Abstract
Considering the vast ongoing challenge of preventing obesity, the time has come to reconceptualize and change the way we study the development of obesity in childhood. The developmental cascade model, which refers to the cumulative consequences and spreading downstream effects of risk and protective factors, offers a longitudinal framework for understanding obesity. This perspective elucidates the way an accumulation of risk factors, across and within biopsychosocial spheres and phases of development, can propel individuals toward obesity. In this article, we use a theory-driven model-building approach and a review of published literature to propose a developmental cascade model of pediatric obesity focused on proximal biopsychosocial influences (e.g., genetic, intrapersonal, familial). A two-stage scoping review conducted in January 2015 and May 2016 identified 1315 unique studies; 310 were included in the final review. The proposed developmental cascade model provides a basis for testing hypothesized cascades with multiple intervening variables and complex longitudinal processes. Moreover, the model informs future research by resolving seemingly contradictory findings on pathways to obesity previously thought to be distinct (low self-esteem, consuming sugary foods, and poor sleep cause obesity) that are actually processes working together over time (low self-esteem causes consumption of sugary foods which disrupts sleep quality and contributes to obesity). The resultant empirical findings of such inquiries are highly informative for identifying the timing and specific targets of preventive interventions across and within developmental phases. The implications of such a cascade model of pediatric obesity for health psychology and developmental and prevention sciences are discussed.
Keywords: biopsychosocial model, childhood obesity, developmental cascade, pediatric obesity, cascade, development, ecological, prevention
Introduction
Pediatric obesity is a complex public health problem affecting the majority of developed countries worldwide (National Research Council and Institute of Medicine, 2011). Rates of obesity among children and adolescents in developed countries, collected in 2013, were 12.9% for boys and 13.4% for girls (Ng et al., 2014). According to the Centers for Disease Control and Prevention, the key contributors to obesity—poor diet and physical inactivity—are among the leading causes of preventable youth deaths (Eaton et al., 2012). By the time youth reach adolescence, an alarming 61% of those who are obese exhibit at least one risk factor for cardiovascular disease (e.g., hypertension, elevated cholesterol) over and above their weight status (May, Kuklina, & Yoon, 2012). Prevention efforts that begin early in childhood are critical considering that 60% of preschool-aged children who are overweight will be overweight at age 12 (Nader et al., 2006). Elevated body mass index (BMI) among children is also very costly. Based on data from 6- to 19-year-olds in the 2002–2005 Medical Expenditure Panel Survey, elevated BMI in childhood was associated with over $2.9 billion annually for prescription drug, emergency department, and outpatient visits (Trasande & Chatterjee, 2009) and the incremental lifetime medical cost for a child who is obese starting at age 10 is $19,000 per child more than a non-obese child (Finkelstein, Graham, & Malhotra, 2014). Despite the remarkable need to prevent childhood obesity, few programs have demonstrated long-lasting effects or been implemented at scale to have an appreciable public health impact (Denzer, Reithofer, Wabitsch, & Widhalm, 2004).
Developmental Ecological Models of Pediatric Obesity
Developing preventive interventions for chronic diseases necessitates a comprehensive understanding of the progression of the disease from a biopsychosocial perspective (Belloc & Breslow, 1972; Engel, 1977). This includes the risk and protective functions of genetic, biological, physiological, and ecological factors, as well as their interactions over time (Barker, 2004; Gillman, 2005). A plethora of risk and protective factors for the development of obesity in childhood and adolescence have been empirically identified (Han, Lawlor, & Kimm, 2010; Monteiro & Victora, 2005; Moreno & Rodríguez, 2007; Reilly et al., 2005; Weng, Redsell, Swift, Yang, & Glazebrook, 2012). Existing models of child and adolescent obesity from biopsychosocial (Goetz & Caron, 1999; Nguyen & Bera, 2016), contextual (Davison & Birch, 2001), and developmental ecological (Harrison et al., 2011) perspectives illustrate the influences of a variety of risk and protective factors on weight gain via interactions among multiple levels, such as the biological/cellular, child, family, peer, community/societal, cultural, and geopolitical levels, among others. Most non-communicable diseases, such as obesity, depression, and diabetes, are the result of interactions between numerous causal patterns and factors, and traditional “compartmental” causation frameworks have limited ability to capture the multiplicity and complexity of influential factors, the dynamic relations between factors across development, and the potential for identifying constructs and processes that have primacy for intervention at specific time points. Thus, the interventions they inform are ultimately limited (Nianogo & Arah, 2015).
Additionally, neither the existing biopsychosocial or contextual models are expressly developmental. Harrison et al. (2011) noted that their developmental ecological model, which is a snapshot in time of the factors that contribute to excess weight gain, “may be adapted to any stage of child development” (p. 51). They put forth a limited scope developmental model that linked interpersonal contexts to child weight through interpersonal mediators, such as negative affect and self-regulation. However, the precise manner in which the levels in the model interact over time, during which developmental period specific factors were expected to exert a salient influence on factors appearing later in the cascade, and whether the pattern of interaction changes between different developmental periods, is absent. Further, Harrist et al. (2012) issued a call to developmental scientists to lend their expertise to the study of pediatric obesity to address identified shortcomings in current models. Despite the need for more comprehensive developmental models, none have since appeared in the literature. The purpose of the current scoping review is to characterize the degree and direction of existing empirical support for a developmental cascade model of pediatric obesity. The developmental cascademodel refers to the cumulative consequences and spreading downstream effects that are the result of interactions and transactions that occur over time, across and within different systems, levels and domains, and generations (Masten & Cicchetti, 2010). The cascade model involves developmental processes that have been described as “snowballing,” “amplification,” “transactional,” and “progressive.” Our approach provides others the information needed to: a) accurately evaluate their confidence in the relationship between constructs; and b) identify those relationships in need of additional research or greater attention when designing future and empirically testing a developmental cascade model of pediatric obesity.
The Promise of a Developmental Cascade Model of Childhood Obesity
Developmental theory suggests that ecological adversity and child, family, and community factors combine to precipitate a developmental trajectory toward a particular outcome. Although many developmental models exist for common chronic disease, behavioral health, and mental health issues in childhood, using a developmental cascade model has proven its utility in directly informing the prevention of youth substance use and antisocial behavior (e.g., Dishion, Véronneau, & Myers, 2010; Dodge, Greenberg, Malone, & Conduct Problems Prevention Research, 2008; Dodge et al., 2009; Sitnick, Shaw, & Hyde, 2014), and also in the areas related to the effects of child maltreatment and exposure to other stressors (Rogosch, Oshri, & Cicchetti, 2010; Sapienza & Masten, 2011). In the field of substance use, the developmental cascade model has been useful at demonstrating how socioeconomic adversity sets the stage for early experiences within the family (prior to age 5) that predict behavior problems in the elementary school context and the formation of antisocial peer groups, which in turn increases the risk of initiating substance use in middle and high school and associated increased risk for delinquency, violence, and high-risk sexual behaviors.
There are several key implications of developmental cascade models that can be empirically tested to inform theory and intervention efforts. Prevention programs for children rely on developmental science to identify intervention targets at different developmental periods that have been established as critical mechanisms of action through meditational analyses involving multiple variables (Sandler, Schoenfelder, Wolchik, & MacKinnon, 2011). Concerning obesity, for example, parents’ maladaptive parenting and family management practices, such as permissive parenting, low parental involvement, and poor limit setting, are associated with pediatric weight gain (e.g., Kitzman-Ulrich et al., 2010) and also hinder their ability to effectively implement healthy lifestyle recommendations in young children (Faith et al., 2012). A developmental cascade model can be used to identify and test salient family management practices that, when altered through a family-centered intervention, result in sustained effects on healthy lifestyle behavior change to reduce weight gain and obesity (Smith, St. George, & Prado, 2017).
From existing empirical developmental cascade models, four core tenets have emerged about the interactions of multiple risk and protective factors and how interventions may disrupt such cascades:
Changes at one step in the cascade lead to broad downstream effects.
There is continuity in child behaviors and ecological influences from early childhood to early adolescence, even though they may differ in form and function.
No single risk or protective factor has a large effect size, but the accumulation of small effects over time is great. Therefore, small increases in protective factors in early childhood can lead to large downstream changes in adolescence.
There is a primacy of early influences, not necessarily because their effects are larger in magnitude than later influences, but because they trigger a cascading process that grows into larger effects over time. Thus, although there are opportunities for preventing obesity and its antecedents across all stages of development, the degree of plasticity decreases substantially with each advancing developmental period, making prevention more difficult.
These implications of developmental cascade models highlight the potential for prevention of obesity in early childhood to have a substantial, sustained, and far-reaching impact. Yet, long-term (>10 years) follow-up studies of preventive interventions in early childhood are rare; few have tested simple mediation, let alone the impact on multiple linked mediators; and it is uncommon to evaluate the longitudinal, transactional effects across multiple biopsychosocial levels. That is, most studies are primarily concerned with long-term stability in one domain; some have evaluated the interactions between two levels (e.g., child and family, child and neighborhood). Developmental cascade models highlight compelling questions that can only be addressed by following participants over long periods and assessing multi-level influences of obesity risk. Since this type of research base is currently very limited for obesity, we have taken an alternative approach to distilling patterns from the extant literature to propose a developmental cascade model of pediatric obesity that can form the basis for future research.
This Study
The aim of the current study was to propose a developmental cascade model of pediatric obesity focused on proximal biopsychosocial influences (e.g., genetic, child, family, and peer) based on existing theories and empirical evidence. The hypothesized conceptual developmental cascade model was refined into the final model using multiple sources and an iterative process. First, using Dishion and Patterson’s (1999) theory-driven model-building approach, we began with existing models for childhood obesity (e.g., Harrist et al. 2011; Nguyen & Bera, 2016) and incorporated the four tenets of developmental cascade models and elements of successful examples from related subfields to develop a hypothesized model. This model informed our search terms and guided during which developmental period specific factors were expected to exert a salient influence on a downstream cascade. We then conducted a scoping review of the empirical literature using the hypothesized developmental cascade model as a guide.
Scoping reviews are intended to synthesize an exploratory research question in a defined area by mapping key concepts, types of evidence, and identifying gaps in research by systematically searching, selecting, and synthesizing existing knowledge (Colquhoun et al., 2014). This type of review differs from a systematic review in that it is not meant to capture all available studies and does not involve a formal evaluation of study quality; although about one quarter of scoping reviews have included some form of quality evaluation (Pham et al., 2014). This review was intended to identify studies that tested a longitudinal relationship between variables in the hypothesized developmental cascade model. These relationships are referred to as “links” in this paper. We then evaluated the empirical support for specific links in the hypothesized developmental cascade model and retained those that had sufficient evidence from rigorous studies, even if limited in quantity. Additionally, new links were added or links were moved to other developmental periods when indicated by the reviewed findings. The overall aim was to proffer a model that was both theoretically derived and empirically supported to guide future inquiry. We did not intend to provide a comprehensive and exhaustive review but to ascertain a sufficient sample of studies to offer an adequate understanding of the existing science.
Method
Search Strategy
A two-stage scoping review of studies published in peer-reviewed journals was conducted to evaluate the support for the hypothesized links. First, a computer-based search of articles published in English in peer-reviewed journals between 1995 and 2015 was performed using Web of Science in January 2015. Search terms were identified by combining the developmental period (“infan*,” “child*,” or “adolescen*”), the hypothesized risk factor (i.e., “self-regulat*”), and the word(s) “weight” and/or “diet*” (asterisks indicate that any characters/letters can follow the last character of the search term). In addition, the search term “longitud*” was added in order to restrict each search to longitudinal studies that provide support for hypothesized casual links in the model. To increase specificity, the search domains were restricted to science, technology, and social sciences, and the search areas within the domains were limited to: nutrition dietetics, endocrinology metabolism, pediatrics, developmental biology, psychology, psychiatry, neurosciences/neurology, behavioral sciences, education/educational research, food-science technology, sociology, ethnic studies, urban studies, social issues, family studies, life sciences biomedicine other topics, biomedical social sciences, and social science other topics. Occasionally, additional areas such as “social work” or “cardiovascular systems cardiology” were included when the original search terms resulted in few studies. In critically evaluating the results of the first search, the authors identified important links to obesity that were not captured. As a result, a second search was conducted in May 2016 that included new search terms that were entered using the same grouping of keywords/phrases, and the parameters of the first search, including publication date range and search domains.
Study Selection
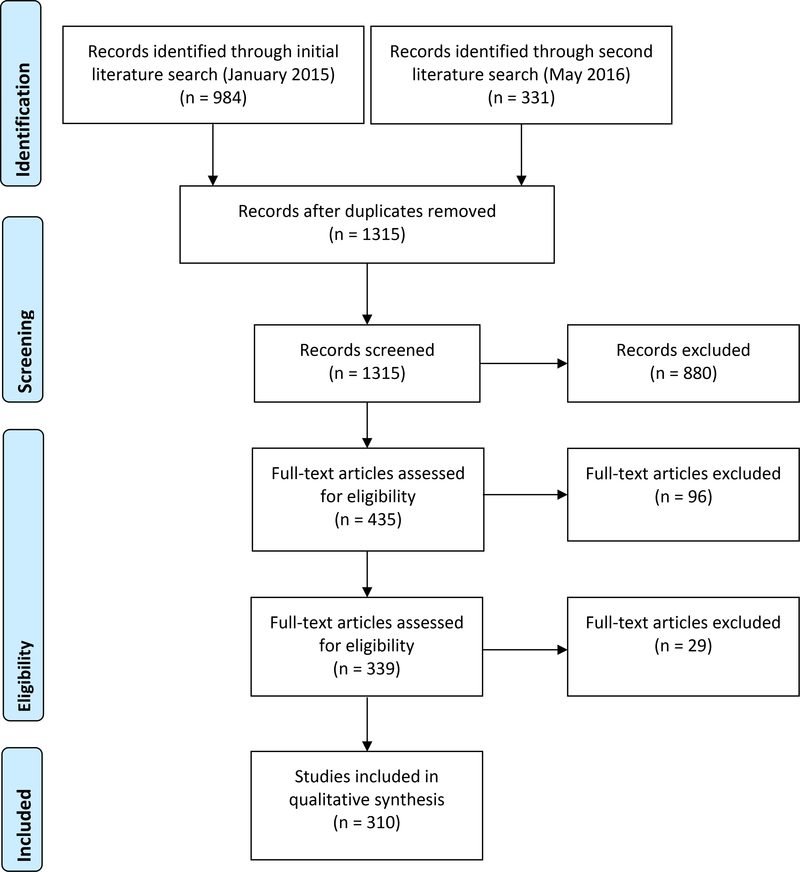
The authors used a three-phase procedure comprising computerized study selection, title and abstract screening, and data extraction from full text to identify the final sample of studies meeting criteria for inclusion. This procedure was applied to the first and second literature searches. The combined results for both searches are presented. The computerized study selection resulted in 1315 articles. Next, a trained undergraduate research assistant and three of the authors (KNE, ML, ZM) screened titles and abstracts using the following exclusion criteria: non-human sample, non-longitudinal design, age of sample ≥18 at wave one, and not relevant to childhood obesity. It is important to note that studies that did not have obesity as the main outcome were still eligible for inclusion if they demonstrated a relationship between two points in the cascade that were studied in the original research for the express purpose of understanding obesity. For example, a study demonstrating that poor inhibitory control in early childhood is related to poorer nutritional intake in pre-adolescence would be included since intake is hypothesized as a risk factor for obesity later in the cascade. As such, obesity or excess weight gain needed to be an element of the study to ensure some degree of relevance to the overall aim of our search.
Data Extraction
The articles that passed the title and abstract review (n = 435) were retained for a review of the full text. A total of 339 articles were retained after the initial full text review. Key study characteristics (e.g., sample, findings) were entered into a spreadsheet. Upon further review during preparation of the article, 29 studies that initially passed full text review were deemed to not meet study criteria and were excluded. Thus, a total of 310 articles were retained. Because this study is a scoping and not a systematic review, we report the study selection using a modified version the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Moher, Liberati, Tetzlaff, Altman, & Group, 2009) as Figure 1. A bibliography of the final 310 articles is included as Supplemental File 1.
Figure 1.
PRISMA review flow diagram
Approach to the Synthesis of Findings
We organized the synthesis of findings by four developmental periods for which particular risk or protective factors are most relevant using the Ages and Stages of Child Development (Child Development Institute, 2017): Prenatal/Infants (< 2 years), Toddlers/Preschoolers (2–5 years), School Age Children (6–12 years), and Adolescents/Teenagers (13–18 years). Although we limited our inclusion criteria to those studies with baseline measurement occurring prior to age 18, we included the term early adulthood in the final developmental period given that studies had to be longitudinal and outcomes were predominantly measured in early adulthood. Some constructs, such as physical activity and dietary habits/nutrition, are included in multiple developmental stages whereas others that could be placed across multiple stages might only be in one. To determine where to place a particular construct, we used the results of the literature review with guidance from theoretical models. When the majority of supporting evidence for the effects of a construct occurred in a single stage, we placed it there accordingly. Next, we elected to present findings related to the influence of parents/caregivers in a separate section because theory and empirical evidence suggests that these influences are salient across development, but we also noted age-appropriate shifts in the application of particular parenting practices. For example, in toddlerhood, caregivers provide positive praise and encouragement of children when they try new and healthy foods offered to them, whereas in later development, praise is given when children and adolescents make healthy choices on their own. Finally, we provide a very brief summary of the influence of distal ecological factors (e.g., neighborhood, community, geopolitical) on the links in the model. The findings discussed in this section were identified outside of the literature review procedures conducted for the other sections of this article and we sought to include previously completed syntheses of the literature rather than source articles.
Detailed Summary of Reviewed Studies: Supplemental File 2.
As part of our review process, we prepared a detailed summary of those studies that were deemed representative and highly informative—this approach was particularly relevant and necessary for active research areas, such as the effect of diet and nutrition on weight, where selectivity was a necessity. For other areas with limited attention or results in our literature search, the majority of identified studies were included in the synthesis. This material is available in Supplemental File 2: Detailed Review of Studies by Developmental Stage. The purpose of this detailed document is to provide the interested reader with a resource for developing nuanced hypotheses. Specifying a developmental cascade model to be tested requires reviewing a large literature that spans developmental stages and multiple constructs. By including this detailed review, it is our hope that it will contribute to a more rapid undertaking of new investigations of such models. In the detailed review, whenever possible, basic characteristics of the study type (e.g., birth cohort) and the participants (e.g., N, mean age, % female, country/region) are provided. Additionally, defining or unique characteristics of the study and sample are noted when they contribute to evaluating the relevance or generalizability of the findings, such as the racial/ethnic composition of the sample and the study methodology.
Results
Although the review resulted in studies from a wide variety of samples, there were a large number from longitudinal and cohort studies from around the world including the Amsterdam Growth and Health Longitudinal Study, the Avon Longitudinal Study of Parents and Children, the National Longitudinal Study of Adolescent Health, Project Eating Among Teens, the National Longitudinal Survey of Youth, the Early Childhood Longitudinal Study-Birth Cohort, and the Dortmund Nutritional and Anthropometric Longitudinally Designed Study, among others. The following synthesized results specific to each developmental stage are presented, along with a summary of the literature concerning distal ecological influences.
Prenatal–Infants Stage
A modest body of methodologically strong research from twin, adoption, cross-generational, epigenetic, and neurotransmitter studies supports a link between genetics and adiposity in the prenatal to infancy period. Maternal health status is also related to child weight in this stage. Most studies focused on the link between child adiposity and parent, usually mother’s, weight status— the effect was especially strong when both parents were overweight—but some research supports a relation with more general maternal health status and child exposure to maternal stress during pregnancy. For example, Stout, Espel, Sandman, Glynn, and Davis (2015) found that fetal exposure to elevated maternal cortisol and corticotropin-releasing hormone was related to patterns of rapid and delayed increase BMI over the first 24 months of life. Concerning the association between the health of the child in utero and later weight status, the strongest associations were found between maternal BMI (before and during pregnancy) and later child BMI than any other in utero factors. Research also supports a link between gestational diabetes and later BMI that is often mediated by gestational size. Concerning infant temperament, our results mirror those of a recent systematic review by Bergmeier, Skouteris, Horwood, Hooley, and Richardson (2014) that included 13 longitudinal and five cross-sectional studies that found support for a relationship between “difficult” child temperament and subsequent weight gain in later stages, suggesting that when children present parents with a greater challenge in effectively managing their behavior, they are more likely to gain weight—most likely due to parents having difficulties setting effective limits on such behaviors as sedentary activity and food consumption.
Socioeconomic status (SES), which is commonly determined by such indices as household income or parental education, despite there being many factors contributing to and related to SES (e.g., race/ethnicity), is a robust area of research as it concerns associations with BMI. The multifaceted nature of SES contributes to the complexity of findings in the literature related to childhood obesity. Race, parental education, income, and location of residence confound the relationship in some studies. Notably, we discuss SES in this developmental stage because its impact on constructs related to obesity begins early in a child’s life. There is clear evidence however that this impact remains important throughout all developmental stages. Experts suggest that SES be assessed as early as possible and tracked over time in developmental research (Duncan, Magnuson, & Votruba-Drzal, 2017). Additionally, the majority of the identified studies assessed SES in this stage. This could be in part due to our inclusion criteria that lead to identifying of a large number of birth cohort and early-starting longitudinal studies.
In general, our findings support those of other recent reviews on the topic that persons born into low SES households were more likely to be obese later in life compared to their counterparts in high SES households (Parsons, Power, Logan, & Summerbell, 1999; Power & Parsons, 2000). However, this conclusion is not consistent across individual studies and samples with some studies finding the opposite relationship. Examining some specific aspects of SES, our review revealed: 1) a positive relationship between both SES and parental education with the nutrition of young children; 2) race/ethnicity is an independent contributor to the development of obesity, with research indicating Hispanic/Latinx, Black, and American Indian being at highest risk (Ogden et al., 2016); and 3) the impact of living with food insecurity (more common in lower-income and ethnic minority families), is unclear for children because the findings are confounded by age, race, family income, and sex. Some evidence suggests that maternal obesity amplifies the relationship between food insecurity and child weight.
Toddlers–Preschoolers Stage
There is an extensive literature on the link between obesity and the dietary habits—both nutritional quality of food consumed and eating behaviors—of toddlers and children up to age 10 years. The quality rather than the quantity of food was found to be more influential to length and weight growth from 18–30 months; diets higher in animal products were associated with heavier toddlers; higher protein intake was related to a higher BMI later; there is a small protective effect of eating fruits and vegetables and drinking fewer sugar-sweetened beverages; snacking while watching television puts children at greater risk for obesity, and relatedly, the relationship between amount of television viewed and child BMI was found to be mediated by dietary intake; and dietary restraint behaviors (i.e., the ability to intentionally limit the amount of food eaten) appears to be positively related to BMI and negatively related to dietary intake. The literature on physical activity in toddlers and young children is limited compared to that conducted in older stages. Our findings support the conclusions of a review paper of published longitudinal studies by Parizkova (2014) in that more vigorous physical activity is associated with greater decreases in BMI over time for heavier children. Concerning rapid weight gain and adiposity rebound, our findings are again mirrored by other recent reviews of the literature that find a positive relationship between risk for obesity later in life and rapid weight gain during infancy and earlier adiposity rebound.
Our findings, and those of two other reviews (Bergmeier et al., 2014; Thamotharan, Lange, Zale, Huffhines, & Fields, 2013), indicate that poor self-regulation and related constructs such as child temperament, self-control, inhibitory control, and impulsivity, are obesogenic risk factors. The longitudinal relations between externalizing behaviors and weight appear to begin in and be most salient between the toddlerhood and early childhood stages. A few studies examining the effect of obesity on externalizing behavior provide support for its co-occurrence with overweight but the longitudinal associations are inconsistent and may differ by gender. The positive relation between adverse events (e.g., trauma, neglect, abuse) in childhood and obesity later in life appears well supported by the data, but there is a need for more prospective study designs.
School Age Children Stage
A number of studies have attempted to shed light on the nuanced relationship between dietary intake and weight in school age children. A recent meta-analysis found moderately strong evidence from methodologically rigorous longitudinal cohort studies to suggest that there is a positive association between dietary energy density and increased risk for adiposity (Perez-Escamilla et al., 2012). However, a number of individual longitudinal studies we reviewed examined overall dietary intake in relation to child BMI change and have found no evidence for the relationship. Among those that appear more robust are links to sugar-sweetened beverage consumption and frequency of eating take-out foods. Eating breakfast more often appears to be protective against weight gain in this stage. A modest corpus of studies shows positive relations between sedentary time and BMI and negative relations with time spent in physical activity, but this is not unequivocal as gender differences as well as SES and other familial factors appear to play a role. Additionally, some studies have identified clusters, such that children with low activity levels, high media use, and low dietary quality had the highest increase in prevalence of overweight, while children with the pattern of high physical activity and average media use and dietary quality had the smallest increase (Spengler, Mess, Schmocker, & Woll, 2014).
Our findings are consistent with those of a recent meta-analysis of cross-sectional and longitudinal study designs indicating that short sleep duration increases the risk of overweight and obesity in childhood and adolescence by a magnitude of two (Fatima & Mamun, 2015). The same relationship seems less strong in adolescence, as the longitudinal studies captured by our search reported insignificant relations between sleep duration and obesity. These findings support focusing on the effects of sleep during school age. Although there is substantial evidence demonstrating that being overweight/obese may lead to lower self-esteem and body satisfaction (e.g., Angle et al., 2005; Frisen, Lunde, & Berg, 2015), only a few studies have found that self-esteem and body image predict changes in weight over time. School age may be particularly salient. Global self-esteem (not related to weight or body image specifically) predicts incidence of obesity, albeit a few studies did not find this relation and gender appears to be a salient moderator. Relatedly, a recent review of five studies that examined the way self-esteem in mid- or late-childhood impacted obesity during adolescence (Incledon, Gerner, Hay, Brennan, & Wake, 2013) found inconsistent findings for the relation between self-esteem and physical appearance and obesity. Incledon et al. (2013) concluded that these inconsistencies may be explained by methodological variability. Concerning parental mental health—most commonly characterized by mother’s level of depression— the literature is inconsistent regarding its effect on child weight and some gender differences were noted. SES was also found to affect the relation between maternal depression and child weight, most often as an amplifier. The majority of studies were with samples of school age children with a few exceptions of slightly younger or older children.
Adolescents–Teenagers Stage
Gender differences are a key focus of research into the link between nutrition and eating behaviors and obesity in the adolescent and teenager stage (age 13–18 years). Among females, higher servings of sugar-sweetened beverages were positively associated with overweight while more servings of fruits and vegetables, lower total caloric intake, less fast food consumption, less availability of high-caloric snack foods at home, and eating take-out foods less frequently were negatively associated with overweight. Among males, eating fewer servings of snacks per day and breakfast consumption were associated with less likelihood of overweight. The effect of alcohol use on weight is also supported by a small body of research involving complex relationships with other factors, such as physical activity and gender. However, the findings are mixed. Numerous studies have demonstrated physical activity decreases significantly for both genders during adolescence as more time is spent in sedentary activities (Gortmaker et al., 2012; Troiano et al., 2008). Our findings support a positive relationship between sedentary time and BMI but support was mixed in our sample of studies and varied by gender, weight status, and type of weight status measure (e.g., BMI, skinfold, body fat). A few studies found no relationship between physical activity and weight.
There are potentially reciprocal relationships between measured body weight, perceived body weight, and depressive symptoms for adolescents. A number of studies have shown a positive relationship between depressive symptoms and overweight/obesity, both cross-sectionally and over time (Korczak, Lipman, Morrison, & Szatmari, 2013); however, reviews of this literature have revealed mixed conclusions (Incledon, Wake, & Hay, 2011). The findings of our review are in support of a positive relationship but with interactions with gender and race/ethnicity. Among obese female adolescents, there was an added effect of peer victimization or bullying contributing to greater depression and lower self-concept that led to higher BMI. This was not the case for obese male adolescents. There is some empirical evidence to support that the way youth perceive their weight and bodies in adolescence may lead to obesity. In general, body size overestimation, compared to accurate perception, and body dissatisfaction and weight concerns increase the risk of later overweight and greater growth in BMI.
A number of corollary health behaviors have a relationship with weight during this stage. Cigarette smoking was the most prevalent in our search, which is typically negatively related to BMI. Of note, two studies in our review found that smoking contributed to being overweight or obesity. Some evidence also suggests that obesity in adolescence increases risk for starting or continuing to use tobacco. As already mentioned, alcohol consumption is generally positively associated with weight gain and BMI. We identified very few studies that included use of illicit drugs and relations were not significant when controlling for other factors.
Parenting and Family Management
Our findings support a link between general family functioning, parent-child relationships, communication, and use of positive behavior support strategies on both weight and related health behaviors. However, this area of the literature is fairly small as it concerns longitudinal studies. A more robust area of study concerns the influence of general parenting styles, as opposed to the more specific feeding styles, on children’s diet, exercise behaviors, and weight. In a systematic review, Sleddens et al. (2011) concluded that children raised with an authoritative (warm and demanding) parenting style have a healthier diet, are more physically active, and have lower BMI’s than those raised with the other styles. Children of permissive or indulgent (high levels of warmth but less demanding) mothers, for example, have been found to be at an increased risk of excess weight. Feeding styles or practices—the strategies that parents use when feeding their children—have been found to prospectively predict eating behaviors and the child’s subsequent obesogenic eating behaviors. For example, emotional feeding (i.e., using food to calm) and encouragement positively relate to the child’s tendency to overeat and higher levels of instrumental feeding (i.e., using food as reward) are related to increases in their BMI.
The home food environment, which is a form of parental control over feeding, has been studied as it relates to childhood obesity, but the number of longitudinal studies is limited and very few studies examined how it relates to the anthropometric measurements of the child. Restrictive and pressuring feeding styles are two other types of parental control. The relation between restrictive feeding practices and weight is equivocal with studies finding an association with both weight gain and weight loss and differential effects on BMI depending on child age. It is important to note that the literature also suggests that the relation between child weight and feeding styles is bidirectional with higher child weight being related to more restrictive feeding practices over time and lower child weight relating to higher levels of pressuring to eat. Somewhat relatedly, the literature is inconclusive on how feeding practices change or remain stable across development.
The findings of our review provided inconsistent support for a link between parental modeling of health behaviors and childhood obesity. However, the broader literature generally supports the relationship between parental modeling and children’s health behaviors, particularly eating behaviors and physical activity. A few studies in our review supported a link between parental eating behaviors on child eating behaviors, but only one study examined the impact of parental modeling on child physical activity—no significant relationship was found.
Distal Ecological Influences
Harrison et al. (2011) proposed an ecological model integrating the latest research findings into a comprehensive and developmentally flexible model. As identified in this study, childhood obesity is influenced by biological and genetic factors, child characteristics, and the family context. It is necessary to underscore that these factors exist within systems including neighborhoods, institutions, communities, and macrosystems such as culture, values, and the broader economic and political environment. For example, characteristics of the biophysical and built environments, including neighborhood safety, proximity of supermarkets, and lower population density have been found to be closely related to child BMI (Dunton et al., 2012). However, Dunton et al.’s systematic review found that most studies are cross-sectional and that findings were inconsistent. This review also found that associations were moderated by gender, age, SES, and population density. A review of the etiology of childhood obesity cited two studies that found that lower priced fruits and vegetables have been related to lower BMI in youth and availability of high-caloric foods in schools has been related to higher BMI respectively (Spruijt‐Metz, 2011). This review also reported that there have been inconsistent findings between exposure to fast-food in neighborhoods and BMI, although exposure has been related to diet. Cultural factors, such as acculturation and proximate factors (i.e., diet, smoking, physical activity/inactivity), also impact childhood obesity. Cultural and social norms also impact child weight through beliefs about portion sizes and ideal body types (Harrison et al., 2011). State and federal policies establish regulations that impact resources and practices. These policies impact costs of healthy foods, food made available at schools, and what foods are marketed to children, which in turn influence child diet and adiposity (Harrison et al., 2011; Kraak, Liverman, Koplan, & Institute of Medicine and National Academies, 2005).
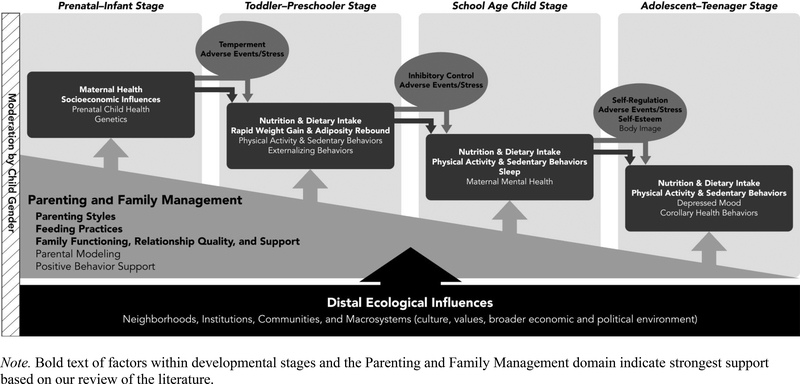
The Developmental Cascade Model of Pediatric Obesity
Figure 2 provides a conceptual developmental cascade model of pediatric obesity after refinement based on the findings of the scoping review, which posits: 1) key risk and protective factors are located within developmental stages; 2) parental influences and family management practices are displayed below to indicate their relevance across stages; 3) ovals in the figure connecting adjacent stages contain risk factors and processes that we hypothesize play a role in amplifying risk from one stage to the next and lead to a spreading of the effects across other risk factors (adverse events/stress, temperament, inhibitory control, self-regulation, self-esteem); 4) distal ecological factors are included below to acknowledge that the child and family constructs above are embedded within and affected by a broader system; and 5) differential effects based on gender should be considered for all links in the model as indicated by the vertical box on the left.
Figure 2.
Developmental cascade model of pediatric obesity
The degree of empirical support for each of the constructs in Figure 2 is depicted by bold font for those with robust support, defined by a clear relationship with excess weight gain, overweight, or obesity, and an ample number of methodologically-rigorous studies with representative samples to be generalizable. Determination of these two levels of evidence was made via consensus among the senior authors (JDS, SMS). They are as follows for each developmental stage: Prenatal–Infants Stage (maternal health, socioeconomic influences); Toddlers–Preschoolers (nutrition and dietary intake, rapid weight gain and adiposity rebound); School Age Children (nutrition and dietary intake, physical activity and sedentary behaviors), Adolescents–Teenagers (nutrition and dietary intake, physical activity and sedentary behaviors). With regard to parenting and family management factors, parenting styles, feeding practices, and family functioning, relationship quality, and support all had fairly robust empirical support in our review. Constructs not in bold have equivocal findings across studies and samples and/or we identified a limited number of methodically-rigorous studies with representative samples. Some predictors of excess weight gain and the development of obesity have far smaller bodies of research, or the findings are inconsistent across studies and samples, at least when published studies were limited to the criteria used in this review. These include the effect of maternal mental health and children’s externalizing behaviors in childhood. The link between certain genetic influences and weight gain, and adverse events and obesity, for example, are fairly strong but the amount of prospective longitudinal studies supporting each are relatively small.
Concerning amplifying factors, children’s capacity for self-regulation in childhood and preadolescence could moderate the relationship between eating behaviors and excess weight gain. Parenting and family management factors play a similar role within the cascade, with the ability to either inhibit the cascade or accelerate its progression. For example, monitoring a child or adolescent’s diet and physical activity behaviors could delay or prevent weight gain, whereas failure to do so could amplify excess weight gain. Finally, potential gender differences in the influence of certain constructs on obesity in childhood were important in many studies we reviewed. The literature is not sufficiently clear to state those relationships in the developmental cascade model that should be moderated by gender, but there is ample evidence to indicate that child gender is non-ignorable in a developmental model such as this and should thus be tested.
Discussion
The purpose of this scoping review was to provide researchers with a model of pediatric obesity from a developmental cascade perspective informed by existing theory, models of children’s health, and findings from the empirical literature. We used a model-building approach to propose a developmental cascade model that was then refined based on the results of a scoping review. In contrast to a systematic review, scoping reviews are intended to synthesize an exploratory research question in a defined area by mapping key concepts, types of evidence, and identifying gaps in research by systematically searching, selecting, and synthesizing existing knowledge (Colquhoun et al., 2014). Rather than capturing all available studies, this type of review is best suited for identifying a corpus of research that is representative of the knowledge in given area. Considering the success of such models in other areas (e.g., substance use), there is great potential for using this perspective to inform the field’s understanding of obesity development and preventive interventions. The developmental cascade model of pediatric obesity and the results of the review are useful for 1) conceptualizing the design of new studies that gather data in accord with the developmental cascade perspective, 2) analyzing existing datasets to answer research questions from this perspective, and 3) identifying, developing, and testing strategies to prevent obesity. The latter is made possible by marrying the findings of developmental cascade model research with the obesity intervention literature.
The developmental cascade model proposed here is a very flexible model that can be used to inform a broad range of developmental and intervention research hypotheses. These models are typically hypothesized based on empirical support of multiple individual links, or mediated relationships, in the existing literature. The developmental cascade model then tests whether these relationships are systematically linked to illuminate a long-term, multi-systemic developmental process. This synthesis alone is salient for developmental science, but the real potential of this perspective emerges when informing preventive interventions meant to disrupt the cascade. These implications are discussed later. First, we now discuss 1) potential methods for empirically testing the proposed cascade model of pediatric obesity; 2) the implications for health psychology and developmental and prevention sciences; and 3) the limitations of this review and future directions for this area of research.
Testing a Developmental Cascade Model
The conceptual developmental cascade model presented in Figure 2 is not necessarily intended to be an empirically testable model in its entirety due to the data requirements to do so, although such a test could be done. Rather, the model is intended to inform a plethora of hypotheses about the different pathways in which specific constructs contribute to obesity over time. The model contains a multitude of interactional processes. Our review identified some studies, albeit few, that suggest the existence of reciprocal relationships between certain constructs and weight-related outcomes. Self-esteem, depressed mood, and weight perception/body image, for example, have been found to both predict and be predicted by weight status, and findings are also somewhat mixed. Some aspects of dietary habits and nutritional intake have similar bidirectional findings reported in the literature, which begs for further inquiry given the paucity of studies specifically testing reciprocal relationships over time.
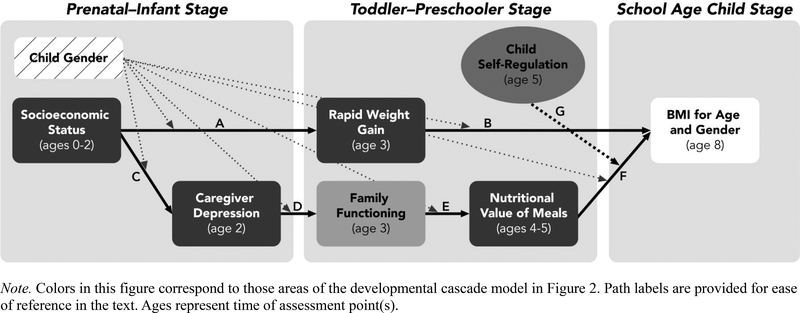
Concerning analytic strategies, previously published studies of developmental cascade models have relied primarily on path analysis with intervening variables performed in a structural equation modeling framework (Dishion et al., 2010; Dodge et al., 2008; Dodge et al., 2009). To illustrate a few of the analytic methods described in this section, we refer the reader to Figure 3. The paths are labeled with capital letters for ease of reference. Most analytic approaches for such models will begin with a form of mediation analysis. Many researchers will be familiar with the traditional mediational model where there is a significant direct effect of the predictor on the presumed mediator and on the distal outcome, a significant direct effect of the mediator on the distal outcome, and a significant indirect effect of the predictor on the outcome via the mediator (Judd, Kenny, & McClelland, 2001). However, tests of one mediating variable do not capture the interactions among multiple factors over time that are core to the developmental cascade model. MacKinnon, Lockwood, Hoffman, West, and Sheets (2002) describe an approach that focuses on the joint significance or product of coefficients of the paths from the predictor to the proposed mediators and from the mediators to the outcome. For example, the product of paths A and B in Figure 3. In the absence of a direct effect of the predictor on the outcome, MacKinnon et al. (2002) refer to the purported mediator as an intervening variable. Models with multiple intervening variables between the predictor and distal outcome are highly relevant to testing hypotheses from a developmental cascade perspective.
Figure 3.
Example of a hypothesized developmental cascade model
Consider one pathway in Figure 3 to test the hypothesis that lower SES (independent variable) between birth and age 2 is associated with higher maternal depression at age 2, which is predictive of poorer family functioning at age 3 and subsequently serving of less nutritious meals to the child between ages 4 and 5, putting the child at higher risk for an elevated BMI at age 8. The test of this pathway with three intervening variables would be the product of paths C, D, E, and F. In this example, the developmental cascade model could be very useful for identifying a pathway that links maternal depression to child BMI when that relationship is not direct or is weakly associated without the inclusion of intervening variables—in this case, family functioning and children’s meals. Additionally, the effects of a moderating variable (self-regulation) on a path(s) of interest could be considered in such a model. This is illustrated in Figure 3 by path G, which indicates a hypothesized effect on path F: the relationship between nutritional value of meals and BMI is stronger for children with lower levels of self-regulation relative to those with higher levels. Concerning moderation, an important finding that emerged in our review is the effect of child gender on numerous links in the model. Figure 3 depicts with unlabeled dashed lines the way in which gender is tested as a moderator of all links in the specified model.
Another potential situation is the case of a variable being tested as a predictor in the cascade or as an amplifier of developmental cascade processes. This is not depicted in Figure 3. An example of this is adverse childhood experiences. There is a growing body of evidence suggesting a relationship between adverse events in childhood and later weight status (Hemmingsson, Johansson, & Reynisdottir, 2014). However, the majority of the studies in the meta-analysis, 19 of 23, were based on retrospective reports of adverse events in childhood (reported in early or later adulthood), meaning that testing as a predictor in a longitudinal model violates a number of assumptions for attributing causality. The researcher could, however, test whether retrospective assessments of adverse events in childhood (collected in adolescence or adulthood) acted to amplify specific pathways in the model using moderation analysis. Thus, adverse events would be tested similarly to the way self-regulation is in the example in Figure 3.
Many variations of longitudinal data analysis used in developmental science (Collins, 2006; Selig & Preacher, 2009; Singer & Willett, 2003) can be applied to test hypotheses from a developmental cascade perspective. Although few examples exist for developmental cascade models specifically, researchers can apply variants of path analysis, latent growth, parallel process, cross-lag panel, and multilevel models to answer such questions. As is typically the case, the modeling approach should be determined by the hypotheses being tested and the available data. A monograph by Dodge et al. (2009) provides a detailed description of the process used to build and test a developmental cascade model using longitudinal data. Dodge et al. also demonstrate a useful estimate derived from their model—they found that by 12th grade, children who accumulated each of the risk factors in the hypothesized cascade had a 91% chance of using illicit substances, compared with a population base rate of 51%. The analytic methods and principles they describe can be applied to a developmental cascade model of pediatric obesity.
As is evident in Figures 2 and 3, the type of data required to test such a model is longitudinal with variables assessed either at one or more specific points in time (i.e., ages of the child) or at evenly-spaced intervals over time when hypothesizing a latent or parallel growth process and sufficient sample sizes to ensure both power and model fit. We hope researchers will begin to test developmental cascade models of pediatric obesity using existing longitudinal datasets to inform new studies and lend further rationale for scheduling assessments across developmental stages.
Implications of the Developmental Cascade Model for Pediatric Obesity Intervention Development and Testing: Focus on Family-Based Constructs and Influences
Developmental cascade models can provide a roadmap for interventionists as they identify salient and modifiable risk and protective factors at specific developmental stages. For children and adolescents, it is crucial to recognize the importance of the biopsychosocial model when intervening (Nguyen & Bera, 2016), and the model presented aligns well with this imperative. Although intraindividual pathways are critical for understanding development of obesity, intervention research consistently demonstrates that involvement of caregivers (e.g., parents) is critical for achieving meaningful and long-lasting prevention effects. From a developmental perspective, there is fairly strong evidence of the influence of the family environment, family management, and parenting on children’s weight gain across development. It has also been well established that involving parents and the home setting in interventions are the most effective (Jang, Chao, & Whittemore; McLean, Griffin, Toney, & Hardeman, 2003). This finding clearly emerged as a salient and malleable target for intervention across stages of development and is potentially the key to disrupting the cascade of obesity in youth. For example, general parenting styles and behaviors have been linked to risk for overweight and obesity as well as more specific health behaviors, such as the consumption of fruits and vegetables. The findings of our review support the general consensus among experts in obesity prevention that interventions ought to be family-centered and target parent- and family-level mechanisms of action to affect the weight gain of the child (Barr-Anderson, Adams-Wynn, DiSantis, & Kumanyika, 2013; Gerards, Sleddens, Dagnelie, de Vries, & Kremers, 2011; Golley, Hendrie, Slater, & Corsini, 2011; Janicke et al., 2014; Monasta et al., 2011; Sleddens et al., 2011; Staniford, Breckon, & Copeland, 2012; Sung-Chan, Sung, Zhao, & Brownson, 2013; Whitlock, O’Connor, Williams, Beil, & Lutz, 2010). The results of this review suggest that it is essential to target parental effects in childhood and adolescence. We focus on this aspect of the model in this section as these variables may be the most readily translated to effective interventions to prevent obesity and excess weight gain (Brotman et al., 2012; Power et al., 2013; Smith, St. George, et al., 2017).
One challenge we faced when it came to searching and reviewing the literature on parenting influences was placing specific practices in developmental stages, as had been done with other variables, because many parenting practices are relevant across development—the specific behavior or skill differs however to be developmentally appropriate. For this reason, we elected to organize the section on Family Management and Parenting by its general component constructs across stages, rather than by specific developmental stage, and to highlight where appropriate what ages the construct seems most relevant and how the parenting construct differs when applied to younger versus older youth. This strategy is consistent with the way developmental cascade models have been used to inform prevention (Dishion & Patterson, 2016).
Parenting styles have been studied extensively relative to parenting and family management practices. This research indicates that authoritative parenting style is associated with healthier weight and eating behaviors. Feeding styles—the strategies that parents use when feeding their children— and parental modeling of eating behaviors also have fairly sizeable bodies of research. Feeding style is clearly related to child eating behaviors, which have been linked to youth’s weight status by other research, and the literature suggests that this relationship is bidirectional. The findings concerning the influence of parental modeling of eating behaviors, dietary intake, and physical activity on child behaviors and weight is somewhat inconsistent however. Despite some support for these links, there are clear confounding factors such as food availability and genetic risk. Given that a recent genome-wide association study with 339,224 individuals, found that common variation accounts for >20% of BMI variation (Locke et al., 2015), more research appears needed to understand the behavioral genetics and epigenetics that contribute to obesity. We found little research in this area that was multivariate and controlled for other potential predictors. Nonetheless, in the context of intervention for childhood obesity, parenting behaviors are of critical importance. With this in mind, we sought to focus on parent behaviors that are observable and modifiable.
Baranowski et al. (2013) pointed out that the concept and measurement of parenting styles is not very conducive to behavioral intervention. Thus, we borrowed from decades of research in parent management training interventions to identify observable parenting behaviors that are known to be modifiable via the broad class of interventions known as parent training (Forgatch, Patterson, & Gewirtz, 2013) that focus on strengthening particular parenting skills, such as positive behavior support (e.g., positive reinforcement, clear expectations) and consistent consequences for rule violations. This approach likely limited our search results, but we argue that this is an important direction for the field. Specifically, more high quality research is needed to further explore the potential benefits of positive behavior support strategies and the proactive structuring of the child’s environment to promote healthy lifestyle behaviors by anticipating the child’s needs and increasing facilitators of success, as there appears to be a dearth of longitudinal studies examining the role of positive behavior support in promoting youth’s health behaviors. The two empirical studies identified were conducted by authors of this review paper (JDS and ZM). However, this construct is broad in its scope by definition. As such, other studies could use measures that approximate positive behavior support behaviors but not by name. Inconsistent naming of parenting constructs is an issue across the literature (Sandler, Ingram, Wolchik, Tein, & Winslow, 2015) and not unique to childhood obesity research.
Parental monitoring of child’s dietary intake and physical activity is a common target of family-based interventions aimed at reducing childhood obesity (Ayala et al., 2010). Given that our search yielded only two studies in this domain, more longitudinal research examining the long-term effects of monitoring on child weight appears warranted. Among our search results, all studies focused on parental monitoring of diet (not activity) and there are mixed findings regarding the association with child weight. Thus, there is a need for research examining relations between monitoring and physical activity, as well as screen time and other forms of sedentary activity. One important note is the implicit, and sometimes explicit, relation between parenting and feeding styles and monitoring of youth behaviors. For example, permissive feeding and parenting styles would inherently suggest low monitoring and control of child eating and physical activity, but they are rarely teased apart. Therein lies the challenge of translating styles to actual behaviors for targeted intervention, and it begs the question of whether interventions are likely to succeed by targeting parental monitoring of diet and activity only without providing support for more fundamental changes in general parenting skills. This issue is described in some detail by Smith, St. George, and Prado (2017) concerning the use of parenting interventions for obesity.
There is also limited but clear support for an effect of general family functioning and related constructs (e.g., parent-child relationship quality, familial support) on child weight (Halliday, Palma, Mellor, Green, & Renzaho, 2013). This relationship has been found in correlational studies where children and adolescents who are overweight/obese have poorer family functioning compared to healthy weight peers (Smith, Montaño, Maynard, & Miloh, 2017; Zeller et al., 2007). These domains are the primary targets of efficacious parent training programs for child behavior problems, but it is not clear to what extent they are explicitly addressed in family-centered interventions for childhood obesity, which typically focus on specific healthy lifestyle behaviors, such as physical activity and diet. Ecological models of childhood obesity intervention suggest that these more general family factors impede or facilitate implementing healthy lifestyle behavior change (Kitzman-Ulrich et al., 2010) and should thus be targeted for intervention. Other ecological influences can affect the effectiveness of family-centered obesity interventions. For example, family adversity (psychosocial risk) and maternal depression were associated with failure in a family lifestyle intervention for children who were overweight or obese (Froehlich, Pott, Albayrak, Hebebrand, & Pauli-Pott, 2011).
Finally, several authors of this paper are concurrently conducting a systematic review of the literature on preventive interventions for obesity across development. We have identified a total of 64 randomized controlled trials that report immediate (post intervention) and sustained effects ( ≥ 6 months post intervention) on weight status and/or related health behaviors (e.g., physical activity, sedentary behavior, diet) (St. George et al., manuscript in development). Despite the developmental cascade model’s emphasis on the importance of earlier stages, only four and 10 of the 64 identified interventions were evaluated with infants and toddlers/preschoolers, respectively. The rest of the trials were evaluated with children and adolescents. Preliminary findings indicate that interventions including infants and toddlers/preschoolers rely largely on universal prevention strategies, are delivered at the family level, and target early feeding practices and positive parenting skills. Interventions evaluated with infants and toddlers/preschoolers were more likely to demonstrate significant improvements in child diet-related outcomes than on weight-related outcomes, sedentary behavior or physical activity. Approximately half of the interventions evaluated with school-age children and adolescents/teenagers were school-based and used universal prevention approaches (e.g., school curriculum changes); on the other hand, interventions in these stages classified as “selected” or “indicated” prevention tended to involve the family for more intensive lifestyle modification. Results of studies evaluated with children and adolescents/teenagers were mixed, with observed immediate effects on outcomes usually wearing off by follow up assessments. While existing interventions generally seem to include some relevant developmental constructs (e.g., parent feeding practices), others are largely missing (e.g., family functioning, positive behavior support). The developmental cascade model suggests well-timed interventions that target key mediating variables stand to have the greatest impact. Yet, few of the interventions included in the review tested for relevant mediation and/or moderation effects (e.g., < 25% of the prenatal-infancy and early childhood interventions). Paired with the developmental cascade perspective presented in this paper, the findings of this review could elucidate some potential reasons that interventions have failed to produce meaningful or sustained effects. For example, the developmental cascade model suggests that intervention failure could be the result of a narrow focus on one level of the system (e.g., child behaviors alone) whereas the development of obesity is multidetermined and accumulative, suggesting targeting multiple constructs across levels (i.e., parent and child) in developmentally specific ways and over time in a dynamic manner.
Limitations and Future Directions
The results of this scoping review need to be considered in the context of three limitations. First, the search strategy combined a large number of key words and limiters that aided us in narrowing a very large literature base to a sample of highly relevant published studies. This approach values identifying a high proportion of relevant studies as opposed to other review methods that value identification of a high number of results that contain the majority of relevant studies, but also contain a large number of irrelevant studies that are discarded during the review process. This is evident in our final proportion of retained studies (23.6%). Relatedly, the inclusion of only longitudinal studies could perhaps obfuscate areas of research that appear limited in this review but otherwise appear in the literature as correlational studies, which can also be informative to generating hypotheses for longitudinal research. We also recognize that relevant studies have been published in the time since we completed our review of the literature.
Second, by design, our search could have missed studies of the relationships between intervening constructs in the model when obesity was not an outcome but the relationships between constructs could be predictive of weight gain further down the developmental cascade. For example, studies of the effects of adverse events in childhood on later depressive symptoms likely would have been missed if that study was not concerned in any way with obesity or dietary behaviors. This literature could however be consulted when hypothesizing cascade models.
Third, this review focused on the proximal influences on childhood weight and less attention was given to ecological influences on weight, such as the neighborhoods and communities in which children and families are embedded, cultural and societal norms and attitudes, political policies, and other factors (Maziak, Ward, & Stockton, 2008). These are described in greater detail in existing models of childhood obesity (Davison & Birch, 2001; Harrison et al., 2011). Interventions at these distal ecological levels include legislative policies to improve school lunches and change the school food environment. Neighborhood, community, and cultural factors are intertwined with sociodemographics, which contributes, in part, to the disproportionate rates and effect of obesity on low-income and racial/ethnic minority populations in developed countries (Singh, Siahpush, & Kogan, 2010). For these reasons, there is a significant emphasis on social determinants of childhood obesity in the literature (Braveman, Egerter, & Williams, 2011; Patrick & Nicklas, 2005). One reason we did not focus on these influences is that they are less conducive to evaluation within a developmental cascade model because they are largely static factors that lend themselves better to analysis of moderation rather than mediation or as an intervening variable. Notwithstanding, the ways in which these factors precipitate the cascade are important to understanding developmental processes and identifying potential intervention strategies. Two ways to integrate distal ecological factors into the analysis of developmental cascade models is to test these influences as moderators or in multilevel models. This will be useful in advancing personalized intervention approaches as the question of “what works for whom and in what settings?” becomes more clear.
Conclusions
This article provides a theory-driven and empirically-informed basis to begin investigating and conceptualizing pediatric obesity as a cascading process across development, which has proven its utility for informing effective preventive interventions in other areas of behavioral health. Myriad longitudinal evaluations can be conducted on the basis of the proposed developmental cascade model in Figure 2. The extent to which data sets exist to do so is unclear given that they were not necessarily designed to obtain the data needed to test a developmental cascade model, which would involve repeated assessments over long stages of time with hypothesized mediators collected at specified points in development. One thing that is clear is that more research is needed to both test, and likely expand upon, the hypothesized causal relationships in the model.
Our proposed developmental cascade model can inform the design of new longitudinal studies of obesity by specifying a sequence of constructs and relevant amplifiers based on a part of the larger cascade model. Apart from the contribution of the developmental cascade perspective, the findings of our review also point to potential areas in need of general inquiry. Not surprisingly, an area of research that needs more empirical study is the influence of specific and observable parenting behaviors that can be modified through intervention. Integration of the findings of randomized intervention trials, particularly as it concerns the mediating role of parenting factors, would augment the sparse developmental literature that was the focus of our review. Using longitudinal intervention trials to inform epidemiologic and developmental research has a long history (Brown & Liao, 1999; Kellam & Rebok, 1992). We urge researchers studying normative developmental processes and obesity prevention strategies to consider using the developmental cascade perspective. We believe this will further the science and speed translation of basic developmental research into actionable interventions to reverse the obesity epidemic in developed countries around the world.
Supplementary Material
Acknowledgments.
Justin Smith was supported by the National Center for Chronic Disease Prevention and Health Promotion of the Centers of Disease Control and Prevention under grant DP006255, awarded to Justin Smith and Cady Berkel. Sara. St. George was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under grant HL133521. The authors thank Krystal Baker, Mariah Meachum, and Sarah Krennerich for their assistance with the study and the preparation of the manuscript, and Brook Belay and Andrea Graham for feedback on an earlier draft of the manuscript.
Footnotes
Competing Interests. The authors have no competing interests or financial relationships, real or perceived, relevant to this article.
References
- Angle S, Keskinen S, Lapinleimu H, Helenius H, Raittinen P, Ronnemaa T, & Simell O (2005). Weight gain since infancy and prepubertal body dissatisfaction. Archives of Pediatrics & Adolescent Medicine, 159(6), 567–571. doi: 10.1001/archpedi.159.6.567 [DOI] [PubMed] [Google Scholar]
- Ayala GX, Elder JP, Campbell NR, Arredondo E, Baquero B, Crespo NC, & Slymen DJ (2010). Longitudinal Intervention Effects on Parenting of the Aventuras para Ninos Study. American Journal of Preventive Medicine, 38(2), 154–162. doi: 10.1016/j.amepre.2009.09.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baranowski T, O’connor T, Hughes S, Sleddens E, Beltran A, Frankel L,… Baranowski J (2013). Houston… We have a problem! Measurement of parenting: Mary Ann Liebert, Inc; 140 Huguenot Street, 3rd Floor New Rochelle, NY 10801 USA. [Google Scholar]
- Barker DJP (2004). The developmental origins of adult disease. Journal of the American College of Nutrition, 23(sup6), 588S–595S. doi: 10.1080/07315724.2004.10719428 [DOI] [PubMed] [Google Scholar]
- Barr-Anderson DJ, Adams-Wynn AW, DiSantis KI, & Kumanyika S (2013). Family-focused physical activity, diet and obesity interventions in African–American girls: a systematic review. Obesity Reviews, 14(1), 29–51. doi: 10.1111/j.1467-789X.2012.01043.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belloc N, & Breslow NE (1972). Relationship of physical health status and health practices. Preventive Medicine, 1, 409–421. [DOI] [PubMed] [Google Scholar]
- Bergmeier H, Skouteris H, Horwood S, Hooley M, & Richardson B (2014). Child temperament and maternal predictors of preschool children’s eating and body mass index. A prospective study. Appetite, 74, 125–132. doi: 10.1016/j.appet.2013.12.006 [DOI] [PubMed] [Google Scholar]
- Braveman P, Egerter S, & Williams DR (2011). The social determinants of health: coming of age. Annual review of public health, 32, 381–398. doi: 10.1146/annurev-publhealth-031210-101218 [DOI] [PubMed] [Google Scholar]
- Brotman LM, Dawson-McClure S, Huang K-Y, Theise R, Kamboukos D, Wang J,… Ogedegbe G (2012). Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics, 129(3), e621–e628. doi: 10.1542/peds.2011-1568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CH, & Liao J (1999). Principles for designing randomized preventive trials in mental health: An emerging developmental epidemiology paradigm. American journal of community psychology, 27(5), 673–710. doi: 10.1023/A:1022142021441 [DOI] [PubMed] [Google Scholar]
- Child Development Institute. (2017). The ages and stages of child development. Retrieved from https://childdevelopmentinfo.com/ages-stages/-.WRyL3VMrJmq
- Collins LM (2006). Analysis of longitudinal data: The integration of theoretical model, temporal design, and statistical model. Annu. Rev. Psychol, 57, 505–528. doi: 10.1146/annurev.psych.57.102904.190146 [DOI] [PubMed] [Google Scholar]
- Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L,… Moher D (2014). Scoping reviews: time for clarity in definition, methods, and reporting. Journal of Clinical Epidemiology, 67(12), 1291–1294. doi: 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- Davison KK, & Birch LL (2001). Childhood overweight: A contextual model and recommendations for future research. Obesity Reviews, 2(3), 159–171. doi: 10.1046/j.1467-789x.2001.00036.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denzer C, Reithofer E, Wabitsch M, & Widhalm K (2004). The outcome of childhood obesity management depends highly upon patient compliance. European Journal of Pediatrics, 163(2), 99–104. doi: 10.1007/s00431-003-1376-7 [DOI] [PubMed] [Google Scholar]
- Dishion TJ, & Patterson GR (1999). Model-building in development psychopathology: A pragmatic approach to understanding and intervention. Journal of Clinical Child Psychology, 28(4), 502–512. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, & Patterson GR (2016). The development and ecology of antisocial behavior: Linking etiology, prevention, and treatment Developmental Psychopathology: John Wiley & Sons, Inc. [Google Scholar]
- Dishion TJ, Véronneau M-H, & Myers MW (2010). Cascading peer dynamics underlying the progression from problem behavior to violence in early to late adolescence. Development and Psychopathology, 22(Special Issue 03), 603–619. doi:doi: 10.1017/S0954579410000313 [DOI] [PubMed] [Google Scholar]
- Dodge KA, Greenberg MT, Malone PS, & Conduct Problems Prevention Research, G. (2008). Testing an idealized dynamic cascade model of the development of serious violence in adolescence. Child Development, 79(6), 1907–1927. doi: 10.1111/j.1467-8624.2008.01233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Malone PS, Lansford JE, Miller S, Pettit GS, & Bates JE (2009). A dynamic cascade model of the development of substance-use onset: Early peer relations problem factors. Monographs of the Society for Research in Child Development, 74(3), 51–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Magnuson K, & Votruba-Drzal E (2017). Moving beyond correlations in assessing the consequences of poverty. Annual Review of Psychology, 68(1), 413–434. doi: 10.1146/annurev-psych-010416-044224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunton G, McConnell R, Jerrett M, Wolch J, Lam C, Gilliland F, & Berhane K (2012). Organized Physical Activity in Young School Children and Subsequent 4-Year Change in Body Mass Index. Archives of Pediatrics & Adolescent Medicine, 166(8), 713–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J,… Centers for Disease Control and Prevention. (2012). Youth risk behavior surveillance - United States, 2011. Morbidity and mortality weekly report. Surveillance summaries (Washington, DC: 2002), 61(4), 1–162. [PubMed] [Google Scholar]
- Engel G (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129–136. [DOI] [PubMed] [Google Scholar]
- Faith MS, Van Horn L, Appel LJ, Burke LE, Carson JAS, Franch HA,… Wylie-Rosett J (2012). Evaluating parents and adult caregivers as “agents of change” for treating obese children: Evidence for parent behavior change strategies and research gaps: a scientific statement from the American Heart Association. Circulation, 125(9), 1186–1207. doi: 10.1161/CIR.0b013e31824607ee [DOI] [PubMed] [Google Scholar]
- Fatima Y, & Mamun A (2015). Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias‐adjusted meta‐analysis. Obesity Reviews, 16(2), 137–149. doi: 10.1111/obr.12245 [DOI] [PubMed] [Google Scholar]
- Finkelstein EA, Graham WCK, & Malhotra R (2014). Lifetime direct medical costs of childhood obesity. Pediatrics, 133(5), 854–862. doi: 10.1542/peds.2014-0063 [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Patterson GR, & Gewirtz AH (2013). Looking Forward: The Promise of Widespread Implementation of Parent Training Programs. Perspect Psychol Sci, 8(6), 682–694. doi: 10.1177/1745691613503478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisen A, Lunde C, & Berg AI (2015). Developmental patterns in body esteem from late childhood to young adulthood: A growth curve analysis. European Journal of Developmental Psychology, 12(1), 99–115. doi: 10.1080/17405629.2014.951033 [DOI] [Google Scholar]
- Froehlich G, Pott W, Albayrak O, Hebebrand J, & Pauli-Pott U (2011). Conditions of Long-term Success in a Lifestyle Intervention for Overweight and Obese Youths. Pediatrics, 128(4), E779–E785. doi: 10.1542/peds.2010-3395 [DOI] [PubMed] [Google Scholar]
- Gerards SMPL, Sleddens EFC, Dagnelie PC, de Vries NK, & Kremers SPJ (2011). Interventions addressing general parenting to prevent or treat childhood obesity. International Journal of Pediatric Obesity, 6(2Part2), e28–e45. doi: 10.3109/17477166.2011.575147 [DOI] [PubMed] [Google Scholar]
- Gillman MW (2005). Developmental origins of health and disease. New England Journal of Medicine, 353(17), 1848–1850. doi:doi: 10.1056/NEJMe058187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz DR, & Caron W (1999). A biopsychosocial model for youth obesity: consideration of an ecosystemic collaboration. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity, 23 Suppl 2, S58–64. doi: 10.1038/sj.ijo.0800861 [DOI] [PubMed] [Google Scholar]
- Golley RK, Hendrie GA, Slater A, & Corsini N (2011). Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns – what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obesity Reviews, 12(2), 114–130. doi: 10.1111/j.1467-789X.2010.00745.x [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Lee R, Cradock AL, Sobol AM, Duncan DT, & Wang YC (2012). Disparities in youth physical activity in the United States: 2003–2006. Medicine and Science in Sports and Exercise, 44(5), 888–893. doi: 10.1249/mss.0b013e31823fb254 [DOI] [PubMed] [Google Scholar]
- Halliday JA, Palma CL, Mellor D, Green J, & Renzaho AMN (2013). The relationship between family functioning and child and adolescent overweight and obesity: a systematic review. International Journal of Obesity, 38, 480. doi: 10.1038/ijo.2013.213 [DOI] [PubMed] [Google Scholar]
- Han JC, Lawlor DA, & Kimm SYS (2010). Childhood obesity. The Lancet, 375(9727), 1737–1748. doi: 10.1016/S0140-6736(10)60171-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, Kim J,… Jacobsohn GC (2011). Toward a developmental conceptualization of contributors to overweight and obesity in childhood: The Six-Cs model. Child Development Perspectives, 5(1), 50–58. doi: 10.1111/j.1750-8606.2010.00150.x [DOI] [Google Scholar]
- Harrist AW, Topham GL, Hubbs‐Tait L, Page MC, Kennedy TS, & Shriver LH (2012). What developmental science can contribute to a transdisciplinary understanding of childhood obesity: an interpersonal and intrapersonal risk model. Child Development Perspectives, 6(4), 445–455. [Google Scholar]
- Hemmingsson E, Johansson K, & Reynisdottir S (2014). Effects of childhood abuse on adult obesity: a systematic review and meta‐analysis. Obesity Reviews, 15(11), 882–893. doi: 10.1111/obr.12216 [DOI] [PubMed] [Google Scholar]
- Incledon E, Gerner B, Hay M, Brennan L, & Wake M (2013). Psychosocial Predictors of 4-Year BMI Change in Overweight and Obese Children in Primary Care. Obesity, 21(3), E262–E270. doi: 10.1002/oby.20050 [DOI] [PubMed] [Google Scholar]
- Incledon E, Wake M, & Hay M (2011). Psychological predictors of adiposity: Systematic review of longitudinal studies. International Journal of Pediatric Obesity, 6(2–2), E1–E11. doi: 10.3109/17477166.2010.549491 [DOI] [PubMed] [Google Scholar]
- Jang M, Chao A, & Whittemore R Evaluating intervention programs targeting parents to manage childhood overweight and obesity: A systematic review using the RE-AIM framework. Journal of Pediatric Nursing: Nursing Care of Children and Families, 30(6), 877–887. doi: 10.1016/j.pedn.2015.05.004 [DOI] [PubMed] [Google Scholar]
- Janicke DM, Steele RG, Gayes LA, Lim CS, Clifford LM, Schneider EM,… Westen S (2014). Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. Journal of Pediatric Psychology. doi: 10.1093/jpepsy/jsu023 [DOI] [PubMed] [Google Scholar]
- Judd CM, Kenny DA, & McClelland GH (2001). Estimating and testing mediation and moderation in within-subject designs. Psychological methods, 6(2), 115. [DOI] [PubMed] [Google Scholar]
- Kellam SG, & Rebok GW (1992). Building developmental and etiological theory through epidemiologically based preventive intervention trials. [Google Scholar]
- Kitzman-Ulrich H, Wilson D, George S, Lawman H, Segal M, & Fairchild A (2010). The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clinical Child and Family Psychology Review, 13(3), 231–253. doi: 10.1007/s10567-010-0073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korczak DJ, Lipman E, Morrison K, & Szatmari P (2013). Are children and adolescents with psychiatric illness at risk for increased future body weight? A systematic review. Developmental Medicine and Child Neurology, 55(11), 980–987. doi: 10.1111/dmcn.12168 [DOI] [PubMed] [Google Scholar]
- Kraak VA, Liverman CT, Koplan JP, & Institute of Medicine and National Academies. (2005). Preventing childhood obesity: health in the balance: National Academies Press. [PubMed] [Google Scholar]
- Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR,… Speliotes EK (2015). Genetic studies of body mass index yield new insights for obesity biology. Nature, 518, 197–206. doi: 10.1038/nature14177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological methods, 7(1), 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and Psychopathology, 22(3), 491. doi: 10.1017/S0954579410000222 [DOI] [PubMed] [Google Scholar]
- May AL, Kuklina EV, & Yoon PW (2012). Prevalence of cardiovascular disease risk factors among US adolescents, 1999− 2008. Pediatrics, 129(6), 1035–1041. doi: 10.1542/peds.2011-1082 [DOI] [PubMed] [Google Scholar]
- Maziak W, Ward K, & Stockton M (2008). Childhood obesity: are we missing the big picture? Obesity Reviews, 9(1), 35–42. [DOI] [PubMed] [Google Scholar]
- McLean N, Griffin S, Toney K, & Hardeman W (2003). Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. International Journal of Obesity, 27, 987. doi: 10.1038/sj.ijo.0802383 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group P (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS med, 6(7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monasta L, Batty G, Macaluso A, Ronfani L, Lutje V, Bavcar A,… Cattaneo A (2011). Interventions for the prevention of overweight and obesity in preschool children: A systematic review of randomized controlled trials. Obesity Reviews, 12(5), e107–e118. [DOI] [PubMed] [Google Scholar]
- Monteiro POA, & Victora CG (2005). Rapid growth in infancy and childhood and obesity in later life – a systematic review. Obesity Reviews, 6(2), 143–154. doi: 10.1111/j.1467-789X.2005.00183.x [DOI] [PubMed] [Google Scholar]
- Moreno LA, & Rodríguez G (2007). Dietary risk factors for development of childhood obesity. Current Opinion in Clinical Nutrition & Metabolic Care, 10(3), 336–341. doi: 10.1097/MCO.0b013e3280a94f59 [DOI] [PubMed] [Google Scholar]
- Nader PR, O’Brien M, Houts R, Bradley R, Belsky J, Crosnoe R,… Susman EJ (2006). Identifying risk for obesity in early childhood. Pediatrics, 118(3), e594–e601. doi: 10.1542/peds.2005-2801 [DOI] [PubMed] [Google Scholar]
- National Research Council and Institute of Medicine. (2011). Early childhood obesity prevention policies. Washington, DC: The National Academies Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C,… Gakidou E (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 384(9945), 766–781. doi: 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen C, & Bera K (2016). Bio-Psycho-Social Approach to the Treatment of Childhood Obesity: A Novel Technique. Journal of Childhood Obesity. [Google Scholar]
- Nianogo RA, & Arah OA (2015). Agent-based modeling of noncommunicable diseases: A systematic review. American Journal of Public Health, 105(3), e20–e31. doi: 10.2105/AJPH.2014.302426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, & Flegal KM (2016). Trends in obesity prevalence among children and adolescents in the united states, 1988–1994 through 2013–2014. JAMA, 315(21), 2292–2299. doi: 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parizkova J (2014). Fatness and fitness related to exercise in normal and obese children and adolescents. Journal of King Saud University Science, 26(4), 245–253. doi: 10.1016/j.jksus.2014.03.002 [DOI] [Google Scholar]
- Parsons TJ, Power C, Logan S, & Summerbell CD (1999). Childhood predictors of adult obesity: a systematic review. International Journal of Obesity, 23, S1–S107. [PubMed] [Google Scholar]
- Patrick H, & Nicklas TA (2005). A review of family and social determinants of children’s eating patterns and diet quality. Journal of the American College of Nutrition, 24(2), 83–92. [DOI] [PubMed] [Google Scholar]
- Perez-Escamilla R, Obbagy JE, Altman JM, Essery EV, McGrane MM, Wong YP,… Williams CL (2012). Dietary Energy Density and Body Weight in Adults and Children: A Systematic Review. Journal of the Academy of Nutrition and Dietetics, 112(5), 671–684. doi: 10.1016/j.jand.2012.01.020 [DOI] [PubMed] [Google Scholar]
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, & McEwen SA (2014). A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Research Synthesis Methods, 5(4), 371–385. doi: 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power C, & Parsons T (2000). Nutritional and other influences in childhood as predictors of adult obesity. Proceedings of the Nutrition Society, 59(2), 267–272. doi: 10.1017/s002966510000029x [DOI] [PubMed] [Google Scholar]
- Power TG, Sleddens EFC, Berge J, Connell L, Govig B, Hennessy E,… St. George SM (2013). Contemporary research on parenting: Conceptual, methodological, and translational issues. Childhood Obesity, 9(s1), S87–S94. doi: 10.1089/chi.2013.0038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I,… Sherriff A (2005). Early life risk factors for obesity in childhood: Cohort study. British Medical Journal, 330, 1357–1364. doi: 10.1136/bmj.38470.670903.E0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogosch FA, Oshri A, & Cicchetti D (2010). From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychopathology, 22(04), 883–897. doi: 10.1017/S0954579410000520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Ingram A, Wolchik SA, Tein J-Y, & Winslow EB (2015). Long-term effects of parenting-focused preventive interventions to promote resilience of children and adolescents. Child Development Perspectives, 9(3), 164–171. doi: 10.1111/cdep.12126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Schoenfelder EN, Wolchik SA, & MacKinnon DP (2011). Long-term impact of prevention programs to promote effective parenting: Lasting effects but uncertain processes. Annual Review of Psychology, 62, 299–329. doi: 10.1146/annurev.psych.121208.131619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapienza JK, & Masten AS (2011). Understanding and promoting resilience in children and youth. Current Opinion in Psychiatry, 24(4), 267–273. doi: 10.1097/YCO.0b013e32834776a8 [DOI] [PubMed] [Google Scholar]
- Selig JP, & Preacher KJ (2009). Mediation models for longitudinal data in developmental research. Research in Human Development, 6(2–3), 144–164. [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence: Oxford university press. [Google Scholar]
- Singh GK, Siahpush M, & Kogan MD (2010). Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health affairs, 29(3), 503–512. doi: 10.1377/hlthaff.2009.0730 [DOI] [PubMed] [Google Scholar]
- Sitnick SL, Shaw DS, & Hyde LW (2014). Precursors of adolescent substance use from early childhood and early adolescence: Testing a developmental cascade model. Development and Psychopathology, 26(01), 125–140. doi:doi: 10.1017/S0954579413000539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleddens EFC, Gerards SMPL, Thijs C, de Vries NK, & Kremers SPJ (2011). General parenting, childhood overweight and obesity-inducing behaviors: A review. International Journal of Pediatric Obesity, 6(2Part2), e12–e27. doi: 10.3109/17477166.2011.566339 [DOI] [PubMed] [Google Scholar]
- Smith JD, Montaño Z, Maynard A, & Miloh T (2017). Family Functioning Predicts Body Mass Index and Biochemical Levels of Youths with Nonalcoholic Fatty Liver Disease. Journal of Developmental & Behavioral Pediatrics, 38(2), 155–160. doi: 10.1097/dbp.0000000000000379 [DOI] [PubMed] [Google Scholar]
- Smith JD, St. George SM, & Prado G (2017). Family-centered positive behavior support interventions in early childhood to prevent obesity. Child Development, 88(2), 427–435. doi: 10.1111/cdev.12738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spengler S, Mess F, Schmocker E, & Woll A (2014). Longitudinal associations of health-related behavior patterns in adolescence with change of weight status and self-rated health over a period of 6 years: results of the MoMo longitudinal study. BMC pediatrics, 14. doi: 10.1186/1471-2431-14-242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruijt‐Metz D (2011). Etiology, treatment, and prevention of obesity in childhood and adolescence: A decade in review. Journal of Research on Adolescence, 21(1), 129–152. doi: 10.1111/j.1532-7795.2010.00719.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- St. George SM, Agosto Y, Molleda L, Soares M, Bahamon M, Prado G, & Smith JD (manuscript in development). A developmental cascade perspective of pediatric obesity: A systematic review of preventive interventions from infancy through late adolescence.. [DOI] [PMC free article] [PubMed]
- Staniford LJ, Breckon JD, & Copeland RJ (2012). Treatment of Childhood Obesity: A Systematic Review. Journal of Child and Family Studies, 21(4), 545–564. doi: 10.1007/s10826-011-9507-7 [DOI] [Google Scholar]
- Stout SA, Espel EV, Sandman CA, Glynn LM, & Davis EP (2015). Fetal programming of children’s obesity risk. Psychoneuroendocrinology, 53, 29–39. doi: 10.1016/j.psyneuen.2014.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung-Chan P, Sung YW, Zhao X, & Brownson RC (2013). Family-based models for childhood-obesity intervention: A systematic review of randomized controlled trials. Obesity Reviews, 14(4), 265–278. doi: 10.1111/obr.12000 [DOI] [PubMed] [Google Scholar]
- Thamotharan S, Lange K, Zale EL, Huffhines L, & Fields S (2013). The role of impulsivity in pediatric obesity and weight status: a meta-analytic review. Clinical psychology review, 33(2), 253–262. doi: 10.1016/j.cpr.2012.12.001 [DOI] [PubMed] [Google Scholar]
- Trasande L, & Chatterjee S (2009). Corrigendum: The Impact of Obesity on Health Service Utilization and Costs in Childhood. Obesity, 17(7), 1473–1473. doi: 10.1038/oby.2009.135 [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, & McDowell M (2008). Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise, 40(1), 181–188. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- Weng SF, Redsell SA, Swift JA, Yang M, & Glazebrook CP (2012). Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Archives of disease in childhood, 97(12), 1019–1026. doi: 10.1136/archdischild-2012-302263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock EP, O’Connor EA, Williams SB, Beil TL, & Lutz KW (2010). Effectiveness of weight management interventions in children: A targeted systematic review for the USPSTF. Pediatrics, 125(2), e396–e418. doi: 10.1542/peds.2009-1955 [DOI] [PubMed] [Google Scholar]
- Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, & Davies WH (2007). Controlled study of critical parent and family factors in the obesigenic environment. Obesity, 15(1), 126–126. doi: 10.1038/oby.2007.517 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.