Abstract
Background and Objectives
This study aimed to evaluate if and how remote activity monitoring (RAM) improves caregiver outcomes for family members providing care for persons living with Alzheimer’s disease or a related dementia (ADRD).
Research Design and Methods
We conducted an embedded experimental mixed methods study of 132 persons living with ADRD and their family caregivers (n = 64 randomly assigned to RAM treatment condition). In addition to baseline and 6-month quantitative survey data on context of care, primary objective stressors, resources, self-efficacy/competence, and distress collected from caregivers, 6-month RAM review checklists contained open-ended, qualitative information on perceived acceptability of the technology.
Results
The RAM system did not exert statistically significant effects on caregiving outcomes over a 6-month period. However, qualitative analyses identified several potential moderators of RAM technology effectiveness that were subsequently tested in post-hoc repeated measures analyses of variance. Caregivers who utilized RAM technology and cared for relatives with: (a) less severe cognitive impairment; and (b) difficulty navigating around the home were more likely to indicate statistically significant increases in competence and self-efficacy, respectively.
Discussion and Implications
We found that the early months spent calibrating and modifying RAM are potentially challenging for families, which may prevent this technology from improving caregiving outcomes during initial months of use. Remote activity monitoring may work optimally for caregivers of persons living with ADRD in specific situations (e.g., earlier stages of dementia; wandering risk), which suggests the need for appropriate needs assessments that can better target such innovations.
Keywords: Alzheimer’s disease, Technology, Smart home, Family caregiving, Informal caregiving, Stress, Depression, Randomized controlled trial, Evaluation, Passive monitoring
The aging of the U.S. population and the sheer costs of delivering health care to older persons have led to the development of technological solutions designed to maintain or improve quality of life for older persons (Chipps, Jarvis, & Ramlall, 2017; Czaja, Boot, Charness, Rogers, & Shant 2017; Lindeman & Gladstone, 2018; Schulz et al., 2015). The provision of long-term care, particularly for individuals living with Alzheimer’s disease and related dementias (ADRD), is labor intensive, complex, and largely assumed by families (Gaugler & Kane, 2015; Wolff et al., 2017). It is unclear how technology can either replace or enhance the delivery of family care for persons living with ADRD. Current sociodemographic trends indicate the number of family caregivers available to care for older relatives is expected to decline in the upcoming decades (National Academies of Sciences, Engineering, Medicine, 2016; Redfoot, Feinberg, & Houser, 2013; Stone, 2015). Concurrent with this trend is the ongoing geriatric workforce shortage, which would further exacerbate the “family care gap” (Gaugler & Kane, 2015; Stone, 2015).
A critical scientific as well as policy and practice question, then, is whether the use of technology can sustain and support ADRD family care (Demiris, 2015; Schulz et al., 2015). The current study aims to address this question by evaluating whether and how remote activity monitoring (RAM) technology improves key family caregiver outcomes over a 6-month period.
Background: Efficacy and Effectiveness of Remote Activity Monitoring
Remote activity monitoring (RAM) involves the use of sensors (e.g., motion detectors, or sensors worn on the body) to monitor the movement/activity of a person living with ADRD, generally in the home or in an assisted living facility (Block et al., 2016; Bossen, Kim, Williams, Steinhoff, & Strieker, 2015; D’Onofrio et al., 2017). Monitoring systems issue alerts to professional or family caregivers if adverse events (e.g., falls) or abnormal behaviors/activities (e.g., wandering) occur. Remote activity monitoring technology may also generate reports of activity patterns over time, allowing caregivers to track changes in activity that may indicate a health problem (e.g., using the restroom more frequently).
The information provided by RAM may contribute to more accurate information on daily activities, improved communication, early identification of problems, and facilitation of caregiving (Nauha, Keranen, Kangas, Jamsa, & Reponen, 2016; Nijhof, van Gemert-Pijnen, Woolrych, & Sixsmith, 2013; Wild, Mattek, Austin, & Kaye, 2016; Williams, Arthur, Niedens, Moushey, & Hutfles, 2013). There are several barriers to implementing and utilizing RAM, including cumbersome devices (Matthews et al., 2015), a lack of user-friendly interfaces (Nauha et al., 2016; Preusse, Mitzner, Fausset, & Rogers, 2017), frequent false alarms (Mitchell et al., 2018; Nauha et al., 2016; Nijhof et al., 2013), and unanticipated technological difficulties (Mitchell et al., 2018; Nauha et al., 2016; Williams et al., 2013). Beyond technical problems, the trade-off between privacy and usefulness of monitoring is an important ethical issue (Mitchell et al., 2018; Mulvenna et al., 2017; Wild, Boise, Lundell, & Foucek, 2008; Williams et al., 2013). Nonetheless, many older adults are interested in the potential of monitoring technologies to improve and maintain their health status and independence (Chaudhuri et al., 2017; Preusse et al., 2017; Shreve, Baier, Epstein-Lubow, & Gardner, 2016; Wild et al., 2008).
Though research on the acceptability and utility of RAM has advanced, there are few randomized controlled studies of the effectiveness of RAM for adults living with ADRD or their family caregivers (Gagnon-Roy et al., 2017; Reeder et al., 2013). Available randomized controlled trials feature smaller samples (N ≤ 60), but suggest potentially positive effects of RAM for family caregivers and older adults (Rowe et al., 2009; Torkamani et al., 2014). A recent, larger controlled evaluation implied positive (albeit not statistically significant) trends on RAM users’ health care costs (Finch, Griffin, & Pacala, 2017).
Conceptual Model
To evaluate RAM, the current study relied on The Stress Process Model (SPM). The SPM has been used extensively to study the manifestation of negative outcomes in dementia caregiving (Pearlin, Mullan, Semple, & Skaff, 1990) and is aligned with conceptualizations of intervention effectiveness in the health information technology literature (Jimison et al., 2008). The SPM is based on the mechanism of “proliferation,” where the emotional stress of care provision to a person living with dementia (primary stress) spreads to other life domains that are then posited to negatively influence global caregiving outcomes such as caregiver mental health or the person living with ADRD’s institutionalization. Psychosocial resources or formal service use may help curtail stress proliferation and protect ADRD caregivers from negative outcomes.
The conceptual framework for the current project integrates constructs from the SPM. Context of care variables represent sociodemographic and background characteristics that may influence outcomes for persons living with ADRD or their family caregivers. Similarly, resource variables such as perceptions of socioemotional support are considered as covariates in the current study’s conceptual model that could potentially alleviate negative outcomes. A final domain of covariates includes primary objective stressors, or indices of ADRD severity that may require greater day-to-day care provision on the part of family members. The proposed conceptual model positions RAM technology as a key resource for family caregivers of persons living with ADRD that could improve caregiver self-efficacy and competence (e.g., being able to handle caregiving problems) and reduce caregiver distress (subjective stress and depressive symptoms).
Research Focus
The current study relies on preliminary 6-month outcome data from a parent mixed methods, randomized controlled evaluation of RAM technology for persons living with ADRD at home. The current study tested the following quantitative hypotheses:
1) At the 6-month follow-up, family caregivers randomly assigned to receive RAM technology would experience significant (p < .05) improvements in self-efficacy and sense of competence when managing a relative’s ADRD compared to caregivers not assigned to receive RAM technology.
2) At the 6-month follow-up, families randomly assigned to receive technology compared to those who did not would report significant reductions in caregiver distress (e.g., subjective stress, depressive symptoms).
An additional question was used to guide the analysis of available qualitative data among family caregivers of persons living with ADRD who utilized the RAM technology over a 6-month period:
1) What made a difference in how RAM was received by participants?
If qualitative themes identified specific SPM variables that could potentially moderate the effectiveness of RAM technology on ADRD caregiver outcomes, a series of post-hoc analyses were conducted to further explore the potential mechanisms of benefit (or lack thereof) for RAM technology in ADRD caregiving situations.
Methods
Design
We utilized an embedded experimental mixed methods design (i.e., collection and analysis of qualitative data within a traditional randomized controlled trial) to examine the preliminary effectiveness of RAM for family caregivers of persons living with ADRD ([QUAN+qual]→QUAN) (Creswell & Plano-Clark, 2010; p. 90). Efficacy (“performance of an intervention under ideal conditions”) and effectiveness (“an intervention’s importance in real-world conditions”) exist on a continuum, and thus it is unlikely that any given intervention is solely an efficacy or effectiveness trial (Singal, Higgins, & Waljee, 2014, p. 1). Although we employ a randomized controlled design, the use of RAM in the everyday homes of persons living with ADRD and their family caregivers and the relatively inclusive sampling plan places the current study closer to effectiveness than efficacy trial. As we are presenting preliminary outcome data from a larger parent trial of RAM that follows persons living with ADRD and their caregivers for up to 18 months, we thus consider this study a “preliminary effectiveness” evaluation.
Remote Activity Monitoring System
The RAM system features motion sensors that are placed throughout the home in order to monitor daily activity. The sensors operate jointly and exchange information on movement. Data collected by the sensors are analyzed using algorithms developed by the RAM provider. Once a baseline activity pattern is established, significant and persistent deviations are communicated to family caregivers, alerting them to abnormal activity patterns that may indicate a possible health condition of the care recipient.
Users can specify conditions that trigger alerts based on unexpected or potentially dangerous activity. For example, sensors can identify if the care recipient is leaving the home at unexpected times or is staying in the bathroom too long. Alerts can be customized to match the expected schedules of each care recipient as well. Caregivers can be alerted by phone or e-mail, and users can create a list of family, friends, and others to contact in the event that the primary caregiver cannot be reached. Care recipients are also given an emergency call pendant that can be worn around the neck. An online dashboard that stores and displays the data collected by RAM is available to caregivers and can be shared with health service providers. The Supplementary Material includes images of the sensors as well as data displays from the online dashboard.
Sample
Inclusion criteria for persons living with ADRD were: (a) English speaking; (b) physician diagnosis of ADRD; (c) not currently receiving RAM or similar services; and (d) ≥ 55 years of age. Caregivers of persons living with ADRD had to: (a) speak English; (b) be ≥ 21 years of age; (c) self-identify as the person most responsible for providing hands-on care to the person living with ADRD; and (d) plan to remain in the area for at least 18 months. Informed consent was obtained from the caregiver (and legally authorized representative). The person living with ADRD provided assent to participate. As of November 30, 2017, 132 ADRD caregivers were scheduled to complete 6 months of follow-up and served as the sample for the current analysis (n = 64 randomized to RAM treatment group; n = 68 to usual care control). The parent mixed methods evaluation of RAM is continuing to enroll new participants until June 2018 to follow for up to 18 months.
Procedure
Research coordinators initiated e-mail, telephone, or mail contact with ADRD caregivers on the University of Minnesota Caregiver Registry or via various newspaper advertisements, community presentations, and similar efforts. If caregivers expressed interest in participating, the research coordinators described the RAM system and explained study procedures. If caregivers agreed to participate, the research coordinators initiated a brief screening procedure. For eligible participants, signed consent and verbal assent of family caregivers and persons living with ADRD were scheduled and obtained, and a baseline survey was administered either online or via traditional mail. Following the completion of baseline surveys, ADRD caregivers were randomly assigned to the RAM treatment condition that received the multisensor RAM system or a usual care control group. Randomization was completed via a list generated from http://randomizer.org; allocation was based on an a priori randomization assignment number. A follow-up survey was then administered to all participating caregivers at 6 months.
Two weeks after randomization to the RAM treatment condition, the Director of Health and Technology Services (HTS) scheduled a visit or telephone conference at the home of the person with ADRD and the enrolled family caregiver. During this initial contact, the HTS conducted a needs assessment to determine the best use and deployment of the RAM system in the person living with ADRD’s home. The HTS assessed the home environment (e.g., square footage, number of bathrooms and bedrooms) and asked questions regarding health conditions and other risk factors such as concerns with eating or weight, hospitalizations, use of assistive devices, and history of falls. Following the needs assessment, the HTS discussed the results with the ADRD caregiver and reviewed how the RAM system operates as well as how to utilize the system. This included a review of the online dashboard. The RAM system was then installed in the person living with ADRD’s home and the HTS programmed the expected performance thresholds and daily routines. The HTS supervised all system maintenance (battery changes, troubleshooting in instances when there was a loss of system contact) and ensured the system operated properly for ADRD caregivers. Caregivers were also free to contact the HTS at any time if an issue arose that required immediate attention (e.g., damaged or inoperable sensor).
Measures
Context of Care
Context of care variables included time since diagnosis, living arrangement of the care recipient, caregiver and care recipient demographics, and similar indicators (see Table 1).
Table 1.
Baseline Demographics of Caregivers and Care Recipients
| Caregiver characteristics | Total (N = 132) | Treatment (n = 64) | Control (n = 68) | p-value | |||
|---|---|---|---|---|---|---|---|
| Age, mean (SD), years | 61.71 | (12.09) | 61.32 | (11.36) | 62.07 | (12.80) | .580 |
| Female, n (%) | 103 | (78.0) | 50 | (79.4) | 53 | (77.9) | .843 |
| Hispanic, n (%) | 2 | (1.5) | 0 | (0.0) | 2 | (3.0) | .226 |
| White, n (%) | 128 | (97.0) | 62 | (96.9) | 66 | (97.1) | .951 |
| Married, n (%) | 109 | (82.6) | 50 | (78.1) | 59 | (86.8) | .191 |
| Living children, mean (SD) | 2.06 | (1.71) | 1.86 | (1.46) | 2.25 | (1.91) | .079 |
| Bachelor’s Degree or higher, n (%) | 88 | (66.7) | 43 | (67.2) | 45 | (66.2) | .902 |
| Above median income, n (%)* | 56 | (42.4) | 23 | (35.9) | 33 | (48.5) | .143 |
| Employed, n (%) | 54 | (40.9) | 26 | (40.6) | 28 | (41.2) | .949 |
| Socioemotional support, mean (SD) | 31.95 | (4.64) | 32.43 | (5.18) | 31.50 | (4.06) | .786 |
| Care recipient characteristics | p-value | ||||||
| Age, mean years (SD) | 77.88 | (9.23) | 78.05 | (9.24) | 77.72 | (9.28) | .993 |
| Female, n (%) | 69 | (52.7) | 34 | (54.0) | 35 | (51.5) | .775 |
| Hispanic, n (%) | 2 | (1.6) | 1 | (1.6) | 1 | (1.5) | .618 |
| White, n (%) | 123 | (93.2) | 59 | (92.2) | 64 | (94.1) | .660 |
| Married, n (%) | 80 | (60.6) | 38 | (59.4) | 42 | (61.8) | .779 |
| Living children, mean (SD) | 2.91 | (2.17) | 2.80 | (2.28) | 3.01 | (2.08) | .933 |
| Bachelor’s Degree or higher, n (%) | 62 | (47.0) | 28 | (43.8) | 34 | (50.0) | .472 |
| Above median income, n (%)* | 78 | (59.1) | 36 | (56.3) | 42 | (61.8) | .520 |
| ADLs, mean (SD) | 2.41 | (2.70) | 2.32 | (2.40) | 2.50 | (2.96) | .202 |
| IADLs, mean (SD) | 7.56 | (3.63) | 7.36 | (3.61) | 7.74 | (3.67) | .894 |
| RMBPC frequency, mean (SD) | 1.47 | (0.57) | 1.56 | (0.57) | 1.40 | (0.56) | .906 |
| Cognitive impairment, mean (SD) | 2.55 | (0.82) | 2.61 | (0.76) | 2.50 | (0.88) | .157 |
| Medicaid, n (%) | 26 | (19.8) | 13 | (20.6) | 13 | (19.1) | .828 |
| Common characteristics | p-value | ||||||
| CG is spouse of care recipient, n (%) | 65 | (49.2) | 29 | (45.3) | 36 | (52.9) | .381 |
| Live together, n (%) | 74 | (56.1) | 36 | (56.3) | 38 | (55.9) | .966 |
| First noticed memory problem in CR, mean (SD), months | 48.82 | (27.59) | 48.47 | (26.56) | 49.15 | (28.70) | .588 |
| First helped CR, mean (SD), months | 34.19 | (23.99) | 35.34 | (23.93) | 33.05 | (24.20) | .874 |
| Time since CR saw doctor for memory problem, mean (SD), months | 41.92 | (27.20) | 43.20 | (27.40) | 40.66 | (27.16) | .531 |
Note: n represents caregiver-care recipient dyad; p-values test if characteristic differs by treatment assignment, chi-square or T-test as appropriate. ADLs = Activities of daily living; CG = Caregiver; CR = Care recipient; IADLs = Instrumental activities of daily living; RMBPC = Revised Memory and Behavior Problem Checklist; SD = Standard deviation.
*≥80k for CG, ≥30k for CR.
Primary Objective Stressors
Primary objective stressors included the person living with ADRD’s dependence on assistance with six activity of daily living (ADL) tasks and six out of eight instrumental activity of daily living (IADL) tasks (α = .89, Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963; α = .96, Lawton & Brody, 1969). The six IADL items utilized were taking medication, cooking/preparing food, housekeeping/cleaning, doing laundry, transportation, and managing finances. An 8-item scale measured the intensity of relatives’ memory losses, communication deficits, and recognition failures at each time point (cognitive impairment; α = .86) (Pearlin et al., 1990). The frequency of behavior problems in the person living with ADRD was measured with the Revised Memory and Behavior Problems Checklist (R-MBPC; α = .89), which consists of a list of 30 common behavior problems in ADRD (Teri et al., 1992).
Resources
Socioemotional support was measured on a 5-item scale to assess the affective assistance provided to the caregiver by relatives or friends at each time point (α = .68; Pearlin et al., 1990).
Caregiver Self-efficacy and Sense of Competence
An 8-item measure of caregiver self-efficacy was utilized (α = .86; Fortinsky, Kercher, & Burant, 2002). Caregivers’ sense of competence was measured with the 7-item Short Sense of Competence Questionnaire (SSCQ), which assesses individuals’ sense of capability in providing assistance to a relative with ADRD (α = .74; Vernooij-Dassen et al., 1999).
Caregiver Distress
It was measured using the 22-item Zarit Burden Interview (α = .93; Hébert, Bravo, & Préville, 2000; Zarit, Reever, & Bach-Peterson, 1980). Two indices of subjective stress were also utilized: a 4-item scale assessing the involuntary aspects of the caregiving role (α = .80; role captivity) and a 3-item scale measuring caregivers’ feelings of emotional and physical fatigue (α = .81; role overload) (Pearlin et al., 1990). The 20-item Center for Epidemiological Studies-Depression (CES-D) scale was used to measure caregiver depressive symptoms (α = .94; Radloff, 1977).
RAM System Review Checklist
The RAM Review Checklist was administered to ADRD caregivers in the treatment condition at the 6-month follow-up survey interval. The checklist consists of 22 Likert scale items and 8 open-ended questions that measure/explore acceptability, feasibility, and perceived utility of RAM (for details, see Mitchell et al., 2018). Only the open-ended questions were analyzed for themes. Example questions include “How easy was RAM to use?” and “Do you feel the alerts generated by RAM worked well? Why or why not?” Themes were mapped onto quantitative baseline variables and included in the post-hoc analyses (see below).
Analysis
Descriptive statistics were calculated for measures of context of care, primary objective stressors, and resources. Chi-square and t tests were used to compare participants in the treatment and usual care control groups. If baseline differences were identified, they were incorporated as covariates in subsequent quantitative analyses. Multivariate repeated measures of analyses of variance (ANOVAs)/covariance were conducted to test study hypotheses. The independent variable in each of these models was treatment assignment (RAM technology or usual care without RAM). Statistical significance was assessed using two-tailed tests with a significance level of 0.05. The sample size of 132 was sufficient to detect between a medium to small effect size using this analytic approach (F = 0.25 to F = 0.10; IntellectusStatistics, 2018).
The qualitative data (N = 49) were coded using Braun and Clarke’s (2006) six steps of thematic analysis. The authors were guided by the research question: “What made a difference in how RAM was received by participants?” The first step was for the coding team to familiarize themselves with the data. To do so, five authors (L. L. Mitchell, C. M. Peterson, J. M. Finlay, R. Zmora, and H. McCarron) individually read all open-ended responses from the 6-month RAM Review Checklist. The second step was to generate initial themes that captured patterned responses relevant to the research question. The authors each took note of potential themes, writing down a tentative name and description for each theme. The authors then discussed and compiled the codes into an initial framework of main overarching themes and subthemes (thus carrying out Braun and Clarke’s third step, searching for themes). The subthemes provided a useful scaffold for the broad overarching themes and delineated a hierarchy of meaning within the data. Steps four and five involved reviewing the thematic framework and defining and naming themes and subthemes, which are part of the ongoing, iterative process of testing and refining the coding system. To accomplish these steps, the five authors each independently coded a subset of approximately 10 responses and then met to discuss discrepancies and make appropriate changes to the thematic framework. These steps were repeated three times until no further changes to the thematic framework were needed. Three authors (L. L. Mitchell, J. M. Finlay, and H. McCarron) then coded all available data applying the finalized thematic framework. Reliability was calculated using NVivo software (Version 11; QSR International, 2015) (average kappa = 0.80, average percent agreement = 94%). To ensure agreement, four authors (L. L. Mitchell, C. M. Peterson, R. Zmora, and H. McCarron) reviewed coding results and resolved all coding discrepancies through discussion. This manuscript represents the sixth step: the write-up of our final thematic analysis.
As part of the embedded experimental mixed methods analysis, we utilized the themes identified from the qualitative analysis to inform subsequent, post-hoc quantitative analyses. Specifically, if the thematic analysis suggested potential variables that could moderate the effectiveness of RAM and were measured in the baseline surveys, they were included as interaction terms (i.e., moderator × treatment × time) in a series of post-hoc, repeated measure ANOVAs to further examine the mechanisms of benefit (or lack thereof). These variables were selected by five of the authors (L. L. Mitchell, J. M. Finlay, H. McCarron, R. Zmora, and C. M. Peterson), who reviewed the list of quantitative measures and came to consensus on which measures or items (if any) best reflected each qualitative theme. All quantitative and mixed methods analyses were conducted with SPSS (Version 24.0; IBM Corporation, 2015).
Results
Sample Characteristics
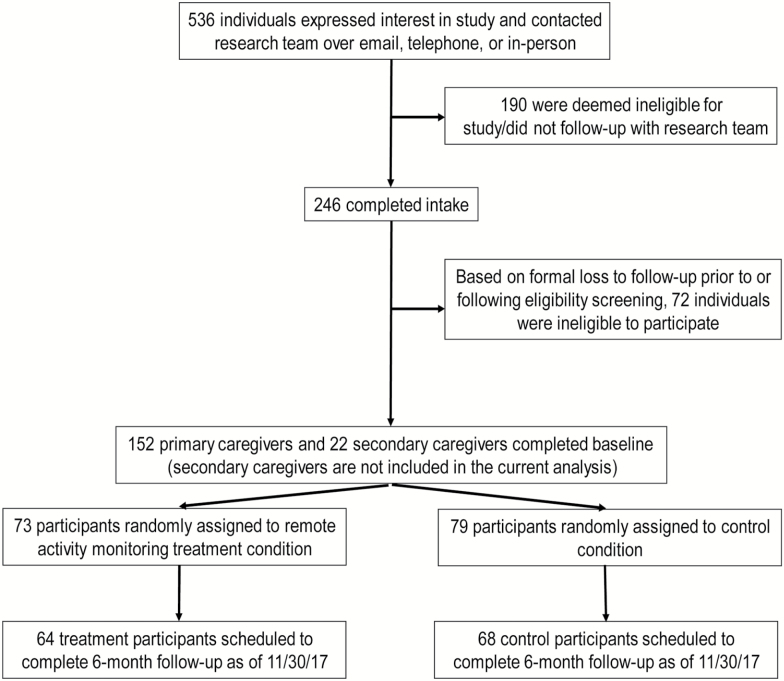
The enrollment process for the current project is shown in Figure 1. Compared to participants who were not lost to follow up, caregivers who were lost to follow up (n = 5) reported higher care recipient ADLs (M = 1.8, SD = 4.0 vs M = 0.7, SD = 1.7, respectively; p < .01) and indicated a longer time interval since their care recipient saw a doctor for memory problems (M = 54.4 months, SD = 46.0 vs M = 41.4 months, SD = 26.3; p < .05). Among those with complete data at follow-up, there were no statistically significant differences between the treatment and control groups on baseline covariates (Table 1).
Figure 1.
Participant enrollment flow. Note: One participant requested that remote activity monitoring (RAM) technology be removed from their home because the care recipient felt the technology was invasive of his privacy. Furthermore, two participants randomized to the treatment group and who received RAM technology were not included as anticipated in the randomization log; sensitivity analyses conducted without these participants did not result in meaningful differences in any of the findings.
Effects of RAM on 6-Month Caregiver Outcomes: Tests of Hypotheses 1 and 2
Baseline and 6-month means of caregiver self-efficacy, sense of competence, and distress are included in Table 2. The use of RAM technology was not significantly associated with changes in the outcomes over the 6-month follow-up (Table 3).
Table 2.
Primary Quantitative Outcomes at Baseline and 6 Months
| Outcomes | Baseline | Six months | ||||||
|---|---|---|---|---|---|---|---|---|
| Treatment | Control | Treatment | Control | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| SSCQ | 24.17 | 5.18 | 24.26 | 5.46 | 23.33 | 5.58 | 23.73 | 5.85 |
| Self-Efficacy | 27.94 | 6.00 | 27.62 | 6.01 | 28.39 | 7.38 | 27.59 | 7.06 |
| Burden | 37.59 | 13.26 | 37.01 | 15.24 | 40.40 | 16.15 | 40.93 | 18.54 |
| Role Captivity | 6.13 | 2.30 | 6.35 | 2.51 | 6.74 | 2.65 | 6.56 | 2.69 |
| Role Overload | 7.95 | 2.66 | 7.41 | 2.67 | 7.51 | 2.80 | 7.42 | 2.74 |
| CES-D | 33.01 | 12.74 | 32.51 | 11.21 | 38.90 | 16.92 | 35.95 | 13.46 |
Note: CES-D = Center for Epidemiological Studies – Depression; SD = Standard deviation; SSCQ = Short Sense of Competence Questionnaire.
Table 3.
Repeated Measures Analysis of Variance
| Effect | MS | df | F | p |
|---|---|---|---|---|
| Self-Efficacy | ||||
| Time | 1.41 | 1 | 0.06 | .801 |
| Time × tx | 0.08 | 1 | 0.00 | .954 |
| Error | 22.10 | 113 | ||
| SSCQ | ||||
| Time | 16.59 | 1 | 1.02 | .315 |
| Time × tx | 5.70 | 1 | 0.35 | .556 |
| Error | 16.32 | 115 | ||
| Burden | ||||
| Time | 724.58 | 1 | 9.52 | .003 |
| Time × tx | 30.14 | 1 | 0.40 | .530 |
| Error | 76.09 | 115 | ||
| Role Captivity | ||||
| Time | 10.74 | 1 | 3.34 | .070 |
| Time × tx | 2.56 | 1 | 0.80 | .374 |
| Error | 3.22 | 114 | ||
| Role Overload | ||||
| Time | 3.51 | 1 | 1.00 | .318 |
| Time × tx | 2.27 | 1 | 0.65 | .422 |
| Error | 3.50 | 124 | ||
| CES-D | ||||
| Time | 1335.42 | 1 | 15.03 | 0 |
| Time × tx | 145.20 | 1 | 1.63 | .204 |
| Error | 88.86 | 122 | ||
Note: Tx = Treatment/Remote activity monitoring; CES-D = Center for Epidemiological Studies – Depression; SSCQ = Short Sense of Competence Questionnaire.
Qualitative Analysis: Factors Related to Acceptability and Utility of RAM
The qualitative analysis identified three major overarching themes that determined how caregivers perceived RAM: (a) characteristics of the caregiver; (b) characteristics of the care recipient; and (c) living arrangement. Here, we discuss the subthemes within each of these three overarching themes and map them onto relevant quantitative/SPM measures available in the surveys (see Table 4 for this information and expanded quotes as well).
Table 4.
Mapping Qualitative Themes onto Quantitative Moderators
| Analogous quantitative variable/moderator | Qualitative subthemes | SPM component | Representative quotes (see text also) |
|---|---|---|---|
| Overarching Theme: Caregiver Characteristics | |||
| Work status | Time constraints and stress level | Context of care | I have not received [RAM] alerts and have not been able to go into the data. In all honesty I have been consumed with some significant health issues with my mother over the past 6 months along with making sure [care recipient’s] needs are met. (wife, age not disclosed) |
| Not available | Comfort with technology | Resource | …impossible to use for those who are not computer savvy (husband, age 88) It’s easy to use (if you have some familiarity with technology)...I like that I can check the system on any internet connected device. (daughter, age 61) |
| Overarching Theme: Care Recipient Characteristics | |||
| ADL/IADLs Memory & behavior problems Wandering |
Care recipient behavior | Primary objective stressor | When I see that she is opening and closing her refrigerator more often in the system, I’ve learned it’s probably time to go grocery shopping with her again” (daughter, age 61). |
| Cognitive impairment ADLs, IADLs Memory & behavior problems |
Dementia status | Primary objective stressor | [Care recipient] has not progressed in the disease to require the monitoring. (wife, age 81) Emergency alerts are tricky with a person as far into dementia as my mother was & we never found a use for them. (daughter, age 54) |
| Overarching Theme: Caregiver and Care Recipient Living Arrangements | |||
| Whether the caregiver lives with the care recipient | Living arrangement | Context of care | I didn’t use it, simply because it was time consuming to handle what I was up to, and since I lived with Mother, I felt like I know what I needed to know about her movements. (daughter, age 54) |
Note: ADLs = Activities of daily living; IADLs = Instrumental activities of daily living; SPM = Stress Process Model.
Caregiver Characteristics
Participants noted characteristics pertaining to themselves that affected level of personal fit with RAM, including their time constraints and stress level and comfort with technology. Six of the 49 participants who provided qualitative data indicated that time constraints interfered with their ability to make use of RAM: “[I] don’t have time to look at what he did all day...may work great for some people just not us” (wife, age 58). In these cases, the use of RAM technology was often seen as an additional task on top of the already difficult burden of caregiving or other life responsibilities. These participants indicated that it did not seem worth their time to learn the system, or that it was simply not feasible for them to use RAM. For these reasons, we identified work status as a potential context of care indicator to consider in subsequent post-hoc quantitative analyses (see Table 4 and below).
Participants’ degree of comfort with technology also appeared as an important factor in determining the usefulness of RAM. Seventeen caregivers reported a lack of comfort with technology as a barrier to their use of the system. On the other hand, eight participants commented that they were relatively comfortable using technology, and this facilitated their use of RAM. However, since no measure of comfort with technology was included in the administered surveys, we were not able to analyze this potential variable further in post-hoc analyses.
Care Recipient Characteristics
Characteristics of the care recipient also influenced caregivers’ perceptions of RAM utility. Specifically, care recipient behaviors and dementia status were mentioned by participants as factors that made RAM more or less helpful in their particular circumstances. Twelve participants discussed specific care recipient behaviors, including sleep patterns and nighttime activity, over- or under-use of household appliances (e.g., phone, refrigerator), and wandering, which were conducive to monitoring and intervention through RAM. For example: “When I see that she is opening and closing her refrigerator more often in the system, I’ve learned it’s probably time to go grocery shopping with her again” (daughter, age 61). Four participants also mentioned aspects of the care recipient’s behavior that made RAM less useful to them. In particular, caregivers whose care recipients did not wander or who had trouble using the pendant were less likely to find the RAM system useful. To capture care recipient behaviors, an item reflecting wandering were included in the post-hoc quantitative analyses.
Eight participants also discussed their care recipient’s dementia status as a factor affecting the utility of RAM. Caregivers identified that the additional supervision provided by RAM was not necessary in early stages of dementia. For caregivers of recipients in later stages of the disease, the care recipient required near-constant in-person supervision, thus obviating the need for RAM. We thus included measures of dementia severity along with ADLs and IADLs and frequency of memory and behavior problems in post-hoc quantitative analyses.
Living Arrangement
Caregivers’ open-ended responses often indicated that their living situations made a difference in their perceptions of RAM utility. Twenty participants referred to the implications of their living arrangements. For example, RAM was less useful for participants who lived with their care recipient and were constantly available to monitor and care for them personally. These participants felt that they had enough information about the care recipient’s activity patterns and needs as a function of living with them, and so the data provided by RAM was superfluous. In contrast, participants who did not live in the same residence as their care recipients tended to report finding RAM more valuable: “Knowing my mom was safely moving around her apartment was a huge help since I do not live in the same town” (daughter, age 55). We included whether the caregiver lived with the care recipient as a moderator in post-hoc quantitative analyses.
Mixed Methods Analysis
The variables identified in the qualitative analysis were included as potential moderators of RAM efficacy on changes in caregiver outcomes over a 6-month period. Specifically, measures of ADL, IADL, R-MBPC, and cognitive impairment scores were dichotomized which corresponded to their highest quartile scores. As wandering was also indicated as a key concern related to RAM utility, a single item from the cognitive impairment scale (“How difficult is it for the person with memory loss to find his/her way around the house?”) was extracted and utilized as a moderator. This variable was dichotomized to compare care recipients who had no or just a little difficulty finding their way around the house to care recipients who found this more difficult. Whether the caregiver lived with the care recipient was also included.
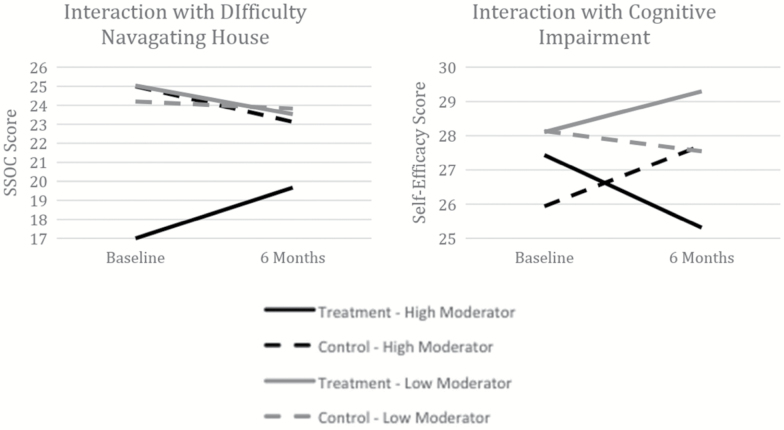
The full results of the post-hoc repeated measures ANOVAs are reported in the Supplementary Material; Figure 2 displays the plotted means of the statistically significant three-way interactions (i.e., treatment × time × moderator). Severity of cognitive impairment was found to moderate the effects of RAM technology on caregivers’ self-efficacy (F = 5.61; p < .05). RAM-using caregivers of relatives experiencing less cognitive impairment reported increased self-efficacy over a 6-month period, whereas RAM-using caregivers of relatives with more severe cognitive impairment indicated decreases in self-efficacy; these longitudinal trends occurred in opposite fashion for controls. Caregivers who utilized RAM technology and provided help to a care recipient with difficulty navigating the home indicated greater increases in sense of competence, indicated by higher mean SSCQ scores, whereas those in the control group and technology users who assisted relatives with fewer problems navigating the home indicated no/slight declines in competence over a 6-month interval (F = 4.42; p < .05).
Figure 2.
Statistically significant three-way interaction results. Note: Treatment in solid line, control in dashed line; high moderator (severe cognitive impairment, difficulty navigating house) in black, low moderator (less severe cognitive impairment, little difficulty navigating house) in gray. CG = caregiver; SSCQ = Short Sense of Competence Questionnaire.
Discussion
We acknowledge that it is not ideal to conduct preliminary outcome analyses in a randomized controlled trial (RCT), particularly if they were not planned a priori (see Counsell, Biri, Fraczek, & Hackshaw, 2017). Although the dependent variables selected in the present study do not represent all of the main outcomes we aim to analyze in the parent 18-month evaluation of RAM (e.g., person with ADRD health service utilization), we will incorporate statistical adjustment of p values in any subsequent evaluation of RAM effectiveness for caregiving outcomes to avoid the potential of inappropriate statistical inference. This will inhibit our ability to detect a statistically significant effect at 18 months for key caregiving outcomes, but will also avoid the risk of “fishing” for findings (i.e., p hacking).
Why proceed with disseminating these preliminary results? As noted by Schulz et al. (2015) and others (e.g., Lindeman & Gladstone, 2018), the classic time frame often required to complete a RCT of sufficient follow-up may not keep pace with the rapid evolution of smart home technologies such as RAM. From a societal perspective, it is critical to share findings of effectiveness to inform families, older consumers, providers, and policymakers to offer important insights as to the limits of RAM in home-based dementia care contexts, as well as under what circumstances such technologies are potentially successful (Gitlin & Maslow, 2017). As Berridge (2018) notes in a recent policy analysis of Medicaid (which has recently emerged as the largest third-party payer of RAM technologies): “Decisions about Medicaid reimbursement of technologies that have the potential to dramatically alter the way older adults receive supportive services are being made without research on their use, social and ethical implications, or outcomes” (p. 1).
To this end, these preliminary findings have ramifications for research, policy and practice. The lack of direct effects may reflect how the RAM technology in this study was deployed. Alerts and activity pattern data were directed to family caregivers rather than a care professional. In some ways this reflects how families would likely use RAM in “real-world” situations, particularly as RAM technologies that are simple to install and operate become more widely available in retail stores (Moylan, 2017). As both the quantitative and qualitative findings of this study imply, the initial months spent calibrating and modifying the system to meet the particular needs of persons living with ADRD and their family caregivers are potentially challenging if families are solely responsible for responding to alerts and activity pattern data (see also Mitchell et al., 2018). The mixed methods findings also imply that RAM technologies may be best suited for persons living with ADRD in the less severe stages of the disease. In particular, this technology may be most useful when an individual is recently diagnosed with ADRD. The access to information on daily activities and early identification of problems may help caregivers feel more confident and competent when using RAM technology. For specific symptoms, such as difficulty navigating the home or wandering, RAM technology use could help to buttress the dementia caregiving situation and help enhance caregivers’ sense that dementia care receipt and delivery occurs more effectively.
From a scientific standpoint, the current paper serves as an important “lesson learned” for other researchers who intend to evaluate RAM or other technologies in the context of ADRD care. Our decision to disseminate preliminary effectiveness of RAM for caregiving outcomes illustrates the need to adequately power for such analyses at the outset; this allows for the required statistical flexibility to respond to the rapid development and evolution of smart home technologies often marketed to families. In addition, the need to optimize the fit between the individual living with ADRD and a smart home technology such as RAM may require broader conceptual/theoretical frameworks. For example, Person-Environment Fit Theory describes the interaction between the competence of an individual with ADRD (which may be characterized by dementia or functional severity) and the environment such as the home (Iwarsson, 2004; Lawton & Nahemow, 1973). In this model, the use of RAM technology to bridge gaps between these two domains may reduce environmental press and promote adaptive behavior and well-being in the person living with ADRD (and their family caregivers, as well).
There are several important limitations to note in addition to those reported earlier. This is a preliminary study of effectiveness; the parent mixed methods, randomized controlled evaluation of RAM technology is currently enrolling participants with the goal of including approximately 200 persons living with ADRD and their caregivers. The study will follow these participants over 18 months and will include a wider array of outcomes (e.g., care recipient service utilization; cost analyses). For these reasons, additional findings related to caregiver outcomes are possible in subsequent analyses. Blinding did not occur in this study, which may influence risk of bias. Due to budget limitations, the purchase of RAM systems in the initial 2 years of the project precluded the hiring of study personnel to perform blinded ratings. The use of online and mail surveys to conduct data collection was implemented to mitigate these concerns. Among those caregivers and persons living with ADRD who did not provide 6-month follow-up data, there were significant differences on two covariates. Not all caregivers in the treatment condition provided 6-month open-ended responses on the RAM Review Checklist. Open-ended responses were generally brief and imprecise, thus limiting the depth and richness of available qualitative data. Comfort with technology, which was identified as an important caregiver characteristic in qualitative analysis, was not assessed quantitatively and could not be examined in the post-hoc analyses. For additional limitations, see Mitchell et al., (2018).
A key policy goal of community-based ADRD care is to assist individuals in remaining in the community with high quality of life. This objective is often accomplished through the delivery of services and supports to family caregivers. One of the particularly exciting aspects of technology is its potential to not only support/supplement existing ADRD family caregiving efforts, but to also substitute for or even prevent the need for such care through proactive monitoring. We found that the RAM system did not improve caregiver outcomes. However, this technology may work for family caregivers of persons living with ADRD in specific situations (e.g., earlier stages of dementia; wandering risk), suggesting the imperative of appropriate needs assessment that can better target/tailor such interventions. The evolution of technology is such that it is no longer a matter of “if” RAM or similar smart-home innovations will be made available for ADRD family caregivers to purchase and use. Instead, ongoing (and more rapid) scientific evaluations of these approaches are required to guide providers, payers and families themselves to optimize decisions related to initial and long-term utilization.
Funding
This work was supported by the Agencies for Healthcare Research & Quality (R18 HS022836 to J. E. Gaugler) and the National Institutes of Health/National Institute on Aging (K02 AG029480 to J. E. Gaugler).
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
The authors would like to thank Ann Emery, Sierra Trost, and Amanda Weinstein for their data collection, management, and coordination expertise. The authors also acknowledge the Director of Health Technology and Services, Sharon Blume of the Lutheran Home Association, as well as GreatCall for their ongoing support of this project. The authors thank the scientific consultants and collaborators on this study as well (Kathleen Buckwalter; George Demiris; Jennifer Kinney; John Nyman; Carolyn Porta; and Bonnie Westra). Most importantly, the authors are grateful for the time and willingness of the family members and persons living with Alzheimer’s disease or related dementias who have and are continuing to participate in this project.
References
- Berridge C. (2018). Medicaid becomes the first third-party payer to cover passive remote monitoring for home care: Policy analysis. Journal of Medical Internet Research, 20, e66. doi: 10.2196/jmir.9650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block V. A. Pitsch E. Tahir P. Cree B. A. Allen D. D. & Gelfand J. M (2016). Remote physical activity monitoring in neurological disease: A systematic review. PloS One, 11, e0154335. doi: 10.1371/journal.pone.0154335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bossen A. L. Kim H. Williams K. N. Steinhoff A. E. & Strieker M (2015). Emerging roles for telemedicine and smart technologies in dementia care. Smart Homecare Technology and Telehealth, 3, 49–57. doi: 10.2147/SHTT.S59500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., & Clarke V (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. doi: 10.1191/1478088706qp063oa [Google Scholar]
- Chaudhuri S. Kneale L. Le T. Phelan E. Rosenberg D. Thompson H. & Demiris G (2017). Older adults’ perceptions of fall detection devices. Journal of Applied Gerontology, 36, 915–930. doi: 10.1177/0733464815591211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chipps J. Jarvis M. A. & Ramlall S (2017). The effectiveness of e-Interventions on reducing social isolation in older persons: A systematic review of systematic reviews. Journal of Telemedicine and Telecare, 23, 817–827. doi: 10.1177/1357633X17733773 [DOI] [PubMed] [Google Scholar]
- Counsell N. Biri D. Fraczek J. & Hackshaw A (2017). Publishing interim results of randomised clinical trials in peer-reviewed journals. Clinical trials (London, England), 14, 67–77. doi: 10.1177/1740774516664689 [DOI] [PubMed] [Google Scholar]
- Creswell J. W., & Plano Clark V. L (2010). Designing and conducting mixed methods research (Vol. 2nd). Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- Czaja S. J., Boot W. R., Charness N., Rogers W. A., & Shant J (2018). Improving social support for older adults through technology: Findings from the PRISM randomized controlled trial. The Gerontologist, 58, 467–477. doi: 10.1093/geront/gnw249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G., Sancarlo D., Ricciardi F., Panza F., Seripa D., Cavallo F.,…, Greco A. (2017). Information and communication technologies for the activities of daily living in older patients with dementia: A systematic review. Journal of Alzheimer’s Disease, 57, 927–935. doi: 10.3233/JAD-161145 [DOI] [PubMed] [Google Scholar]
- Demiris G. (2015). Information technology to support aging: Implications for caregiving. In J. E. Gaugler & R. L. Kane (Eds.), Family caregiving in the new normal. (pp. 211–223). San Diego, CA: Academic Press. [Google Scholar]
- Finch M. Griffin K. & Pacala J. T (2017). Reduced healthcare use and apparent savings with passive home monitoring technology: A pilot study. Journal of the American Geriatrics Society, 65, 1301–1305. doi: 10.1111/jgs.14892 [DOI] [PubMed] [Google Scholar]
- Fortinsky R. H. Kercher K. & Burant C. J (2002). Measurement and correlates of family caregiver self-efficacy for managing dementia. Aging & Mental Health, 6, 153–160. doi: 10.1080/13607860220126763 [DOI] [PubMed] [Google Scholar]
- Gagnon-Roy M. Bourget A. Stocco S. Courchesne A. L. Kuhne N. & Provencher V (2017). Assistive technology addressing safety issues in dementia: A scoping review. The American Journal of Occupational Therapy, 71, 7105190020p1–7105190020p10. doi: 10.5014/ajot.2017.025817 [DOI] [PubMed] [Google Scholar]
- Gaugler J. E., & Kane R. L (2015). Family caregiving in the new normal (Vol. 1st). San Diego, CA: Academic Press. [Google Scholar]
- Gitlin L. N., & Maslow K (2017). Research Summit on Dementia Care: Overview and recommendations Retrieved January 12, 2018, from https://aspe.hhs.gov/advisory-council-october-2017-meeting-presentation-care-summit-overview-and-recommendations.
- Hébert R., Bravo G., & Préville M (2000). Reliability, validity and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Canadian Journal on Aging, 19, 494–507. [Google Scholar]
- IBM Corporation (2015). IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. [Google Scholar]
- IntellectusStatistics (2018). Sample Size: Repeated Measures ANOVA Retrieved from https://www.intellectusstatistics.com/sample-size-write-up/sample-size-repeated-measures-anova/.
- Iwarsson S. (2004). Assessing the fit between older people and their home environments—An occupational therapy research perspective. In H.-W. Wahl R. Scheidt, & P. Windley (Eds.), Focus on aging in context: Socio-physical environments. Annual review of the Gerontological Society of America 2003 (pp. 85–109). New York: Springer. [Google Scholar]
- Jimison H., Gorman P., Woods S., Nygren P., Walker M., Norris S., & Hersh W (2008). Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved. Rockville, MD: Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK38653/. [PMC free article] [PubMed] [Google Scholar]
- Katz S. Ford A. B. Moskowitz R. W. Jackson B. A. & Jaffe M. W (1963). Studies of illness in the aged. The index of adl: A standardized measure of biological and psychosocial function. JAMA, 185, 914–919. [DOI] [PubMed] [Google Scholar]
- Lawton M. P., & Brody E. M. (1969). Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist, 9, 179–186. [PubMed] [Google Scholar]
- Lawton M. P., & Nahemow L (1973). Ecology and the aging process. In C. Eisdorfer & M. P. Lawton (Eds.), Psychology of adult development and aging (pp. 619–674). Washington, DC: American Psychological Association. [Google Scholar]
- Lindeman D., & Gladstone C (2018). Technology and caregiving: Emerging interactions and directions for research. Paper presented at the Research Priorities in Caregiving Summit, University of California-Davis. [Google Scholar]
- Matthews J. T., Lingler J. H., Campbell G. B., Hunsaker A. E., Hu L., Pires B. R.,…, Schulz R. (2015). Usability of a Wearable Camera System for Dementia Family Caregivers. Journal of Healthcare Engineering, 6, 213–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell L. L., Peterson C. M., Rud S., Jutkowitz E., Sarkinen A., Trost S., Porta C. M., Finlay J. M., & Gaugler J. E (2018). “It’s like a cyber-security blanket:” The utility of remote activity monitoring in family dementia care. Journal of Applied Gerontology. doi: 10.1177/0733464818760238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moylan M. (2017). Best Buy bets on tech for monitoring elderly parents Retrieved from https://www.mprnews.org/story/2017/07/27/best-buy-bets-on-tech-for-monitoring-elderly-parents.
- Mulvenna M. Hutton A. Coates V. Martin S. Todd S. Bond R. & Moorhead A (2017). Views of caregivers on the ethics of assistive technology used for home surveillance of people living with dementia. Neuroethics, 10, 255–266. doi: 10.1007/s12152-017-9305-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine (2016). Families caring for an aging America. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Nauha L., Keranen N. S., Kangas M., Jamsa T., & Reponen J (2016). Assistive technologies at home for people with a memory disorder. Dementia. doi: 10.1177/1471301216674816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijhof N. van Gemert-Pijnen L. J. Woolrych R. & Sixsmith A (2013). An evaluation of preventive sensor technology for dementia care. Journal of Telemedicine and Telecare, 19, 95–100. doi: 10.1258/jtt.2012.120605 [DOI] [PubMed] [Google Scholar]
- Pearlin L. I. Mullan J. T. Semple S. J. & Skaff M. M (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30, 583–594. [DOI] [PubMed] [Google Scholar]
- Preusse K. C. Mitzner T. L. Fausset C. B. & Rogers W. A (2017). Older Adults’ Acceptance of Activity Trackers. Journal of Applied Gerontology, 36, 127–155. doi: 10.1177/0733464815624151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- QSR International.(2015). Released 2015. NVivo for Windows, Version 11. [Google Scholar]
- Radloff L. (1977). The center for epidemiological studies-depression scale: A self-report depression scale for research in the general population. Applied Psychological Measurements, 3, 385–401. [Google Scholar]
- Redfoot D., Feinberg L., & Houser A (2013). The aging of the baby boom and the growing care gap: A look at future declines in the availability of family caregivers Retrieved from https://www.aarp.org/content/dam/aarp/research/public_policy_institute/ltc/2013/baby-boom-and-the-growing-care-gap-in-brief-AARP-ppi-ltc.pdf.
- Reeder B. Meyer E. Lazar A. Chaudhuri S. Thompson H. J. & Demiris G (2013). Framing the evidence for health smart homes and home-based consumer health technologies as a public health intervention for independent aging: A systematic review. International Journal of Medical Informatics, 82, 565–579. doi: 10.1016/j.ijmedinf.2013.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe M. A., Kelly A., Horne C., Lane S., Campbell J., Lehman B.,…, Benito A. P. (2009). Reducing dangerous nighttime events in persons with dementia by using a nighttime monitoring system. Alzheimer’s & Dementia, 5, 419–426. doi: 10.1016/j.jalz.2008.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R. Wahl H. W. Matthews J. T. De Vito Dabbs A. Beach S. R. & Czaja S. J (2015). Advancing the aging and technology agenda in gerontology. The Gerontologist, 55, 724–734. doi: 10.1093/geront/gnu071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shreve J., Baier R., Epstein-Lubow G., & Gardner R (2016). Dementia caregivers’ technology preferences: Design insights from qualitative interviews. Gerontechnology, 14, 89–96. [Google Scholar]
- Singal A. G. Higgins P. D. & Waljee A. K (2014). A primer on effectiveness and efficacy trials. Clinical and Translational Gastroenterology, 5, e45. doi: 10.1038/ctg.2013.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone R. I. (2015). Factors affecting the future of family caregiving in the United States. In J. E. Gaugler & R. L. Kane (Eds.), Family caregiving in the new normal. (pp. 57–77). San Diego, CA: Academic Press. [Google Scholar]
- Teri L. Truax P. Logsdon R. Uomoto J. Zarit S. & Vitaliano P. P (1992). Assessment of behavioral problems in dementia: The revised memory and behavior problems checklist. Psychology and Aging, 7, 622–631. [DOI] [PubMed] [Google Scholar]
- Torkamani M., McDonald L., Saez Aguayo I., Kanios C., Katsanou M. N., Madeley L.,…, Jahanshahi M; ALADDIN Collaborative Group (2014). A randomized controlled pilot study to evaluate a technology platform for the assisted living of people with dementia and their carers. Journal of Alzheimer’s disease, 41, 515–523. doi: 10.3233/JAD-132156 [DOI] [PubMed] [Google Scholar]
- Vernooij-Dassen M. J. Felling A. J. Brummelkamp E. Dauzenberg M. G. van den Bos G. A. & Grol R (1999). Assessment of caregiver’s competence in dealing with the burden of caregiving for a dementia patient: A Short Sense of Competence Questionnaire (SSCQ) suitable for clinical practice. Journal of the American Geriatrics Society, 47, 256–257. [DOI] [PubMed] [Google Scholar]
- Wild K. Boise L. Lundell J. & Foucek A (2008). Unobtrusive in-home monitoring of cognitive and physical health: Reactions and perceptions of older adults. Journal of Applied Gerontology, 27, 181–200. doi: 10.1177/0733464807311435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild K. V. Mattek N. Austin D. & Kaye J. A (2016). “Are You Sure?”: Lapses in self-reported activities among healthy older adults reporting online. Journal of Applied Gerontology, 35, 627–641. doi: 10.1177/0733464815570667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K. Arthur A. Niedens M. Moushey L. & Hutfles L (2013). In-home monitoring support for dementia caregivers: A feasibility study. Clinical Nursing Research, 22, 139–150. doi: 10.1177/1054773812460545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff J. L., Mulcahy J., Huang J., Roth D. L., Covinsky K., & Kasper J. D (2017). Family caregivers of older adults, 1999–2015: Trends in characteristics, circumstances, and role-related appraisal. The Gerontologist. doi: 10.1093/geront/gnx093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit S. H., Reever K. E., &Bach-Peterson, J. (1980). Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist, 20, 649–655. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.