Abstract
Pancreatic cystic neoplasms (PCNs) are being increasingly detected because of rapid advances in radiologic technology and an increased imaging demand. The management of PCNs is challenging as most of these neoplasms are asymptomatic, but have malignant potential, and surgical resection has substantial perioperative morbidity and mortality. Endoscopic ultrasonography (EUS)-guided ablation, as a minimally invasive treatment, has received increasing attention in the past few years. However, the resolution after EUS-guided ablative therapy still needs to be improved. In this case report, EUS-guided radiofrequency ablation combined with lauromacrogol ablation was applied for the first time in the treatment of PCN, and it showed complete resolution at a 3-month follow-up.
Keywords: Pancreatic cystic neoplasms, endoscopic ultrasonography, radiofrequency ablation, lauromacrogol ablation
INTRODUCTION
The widespread utilization and technical advancement in abdominal imaging have resulted in an increased identification of pancreatic cystic neoplasms (PCNs), especially the asymptomatic and small ones (1). The prevalence and clinical variability of PCNs have presented a significant treatment challenge for physicians (2,3). Surgical resection and surveillance are the standard management approaches at present. Surgical resection has substantial perioperative morbidity and mortality; surveillance increases economic and psychological burden of the patients, and it may also lead to delayed treatment because the current differential diagnosis is still limited (2,4). Meantime, a substantial portion of PCNs remains indeterminate even after comprehensive evaluation (5). Therefore, it is a clinical dilemma whether to operate or observe an incidentally detected PCN. This dilemma has raised the need to develop a safe, effective, and minimally invasive treatment for PCNs. In this case report, EUS-guided radiofrequency ablation (RFA) combined with lauromacrogol ablation was for the first time reported to provide a new minimally invasive therapeutic method.
CASE PRESENTATION
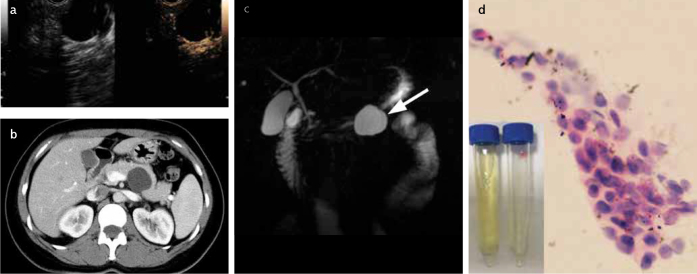
A previously healthy 53-year-old woman presented with a 3-year history of pancreatic cystic neoplasm detected via transabdominal ultrasonography (US) during a health examination. The neoplasm had increased 1 cm in the past year at US follow-up. The patient occasionally complained about abdominal discomfort. For further diagnosis, endoscopic ultrasonography, and fine-needle aspiration (FNA) were performed. EUS showed that the cyst in the pancreatic tail was septated with maximum section size 3.5×2.9 cm, and the cystic wall and septa were enhanced on contrast-enhanced EUS (CEEUS), which also presented in other images (Figure 1a–c). The cytological examination of aspirated fluid indicated serous cystadenoma (Figure 1d). The patient had severe psychological burden and refused surgical resection due to the perioperative morbidity, therefore EUS-guided ablation was performed. The patient signed the informed consent form prior to the therapy.
Figure 1. a–d.
Pretreatment images: (a) Endoscopic ultrasonography (EUS) shows the cyst is septated without solid components, and contrast-enhanced EUS (CEEUS) reveals that the cystic wall and septa are enhanced; (b) computed tomography (CT) shows one cystic lesion with clear border in the tail of the pancreas; (c) magnetic resonance cholangiopancreatography (MRCP) reveals no communication between the lesion and the pancreatic duct; (d) the aspirated fluid from the cyst is clear and transparent, and the cytological examination of the fluid showed cuboidal epithelial cells without mucin vacuole (Hematoxylin-eosin stain; original magnification, ×400)
Endoscopic ultrasonography guided RFA was first applied under three different angles via Habib EUS-RFA catheter (Emcision Ltd, London, UK) with 8W of power for 2 min in each place (Figure 2a, Video 1). After 2 months, EUS showed the maximum section size 2.8 cm×2.5 cm, and CEEUS revealed cystic wall enhancement without septa enhancement (Figure 2b). Then 10 ml of 1% lauromacrogol (Tianyu Pharmaceutical Co. Ltd, Shanxi, China) were injected into the cyst, followed by a triple lavage, and finally 10 ml were retained in the cyst (Figure 2c, Video 1). After 3 months, MRI revealed the neoplasm disappeared (Figure 3). There were no adverse events during and after the procedures.
Figure 2. a–c.
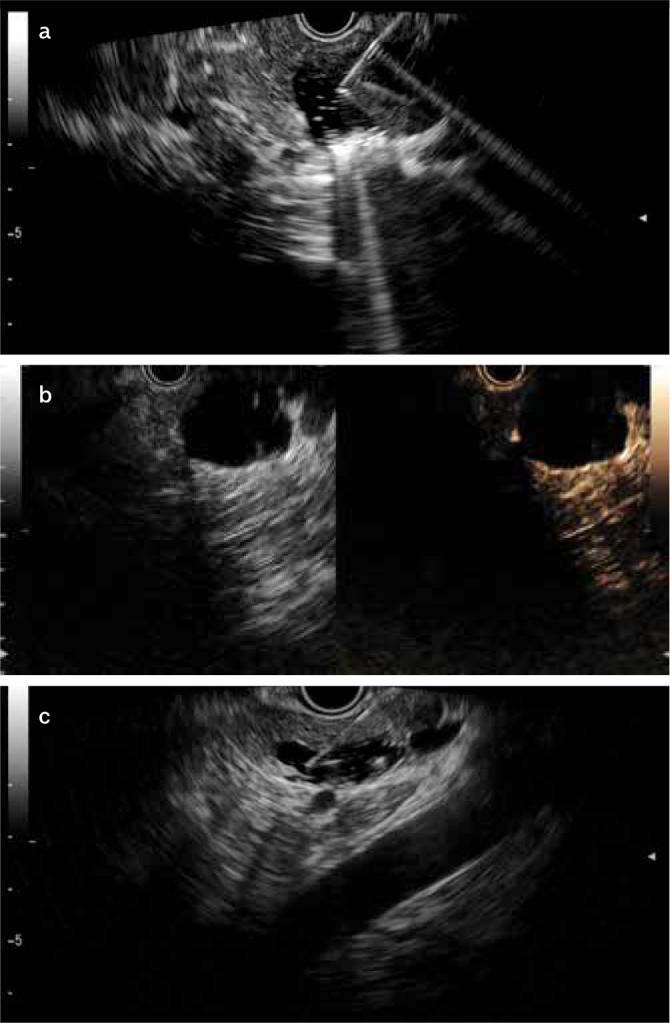
(a) The Habib EUS-RFA catheter is positioned within the cyst, and bubbles present after activation. (b) EUS, the second month after the EUS-RFA, shows the lesion is getting smaller, and the cystic wall is still enhanced without septa enhancement on CEEUS. (c) Lauromacrogol through the 19-gauge needle under EUS is injected into the cyst
EUS-RFA: Endoscopic ultrasonography radiofrequency ablation; CEEUS: contrast-enhanced endoscopic ultrasonography
Figure 3. a–c.
MRI examination: (a) pretreatment, a cystic lesion 3.5 cm×3.0 cm×3.1 cm in size; (b) a month after the EUS-RFA, the size is 3.5 cm×3.0 cm×3.1 cm; (c) 3 months after the combination treatment, the lesion disappears
DISCUSSION
The EUS-guided ablation for PCNs has received an increasing attention due to minimal invasion and possible direct imaging of the lesions (2). One of the EUS-guided ablations of PCNs is ethanol lavage with or without an injection of anti-tumoral agents. The pooled rate of complete cyst resolution is 56.2% at a follow-up of 2–118 months (6). The adverse events are significant, with a reported risk of abdominal pain ranging from 2% to 24%, and acute pancreatitis from 2% to 10% (7). However, the efficacy of ethanol lavage (EL) remains controversial and reports of patients undergoing surgery after EL showed a low rate of epithelial ablation (8,9). The septation in the PCNs also reduces the efficacy of EL (2,10). Then EUS-guided RFA, the other type of EUS-guided ablation, was investigated in the treatment of PCNs. Pai et al. (10) used RFA in management of 6 patients with PCNs, and all the procedures were successfully finalized with a complete resolution in 2 out of 6 patients at a 3- to 6-month follow-up; two patients had mild abdominal pain and no post-procedural pancreatitis, and other complications were observed. That is the only clinical study on EUS-RFA for PCNs, to date and the preliminary data show the procedure is feasible and safe.
In this case, EUS-guided RFA combined with lauromacrogol ablation was used for the first time, with a complete resolution at a 3-month follow-up. Under EUS guidance, RFA allows targeted delivery of heat energy and causes sustained thermal damage to the epithelium and septation of the cyst (2,11,12). However, for the irregular cystic lesions, the RFA destruction of the cystic wall may be variable due to the influence of distance between the RFA active electrode tip and the lesion. As the distance increases, the damage becomes weak. At a 2-month follow-up after RFA, the cystic wall enhancement still could be observed on CEEUS. To achieve complete resolution, EUS-guided injection of lauromacrogol was supplemented. Lauromacrogol is another type of sclerosing agent; its major ingredient is polyoxyethylene lauryl ether, and it also contains ethanol and sterilized water. It can induce vascular occlusion and has been widely used for esophageal varices and hemangiomas in China (13). For cystic lesions, lauromacrogol can induce denaturation of the epithelial cells followed by aseptic inflammation, adhesion, fibrosis, and then closure of the cysts, and it also has a local anesthetic effect. It has been used in hepatic, renal, and endometrial cysts, and presented lower rates of adverse events than ethanol in the comparison study on the two ablative agents for cystic lesions (13–15).
The combination of the EUS-guided physical and chemical ablation takes their advantages to achieve the best outcome. For multiloculated cysts, even one missed locule of ablative agent may result in cyst regeneration and treatment failure, so RFA is used to destroy the septation to make up for the deficiency of ablative agent injection. The injection of ablative agent also compensates for the heterogeneous destruction of RFA. Most notably, the effect of the combination of the chemical and physical ablation is greater than any one alone, which decreases risks of residue and recurrence. Park and his colleagues had proven this point in one animal study (11). They used porcine gallbladders as PCNs models, and EUS-RFA with or without ethanol ablation was carried out. After histological evaluation, RFA plus EL resulted in a greater percentage of denuded gallbladder mucosa than RFA alone (97.5% vs. 55.8%) (11).
The EUS-RFA combined with lauromacrogol ablation seems to be another reasonable strategy for improving minimally invasive treatment outcomes of PCNs. However, the safety, efficacy, and optimum indications still remain to be investigated in a large and long-term follow-up study with different PCNs types and sizes.
Supplementary Information
The diagnosis and treatment of the pancreatic cystic neoplasm.
Acknowledgements
The authors would like to thank all the staff of PLA General Hospital who took care of the patient.
Footnotes
Informed Consent: Written informed consent was obtained from the patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - E.L.; Design - E.L., X.F.; Supervision - X.F., E.L., N.C., H.L.; Materials - X.F.İ E.L., N.C., H.L.; Data Collection and/or Processing - X.F., E.L., N.C., H.L.; Analysis and/or Interpretation - X.F., E.L., N.C., H.L.; Literature Search - X.F., E.L., N.C., H.L.; Writing - X.F., E.L.; Critical Reviews - X.F., E.L., N.C., H.L.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Othman MO, Buscaglia JM. Get ready to meet the growing demand from patients with pancreatic cysts. Clin Gastroenterol Hepatol. 2016;14:594–6. doi: 10.1016/j.cgh.2015.12.023. https://doi.org/10.1016/j.cgh.2015.12.023 [DOI] [PubMed] [Google Scholar]
- 2.Arshad HM, Bharmal S, Duman DG, Liangpunsakul S, Turner BG. Advanced endoscopic ultrasound management techniques for preneoplastic pancreatic cystic lesions. J Investig Med. 2017;65:7–14. doi: 10.1136/jim-2016-000167. https://doi.org/10.1136/jim-2016-000167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singhi AD, Zeh HJ, Brand RE, et al. American Gastroenterological Association guidelines are inaccurate in detecting pancreatic cysts with advanced neoplasia: a clinicopathologic study of 225 patients with supporting molecular data. Gastrointest Endosc. 2016;83:1107–17. doi: 10.1016/j.gie.2015.12.009. https://doi.org/10.1016/j.gie.2015.12.009 [DOI] [PubMed] [Google Scholar]
- 4.Stark A, Donahue TR, Reber HA, Hines OJ. Pancreatic cyst disease: A Review. Jama. 2016;315:1882–93. doi: 10.1001/jama.2016.4690. https://doi.org/10.1001/jama.2016.4690 [DOI] [PubMed] [Google Scholar]
- 5.Oh HC, Brugge WR. EUS-guided pancreatic cyst ablation: a critical review (with video) Gastrointest Endosc. 2013;77:526–33. doi: 10.1016/j.gie.2012.10.033. https://doi.org/10.1016/j.gie.2012.10.033 [DOI] [PubMed] [Google Scholar]
- 6.Kandula M, Moole H, Cashman M, Volmar FH, Bechtold ML, Puli SR. Success of endoscopic ultrasound-guided ethanol ablation of pancreatic cysts: a meta-analysis and systematic review. Indian J Gastroenterol. 2015;34:193–9. doi: 10.1007/s12664-015-0575-2. https://doi.org/10.1007/s12664-015-0575-2 [DOI] [PubMed] [Google Scholar]
- 7.Signoretti M, Valente R, Repici A, Delle Fave G, Capurso G, Carrara S. Endoscopy-guided ablation of pancreatic lesions: Technical possibilities and clinical outlook. World J Gastrointest Endosc. 2017;9:41–54. doi: 10.4253/wjge.v9.i2.41. https://doi.org/10.4253/wjge.v9.i2.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vazquez-Sequeiros E, Maluf-Filho F. Endosonography-guided ablation of pancreatic cystic tumors: Is it justified? Gastrointest Endosc. 2016;83:921–3. doi: 10.1016/j.gie.2015.10.032. https://doi.org/10.1016/j.gie.2015.10.032 [DOI] [PubMed] [Google Scholar]
- 9.DeWitt J, McGreevy K, Schmidt CM, Brugge WR. EUS-guided ethanol versus saline solution lavage for pancreatic cysts: a randomized, double-blind study. Gastrointest Endosc. 2009;70:710–23. doi: 10.1016/j.gie.2009.03.1173. https://doi.org/10.1016/j.gie.2009.03.1173 [DOI] [PubMed] [Google Scholar]
- 10.Pai M, Habib N, Senturk H, et al. Endoscopic ultrasound guided radiofrequency ablation, for pancreatic cystic neoplasms and neuroendocrine tumors. World J Gastrointest Surg. 2015;7:52–9. doi: 10.4240/wjgs.v7.i4.52. https://doi.org/10.4240/wjgs.v7.i4.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park JS, Seo DW, Song TJ, et al. Endoscopic ultrasound-guided ablation of branch-duct intraductal papillary mucinous neoplasms: Feasibility and safety tests using porcine gallbladders. Dig Endosc. 2016;28:599–606. doi: 10.1111/den.12628. https://doi.org/10.1111/den.12628 [DOI] [PubMed] [Google Scholar]
- 12.Waung JA, Todd JF, Keane MG, Pereira SP. Successful management of a sporadic pancreatic insulinoma by endoscopic ultrasound- guided radiofrequency ablation. Endoscopy. 2016;4:E144–5. doi: 10.1055/s-0042-104650. https://doi.org/10.1055/s-0042-104650 [DOI] [PubMed] [Google Scholar]
- 13.Liu W, Wang L, Guo CX. The effects of lauromacrogol injection into rat endometrial cysts: a preliminary experimental study. Arch Gynecol Obstet. 2016;294:555–9. doi: 10.1007/s00404-016-4095-9. https://doi.org/10.1007/s00404-016-4095-9 [DOI] [PubMed] [Google Scholar]
- 14.Xue J, Geng X. Curative effect of lauromacrogol and absolute ethyl alcohol injection guided by ultrasound on simplex hepatic cyst. Pak J Pharm Sci. 2015;28:697–700. [PubMed] [Google Scholar]
- 15.Dell’Atti L. Comparison between the use of 99% ethanol and 3% polidocanol in percutaneous echoguided sclerotherapy treatment of simple renal cysts. Urol Ann. 2015;7:310–4. doi: 10.4103/0974-7796.152026. https://doi.org/10.4103/0974-7796.152026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The diagnosis and treatment of the pancreatic cystic neoplasm.