptive characteristics of states with legislation compared with states without legislation. Survey weights were not used in the difference-in-difference models because individual-level error terms clustered within a larger group (each state) could yield inappropriately inflated SEs.25 Additionally, we did not a priori expect large heterogeneous effects because the survey was not sampled by the outcome of interest.25 However, we still ran the main models using the survey weights to compare with our main models that did not include survey weights.
We estimated several additional models. First, we assessed potential violations of the parallel trends assumption of the difference-in-difference model.20 Specifically, we examined whether trends in sexual behavior before policy implementation differed in states passing policies versus those that did not. Second, we estimated our main models by subgroups of age, sex, grade, and race and/or ethnicity. Bonferroni corrections were used to account for multiple testing. With 18 main regressions run for the analysis, results were considered statistically significant when the P value was <.003. Third, because an assumption of this model is that the effects are immediate, we did a lagged analysis to see what happened when we looked at the effect of the legislation among students years after it was passed. The idea of the lag is that most HPV vaccination education and coverage should be affecting 11- to 12-year-olds, and our YRBSS data are taken from older students (mainly 15–18-year-olds), so looking at a lagged timing of legislation will let us see if the effect of the legislation was limited to kids who were age 11 to 12 at the time of the legislation. Additionally, in the lagged analysis, we also account for the fact that implementation of the legislation most often happened the year after the policy was passed. However, because states did not always report their data for every survey year, we do not have as many states reporting their data after 2011, and lagged results should be interpreted with caution. Fourth, as a prespecified falsification test, we also examined lead effects because the first HPV vaccine was approved in 2006.26 This study is exempt from human subjects review by the institutional review board given the use of publicly available, deidentified data.
Results
From 2001 to 2015, 886 981 high school students participated in the state YRBSS surveys. Of those respondents, 224 177 (25.3%) reported having sexual intercourse in the last 3 months, 491 161 (55.4%) reported that they did not have sexual intercourse in the last 3 months, and 171 643 (19.4%) did not respond to that question. A total of 715 338 high school students reported the number of sexual partners during the last 3 months (80.6% of all students participating), and 217 077 high school students who ever had sexual intercourse in the last 3 months reported condom use during last sexual intercourse in the YRBSS (96.8% of students who reported having sexual intercourse in the last 3 months). Students in states with HPV legislation were similar to students in states without HPV legislation in terms of sex, grade, race, smoking, and alcohol use before and after most states passed legislation in 2007 (Table 1). The average age of students in states with legislation was 16.0 years old, and the average age of students in states without legislation was 16.1 years old. States with legislation and states without legislation had a similar percentage of students who ever had been taught about AIDS in school, with a greater percentage being taught about AIDS in school before 2007 (91.8%) than after 2007 (89.2%). The percentage of students ever having sexual intercourse in the last 3 months and the percentage of students reporting condom use during last sexual intercourse was similar for states with and without HPV legislation and decreased slightly from before 2007 to after 2007.
TABLE 1.
Characteristics of Students in States With HPV Legislation and States Without HPV Legislation Overall and by Prelegislation and Postlegislation Time Periods
| 2001–2015 | 2001–2005 | 2007–2015 | |||
|---|---|---|---|---|---|
| All States (n = 886 981), % | No Legislation (n = 122 164), % | HPV Legislation (n = 95 728), % | No Legislation (n = 282 363), % | HPV Legislation (n = 386 726), % | |
| Age, y | |||||
| ≤14 | 11.1 | 9.7 | 11.7 | 10.4 | 11.9 |
| 15 | 25.7 | 26.3 | 26.5 | 25.2 | 25.6 |
| 16 | 25.8 | 26.2 | 25.7 | 25.8 | 25.7 |
| 17 | 23.3 | 22.7 | 22.3 | 23.9 | 23.3 |
| 18 | 14.2 | 15.1 | 13.9 | 14.8 | 13.4 |
| Sex | |||||
| Male | 50.8 | 50.8 | 50.7 | 50.9 | 50.8 |
| Female | 49.2 | 49.3 | 49.3 | 49.2 | 49.2 |
| Grade | |||||
| 9 | 28.7 | 30.4 | 30.2 | 27.8 | 28.2 |
| 10 | 25.8 | 25.8 | 26.0 | 25.9 | 25.8 |
| 11 | 23.5 | 23.0 | 22.9 | 23.8 | 23.6 |
| 12 | 22.0 | 20.9 | 20.9 | 22.5 | 22.5 |
| Race | |||||
| White | 58.4 | 65.7 | 63.4 | 56.9 | 55.0 |
| African American or Hispanic or other | 41.6 | 34.3 | 36.6 | 43.1 | 45.0 |
| Smoking in last 3 mo | |||||
| Yes | 17.5 | 22.6 | 22.5 | 15.8 | 15.3 |
| No | 82.5 | 77.4 | 77.5 | 84.2 | 84.7 |
| Alcohol use in last 3 mo | |||||
| Yes | 38.5 | 43.5 | 43.8 | 35.6 | 36.8 |
| No | 61.5 | 56.5 | 56.2 | 64.4 | 63.2 |
| Taught about AIDS in school | |||||
| Yes | 90.1 | 91.9 | 91.8 | 89.3 | 89.1 |
| No | 9.9 | 8.1 | 8.2 | 10.7 | 10.9 |
| Condom use during last sexual intercourse | |||||
| Yes | 60.8 | 63.0 | 62.8 | 60.0 | 59.8 |
| No | 39.2 | 37.0 | 37.2 | 40.0 | 40.2 |
| Sexual intercourse in last 3 mo | |||||
| Yes | 33.3 | 35.2 | 33.7 | 33.0 | 32.7 |
| No | 66.7 | 64.8 | 66.3 | 67.0 | 67.4 |
Percentages are adjusted for survey weights; the question regarding being taught about AIDS in school is not available for states that participated in the 2015 sample (n = 461 218 for 2001–2015). Condom use is restricted to students who reported having sexual intercourse in the last 3 mo.
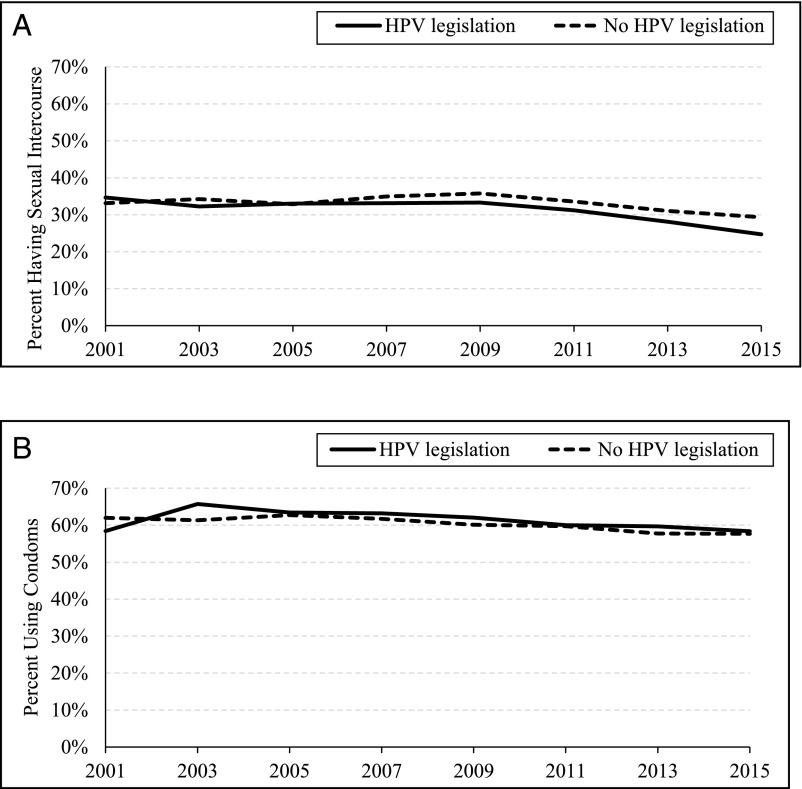
Difference-in-difference models revealed no substantive or statistically significant changes in recent sexual intercourse or condom use (Table 2). In Fig 1, we plot trends in adolescent sexual behaviors from 2001 to 2015, in which most legislation was enacted in 2007, and it reveals no difference in risky sexual behaviors in states with legislation compared with states without legislation. The difference-in-difference estimates were consistent with this. Students in states passing HPV legislation decreased recent sexual intercourse by 0.90 percentage points (95% confidence interval [CI]: −2.33 to 0.52) and increased condom use during last sexual encounter by 0.96 percentage points (95% CI: −0.97 to 2.89) compared with students in states without legislation. When the results were separated by the type of legislation, there continued to be no significant difference in sexual intercourse or condom use for states with HPV legislation compared with states without HPV legislation. For legislation regarding education, recent sexual intercourse decreased by 0.73 percentage points (95% CI: −2.20 to 0.74), and condom use decreased by 0.55 percentage points (95% CI: −4.49 to 3.39). For legislation regarding vaccination cost, recent sexual intercourse increased by 0.29 percentage points (95% CI: −1.96 to 2.54), and condom use increased by .63 percentage points (95% CI: −1.23 to 2.48).
TABLE 2.
Change in the Proportion of Sexual Behaviors in States With Legislation Compared With States Without Legislation
| Sexual Intercourse During the Last 3 Mo | Condom Use During Last Sexual Intercourse | |||||
|---|---|---|---|---|---|---|
| Percentage Point Change | (95% CI) | P | Percentage Point Change | (95% CI) | P | |
| Among all students | ||||||
| Any legislation | −0.90 | (−2.33 to 0.52) | .21 | 0.96 | (−0.97 to 2.89) | .32 |
| Legislation about vaccine cost and accessibility | 0.29 | (−1.96 to 2.54) | .80 | –0.55 | (−4.49 to 3.39) | .78 |
| Legislation about HPV education | −0.73 | (−2.20 to 0.74) | .32 | 0.63 | (−1.23 to 2.48) | .50 |
| Among different student populations (any legislation) | ||||||
| Sex | ||||||
| Male | −0.67 | (−2.47 to 1.14) | .46 | 0.047 | (−2.41 to 2.51) | .97 |
| Female | −1.11 | (−2.59 to 0.37) | .14 | 1.78 | (−0.82 to 4.37) | .18 |
| Age, y | ||||||
| <17 | −1.07 | (−2.49 to 0.34) | .13 | 1.64 | (−0.94 to 4.23) | .21 |
| 17 or 18 | −0.52 | (−2.67 to 1.64) | .63 | 0.44 | (−1.97 to 2.86) | .71 |
| Race and/or ethnicity | ||||||
| White | −0.96 | (−2.65 to 0.73) | .26 | 0.83 | (−1.59 to 3.25) | .49 |
| African American or Hispanic or other | −0.55 | (−2.28 to 1.18) | .52 | 2.06 | (−0.76 to 4.87) | .15 |
Each cell represents a separate regression with the dependent variables noted in the columns. For each dependent variable, the model includes survey year fixed effects, age, sex, and current grade fixed effects. Models include state-specific linear time trends and state fixed effects.
FIGURE 1.
Adolescent sexual behaviors over time in states with HPV legislation and states without HPV legislation. A, Sexual intercourse during the last 3 months. B, Condom use during last sexual intercourse. In A, we show the percentage of adolescents ever having sexual intercourse over the last 3 months for states that passed HPV legislation (solid black line) and states that did not pass HPV legislation (dashed black line). In B, we show the percentage of adolescents using condoms the last time they had sexual intercourse for states that passed HPV legislation (solid black line) and states that did not pass HPV legislation (dashed black line). Most states that passed HPV legislation did so in 2007. The first HPV vaccination was approved by the US Food and Drug Administration in 2006.
In additional analyses, we did not find evidence that the parallel trends assumption was violated (Supplemental Table 5). Subgroup analyses revealed some difference by age, sex, and ethnicity, but no group showed statistically significant increases in any sexual behaviors after the policy. It appeared that girls had larger decreases in recent sexual intercourse and had larger increases in condom use than boys. Students under age 17 had larger decreases in recent sexual intercourse and larger increases in condom use than students ages 17 or 18. There were no differences seen by race and/or ethnicity for the number of sexual partners. White students saw a smaller percentage point increase in condom use than African American, Hispanic, and other race and/or ethnicity students. There was no difference when CHIP, Medicaid, political party, unemployment, teen-aged pregnancy rates, and sexually transmitted disease rates were included in the models (Supplemental Table 6). Analyses in which we examined lagged impacts suggested a substantive, but not statistically significant, 6.1% point decrease (P = .009) in recent sexual intercourse and a 5.9% point increase (P = .046) in condom use (prespecified P value threshold of P < .003) (Supplemental Table 7). Results did not differ for the secondary outcome examined of number of sexual partners during the last 3 months. For the secondary outcome of number of sexual partners in the last 3 months, there was a nonsignificant decrease in the number of sexual partners by 0.02 (P = .18) in states that enacted HPV legislation compared with states that did not enact HPV legislation (Table 3). Lastly, as expected, the estimates from models in which we included the YRBSS sample weights were less precisely estimated, but the interpretation of the main effects was similar (Supplemental Table 8).
TABLE 3.
Change in the Average Number of Sexual Partners in the Last 3 Months in States With Legislation Compared With States Without Legislation
| No. Sexual Partners in Last 3 Mo | |||
|---|---|---|---|
| Average No. Change | (95% CI) | P | |
| Among all students | |||
| Any legislation | −0.020 | (−0.050 to 0.010) | .18 |
| Legislation about vaccine cost and accessibility | −0.016 | (−0.066 to 0.035) | .54 |
| Legislation about HPV education | 0.0097 | (−0.042 to 0.022) | .54 |
| Among different student populations (any legislation) | |||
| Sex | |||
| Male | −0.032 | (−0.080 to 0.016) | .18 |
| Female | −0.0096 | (−0.030 to 0.011) | .35 |
| Age, y | |||
| <17 | −0.022 | (−0.052 to 0.0082) | .15 |
| 17 or 18 | −0.013 | (−0.056 to 0.030) | .55 |
| Race and/or ethnicity | |||
| White | −0.013 | (−0.047 to 0.022) | .47 |
| African American or Hispanic or other | −0.025 | (−0.065 to 0.016) | .22 |
Each cell represents a separate regression with the dependent variables noted in the columns. For each dependent variable, the model includes survey year fixed effects, age, sex, and current grade fixed effects. Models include state-specific linear time trends and state fixed effects.
Discussion
In this national study, we found no association between the passage of legislation designed to increase uptake of the HPV vaccine and sexual behaviors among high school–going adolescents in the United States. This finding was consistent across subgroups and robust to different specifications and sensitivity tests.
Despite long-standing knowledge of the protective benefits of the HPV vaccine, vaccination rates in the United States remain low.27 Even among those receiving the vaccine, the timing of HPV vaccination often occurs after sexual debut and HPV exposure, reducing its potential efficacy. A study conducted in the NHANES found that 43% of girls with at least 1 dose of the HPV vaccine had sex before or during the same year as their first HPV vaccination.28 Ensuring that adolescents receive the HPV vaccination before their first sexual experience is important to helping prevent the negative health effects of HPV infections. Policies to educate adolescents and their families about the benefits of vaccination and increase access will likely be an important part of the policy response to improve vaccination rates.
Thus far, researchers have found minimal, if any, benefits of these policies on vaccination rates.29–32 In states that have implemented these policies, the ultimate legislation passed was often less expansive than other debated options. The less-expansive options passed included additions such as opt-out options for vaccine mandates that may have reduced the number of adolescents vaccinated and weakening of the policy to just be educational.29 The weakening of the legislation was in part due to concerns about behavioral responses to the policy in addition to a number of other concerns around ethics, health benefits, and side effects.14–16 In our study, we show that the policy options implemented thus far have not raised the risk of risky sexual activity. Additionally, adolescents appear to be engaged in less sexual intercourse over time, even with increasing availability of HPV vaccination. The percentage of adolescents that have ever had sex, that had sex before age 13, and that had sex with 4 or more people has decreased from 1991 to 2015, and adolescent pregnancy rates have dropped from 1990 to 2014.33,34 However, we found that condom use during last sexual intercourse appeared to decrease slightly from 2001 to 2015. Our findings and this broader context both can be used to support calls to adopt stronger vaccination education and access policies.
This study is subject to a number of limitations. First, we considered the effects of passage of HPV-related legislation, which may differ from the actual consequences of policy implementation. Second, similar policies in different states may have been implemented differently. Data on exact implementation were not available, and therefore we were not able to assess heterogeneity in policy effects across states. Third, we only examined legislative rulings regarding HPV vaccination. Many states may be providing HPV education and funding through state public health departments that do not require legislation. Nonlegislative HPV initiatives were not accounted for in our analysis because of the difficulty in finding these data. Fourth, any unobserved or omitted state-year confounders that are correlated with both the HPV legislation and the adolescent sexual behavior outcomes could bias our analysis. We attempted to adjust for these potential confounders in a variety of ways and conducted several sensitivity checks. However, we cannot fully rule out the possibility of residual bias.
Fifth, there are missing data on the number of sexual partners (19.4%) and condom use (3.2%), which may create a selection bias if students not reporting their sexual behaviors did so in a way that was also related to their state’s HPV legislation policy. For example, if students with riskier behaviors are less likely to report their behaviors on the survey, and they are more likely to live in states that passed HPV legislation, we may be worried about selection bias. However, it seems that teenagers’ reporting of their sexual behaviors may not be related to their state’s HPV legislation policy, so we are not strongly concerned about this bias. Sixth, we also do not have complete information on all states with HPV legislation policies in the YRBSS state survey sample, so with our results, although coming from a wide regional distribution in the United States, we should take into account that results may not be generalizable to states not included in the analysis.
Conclusions
HPV legislation does not appear to have a detrimental effect on adolescent sexual behaviors. This study, taken with the other studies in which researchers look at the impact of HPV vaccines on adolescent sexual behavior and the low vaccination rates in the United States, can be used to provide support for the reintroduction and strengthening of legislation regarding the HPV vaccine. Concern that legislation will increase risky adolescent sexual behaviors should not be used when deciding to pass legislation regarding HPV vaccination.
Glossary
- CHIP
Children’s Health Insurance Program
- CI
confidence interval
- HPV
human papillomavirus
- YRBSS
Youth Risk Behavior Surveillance System
Footnotes
Dr Cook conceptualized and designed the study, drafted the initial manuscript, ran the analysis, revised the manuscript, contributed to and supervised the analysis of the data, and had input on the design of the study; Dr Venkataramani conceptualized and designed the study, revised the manuscript, contributed to and supervised the analysis of the data, and had input on the design of the study; Drs Kim, Tamimi, and Holmes revised the manuscript, contributed to and supervised the analysis of the data, and had input on the design of the study; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grants R25 CA 98566-10, T32 CA 009001-40, and T32 ES 007069. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Satterwhite CL, Torrone E, Meites E, et al. . Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40(3):187–193 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Sexually Transmitted Disease Surveillance 2014. Atlanta, GA: US Department of Health and Human Services; 2015 [Google Scholar]
- 3.Food and Drug Administration June 8, 2006 Approval Letter - Human Papillomavirus Quadrivalent (Types 6, 11, 16, 18) Vaccine, Recombinant. Rockville, MD: Department of Health and Human Services; 2006. Available at: http://wayback.archive-it.org/7993/20170722145339/https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm111283.htm. Accessed July 7, 2018 [Google Scholar]
- 4.Food and Drug Administration October 16, 2009 Approval Letter - Cervarix. Rockville, MD: Department of Health and Human Services; 2009. Available at: http://wayback.archive-it.org/7993/20170723025640/https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm186959.htm. Accessed July 7, 2018 [Google Scholar]
- 5.Food and Drug Administration December 10, 2014 Approval Letter - GARDASIL 9. Rockville, MD: Department of Health and Human Services; 2014. Available at: https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm426520.htm. Accessed July 7, 2018 [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59(20):630–632 [PubMed] [Google Scholar]
- 7.Markowitz LE, Dunne EF, Saraiya M, et al. ; Centers for Disease Control and Prevention (CDC) . Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP) [published correction appears in MMWR Recomm Rep. 2014;63(49):1182]. MMWR Recomm Rep. 2014;63(RR–05):1–30 [PubMed] [Google Scholar]
- 8.Walker TY, Elam-Evans LD, Singleton JA, et al. . National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(33):874–882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liddon NC, Hood JE, Leichliter JS. Intent to receive HPV vaccine and reasons for not vaccinating among unvaccinated adolescent and young women: findings from the 2006-2008 National Survey of Family Growth. Vaccine. 2012;30(16):2676–2682 [DOI] [PubMed] [Google Scholar]
- 10.Beavis AL, Levinson KL. Preventing cervical cancer in the United States: barriers and resolutions for HPV vaccination. Front Oncol. 2016;6:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haber G, Malow RM, Zimet GD. The HPV vaccine mandate controversy. J Pediatr Adolesc Gynecol. 2007;20(6):325–331 [DOI] [PubMed] [Google Scholar]
- 13.National Conference of State Legislatures HPV vaccine: state legislation and statutes. Available at: www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx. Accessed October 8, 2016
- 14.Casciotti DM, Smith KC, Andon L, Vernick J, Tsui A, Klassen AC. Print news coverage of school-based human papillomavirus vaccine mandates. J Sch Health. 2014;84(2):71–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charo RA. Politics, parents, and prophylaxis–mandating HPV vaccination in the United States. N Engl J Med. 2007;356(19):1905–1908 [DOI] [PubMed] [Google Scholar]
- 16.Vamos CA, McDermott RJ, Daley EM. The HPV vaccine: framing the arguments FOR and AGAINST mandatory vaccination of all middle school girls. J Sch Health. 2008;78(6):302–309 [DOI] [PubMed] [Google Scholar]
- 17.Colgrove J, Abiola S, Mello MM. HPV vaccination mandates–lawmaking amid political and scientific controversy. N Engl J Med. 2010;363(8):785–791 [DOI] [PubMed] [Google Scholar]
- 18.Gostin LO. Mandatory HPV vaccination and political debate. JAMA. 2011;306(15):1699–1700 [DOI] [PubMed] [Google Scholar]
- 19.Jena AB, Goldman DP, Seabury SA. Incidence of sexually transmitted infections after human papillomavirus vaccination among adolescent females. JAMA Intern Med. 2015;175(4):617–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2402 [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention Youth risk behavior survey questionnaire. 1991–2015. Available at: https://www.cdc.gov/healthyyouth/data/yrbs/questionnaires.htm. Accessed October 27, 2016
- 22.Brener ND, Kann L, Shanklin S, et al. ; Centers for Disease Control and Prevention (CDC) . Methodology of the Youth Risk Behavior Surveillance System–2013. MMWR Recomm Rep. 2013;62(RR-1):1–20 [PubMed] [Google Scholar]
- 23.Greene W. The behaviour of the maximum likelihood estimator of limited dependent variable models in the presence of fixed effects. Econom J. 2004;7(1):98–119 [Google Scholar]
- 24.Bertrand M, Duflo E, Mullainathan S. How much should we trust differences-in-differences estimates?*. Q J Econ. 2004;119(1):249–275 [Google Scholar]
- 25.Solon G, Haider SJ, Wooldridge JM. What are we weighting for? J Hum Resour. 2015;50(2):301–316 [Google Scholar]
- 26.Prasad V, Jena AB. Prespecified falsification end points: can they validate true observational associations? JAMA. 2013;309(3):241–242 [DOI] [PubMed] [Google Scholar]
- 27.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. . National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;850–858. Available at: https://www.cdc.gov/mmwr/volumes/65/wr/mm6533a4.htm. Accessed July 7, 2018 [DOI] [PubMed] [Google Scholar]
- 28.Petrosky EY, Liu G, Hariri S, Markowitz LE. Human papillomavirus vaccination and age at first sexual activity, National Health and Nutrition Examination Survey. Clin Pediatr (Phila). 2017;56(4):363–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perkins RB, Lin M, Wallington SF, Hanchate AD. Impact of school-entry and education mandates by states on HPV vaccination coverage: analysis of the 2009-2013 National Immunization Survey-Teen. Hum Vaccin Immunother. 2016;12(6):1615–1622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pierre-Victor D, Page TF, Trepka MJ, Stephens DP, Li T, Madhivanan P. Impact of Virginia’s school-entry vaccine mandate on human papillomavirus vaccination among 13-17-year-old females. J Womens Health (Larchmt). 2017;26(3):266–275 [DOI] [PubMed] [Google Scholar]
- 31.Cuff RD, Buchanan T, Pelkofski E, Korte J, Modesitt SP, Pierce JY. Rates of human papillomavirus vaccine uptake amongst girls five years after introduction of statewide mandate in Virginia. Am J Obstet Gynecol. 2016;214(6):752.e1–752.e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pierre-Victor D, Trepka MJ, Page TF, Li T, Stephens DP, Madhivanan P. Impact of Louisiana’s HPV vaccine awareness policy on HPV vaccination among 13- to 17-year-old females. Health Educ Behav. 2017;44(4):548–558 [DOI] [PubMed] [Google Scholar]
- 33.Kann L, McManus T, Harris WA, et al. . Youth risk behavior surveillance - United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174 [DOI] [PubMed] [Google Scholar]
- 34.Hamilton BE, Martin JA, Osterman MJK, Curtin SC, Mathews TJ. Births: Final Data for 2014. Hyattsville, MD: National Center for Health Statistics; 2015 [PubMed] [Google Scholar]