Abstract
Purpose:
To report our experience with 2 cases of Capnocytophaga keratitis.
Methods:
This is a retrospective study of case reports. We present the clinical presentation, diagnosis, and treatment strategies of 2 patients who presented with Capnocytophaga keratitis.
Results:
Both patients had risk factors including systemic immune compromise and ocular trauma. Both patients had robust inflammatory keratitis with necrosis. Case 1 demonstrates identification of Capnocytophaga with traditional microbiologic techniques. Case 2 demonstrates the use of unbiased metagenomic deep sequencing for identification of this unusual corneal pathogen.
Conclusions:
Capnocytophaga is a rare and aggressive infection. Even when traditional culture identifies the pathogen rapidly, keratitis can progress to perforation. In cases of severe keratitis in which traditional culture methods are unrevealing, metagenomic deep sequencing has potential to provide actionable diagnoses.
Key Words: Capnocytophaga keratitis, infectious keratitis, metagenomic deep sequencing
Capnocytophaga keratitis is a rare and aggressive ocular infection.1–4 The largest case series, including 10 cases, was reported in 2000.1 Five of these cases resulted in enucleation. We report our recent experience with 2 cases of Capnocytophaga keratitis to remind clinicians of this unusual and destructive infection and to highlight how both diagnosis and management of this infrequent bacterial infection are often challenging.
CASE REPORTS
Case 1
A 58-year-old man presented with a medical history significant for chronic myelogenous leukemia (CML) status after allogenic bone marrow transplant. Ocular history was significant for severe ocular graft-versus-host disease, keratoconjunctivitis sicca, and bilateral neurotrophic keratopathy. His left eye was recently treated for a culture-positive Streptococcus viridans corneal ulcer with hypopyon, and he recovered 20/60 acuity. The patient re-presented (Fig. 1A, left) with new, left large central corneal epithelial ulceration, 2 paracentral areas of corneal infiltration, and a 3.5-mm hypopyon. Hourly fortified cefazolin (50 mg/mL) and topical moxifloxacin were initiated. Three days after culture, microbiology identified growth of numerous Capnoctyophaga cynodegmi species. The patient reported, while celebrating his recovery from S. viridans keratitis, that he let his dog lick him all over his face, including his neurotrophic corneas. Four days after presentation, the patient developed Seidel-positive inferior paracentral perforation requiring an emergency glue procedure (Fig. 1A, middle). Because sensitivities for this rare pathogen require send-out evaluation, a review of previous Capnocytophaga case reports1–3 suggested treatment with topical clindamycin. Compounded clindamycin 5% was initiated hourly. The glue remained in place for 2 months and subsequently fell off. Visual acuity improved to 20/200. The globe remained intact, and the area of previous perforation had vascularized (Fig. 1A, right).
FIGURE 1.
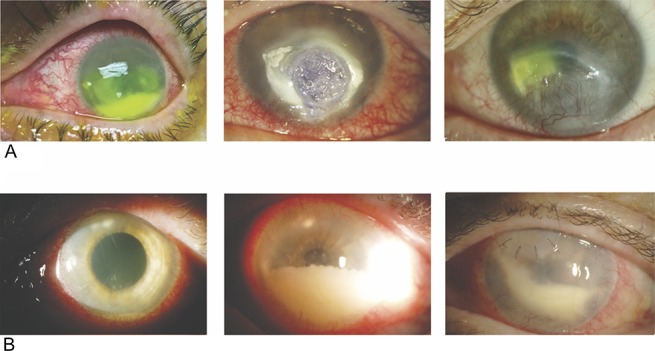
Slit-lamp photographs of both cases. A, Case 1; left panel: presentation photograph with infiltrates and hypopyon; middle panel: 4 days after presentation with perforation requiring glue; right panel: 2 months after glue. B, Case 2; left panel: presentation photograph with superior mid-stromal peripheral and paracentral subepithelial infiltrates with hypopyon; middle panel: progressive inflammation; right panel: small superonasal patch graft was performed after diagnostic deep corneal biopsy. Robust AC inflammation remains. Fluid from an AC tap at this point was sent for metagenomic deep sequencing.
Case 2
A 64-year-old woman with a history of rheumatoid arthritis being treated with rituximab infusions sustained an outdoor foreign body injury after using motorized landscaping equipment. She developed ocular irritation and decreased vision and was treated at an outside facility. She presented 1 month into treatment for consultation after having failed therapy with topical prednisolone acetate 1% and topical ciprofloxacin. Her left cornea disclosed several superior mid-stromal peripheral and tiny paracentral subepithelial infiltrates (Fig. 1B, left). A 1-mm hypopyon was present. Multiple Gram stains, potassium hydroxide (KOH) stains, and cultures obtained from epithelial scrapings over the areas of subepithelial infiltrates were unrevealing. Confocal examination demonstrated nonspecific inflammatory changes. The stromal lesions progressed deeper. Because the scattered superficial infiltrates were clinically concerning for satellite lesions, the patient was treated aggressively with topical, intrastromal, and oral antifungal therapy (including amphotericin B, voriconazole, and natamycin). Over the next 2 months, the patient developed progressive worsening of anterior chamber inflammation associated with endothelial plaques (Fig. 1B, middle). Aqueous fluid from 2 anterior chamber washout procedures as well as corneal punch biopsy and patch graft of the necrotic superior mid-stromal infiltrates (Fig. 1B, right), did not identify any organisms using aerobic and anaerobic media. A robust inflammatory reaction persisted after a patch graft. Aqueous fluid from a third washout procedure was sent to a Clinical Laboratory Improvement Amendments-certified laboratory for universal polymerase chain reaction for fungal genomes and tested negative. Residual aqueous fluid was sent to the Proctor Foundation for metagenomic deep sequencing (MDS). MDS is an unbiased high-throughput sequencing approach that interrogates all potential genomes in a clinical sample. MDS was performed as previously described.5 This study adhered to the tenets of the Declaration of Helsinki. The Institutional Review Board of the University of California, San Francisco, approved the study (16-19151), and informed consent was obtained from the patient. Two species of Capnocytophaga, Capnocytophaga canimorsus, and C. cynodegmi were identified (Fig. 2A). Orthogonal validation with partial 16S rRNA gene reverse transcription polymerase chain reaction and Sanger sequencing of the remaining RNA from the patient's aqueous specimen confirmed the presence of Capnocytophaga genome (Fig. 2B). The patient was placed on topical clindamycin 5% with subsequent complete resolution of inflammation and infiltration in 6 weeks. After the MDS results, the patient reported that she lives with numerous cats and dogs. Her acuity postresolution is hand motions from irregular astigmatism from the patch graft and dense cataract that progressed during the severe inflammatory episode. Penetrating keratoplasty with cataract surgery is planned.
FIGURE 2.
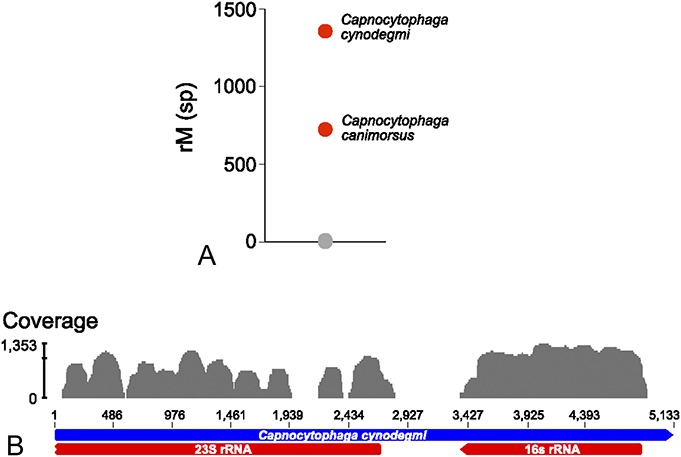
Identification of Capnocytophaga canimorsus and Capnoctyophaga cynodegmi by metagenomic deep sequencing. A, Organisms identified in the patient's aqueous sample are plotted as a function of matched read pairs per million read pairs (rM) at the species level based on nucleotide alignment. Sequencing reads aligned to C. canimorsus and C. cynodegmi (red circles) predominated the sample. Gray circles indicate background sequencing reads. B, Capnocytophaga cynodegmi sequences from case 2 assembled against the reference C. cynodegmi genome (GenBank NZ_CP022378).
DISCUSSION
Capnocytophaga is a gram-negative rod-shaped bacterium that is part of the normal oral flora of humans, dogs, and cats.2,6 Human infection from Captocytophaga is rare. Ocular infection is similarly uncommon, and although endophthalmitis7 and blepharoconjunctivitis8 are reported, keratitis is the most common clinical presentation. On review of available case reports,1–4,7 almost all Capnocytophaga ocular infections occur in hosts with secondary risk factors such as immune compromise and trauma. In addition, Capnocytophaga keratitis often presents with a fairly rapid course to fulminant inflammation. Deep stromal infiltration with progression to necrosis is common, and infections associated with Capnocytophaga are associated with a poor visual outcome.1–4,7,9 Although several species of Capnocytophaga are part of the normal human oral flora, C. canimorsus and C. cynodegmi are found only in feline and canine oral flora. A recent report of 7 cases of Capnocytophaga keratitis in dogs similarly demonstrates an aggressive course with keratomalacia and poor prognosis.6
Herein, we present 2 recent cases of Capnocytophaga keratitis, each illustrating some important aspects of this disease. Both cases demonstrated Capnocytophaga occurring in the setting of a compromised host. Both cases demonstrated robust ocular inflammation with hypopyon and stromal necrosis. Both cases provided a history of frequent contact with pet dogs and cats. Both cases improved with administration of topical clindamycin.
With case 1, despite prompt identification of Capnocytophaga, perforation still occurred within 4 days of presentation. Sensitivity information on unusual pathogens often takes significant time. In vitro Capnocytophaga susceptibility testing is further complicated by relatively slow, fastidious, growth of the organism and lack of laboratory standard guidelines for antimicrobial susceptibilities. Review of previous case reports describing the efficacy of topical clindamycin in similar cases was helpful in management of this case.
Case 2 demonstrated the downfall of a ∼60% sensitivity for the current gold standard cornea culture to identify pathogens responsible for infectious keratitis.10 Cornea cultures are particularly challenging for deeper infections and infections with an intact epithelium. In addition, with some strains of Capnocytophaga being fastidious in culture and difficult to isolate, standard culture techniques may be underestimating its occurrence. In cases in which the suspicion for infection is high but conventional diagnostics are unrevealing, MDS has the potential to provide an actionable diagnosis, as shown with this case. The unbiased nature of MDS, where it can detect any viable pathogen in a clinical specimen, is particularly useful when the causative infection is rare and hence might not be on the differential diagnosis. Although more validation studies are required before MDS can be routinely offered to practicing ophthalmologists, this approach holds promise as a complementary approach to conventional diagnostics for ocular surface or corneal infections.
Footnotes
Supported by the Research to Prevent Blindness Career Development Award (T. Doan), the National Eye Institute of the National Institutes of Health under Award Number K08EY026986 (T. Doan), and Building Interdisciplinary Careers in Women's Health of the National Institutes of Health K12HD085850 (J. Shantha).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Alexandrakis G, Palma LA, Miller D, et al. Capnocytophaga keratitis. Ophthalmology. 2000;107:1503–1506. [DOI] [PubMed] [Google Scholar]
- 2.Chodosh J. Cat's tooth keratitis: human corneal infection with Capnocytophaga canimorsus. Cornea. 2001;20:661–663. [DOI] [PubMed] [Google Scholar]
- 3.Oshida T, Kamura Y, Sawa M. Demographic study of expulsive hemorrhages in 3 patients with infectious keratitis. Cornea. 2011;30:784–786. [DOI] [PubMed] [Google Scholar]
- 4.Ghosheh FR, Ehlers JP, Ayres BD, et al. Corneal ulcers associated with aerosolized crack cocaine use. Cornea. 2007;26:966–969. [DOI] [PubMed] [Google Scholar]
- 5.Doan T, Wilson MR, Crawford ED, et al. Illuminating uveitis: metagenomic deep sequencing identifies common and rare pathogens. Genome Med. 2016;8:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ledbetter EC, Franklin-Guild RJ, Edelmann ML. Capnocytophaga keratitis in dogs: clinical, histopathologic, and microbiologic features of seven cases. Vet Ophthalmol. 2018. [epub ahead of print]. 10.1111/vop.12549. [DOI] [PubMed] [Google Scholar]
- 7.Rubsamen PE, McLeish WM, Pflugfelder S, et al. Capnocytophaga endophthalmitis. Ophthalmology. 1993;100:456–459. [DOI] [PubMed] [Google Scholar]
- 8.Wasserman D, Asbell PA, Friedman AJ, et al. Capnocytophaga ochracea chronic blepharoconjunctivitis. Cornea. 1995;14:533–535. [PubMed] [Google Scholar]
- 9.Font RL, Jay V, Misra RP, et al. Capnocytophaga keratitis: a clinicopathologic study of three patients, including electron microscopic observations. Ophthalmology. 1994;101:1929–1934. [DOI] [PubMed] [Google Scholar]
- 10.McLeod SD, Kolahdouz-Isfahani A, Rostamian K, et al. The role of smears, cultures, and antibiotic sensitivity testing in the management of suspected infectious keratitis. Ophthalmology. 1996;103:23–28. [DOI] [PubMed] [Google Scholar]


