Abstract
This systematic review and meta-analysis examined the dose-response relationship between exercise and cognitive function in older adults with and without cognitive impairments. We included single-modality randomized controlled aerobic, anaerobic, multicomponent or psychomotor exercise trials that quantified training frequency, session and program duration and specified intensity quantitatively or qualitatively. We defined total exercise duration in minutes as the product of program duration, session duration, and frequency. For each study, we grouped test-specific Hedges’ d (n = 163) and Cohen’s d (n = 23) effect sizes in the domains Global cognition, Executive function and Memory. We used multilevel mixed-effects models to investigate dose-related predictors of exercise effects. In healthy older adults (n = 23 studies), there was a small positive effect of exercise on executive function (d = 0.27) and memory (d = 0.24), but dose-parameters did not predict the magnitude of effect sizes. In older adults with cognitive impairments (n = 13 studies), exercise had a moderate positive effect on global cognition (d = 0.37). For older adults with cognitive impairments, we found evidence for exercise programs with a short session duration and high frequency to predict higher effect sizes (d = 0.43–0.50). In healthy older adults, dose-parameters did not predict the magnitude of exercise effects on cognition. For older adults with cognitive impairments, exercise programs with shorter session duration and higher frequency may generate the best cognitive results. Studies are needed in which different exercise doses are directly compared among randomized subjects or conditions.
Introduction
The number of dementia patients may triple to 135M globally by 2050 [1]. Dementia is characterized by a progressive decline in neurocognitive function. Pharmacological treatments may moderate symptoms but can cause adverse effects [2]. Exercise might be an effective and safe alternative to drugs to slow cognitive decline. Exercise may improve certain cognitive functions in old age by inducing the release of brain-derived neurotrophic factor (BDNF [3,4]) and insulin-like growth factor-1 (IGF-1 [5,6]), thereby potentially facilitating structural and connectivity changes in the hippocampus, temporal lobe, frontal areas and corpus callosum [7–11], structures that are activated during tasks requiring executive function, attention, processing speed and memory.
Exercise type and dose-parameters may determine the magnitude of effects on cognition and how long these effects persist after an intervention [12,13]. Dose-parameters include program duration (number of weeks), session duration (length of each session in minutes including warm-up and cool-down), frequency (session rate per week) and intensity. Exercise intensity refers to the amount of effort or energy that is required to perform a physical activity [14] and is often expressed as percentage of maximal oxygen update (VO2max) required during a physical activity [15].
High compared with low exercise dose-parameters tend to predict better physical fitness outcomes in older adults. Meta-analyses revealed that longer program duration [16–18] and higher intensity [16,18] were associated with gains in muscle strength and VO2max of older adults. Program duration also correlated with gains in endurance, lower extremity muscle strength, balance and levels of Activities of Daily Living (ADL) in older subjects with dementia [19]. Exercise intensity was related to improvements in fitness- and health-related parameters such as VO2max and mortality in healthy middle-aged and older adults [20–25]. Exercise-induced improvements in physical fitness may facilitate brain plasticity and secondarily improvements in cognitive function through increases in brain activation. Indeed, higher cardiorespiratory fitness [26,27] and exercise-induced adaptions in blood lactate [28] were previously associated with higher brain activation in anterior and motor areas [26,27], fronto-cingulo-parietal networks [28] and better executive performance [26,27]. Considering that exercise dose-parameters are related to increases in fitness, and fitness increases may in turn be related to cognitive function by facilitating brain plasticity, exercise dose-parameters may be related to increases in cognitive functions. Indeed, in healthy young and older adults, high dose-parameters of acute exercise were related to gains in executive function such as processing speed and inhibitory control [29–32]. Exercise-induced cognitive benefits of acute exercise may accumulate to greater and lasting cognitive improvements with chronic exercise in a dose-specific way.
The relationship between exercise dose-parameters and cognitive functions in chronic exercise studies is still not fully understood. A meta-analysis suggested that exercising for 45–60 minutes per session, at least at moderate intensity, and at the highest feasible frequency can improve global cognition, attention, executive function and (working) memory in healthy adults over 50 [33], but the authors did not examine total dose. A meta-analysis of 18 randomized controlled trials (RCTs) [34] showed that weekly exercise duration (≤150 or >150 minutes) was not related to changes in cognitive function in older adults with cognitive impairments, specifically Alzheimer’s disease (AD) and non-AD dementia, but other dose-parameters were not investigated. There is thus a need to systematically review whether improvements in cognitive function scale with exercise dose-parameters separately and as total dose and if dosing effects vary with cognitive status. The aim of the present review was to examine the relationship between exercise dose-parameters (program and session duration, frequency, intensity) and cognitive function (global cognition, executive function, memory) in adults with vs. without cognitive impairments. We quantified the dose-response relationship separately between the responses to aerobic, anaerobic, multimodal, and psychomotor interventions and changes in global cognition, executive function, and memory using advanced statistical modeling. We hypothesized that the magnitude of exercise effects on global cognition, executive function, and memory is related to exercise dose-parameters separately or combined as total dose. The results of the present study can be used to update exercise recommendations and implement exercise programs for older adults with and without cognitive impairments.
Methods
The current protocol is registered with the Open Science Framework (url: https://osf.io/qe43p/). PRISMA guidelines were followed [35] (S1 Checklist).
Search strategy and selection criteria
We searched databases PubMed, Embase, Psycinfo, Web of Science and the Cochrane Central Register of Controlled Trials from inception (database-specific onset date) through December 4th, 2017. We included human studies that were Randomized Controlled Trials (RCTs). Specific Emtree (Embase) and MeSH (PubMed) terms included exercise, cognition, memory and executive function. Nonspecific terms represented activity, training type, cognitive outcome and study design. We filtered studies with children, adolescents or patient populations other than Mild Cognitive Impairment (MCI), Vascular Cognitive Impairment (VCI) or dementia, protocol papers and virtual designs. S1 Table lists the search terms.
Two authors (LS and MvH) independently selected articles for inclusion by screening the titles and abstracts (95.3% agreement) resulting in full-text screening of the articles in question. Full-text screening was done for all articles (LS) selected by either one of the authors. Lastly, we handsearched reviews for relevant articles (LS).
Inclusion- and exclusion criteria
We included studies that satisfied the following criteria: (1) participants were aged ≥18 years, (2) participants were healthy or diagnosed with MCI, VCI or dementia, (3) the intervention consisted of aerobic, anaerobic, multicomponent or psychomotor exercise of any intensity or frequency, and a duration of ≥4 weeks (as meaningful improvements are believed to appear after ≥4 weeks of exercise [36]), (4) the exact range of frequency and session duration was specified, (5) the training intensity was specified descriptively (e.g., ‘moderate intensity’) or objectively, (6) there was a cognitive outcome measure measured by neuropsychological tests. Studies were excluded if: (1) the physical intervention included a non-physical component and (2) the control group performed non-contrasting activities (contrasting activities include non-physical activity or stretching and toning).
Data extraction
We extracted the following data from the included studies: sample characteristics (sample size, age, gender, education, cognitive health status), intervention parameters (exercise mode, program and session duration, frequency and intensity) and outcome measures (means, standard deviations or F-values of the cognitive tests at baseline and post-intervention). If necessary, the original authors were contacted for any missing data.
Dose
We calculated exercise duration in minutes for every study using the program duration (weeks), session duration (minutes) and frequency. We averaged frequency, total session duration and intensity measures if necessary (i.e., if sessions lasted 30–40 minutes, we used 35 minutes as average).
For aerobic and psychomotor exercise, intensity was expressed as % maximum heartrate (HRmax), % heart rate reserve (HRR), or % maximum oxygen update (VO2max). For anaerobic exercise, we multiplied the target number of sets and repetitions with the training intensity in % one repetition maximum (1RM, the maximum amount of weight that a person can lift once) or VO2max. For multicomponent exercise, we calculated the average intensity of the aerobic and anaerobic intensity coefficients if both could be calculated from the data.
If intensity was given descriptively or in terms of the rate of perceived exertion (RPE Borg scale [37]), we took the corresponding heart rate in accordance with the American College of Sports Medicine guidelines [36]. We set ‘light’ intensity as 30–40% HRR/1RM, ‘moderate’ intensity as 60–80% of HRR/1RM and ‘high’ intensity as 80–100% HRR/1RM.
Effect size
We calculated Hedges’ g effect sizes (ESs) for each cognitive outcome. We subtracted the mean change (post-pre) in the control group from the mean change in the exercise group and divided this difference by the pooled standard deviation of the baseline scores [38]. We obtained Hedges’ d by adjusting Hedges’ g for small sample size bias [39].
If means and standard deviations could not be retrieved from the text, we retrieved the F statistic for the Group x Time interaction and used it to calculate Cohen’s d:
We also adjusted Cohen’s d for small sample size bias. When a lower test score represented better performance, we multiplied Hedges’ (n = 163) and Cohen’s (n = 23) d with -1, so that a positive d always indicates better performance in the exercise group. We considered Hedges’ and Cohen’s d = 0.2, d = 0.5 and d = 0.8 as, respectively, small, medium and large effect sizes [40].
We grouped the effect sizes of the cognitive tests in 1) global cognition, 2) executive function, or 3) memory. We identified tests as falling in one of these domains by using the categorization of the respective authors (i.e., if a test was described as a global cognitive test, we grouped the test in global cognition). When a test was described as memory test in some papers but as executive function test in others (e.g., working memory tests), we used the categorization that most authors adhered to. For this reason, two authors (LS and MvH) decided to group working memory tests within the executive function domain. Appendices 4a and 4b list the tests that were grouped in each domain for every study. We excluded cognitive tests that could not be grouped within our domains (e.g., reading ability or visuospatial ability). 95% Confidence intervals for the average ESs were calculated with the formula
where SE is the standard error:
[39].
Study quality
One author (LS) evaluated the quality of the included studies using the 11-item Physiotherapy Evidence Database (PEDro) scale [41]. The PEDro scale rates the methodological quality of a study based off of randomization, allocation, blinding, analyses and reporting of outcomes. Scores ≤3 indicate poor study quality, 4–5 fair quality and 6–10 good to excellent quality.
Statistical analyses
We computed means and standard deviations. We used the SPSS MeanES macro ([42,43], SPSS 23.0, IBM, Armonk, NY) to generate mean effect sizes and indices of heterogeneity (Cochran’s Q, I2) [44] for the forest plots, and S2 and S3 Tables. I2 values<0.25 were indicative of limited heterogeneity, 0.25<I2<0.50 indicated moderate heterogeneity and I2>0.50 large heterogeneity [44]. We used R version 3.4.3 (R Core Team, 2013) and the R Metafor package [45] to analyze the data and set two-tailed significance at p≤0.05. Publication bias was evaluated with a funnel plot (S1 Fig) [46]. To analyze the effects of multiple moderators on ESs, we used multilevel mixed effects (with effect size ID and study ID as random effects) models using restricted maximum likelihood estimation [47,48]. Such models account for dependencies between test-specific effect sizes by taking into account the nesting of multiple effect sizes within studies. We used mixed-effects models to examine: 1) differences in exercise effects between healthy older adults with and without cognitive impairments; 2) differences in exercise effects for global cognition vs. executive function and memory; 3) differences in exercise effects across the four exercise types (aerobic, anaerobic, multimodal, psychomotor); 4) associations between a) total exercise duration and b) intensity and cognitive effects, and 5) associations between the separate dose-parameters (program duration, session duration, frequency) and cognitive effects.
Results
Study characteristics
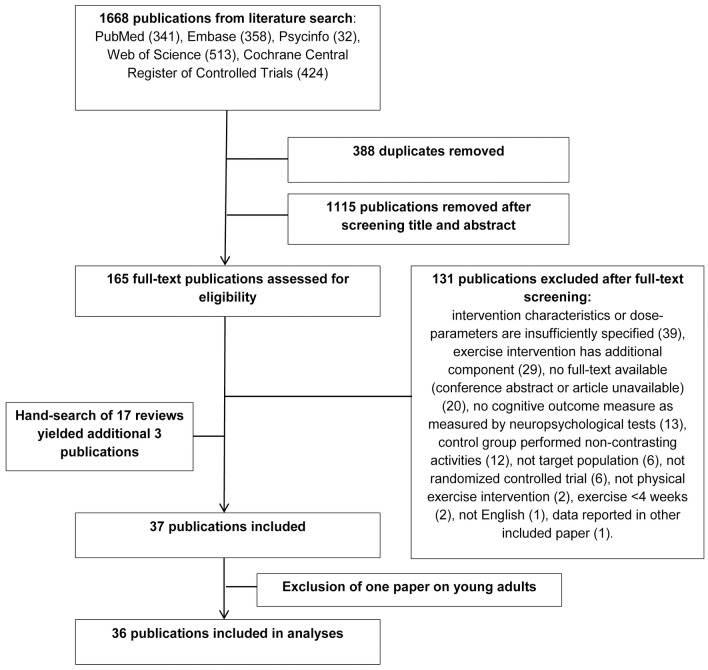
Fig 1 depicts the selection process. A total of 37 studies were eligible for inclusion [49–86]. As 36 of the 37 studies included older populations (>50), we excluded one study with young adults [86] to facilitate comparison. Tables 1 and 2 list the included studies.
Fig 1. Study selection process.
Table 1. Study characteristics for included studies with healthy older adults.
| Author, year | N (#♀) Intervention/control |
Age (M±SD) Intervention/control |
Baseline MMSE (M±SD) Intervention/control |
Intervention type (ar/an/mc/pm)a | Intervention activities | Program duration (weeks), session duration (minutes), frequency(#/wk) | Exercise intensity | Control |
|---|---|---|---|---|---|---|---|---|
| Albinet et al., 2010 | 12(6) / 12(7) | 70.9±4.9 / 70.4±3.4 | 28.5±1.1 / 29±0.9 | ar | walking, circuit-training, step, gradually running | 12,60,3 | 40–60% HRR+HRrest | stretching |
| Albinet et al., 2016 | 19(13) / 17(13) | 67±5 / 66±5 | 29.1±1.1 / 28.7±1.5 | ar | aerobics, swimming | 21,60,2 | 40–65% HRR | stretching |
| Ansai & Rebelatto, 2015 | 23(17) / 23(15) 23(15) / 23(15) |
81.9±1.9 / 82.6±2.6 82.8±2.8 / 82.6±2.6 |
24.3±3.3 / 25.3±3.5 25.1±3.4 / 25.3±3.5 |
mc an | cycle ergometer & strength exercises of major muscle groups with extra loading leg press, chest press, calf, back extension, abdominal and rowing | 16,60,3 | AR: 60–85% of HRR, AN: 70–80% of 1RM corresponding to RPE 14–17, 2 sets of 1–15 repetitions 90–100% 1RM as referred by authors, 3 sets of 10–12 repetitions | non-active |
| ……‥ | ……‥ | |||||||
| Best et al., 2015 | 54♀♀ / 49♀♀ | 69.5±2.7 / 70.0±3.3; | 28.5±1.3 / 28.8±1.2; | an | resistance training with machine and non-machine exercises | 52,60,1 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone |
| 52♀♀ / 49♀♀ | 69.4±3.0 / 70.0±3.3 | 28.6±1.5 / 28.8±1.2 | an | resistance training with machine and non-machine exercises | 52,60,2 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone | |
| Coetsee & Terblanche, 2017 | 13(10) / 19(11) | 64.5±6.3 / 62.5±5.6 | MoCA: 27.9±1.5 / 28.2±1.6 |
ar | high-intensity interval treadmill walking | 16,30,3 | 4 intervals of 4 minutes at 90–95% HRmax, interspersed by 3 minutes active recovery at 70% HRmax |
no exercise |
| 13(10) / 19(11) | 61.6±5.8 / 62.5±5.6 | MoCA: 27.6±1.3 / 28.2±1.6 |
ar | continuous treadmill walking | 16,47,3 | 70–75% Hrmax | no exercise | |
| 22(15) / 19(11) | 62.4±5.1 / 62.5±5.6 | MoCA: 27.5±1.3 / 28.2±1.6 |
an | upper and lower body resistance exercises using machines and free weights | 16,30,3 | 50–100% of 10RM, 10 sets of 10 repetitions | no exercise | |
| Dao et al., 2013 | 37♀♀ / 36♀♀ | 69.2±2.6 / 69.8±3.2; | 28.8±1.2 / 28.8±1.2; | an | resistance training with machine and non-machine exercises | 52,60,1 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone |
| 41♀♀ / 36♀♀ | 69.4±3.0 / 69.8±3.2 | 28.5±1.6 / 28.8±1.2 | an | resistance training with machine and non-machine exercises | 52,60,2 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone | |
| Fabre et al., 2002 | 8(6)/ 8(7) | 65.4±2.2 / 65.7±1.5 | nrb | ar | walking and running | 8,60,2 | Ventilatory threshold corresponding to 50–70% HRmax | leisure activities |
| Ferreira et al., 2015 | 22(15) / 22(19) | 66.2±5.6 / 69.2±4.8 | 28.8±1.6 / 28.7±1.5 | ar | supervised walking | 24,40–50,3 | 60–80% HRR | social interaction |
| Iuliano et al., 2015 | 20(11) / 20(12) | 65.80±6.32 / 66.47±6.32 | nrb | an | whole-body strength exercises on isotonic machines | 12,30,3 | 60–85%1RM, 3 sets of 6–12 repetitions | non-active |
| 20(12) / 20(12) | 68.44±6.40 / 66.47±6.32 | nrb | ar | cardiovascular training on ergometer machines | 12,30,3 | 50–80% HRR | non-active | |
| 20(13) / 20(12) | 66.67±5.83 / 66.47±6.32 | nrb | pm | postural and balance exercises | 12,40,3 | 30–40% HRmax corresponding to ‘low intensity’ exercise | non-active | |
| Jonasson et al., 2017 | 29(15) / 29(17) | 68.4±2.54 / 69.0±2.91 | 28.7±1.16 / 29.5±0.64 | ar | walking or jogging, cycling or training on cross-trainer | 24,30–60, 3 | 40–80% HRmax | stretching and toning |
| Kimura et al., 2010 | 65(40) / 54(30) | 73.6±4.7 / 75.2±6.3 | 27.8±1.8 / 27.9±2.1 | an | progressive resistance and balance training | 12,90,2 | 60–100% of 1RM corresponding to ‘moderate to high intensity’, 2–3 sets of 10 repetitions | health education |
| Liu-Ambrose et al., 2010 | 54♀♀ / 49♀♀ | 69.5±2.7 / 70.0±3.3 | 28.5±1.3 / 28.8±1.2 | an | resistance training with machine and non-machine exercises | 52,60,1 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone |
| 52♀♀ / 49♀♀ | 69.4±3.0 / 70.0±3.3 | 28.6±1.5 / 28.8±1.2 | an | resistance training with machine and non-machine exercises | 52,60,2 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone | |
| Liu-Ambrose et al., 2012 | 20♀♀ / 17♀♀ | 69.7±2.8 / 69.2±3.2 | 28.6±1.2 / 29.1±1.1 | an | resistance training with machine and non-machine exercises | 52,60,1 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone |
| 15♀♀ / 17♀♀ | 68.9±3.2 / 69.2±3.2 | 29.1±0.8 / 29.1±1.1 | an | resistance training with machine and non-machine exercises | 52,60,2 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone | |
| Maass et al., 2015 | 21(11) / 19(11) | 68.8±4.5 / 67.9±4.1 | 28.95±0.92 / 28.95±0.91 | ar | interval training on stationary treadmills | 12,40,3 | 65–70% HRR | progressive muscle relaxation/stretching |
| Madden et al., 1989 | 25(11) / 26(14) | 66.52±4.07 / 66.62±3.54 | nrb | ar | supervised bicycle ergometry, walking/jogging | 16,60,3 | 70% HRR | wait list |
| Muscari et al., 2010 | 60(28) / 60(30) | 68.8±2.5 / 69.9±2.8 | 26.7±nr/27±nr | ar | cycle ergometer, treadmill and free-body activity | 52,60,3 | 70% HRmax | lifestyle education |
| Nouchi et al., 2013 | 32(nr**) / 32(nr**) | 66.75±4.61 / 67.06±2.82 | 27.91±1.25 / 27.94±1.27 | mc | combination aerobic, strength and stretching exercise | 4,30,3 | 60–80% HRmax | wait list |
| Ruscheweyh et al., 2011 | 20(14) / 21(14) | 60.1±6.2 / 58.1±6.7 | 29.5±0.8 / 29.3±0.8 | ar | nording walking | 24,50,3–5 | 50–60% maximal exertion | non-active |
| 21(13) / 21(14) | 62.5±6.4 / 58.1±6.7 | 29.2±0.8 / 29.3±0.8 | pm | stretching, limbering and toning of upper and lower extremities | 24,50,3–5 | 30–40% maximal exertion | non-active | |
| Shatil et al., 2013 | 31(22) / 29(19) | 79±5.76 / 81±5.25 | nrb | mc | cardiovascular workout seated and standing, strength training, flexibility training | 16,45,3 | 30–40% HRmax corresponding to ‘low intensity exercise’ | book club |
| Tsai et al., 2015 | 24♂♂ / 24♂♂ | 70.79±3.39 / 72.00±4.14 | 27.88±1.19 / 28.21±0.98 | an | core exercises with machines and free weights | 52,60,3 | 75–80% of 1RM, 3 sets of 10 repetitions | non-active |
| Tsai et al., 2017 | 21♂♂ / 21♂♂ | 66.2±4.9 / 65.7±3.5 | 27.5±3.03 / 27.7±1.80 | ar | cycling on bicycle ergometer or walking on treadmill | 24,40,3 | 70–75% HRR | balance and stretching |
| Tsutsumi et al., 1997 | 13(3) / 14(3) | 67.8±4.9 / 69.8±4.6 | nrb | an | major muscle exercises with weight machines | 12,20–34,3 | 75–85% of 1RM, 2 sets of 8–10 repetitions | no exercise |
| 14(3) / 14(3) | 68.9±7.5 / 69.8±4.6 | nrb | an | major muscle exercises with weight machines | 12,34–60,3 | 55–65% of 1RM, 2 sets of 14–16 repetitions | no exercise | |
| Vedovelli et al., 2017 | 20♀♀ / 9♀♀ | 83.0±6.5 / 77.3±9.9 | 24.1±3.30 / 24.8±3.30 | mc | walking, upper and lower body strengthening exercises | 12,60,3 | 75–85% HRmax, 50–75% 1RM, 3 sets of 10 repetitions | non-active |
aAr = aerobic; an = anaerobic; mc = multi-component; pm = psychomotor.
bnr = not reported.
Table 2. Study characteristics for included studies with older adults with cognitive impairments.
| Author, year | Populationa | N (#♀) Intervention/control |
Age (M±SD) Intervention/control |
Baseline MMSE (M±SD) Intervention/control |
Intervention typeb (ar/an/mc/pm) | Intervention activities | Program duration (weeks), session duration (minutes), frequency(#/wk) | Exercise intensity | Control |
|---|---|---|---|---|---|---|---|---|---|
| Baker et al., 2010 | MCI | 19(10) / 10(5) | 65.3±9.4♀; 70.9±6.7♂ / 74.6±11.1♀; 70.6±6.1♂ | 28.4±1.7♀; 25.6±2.4♂ / 28.6±1.7♀; 27.2±1.8♂ | ar | treadmill, stationary bicycle, elliptical trainer | 24,45–60,4 | (gradual increase to) 75–85% HRR | stretching |
| Bossers et al., 2015 | dementia | 37(29) / 36(25) | 85.7±5.1 / 85.4±5.0 | 15.8±4.3 / 15.9±4.2 | mc | walking + lower-limb strength exercises | 9,30,4 | AR: 50–85% HRmax; AN: 60–100% 1RM corresponding to RPE>12, 2 sets of 6–12 repetitions | social visits |
| 36(28) / 36(25) | 85.4±5.4 / 85.4±5.0 | 15.2±4.8 / 15.9±4.2 | ar | walking | 9,30,4 | 50–85% HRmax | social visits | ||
| Ten Brinke et al., 2015 | probable MCI | 14♀♀ / 13♀♀ | 76.1±3.4 / 75.5±3.9 | 27.5±1.51 / 27.2±1.9 | ar | outdoor walking | 24,60,2 | RPE 13–15, 40–80% HRR | balance and tone |
| 12♀♀ / 13♀♀ | 73.8±3.7 / 75.5±3.9 | 26.7+2.6 / 27.2±1.9 | an | whole-body strength exercises with and without machines | 24,60,2 | 60–80% 1RM corresponding to RPE 13–15, 2 sets of 6–8 repetitions | balance and tone | ||
| Davis et al., 2013 | probable MCI | 30♀♀ / 28♀♀ | 75.5±3.5 / 75.0±3.7 | MoCA: 22.2+2.8 / 22.5±2.8 |
ar | outdoor walking | 24,60,2 | 40–60% HRR | balance and tone |
| 28♀♀ / 28♀♀ | 74.1±3.6 / 75.0±3.7 | MoCA: 21.4+3.4 / 22.5±2.8 |
an | whole-body strength exercises with and without machines | 24,60,2 | 80–100% of 1RM corresponding to ‘high intensity’, 2 sets of 6–8 repetitions | balance and tone | ||
| De Souto Barreto et al., 2017 | dementia | 44(41) / 47(36) | 88.3±5.1 / 86.9±5.8 | 11.4±6.2 / 10.8±5.5 | mc | aerobic, coordination en strengthening exercises | 24,60,2 | 60–80% of HRR/1RM | social activites |
| Kemoun et al., 2010 | dementia | 16(12) / 15(11) | 82.0±5.8 / 81.7±5.1 | 12.6 / 12.9 | mc | exercises in walking, equilibrium, stamina | 15,60,3 | 60–70% HRR | non-active |
| Kwak et al., 2006 | dementia | 15♀♀ / 15♀♀ | 79.67±6.64 / 82.27±7.09 | 14.53±5.34 / 13.47±7.04 | an | chair exercise + stretching | 52,30–40,2–3 | 30–60% VO2max + 2–3 sets of 2–20 repetitions with 7–8 exercises | nr c |
| Liu-Ambrose et al., 2016 | VCI | 35(19)/ 35/(17) | 74.8±8.4 / 73.7±8.3 | 26.3±2.7 / 26.4±3.1 | ar | walking | 24,60,3 | 40–60% HRR | usual care + education |
| Nagamatsu et al., 2013 | probable MCI | 30♀♀ / 28♀♀ | 75.6±3.6 / 75.1±3.6 | 27.4±1.5 / 27.1±1.7 | ar | outdoor walking | 26,60,2 | RPE 13–15, 40–80% HRR | balance and tone |
| 28♀♀ / 28♀♀ | 73.9±3.4 / 75.1±3.6 | 27.0+1.8 / 27.1±1.7 | an | whole-body strength exercises with and without machines | 26,60,2 | 60–80% 1RM corresponding to RPE 13–15, 2 sets of 6–8 repetitions | balance and tone | ||
| Ruiz et al., 2015 | cognitive impairments | 20(16) / 20(16) | 92.3±2.3 / 92.1±2.3 | 18.5±6.2 / 16.4±6.5 | mc | aerobic exercise on cycle-ergometer and lower-limb strength exercises | 8,40–45,3 | 30–40%HRmax corresponding to Borg RPE 10–12, 30–70%1RM, 2–3 sets of 6–8 repetitions | standard care |
| Telenius et al., 2015 | dementia | 87(63) / 83(62) | 87.3±7.0 / 86.5±7.7 | 15.5±0.6 / 15.7±4.9 | mc | strength, balance, and gait exercises | 12,50–60,2 | 12RM, 80–100% of 1RM corresponding to ‘high intensity’, | stretching and relaxing activities |
| Varela et al., 2011 | MCI | 17(nr**) / 15(nr**) | 79.24±10.07 / 79.40±6.72 | 19.86±5.12 / 21.80±3.23 | ar | lower intensity cycling in recumbent bike | 12,30,3 | 40% HRR | recreational activities |
| 16(nr**) / 15(nr**) | 76.44±11.38 / 79.40±6.72 | 20.81±4.69 / 21.80±3.23 | ar | higher intensity cycling in recumbent bike | 12,30,3 | 60% HRR | recreational activities | ||
| Wei & Ji, 2014 | MCI | 30(9) / 30(11) | 66.73±5.48 / 65.27±4.63 | 24.33±1.65 / 25.00±1.29 | mc | handball exercises | 24,30,5 | 60% HRmax | original life entertainment |
aMCI = mild cognitive impairment; VCI = vascular cognitive impairment.
bar = aerobic; an = anaerobic; mc = multi-component; pm = psychomotor.
cnr = not reported.
In total, there were 2007 participants (1772 women). If studies reported different test results of exactly the same samples, we nested the test-specific effect sizes within one study. Studies that only used parts of the same samples were treated as separate studies in the analyses. Although we acknowledge that this induces some non-independence, this method allows for effect sizes to be paired with the correct sample characteristics and sample size. The mean age weighted for sample size was 72.8±6.57 years.
The funnel plot (S1 Fig) revealed some publication bias. Egger’s test was indicative of significant asymmetry (bias = 1.77 (95%CI 0.72–2.81)). The asymmetry was partly due to three studies [64,68,85] which yielded effect sizes >1 with moderate to small sample sizes (respectively n = 60, n = 32, n = 31). These studies remained included in the analyses.
There was a small inverse weighted correlation between higher PEDro score and lower ESs (r = -0.200, p≤0.01).
Tables 3 and 4 show the descriptive statistics for the dose-parameters, total exercise duration (minutes) and intensity (arbitrary unit (a.u.), for details see paragraph Dose in Methods). S4 and S5 Tables list the correlations weighted for sample size per study between dose-parameters and sociodemographic factors. Program duration, session duration and frequency highly correlated for all older adults, with longer programs often having longer but fewer sessions/week.
Table 3. Weighteda descriptive statistics for dose-parameters.
| Healthy | Impaired | Total | |
|---|---|---|---|
| Mean # participants (SD) | 49.4 (22.7) | 54.3 (23.6) | 50.8 (23.0) |
| Mean age (SD) | 70.3 (5.32) | 78.3 (5.59) | 72.8 (6.57) |
| Mean MMSE (SD) | 27.7 (2.49) | 22.9 (5.64) | 25.4 (5.00) |
| Mean program duration in weeks (SD) | 22.9 (16.5) | 21.1 (7.87) | 22.3 (14.4) |
| Mean session duration in minutes (SD) | 49.3 (14.3) | 52.0 (12.8) | 50.1 (13.9) |
| Mean frequency (#/week, SD) | 2.63 (0.67) | 2.60 (0.88) | 2.62 (0.75) |
| Mean total exercise duration in minutes (SD) | 2752.4 (1992.1) | 2647.8 (1053.2) | 2720.0 (1761.7) |
aDescriptive statistics weighted for n per study.
Table 4. Weighteda descriptive statistics for total exercise duration and intensity per exercise category.
| Aerobic | Anaerobic | Multicomponent | Psychomotor | ||
|---|---|---|---|---|---|
| Mean total exercise duration in minutes (SD) | Healthy | 2974.0b (1896.7) | 3627.8c (2232.0) | 1520.1c (938.1) | 1940.4b (1198.4) |
| Cognitive impairments | 2822.8b (1109.5) | 3155.6c (277.3) | 1670.1c (880.1) | - | |
| Mean intensitybc (SD) | Healthy | 65.2b (7.65) | 1655.0c (528.3) | 198.8c (316.0) | 35.0b (n/a) |
| Cognitive impairments | 58.9b (5.45) | 1112.6c (68.9) | 514.0c (384.3) | - |
aDescriptive statistics weighted for n per study.
b%HRR/HRmax/VO2max.
ca.u. arbitrary unit.
Dose-response association of exercise on cognition in healthy older populations
The 23 studies in this category included 1225 participants (1134 women). Mean age was 70.3±5.32 and mean Mini Mental State Examination (MMSE) score was 27.7±2.49 (Table 1).
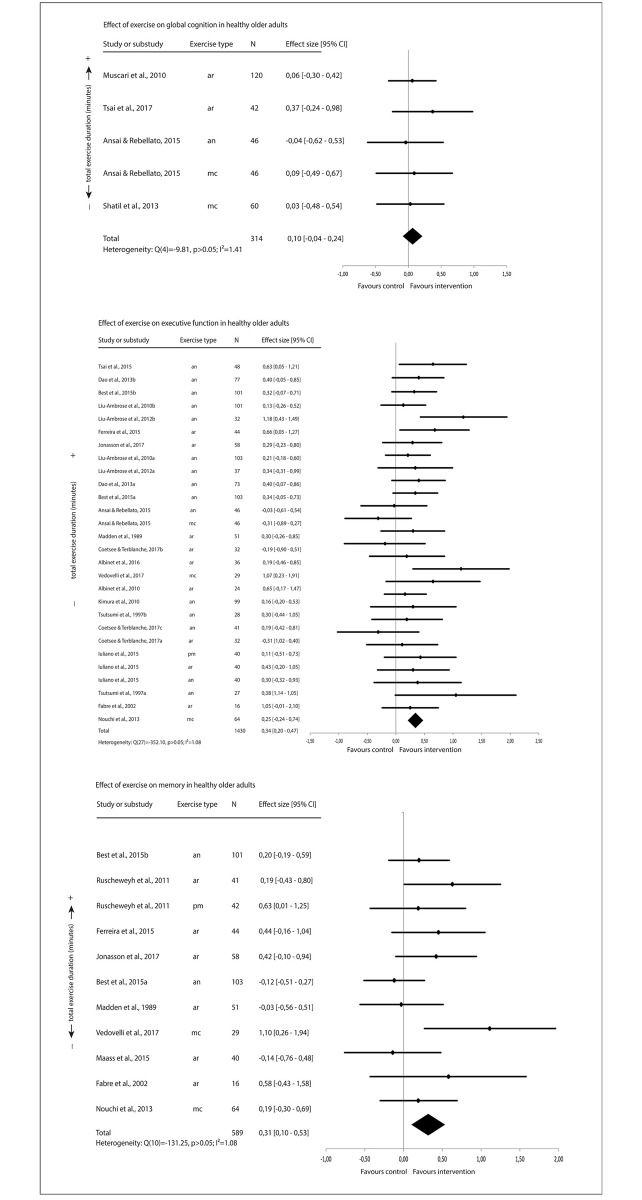
The forest plots (Fig 2) show a small positive exercise effect on averaged executive function and averaged memory but not on averaged global cognition.
Fig 2. Effect of exercise on cognitive function in healthy older adults.
Dose-response association of exercise on cognition in older populations with cognitive impairments
There were 13 studies in older populations with cognitive impairments with varying etiologies (Table 2). In total, there were 782 participants (676 women). The mean age was 78.3±5.64and mean MMSE score was 22.9±5.64.
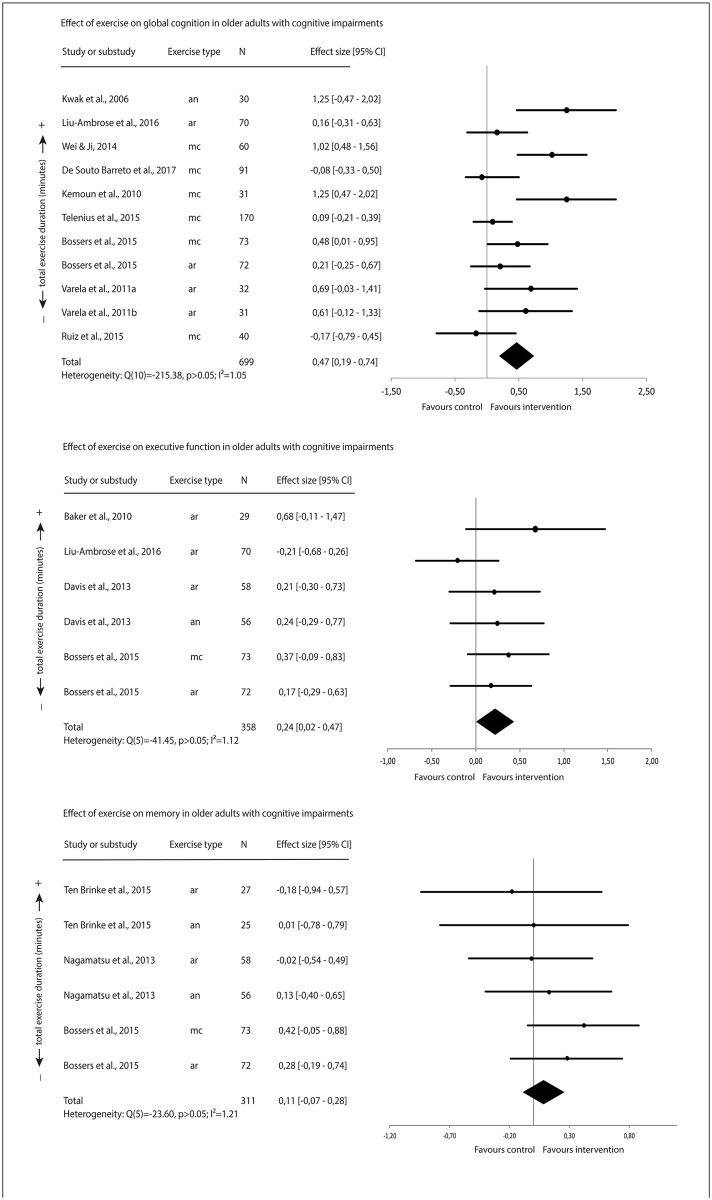
Fig 3 displays the forest plots of the averaged effect sizes. There was a moderate positive effect of exercise on averaged global cognition, and a small positive effect of exercise on averaged executive function. There was no evidence for a significant effect of exercise onaveraged memory.
Fig 3. Effect of exercise on cognitive function in older adults with cognitive impairment.
Mixed-effects models
Mixed-effects models revealed a significant but small overall effect size of d = 0.24 (p≤0.001). The variation in test-specific effect sizes within vs. between studies was respectively 4.8% (p>0.05) and 41.4% (p≤0.001).
Table 5 shows the outcomes for the moderator analyses. For older adults with and without cognitive impairments combined, there were no significant predictors of effect size (healthy, cognitive impairments; F(1,184) = 0.168, p>0.05), cognitive domain (global cognition, executive function, memory; F(2,183) = 0.870, p>0.05), type of exercise (aerobic, anaerobic, multicomponent, psychomotor; F(3,182) = 0.322, p>0.05), program duration (4–12 weeks, 13–24 weeks, >24 weeks; F(2,137) = 1.157, p>0.05), session duration (0–30 minutes, 31–45 minutes, >45 minutes; F(2,183) = 0.816, p>0.05); frequency (1/week, 2/week, 3/week, ≥4/week; F(3,182) = 1.242, p>0.05); total exercise duration (F(1,184) = 0.302, p>0.05), intensity (aerobic training: F(2,77 = 2.396, p>0.05; anaerobic training: F(2,53) = 1.127, p>0.05; multimodal training: F(2,40) = 0.243, p>0.05; psychomotor training not applicable). For healthy older adults specifically, there were no significant predictors of effect size (S6 Table). However when only older adults with cognitive impairments were considered session duration and frequency appeared significant predictors (S6 Table). Post-hoc tests revealed that programs with shorter session duration and higher frequency significantly predicted higher effect sizes (Table 5).
Table 5. Moderator analyses and mean cognitive effect sizes in the mixed-effects model.
| Total | Healthy | Cognitive impairments | Moderator? | ||||
|---|---|---|---|---|---|---|---|
| Total group | Healthy only (post-hoc) | Cognitive impairments only (post-hoc) | |||||
| Group | No† | No† | No† | ||||
| Healthy | d = 0.26** [0.15, 0.37] |
- | - | ||||
| Cognitive impairments | d = 0.22* [0.05, 0.39] |
- | - | ||||
| Cognitive domain | No† | No† | No† | ||||
| Global cognition | d = 0.31** [0.14, 0.49] |
d = 0.17 [-0.13, 0.46] |
d = 0.37** [0.15, 0.60] |
||||
| Executive function | d = 0.25** [0.14, 0.36] |
d = 0.27** [0.15, 0.40] |
d = 0.16 [-0.11, 0.43] |
||||
| Memory | d = 0.19** [0.05, 0,.32] |
d = 0.24** [0.06, 0.41] |
d = 0.09 [-0.11, 0.29] |
||||
| Exercise type | No† | No† | No† | ||||
| Aerobic | d = 0.20** [0.05, 0.35] |
d = 0.22* [0.03, 0.41] |
d = 0.22 [-0.20, 0.64] |
||||
| Anaerobic | d = 0.26** [0.09, 0.42] |
d = 0.27** [0.09, 0.46] |
d = 0.22 [-0.20, 0.64] |
||||
| Multicomponent | d = 0.32** [0.12, 0.53] |
d = 0.30 [-0.01, 0.60] |
d = 0.36* [0.04, 0.68] |
||||
| Psychomotor | d = 0.28 [-0.20, 0,76] |
d = 0.29 [-0.21, 0.78] |
n/a | ||||
| Program duration (weeks) | No† | No† | No† | ||||
| Short (4–12) | d = 0.33** [0.18, 0.48] |
d = 0.36** [0.17, 0.54] |
d = 0.29 [-0.01, 0.58] |
||||
| Moderate (13–24) | d = 0.21** [0.07, 0.35] |
d = 0.14 [-0.04, 0.32] |
d = 0.34 [0.05, 0.53] |
||||
| Long (≥24) | d = 0.17* [0.01, 0.34] |
d = 0.29* [0.06, 0.52] |
d = 0.10 [-0.16, 0.36] |
||||
| Session duration (minutes) | Yes: F(2,51) = 5.756, p≤0.01** | ||||||
| Short (≤30) | d = 0.33** [0.14, 0.53] |
d = 0.22 [-0.03, 0.47] |
d = 0.43 [0.24, 0.62] |
β = 0.38, 95%CI [0.15, 0.60]** | |||
| Moderate (31–45) | d = 0.14 [-0.11, 0.38] |
d = 0.11 [-0.16, 0.38] |
d = 0.28 [-0.26, 0.82] |
β = 0.23, 95%CI [-0.33, 0.78] | |||
| Long (≥45) | d = 0.24** [0.12, 0.36] |
d = 0.31** [0.16, 0.45] |
d = 0.05 [-0.07, 0.17] |
Reference | |||
| Frequency (#week) | No† | No† | Yes: F(2,51) = 3.589, p≤0.05* | ||||
| 1/week | d = 0.32 [-0.03, 0.68] |
d = 0.23 [-0.17, 0.63] |
n/a | n/a | |||
| 2/week | d = 0.18* [0.01, 0.36] |
d = 0.34* [0.07, 0.62] |
d = 0.05 [-0.15, 0.26] |
Reference | |||
| 3/week | d = 0.25** [0.13, 0.37] |
d = 0.23** [0.09, 0.37] |
d = 0.35* [0.04, 0.66] |
β = 0.22, 95%CI [-0.16, 0.61] | |||
| ≥4/week | d = 0.51** [0.24, 0.78] |
d = 0.41 [-0.19, 1.00] |
d = 0.50** [0.24, 0.76] |
β = 0.42, 95%CI [0.06, 0.78]* | |||
| Total exercise duration (minutes) | β = 0.00 [-0.00, 0.00] |
β = 0.00 [-0.00, 0.00] |
β = -0.00 [-0.00, 0.00] |
No† | No† | No† | |
| Intensity | |||||||
| Aerobic exercise | Low intensity 30–50b |
d = 0.52* [0.09, 0.95] |
d = 0.65c [-0.32, 1.62] |
d = 0.42 [-0.10, 0.93] |
No† | No† | No† |
| Moderate intensity 51–80b |
d = 0.20** [0.06, 0.34] |
d = 0.25** [0.07, 0.43] |
d = 0.06 [-0.12, 0.24] |
||||
| High intensity 81–100b |
d = -0.30 [-0.92, 0.32] |
d = -0.30 [-0.94, 0.34] |
- | ||||
| Anaerobic exercise | Low intensity Tertile 1 (i≤1260a) |
d = 0.13* [0.02, 0.24] |
d = 0.19 [-0.01, 0.40] |
d = 0.14 [-0.03, 0.31] |
No† | No† | No† |
| Moderate intensity Tertile 2 (i = 1261–1800a) |
d = 0.33* [0.03, 0.63] |
d = 0.33 [-0.03, 0.69] |
- | ||||
| High intensity Tertile 3 (i≥1800a) |
d = 0.23** [0.07, 0.40] |
d = 0.24* [0.03, 0.44] |
- | ||||
| Multicomponent exercise | Low intensity Tertile 1 (i≤63a) |
d = 0.47 [-0.32, 1.26] |
d = 0.03 [-1.77, 1.84] |
d = 1.02 [-0.35, 2.39]c |
No† | No† | No† |
| Moderate intensity Tertile 2 (i = 64–610a) |
d = 0.22 [-0.30, 0.74] |
d = 0.24 [-1.57, 2.04] |
d = 0.21 [-0.47, 0.89] |
||||
| High intensity Tertile 3 (i≥611a) |
d = 0.47 [-0.17, 1.10] |
d = 0.49 [-0.80, 1.79] |
d = 0.42 [-0.80, 1.64] |
||||
| Psychomotor exercise | Low intensity 30–50b |
d = 0.29 [-0.32, 0.90] |
d = 0.29 [-0.32, 0.90] |
- | No† | No† | No† |
| Moderate intensity 51–80b |
- | - | - | ||||
| High intensity 81–100b |
- | - | - | ||||
aArbitrary unit.
b%HRR/HRmax/VO2max.
cN = 1.
*significant from 0 at p≤0.05;
**significant from 0 at p≤0.01.
†p-value >0.05, see text and S6 Table for details.
Discussion
Summary of results
We examined the dose-response relationship between a broad sampling of exercises and cognitive function in older adults with and without cognitive impairments. In healthy older adults, there was a small positive effect of exercise on executive function and memory, but not global cognition. In older adults with cognitive impairments, exercise had a moderate positive effect on global cognition, but not executive function or memory. For healthy older adults, there were no significant dose-predictors of cognitive effect sizes. For older adults with cognitive impairments only, programs with shorter sessions and higher frequencies predicted higher cognitive effect sizes.
Relationship between exercise dose and cognition in healthy older adults
Although exercise carried some beneficial effects for executive function (d = 0.25) and memory (d = 0.24) in healthy older adults, these effects were small and not dose-dependent. The finding that exercise was positively related to executive function and memory in healthy older adults is in line with previous studies in healthy older populations [87–89]. Beneficial effects of exercise on executive function and memory may be fueled by exercise-induced increases in functional connectivity [90], up-regulation of BDNF [89], neocortical modifications [87], and increases in predominantly left hippocampal volume (see [91] for a review). Because optimal executive function and memory are a prerequisite for performing ADLs, the data supports current recommendations for an active lifestyle throughout old age [36].
We found lower exercise effects on cognition in healthy older adults (d = 0.17–0.27) compared with other reviews [33,92], which could be due to the inclusion of only studies that specified all dose-parameters including intensity. Indeed, Northey et al. [33] showed a lower mean cognitive effect when only studies that specified exercise intensity were included in the analysis (d = 0.10–0.16) vs. when all studies were included (d = 0.09–0.69). It is possible that studies that specify dose-parameters are better controlled, yielding smaller effects [93]. This speculation is supported by the small inverse correlation (r = -0.200) between study quality and effect size in our review.
Contrary to meta-analyses showing beneficial effects of longer program duration and higher exercise intensity on physical fitness-parameters [16–18], program duration and intensity did not predict cognitive effects in our review. The finding that longer program duration was not predictive of more cognitive effects is in line with Northey et al. [33]. Although changes in physical fitness-parameters may predict brain plasticity changes, these may not always translate to cognitive benefits [28]. A threshold at which cognitive changes occur is yet to be defined by future studies and can help determine the optimal exercise dose for cognitive improvements. With regards to program duration, the majority of studies in our review reported interventions ≤6 months, and only 3 interventions lasted >6 (i.e., 12) months. Possibly, 6–12 months of exercise is not enough to elicit detectable cognitive effects, considering that early signs of neurodegeneration may emerge in many healthily aging individuals [94]. A lack of intensity effects may stem from heterogeneity sources between the included studies. Some forms of training might be more efficacious than others for physical and cognitive benefits, even when performed at equivalent intensities. For example, walking may be more efficacious than (stationary) cycling at the same intensity, as walking involves the transport of body mass, increasing muscle energy expenditure [95]. Consequently, variation in types of training within exercise categories may have confounded intensity effects. Furthermore, there were differences in intensity measures between studies. For example, aerobic intensity could either be reported in %HRmax, %HRR or %VO2max and we were unable to differentiate between them when calculating the dose-coefficients. This may have inflated the variance in intensity-coefficients. Heterogeneity sources may also have confounded relationships between total dose and the other dose-parameters with cognition. Differences in inclusion criteria yielded variations in the baseline levels of physical activity (PA) of the participants: in four studies [49,51,52,82] only sedentary participants were included, whereas the other studies did not focus on sedentary adults (only). A generally low level of PA has previously been linked to suboptimal cognitive function [96,97]. Participants with lower levels of physical activity may show greater responsiveness to exercise. As PA baseline differences were unaccounted for in the current analyses, they may have confounded a potential dose-response relationship. In addition, differences in cognitive measures may greatly influence the magnitude of the effect. The relationship between exercise dose-parameters and cognitive effects may strongly rely upon the cognitive task difficulty [29,98]. In the current review, we grouped the cognitive tests in three domains: global cognition, executive function, and memory. This may have inflated the variance in effect sizes, potentially diminishing a dose-response relationship between exercise and cognition. To conclude, it is conceivable that the many sources of heterogeneity in the current sample prevented the discovery of an exercise dose-effect on cognition in healthy older adults.
Dose-response association between exercise and cognition in older populations with cognitive impairments
In older adults with cognitive impairments, exercise had a significant but small positive effect on global cognition (d = 0.37). The effect of exercise on global cognition appeared to stem predominantly from multicomponent training programs. There are a few reasons why multicomponent exercise may be more beneficial than single-modality training. Aerobic and resistance training each may be associated with favorable changes in neurobiological mechanisms (e.g., BDNF, IGF-1, VEGF, homocysteine) [3,5,11,99]. Such changes likely complement each other when aerobic and resistance exercises are performed simultaneously. Also, adding resistance exercise to aerobic training may enhance the neuromotor training stimulus, thereby enhancing cognitive benefits. There is some evidence that adding a balance component to aerobic and strength exercise could result in greater EF and visuospatial ability improvements [100].
Shorter session duration and higher frequency predicted greater cognitive effects. Short sessions may induce less fatigue, which can positively impact the ability and motivation to exercise. High session frequency may decrease overall sedentary time and stabilize levels of exercise-induced neurobiological factors, thereby improving neurocognitive health. However, the relationships between exercise-induced neurobiological mechanisms and dose-parameters are yet to be elucidated in future studies. Last, low session duration and high frequency were mainly evident in shorter programs. This attests for a significant confounding role of life-events during longer exercise programs for patients with cognitive impairments. Additionally, dementia decline may become more pronounced in longer programs. Although a short-term exercise program with low session duration and high frequency may convince patients of the beneficial effects of exercise, it is unlikely that initial effects persist after an intervention. Structural embedding of exercise may be necessary to maintain cognitive function in patients with cognitive impairments. The absence of a relationship between total exercise duration and cognition likely results from a counterbalancing effect between short session duration and higher frequency.
In older adults with cognitive impairments especially, there is a paucity of data concerning exercise dose-parameters and effects on cognitive function. In the current review, only one study compared different exercise doses (lower (40%HRR) vs. higher (60%HRR) intensity cycling) on cognitive function [83]. A lack of intensity effects in the present review could be explained by additional sources of heterogeneity discussed for healthy older adults. First, there were fewer studies in older adults with cognitive impairments. Second, although there was less variation in the cognitive tests used, cognitive test performance variation is generally larger in this population. Thus, the cognitive measures remain a source of large heterogeneity. Third, activities pursued by the control group may affect effect size. Control group activities may be beneficial to cognition for participants who are at high risk of cognitive decline [101]. Future research should investigate whether physical activity is preferable to other activities in improving cognition in older patients with cognitive impairments.
Limitations
The statistical power of the current analyses is limited by the high level of heterogeneity between studies, dependencies between studies that reported on the same samples, multiple testing and the relative low number of studies in each model. Current results should be carefully interpreted in light of potential type I error inflation, especially when taking into account the additional possible effect due to multiple comparisons. It must be noted that, while significant (d = 0.25–0.37, p<0.05), the small exercise effects on cognition may be of limited clinical relevance. We are uncertain how much change on our composite cognitive domains reflects a clinically relevant change, as we lack observational data linking cognitive changes to health outcomes in our review. Another important limitation is the unclear weighting with which each exercise parameter contributes to the exercise effects and a possible dose-response relationship. We weighted the parameters program duration, session duration, frequency and intensity equally in the determination of exercise dose. However, evidence for such an assumption is lacking because there are no studies that examined the unique contribution of each exercise parameter in isolation. We also assumed that if dose-parameters were not specified in a paper, that the specific range of dose-parameters was not recorded during a trial. It is possible that we have wrongfully excluded some studies because of this assumption. In addition, we cannot confirm the linear or inverted U-shape of the dose-response relationships between exercise and cognition. Furthermore, in the current review, we only included studies where the exact range of dose-parameters was specified. Consequently, we excluded several studies where dose-parameters gradually increased. However, it must be noted that the American College of Sports Medicine [36] specifically encourages a gradual increase of exercise dose-parameters for vulnerable older individuals. Last, the cognitively impaired older groups consisted of older adults with dementia (n = 5 studies), (probable) MCI (n = 6; n = 1 specified as amnestic MCI), VCI (n = 1) or ‘persons with cognitive impairments’ (n = 1). S7 Table shows the verification methods for cognitive status. From a clinical perspective, these syndrome groups are different and we acknowledge the heterogeneity that results from categorizing these subjects as ‘older adults with cognitive impairments’. With respect to MCI, only one study classified subjects with specifically amnestic MCI. There may be differences in brain structure and cognitive function between patients with amnestic vs. non-amnestic MCI [102]. Consequently, exercise may have differential effects on cognition in patients with amnestic vs. non-amnestic MCI, but we were unable to account for such differentiation. In addition, from a clinical perspective, it is valuable to know whether the dose-response relationship between exercise and cognition is different for different syndromes and grades of cognitive pathology. Unfortunately, there are currently not enough studies to provide such information.
Recommendations for future research
The shortage of studies (six for healthy older adults, one with older adults with cognitive impairments) that compare effects of different exercise doses illustrates the need for within-study variations in dose-parameters, e.g., comparing different exercise doses directly among randomized subjects or conditions allows for a better fit between exercise and its functional benefits for every participant. In addition, the main sources of heterogeneity in the included studies are the types of exercise, research methods, target populations, and cognitive tests. To improve comparison between studies, future studies could reduce such sources of heterogeneity by collecting and reporting as many program-related characteristics as possible, such as a detailed description of the protocol and measures of adherence and compliance.
Conclusion
The current review cannot confirm nor can reject previously established guidelines on the optimal exercise dose and intensity for healthy older adults. Adhering to these guidelines, older adults should perform a combination of aerobic and anaerobic exercises, of moderate intensity, for at least three times per week, on as many days of the week as feasible [36]. For older adults with cognitive impairments, programs with shorter session duration and higher frequency may generate the best cognitive results. For lasting effects it is recommended to structurally embed exercise in daily life. Health professionals are advised to tailor exercise prescriptions to each individual, as to maximize conformity to exercise programs and ensure long-lasting benefits.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability
The data available from our Open Science Framework project, URL: https://osf.io/qe43p/.
Funding Statement
The current study was supported by the Deltaplan Dementia (LS, TH, EvdZ, MvH: ZonMW, Dutch Ministry of Health: Memorabel, project number 733050303, received by TH, EvdZ, MvH, url: https://www.zonmw.nl/nl/over-zonmw/ehealth-en-ict-in-de-zorg/programmas/project-detail/memorabel/train-the-sedentary-brain-move-smart-to-reduce-the-risk-of-dementia/), University of Groningen (all authors, url: https://www.rug.nl/?lang=en) and the University Medical Center Groningen (LS, TH, SlBvG, MvH, url: https://www.umcg.nl/EN/corporate/Paginas/default.aspx). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Dementia. 2017. Available at: http://www.who.int/mediacentre/factsheets/fs362/en/. Accessed June 18, 2018.
- 2.Cummings J, Aisen PS, DuBois B, Frolich L, Jack CR Jr, Jones RW, et al. Drug development in Alzheimer’s disease: the path to 2025. Alzheimers Res Ther 2016. September 20;8:39-016-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rasmussen P, Brassard P, Adser H, Pedersen MV, Leick L, Hart E, et al. Evidence for a release of brain-derived neurotrophic factor from the brain during exercise. Exp Physiol 2009. October;94(10):1062–1069. 10.1113/expphysiol.2009.048512 [DOI] [PubMed] [Google Scholar]
- 4.Enette L, Vogel T, Fanon JL, Lang PO. Effect of Interval and Continuous Aerobic Training on Basal Serum and Plasma Brain-Derived Neurotrophic Factor Values in Seniors: A Systematic Review of Intervention Studies. Rejuvenation Res 2017. June 28. [DOI] [PubMed] [Google Scholar]
- 5.Cassilhas RC, Viana VA, Grassmann V, Santos RT, Santos RF, Tufik S, et al. The impact of resistance exercise on the cognitive function of the elderly. Med Sci Sports Exerc 2007. August;39(8):1401–1407. 10.1249/mss.0b013e318060111f [DOI] [PubMed] [Google Scholar]
- 6.Schwarz AJ, Brasel JA, Hintz RL, Mohan S, Cooper DM. Acute effect of brief low- and high-intensity exercise on circulating insulin-like growth factor (IGF) I, II, and IGF-binding protein-3 and its proteolysis in young healthy men. J Clin Endocrinol Metab 1996. October;81(10):3492–3497. 10.1210/jcem.81.10.8855791 [DOI] [PubMed] [Google Scholar]
- 7.Erickson KI, Prakash RS, Voss MW, Chaddock L, Hu L, Morris KS, et al. Aerobic fitness is associated with hippocampal volume in elderly humans. Hippocampus 2009. October;19(10):1030–1039. 10.1002/hipo.20547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maass A, Duzel S, Brigadski T, Goerke M, Becke A, Sobieray U, et al. Relationships of peripheral IGF-1, VEGF and BDNF levels to exercise-related changes in memory, hippocampal perfusion and volumes in older adults. Neuroimage 2016. May 1;131:142–154. 10.1016/j.neuroimage.2015.10.084 [DOI] [PubMed] [Google Scholar]
- 9.Colcombe SJ, Erickson KI, Scalf PE, Kim JS, Prakash R, McAuley E, et al. Aerobic exercise training increases brain volume in aging humans. The journals of gerontology. Series A, Biological sciences and medical sciences 2006;61(11):1166–1170. [DOI] [PubMed] [Google Scholar]
- 10.Gomez-Pinilla F, Hillman C. The influence of exercise on cognitive abilities. Compr Physiol 2013. January;3(1):403–428. 10.1002/cphy.c110063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Voss MW, Erickson KI, Prakash RS, Chaddock L, Kim JS, Alves H, et al. Neurobiological markers of exercise-related brain plasticity in older adults. Brain Behav Immun 2013. February;28:90–99. 10.1016/j.bbi.2012.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci 2003;14(2):125–130. 10.1111/1467-9280.t01-1-01430 [DOI] [PubMed] [Google Scholar]
- 13.Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S. Exercise programs for people with dementia. Cochrane Database Syst Rev 2015. April 15;4:CD006489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. What is moderate-intensity and vigorous-intensity physical activity? 2017, Available at: http://www.who.int/dietphysicalactivity/physical_activity_intensity/en/.
- 15.Powers S.K. & Howley E.T. Exercise physiology: Theory and application to fitness and performance. New York: McGraw-Hill Humanities/Social Sciences/Languages; 2011. [Google Scholar]
- 16.Borde R, Hortobagyi T, Granacher U. Dose-Response Relationships of Resistance Training in Healthy Old Adults: A Systematic Review and Meta-Analysis. Sports Med 2015. December;45(12):1693–1720. 10.1007/s40279-015-0385-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silva NL, Oliveira RB, Fleck SJ, Leon AC, Farinatti P. Influence of strength training variables on strength gains in adults over 55 years-old: a meta-analysis of dose-response relationships. J Sci Med Sport 2014. May;17(3):337–344. 10.1016/j.jsams.2013.05.009 [DOI] [PubMed] [Google Scholar]
- 18.Oja P, Kelly P, Murtagh EM, Murphy MH, Foster C, Titze S. Effects of frequency, intensity, duration and volume of walking interventions on CVD risk factors: a systematic review and meta-regression analysis of randomised controlled trials among inactive healthy adults. Br J Sports Med 2018. June;52(12):769–775. 10.1136/bjsports-2017-098558 [DOI] [PubMed] [Google Scholar]
- 19.Blankevoort CG, van Heuvelen MJ, Boersma F, Luning H, de Jong J, Scherder EJ. Review of effects of physical activity on strength, balance, mobility and ADL performance in elderly subjects with dementia. Dement Geriatr Cogn Disord 2010;30(5):392–402. 10.1159/000321357 [DOI] [PubMed] [Google Scholar]
- 20.MacInnis MJ, Gibala MJ. Physiological adaptations to interval training and the role of exercise intensity. J Physiol 2017. May 1;595(9):2915–2930. 10.1113/JP273196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foulds HJ, Bredin SS, Charlesworth SA, Ivey AC, Warburton DE. Exercise volume and intensity: a dose-response relationship with health benefits. Eur J Appl Physiol 2014. August;114(8):1563–1571. 10.1007/s00421-014-2887-9 [DOI] [PubMed] [Google Scholar]
- 22.Nemoto K, Gen-no H, Masuki S, Okazaki K, Nose H. Effects of high-intensity interval walking training on physical fitness and blood pressure in middle-aged and older people. Mayo Clin Proc 2007. July;82(7):803–811. [DOI] [PubMed] [Google Scholar]
- 23.Adamson SB, Lorimer R, Cobley JN, Babraj JA. Extremely short-duration high-intensity training substantially improves the physical function and self-reported health status of elderly adults. J Am Geriatr Soc 2014. July;62(7):1380–1381. 10.1111/jgs.12916 [DOI] [PubMed] [Google Scholar]
- 24.Etman A, Pierik FH, Kamphuis CB, Burdorf A, van Lenthe FJ. The role of high-intensity physical exercise in the prevention of disability among community-dwelling older people. BMC Geriatr 2016. November 9;16(1):183 10.1186/s12877-016-0334-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schnohr P, Marott JL, Jensen JS, Jensen GB. Intensity versus duration of cycling, impact on all-cause and coronary heart disease mortality: the Copenhagen City Heart Study. Eur J Prev Cardiol 2012. February;19(1):73–80. 10.1177/1741826710393196 [DOI] [PubMed] [Google Scholar]
- 26.Prakash RS, Voss MW, Erickson KI, Lewis JM, Chaddock L, Malkowski E, et al. Cardiorespiratory fitness and attentional control in the aging brain. Front Hum Neurosci 2011. January 14;4:229 10.3389/fnhum.2010.00229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong CN, Chaddock-Heyman L, Voss MW, Burzynska AZ, Basak C, Erickson KI, et al. Brain activation during dual-task processing is associated with cardiorespiratory fitness and performance in older adults. Front Aging Neurosci 2015. August 12;7:154 10.3389/fnagi.2015.00154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pensel MC, Daamen M, Scheef L, Knigge HU, Rojas Vega S, Martin JA, et al. Executive control processes are associated with individual fitness outcomes following regular exercise training: blood lactate profile curves and neuroimaging findings. Sci Rep 2018. March 20;8(1):4893-018-23308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chang YK, Etnier JL. Exploring the dose-response relationship between resistance exercise intensity and cognitive function. J Sport Exerc Psychol 2009. October;31(5):640–656. [DOI] [PubMed] [Google Scholar]
- 30.Chang YK, Chu CH, Wang CC, Wang YC, Song TF, Tsai CL, et al. Dose-response relation between exercise duration and cognition. Med Sci Sports Exerc 2015. January;47(1):159–165. 10.1249/MSS.0000000000000383 [DOI] [PubMed] [Google Scholar]
- 31.Kamijo K, Hayashi Y, Sakai T, Yahiro T, Tanaka K, Nishihira Y. Acute effects of aerobic exercise on cognitive function in older adults. J Gerontol B Psychol Sci Soc Sci 2009. May;64(3):356–363. 10.1093/geronb/gbp030 [DOI] [PubMed] [Google Scholar]
- 32.Tomporowski PD. Effects of acute bouts of exercise on cognition. Acta Psychol (Amst) 2003. March;112(3):297–324. [DOI] [PubMed] [Google Scholar]
- 33.Northey JM, Cherbuin N, Pumpa KL, Smee DJ, Rattray B. Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. Br J Sports Med 2017. April 24. [DOI] [PubMed] [Google Scholar]
- 34.Groot C, Hooghiemstra AM, Raijmakers PG, van Berckel BN, Scheltens P, Scherder EJ, et al. The effect of physical activity on cognitive function in patients with dementia: A meta-analysis of randomized control trials. Ageing Res Rev 2016. January;25:13–23. 10.1016/j.arr.2015.11.005 [DOI] [PubMed] [Google Scholar]
- 35.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009. July 21;6(7):e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- 37.Borg G. Borg’s Perceived exertion and pain scales. Champaign, IL: Human Kinetics; 1998. [Google Scholar]
- 38.Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. New York, NY: Academic Press; 1985. [Google Scholar]
- 39.Nakagawa S, Cuthill IC. Effect size, confidence interval and statistical significance: a practical guide for biologists. Biol Rev Camb Philos Soc 2007. November;82(4):591–605. 10.1111/j.1469-185X.2007.00027.x [DOI] [PubMed] [Google Scholar]
- 40.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 41.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 2009;55(2):129–133. [DOI] [PubMed] [Google Scholar]
- 42.Lipsey M., & Wilson D. Practical meta-analysis. 2001; Thousand Oaks, CA: Sage. [Google Scholar]
- 43.Wilson DB. Meta-analysis macros for SAS, SPSS, and Stata. 2010. Retrieved on October 25, 2018, from http://mason.gmu.edu/~dwilsonb/ma.html.
- 44.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003. September 6;327(7414):557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Viechtbauer W. Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software 2010;36(3). [Google Scholar]
- 46.Van Rhee, H.J., Suurmond, R., & Hak, T. User manual for Meta-Essentials: Workbooks for meta-analysis (Version 1.0). 2015.
- 47.Hox J., De Leeuw E. Multilevel models for meta-analysis. Multilevel modeling: methodological advances, issues, and applications. 2003.
- 48.Wibbelink CJM, Assink M. Manual for conducting a three-level meta-analysis in R. Amsterdam: Universiteit van Amsterdam; 2015. [Google Scholar]
- 49.Albinet CT, Boucard G, Bouquet CA, Audiffren M. Increased heart rate variability and executive performance after aerobic training in the elderly. Eur J Appl Physiol 2010. July;109(4):617–624. 10.1007/s00421-010-1393-y [DOI] [PubMed] [Google Scholar]
- 50.Albinet CT, Abou-Dest A, Andre N, Audiffren M. Executive functions improvement following a 5-month aquaerobics program in older adults: Role of cardiac vagal control in inhibition performance. Biol Psychol 2016. March;115:69–77. 10.1016/j.biopsycho.2016.01.010 [DOI] [PubMed] [Google Scholar]
- 51.Ansai JH, Rebelatto JR. Effect of two physical exercise protocols on cognition and depressive symptoms in oldest-old people: A randomized controlled trial. Geriatr Gerontol Int 2015. September;15(9):1127–1134. 10.1111/ggi.12411 [DOI] [PubMed] [Google Scholar]
- 52.Baker LD, Frank LL, Foster-Schubert K, Green PS, Wilkinson CW, McTiernan A, et al. Effects of aerobic exercise on mild cognitive impairment: A controlled trial. Arch Neurol 2010;67(1):71–79. 10.1001/archneurol.2009.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Best JR, Chiu BK, Liang Hsu C, Nagamatsu LS, Liu-Ambrose T. Long-Term Effects of Resistance Exercise Training on Cognition and Brain Volume in Older Women: Results from a Randomized Controlled Trial. J Int Neuropsychol Soc 2015. November;21(10):745–756. 10.1017/S1355617715000673 [DOI] [PubMed] [Google Scholar]
- 54.Bossers WJ, van der Woude LH, Boersma F, Hortobagyi T, Scherder EJ, van Heuvelen MJ. A 9-Week Aerobic and Strength Training Program Improves Cognitive and Motor Function in Patients with Dementia: A Randomized, Controlled Trial. Am J Geriatr Psychiatry 2015. November;23(11):1106–1116. 10.1016/j.jagp.2014.12.191 [DOI] [PubMed] [Google Scholar]
- 55.Brinke LF, Bolandzadeh N, Nagamatsu LS, Hsu CL, Davis JC, Miran-Khan K, et al. Aerobic exercise increases hippocampal volume in older women with probable mild cognitive impairment: a 6-month randomised controlled trial. Br J Sports Med 2015;49(4):248–254. 10.1136/bjsports-2013-093184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coetsee C, Terblanche E. The effect of three different exercise training modalities on cognitive and physical function in a healthy older population. Eur Rev Aging Phys Act 2017. August 10;14:13-017-0183-5. eCollection 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dao E, Davis JC, Sharma D, Chan A, Nagamatsu LS, Liu-Ambrose T. Change in body fat mass is independently associated with executive functions in older women: a secondary analysis of a 12-month randomized controlled trial. PLoS One 2013;8(1):e52831 10.1371/journal.pone.0052831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Davis JC, Bryan S, Marra CA, Sharma D, Chan A, Beattie BL, et al. An Economic Evaluation of Resistance Training and Aerobic Training versus Balance and Toning Exercises in Older Adults with Mild Cognitive Impairment. PLoS ONE 2013;8(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.de Souto Barreto P, Cesari M, Denormandie P, Armaingaud D, Vellas B, Rolland Y. Exercise or Social Intervention for Nursing Home Residents with Dementia: A Pilot Randomized, Controlled Trial. J Am Geriatr Soc 2017. May 19. [DOI] [PubMed] [Google Scholar]
- 60.Fabre C, Chamari K, Mucci P, Masse-Biron J, Prefaut C. Improvement of cognitive function by mental and/or individualized aerobic training in healthy elderly subjects. Int J Sports Med 2002;23(6):415–421. 10.1055/s-2002-33735 [DOI] [PubMed] [Google Scholar]
- 61.Ferreira L, Tanaka K, Santosgalduróz RF, Galduróz JCF. Respiratory training as strategy to prevent cognitive decline in aging: A randomized controlled trial. Clin Interventions Aging 2015;10:593–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Iuliano E, di Cagno A, Aquino G, Fiorilli G, Mignogna P, Calcagno G, et al. Effects of different types of physical activity on the cognitive functions and attention in older people: A randomized controlled study. Exp Gerontol 2015. October;70:105–110. 10.1016/j.exger.2015.07.008 [DOI] [PubMed] [Google Scholar]
- 63.Jonasson LS, Nyberg L, Kramer AF, Lundquist A, Riklund K, Boraxbekk CJ. Aerobic Exercise Intervention, Cognitive Performance, and Brain Structure: Results from the Physical Influences on Brain in Aging (PHIBRA) Study. Front Aging Neurosci 2017. January 18;8:336 10.3389/fnagi.2016.00336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kemoun G, Thibaud M, Roumagne N, Carette P, Albinet C, Toussaint L, et al. Effects of a physical training programme on cognitive function and walking efficiency in elderly persons with dementia. Dement Geriatr Cogn Disord 2010;29(2):109–114. 10.1159/000272435 [DOI] [PubMed] [Google Scholar]
- 65.Kimura K, Obuchi S, Arai T, Nagasawa H, Shiba Y, Watanabe S, et al. The influence of short-term strength training on health-related quality of life and executive cognitive function. J Physiol Anthropol 2010;29(3):95–101. [DOI] [PubMed] [Google Scholar]
- 66.Kwak YS, Um SY, Son TG, Kim DJ. Effect of regular exercise on senile dementia patients. Int J Sports Med 2008. June;29(6):471–474. 10.1055/s-2007-964853 [DOI] [PubMed] [Google Scholar]
- 67.Liu-Ambrose T, Nagamatsu LS, Graf P, Beattie BL, Ashe MC, Handy TC. Resistance training and executive functions: A 12-month randomized controlled trial. Arch Intern Med 2010;170(2):170–178. 10.1001/archinternmed.2009.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu-Ambrose T, Nagamatsu LS, Voss MW, Khan KM, Handy TC. Resistance training and functional plasticity of the aging brain: A 12-month randomized controlled trial. Neurobiol Aging 2012;33(8):1690–1698. 10.1016/j.neurobiolaging.2011.05.010 [DOI] [PubMed] [Google Scholar]
- 69.Liu-Ambrose T, Best JR, Davis JC, Eng JJ, Lee PE, Jacova C, et al. Aerobic exercise and vascular cognitive impairment: A randomized controlled trial. Neurology 2016. November 15;87(20):2082–2090. 10.1212/WNL.0000000000003332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Maass A, Duzel S, Goerke M, Becke A, Sobieray U, Neumann K, et al. Vascular hippocampal plasticity after aerobic exercise in older adults. Mol Psychiatry 2015. May;20(5):585–593. 10.1038/mp.2014.114 [DOI] [PubMed] [Google Scholar]
- 71.Madden DJ, Blumenthal JA, Allen PA, Emery CF. Improving aerobic capacity in healthy older adults does not necessarily lead to improved cognitive performance. Psychol Aging 1989;4(3):307–320. [DOI] [PubMed] [Google Scholar]
- 72.Moreau D, Morrison AB, Conway AR. An ecological approach to cognitive enhancement: complex motor training. Acta Psychol (Amst) 2015. May;157:44–55. [DOI] [PubMed] [Google Scholar]
- 73.Muscari A, Giannoni C, Pierpaoli L, Berzigotti A, Maietta P, Foschi E, et al. Chronic endurance exercise training prevents aging-related cognitive decline in healthy older adults: a randomized controlled trial. Int J Geriatr Psychiatry 2010. October;25(10):1055–1064. 10.1002/gps.2462 [DOI] [PubMed] [Google Scholar]
- 74.Nagamatsu LS, Chan A, Davis JC, Beattie BL, Graf P, Voss MW. Physical activity improves verbal and spatial memory in older adults with probable mild cognitive impairment: a 6-month randomized controlled trial. Journal of aging research 2013;2013:Article Number: 861893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nouchi R, Taki Y, Takeuchi H, Sekiguchi A, Hashizume H, Nozawa T, et al. Four weeks of combination exercise training improved executive functions, episodic memory, and processing speed in healthy elderly people: evidence from a randomized controlled trial. Age (Dordr) 2014. April;36(2):787–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ruiz JR, Gil-Bea F, Bustamante-Ara N, Rodriguez-Romo G, Fiuza-Luces C, Serra-Rexach JA, et al. Resistance training does not have an effect on cognition or related serum biomarkers in nonagenarians: a randomized controlled trial. Int J Sports Med 2015. January;36(1):54–60. 10.1055/s-0034-1375693 [DOI] [PubMed] [Google Scholar]
- 77.Ruscheweyh R, Willemer C, Krueger K, Duning T, Warnecke T, Sommer J, et al. Physical activity and memory functions: An interventional study. Neurobiol Aging. 2011. July;32(7)1304–1319. 10.1016/j.neurobiolaging.2009.08.001 [DOI] [PubMed] [Google Scholar]
- 78.Shatil E. Does combined cognitive training and physical activity training enhance cognitive abilities more than either alone? A four-condition randomized controlled trial among healthy older adults. Front Aging Neurosci. 2013; 26(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Telenius EW, Engedal K, Bergland A. Long-term effects of a 12 weeks high-intensity functional exercise program on physical function and mental health in nursing home residents with dementia: a single blinded randomized controlled trial. BMC Geriatr 2015. December 3;15:158-015-0151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tsai C-, Wang C-, Pan C-, Chen F-. The effects of long-term resistance exercise on the relationship between neurocognitive performance and GH, IGF-1, and homocysteine levels in the elderly. Front Behav Neurosci 2015;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tsai CL, Pan CY, Chen FC, Tseng YT. Open- and Closed-Skill Exercise Interventions Produce Different Neurocognitive Effects on Executive Functions in the Elderly: A 6-Month Randomized, Controlled Trial. Front Aging Neurosci 2017. September 12;9:294 10.3389/fnagi.2017.00294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tsutsumi T, Don BM, Zaichkowsky LD, Delizonna LL. Physical fitness and psychological benefits of strength training in community dwelling older adults. Appl Human Sci 1997;16(6):257–266. [DOI] [PubMed] [Google Scholar]
- 83.Varela S, Ayan C, Cancela JM, Martin V. Effects of two different intensities of aerobic exercise on elderly people with mild cognitive impairment: a randomized pilot study. Clin Rehabil 2012. May;26(5):442–450. 10.1177/0269215511425835 [DOI] [PubMed] [Google Scholar]
- 84.Vedovelli K, Giacobbo BL, Correa MS, Wieck A, Argimon IIL, Bromberg E. Multimodal physical activity increases brain-derived neurotrophic factor levels and improves cognition in institutionalized older women. Geroscience 2017. July 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wei XH, Ji LL. Effect of handball training on cognitive ability in elderly with mild cognitive impairment. Neurosci Lett 2014;566:98–101. 10.1016/j.neulet.2014.02.035 [DOI] [PubMed] [Google Scholar]
- 86.Moreau D, Morrison AB, Conway AR. An ecological approach to cognitive enhancement: complex motor training. Acta Psychol (Amst) 2015. May;157:44–55. [DOI] [PubMed] [Google Scholar]
- 87.Dai CT, Chang YK, Huang CJ, Hung TM. Exercise mode and executive function in older adults: an ERP study of task-switching. Brain Cogn 2013. November;83(2):153–162. 10.1016/j.bandc.2013.07.007 [DOI] [PubMed] [Google Scholar]
- 88.Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci U S A 2011. February 15;108(7):3017–3022. 10.1073/pnas.1015950108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Leckie RL, Oberlin LE, Voss MW, Prakash RS, Szabo-Reed A, Chaddock-Heyman L, et al. BDNF mediates improvements in executive function following a 1-year exercise intervention. Frontiers in human neuroscience 2014;8(DEC). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Voss MW, Prakash RS, Erickson KI, Basak C, Chaddock L, Kim JS, et al. Plasticity of brain networks in a randomized intervention trial of exercise training in older adults. Front Aging Neurosci 2010. August 26;2: 10.3389/fnagi.2010.00032 eCollection 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Firth J, Stubbs B, Vancampfort D, Schuch F, Lagopoulos J, Rosenbaum S, et al. Effect of aerobic exercise on hippocampal volume in humans: A systematic review and meta-analysis. Neuroimage 2018. February 1;166:230–238. 10.1016/j.neuroimage.2017.11.007 [DOI] [PubMed] [Google Scholar]
- 92.Scherder E, Scherder R, Verburgh L, Konigs M, Blom M, Kramer AF, et al. Executive functions of sedentary elderly may benefit from walking: a systematic review and meta-analysis. Am J Geriatr Psychiatry 2014. August;22(8):782–791. 10.1016/j.jagp.2012.12.026 [DOI] [PubMed] [Google Scholar]
- 93.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273(5):408–412. [DOI] [PubMed] [Google Scholar]
- 94.Wyss-Coray T. Ageing, neurodegeneration and brain rejuvenation. Nature 2016. November 10;539(7628):180–186. 10.1038/nature20411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Umberger BR, Gerritsen KG, Martin PE. A model of human muscle energy expenditure. Comput Methods Biomech Biomed Engin 2003. April;6(2):99–111. 10.1080/1025584031000091678 [DOI] [PubMed] [Google Scholar]
- 96.Vaynman S, Gomez-Pinilla F. Revenge of the “Sit”: How lifestyle impacts neuronal and cognitive health through molecular systems that interface energy metabolism with neuronal plasticity. J Neurosci Res 2006. September/01;84(4):699–715. 10.1002/jnr.20979 [DOI] [PubMed] [Google Scholar]
- 97.Voss MW, Carr LJ, Clark R, Weng T. Revenge of the “sit” II: Does lifestyle impact neuronal and cognitive health through distinct mechanisms associated with sedentary behavior and physical activity? Mental Health and Physical Activity 2014. March/01;7(1):9–24. [Google Scholar]
- 98.Tempest GD, Davranche K, Brisswalter J, Perrey S, Radel R. The differential effects of prolonged exercise upon executive function and cerebral oxygenation. Brain Cogn 2017. April;113:133–141. 10.1016/j.bandc.2017.02.001 [DOI] [PubMed] [Google Scholar]
- 99.Vincent KR, Braith RW, Bottiglieri T, Vincent HK, Lowenthal DT. Homocysteine and lipoprotein levels following resistance training in older adults. Prev Cardiol 2003. Fall;6(4):197–203. [DOI] [PubMed] [Google Scholar]
- 100.Merom D, Grunseit A, Eramudugolla R, Jefferis B, Mcneill J, Anstey KJ. Cognitive benefits of social dancing and walking in old age: The dancing mind randomized controlled trial. Front Aging Neurosci 2016;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Krell-Roesch J, Vemuri P, Pink A, Roberts RO, Stokin GB, Mielke MM, et al. Association Between Mentally Stimulating Activities in Late Life and the Outcome of Incident Mild Cognitive Impairment, With an Analysis of the APOE epsilon4 Genotype. JAMA Neurol 2017. March 1;74(3):332–338. 10.1001/jamaneurol.2016.3822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Csukly G, Siraly E, Fodor Z, Horvath A, Salacz P, Hidasi Z, et al. The Differentiation of Amnestic Type MCI from the Non-Amnestic Types by Structural MRI. Front Aging Neurosci. 2016;8: 52 10.3389/fnagi.2016.00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
The data available from our Open Science Framework project, URL: https://osf.io/qe43p/.