Abstract
This article explains, based on a long-term observation, the hard-tissue reaction to different endosseous implant surfaces and different implant designs. A patient who had received a full maxillary implant-supported restoration on basal implants and compression screws followed by immediate loading presented no clinical problems at the 20-year follow-up, but the X-ray examination revealed different hard tissue reactions to different implant types. No bone loss was found around lateral basal implants with fully polished vertical aspects, whereas crater-like bone loss was observed around the vertical shafts of implants with a roughened surface and macromechanical retentions. The case seems to indicate that roughened surfaces around the crestal transmucosal aspect of a dental implant may promote vertical bone loss and peri-implantitis.
Keywords: Bone loss, implant success, implant surface characteristics, lateral basal Implants, peri-implantitis, transmucosal implant diameter
INTRODUCTION
From the 1st day one of modern dental implantology until about the middle of the 1990s, implant bodies were manufactured without enlarged surface areas even when using an immediate-loading protocol.[1] Sandblasting and acid etching were unknown at the time, and the massive marketing efforts undertaken by various dental implant manufacturers had not yet set in. These marketing campaigns and the idea of “specific,” “bone-friendly,” and “accelerating” surfaces allowed various manufacturers to raise their prices for implants and to create a mental environment in which clinicians quickly forgot that “osseointegration” as defined by Per-Ingvar Brånemark[2] was first observed on polished titanium surfaces and that these surfaces had been used for decades and very successfully at that time, and seemingly again today.
The patient whose case is described in the present article had been treated at a time when various designs of lateral basal implants were available on the market; clinicians had not yet developed a preference for a specific surface configuration. This case with a long follow may be useful to reconsider the use of rough surfaces.
MATERIALS AND METHODS
In early 1998, a 42-year-old male patient, otherwise healthy but fully edentulous patient, a very heavy smoker, requested dental implant treatment for his upper jaw. The patient was mainly concerned about not being able to properly taste his food and combat an emetic tendency when wearing his complete maxillary denture; he was, on the other hand, not at all bothered by his mandibular denture.
Under local anesthesia, a circular full-thickness flap was raised, and six lateral basal implants and three compression-screw implants were inserted [Figures 1–4]. Lateral basal implants at that time were manufactured from commercially pure Grade 1 titanium, whereas compression screws were made from Ti6 Al4V titanium alloy with a sandblasted (Al2O3, 50 μm) and etched endosseous surface [Table 1]. On the day the implants were placed; the treatment provider had implants from various brands on hand and used them as a “mix,” with the sole clinical consideration being proper anchorage in the cortical bone for good retention and load transmission. The development (evolution) of true “lateral basal implants” involved the following steps:
Figure 1.

Single base-plate lateral basal implant with ribbed shaft and full sandblasting, as used since the mid-1990s. The surface enlargement implemented the ideas that circulated in mainstream dental implantology, where it was claimed that to obtain better retention, the surface of the implant had to be roughened
Figure 4.
Close-up of the implants in the upper left quadrant
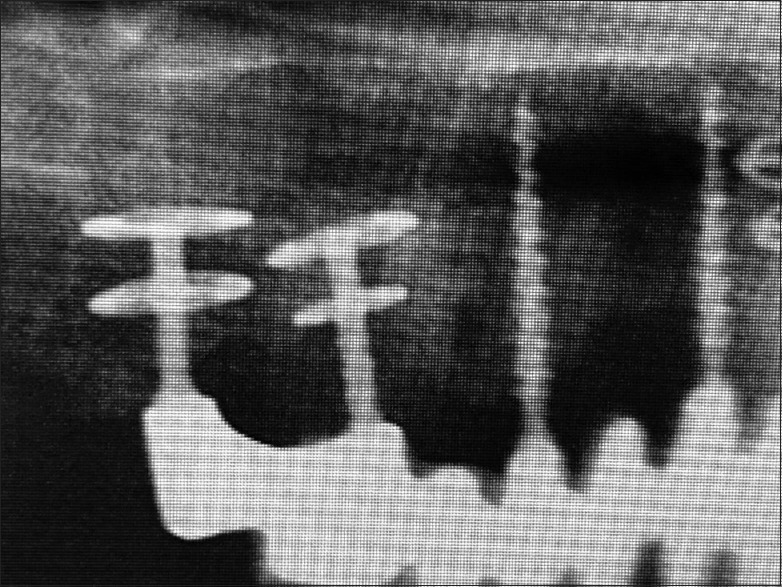
Table 1.
Description and surface characteristics of all implants used in the case
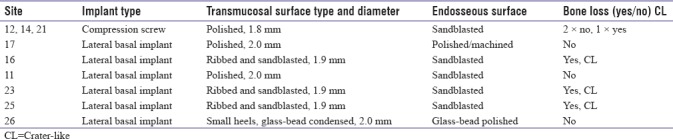
Figure 3.
Close-up of implants 16 and 17. The fully machined/polished implant at site 17 appears fully integrated and polished without any bone loss after 20 years. The implant with its ribbed and sandblasted shaft at site 17 exhibits crater-like bone loss extending at least to the crestal disk plate. We cannot know, however, if the same would have been resulted, if the shaft would be sand-blasted but not ribbed
Initially, starting around 1988, all implants were produced with sandblasted endosseous and transmucosal surfaces [Figure 1]
After about 1996, implants with a polished surface appeared on the market. Some of them were fully polished [Figure 5], while in others the base plates were still sandblasted and only the vertical implant parts were left polished.[3]
Figure 5.

Single-disk lateral basal implant as produced approximately from 2000 onward. The implant is fully machined, and no surface modification is applied whatsoever
The lateral basal implants were chosen to accommodate the morphology of the bone and obtain bilateral (vestibular and palatal) cortical support for the base plates.
During the 20 years in service, a total of three metal-ceramic bridges were delivered to keep the occlusion, mastication, and vertical situation stable and to accommodate the patient's esthetic needs [Figure 6].
Figure 6.

The fourth metal-ceramic bridge before delivery in 2018. All bridges had been cemented with long-term temporary cement and exhibited a highly symmetrical design, allowing an equal bilateral pattern of chewing
RESULTS
A thorough look at each individual implant after 20 years on the panoramic radiograph reveals that rough implant surfaces (maybe in combination with the macrotexture of the shaft) favor the development of vertical bone loss [Table 1].
All lateral basal implants were equipped with a screw-connected abutment (on an external M 1.8 thread) for cementation. No anti-rotational feature was available between the abutment and the implant. Compression screws featured a single-piece design.
The results of the treatment are shown in Figures 2,6 and 7 and discussed in the figure legends.
Figure 2.
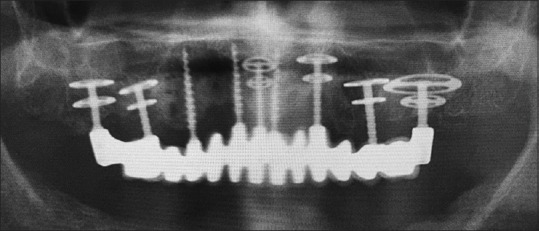
A 20-year postoperative maxillary radiograph. Crater-like bone loss is only present around implants 15, 23 and 25; no other implants areaffected. Lateral basal implants were anchored in the lateral and palatal cortical bone of the maxilla. Enlargened sections of this panoramic picture is dispayed
Figure 7.

At the 20-year follow-up, the mucosa around implants 12 and 25 presented as slightly red and the vestibular mucosa around implant 25 appeared irregular and swollen with signs of inflammation. All implants were stable, and the patient reported no pain
Two of the three compression screws (KOS 3.0 15) showed no vertical or crater-like bone loss after 20 years in function; one compression screw showed 2 mm of crestal bone loss after this period. Implant 23 exhibited crater-like bone loss up to the fifth rib, that is, up to a depth of 5 mm. The double-disk implant 25 – External (thread) Double Disk 9/7 H6, ribbed to the crestal disk plate and fully sandblasted – exhibited peri-implantitis,[4] for example, nonintegration of the vertical shaft all the way up to the basal disk plate and bone loss medial to the inter-disk distance. Implant 27 – EDD 15/9 H4, with a surface condensed through blasting with glass beads, a surface treatment resulting in a very smooth and homogeneous implant surface – appeared fully integrated, with no vertical or crater-like bone loss after 20 years.
The results can be summarized as follows:
None of the lateral basal implants featuring polished shafts showed any signs of bone loss after 20 years in use
All of the lateral basal implants featuring sandblasted shafts showed crater-like bone loss of at least 5 mm
Compression-screw implants with polished and thin mucosal contact surfaces showed not >2 mm vertical bone loss after 20 years; two of these three implants showed no vertical bone loss at all after 20 years in function
Although three implants were affected by peri-implantitis with crater-like bone loss of >5 mm, the patient did not complain about any pain or discomfort.
DISCUSSION
Lateral basal implants have been in use since 1973 when Julliet introduced his T3D implant in France.[5] These designs utilize the lateral/vestibular and the lingual/palatal cortical bone for the initial (immediate) transmission of masticatory loads, while the implant osseointegrates in the core pats over time. The implants show a dual mode of integration: All slots are first filled with woven bone that is later remodeled. The base plates are on average 0.6 mm high; the inter-disk distance is 3 mm. Practitioners (and the manufacturers of lateral basal implants advised by them) understood very early that they could not benefit from any “specific” implant surface when it comes to immediate-loading protocols. Regardless of this we keep seeing, to this very day, that all large implant manufacturers try to sell their (roughened and somehow “specific”) Implant surfaces at elevated prices, and quite a few of them try to justify this price by mentioning that that this surface leads to faster integration (“Cut Time into Half”). Straumann for some years, even falsely claimed that their surface cut the time needed in half. The fact that these companies find customers for such a combination [rough/specific surface for immediate loading] only shows how seriously preclinical and clinical education at dental schools is out of date. Properly educated dentist would not believe in such a combination and definitively not spend extra money for this.
Lateral basal implants are used predominately in cases with reduced vertical bone supply, utilizing as they do the full width of the bone. Another good reason for using these designs is the possibility of using an immediate-loading protocol. Disadvantages of lateral basal implants are the necessity of flap reparation (flapless placement is not possible) and the reduced stability against lateral forces (i.e., cross-arch stabilization through the bridge or application of bone screws to screw-lock the base plates are necessary).
Compression screw implants show a conical design of the endosseous implant body, combined with quite voluminous threads (thread depth 0.25 mm or more). They are inserted into undersized drill holes, thereby compressing the surrounding spongious bone. Their use requires the presence of compressible bone; hence, they are not indicated for use in very dense bone (D1 according to Lekholm and Zarb) or nonmineralized bone (D4 according to Lekholm and Zarb) or in class D5 or D6 bone according to Paraskevic.[6]
The case presented here clearly illustrates the clinical differences between polished vertical mucosal penetration surfaces (implant shafts) and rough shafts with macroretentions.
It also shows clearly that the clinical success of lateral basal implants does not depend on osseointegration of the vertical parts of the implant and that only the base plate(s) in the region of the cortical aspects of the jaw bone must be in stable contact with bone for clinical success.
Our results compare well to the long-term findings of Simion et al.,[7] Scortecci et al.,[8] and Ihde.[9]
One advantage of lateral basal implants over crestal implant types is the fact that osseointegration along the vertical implant part is not required for implant success. The success of these implants in function depends solely on the transmission of loads between the base plates and the cortical bone into which the base plates integrate. Hence, immediate loading of lateral basal implants is possible even also in cases where implants are placed, for example, trans-sinusal or into fresh extraction sockets.
As this is only a report about one single case, further research on more cases or case series is necessary to confirm the findings.
CONCLUSION
If a combination of lateral basal implants and compression screws is used to restore an edentulous maxilla, good long-term results are possible. This treatment modality facilitates an immediate-loading protocol.
Polished vertical (transmucosal) implant surfaces on lateral basal implants and a thin diameter at the point of mucosal penetration provide a sustainable environment for a stable (unaltered) bone level even after 20 years.
If lateral basal implants with sandblasted shaft and macroretentions (ribbed shafts) are used, crater-like bone loss is observed after a number of years.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Linkow LL, Miller RJ. Immediate loading of endosseous implants is not new. J Oral Implantol. 2004;30:314–7. doi: 10.1563/0683.1. [DOI] [PubMed] [Google Scholar]
- 2.Brånemark PI, Adell R, Albrektsson T, Lekholm U, Lundkvist S, Rockler B. Osseointegrated titanium fixtures in the treatment of edentulousness. Biomaterials. 1983;4:25–8. doi: 10.1016/0142-9612(83)90065-0. [DOI] [PubMed] [Google Scholar]
- 3.Ihde S, editor. Heidelberg: Springer; 2004. Principles of BOI. [Google Scholar]
- 4.Kopp S, Maier T, Ihde S. Peri-implantitis and implant characteristics in dental implantology: A systematic review. CMF Implant Dir. 2011;6:97–124. [Google Scholar]
- 5.Julliet Jean-Marc: United States Patent 3,925,892 [Google Scholar]
- 6.Ihde S, Ihde A, Lysenko V, Konstantinovic V, Palka L. New systematic terminology of cortical bone areas for osseo-fixated implants in strategic oral implantology. J Anat. 2016;1:7. [Google Scholar]
- 7.Simion M, Nevins M, Rasperini G, Tironi F. A 13- to 32-year retrospective study of bone stability for machined dental implants. Int J Periodontics Restorative Dent. 2018;38:489–93. doi: 10.11607/prd.3694. [DOI] [PubMed] [Google Scholar]
- 8.Scortecci GM, Misch CE, Benner KU, editors. London: Martin Dunitz; 2000. Implant and Restorative Dentistry. [Google Scholar]
- 9.Ihde S. Outcomes of immediately loaded full arch reconstructions on basal implants and teeth in the mandible: Restrospective report on 115 consecutive cases during a period of up to 134 months. CMF Implant Dir. 2008;1:50–60. [Google Scholar]


