Abstract
Objective:
Maternal return to work within 12 weeks of delivery is associated with poor child health and development. However, little is known about the impact of return to work on child obesity risk. We examined whether timing of maternal return to work is associated with rapid infant weight gain from 0–6 months and weight-for-length at 1 year.
Methods:
Secondary data analysis of 279 mother-newborn dyads from the INSIGHT Study, a randomized controlled trial evaluating a responsive parenting (RP) intervention. Rapid infant weight gain from 0–6 months was assessed using conditional weight gain scores. Infant weight-for-length was calculated using World Health Organization reference values. Analysis of variance (ANOVA) examined whether infant weight outcomes differed by timing of maternal return to work (≤12 weeks vs. >12 weeks after delivery). Moderation by study group (RP intervention vs. safety control) and mediation by breastmilk feeding were examined in ANOVA models.
Results:
Among 261 mothers approximately half (n=130) returned to work within 12 weeks. Compared to infants of mothers who returned to work after 12 weeks, infants of mothers who returned to work within 12 weeks had higher conditional weight gain scores from 0–6 months (p = 0.006) and were heavier at 1 year (p = 0.05). These associations were not moderated by study group or mediated by breastmilk feeding.
Conclusion:
Maternal return to work within 12 weeks was associated with rapid infant weight gain in the first 6 months and higher weight-for-length at 1 year, though the mechanisms to explain our findings are unclear.
Keywords: maternal employment, Family and Medical Leave Act, rapid weight gain, infant growth, childhood obesity
Introduction
Women make up nearly half of the paid workforce, and the number of dual-income families is rising.1 Following childbirth, 41% of mothers return to work within 12 weeks and the majority are working within a year.2 The federally-mandated Family and Medical Leave Act (FMLA) of 1993 allows up to 12 weeks of job-protected leave for childbearing or family care.3 However, only 56% of employed mothers qualify for FMLA,4 and many eligible employees cannot afford to take unpaid leave.5 This is unfortunate because return to work within 12 weeks of giving birth is associated with poorer child health and development.6, 7 For example, using propensity score-matched samples and adjusting for demographic and state-level controls (e.g., unemployment), maternal return to work within 12 weeks of delivery was associated with a greater likelihood of behavioral problems at age 4 and reduced child immunizations.7
Child obesity risk is positively associated with the number of maternal hours worked8–10 and maternal employment duration across childhood.11–13 However, it remains unclear whether the timing of mothers’ return to work is associated with obesity risk early in life. Although maternal employment is often associated with use of childcare,14 they are not the same construct. This is evidenced by US data showing that 12.3% of employed mothers do not have regular childcare arrangements, whereas 28.2% of unemployed mothers do in fact utilize childcare on a regular basis.14 Recent reviews report inconsistent evidence for a relationship between childcare and obesity risk,15, 16 which may be because few studies examine the timing of childcare initiation.17–19 Though childcare initiation may be similar to timing of return to work, to inform family leave policies, an important question is whether return to work within the timeframe allotted by FMLA is associated with weight outcomes such as rapid infant weight gain, which is a risk factor for later obesity20 and obesity-related comorbidities.21
The aim of this secondary data analysis was to examine whether infant weight outcomes differ by the timing of maternal return to work after delivery (≤12 weeks vs. >12 weeks) among participants in the Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) Study.22 We hypothesized that infants of mothers who returned to work within 12 weeks would be more likely to experience rapid weight gain from 0–6 months and weigh more at 1 year. Previous research has shown associations between demographic characteristics and infant weight,23, 24 thus we examined potential confounding effects of maternal age, pre-pregnancy body mass index (BMI), and socioeconomic and marital status. Given previously reported positive effects of the INSIGHT responsive parenting (RP) intervention on early life weight outcomes,25, 26 we explored study group (RP intervention vs. control) as a potential moderator. Return to work is associated with shorter breastfeeding duration.27,28 The protective association of breastfeeding duration appears to be more consistent when exclusivity of breastfeeding is known.29 Thus, we examined whether breastmilk feeding duration and/or exclusivity were associated with infant weight outcomes and whether these variables mediated the association between return to work and weight outcomes.
Methods
Study Design and Participants
The current study is a secondary data analysis of INSIGHT, a randomized controlled trial evaluating a multi-component RP intervention designed to prevent rapid infant weight gain and childhood obesity among first-born infants.22 Mother-infant dyads were recruited from a maternity ward in Central Pennsylvania. First-time mothers were eligible for the study if they were English-speaking, ≥20 years of age, and their newborns were full-term (≥37 weeks’ gestation), singleton and weighed ≥2500g at birth. Mother-infant dyads were randomized 2 weeks after delivery into two study arms (i.e., RP intervention or safety control), stratified by birth weight-for-gestational age (<50th percentile or ≥50th percentile) and intended feeding mode (breastfeeding or formula). Trained nurses delivered intervention components during home visits at infant ages 3–4 weeks, 16 weeks, 28 weeks, and 40 weeks, and at clinic visits at 1 year. Enrollment and data collection through 1 year spanned January 2012 to March 2015. Of the 279 mother-infant dyads who participated in the 3–4 week home visit, the present study included participants with data on return to work after delivery (n=261). Additional details regarding study procedures, recruitment and eligibility criteria have previously been published.22 This study was approved by the Human Subjects Protection Office of the Penn State College of Medicine and registered at http://www.clinicaltrials.gov prior to participant enrollment.
Measures
Background Characteristics
Demographic information was collected from participants at enrollment (e.g., race/ethnicity, household income, marital status). Data extracted from medical records included maternal age, pre-pregnancy weight (kilograms), infant gestational age, sex, birth weight, and length. Maternal height was measured in duplicate to the nearest 0.1 cm or extracted from medical records, and used to calculate pre-pregnancy BMI (kg/m2).
Infant Anthropometrics
Nurses measured infant weight and recumbent length at home visits prior to age 1 year. At the 1-year visit, research nurses blinded to study condition measured anthropometrics. Weight was measured to the nearest 0.01 kg using an electronic scale (Seca 354). Recumbent length was measured to the nearest 0.1 cm with a portable stadiometer (Shorr productions). Weight and length were measured in duplicate and a third measurement was obtained if the two values differed by more than 0.05 kg for weight or 1 cm for height. The average of measurements was used for analyses. Height and weight were plotted over the course of the study, and at no point were any values considered implausible. Weight-for-length was converted to percentiles and z-scores using the World Health Organization growth charts.30
Rapid weight gain from birth to six months (28 weeks) was assessed using conditional weight gain scores (CWG).25 Based on previously described procedures,31 CWG scores were calculated as the standardized residuals of weight-for-age at 28 weeks regressed on weight-for-age at birth, adjusting for length-for-age at birth and 28 weeks and infant age at the 28-week study visit. CWG is normally distributed with a mean of 0 and standard deviation of 1. Positive CWG scores indicate relatively faster weight gain, whereas negative CWG scores indicate relatively slower weight gain compared to the sample mean.
Timing of return to work
Maternal employment was assessed at 8- and 20-weeks from phone interviews. Mothers who were working outside of the home indicated the date that they returned to work. Timing of mothers’ return to work was dichotomized into two groups: 1) mothers who returned to work ≤12 weeks after delivery and 2) mothers who returned to work >12 weeks or not at all. 12 weeks was chosen, as it is the length of maternity leave allowed by FMLA.3
Potential moderators and mediators
Because infants in the RP intervention had lower mean CWG from birth to six months and a reduced prevalence of overweight at 1 year compared to infants in the control group,25 study group was included in all analyses with weight outcomes. At 2, 8, and 20 weeks mothers were asked whether they were currently breastfeeding. If not currently breastfeeding, mothers indicated their child’s age when they stopped breastfeeding. In line with previous studies,32, 33 a dichotomous variable for breastfeeding duration was created (<4 months vs. ≥4 months). The number of feedings as breastmilk or formula was measured at 16 and 28 weeks using a modified food frequency questionnaire from the Infant Feeding Practices Study 2.34 Exclusive breastmilk feeding was defined as 100% of milk feedings (at the breast or by bottle) as breastmilk with all other cases defined as not exclusively fed breastmilk. Additionally, mothers who were exclusively breastmilk feeding at 2 weeks were asked how long they intended to breastfeed.
Statistical Analysis
Analysis of variance (ANOVA) was used to determine whether timing of return to work was associated with infant weight outcomes. We examined mean differences in the following weight outcomes by maternal return to work at ≤12 weeks or not: 1) CWG from 0–6 months and 2) weight-for-length percentiles and z-scores at 1 year. Maternal age, pre-pregnancy BMI, household income, education, and marital status were explored as potential covariates. A Kolmogorov-Smirnov 2-sample test was used to determine whether there was a significant difference in the distribution of CWG by timing of return to work. To test whether the association between timing of return to work and infant weight outcomes differed for infants in the RP intervention versus the control group, study group was examined as a moderator by adding an interaction term to the ANOVA models. Analyses examining breastmilk feeding duration and exclusive breastmilk feeding as mediators of the association between return to work and weight outcomes were conducted using the Sobel test.35
ANOVAs were performed using all available cases for each weight outcome. This resulted in 256 cases in analyses examining CWG and 250 cases in analyses examining 1-year weight-for-length. Sensitivity analyses were conducted by excluding each of the following subgroups: 1) mothers who dropped from the study before 1 year (n=29), 2) mothers who indicated they returned to school (n=11), and 3) mothers who had not returned to work by 1 year (n=55). Exclusion of these cases did not change results, thus all available cases were included in the present analyses. All analyses were conducted using the SAS software, version 9.4 (SAS Institute).
Results
Approximately half (n=130) of mothers returned to work by the time their child was 12 weeks old, with 15 of these mothers returning by 6 weeks. Among 131 mothers who did not return to work by 12 weeks, 64 returned between 12 and 28 weeks, 5 returned between 28 weeks and 1 year, and 55 mothers had not returned by 1 year. An additional 7 mothers had missing employment data after 12 weeks. Sample demographics by maternal return to work are shown in Table 1. The majority of mothers were Non-Hispanic White (87%), married (75%), college graduates (64%), and reported an annual household income ≥$50,000 (75%). Compared to mothers who returned to work after 12 weeks, mothers who returned to work within 12 weeks were less likely to exclusively feed breastmilk at 16 (p=0.04) and 28 (p=0.004) weeks, fed breastmilk for a shorter duration (M=6.1 ± 5.6 vs. M=8.3 ± 6.4 months, p=0.004), and introduced a bottle earlier (M=8.7 ± 12.8 vs. M=13.8 ± 18.6 days, p=0.01). Among mothers who were exclusively breastmilk feeding at 2 weeks, there was no difference in their intended duration to breastfeed by timing of return to work (p=0.73) or in the percent who met or exceeded their breastfeeding duration goal (p=0.46).
Table 1.
Demographic characteristics by maternal return to work status (n=261)
| Characteristic | Returned ≤12 weeks (n=130) |
Returned >12 weeks/not at all (n=131) |
|---|---|---|
| Mother | ||
| Age, mean (SD), y | 28.6 (4.6) | 29 (4.8) |
| Pre-pregnancy BMI, mean (SD)* | 26.3 (5.9) | 24.7 (4.6) |
| Non-Hispanic White, No. (%) | 123 (94.6) | 119 (91.5) |
| Married, No. (%) | 98 (75.4) | 101 (77.1) |
| Annual household income, No. (%), $ | ||
| <$10,000 | 2 (1.5) | 7 (5.3) |
| $10,000-$24,999 | 6 (4.6) | 10 (7.6) |
| $25,000-$49,999 | 17 (13.1) | 10 (7.6) |
| $50,000-$74,999 | 34 (26.2) | 33 (25.2) |
| $75,000-$99,999 | 29 (22.3) | 25 (19.1) |
| >$100,000 | 35 (26.9) | 37 (28.2) |
| Don’t know/decline to answer | 7 (5.4) | 9 (6.9) |
| Education, No. (%) | ||
| High school graduate or less | 15 (11.5) | 11 (8.4) |
| Some college | 32 (24.6) | 35 (26.7) |
| College graduate | 48 (36.9) | 50 (38.2) |
| Graduate degree or higher | 35 (26.9) | 35 (26.7) |
| Infant | ||
| Male sex, No. (%) | 65 (50.0) | 69 (52.7) |
| Gestational age, mean (SD), wk | 39.6 (1.2) | 39.5 (1.2) |
| Birth weight, mean (SD), kg | 3.5 (0.5) | 3.4 (0.4) |
| Birth length, mean (SD), cm | 50.9 (2.3) | 50.9 (2.4) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
p=0.03
Maternal age, race/ethnicity, marital status, education, and household income did not differ by return to work and were not associated with infant weight outcomes. Mothers who returned within 12 weeks were more likely to have overweight or obesity compared to mothers who did not return by 12 weeks (48% vs. 35%, p=0.03, Table 1). Pre-pregnancy BMI was not associated with CWG or weight-for-length at 1 year, and controlling for pre-pregnancy BMI did not change the associations between return to work and weight outcomes (data not shown). More parsimonious models excluding potential covariates and pre-pregnancy BMI are presented.
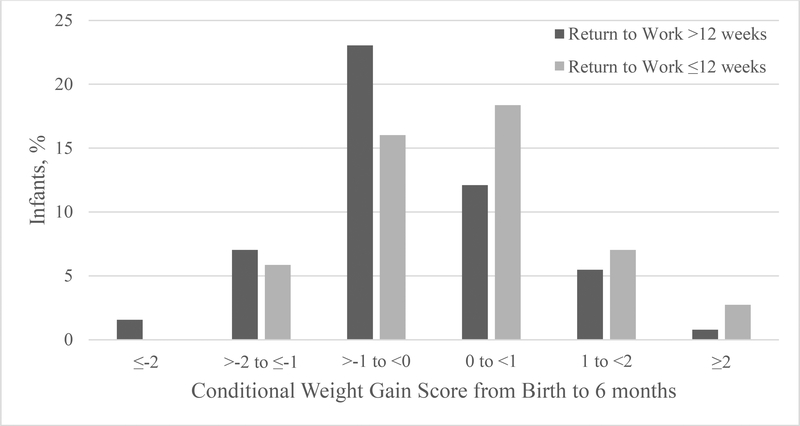
Infants of mothers who returned to work within 12 weeks experienced faster than average weight gain from 0–6 months [M {95%CI}=0.16 {−0.01–0.34}] compared to infants of mothers who did not return within 12 weeks, who had slower than average weight gain (M{95%CI}=−0.18 {−0.35–0.00}; F=7.67, p=0.006). Figure 1 illustrates that compared to infants of mothers who returned to work after 12 weeks, the distribution of CWG for infants of mothers who returned to work within 12 weeks was shifted to the right, indicating faster weight gain among this group (Kolmogorov-Smirnov asymptotic test, 0.2, p=0.01). CWG does not intuitively translate to child weight gain and may be difficult to interpret.31 Comparing mean weight gain from 0–6 months between the two groups can serve as a proxy for the effect size. Infants of mothers who returned within 12 weeks had a mean weight gain of 4.62 kg from 0–6 months, whereas infants of mothers who returned after 12 weeks had a mean weight gain of 4.44 kg; a difference of 0.18 kg. Study group did not moderate the association between return to work and CWG (F=0.14, p=0.71), suggesting that the RP intervention was effective in reducing rapid weight gain during the first six months regardless of whether mothers returned to work within 12 weeks. Breastmilk feeding duration <4 months and exclusive breastmilk feeding at 16 weeks were not associated with CWG and did not mediate the relationship between return to work and CWG (Breastmilk feeding duration <4 months Sobel test p=0.94; Exclusive breastmilk feeding at 16 weeks Sobel test p=0.31).
Figure 1.
Conditional weight gain from birth to 6 months by maternal return to work (p=0.01)
Infants of mothers who returned to work after 12 weeks had lower conditional weight gain scores indicating slower weight gain from birth to 6 months. Conditional weight gain scores greater than 0 reflect more rapid weight gain (Kolmogorov-Smirnov asymptotic test, 0.2, p=0.01).
Weight-for-length percentiles at 1 year were higher for infants of mothers who returned to work within 12 weeks [M {95%CI}=64.2 {59.5–69.0}] compared to infants of mothers who did not return within 12 weeks [M {95%CI}=57.7 {59.5–69.0}; F=3.74, p=0.05], though both groups were classified on average as normal weight (weight-for-length percentile <85th percentile).The association between timing of return to work and weight-for-length percentile at 1 year was not moderated by study group (F=0.11, p=0.74). Breastmilk feeding duration <4 months was not associated with weight-for-length percentile. Controlling for study group, infants who were exclusively fed breastmilk at 16 weeks had a lower weight-for-length percentile at 1 year [M {95%CI}=56.1 {50.8–61.3}] compared to infants who were not exclusively fed breastmilk [M {95%CI}=63.9 {59.6–68.2}; F=4.85, p=0.01]. Although exclusive breastmilk feeding attenuated the association between return to work and weight-for-length percentile (p=0.05 to p=0.11), exclusive breastmilk feeding did not mediate this relationship (Sobel test p=0.16). . Results at 1-year were similar when examining weight-for-length z-scores instead of percentiles and when using duration of breastmilk feeding <6 months and exclusive breastmilk feeding at 28 weeks (data not shown).
Discussion
In this secondary analysis, infants of mothers who returned to work within 12 weeks of delivery gained weight more rapidly from 0–6 months and were heavier at 1 year compared to infants whose mothers returned to work after 12 weeks or not at all. Previous studies show that maternal return to work within the first 12 weeks after delivery is negatively associated with child health and development.7 We provide initial evidence that an earlier return to work may increase the risk for rapid infant weight gain and higher weight-for-length at 1 year. Although the observed difference in weight gain by return to work was small (i.e., 0.18 kg), it may be of public health importance at a population level given the potential for improvements in US parental leave policies (e.g., longer duration, paid leave). Rapid infant weight gain is an undesirable early growth pattern,20, 36 thus our results add to evidence supporting the need to reevaluate existing policies. The US is the only developed country that does not offer paid maternity leave, and compared to other developed countries the length of leave provided at a national level is the shortest across all types of leave.37 In contrast, Sweden, Norway, and Denmark provide 68, 52, and 28 weeks of paid leave, respectively.37 These countries have substantially lower childhood obesity rates compared to the US. In the US, 17% of 2–19 yearolds have obesity38 compared to estimates that range between 2–5% in these Scandinavian countries.39, 40 Although other factors (e.g., nutrition environment, healthcare, poverty, breastfeeding rates) likely contribute to differing obesity rates between the US and Scandinavia, universal access to paid parental leave may be a contributor. It is important to consider differences in cultural values surrounding family policies. For example, Scandinavia has a history of generous work-family policies and a culture that supports women’s participation in the labor force.41 Further, breastfeeding is highly valued in these countries, which is reflected in higher breastfeeding rates compared to the US.42 Parental leave policies may benefit child health differently for countries that provide greater acceptance/support for breastfeeding compared to countries that do not.
Study group did not moderate the effect of return to work on infant weight outcomes. Regardless of timing of return to work, the INSIGHT RP intervention was effective in reducing rapid weight gain and weight-for-length at 1 year, a primary objective of the INSIGHT intervention.22 We found that mothers who returned to work within 12 weeks of delivery breastfed for a shorter duration and were less likely to exclusively breastfeed, consistent with a large body of work indicating that return to work and breastfeeding cessation are strongly linked.27 In our sample, duration of breastmilk feeding was not associated with infant weight outcomes. Exclusive breastmilk feeding at 16 weeks was not associated with rapid weight gain, but was associated with weight-for-length percentile at 1 year. However, exclusive breastmilk feeding did not mediate the association between return to work and 1-year weight-for-length. It is unclear whether the association between exclusive breastmilk feeding and weight-for-length in our sample was driven by greater intensity of feeding breastmilk or greater intensity of feeding at the breast. Due to our relatively small sample size and lack of adequate information related to bottle feeding at 16 weeks, we were not able to examine these differences.
Our findings are consistent with previous research showing associations between other aspects of maternal employment and higher BMI in children 3–15 years of age.8–13 Studies consistently show stronger positive associations between work hours and child overweight among Non-Hispanic White families and mothers with higher educational attainment,8, 9 sample populations with characteristics similar to the INSIGHT cohort. For example, Hawkins and colleagues9 found a greater likelihood of overweight among 3-year-olds for every 10 hours a mother worked per week; however, the association was only significant for children in households with annual income greater than $57,750. Maternal hours spent at work implies a trade-off between income and time engaged with the child. According to economic theories of parental leave, leave policies affect infant health by increasing parental time whereas they would only affect infant health outcomes through medical care or household commodities if policies increase income.43 For lower income families, the additional income from more working hours may outweigh negative outcomes associated with less parental time. On the other hand, higher income families may be better equipped to manage an income loss resulting from maternal time off for childbirth thus allowing one to see differences in child outcomes associated with parental time. Benefits to child health associated with greater parental time may be greater for a more educated compared to a less educated mother.44 We hypothesize that the association between return to work and infant weight outcomes would be null or attenuated among families with lower socioeconomic status.
Our results are also similar to findings from a study of childcare and infant weight.19 Kim and Peterson19 showed that infants who initiated childcare between 3–6 months, but not 0–3 or 6–12 months, gained more weight from birth to 9 months compared to infants in parental care. We extend these findings by showing that maternal return to work within 3 months is associated with infant weight through 1 year. Also in line with our results, feeding practices did not play a mediating role between childcare initiation and weight gain.19 It appears that the timing of return to work, which may also translate to childcare initiation for some dual-earner and single parent households, may play a role in obesity risk. We did not have adequate information in our sample regarding childcare arrangements to disentangle contributions of childcare and maternal employment to obesity risk. A future study specifically designed to investigate the effects of both maternal employment and childcare initiation on obesity risk is needed.
A strength of our study was examining return to work by the amount of leave allotted by FMLA. However, we were limited by not having access to mothers’ FMLA eligibility and utilization or employer provided leave. It is unknown whether mothers who returned within 12 weeks did so due to a lack of job-protected leave, or for other reasons (e.g., financial, career goals, social norms). Our results are intended to generate future research that specifically examines the association between return to work and infant weight as a function of parental leave policies. Additional limitations include a modest sample size and the inability to assess differences by socioeconomic status or race/ethnicity. Research with diverse samples is needed, particularly in high-risk samples given that low-income and ethnic minority children are disproportionately affected by obesity.45 Finally, our results may not be generalizable to mothers with multiple children, which is important to consider knowing that the proportion of mothers returning to work within the first 9 months after childbirth decreases after third or later born children compared to first or second births.2
In conclusion, infants of mothers who returned to work within 12 weeks after delivery experienced faster weight gain from 0–6 months and had higher weight-for-length at 1 year compared to infants of mothers who returned to work after 12 weeks or not at all. Our findings did not differ according to study group and although exclusive breastmilk feeding was associated with both return to work and weight at 1 year it did not mediate this relationship. Additional research examining other potential mechanisms (e.g., parent feeding styles, behaviors of other caregivers) that may explain the association between return to work within 12 weeks after delivery and infant weight outcomes is warranted.
Acknowledgements
The authors acknowledge Michele Marini, MS, Jessica Beiler, MPH, Jennifer Stokes, RN, Patricia Carper, RN, Amy Shelly, LPN, Gabrielle Murray, RN, Heather Stokes, Susan Rzucidlo, MSN, RN, and Lindsey Hess, MS for their assistance with this project.
Sally G. Eagleton –assisted with data analysis, drafted the manuscript, participated in critical revision of the manuscript, and approved the final manuscript as submitted.
Emily E. Hohman – led the data management, performed the data analyses, participated in critical revision of the manuscript, and approved the final manuscript as submitted.
Nicole Verdiglione- participated in data collection and critical revisions of the manuscript, and approved the final manuscript as submitted.
Leann L. Birch - co-led all aspects of the study concept, design, and analysis, participated in critical revision of the manuscript, and approved the final manuscript as submitted.
Ian M. Paul – co-led all aspects of the study concept, design, and analysis, participated in critical revisions of the manuscript, and approved the final manuscript as submitted.
Jennifer S. Savage – contributed to the design of the study, intervention curriculum development, assisted with data analysis, mentored graduate student in drafting the manuscript, participated in critical revision of the manuscript, and approved the final manuscript as submitted.
Funding Source: This research was supported by grant R01DK088244. Additional support was received from the Children’s Miracle Network at Penn State Children’s Hospital. USDA Grant #2011–67001-30117 supported graduate students. REDCap support was received from The Penn State Clinical & Translational Research Institute, Pennsylvania State University CTSA, NIH/NCATS Grant Number UL1 TR000127.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest relevant to this article.
Clinical Trial registry name and registration number: The Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) Study.
https://clinicaltrials.gov/ct2/show/NCT01167270. Registry number: NCT01167270. Registered 21 July 2010.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.The Council of Economic Advisers. The Economics of Paid and Unpaid Leave. In: States EOotPotU, editor.2014. p. 1–26.
- 2.Han WJ, Ruhm CJ, Waldfogel J, Washbrook E. The timing of mothers’ employment after childbirth. Mon Labor Rev. 2008;131:15–27. [PMC free article] [PubMed] [Google Scholar]
- 3.Family and Medical Leave Act of 1993. 29 USC §§ 2601–26542006. [Google Scholar]
- 4.Waldfogel J Family and medical leave: Evidence from the 2000 surveys. Mon Labor Rev. 2001;124:17–23. [Google Scholar]
- 5.Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101:217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baum CL. Does early maternal employment harm child development? An analysis of the potential benefits of leave taking. J Labor Econ. 2003;21:409–448. [Google Scholar]
- 7.Berger LM, Hill J, Waldfogel J. Maternity leave, early maternal employment and child health and development in the US. Econ J. 2005;115:F29–F47. [Google Scholar]
- 8.Anderson PM, Butcher KF, Levine PB. Maternal employment and overweight children. J Health Econ. 2003;22:477–504. [DOI] [PubMed] [Google Scholar]
- 9.Hawkins SS, Cole TJ, Law C. Maternal employment and early childhood overweight: findings from the UK Millennium Cohort Study. International Journal of Obesity. 2008;32:30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Datar A, Nicosia N, Shier V. Maternal work and children’s diet, activity, and obesity. Soc Sci Med. 2014;107:196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziol-Guest KM, Dunifon RE, Kalil A. Parental employment and children’s body weight: Mothers, others, and mechanisms. Soc Sci Med. 2013;95:52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hope S, Pearce A, Whitehead M, Law C. Parental employment during early childhood and overweight at 7-years: findings from the UK Millennium Cohort Study. BMC Obes. 2015;2:Epub 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrissey TW. Trajectories of growth in body mass index across childhood: Associations with maternal and paternal employment. Soc Sci Med. 2013;95:60–68. [DOI] [PubMed] [Google Scholar]
- 14.Laughlin L Who’s minding the kids? Child care arrangements: Spring 2011 In: Current Population Reports USCB, editor. Washington, DC: 2013. p. 27–135. [Google Scholar]
- 15.Black L, Matvienko‐Sikar K, Kearney P. The association between childcare arrangements and risk of overweight and obesity in childhood: a systematic review. Obes Rev. 2017;18(10):1170–1190. [DOI] [PubMed] [Google Scholar]
- 16.Swyden K, Sisson S, Lora K, Castle S, Copeland K. Association of childcare arrangement with overweight and obesity in preschool-aged children: a narrative review of literature. International Journal of Obesity. 2017;41(1):1. [DOI] [PubMed] [Google Scholar]
- 17.Lehto R, Mäki P, Ray C, Laatikainen T, Roos E. Childcare use and overweight in F inland: crosssectional and retrospective associations among 3‐and 5‐year‐old children. Pediatric obesity. 2016;11(2):136–143. [DOI] [PubMed] [Google Scholar]
- 18.Zahir N, Heyman M, Wojcicki J. No association between childcare and obesity at age 4 in lowincome L atino children. Pediatric obesity. 2013;8(2):e24–e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J, Peterson KE. Association of infant child care with infant feeding practices and weight gain among US infants. Archives of pediatrics & adolescent medicine. 2008;162(7):627–633. [DOI] [PubMed] [Google Scholar]
- 20.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331:929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardner DSL, Hosking J, Metcalf BS, Jeffery AN, Voss LD, Wilkin TJ. Contribution of Early Weight Gain to Childhood Overweight and Metabolic Health: A Longitudinal Study (EarlyBird 36). Pediatrics. 2009;123(1):e67–e73. [DOI] [PubMed] [Google Scholar]
- 22.Paul IM, Williams JS, Anzman-Frasca S, Beiler JS, Makova KD, Marini ME, et al. The Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) study. BMC Pediatr. 2014;14:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. [DOI] [PubMed] [Google Scholar]
- 24.Weng SF, Redsell SA, Swift JA, Yang M, Glazebrook CP. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child. 2012;97:10191026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Savage JS, Birch LL, Marini M, Anzman-Frasca S, Paul IM. Effect of the INSIGHT responsive parenting intervention on rapid infant weight gain and overweight status at age 1 year: A randomized clinical trial. JAMA Pediatr. 2016;170:742–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paul IM, Savage JS, Anzman-Frasca S, et al. Effect of a responsive parenting educational intervention on childhood weight outcomes at 3 years of age: The insight randomized clinical trial. JAMA. 2018;320(5):461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chatterji P, Frick K. Does returning to work after childbirth affect breastfeeding practices? Rev Econ Househ. 2005;3:315–335. [Google Scholar]
- 28.Fein SB, Roe B. The effect of work status on initiation and duration of breast-feeding. Am J Public Health. 1998;88:1042–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dewey KG. Is breastfeeding protective against child obesity? J Hum Lact. 2003;19:9–18. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization; WHO Child Growth Standards Length/height-for-age, weight-forage, weight-for-length, weight-for-height and body mass index-for-age. Department of Nutrition for Health and Development; 2006. [Google Scholar]
- 31.Griffiths LJ, Smeeth L, Hawkins SS, Cole TJ, Dezateux C. Effects of infant feeding practice on weight gain from birth to 3 years. Arch Dis Child. 2009;94:577–582. [DOI] [PubMed] [Google Scholar]
- 32.Gillman MW, Rifas-Shiman SL, Camargo CA Jr, Berkey CS, Frazier AL, Rockett HR, et al. Risk of overweight among adolescents who were breastfed as infants. JAMA. 2001;285(19):2461–2467. [DOI] [PubMed] [Google Scholar]
- 33.Harder T, Bergmann R, Kallischnigg G, Plagemann A. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 2005;162(5):397–403. [DOI] [PubMed] [Google Scholar]
- 34.Fein SB, Labiner-Wolfe J, Shealy KR, Li R, Chen J, Grummer-Strawn LM. Infant Feeding Practices Study II: study methods. Pediatrics. 2008;122 Suppl 2:S28–35. [DOI] [PubMed] [Google Scholar]
- 35.Jasti S, Dudley WN, Goldwater E. SAS Macros for Testing Statistical Mediation in Data With Binary Mediators or Outcomes. Nursing Research. 2008;57(2):118–122. [DOI] [PubMed] [Google Scholar]
- 36.Druet C, Stettler N, Sharp S, Simmons RK, Cooper C, Davey Smith G, et al. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr Perinat Epidemiol. 2012;26(1):19–26. [DOI] [PubMed] [Google Scholar]
- 37.Tanaka S Parental Leave and Child Health across OECD Countries. Econ J. 2005;115(501):F7–F28. [Google Scholar]
- 38.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014;384(9945):766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmidt Morgen C, Rokholm B, Sjoberg Brixval C, Schou Andersen C, Geisler Andersen L, Rasmussen M, et al. Trends in prevalence of overweight and obesity in danish infants, children and adolescents--are we still on a plateau? PloS one. 2013;8(7):e69860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Budig MJ, Misra J, Boeckmann I. The motherhood penalty in cross-national perspective: The importance of work–family policies and cultural attitudes. Soc Politics. 2012;19(2):163–193. [Google Scholar]
- 42.database OF. CO1.5 Breastfeeding rates. OECD Social Policy Division 2009. [Google Scholar]
- 43.Ruhm CJ. Parental leave and child health. J Health Econ. 2000;19(6):931–960. [DOI] [PubMed] [Google Scholar]
- 44.Fertig A, Glomm G, Tchernis R. The connection between maternal employment and childhood obesity: inspecting the mechanisms. Rev Econ Househ. 2009;7(3):227. [Google Scholar]
- 45.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the united states, 1988–1994 through 2013–2014. JAMA. 2016;315(21):22922299. [DOI] [PMC free article] [PubMed] [Google Scholar]