Abstract
Selenium (Se) is an essential micronutrient that has several important functions in animal and human health. The biological functions of Se are carried out by selenoproteins (encoded by twenty-five genes in human and twenty-four in mice), which are reportedly present in all three domains of life. As a component of selenoproteins, Se has structural and enzymatic functions; in the latter context it is best recognized for its catalytic and antioxidant activities. In this review, we highlight the biological functions of Se and selenoproteins followed by an elaborated review of the relationship between Se and female reproductive function. Data pertaining to Se status and female fertility and reproduction are sparse, with most such studies focusing on the role of Se in pregnancy. Only recently has some light been shed on its potential role in ovarian physiology. The exact underlying molecular and biochemical mechanisms through which Se or selenoproteins modulate female reproduction are largely unknown; their role in human pregnancy and related complications is not yet sufficiently understood. Properly powered, randomized, controlled trials (intervention vs. control) in populations of relatively low Se status will be essential to clarify their role. In the meantime, studies elucidating the potential effect of Se supplementation and selenoproteins (i.e., GPX1, SELENOP, and SELENOS) in ovarian function and overall female reproductive efficiency would be of great value.
Keywords: female reproduction, fertility, GPX1, infertility, ovarian function, oxidative stress, pre-eclampsia, selenium, selenoproteins
1. Introduction
Selenium (Se) is known as an essential trace mineral that has several important functions at the level of the cell and organism in animal and human health, and therefore it is relevant to various patho-physiological conditions [1]. The biological functions of Se are primarily carried out by selenoproteins (selenium-containing proteins, products of twenty-five genes in human and twenty-four in mouse), which are reportedly demonstrated in all three realms of life, viz. eukaryotes, archaea, and eubacteria, and they were also observed in viruses [2,3,4]. As a component of selenoproteins, Se plays structural and enzymatic roles; in the latter context it is best recognized for its catalytic and antioxidant activities [1].
Among identified mammalian selenoproteins, only a few have hitherto been functionally characterized [4]. Albeit selenoproteins represent various molecular pathways and perform a variety of essential biological functions; they all contain at least one selenocysteine (Sec), a Se containing amino acid (The 21st naturally occurring “proteinogenic” amino acid, as it is inserted into proteins during biosynthesis, in contrast to post-translationally modified amino acids [3,5]), and the majority of them perform oxido-reductase roles [4,6]. Important cellular processes, including synthesis of desoxynucleotides for deoxyribonucleic acid (DNA), scavenging of detrimental signaling peroxides, reduction of oxidized proteins and membranes, redox signaling control, metabolism of thyroid hormones, protein folding and Se transportation and storage, are thus far reported to depend on selenoproteins [4]. The brief descriptions of select mammalian selenoproteins having relevance to fertility, reproduction, and development are summarized in Table 1.
Table 1.
Brief description of select mammalian selenoproteins having implication/role in fertility, reproduction, and development.
| Selenoprotein | Symbol [5] | General Description/Function [1,6,7] | Potential Implication in Reproductive Function |
|---|---|---|---|
| Glutathione peroxidase 1 | GPX1 | Antioxidant protection | Important role in female reproductive function; i.e., implication in determining the follicle growth, maturation, and dominance in both cows and women [8,9]. Implication in the follicular microenvironment [10]. Potential antioxidant role in follicle dominance protecting the dominant follicle from increasing levels of reactive oxygen species (ROS) [8,9]. |
| Glutathione peroxidase 2 | GPX2 | Antioxidant protection | Implicated in protection of embryos and extra-embryonic tissues against ROS generated in ontogenetic periods [11]. |
| Glutathione peroxidase 3 | GPX3 | Maintenance of cellular redox status Antioxidant in extracellular fluids |
Gpx3 has been identified as an essential enzyme in the defense against oxidative stress during the postovulatory process of endometrial remodeling (decasualization) in preparation for implantation by reducing H2O2 in the endometrium [12]. Implicated in normal human pregnancy and birth [13]. Implicated in maternal-fetal selenium transfer mechanism [14]. Role in pre-eclampsia and pregnancy-related hypertensive conditions [15]. Implicated in preventing the oxidative stress- induced cell apoptosis during growth of large healthy follicles [16]. |
| Glutathione peroxidase 4 | GPX4 | Detoxification of lipid hydroperoxides, Antioxidant role in membranes, serves as structural protein in sperm, Apoptosis. Membrane-associated. Present at high concentrations in the testis, where it is important for sperm motility and viability, male fertility |
Essential for embryonic development [17,18]. Potential implication in pre-eclampsia [19,20,21]. Implication in male fertility [22]. |
| Glutathione peroxidase 5 | GPX5 | Antioxidant role during sperm maturation, H2O2 scavenger [23] |
Implicated in protection of sperm from oxidative damage that could compromise their integrity and, as a consequence, embryo viability [24]. |
| Thioredoxin reductase 1 | TXNRD1 | Part of the thioredoxin system, Antioxidant role, redox regulation, cell signaling. Controls activity of transcription factors, cell proliferation, apoptosis |
Implication in early embryonic development [25,26]. |
| Thioredoxin reductase 2 | TXNRD2 | Part of the thioredoxin system, Antioxidant role, redox regulation, cell signaling |
Potential role in embryogenesis [27]. |
| Thioredoxin-glutathione reductase | TXNRD3 | Part of the thioredoxin system, Antioxidant role, redox regulation, cell signaling |
Role in disulfide bond formation and sperm maturation [28]. |
| Iodothyronine deiodinase 1 | DIO1 | Conversion of T4 to T3 and T4 to reverse T3, Production of T3 in the thyroid and peripheral tissues |
Implication in autoimmune thyroid disease and postpartum thyroid disease [29]. Dio2 and Dio3 are highly expressed at the site of implantation in pregnant rat [30]. High expression of DIO3 at utero-plecental unit and fetal epithelia has also been reported in human, Potential role in preventing the overexposure of fetus to T3 [31]. |
| Iodothyronine deiodinase 2 | DIO2 | Conversion of T4 to T3, T3 production in peripheral tissues |
|
| Iodothyronine deiodinase 3 | DIO3 | Conversion T4 to reverse T3, Production of rT3 |
|
| Selenoprotein H | SELENOH | Not fully known, potential implication in upregulation of genes relevant to glutathione synthesis | Implicated in placental oxidative stress by regulating mitochondrial biogenesis in trophoblasts (Swan-71, JEG-3 and BeWo cells) [32]. |
| Selenoprotein P | SELENOP | By and large implicated in Se transportation and antioxidant defense, Regarded as a major contributor to plasma selenium and a good indicator of Se status, Essential for male fertility; its deficiency leads to infertility characterized by abnormal spermatozoa in mice |
Implicated in maternal-fetal selenium transfer mechanism [14]. Implication in male fertility [33,34]. Involved in delivery of Se to spermatogenic cells [35]. Required for mouse sperm development [36]. Potential implication in pregnancy and pre-eclampsia [13,15,37]. |
| Selenoprotein S | SELENOS | Cellular redox balance, Possible influence in inflammatory response |
Relevant to pre-eclampsia [29,38]. Localized to the granulosa cells of large healthy and atretic follicles and also expressed in the thecal layers. Potential role in bovine follicular development [8]. |
| Selenoprotein V | SELENOV | Unknown, possible role in redox regulation | Testis-specific expression in rodents [39], in situ hybridization experiments have shown high levels of Selenov mRNA in seminiferous tubules in mice, but its exact role in spermatogenesis remains elusive [3,39]. |
Selenium is generally supplemented as organo-Se compounds or in the form of inorganic Se. It has been demonstrated that the form of Se has an important bearing on its potential beneficial and/or untoward toxic effects on the health and growth of organism [7,40,41]. A consideration of Se speciation in plant and animal food origins is of great importance and requires a thorough apprehension of the putative bio-synthetic mechanisms through which Se is assimilated in plants and how such forms undergo metabolism in animals [42]. A rising discernment is apparent regarding the fact that both total uptake and the form of dietary Se consumed are of equal importance in terms of the health benefits produced. Nevertheless, the latter may be of greater value in this regard [42]. The recommended dietary allowance (RDA) of Se in different mammalian species is listed in Table 2.
Table 2.
Recommended Dietary Allowance (RDA) of selenium for human and different animal species.
| Species | RDA |
|---|---|
| Human | Male: 55 µg/day * [43]; Female: 55 µg/day * [43] Female during pregnancy: 60 µg/day * [43] |
| Sheep | 100–200 µg/kg DM of feed/day [44] |
| Goat | 100–200 µg/kg DM of feed/day [44] |
| Growing Pigs Gestating and Lactating Sows |
150–300 µg/kg DM of feed/day [45] 150 µg/kg DM of feed/day [45] |
| Horse | 100 µg/kg DM of feed/day [46] |
| Donkey | 150 µg/100 kg body weight [47] |
| Dairy cows | 100 µg/kg DM of feed/day [48] |
| Beef cows | 300 µg/kg DM of feed/day [49] |
| Calves | 100 µg/kg DM of feed/day [48] |
| Camel | 400–800 µg/day [50] |
* Healthy adults (age: >18 years); values for United States and Canada. For further detailed information regarding RDAs of Se; readers are referred to Rayman et al. [51]. DM, Dry Matter.
Few studies on mammalian species have demonstrated the association between Se status and reproductive function in both males [52,53] and females [53,54]. There is evidence regarding the implication of Se in a number of adverse pregnancy health conditions such as pre-eclampsia, autoimmune thyroid disease, miscarriage, and preterm birth [29]. Moreover, in cattle, Se deficiency might have significant bearing and an economic impact on aspects such as decreased fertility rate, retention of placenta, and the occurrence of reproductive diseases; i.e., metritis [55]. The increased fertility following the addition of Se is ascribed to the decrease in embryonic death during the first thirty days of pregnancy [55]. Most female based studies are mainly centered on the role of Se in pregnancy [56,57,58,59,60]; only recently has some light been shed on its potential role in oocyte development and ovarian physiology [8,53,61].
2. Transport of Se and Selenoproteins
It has been reported that Se inadequacy causes a fall in the concentration of selenoproteins [62] Bösl and colleagues demonstrated that the inability of the homozygous Trsp (−/−) embryos to synthesize selenoproteins contributes to their embryonic death [63]. Selenoprotein synthesis is mediated by tRNASec; however, it is unlikely that the amount of tRNASec itself is the rate-limiting component in selenoprotein synthesis. It is rather likely that the availability of Se itself plays an essential role [63]. Thus, it is necessary for the pregnant dam to supply the embryo and the fetus with Se to support selenoprotein synthesis [14]. The placental transfer of Se is bidirectional, and might have potential bearing on its net retention in tissues of dam, fetus, and neonate [7,64]. The phenomena that, whether Se readily crosses the placental tissues in women or is, in reality, saturated and contained in the placental tissues, remains largely elusive [7,65]. Two extracellular selenoproteins, viz. selenoprotein P (Selenop) and glutathione peroxidase 3 (Gpx3), contain ca. 97% of Se in mouse plasma [14,66]. Selenoprotein P, produced largely in liver, carries Se to most of the other tissues [14,67], however, information regarding the involvement of Gpx3 in Se transport is relatively sparse [14]. As for Selenop, its transport is mediated via binding with Apolipoprotein E receptor-2 (apoER2), which serves as a mediator for the endocytosis of Se from systemic circulation [14]. Placental apoER2 seems to possess Selenop intake attributes similar to apoER2 in many other organs and tissues [14]. Lately, it has been reported that Selenop and Gpx3 are potentially involved in the transport of Se from the pregnant female to the developing fetal tissues and organs [14]. These findings lend exciting insights regarding the putative mechanisms (yolk sac and placental mechanisms) by which the transfer is achieved [14].
In a mouse model, it has been demonstrated that the visceral yolk sac mediated maternal-fetal Se transfer occurs in early pregnancy and later in gestation via the placenta [14,68]. The visceral yolk sac absorbs the fluid from the uterus that includes Selenop and Gpx3, whereas the placenta imbibes Selenop from dam’s blood through apoER2-arbitrated endocytosis [14]. These two uptake mechanisms are selenoprotein dependent and work during bodily circumstances such as Se inadequacy [14]. Nevertheless, there is a precedent regarding Se transport that does not seem to be dependent on Selenop and Gpx3 (plasma selenoproteins) [14]. Mice with both Selenop and Gpx3 knocked out were viable when given a high Se diet, indicating the implication of other routes by which Se could reach tissues [14,66,68]. Therefore, there seems to be two levels of specific Se transfer; i.e., the lower-tier mechanism and the upper-tier mechanism [14]. The lower-tier mechanism (possibly involving selenosugar or another small-molecule form of the element) does not seem to have direct dependence on selenoproteins [14]. However, it is highly dependent on the Se status of the pregnant dam and, thus, gets less efficient in conditions of Se inadequacy and functions under Se-adequate conditions [14,68]. On the other hand, the upper-tier mechanism (Selenop-apoER2 mechanism [69]) ensures the transport of Se to target tissues according to their need, even when dietary Se is limiting [14]. As demonstrated by Burk et al., the Se transport via the visceral yolk sac has the features of an upper-tier transport mechanism [14]. Even though it is not mediated via selenoproteins receptors, it obviously depends on selenoprotein intake by cells and seems to function in conditions of Se inadequacy [14]. Therefore, both the visceral yolk sac and the placenta function through the upper-tier mechanism (selenoprotein-dependent) for maternal-fetal Se transport that should protect the fetus in Se-deficient pregnant females [14,68].
3. Expression of Selenoproteins in Female Reproductive Tissues
Both the inorganic and organic forms of Se are reportedly involved in regulation of the expression of SELENOP [7]. It has been demonstrated that the content of Se and the expression of selenoproteins concurrently rise in placenta during the gestation period in rats [7]. Many selenoproteins, viz. Selenop, iodothyronine deiodinase 3 (Dio3) and thioredoxin reductase (Txnrd), are expressed in the uterus [7,70]. Meanwhile, evidence is also available regarding the expression of other selenoprotein genes such as GPX1, GPX2, GPX3, GPX4, SELENOS, (also called VIMP), SELENOT, SELENOF, SELENOH, SEPHS2, DIO3, DIO1, and SELENOM in granulosa cells of bovine ovaries [8]. Up-regulated expression of SELENOP and down-regulated expression of GPX1 and GPX3 have been reported in small atretic bovine follicles with respect to healthy bovine follicles [71]. Altered placental and uterine Selenop expressions have been observed with advancing pregnancy in mice [7,72]. Usually the level of Selenop expression increases four days prior to the birth and reaches its maximum level at full-term in mice [72]. However, preterm expression of Selenop is also witnessed in fetal liver in mice [72].
Thyroid hormones have significant importance in mammalian reproduction efficiency and during developmental stages [73]. Insufficient production of thyroid hormones in humans and rodents has been linked to reduced fertility, disturbances in the estrus cycle, impaired architecture of the uterus and implantation, and other problems relating to the maintenance of gestation [73]. Galton and colleagues reported significantly higher expression levels of Dio3 mRNA in uteri of pregnant rats [30]. The expression of Dio3 is time and region specific; i.e., highly expressed as early as day nine of gestation and localized in mesometrial and anti-mesometrial decidua of the uterus [7,30]. Both Dio3 mRNA and activity were observed at the site of implantation [30]. This high expression level of Dio3 at the implantation site is presumptuously entailed to prevent the developing fetus from excess exposure to maternal thyroid hormones [7,30]. Likewise, in human placental cells, DIO3 activity is raised with increasing gestational age [7,74]. This evidence strongly indicates that the pregnant uterine placental tissues have an essential function in regulating the exposure levels of the fetus to maternal thyroid hormones [30]. Higher DIO3 expression has also been reported in the syncytiotrophoblast and cytotrophoblasts, endothelial linings of vessels in the placenta and amnion sheath in the umbilical cord, deciduas in uterus, epithelium of human fetus, and non-pregnant human endometrium [31]. These findings indicate that the regional modulation of thyroid status is crucial at all phases of reproduction in females [31]. Many other factors are considered to play their role in the placenta and the uterus [7]. The redox proteins thioredoxin (TRX) and TXNRD have location-specific expressions in human and rodent placenta [7,75,76]. Histochemical observations have revealed that both of these are concentrated in trophoblasts, epithelial tissue of the endometrium and stromal cells in the stem villi [7,75,76]. They are reported to protect the tissues of placenta during inflammatory conditions [7,75,76].
4. Selenium in Follicular Development and Ovarian Function
Growth of granulosa cells is considered an important feature during the developmental process of follicles; i.e., the folliculogenesis. The proliferation of small primary follicles (with fewer granulosa cells) to maturing pre-ovulatory follicles (with many strata of cells) is the characteristic event in folliculogenesis [77]. In animal experiments, it has been demonstrated that Se might regulate the growth of the granulosa cells and 17β-estradiol bio-synthesis in adult ovaries in vitro [77]. Recent studies have also elucidated that Se and selenoproteins levels are increased in large healthy follicles and might perform a vital antioxidant function during later growth and the proliferation of follicles [8]. However, the regulatory role that Se is believed to play in the function and development of ovaries in a fetus remains poorly understood [78]. Grazul-Bilska and colleagues have reported that high Se levels (80 μg/kg bw) in a maternal diet repressed the growth of primordial, secondary, and antral follicles, stroma, and blood vasculature in ovaries of fetus in sheep compared to the Se adequate group (6 μg/kg bw). The number of proliferating primordial follicles and the labeling index (percentage of proliferating cells) of primordial follicles was reduced following high Se diets [78].
4.1. Evidence from In Vitro and Animal Model Studies
Sodium selenite (inorganic Se) not only improves the oocyte growth, but also enhances the proliferation rate in theca and granulosa cells. In corroboration to this hypothesis, an in vitro study conducted by Basini and Tamanini showed that sodium selenite (5 ng/mL) supplementation triggered the proliferation of bovine granulosa cells and provided some stimulatory effects on E2 synthesis. These effects could be arbitrated, at least in part, via repression of nitric oxide production [77]. Furthermore, there is also a possibility that these effects may be influenced by the unidentified Se-dependent antioxidant enzymes in granulosa cells [77]. In another in vitro study, Kamada and Ikumo have demonstrated the implication of Se (5 and 200 ppb added in culture medium) in ameliorating the proliferation of bovine luteal cells, potentially by limiting the detrimental effects of ROS [79]. Moreover, it has been reported that GPX simulates the ability of FSH to repress apoptosis in cultured ovarian follicles of rat [80]. Additionally, Se deficiency has been demonstrated to give rise to ovarian degeneration and atresia of follicles in rats [81]. Recently, Yao and colleagues conducted an in vitro study to elucidate the underlying mechanisms through which Se exerts its effects on the proliferation and steroid hormone bio-synthesis in luteinized-granulosa cells in goat [61]. The biomarkers such as proliferating cell nuclear antigen (PCNA), Akt, and phosphoinositide 3-kinase (PI3K) were mainly expressed in ovarian oocytes and granulosa cells [61]. The proliferation of luteinized-granulosa cells was significantly stimulated following 5 ng/mL Se treatment [61]. This proliferation, may be ascribed to the increased expression of biomarkers such as PCNA, cyclin-dependent kinase 1 (CDK1), phosphorylated adenosine monophosphate-activated protein kinase (p-AMPK; Thr172), and phosphorylated Akt (p-Akt; Ser473) and reductions in expression of p21 [61]. Similarly, the estradiol production was significantly enhanced [61], and the expression of antioxidant (GPX and SOD2) and steroidogenesis-related genes (3β-HSD and StAR) were also significantly increased following Se treatment [61]. Furthermore, the bioaccumulation of Se in bovine ovarian tissue has also been investigated recently [8]. Using X-ray fluorescence imaging, Ceko and colleagues have reported that Se was consistently identified in the granulosa cell stratum of large healthy follicles, meanwhile, compared to corpora lutea, approximately a ten-fold higher Se was observed in the wall of the bovine follicles [8]. Besides, among selenoprotein genes (GPX1, GPX3, VIMP and SELENOM) in bovine granulosa cells, only GPX1 was significantly up-regulated in large healthy follicles compared to small healthy or atretic follicles [8]. These observations also suggest a potential role for this selenoprotein (antioxidant) in follicle dominance; i.e., shielding the dominant follicle from rising levels of ROS and resultant oxidative damage.
4.2. Evidence from Human Models Studies
The relationship between female fertility, Se status, and Se-dependent GPX (catalytic) activity has been demonstrated in very few studies that, in general, observed relatively low serum and follicular fluid levels to be linked with a higher infertility occurrence [82]. In 1995, Paszkowski and co-workers for the first time reported that there are noticeable traces of Se in human follicular fluid and manifestation of Se-dependent enzymatic activity [10]. One hundred thirty-five samples of follicular fluid obtained from 112 patients during transvaginal oocyte retrieval were evaluated and authors observed that the patients with idiopathic infertility had significantly reduced follicular Se levels compared to those with known causes of infertility such as tubal infertility or male factor related infertility [10]. Based on their findings, authors inferred that the antioxidant activity of selenoenzyme GPX in the microenvironment of follicles may play a significant role in gametogenesis and fertilization [10]. Recently, Ceko’s group investigated and proposed a substantial function and essentiality of GPX1 in determining the follicle growth, maturation, and dominance in human follicles [8]. For this purpose, human cumulus cells (CCs) derived from cumulus-oocyte complexes (COCs) obtained for both in vitro fertilization (IVF) and intra-cytoplasmic sperm injection were utilized [8]. These CCs recovered from COCs before embryo transfers that ensued in a pregnancy demonstrated significantly higher GPX1 expression compared to those that failed to result in a pregnancy [8]. The fact that many researchers have demonstrated a pronounced reduction in GPX1 expression under deficient dietary Se conditions highlights the possibility that ovarian pathologies may, partially, be ameliorated through Se supplementation [8]. These findings will serve as bases for epidemiological studies tending to outline the dietary uptake of Se, GPX1 expression in vivo, and the occurrence of ovulation related diseases [8,9].
5. Implication of Se in Ovarian Pathologies and Assisted Reproductive Technologies-related Oxidative Stress
The association between oxidative stress, reduced female fertility, and Se inadequacy is another scientific domain that is compelling us for further detailed investigations and understanding [83]. A possible instructive fact is that, excessive generation of ROS in endometriosis, such as in polycystic ovary syndrome, may presumably cause an extravagant expenditure of Se, because of its antioxidant attributes. However, then again, an elemental low Se status leads to an imbalance of antioxidant with an accretion of ROS which, by and large, is regarded as a predisposing factor for polycystic ovary syndrome. In any case, a low Se status in body causes a reduced resistance to free radical-induced injury; this may be attributed to its involvement in the formation of selenoproteins combined with its antioxidant ability [84].
5.1. Human Studies
The identification of patients suffering infertility or primary ovarian insufficiency (POI) with ovarian autoimmunity may lend the substitute treatment schemes from those due to chemotherapeutic, environmental, genetical, and radiation related factors [85]. Selenium-binding protein 1 (SBP1) is unique to ovarian autoimmunity related with infertility and POI [85]. Edassery and colleagues identified antigens frequently affiliated with serum auto-antibodies in women with idiopathic infertility and POI. Significantly higher levels of SBP1 were observed in women suffering from idiopathic infertility and premature ovarian failure [85]. In India, Singh et al. studied the markers of oxidative stress in the follicular fluid of women with endometriosis and tubal infertility undergoing IVF and observed a significantly (compared to controls) increased production of ROS and malonaldehyde in the follicular fluid of patients suffering from endometriosis [86]. Moreover, significantly lower Se levels were recorded in infertile women with endometriosis compared to women enduring tubal infertility [86]. In 2013, a study from Turkey, demonstrated significantly lower plasma Se concentrations in 36 women with polycystic ovary syndrome compared to the control group (n = 33 body mass index-matched healthy women) [87]. These reduced Se levels in women with polycystic ovary syndrome may be associated to hyperandrogenism [87].
Furthermore, it has been reported that appropriate supplementation of micronutrients including Se may have significant implication in the redox balance of follicular micro-environment and, consequently, on IVF results [88]. Two recent ART-related clinical studies (Luddi et al. [88] and Jiménez Tuñón et al. [89]) have demonstrated that Se supplementation (in the form of micronutrient supplement) may ameliorate the outcome of IVF (Table 3). Both of these studies were relatively underpowered, with very small number of enrolled subjects in either case. Another apparent limitation of these two studies is that Se was supplemented in combination with other micronutrients, therefore, the camouflaged effects of other essential trace elements cannot be entirely ruled out. These findings, to some degree, may serve as a useful foundation for the clinical practitioners in the management of women undergoing IVF treatment [88]. Nevertheless, we may benefit more by extending our apprehension of maternal nutrition in pregnancy to incorporate simultaneous mechanistic and epidemiological studies, particularly on multiple micronutrients and their interactions in order to fully elucidate the importance of these factors in successful reproduction and pregnancy [90].
Table 3.
Studies demonstrating the implication of selenium (as micronutrient supplement) in ameliorating the in vitro fertilization (IVF) outcomes.
| Study Design | Type and Duration of Treatment | No. of Subjects Enrolled | Key Results Relevant to IVF | Ref. |
|---|---|---|---|---|
| Open label preliminary clinical trial (Italy) | Elevit, Bayer containing Se (50 μg) for three months | 18 patients aging >39 years; undergoing IVF/intracytoplasmic sperm injection (ICSI) treatment | The follicular fluid and serum proteins were protected from oxidative injury when aged women were supplemented with micronutrients ahead of IVF cycles. Significant increase in the mean values of good quality oocytes (recovered from women following the micronutrient supplement) was also observed. | [88] |
| Double-blind, randomized prospective study (Spain) | Seidivid, containing Se (27.5 μg) 2 months prior to ovarian puncture | 120 patients going through assisted reproductive interventions | Significantly improved embryonic quality was recorded. No significant improvement in the results (relating to follicle number, oocyte maturation, quality of vitrified embryos) was recorded. |
[89] |
5.2. In Vitro Studies
Generally, the embryos are, in particular, sensitive to oxidative damage, since they reportedly have lower antioxidant enzymatic activity compared to adults [91,92]. Nevertheless, in order to maintain the viability and quality of embryo, a rigorously characterized culture media is a prerequisite. Albeit, many embryo culture media are available nowadays, the optimum milieu is not greatly achieved and investigations focusing on blastocyst-promoting substances are still en route [93,94]. To ensure the adequate biosynthesis of selenoprotein in cultured cells, Se is contained in all mainstream tissue culture media [94,95,96]. For its potential enzymic activity, Se-dependent GPX does not only require Se and pyridoxine but, it also depends on glutathione (GSH) availability [97]. The amount of GSH in the porcine oocyte surmounts the needs for fertilization, but during pre-implantation development, embryonic GSH unremittingly reduces and attains a lowest point at the blastocyst stage. It is noteworthy that, the highest levels of endogenous ROS are also generated at this stage [98]. Presumably, these lower and higher levels of GSH and ROS respectively, have a possible function in the process of normal differentiation [99,100]; therein, ROS may have an essential functional and regulatory role pertaining to the apoptosis in the mouse blastocyst [99].
Selenium supplementation in embryo culture has been implicated in improving the developmental competence and overall quality of porcine parthenogenetic embryos by limiting the oxidative injury and programmed cell death [94]. The addition of sodium selenite (2.5 and 25 ng/mL) to the culture medium enhanced the blastocyst rate, cell number, and inner cell mass rate, reduced the apoptosis, the ratio of BAX/BCL-xL genes and the expression of Caspase 3, and improved the expression of GPX and ERK1/2 in porcine parthenogenetic embryos [94]. Moreover, Se supplementation has also been implicated in improving the intracellular GPX concentrations and activity, modulating the gene expression during in vitro oocyte maturation and ameliorating the blastocyst development and quality of in vitro fertilized bovine embryos. Recently in China, one research group has studied the Se concentrations in follicular fluid and the effects of Se supplementation on meiosis, DNA integrity in CCs, developmental competence of oocytes, GPX activity in denuded oocytes, and expression of Se-related genes in the yak oocytes during in vitro maturation [53]. Following supplementation of in vitro maturation medium with Se (2 and 4 µg/mL sodium selenite), the DNA damage was significantly reduced in cumulus cells. Meanwhile, total GPX activity, blastocyst formation rate, and the expression of selenoprotein-related genes were significantly increased in Se supplemented groups compared to the control (0 µg /mL sodium selenite) group [53].
In another in vitro study elucidating the role of sodium selenite, Abedelahi’s group reported that Se supplementation (5 or 10 ng/mL sodium selenite added in culture medium) ameliorated the ROS-induced oxidative stress and improved the total antioxidant capacity (TAC) and GPX activity in pre-antral follicles obtained from vitrified and non-vitrified ovarian tissues [101]. The development rate of follicles, oocytes, and embryos was significantly improved in Se treated groups [101]. Similarly, in their earlier in vitro study, the same group demonstrated that sodium selenite (5 and 10 ng/mL sodium selenite added in culture medium) exerts a dose-dependent ameliorative effect on growth and viability of follicles and oocytes, and these effects are presumably due to its proliferative and broader antioxidant capacity [102]. Taken as a whole, these findings, in some way, represent an approach towards attaining improved in vitro oocyte maturation and developmental capacity in mammalian oocytes and embryos, and may serve as a base for future research in this domain.
6. Effects of Maternal Dietary Se Supplementation
During gestation, dietary Se supplementation cannot only enhance antioxidant activity and stimulate the production of estradiol, progesterone and T4, but it also improves the overall metabolism of major nutrients [103]. In a few recent studies, the effects of maternal supplementation with organic and inorganic Se in combination with other vitamins such as pyridoxine were evaluated. It has been reported that pyridoxine has an important implication in the adequate flow of organic Se towards the Se-dependent GPX system in response to oxidative stress [104,105,106]. In any case, animal studies reporting the effects of maternal dietary Se supplementation on oxidative stress, antioxidant activity, embryo development, and reproductive efficiency are presented in Table 4.
Table 4.
Effects of maternal dietary Se supplementation on oxidative stress, antioxidant activity, embryo development and reproductive efficiency.
| Model | Treatment Regime | Key Findings as Reported by Authors | Ref. |
|---|---|---|---|
| Pregnant goats | 0 mg (control group), 0.5, 2.0 and 4.0 mg Se/kg DM during gestation period | Organic Se supplementation significantly improved the total antioxidant capacity (TAC), activity of GPX and SOD. The levels of estradiol, progesterone and T4 were also significantly increased | [103] |
| Gilts | Organic (0.3 mg/kg Se- enriched yeast) and inorganic (0.3 mg/kg sodium selenite) Se (combined with pyridoxine) | Organic Se (with pyridoxine) substantially induced the transcriptome of porcine expanded blastocysts compared to gilts in the control group. Organic Se (with pyridoxine) more noticeably affected the metabolism in porcine expanded blastocysts compared to those supplemented with inorganic Se (with pyridoxine). Organic Se selectively stimulated the genes implicated in antioxidant defense. In expanded blastocysts from organic Se supplemented gilts, other members of the thioredoxin family and ubiquinones seem to embellish the antioxidant activity and the modulation of cell proliferation |
[104] |
| Gilts | Basal diet 0.3 mg/kg and 2.4 mg/kg of Se and pyridoxine, respectively; 0.3 mg/kg sodium selenite without pyridoxine; 0.3 mg/kg sodium selenite +10 mg/kg pyridoxine; 0.3 mg/kg of Se-enriched yeast without pyridoxine; 0.3 mg/kg of Se-enriched yeast +10 mg/kg pyridoxine | Both Se level and source significantly enhanced Se concentration in the organs of gilts and the embryos. Selenium level showed implication on total GPX activities in mitochondria |
[105] |
| Hyperovulatory first-parity gilts | Control group: Se 0.2 mg/kg; control +sodium selenite 0.3 mg/kg; control +Se-enriched yeast 0.3 mg/kg |
The Se content of individual embryos was higher in the Se-supplemented group compared to the control. The uterine transfer of Se to embryos was ameliorated and this was concomitant with an improved embryo development. GPX was improved following Se supplementation | [107] |
| Multi-parous sows | sodium selenite 0.30 mg Se/kg organic Se 0.30 mg Se/kg |
Organic Se significantly increased SOD activity, GPX and glutathione (GSH) content, Se level, total antioxidant activity, number of live and weaned pigs. Whereas organic Se significantly decreased malondialdehyde (MDA) contents compared to the inorganic Se | [108] |
| Rat | Se deficient (0.01 ppm) Se sufficient (0.5 ppm) |
In Se deficient group, higher mortality at birth; reduced viability and survival parameters, impaired growth, and development of liver in offspring accompanied with reduced hepatic Se concentrations, GPX and CAT activities, and increased SOD activity and protein oxidation were observed. However, Se sufficient diet ameliorated all aforementioned indices. |
[109] |
| Gilts | Basal diet (control group); Basal diet +0.3 mg/kg of sodium selenite; sodium selenite +10 mg/kg pyridoxine; Basal diet +0.3 mg/kg of Se-enriched yeast; Se-enriched yeast +10 mg/kg pyridoxine |
Organic Se supplementation along with dietary B6 (pyridoxine) increased the expressions of GPX1, GPX3, GPX4 | [106] |
7. Selenium and Placental Oxidative Stress
Selenium supplementation is considered an essential tool for the expressions and activities of endogenic antioxidants such as GPX and TXNRD; thus, it may likely ameliorate the oxidative stress- induced damage in experimental cell models, furnishing key mechanistic insights related to the safer utility of trace mineral supplementation in alleviating certain gestation-related diseases [32,110,111,112]. Placental oxidative stress is an important element in the pathophysiology and development of pregnancy-related complications; i.e., pre-eclampsia, intra-uterine growth restriction, gestational diabetes, and preterm labor [110]. A thorough apprehension of placental oxidative stress-induced trophoblastic apoptosis might furnish insights regarding the possible novel interventions for pre-eclampsia, which reportedly accounts for over eighty thousand premature births each year in the USA and, with the same token, is reckoned to cause around seventy-five thousands maternal deaths each year world-wide [19,111]. Recently, few reports have highlighted the possible mechanisms through which Se improves the overall mitochondrial function of trophoblastic cells and triggers mitochondrial biogenesis [32,59,110,111,112]. The findings of these studies have demonstrated that the ameliorative effects of Se are mediated through improved antioxidant generation and function, and a reduction in ROS production therefore escorting the mitochondrial function as well as increased expression of biogenesis activators [112]. Besides, SELENOH has been reported to activate the transcription factors such as NRF1 and PGC-1α to ameliorate mitochondrial biogenesis in trophoblastic cells [113]. These findings are enticing and will be useful for understanding the putative mechanisms through which trophoblastic cells react and respond to oxidative stress and how Se regulates the upregulation of associated genes and ameliorates the cell survival rate and their invasive ability by mediating the mitochondrial activity [114]. Recent studies assessing the role of Se supplementation in ameliorating the mitochondrial biogenesis and function in placental trophoblastic cell lines are detailed in Table 5.
Table 5.
Main characteristics and results of recent studies assessing the effect of selenium supplementation on mitochondrial function and expression of mitochondrial biogenesis markers in placental trophoblast cell lines.
| Model | Treatment Regime | Key Findings and Implications | References |
|---|---|---|---|
| Placental trophoblast-like cell lines (BeWo, JEG-3 and Swan-71) | Sodium selenite (100 nM) for 24 h Selenomethionine (500 nM) for 24 h |
Following Se supplementation, significantly higher mitochondrial respiration was observed in trophoblast-like cell lines compared to untreated control group. Interestingly, the treated Swan-71 cells were observed to have higher mitochondrial content (measured on basis of the ratio of mitochondrial DNA [mtDNA] to nuclear DNA [nDNA]) in both Se supplemented groups. The expression of four mitochondrial genes; i.e., MTRT1, MTRT2, MTRT3 and MTRT4 genes was significantly improved in cells treated with inorganic Se, whereas expression of only two out of these four genes was significantly improved in cells treated with organic Se. The other mitochondrial biogenesis markers; i.e., SELENOH, peroxisome proliferator-activated receptor γ coactivator-1alpha (PGC-1α) and nuclear respiratory factor-1 (NRF-1) were also significantly improved in Swan-71 cells after treatment with both organic and inorganic Se. |
[110] |
| First trimester villous placental tissue | Sodium selenite (100 nM) for 4, 12, 14, 24, 48 or 96 h. | The mitochondrial respiration (increased oxidative phosphorylation through complex IV) was significantly improved in trimester villous placental tissue explants following four hours of culture in sodium selenate treated group. | [110] |
| Placental trophoblast cell lines (BeWo, JEG-3 and Swan-71) | Sodium selenite and Selenomethionine. (Dose-dependent manner i.e., 0, 50, 100, 200, 400, 800, 1200, 1600 or 2000 nM for 24 h). Cells were treated with mitochondrial inhibitors rotenone or antimycin to induce the oxidative stress |
The expression and activity of key selenoproteins, namely, GPX and TXNRD was significantly improved (in a dose-dependent manner) in Swan-71 cells following supplementation with both sources of Se. Selenium supplementation significantly reduced the ROS- induced oxidative stress in both treated groups. Moreover, rotenone or antimycin-induced cellular toxicity was also significantly reduced in Swan-71 cells following Se supplementation. The uncontrolled apoptosis and expression of Bcl-2 in BeWo, JEG-3 and Swan-71 cells were significantly reduced. |
[111] |
| Hypoxia exposed human extravillous trophoblast cell line HTR-8/Svneo | 0.5 nM selenium for 72 h | Selenium supplementation under hypoxia increased the migration and proliferation of trophoblastic cells by ameliorating the mitochondrial oxidative stress and improved the expression of antioxidant genes i.e., heme oxygenase 1, 2 (HO-1 and HO-2) and SOD. | [114] |
| Placental trophoblast cell lines BeWo, JEG-3 and Swan-71 | Sodium selenite (100 nM) | Selenium supplementation efficaciously stimulated the mitochondrial biogenesis, increasing the number of mitochondria in trophoblastic cells. The consumption of oxygen was comparatively higher in the Se treated cells compared to the control group. The mitochondrial respiration indicated that the oxygen streaming was significantly enhanced in Se treated trophoblastic cells. The ratio of mitochondrial gene/nuclear gene was higher in the cells supplemented with Se. Meanwhile, Se supplementation also improved the expression of SELENOH, NRF-1 and PGC-1α |
[112] |
| Trophoblast cells (BeWo, JEG-3 and Swan-71) | Sodium selenite (100 nM) Selenomethionine (500 nM) Oxidative stress was induced in the cells with the addition of increasing doses of Antimycin C, Rotenone and Resazurin |
A dose-dependent reduction in the cellular activity in BeWo, JEG-3 and Swan-71 was observed when treated for 4 h with increasing concentrations of Antimycin (40–320 μM) and Rotenone (100–800 nM). However, prior incubation with sodium selenite and selenomethionine protected the trophoblast cells from oxidative stress. Following Se supplementation, the activity of GPX and TXNRD was significantly improved (in a dose-dependent manner). Induced cellular oxidative stress was significantly ameliorated following supplementation with both organic and inorganic Se. |
[32] |
| Human trophoblast cell lines BeWo and JEG-3 | Sodium selenite (100 nM) Selenomethionine (500 nM) Oxidative stress was induced using H2O2 (0–800 µM), tert-butyl hydrogen peroxide (t-butyl H2O2, 0–50 µM), cumene hydrogen peroxide (cumene H2O2, 0–50 µM) |
The activity of GPX and TXNRD was significantly improved (in a dose-dependent manner). Induced cellular oxidative stress was significantly reversed following supplementation with both organic and inorganic Se. |
[59] |
8. Role of Se in Pregnancy
It is well established that Se participates in the bio-synthesis of selenoproteins such as GPX, SELENOP, TXNRD family, and may have an essential role in pregnancy. In particular, oxidative injury may be increased during this phase [115]. Consequently, antioxidant defense mechanisms have a central role to play in modulating events mediated by oxidative stress and could be related to perinatal morbidity and mortality [116,117,118]. It must be emphasized that the implication of Se status in the progression of pregnancy complications is yet to be properly instituted. Nevertheless, the association between low Se status and the occurrence of adverse fetal outcomes has been suggested. Because a larger number of available studies are either cross-sectional or case–control, their findings are not suitable to the assessment of causal relationships. Therefore, it could be assumed that either low Se status is implicated in the causal process of such pregnancy complications and subsequent outcomes or simply indicate a maternal physiological response to the raised oxidative stress states [119].
The hypothesis, “whether the pre-pregnancy Se status is of more significance in precluding the hypertensive pregnancy conditions than status in pregnancy”, itself is still inconclusive and needs further elucidation [15]. The periconceptual events that are potentially to be affected by Se status include the oocyte development, fertilization, and implantation [8,15]. Nevertheless, the recommendations prevail for increased Se intake during the gestation period [120]. Moreover, the best timing of Se supplementation during pregnancy is one of the well identified gaps amongst the studies concerning the role of Se on reproductive health; therefore, hitherto it is currently unclear what exactly should be the optimum timing of Se supplementation [121]. The scarcity of such key information pertaining to Se is by and large endorsed by other reports encouraging further elucidation with regard to the potential impact of appropriate timings of trace element supplementation on pregnancy results [122,123]. In 2017, Mamon and Ramos conducted a study to figure out the optimal timing of Se supplementation (3.0 μg per day) during pregnancy at different stages of the peri-conception period in a murine model [121]. Improved quality of blastocysts and reduced pre-implantation loss was observed in pre-gestation only and gestation only supplementation groups compared to the control and pre-gestation-to-gestation supplementation groups [121]. These findings highlight that pre-gestation only and gestation only are the optimal peri-conception phases for Se supplementation to achieve improved developmental competence in blastocysts and pre-implantation success [121].
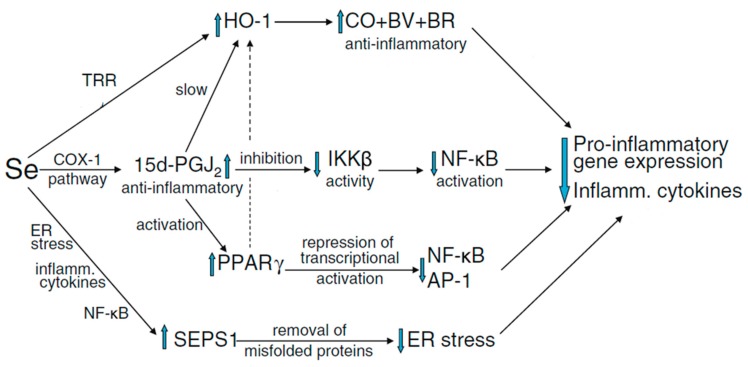
Recently, a very small number of properly powered and well-conducted studies have shown that Se is implicated in a number of complications related to pregnancy [15,37,124,125]. Positive correlation of serum Se and SELENOP levels is generally observed in populations with a borderline Se supply [124]. Furthermore, it has been shown that during the course of normal pregnancy, the whole blood Se concentrations fall considerably (12%) with advancing gestation [37,126,127]. Keeping the plasma volume expansion aside, another potential reason of a fall in concentration of Se in blood during pregnancy is probably to be the transport of Se to the fetus mediated via SELENOP, which is expressed in the placental tissues [68,72]. Conversely, higher Se status has been linked with a lower risk of miscarriage and preterm birth, however, the level of manifestation from randomized controlled trials is stronger for the beneficial role of higher Se intake and or status in pre-eclampsia and autoimmune thyroid disease. The capability of Se to ameliorate the oxidative stress, endoplasmic reticulum stress and inflammation (Figure 1), to shield the endothelium, to regulate the production of eicosanoid, to modulate the vascular tone, and repress the infection is probably crucial in the context of these conditions [29].
Figure 1.
Possible mechanisms by which Se may reduce inflammation resulting from oxidative and ER stress. Abbreviations: ER, endoplasmic reticulum; SEPS1, selenoprotein S; 15d-PGJ2, 15-deoxy-∆12,14-prostaglandin J2; IKKβ, IκB-kinase β; TRR, thioredoxin reductase; BV, billiverdin; BR, billirubin; PPAR-γ, peroxisome proliferator-activated nuclear receptor-γ (adopted by permission from [29], Springer Nature, New York, USA).
In one UK based high-quality double-blind, placebo-controlled, pilot trial, two hundred thirty primiparous pregnant females were randomized to Se treatment (60 μg/d, as Se-enriched yeast) or placebo from weeks twelve to fourteen of pregnancy till delivery [37]. Between 12 and 35 weeks, the whole blood Se concentrations were significantly increased in the Se supplemented group but reduced significantly in the placebo block. Similarly, at 35 weeks, significantly higher levels of whole blood Se and plasma SELENOP were recorded in the Se supplemented group compared to the placebo block [37]. Moreover, an inverse relationship between Se supplementation and serum soluble vascular endothelial growth factor receptor-1 (sFlt-1) was demonstrated in this study, suggesting that Se supplementation was beneficial in limiting the production of sFlt-1 that has anti-angiogenic effects and contributes to the pathophysiology of pre-eclampsia. This is the only report available to have investigated the effect of Se supplementation in a population with low Se status that studied an outcome related to the risk of pre-eclampsia [37]. In any case, there has been another recent report on Se status declining in Polish pregnant women trimester by trimester, causing the majority of pregnant women to develop severe Se deficiency. A progressive decline in the mean levels of Se and SELENOP were observed during the course of gestation in enrolled pregnant women [124]. In this study, a positive correlation was observed between serum Se and SELENOP concentrations across all three trimesters in the full group of pregnant women [124]. Similar observations were recorded in another recently reported Polish Mother and Child Cohort in which plasma Se concentrations declined from 1st to 3rd trimester by 23 % (48.3 +/− 10.6 to 37.3 +/− 9.8 μg/L) [125].
Intra-uterine growth restriction, (affecting 10–15 % of pregnant women) is a principal cause of peri-natal morbidity and mortality [128,129]. It has been reported that higher levels of ROS and inflammatory biomarkers have a central play in development and pathology of intra-uterine growth restriction [130,131]. Mesdaghinia and colleagues conducted a randomized double-blind placebo-controlled trial to evaluate the effects of supplemental Se on clinical signs and metabolic status in pregnant women (n = 60) at risk of bearing the intra-uterine growth restriction [131]. Entrants were randomly designated to take either 100 μg Se (tablet) supplement (n = 30) or placebo (n = 30) for full ten weeks (from seventeen to twenty-seven weeks of pregnancy). Following ten weeks long Se supplementation, a higher number of females in the Se-treated block showed higher pulsatility index (<1.45) in comparison to the placebo block [131]. Moreover, the plasma levels of TAC, GSH and high-sensitivity C-reactive protein were also significantly changed in the Se-treated block compared to the placebo block [131].
It is pertinent to mention that Se has also been implicated in other pregnancy associated complications such as recurrent miscarriage [56,132,133], small for gestational age infants [119,134], and postpartum thyroid dysfunction [135]. There is evidence from some randomized controlled trials and observational studies that Se (probably as component of selenoproteins) could reduce thyroid peroxidase antibodies levels, hypothyroidism, and postpartum thyroid diseases [136]. Pregnant women positive for thyroid peroxidase antibodies are at a higher risk of developing postpartum thyroid dysfunction (PPTD) and permanent hypothyroidism [135]. Selenium has also been implicated in reducing thyroid inflammatory activities in subjects with autoimmune thyroiditis [135]. In one high-quality randomized, controlled trial conducted in thyroid peroxidase antibodies-positive (TPOAb-positive) pregnant women [135], it was reported that Se supplementation (200 μg selenomethionine/day) significantly reduced TPOAb titer, thyroiditis, postpartum thyroid disease, and permanent hypothyroidism compared to the placebo group [135]. Even though the ingratiatory manifestations are already available in extant literature suggesting that supplemental Se would, in some way, benefit some of these complications in Se-deficient subjects; nonetheless, the results from ongoing (if any) or future intervention trials have the potential to reinforce or controvert the argument regarding increasing Se uptake.
9. Implication of Se and Selenoproteins in Reproductive Cancer
The implication of Se in carcinogenesis and cancer therapy has been a topic of controversial discussion for many decades, and the prevention, inhibition, or progression of cancer by selenoproteins is still a subject of on-going debate [137]. Ovarian cancer is ranked as the 5th leading cause of cancer deaths in women and has the highest overall mortality and a poor five-year survival rates [138]. Over ninety percent of the cases of ovarian cancer are epithelial ovarian cancer (EOC), which presents a series of etiologically and molecularly distinct disorders [138]. Some evidence exists in the available literature regarding the implication of Se and selenoproteins in female reproductive cancers such as ovarian cancer [139]. Significantly lower mean concentrations of Se and GPX activity have been noticed in the plasma of subjects bearing benign neoplasia and cancer of the uterine cervix, uterine corpus or ovary compared to healthy women [140]. These findings suggest that the lower antioxidant capacity (Se-related) may favor the development of female reproductive system-related tumorigenic diseases [140]. Agnani et al. reported a stage-dependent decrease in the activity of GPX3 in women suffering papillary serous ovarian cancer [139]. In the meantime, reduced serum GPX3 levels are observed in women with recurrent disease and these level-dependent reductions become more marked when patients and controls are stratified to admit only women older than 50 years of age [139]. Furthermore, both in rats as well as humans, GPX3 was also observed to be down-regulated in all grades of endometrial adenocarcinoma, irrespective of tumor grade [139,141]. In some of the previous studies, it has been reported that expression of GPX3 is higher in clear cell epithelial ovarian carcinoma tissues compared to the control [142,143,144]. Even though the underlying molecular mechanisms are not yet sufficiently understood, these results indicate that GPX3 activity is tumor-specific [138]. In one recent report, Wu and colleagues have reported that GPX3 was observed to be down-regulated in a platinum-sensitive group compared to the platinum-resistant group [138]. The putative mechanisms involved in mediating the GPX3 tumor-suppressing role are primarily attributed to promoter hyper-methylation, dysregulation of c-Met expressions, and the enzymic role of antioxidants that scavenge the detrimental free radicals [138]. However, the exact underlying mechanisms, in response to antitumor drugs, remain largely elusive and require further elucidation [138]. Nevertheless, Se and selenoproteins may provide targets for reproductive cancer treatment or prevention strategies.
10. Conclusions
In this review, we provide a comprehensive spotlight on the potential role of Se and selenoproteins in overall reproduction efficiency and many disorders related to both animal and human reproduction. It is obvious from the findings of previous studies (both animal and human) that Se and selenoproteins are essential for optimal reproduction in females, presumably because of their implication in the regulation and modulation of antioxidant balance.
The role of Se and selenoproteins in many domains of female reproduction, such as the effects of maternal dietary Se supplementation on oxidative stress, role of Se in fetal ovarian development and function, and the implication of Se supplementation in ameliorating the placental oxidative stress, is poorly understood and requires through consideration. Moreover, little attention has been paid to the pre-conception period, or focus on general reproductive efficiency and health when it comes to ovarian physiology, in particular, the synthesis of hormones and the development of ovarian follicles. Only recently has some evidence on the possible role of Se and selenoproteins in oocyte maturation and fertilization emerged from in vitro animal trials; but large, well powered, in vivo controlled trials are still sparse. Furthermore, the level of evidence regarding the role of Se and selenoproteins in different ovarian pathologies including cancer is very low and inconclusive. In the meantime, the implication of Se and selenoproteins in ameliorating the oxidative and nitrosative stress induced in assisted reproductive technologies such as IVF and embryo development is not yet sufficiently understood. Besides, there are many other questions regarding the role of Se and selenoproteins in female reproduction (animal and human) that remain unrequited. Answers to these questions as well as a further elucidation of the roles of Se and selenoproteins should help to explicate the potential biological functions of this potent micronutrient (Se) in female reproductive efficiency and health.
The response curve for Se supplementation appears to be U-shaped; i.e., beneficial in Se-deficient individuals and with potential health related risks in those who are supplemented in excess concentrations [145]. Therefore, we must be careful not to encourage the excessive intake of Se supplements, in particular people of adequate or high status. As for the implication of Se supplementation in pregnancy, the outcomes of sparse yet high-quality properly powered, randomized, controlled trials in populations of relatively low Se status are enticing [37], however, higher numbers of such trials (double-blind, placebo-controlled, two-group studies with proper follow-up) are required to further elucidate the exact underlying molecular and biochemical mechanisms through which Se or selenoproteins might have beneficial effects in reducing the markers of risk of pregnancy-related complications such as pre-eclampsia. In this context, the current ongoing trials (if any) and the meta-analysis should soon enable the development of proper recommendations. Nevertheless, as a matter of fact, there is a profuseness of specialized supplements (containing Se) marketed to pregnant women and the percentage of pregnant women consuming such supplements is now very high in developed countries; it is getting increasingly hard to enroll subjects (pregnant women) in randomized control trials.
To sum up, the level and quality of available evidence regarding the ameliorative effects of both Se and selenoproteins in female reproduction are high; however, the volume of such research is not yet sufficient enough to draw solid conclusions. Therefore, studies elucidating the potential effect of Se supplementation and selenoproteins (i.e., GPX, SELENOP, SELENOS and allied) in ovarian function, pregnancy-related complications, and overall female reproductive efficiency would be of great value and will add more to the tally of the already known benefits of this trace mineral.
Acknowledgments
All authors are thankful to Margaret Rayman, Department of Nutritional Sciences, University of Surrey, UK, for helpful discussion and guidance for drafting the original draft of this manuscript. We also acknowledge many researchers for sharing their valuable literature through personal communication.
Author Contributions
G.-B.Z. conceived the idea, provided guidance and edited the article for submission. I.H.Q. designed the study, compiled the information and drafted the manuscript. C.A. helped in drafting, reviewing and initial editing of manuscript. H.Y., B.P., C.-J.Z. and H.H. were involved in reorganizing the structure of the article and tables, edited the text and introduced new information. E.Z. and C.-J.Z. revised the manuscript and introduced new information. All authors read and approved the final manuscript.
Funding
This work was supported in part by the China Agriculture Research System (Grant NO.CARS-36) and the National Natural Science Foundation of China (Grant No.31572398).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Rayman M.P. The importance of selenium to human health. The Lancet. 2000;356:233–241. doi: 10.1016/S0140-6736(00)02490-9. [DOI] [PubMed] [Google Scholar]
- 2.Labunskyy V.M., Hatfield D.L., Gladyshev V.N. Selenoproteins: molecular pathways and physiological roles. Physiol. Rev. 2014;94:739–777. doi: 10.1152/physrev.00039.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kryukov G.V., Castellano S., Novoselov S.V., Lobanov A.V., Zehtab O., Guigó R., Gladyshev V.N. Characterization of mammalian selenoproteomes. Science. 2003;300:1439–1443. doi: 10.1126/science.1083516. [DOI] [PubMed] [Google Scholar]
- 4.Papp L.V., Lu J., Holmgren A., Khanna K.K. From selenium to selenoproteins: synthesis, identity, and their role in human health. Antioxid. Redox Signaling. 2007;9:775–806. doi: 10.1089/ars.2007.1528. [DOI] [PubMed] [Google Scholar]
- 5.Gladyshev V.N., Arnér E.S., Berry M.J., Brigelius-Flohé R., Bruford E.A., Burk R.F., Carlson B.A., Castellano S., Chavatte L., Conrad M. Selenoprotein gene nomenclature. J. Biol. Chem. 2016;291:24036–24040. doi: 10.1074/jbc.M116.756155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zoidis E., Seremelis I., Kontopoulos N., Danezis G.P. Selenium-Dependent Antioxidant Enzymes: Actions and Properties of Selenoproteins. Antioxidants. 2018;7:66. doi: 10.3390/antiox7050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pappas A., Zoidis E., Surai P., Zervas G. Selenoproteins and maternal nutrition. Comp. Biochem. Physiol. Part. B: Biochem. Mol. Biol. 2008;151:361–372. doi: 10.1016/j.cbpb.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Ceko M.J., Hummitzsch K., Hatzirodos N., Bonner W.M., Aitken J.B., Russell D.L., Lane M., Rodgers R.J., Harris H.H. X-Ray fluorescence imaging and other analyses identify selenium and GPX1 as important in female reproductive function. Metallomics. 2015;7:71–82. doi: 10.1039/C4MT00228H. [DOI] [PubMed] [Google Scholar]
- 9.Ceko M.J., Hummitzsch K., Bonner W.M., Aitken J.B., Spiers K.M., Rodgers R.J., Harris H.H. Localization of the trace elements iron, zinc and selenium in relation to anatomical structures in bovine ovaries by X-ray fluorescence imaging. Microsc. Microanal. 2015;21:695–705. doi: 10.1017/S1431927615000380. [DOI] [PubMed] [Google Scholar]
- 10.Paszkowski T., Traub A., Robinson S., McMaster D. Selenium dependent glutathione peroxidase activity in human follicular fluid. Clin. Chim. Acta. 1995;236:173–180. doi: 10.1016/0009-8981(95)98130-9. [DOI] [PubMed] [Google Scholar]
- 11.Baek I.J., Yon J.M., Lee S.R., Kim M.R., Hong J., Lee B., Yun Y., Nam S.Y. Differential Expression of Gastrointestinal Glutathione Peroxidase (GI-GPx) Gene during Mouse Organogenesis. Anat. Histol. Embryo. 2011;40:210–218. doi: 10.1111/j.1439-0264.2010.01061.x. [DOI] [PubMed] [Google Scholar]
- 12.Xu X., Leng J.-Y., Gao F., Zhao Z.-A., Deng W.-B., Liang X.-H., Zhang Y.-J., Zhang Z.-R., Li M., Sha A.-G. Differential expression and anti-oxidant function of glutathione peroxidase 3 in mouse uterus during decidualization. FEBS Lett. 2014;588:1580–1589. doi: 10.1016/j.febslet.2014.02.043. [DOI] [PubMed] [Google Scholar]
- 13.Santos C., García-Fuentes E., Callejón-Leblic B., García-Barrera T., Gómez-Ariza J.L., Rayman M.P., Velasco I. Selenium, selenoproteins and selenometabolites in mothers and babies at the time of birth. Br. J. Nutr. 2017;117:1304–1311. doi: 10.1017/S0007114517001155. [DOI] [PubMed] [Google Scholar]
- 14.Burk R.F., Olson G.E., Hill K.E., Winfrey V.P., Motley A.K., Kurokawa S. Maternal-fetal transfer of selenium in the mouse. FASEB J. 2013;27:3249–3256. doi: 10.1096/fj.13-231852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rayman M.P., Bath S.C., Westaway J., Williams P., Mao J., Vanderlelie J.J., Perkins A.V., Redman C.W. Selenium status in UK pregnant women and its relationship with hypertensive conditions of pregnancy. Br. J. Nutr. 2015;113:249–258. doi: 10.1017/S000711451400364X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hayashi K.-G., Ushizawa K., Hosoe M., Takahashi T. Differential genome-wide gene expression profiling of bovine largest and second-largest follicles: identification of genes associated with growth of dominant follicles. Reprod. Biol. Endocrinol. 2010;8:11. doi: 10.1186/1477-7827-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yant L.J., Ran Q., Rao L., Van Remmen H., Shibatani T., Belter J.G., Motta L., Richardson A., Prolla T.A. The selenoprotein GPX4 is essential for mouse development and protects from radiation and oxidative damage insults. Free Radical Biol. Med. 2003;34:496–502. doi: 10.1016/S0891-5849(02)01360-6. [DOI] [PubMed] [Google Scholar]
- 18.Imai H., Hirao F., Sakamoto T., Sekine K., Mizukura Y., Saito M., Kitamoto T., Hayasaka M., Hanaoka K., Nakagawa Y. Early embryonic lethality caused by targeted disruption of the mouse PHGPx gene. Biochem. Biophys. Res. Commun. 2003;305:278–286. doi: 10.1016/S0006-291X(03)00734-4. [DOI] [PubMed] [Google Scholar]
- 19.Mistry H.D., Wilson V., Ramsay M.M., Symonds M.E., Pipkin F.B. Reduced selenium concentrations and glutathione peroxidase activity in preeclamptic pregnancies. Hypertension. 2008;52:881–888. doi: 10.1161/HYPERTENSIONAHA.108.116103. [DOI] [PubMed] [Google Scholar]
- 20.Peng X., Lin Y., Li J., Liu M., Wang J., Li X., Liu J., Jia X., Jing Z., Huang Z. Evaluation of Glutathione Peroxidase 4 role in Preeclampsia. Sci. Rep. 2016;6:33300. doi: 10.1038/srep33300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malinova M., Paskaleva V. Selenium and glutathione peroxidase in patients with preeclampsia. Akush. Ginekol. 2013;52:3–7. [PubMed] [Google Scholar]
- 22.Imai H., Hakkaku N., Iwamoto R., Suzuki J., Suzuki T., Tajima Y., Konishi K., Minami S., Ichinose S., Ishizaka K. Depletion of selenoprotein GPx4 in spermatocytes causes male infertility in mice. J. Biol. Chem. 2009;284:32522–32532. doi: 10.1074/jbc.M109.016139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahsan U., Kamran Z., Raza I., Ahmad S., Babar W., Riaz M., Iqbal Z. Role of selenium in male reproduction—A review. Anim. Reprod. Sci. 2014;146:55–62. doi: 10.1016/j.anireprosci.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 24.Chabory E., Damon C., Lenoir A., Kauselmann G., Kern H., Zevnik B., Garrel C., Saez F., Cadet R., Henry-Berger J. Epididymis seleno-independent glutathione peroxidase 5 maintains sperm DNA integrity in mice. J. Clin. Investing. 2009;119:2074–2085. doi: 10.1172/JCI38940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jakupoglu C., Przemeck G.K., Schneider M., Moreno S.G., Mayr N., Hatzopoulos A.K., de Angelis M.H., Wurst W., Bornkamm G.W., Brielmeier M. Cytoplasmic thioredoxin reductase is essential for embryogenesis but dispensable for cardiac development. Mol. Cell. Biol. 2005;25:1980–1988. doi: 10.1128/MCB.25.5.1980-1988.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bondareva A.A., Capecchi M.R., Iverson S.V., Li Y., Lopez N.I., Lucas O., Merrill G.F., Prigge J.R., Siders A.M., Wakamiya M. Effects of thioredoxin reductase-1 deletion on embryogenesis and transcriptome. Free Radical Biol. Med. 2007;43:911–923. doi: 10.1016/j.freeradbiomed.2007.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conrad M., Jakupoglu C., Moreno S.G., Lippl S., Banjac A., Schneider M., Beck H., Hatzopoulos A.K., Just U., Sinowatz F. Essential role for mitochondrial thioredoxin reductase in hematopoiesis, heart development, and heart function. Mol. Cell. Biol. 2004;24:9414–9423. doi: 10.1128/MCB.24.21.9414-9423.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Su D., Novoselov S.V., Sun Q.-A., Moustafa M.E., Zhou Y., Oko R., Hatfield D.L., Gladyshev V.N. Mammalian selenoprotein thioredoxin-glutathione reductase roles in disulfide bond formation and sperm maturation. J. Biol. Chem. 2005;280:26491–26498. doi: 10.1074/jbc.M503638200. [DOI] [PubMed] [Google Scholar]
- 29.Rayman M.P. Selenium. Springer; New York, NY, USA: 2011. Selenium and adverse health conditions of human pregnancy; pp. 531–544. [Google Scholar]
- 30.Galton V.A., Martinez E., Hernandez A., Germain E.A.S., Bates J.M., Germain D.L.S. Pregnant rat uterus expresses high levels of the type 3 iodothyronine deiodinase. J. Clin. Investing. 1999;103:979–987. doi: 10.1172/JCI6073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang S.A., Dorfman D.M., Genest D.R., Salvatore D., Larsen P.R. Type 3 iodothyronine deiodinase is highly expressed in the human uteroplacental unit and in fetal epithelium. J. Clin. Endocrinol. Metab. 2003;88:1384–1388. doi: 10.1210/jc.2002-021291. [DOI] [PubMed] [Google Scholar]
- 32.Khera A., Vanderlelie J., Perkins A. Selenium supplementation protects trophoblast cells from mitochondrial oxidative stress. Placenta. 2013;34:594–598. doi: 10.1016/j.placenta.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Michaelis M., Gralla O., Behrends T., Scharpf M., Endermann T., Rijntjes E., Pietschmann N., Hollenbach B., Schomburg L. Selenoprotein P in seminal fluid is a novel biomarker of sperm quality. Biochem. Biophys. Res. Commun. 2014;443:905–910. doi: 10.1016/j.bbrc.2013.12.067. [DOI] [PubMed] [Google Scholar]
- 34.Renko K., Werner M., Renner-Muller I., Cooper T.G., Yeung C.H., Hollenbach B., Scharpf M., Kohrle J., Schomburg L., Schweizer U. Hepatic selenoprotein P (SePP) expression restores selenium transport and prevents infertility and motor-incoordination in Sepp-knockout mice. Biochem. J. 2008;409:741–749. doi: 10.1042/BJ20071172. [DOI] [PubMed] [Google Scholar]
- 35.Olson G.E., Winfrey V.P., NagDas S.K., Hill K.E., Burk R.F. Apolipoprotein E receptor-2 (ApoER2) mediates selenium uptake from selenoprotein P by the mouse testis. J. Biol. Chem. 2007;282:12290–12297. doi: 10.1074/jbc.M611403200. [DOI] [PubMed] [Google Scholar]
- 36.Olson G.E., Winfrey V.P., NagDas S.K., Hill K.E., Burk R.F. Selenoprotein P is required for mouse sperm development. Biol. Reprod. 2005;73:201–211. doi: 10.1095/biolreprod.105.040360. [DOI] [PubMed] [Google Scholar]
- 37.Rayman M.P., Searle E., Kelly L., Johnsen S., Bodman-Smith K., Bath S.C., Mao J., Redman C.W. Effect of selenium on markers of risk of pre-eclampsia in UK pregnant women: a randomised, controlled pilot trial. Br. J. Nutr. 2014;112:99–111. doi: 10.1017/S0007114514000531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moses E.K., Johnson M.P., Tommerdal L., Forsmo S., Curran J.E., Abraham L.J., Charlesworth J.C., Brennecke S.P., Blangero J., Austgulen R. Genetic association of preeclampsia to the inflammatory response gene SEPS1. Am. J. Obstet. Gynecol. 2008;198:20. doi: 10.1016/j.ajog.2007.09.024. [DOI] [PubMed] [Google Scholar]
- 39.Turanov A.A., Malinouski M., Gladyshev V.N. Selenium and male reproduction. In: Hatfield D., Berry M., Gladyshev V., editors. Selenium: Its Molecular Biology and Role in Human Health. Springer; New York, NY, USA: 2011. pp. 409–417. [Google Scholar]
- 40.Letavayová L., Vlčková V., Brozmanová J. Selenium: from cancer prevention to DNA damage. Toxicology. 2006;227:1–14. doi: 10.1016/j.tox.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 41.Schrauzer G.N. Selenomethionine: A review of its nutritional significance, metabolism and toxicity. J. Nutr. 2000;130:1653–1656. doi: 10.1093/jn/130.7.1653. [DOI] [PubMed] [Google Scholar]
- 42.Rayman M.P., Infante H.G., Sargent M. Food-chain selenium and human health: spotlight on speciation. Br. J. Nutr. 2008;100:238–253. doi: 10.1017/S0007114508922522. [DOI] [PubMed] [Google Scholar]
- 43.Institute of Medicine: Panel on Dietary Antioxidants and Related Compounds: Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington (DC) [(accessed on 19 November 2018)]; Available online: https://www.ncbi.nlm.nih.gov/books/NBK225470/
- 44.Council N.R. Nutrient Requirements of Small Ruminants: Sheep, Goats, Cervids, and New World Camelids. The National Academies Press; Washington, DC, USA: 2007. p. 384. [Google Scholar]
- 45.Surai P.F., Fisinin V.I. Selenium in Pig Nutrition and reproduction: Boars and semen quality—A Review. Asian-Australas. J. Anim. Sci. 2015;28:730. doi: 10.5713/ajas.14.0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Council N.R. Nutrient Requirements of Horses: Sixth Revised Edition. The National Academies Press; Washington, DC, USA: 2007. p. 360. [Google Scholar]
- 47.Geor R.J., Coenen M., Harris P. Equine Applied and Clinical Nutrition E-Book: Health, Welfare and Performance. FEMS Microbiol. Lett. 2014;57:73–77. [Google Scholar]
- 48.Council N.R. Nutrient Requirements of Dairy Cattle: Seventh Revised Edition, 2001. The National Academies Press; Washington, DC, USA: 2001. p. 408. [Google Scholar]
- 49.Council N.R. Nutrient Requirements of Beef Cattle: Seventh Revised Edition: Update 2000. The National Academies Press; Washington, DC, USA: 2000. p. 248. [Google Scholar]
- 50.Faye B., Seboussi R. Selenium in camel–A review. Nutrients. 2009;1:30–49. doi: 10.3390/nu1010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rayman M.P. The use of high-selenium yeast to raise selenium status: how does it measure up? Br. J. Nutr. 2004;92:557–573. doi: 10.1079/BJN20041251. [DOI] [PubMed] [Google Scholar]
- 52.Foresta C., Flohé L., Garolla A., Roveri A., Ursini F., Maiorino M. Male fertility is linked to the selenoprotein phospholipid hydroperoxide glutathione peroxidase. Biol. Reprod. 2002;67:967–971. doi: 10.1095/biolreprod.102.003822. [DOI] [PubMed] [Google Scholar]
- 53.Xiong X., Lan D., Li J., Lin Y., Li M. Selenium supplementation during in vitro maturation enhances meiosis and developmental capacity of yak oocytes. Anim. Sci. J. 2018;89:298–306. doi: 10.1111/asj.12894. [DOI] [PubMed] [Google Scholar]
- 54.Kommisrud E., Østerås O., Vatn T. Blood selenium associated with health and fertility in Norwegian dairy herds. Acta Vet. Scand. 2005;46:229. doi: 10.1186/1751-0147-46-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mehdi Y., Dufrasne I. Selenium in cattle: a review. Molecules. 2016;21:545. doi: 10.3390/molecules21040545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Al-Kunani A., Knight R., Haswell S., Thompson J., Lindow S. The selenium status of women with a history of recurrent miscarriage. BJOG: An. Int. J. Obstet. Gynaecol. 2001;108:1094–1097. doi: 10.1111/j.1471-0528.2001.00253.x. [DOI] [PubMed] [Google Scholar]
- 57.Güvenç M., Güven H., Karataş F., Aygün A.D., Bektaş S. Low levels of selenium in miscarriage. J. Trace Elements Exp. Med. 2002;15:97–101. doi: 10.1002/jtra.10004. [DOI] [Google Scholar]
- 58.Rumiris D., Purwosunu Y., Wibowo N., Farina A., Sekizawa A. Lower rate of preeclampsia after antioxidant supplementation in pregnant women with low antioxidant status. Hypertens. Pregnancy. 2006;25:241–253. doi: 10.1080/10641950600913016. [DOI] [PubMed] [Google Scholar]
- 59.Watson M., Van Leer L., Vanderlelie J., Perkins A. Selenium supplementation protects trophoblast cells from oxidative stress. Placenta. 2012;33:1012–1019. doi: 10.1016/j.placenta.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 60.Tsuzuki S., Morimoto N., Hosokawa S., Matsushita T. Associations of maternal and neonatal serum trace element concentrations with neonatal birth weight. PLoS ONE. 2013;8:e75627. doi: 10.1371/journal.pone.0075627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yao X., Ei-Samahy M., Fan L., Zheng L., Jin Y., Zhang G., Liu Z., Wang F. In vitro influence of selenium on the proliferation of and steroidogenesis in goat luteinized granulosa cells. Theriogenology. 2018;114:70–80. doi: 10.1016/j.theriogenology.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 62.Hill K.E., Lyons P.R., Burk R.F. Differential regulation of rat liver selenoprotein mRNAs in selenium deficiency. Biochem. Biophys Res. Commun. 1992;185:260–263. doi: 10.1016/S0006-291X(05)80984-2. [DOI] [PubMed] [Google Scholar]
- 63.Bösl M.R., Takaku K., Oshima M., Nishimura S., Taketo M.M. Early embryonic lethality caused by targeted disruption of the mouse selenocysteine tRNA gene (Trsp) Proc. Natl. Acad. Sci. 1997;94:5531–5534. doi: 10.1073/pnas.94.11.5531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee A.M., Huel G., Godin J., Hellier G., Sahuquillo J., Moreau T., Blot P. Inter-individual variation of selenium in maternal plasma, cord plasma and placenta. Sci. Total Environ. 1995;159:119–127. doi: 10.1016/0048-9697(95)04123-I. [DOI] [PubMed] [Google Scholar]
- 65.Eisenmann C., Miller R. The placental transfer and toxicity of selenite relative to cadmium in the human term perfused placenta. Placenta. 1994;15:883–895. doi: 10.1016/S0143-4004(05)80189-4. [DOI] [PubMed] [Google Scholar]
- 66.Olson G.E., Whitin J.C., Hill K.E., Winfrey V.P., Motley A.K., Austin L.M., Deal J., Cohen H.J., Burk R.F. Extracellular glutathione peroxidase (Gpx3) binds specifically to basement membranes of mouse renal cortex tubule cells. Am. J. Physiol. Ren. Physiol. 2009;298:F1244–F1253. doi: 10.1152/ajprenal.00662.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Burk R.F., Hill K.E. Selenoprotein P—expression, functions, and roles in mammals. Biochim. et Biophys. Acta Gen. Subj. 2009;1790:1441–1447. doi: 10.1016/j.bbagen.2009.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Burk R.F., Hill K.E. Regulation of selenium metabolism and transport. Annu. Rev. Nutr. 2015;35:109–134. doi: 10.1146/annurev-nutr-071714-034250. [DOI] [PubMed] [Google Scholar]
- 69.Kurokawa S., Hill K.E., McDonald W.H., Burk R.F. Long-isoform mouse selenoprotein P (Sepp1) supplies rat myoblast L8 cells with selenium via endocytosis mediated by heparin-binding properties and apolipoprotein E receptor-2 (apoER2) J. Biol. Chem. 2012;287:28717–28726. doi: 10.1074/jbc.M112.383521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bou-Resli M., Dashti H., Mathew T., Al-Zaid N. Pre-and postnatal tissue selenium of the rat in the growing state. Neonatology. 2001;80:169–172. doi: 10.1159/000047138. [DOI] [PubMed] [Google Scholar]
- 71.Hatzirodos N., Hummitzsch K., Irving-Rodgers H.F., Harland M.L., Morris S.E., Rodgers R.J. Transcriptome profiling of granulosa cells from bovine ovarian follicles during atresia. BMC Genomics. 2014;15:40. doi: 10.1186/1471-2164-15-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kasik J., Rice E. Selenoprotein P expression in liver, uterus and placenta during late pregnancy. Placenta. 1995;16:67–74. doi: 10.1016/0143-4004(95)90082-9. [DOI] [PubMed] [Google Scholar]
- 73.Galton V.A., Martinez E., Hernandez A., St. Germain E.A., Bates J.M., St. Germain D.L. The type 2 iodothyronine deiodinase is expressed in the rat uterus and induced during pregnancy. Endocrinology. 2001;142:2123–2128. doi: 10.1210/endo.142.5.8169. [DOI] [PubMed] [Google Scholar]
- 74.Koopdonk-Kool J.M., De Vijlder J., Veenboer G.J., Ris-Stalpers C., Kok J.H., Vulsma T., Boer K., Visser T.J. Type II and type III deiodinase activity in human placenta as a function of gestational age. J. Clin. Endocrinol. Metab. 1996;81:2154–2158. doi: 10.1210/jcem.81.6.8964844. [DOI] [PubMed] [Google Scholar]
- 75.Ejima K., Koji T., Nanri H., Kashimura M., Ikeda M. Expression of thioredoxin and thioredoxin reductase in placentae of pregnant mice exposed to lipopolysaccharide. Placenta. 1999;20:561–566. doi: 10.1053/plac.1999.0415. [DOI] [PubMed] [Google Scholar]
- 76.Ejima K., Nanri H., Toki N., Kashimura M., Ikeda M. Localization of thioredoxin reductase and thioredoxin in normal human placenta and their protective effect against oxidative stress. Placenta. 1999;20:95–101. doi: 10.1053/plac.1998.0338. [DOI] [PubMed] [Google Scholar]
- 77.Basini G., Tamanini C. Selenium stimulates estradiol production in bovine granulosa cells: possible involvement of nitric oxide. Domes. Anim. Endocrinol. 2000;18:1–17. doi: 10.1016/S0739-7240(99)00059-4. [DOI] [PubMed] [Google Scholar]
- 78.Grazul-Bilska A.T., Caton J.S., Arndt W., Burchill K., Thorson C., Borowczyk E., Bilski J.J., Redmer D.A., Reynolds L.P., Vonnahme K.A. Cellular proliferation and vascularization in ovine fetal ovaries: Effects of undernutrition and selenium in maternal diet. Reproduction. 2009;137:699–707. doi: 10.1530/REP-08-0375. [DOI] [PubMed] [Google Scholar]
- 79.Kamada H., Ikumo H. Effect of selenium on cultured bovine luteal cells. Anim. Reprod. Sci. 1997;46:203–211. doi: 10.1016/S0378-4320(96)01617-X. [DOI] [PubMed] [Google Scholar]
- 80.Tilly J.L., Tilly K. Inhibitors of oxidative stress mimic the ability of follicle-stimulating hormone to suppress apoptosis in cultured rat ovarian follicles. Endocrinology. 1995;136:242–252. doi: 10.1210/endo.136.1.7828537. [DOI] [PubMed] [Google Scholar]
- 81.Grabek M., Swies Z., Borzecki A. The influence of selenium on the reproduction of rats. Eur. PMC. 1991;46:103–105. [PubMed] [Google Scholar]
- 82.Özkaya M.O., Nazıroğlu M., Barak C., Berkkanoglu M. Effects of multivitamin/mineral supplementation on trace element levels in serum and follicular fluid of women undergoing in vitro fertilization (IVF) Biol. Trace Elem. Res. 2011;139:1–9. doi: 10.1007/s12011-010-8637-x. [DOI] [PubMed] [Google Scholar]
- 83.Ruder E.H., Hartman T.J., Goldman M.B. Impact of oxidative stress on female fertility. Curr. Opin. Obstet. Gynecol. 2009;21:219–222. doi: 10.1097/GCO.0b013e32832924ba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mehdi Y., Hornick J.-L., Istasse L., Dufrasne I. Selenium in the environment, metabolism and involvement in body functions. Molecules. 2013;18:3292–3311. doi: 10.3390/molecules18033292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Edassery S.L., Shatavi S.V., Kunkel J.P., Hauer C., Brucker C., Penumatsa K., Yu Y., Dias J.A., Luborsky J.L. Autoantigens in ovarian autoimmunity associated with unexplained infertility and premature ovarian failure. Fertil. Steril. 2010;94:2636–2641. doi: 10.1016/j.fertnstert.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Singh A.K., Chattopadhyay R., Chakravarty B., Chaudhury K. Markers of oxidative stress in follicular fluid of women with endometriosis and tubal infertility undergoing IVF. Reprod. Toxicol. 2013;42:116–124. doi: 10.1016/j.reprotox.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 87.Coskun A., Arikan T., Kilinc M., Arikan D.C., Ekerbiçer H.Ç. Plasma selenium levels in Turkish women with polycystic ovary syndrome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013;168:183–186. doi: 10.1016/j.ejogrb.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 88.Luddi A., Capaldo A., Focarelli R., Gori M., Morgante G., Piomboni P., De Leo V. Antioxidants reduce oxidative stress in follicular fluid of aged women undergoing IVF. Reprod. Biol. Endocrinol. 2016;14:57. doi: 10.1186/s12958-016-0184-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jiménez Tuñón J.M., Trilles P.P., Molina M.G., Duvison M.H., Pastor B.M., Martín P.S., Martín F.S., Sánchez-Borrego R. A Double-Blind, Randomized Prospective Study to Evaluate the Efficacy of Previous Therapy With Melatonin, Myo-inositol, Folic Acid, and Selenium in Improving the Results of an Assisted Reproductive Treatment. Clin. Med. Insight. Ther. 2017;9:1179559X17742902. doi: 10.1177/1179559X17742902. [DOI] [Google Scholar]
- 90.Wilson R.L., Bianco-Miotto T., Leemaqz S.Y., Grzeskowiak L.E., Dekker G.A., Roberts C.T. Early pregnancy maternal trace mineral status and the association with adverse pregnancy outcome in a cohort of Australian women. J. Trace Elem. Med. Biol. 2018;46:103–109. doi: 10.1016/j.jtemb.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 91.Parman T., Wiley M.J., Wells P.G. Free radical-mediated oxidative DNA damage in the mechanism of thalidomide teratogenicity. Nat. Med. 1999;5:582–585. doi: 10.1038/8466. [DOI] [PubMed] [Google Scholar]
- 92.Winn L.M., Wells P.G. Maternal administration of superoxide dismutase and catalase in phenytoin teratogenicity1. Free Radical Biol. Med. 1999;26:266–274. doi: 10.1016/S0891-5849(98)00193-2. [DOI] [PubMed] [Google Scholar]
- 93.Thompson J. In vitro culture and embryo metabolism of cattle and sheep embryos—a decade of achievement. Anim. Reprod. Sci. 2000;60:263–275. doi: 10.1016/S0378-4320(00)00096-8. [DOI] [PubMed] [Google Scholar]
- 94.Uhm S.J., Gupta M.K., Yang J.H., Lee S.H., Lee H.T. Selenium improves the developmental ability and reduces the apoptosis in porcine parthenotes. Mol. Reprod. Dev. 2007;74:1386–1394. doi: 10.1002/mrd.20701. [DOI] [PubMed] [Google Scholar]
- 95.McKeehan W.L., Hamilton W.G., Ham R.G. Selenium is an essential trace nutrient for growth of WI-38 diploid human fibroblasts. Proc. Natl. Acad. Sci. 1976;73:2023–2027. doi: 10.1073/pnas.73.6.2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hewlett G. Strategies for optimising serum-free media. Cytotechnology. 1991;5:3–14. doi: 10.1007/BF00365530. [DOI] [PubMed] [Google Scholar]
- 97.Ufer C., Wang C.C. The roles of glutathione peroxidases during embryo development. Front. Mol. Neurosci. 2011;4:12. doi: 10.3389/fnmol.2011.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yoshida M., Ishigaki K., Nagai T., Chikyu M., Pursel V.G. Glutathione concentration during maturation and after fertilization in pig oocytes: relevance to the ability of oocytes to form male pronucleus. Biol. Reprod. 1993;49:89–94. doi: 10.1095/biolreprod49.1.89. [DOI] [PubMed] [Google Scholar]
- 99.Pierce G.B., Parchment R.E., Lewellyn A.L. Hydrogen peroxide as a mediator of programmed cell death in the blastocyst. Differentiation. 1991;46:181–186. doi: 10.1111/j.1432-0436.1991.tb00880.x. [DOI] [PubMed] [Google Scholar]
- 100.Parchment R. The implications of a unified theory of programmed cell death, polyamines, oxyradicals and histogenesis in the embryo. Int. J. Dev. Biol. 2003;37:75–83. [PubMed] [Google Scholar]
- 101.Abedelahi A., Salehnia M., Allameh A., Davoodi D. Sodium selenite improves the in vitro follicular development by reducing the reactive oxygen species level and increasing the total antioxidant capacity and glutathione peroxide activity. Hum. Reprod. 2010;25:977–985. doi: 10.1093/humrep/deq002. [DOI] [PubMed] [Google Scholar]
- 102.Abedelahi A., Salehnia M., Allameh A. The effects of different concentrations of sodium selenite on the in vitro maturation of preantral follicles in serum-free and serum supplemented media. J. Assist. Reprod. Genet. 2008;25:483–488. doi: 10.1007/s10815-008-9252-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shi L., Ren Y., Zhang C., Yue W., Lei F. Effects of organic selenium (Se-enriched yeast) supplementation in gestation diet on antioxidant status, hormone profile and haemato-biochemical parameters in Taihang Black Goats. Anim. Feed Sci. Technol. 2018;238:57–65. doi: 10.1016/j.anifeedsci.2018.02.004. [DOI] [Google Scholar]
- 104.Dalto B., Tsoi S., Audet I., Dyck M.K., Foxcroft G., Matte J.J. Gene expression of porcine blastocysts from gilts fed organic or inorganic selenium and pyridoxine. Reproduction. 2015;149:31–42. doi: 10.1530/REP-14-0408. [DOI] [PubMed] [Google Scholar]
- 105.Dalto D.B., Audet I., Lapointe J., Matte J.J. The importance of pyridoxine for the impact of the dietary selenium sources on redox balance, embryo development, and reproductive performance in gilts. J. Trace Elem. Med. Biol. 2016;34:79–89. doi: 10.1016/j.jtemb.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 106.Dalto D.B., Roy M., Audet I., Palin M.-F., Guay F., Lapointe J., Matte J.J. Interaction between vitamin B6 and source of selenium on the response of the selenium-dependent glutathione peroxidase system to oxidative stress induced by oestrus in pubertal pig. J. Trace Elem. Med. Biol. 2015;32:21–29. doi: 10.1016/j.jtemb.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 107.Fortier M.E., Audet I., Giguere A., Laforest J.P., Bilodeau J.F., Quesnel H., Matte J.J. Effect of dietary organic and inorganic selenium on antioxidant status, embryo development, and reproductive performance in hyperovulatory first-parity gilts. J. Anim. Sci. 2012;90:231–240. doi: 10.2527/jas.2010-3340. [DOI] [PubMed] [Google Scholar]
- 108.Chen J., Han J., Guan W., Chen F., Wang C., Zhang Y., Lv Y., Lin G. Selenium and vitamin E in sow diets: I. Effect on antioxidant status and reproductive performance in multiparous sows. Anim. Feed Sci. Technol. 2016;221:111–123. doi: 10.1016/j.anifeedsci.2016.08.022. [DOI] [Google Scholar]
- 109.Nogales F., Ojeda M.L., Fenutría M., Murillo M.L., Carreras O. Role of selenium and glutathione peroxidase on development, growth, and oxidative balance in rat offspring. Reproduction. 2013;146:659–667. doi: 10.1530/REP-13-0267. [DOI] [PubMed] [Google Scholar]
- 110.Khera A., Dong L.-F., Holland O., Vanderlelie J., Pasdar E.A., Neuzil J., Perkins A.V. Selenium supplementation induces mitochondrial biogenesis in trophoblasts. Placenta. 2015;36:863–869. doi: 10.1016/j.placenta.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 111.Khera A., Vanderlelie J.J., Holland O., Perkins A.V. Overexpression of endogenous anti-oxidants with selenium supplementation protects trophoblast cells from reactive oxygen species-induced apoptosis in a Bcl-2-dependent manner. Biol. Trace Elem. Res. 2017;177:394–403. doi: 10.1007/s12011-016-0870-5. [DOI] [PubMed] [Google Scholar]
- 112.Perkins A., Khera A., Holland O., Vanderlelie J. Trophoblast mitochondrial biogenesis and functionality is increased with selenium supplementation. Placenta. 2016;45:118. doi: 10.1016/j.placenta.2016.06.197. [DOI] [Google Scholar]
- 113.Mendelev N., Mehta S.L., Idris H., Kumari S., Li P.A. Selenite stimulates mitochondrial biogenesis signaling and enhances mitochondrial functional performance in murine hippocampal neuronal cells. PLoS One. 2012;7:e47910. doi: 10.1371/journal.pone.0047910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Na J.Y., Seok J., Park S., Kim J.S., Kim G.J. Effects of selenium on the survival and invasion of trophoblasts. Clin. Exp. Reprod. Med. 2018;45:10–16. doi: 10.5653/cerm.2018.45.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fialova L., Malbohan I., Kalousova M., Soukupova J., Krofta L., Štipek S., Zima T. Oxidative stress and inflammation in pregnancy. Scand. J. Clin. Lab. INVEST. 2006;66:121–128. doi: 10.1080/00365510500375230. [DOI] [PubMed] [Google Scholar]
- 116.Orhan H., Önderoglu L., Yücel A., Sahin G. Circulating biomarkers of oxidative stress in complicated pregnancies. Arch. Gynecol. Obst. 2003;267:189–195. doi: 10.1007/s00404-002-0319-2. [DOI] [PubMed] [Google Scholar]
- 117.Karowicz-Bilinska A., Kędziora-Kornatowska K., Bartosz G. Indices of oxidative stress in pregnancy with fetal growth restriction. Free Radical Res. 2007;41:870–873. doi: 10.1080/10715760701291647. [DOI] [PubMed] [Google Scholar]
- 118.Hracsko Z., Orvos H., Novak Z., Pal A., Varga I.S. Evaluation of oxidative stress markers in neonates with intra-uterine growth retardation. Redox Rep. 2008;13:11–16. doi: 10.1179/135100008X259097. [DOI] [PubMed] [Google Scholar]
- 119.Mariath A.B., Bergamaschi D.P., Rondó P.H., Ana C.A.T., de Fragas Hinnig P., Abbade J.F., Diniz S.G. The possible role of selenium status in adverse pregnancy outcomes. Br. J. Nutr. 2011;105:1418–1428. doi: 10.1017/S0007114510005866. [DOI] [PubMed] [Google Scholar]
- 120.Richard K., Holland O., Landers K., Vanderlelie J.J., Hofstee P., Cuffe J.S., Perkins A.V. Effects of maternal micronutrient supplementation on placental function. Placenta. 2017;54:38–44. doi: 10.1016/j.placenta.2016.12.022. [DOI] [PubMed] [Google Scholar]
- 121.Mamon M.A.C., Ramos G.B. Maternal selenium-supplementation at various stages of periconception period: influence on murine blastocyst morphology and implantation status. J. Anim. Sci. Technol. 2017;59:7. doi: 10.1186/s40781-017-0132-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cetin I., Berti C., Calabrese S. Role of micronutrients in the periconceptional period. Hum. Reprod. Update. 2009;16:80–95. doi: 10.1093/humupd/dmp025. [DOI] [PubMed] [Google Scholar]
- 123.Berti C., Biesalski H., Gärtner R., Lapillonne A., Pietrzik K., Poston L., Redman C., Koletzko B., Cetin I. Micronutrients in pregnancy: current knowledge and unresolved questions. Clin. Nutr. 2011;30:689–701. doi: 10.1016/j.clnu.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 124.Ambroziak U., Hybsier S., Shahnazaryan U., Krasnodębska-Kiljańska M., Rijntjes E., Bartoszewicz Z., Bednarczuk T., Schomburg L. Severe selenium deficits in pregnant women irrespective of autoimmune thyroid disease in an area with marginal selenium intake. J. Trace Elem. Med. Biol. 2017;44:186–191. doi: 10.1016/j.jtemb.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 125.Polanska K., Krol A., Sobala W., Gromadzinska J., Brodzka R., Calamandrei G., Chiarotti F., Wasowicz W., Hanke W. Selenium status during pregnancy and child psychomotor development—Polish Mother and Child Cohort study. Pediatr. Res. 2016;79:863. doi: 10.1038/pr.2016.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Butler J.A., Whanger P.D., Tripp M.J. Blood selenium and glutathione peroxidase activity in pregnant women: comparative assays in primates and other animals. Am. J. Clin. Nutr. 19821982;36:15–23. doi: 10.1093/ajcn/36.1.15. [DOI] [PubMed] [Google Scholar]
- 127.Zachara B., Wardak C., Didkowski W., Maciag A., Marchaluk E. Changes in blood selenium and glutathione concentrations and glutathione peroxidase activity in human pregnancy. Gynecol. Obst. Invest. 1993;35:12–17. doi: 10.1159/000292655. [DOI] [PubMed] [Google Scholar]
- 128.Jarvis S., Glinianaia S.V., Torrioli M.-G., Platt M.-J., Miceli M., Jouk P.-S., Johnson A., Hutton J., Hemming K., Hagberg G. Cerebral palsy and intrauterine growth in single births: European collaborative study. The Lancet. 2003;362:1106–1111. doi: 10.1016/S0140-6736(03)14466-2. [DOI] [PubMed] [Google Scholar]
- 129.Dikbas L., Yapca O.E., Dikbas N., Gundogdu C. Paraoxonase-2 and paraoxonase-3: comparison of mRNA expressions in the placentae of unexplained intrauterine growth restricted and noncomplicated pregnancies. J. Mat.-Fet. Neonatal Med. 2017;30:1200–1206. doi: 10.1080/14767058.2016.1209480. [DOI] [PubMed] [Google Scholar]
- 130.Takagi Y., Nikaido T., Toki T., Kita N., Kanai M., Ashida T., Ohira S., Konishi I. Levels of oxidative stress and redox-related molecules in the placenta in preeclampsia and fetal growth restriction. Virchows Arch. 2004;444:49–55. doi: 10.1007/s00428-003-0903-2. [DOI] [PubMed] [Google Scholar]
- 131.Mesdaghinia E., Rahavi A., Bahmani F., Sharifi N., Asemi Z. Clinical and Metabolic Response to Selenium Supplementation in Pregnant Women at Risk for Intrauterine Growth Restriction: Randomized, Double-Blind, Placebo-Controlled Trial. Biol. Trace Elem. Res. 2017;178:14–21. doi: 10.1007/s12011-016-0911-0. [DOI] [PubMed] [Google Scholar]
- 132.Barrington J., Lindsay P., James D., Smith S., Roberts A. Selenium deficiency and miscarriage: A possible link? Int. J. Obstet. Gynaecol. 1996;103:130–132. doi: 10.1111/j.1471-0528.1996.tb09663.x. [DOI] [PubMed] [Google Scholar]
- 133.Koçak İ., Aksoy E., Üstün C. Recurrent spontaneous abortion and selenium deficiency. Int. J. Obstet. Gynaecol. 1999;65:79–80. doi: 10.1016/S0020-7292(99)00022-3. [DOI] [PubMed] [Google Scholar]
- 134.Mistry H.D., Kurlak L.O., Young S.D., Briley A.L., Broughton Pipkin F., Baker P.N., Poston L. Maternal selenium, copper and zinc concentrations in pregnancy associated with small-for-gestational-age infants. Mat. Child Nutr. 2014;10:327–334. doi: 10.1111/j.1740-8709.2012.00430.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Negro R., Greco G., Mangieri T., Pezzarossa A., Dazzi D., Hassan H. The influence of selenium supplementation on postpartum thyroid status in pregnant women with thyroid peroxidase autoantibodies. J. Clin. End. Metab. 2007;92:1263–1268. doi: 10.1210/jc.2006-1821. [DOI] [PubMed] [Google Scholar]
- 136.Rayman M.P. Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proc. Nutr. Soci. 2018:1–11. doi: 10.1017/S0029665118001192. [DOI] [PubMed] [Google Scholar]
- 137.Brigelius-Flohé R., Arnér E.S. Selenium and selenoproteins in (redox) signaling, diseases, and animal models-200 year anniversary issue. Eur. PMC. 2018;127:1–2. doi: 10.1016/j.freeradbiomed.2018.09.026. [DOI] [PubMed] [Google Scholar]
- 138.Wu W., Wang Q., Yin F., Yang Z., Zhang W., Gabra H., Li L. Identification of proteomic and metabolic signatures associated with chemoresistance of human epithelial ovarian cancer. Int. J. Clin. Oncol. 2016;49:1651–1665. doi: 10.3892/ijo.2016.3652. [DOI] [PubMed] [Google Scholar]
- 139.Agnani D., Camacho-Vanegas O., Camacho C., Lele S., Odunsi K., Cohen S., Dottino P., Martignetti J.A. Decreased levels of serum glutathione peroxidase 3 are associated with papillary serous ovarian cancer and disease progression. J. Ovarian Res. 2011;4:18. doi: 10.1186/1757-2215-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Piekutowski K., Makarewicz R., Zachara B. The antioxidative role of selenium in pathogenesis of cancer of the female reproductive system. Neoplasma. 2007;54:374–378. [PubMed] [Google Scholar]
- 141.Falck E., Karlsson S., Carlsson J., Helenius G., Karlsson M., Klinga-Levan K. Loss of glutathione peroxidase 3 expression is correlated with epigenetic mechanisms in endometrial adenocarcinoma. Cancer Cell Int. 2010;10:46. doi: 10.1186/1475-2867-10-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Saga Y., Ohwada M., Suzuki M., Konno R., Kigawa J., Ueno S., Mano H. Glutathione peroxidase 3 is a candidate mechanism of anticancer drug resistance of ovarian clear cell adenocarcinoma. Oncol. Rep. 2008;20:1299–1303. doi: 10.3892/or_00000144. [DOI] [PubMed] [Google Scholar]
- 143.Lee H.J., Do J.H., Bae S., Yang S., Zhang X., Lee A., Choi Y.J., Park D.C., Ahn W.S. Immunohistochemical evidence for the over-expression of Glutathione peroxidase 3 in clear cell type ovarian adenocarcinoma. Med. Oncol. 2011;28:010–9659. doi: 10.1007/s12032-010-9659-0. [DOI] [PubMed] [Google Scholar]
- 144.Hough C.D., Cho K.R., Zonderman A.B., Schwartz D.R., Morin P.J. Coordinately up-regulated genes in ovarian cancer. Cancer Res. 2001;61:3869–3876. [PubMed] [Google Scholar]
- 145.Rayman M.P., Winther K.H., Pastor-Barriuso R., Cold F., Thvilum M., Stranges S., Guallar E., Cold S. Effect of long-term selenium supplementation on mortality: results from a multiple-dose, randomised controlled trial. Free Radical Biol. Med. 2018 doi: 10.1016/j.freeradbiomed.2018.02.015. [DOI] [PubMed] [Google Scholar]