Abstract
Objectives
Among autoimmune diseases, rheumatoid arthritis (RA) is the most common chronic inflammatory disease of the joints. Its pathogenesis is still not fully understood, but the gained knowledge has contributed to the development of modern treatment. The introduction of biological therapy for RA has been a breakthrough in the standard approach to the treatment of this disease.
Material and methods
The study material was retrospectively collected in the Rheumatology and Systemic Tissue Diseases Clinic and Rheumatology Outpatient Clinic in dr. Jan Biziel University Hospital No. 2 in Bydgoszcz. Patients were divided into 3 groups: patients receiving infliximab – 43 patients, etanercept – 27 patients and adalimumab – 34 patients. In the study, the pharmacoeconomic analysis included direct and indirect medical costs. Direct medical costs analyzed in the study included costs for the purchase of medications, diagnostic and imaging costs, and medical consultations and hospitalization costs. The analysis included all direct medical costs incurred by the hospital and the patient, as well as indirect costs outside the healthcare sector – that is, the Polish Social Insurance Institution benefits (disability benefits, rehabilitation benefits, sickness absences). Direct medical costs are also presented from the perspective of the payer – The Polish National Health Fund – taking into account the cost and percentage share of medical expenses.
Results
The analysis concerned resources used since the beginning of treatment with a given biological medication for 24 months or earlier if disease remission occurred.
A cost-benefit analysis was carried out in the study using biosimilar medications present on the market in relation to the treatment regimens. Considering the total cost, if only Inflectra were used in therapy, PLN 18 151.98 per patient could be saved, and in the case of Remsima, PLN 16 385.14. In less than 19 months, to use infliximab for 43 patients, PLN 780 475.80 more would have to be spent than in the case of the biosimilar medication Inflectra, and PLN 704 561 in the case of Remsima.
The highest total cost is generated by treatment with adalimumab, followed by etanercept, and infliximab. Of the costs analyzed, a significant majority was for biological treatment.
Conclusions
Given the Polish financial conditions, the best solution now is to reduce the prices of biological medications. This is possible through the introduction of biosimilar medications that, when placed on the market, reduce the price of the original medication, as is currently the case with Remicade and Enbrel. The introduction of Inflectra and Remsima, as well as Benepali and Erelzi, has reduced the price base of original medications to similar levels of treatment with biosimilar medications. The wider use of biological treatment would also reduce indirect costs.
Keywords: rheumatology, costs, rheumatoid arthritis, biological treatment
Introduction
Among autoimmune diseases, rheumatoid arthritis (RA) is the most common chronic inflammatory disease of the joints. Its pathogenesis is still not fully understood, but the gained knowledge has contributed to the development of modern treatment. The introduction of biological therapy for RA has been a breakthrough in the standard approach to the treatment of this disease. In most patients, their use in the treatment of RA results in a rapid therapeutic effect in the form of lowering disease activity and improving functional status.
The proven efficacy of biological therapy for RA should result in its widespread use. Nevertheless, in order to be able to implement such a solution, large financial expenditures are needed. The increasing costs of medical services, with still limited resources dedicated to healthcare, have made it necessary to make economic evaluations of health programs. Pharmacoeconomic analysis, by comparing the costs and outcomes of alternative therapies, provide a clear overview of available treatments. Their goal is to provide reliable, evidence-based information to help to decide on the best treatment regimen.
Material and methods
The study material was retrospectively collected in the Rheumatology and Systemic Tissue Diseases Clinic and Rheumatology Outpatient Clinic in dr. Jan Biziel University Hospital No. 2 in Bydgoszcz in the years 2009–2014. Data are based on the records of patients with rheumatoid arthritis diagnosed according to the 1987 ACR criteria, who were treated with etanercept, infliximab, and adalimumab. For the analysis, 104 patients were enrolled.
Patients were divided into 3 groups:
Patients taking infliximab (INF) formed a group of 43 persons (30 women and 13 men) aged 27 to 71 years (average age 47 years). At the time of initiation of biological therapy, men had RA for an average of 6.5 years, women for 9 years.
Patients taking etanercept (ETA) formed a group of 27 persons (24 women and 3 men) aged 20 to 60 years (average age 51 years). At the time of initiation of biological therapy, men had RA for an average of 13 years, women for 12 years.
Patients taking adalimumab (ADA) formed a group of 34 persons (23 women and 11 men) aged 25 to 77 years (average age 54 years). At the time of initiation of biological therapy, men had RA for an average of 4.5 years, women for 8 years.
Patients have received medications under the National Health Fund (Narodowy Fundusz Zdrowia – NFZ) therapeutic programs. Each patient had to meet the required inclusion and exclusion criteria as prescribed in the rules of the therapeutic program.
Laboratory tests upon enrollment in the program and at the monitoring visit were performed before treatment and in the period within 90 days (±14 days) after the first dose. Regardless of the chosen drug in therapy, the most commonly performed laboratory examinations were: determination of C-reactive protein concentration (CRP), erythrocyte sedimentation rate (ESR), blood morphology, creatinine, sodium, and potassium levels, and determination of liver enzyme activity – alanine aminotransferase (ALT) and aspartate aminotransferase (AST).
In the present study, the pharmacoeconomic analysis included direct and indirect medical costs. Direct medical costs included costs for the purchase of medications, diagnostic and imaging costs, medical consultations and hospitalization costs.
The costs of laboratory tests and imaging examinations and services provided by the hospital were obtained on the basis of the price list of the hospital’s medical services. Prices of biological medications were obtained from the hospital pharmacy in December 2014, while the prices of other medications were obtained from a public pharmacy. Prices of biosimilar medications (Benepali and Erelzi) were established on the basis of the lists of reimbursed medications as of November 1, 2017.
The indirect costs analyzed in the study included costs related to reduced productivity, such as disability benefits, rehabilitation benefits, and sickness absences. The obtained data came from the Polish Social Insurance Institution (ZUS), branches in Bydgoszcz, Toruń, and Chełmno. The consent to data processing, including information on benefits from ZUS, was obtained from 85 patients.
Results
The analysis included all direct medical costs incurred by the hospital and the patient, as well as indirect costs outside the healthcare sector – that is, ZUS benefits (disability benefits, rehabilitation benefits, and sickness absences). Direct medical costs are also presented from the perspective of the payer, NFZ, taking into account the cost and percentage share of medical expenses.
The analysis concerned resources used since the beginning of treatment with a given biological medication for 24 months or earlier if disease remission occurred.
Direct medical costs were calculated by summing up:
costs of diagnostic examinations,
hotel costs,
costs of medications: biological and accompanying treatment,
costs of medical consultation.
For the costs of biological medications, in the case of infliximab, the cost of the infusion fluids needed to prepare the medication has been added. The direct total medical costs are shown in Table I.
Table I.
Medical costs according to treatment regimen
| Costs source | Cost (PLN) | |||||
|---|---|---|---|---|---|---|
| Total | Average per patient | |||||
| Infliximab | Etanercept | Adalimumab | Infliximab | Etanercept | Adalimumab | |
| Diagnostic examinations | 67 347 | 28 718 | 20 391 | 1 566 | 1 063 | 599 |
| Hospitalization | 216 219 | – | – | 5 028 | – | – |
| Biological medications | 2 445 334 | 1 849 898 | 2 527 350 | 56 868 | 68 514 | 74 333 |
| Other medications (including DMARD and glucocorticosteroids) | 21 954 | 8 066 | 121 718 | 510 | 298 | 3 579 |
| Medical examinations | 12 480 | 80 704 | 101 337 | 290 | 2 989 | 2 980 |
| Total | 2 763 335 | 1 967 387 | 2 770 797 | 64 263 | 72 866 | 81 494 |
In all analyzed treatment regimens, the main factor that generates about 90% of total costs was the purchased biological medications.
A cost-benefit analysis was carried out in the study using biosimilar medications present on the market in relation to the treatment regimens. In Poland, there are currently two medications that have counterparts in the form of biosimilar medications, that is, infliximab (Remicade) – Inflektra and Remsima, and etanercept (Enbrel) – Benepali and Erelzi. The total cost of biological treatment also includes the cost of other biological medications, because in the event of intolerance, side effects, or lack of response to infliximab, patients are switched to another therapy: with etanercept, adalimumab, or rituximab. The simulation of using Inflectra instead of infliximab is shown in Table II.
Table II.
Comparison of infliximab treatment costs and presumed costs using Inflectra
| Treatment regimen | Price of the vial | Total cost (PLN) | |
|---|---|---|---|
| Total | Average per patient | ||
| Infliximab | 2 113 | 2 444 354 | 56 845 |
| Inflectra | 1 190 | 1 663 878 | 38 693 |
| Percentage difference (%) | 43.70 | 31.93 | 31.93 |
| Price difference | 923 | 780 475 | 18 151 |
Considering the total cost, if only Inflectra were used in therapy, PLN 18 151.98 per patient could be saved, and in the case of Remsima, PLN 16 385.14. In less than 19 months, to use infliximab for 43 patients, PLN 780 475.80 more would have to be spent than in the case of the biosimilar medication Inflectra, and PLN 704 561 in the case of Remsima.
In a similar way, computations are presented comparing etanercept with the biosimilar medications Benepali and Erelzi. The cost of infliximab treatment also includes the cost of medications used in the case of intolerance, side effects, or lack of response to treatment. For both medications (Infliximab and Remsima), the cost of the infusion fluids needed to prepare them should be added.
Because Inflectra and Remsima were introduced to the Polish market in 2014, there are no long-term data on tolerability and adverse events. For this reason, the above calculations are estimated.
An analysis of indirect costs generated outside the healthcare sector was conducted, related to reduced patient productivity – ZUS benefits (disability benefits, rehabilitation benefits, and sickness absences). The analysis included the patient’s follow-up period in the study until the remission of the disease, or for a period of 24 months.
Approvals were obtained from 85 patients (27 from the adalimumab group, 21 from the etanercept group, 37 from the infliximab group) for the processing of personal data, including data on ZUS benefits. A general summary of the number of people generating indirect costs is presented in Table III.
Table III.
General summary of the number of people who generate indirect costs taking into account age, according to the treatment regimen
| Infliximab | Etanercept | Adalimumab | |
|---|---|---|---|
| Disability pension | 6 | 3 | 6 |
| Pension | 6 | 5 | 6 |
| Survivor's pension | 1 | 2 | 2 |
| Social pension | 1 | 0 | 0 |
| Age range | 27–71 | 20–60 | 25–77 |
| Age average | 47 | 51 | 54 |
According to the data obtained from ZUS, the highest indirect costs per patient were generated by the adalimumab treatment group. Patients receiving infliximab and etanercept had lower values of ZUS benefits.
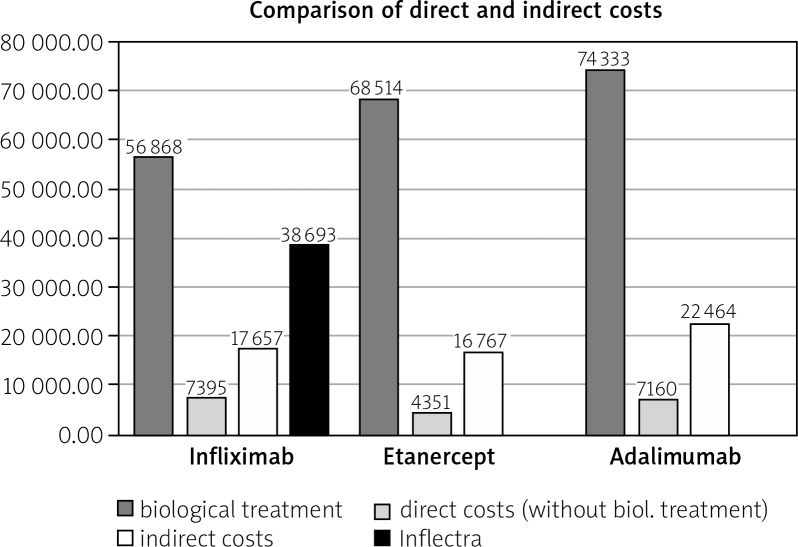
Total costs include both direct and indirect costs related to biological treatment. Figure 1 shows the share of total costs taking into account the cost of a biosimilar medication (Inflectra). The percentage share of individual costs is shown in Table IV.
Fig. 1.
Share of total costs according to the treatment regimen per patient (Remsima costs are similar to Inflectra costs).
Table IV.
Percentage share of individual costs according to treatment regimen per patient
| Infliximab | Etanercept | Adalimumab | |
|---|---|---|---|
| Total costs | 81 921 | 89 633 | 103 958 |
| Costs of biological treatment (%) | 69.41 | 76.44 | 71.50 |
| Indirect costs (%) | 21.56 | 18.71 | 21.61 |
| Other direct costs (%) | 9.03 | 4.85 | 6.89 |
The highest total cost is generated by treatment with adalimumab, followed by etanercept, and infliximab. Of the costs analyzed, a significant majority was for biological treatment. On average, the amount needed to be spent per patient ranges from PLN 56 868.24 in the case of infliximab to PLN 74 333.82 in the case of adalimumab. These amounts account for around 70% of total costs. Indirect costs range from PLN 16 767.43 for etanercept to PLN 22 464.49 for adalimumab and represent a percentage that fluctuates within 22% of the total value. Only in the case of etanercept does this value drop to about 19%.
The study compares 3 biological therapies used in the therapeutic health program reimbursed by NFZ: infliximab, etanercept, and adalimumab. Pharmacoeconomic analysis has been carried out to provide a full picture of costs. The study covered both direct and indirect costs. The juxtaposition of all direct costs has shown that the most cost-effective therapy is infliximab treatment. This also applies to total costs per patient.
Discussion
The RA morbidity in Europe and North America is 0.5–1% of the population [1]. Modern treatment of RA requires not only huge medical knowledge, but also great clinical experience. Current, standardized therapy with disease-modifying antirheumatic drugs (DMARDs) does not allow for low disease activity or remission in all patients. The alternative is the use of biological therapy. In Poland, about 1% of RA patients have access to up-to-date treatment [2]. Patients are included in the therapeutic program implemented by the NFZ. The NFZ budget for biological treatment, although increasingly large, does not provide access for most patients who need biological treatment. The situation in other countries of Central and Eastern Europe is quite different (Table V).
Table V.
Comparison of number of patients (%) with RA on biological treatment in different European countries taking into account the estimated population of patients [8]
| Country | Population of the country | Population of the patients (0.5–1%) | Number of patients treated | Percent of treated population of patients |
|---|---|---|---|---|
| Poland | 38 540 000 | 192 700–385 400 | 2569 | 1.33–0.66 |
| Czech Rep. | 10 512 782 | 52 564–105 128 | 2295 | 4.36–2.18 |
| Sweden | 9 500 000 | 47 500–95 000 | 10 816 | 22.76–11.38 |
| Germany | 80 327 900 | 401 640–803 280 | 80 965 | 20.16–10.08 |
| Italy | 59 520 464 | 297 602–595 204 | 37 407 | 12.56–6.28 |
| Spain | 47 265 321 | 236 325–472 650 | 44 363 | 18.76–9.38 |
| England | 53 012 000 | 265 060–530 120 | 60 783 | 22.92–11.46 |
| France | 65 800 000 | 329 000–658 000 | 19 907 | 6.04–3.02 |
Considering the rising costs and needs for other healthcare services, it seems doubtful to allocate sufficient funds to cover the current need for biological treatment. Patients whose standard DMARD treatment does not produce adequate results and does not slow the progress of the disease are forced to use disability pension or sickness absence, whereas a well-timed diagnosis combined with rapid and effective implementation of biological therapy provides a significant reduction in the activity of the disease and even the occurrence of remission and thus the return of the patient to full professional activity [3].
According to available sources, indirect costs, both within and outside the health service sector, are several times higher than direct costs associated with the treatment of RA [4]. According to the analysis, increased spending on biological treatment would significantly reduce expenditure in the indirect costs sector [5]. This does not mean, however, that savings should not be sought in the case of direct costs. A number of sources and own research confirm that approximately 90% of the expenditure associated with the use of biological therapy is the cost of purchasing the medications themselves [4, 6, 7].
Despite many publications indicating that the introduction of more widely available biological therapy would result in higher GDP values due to the professional activity of the patients, NFZ continues to allocate too low funds for this purpose [9–11].The conclusions drawn from the analysis of the organization of the rheumatological system mainly focus on the poor treatment of young people with RA, refraining from attempts to maintain the occupational activity of RA patients and incurring increasingly higher costs of development of motor disability in patients before the age of 65 [12].
Unfortunately, in Poland, there is still a lack of a well-organized healthcare system and cooperation among decision makers. The situation in the field of healthcare is constantly changing. However, even if on the level of the assumptions and priorities the new solutions are evaluated positively, in reality there is a real problem with their effectiveness. Therefore, the decision to introduce an appropriate therapy should be preceded by extensive pharmacoeconomic analysis. In this study, both direct and indirect costs were calculated for 3 biological therapies. In line with the recommendations of Good Pharmacoeconomic Practice (GDP), when considering the choice of therapy, consideration is given to the economic balance of both the costs of treatment and the social costs incurred as a result of the loss of the patient’s productivity. However, indirect costs were mainly focused on costs obtained from ZUS: disability benefits, rehabilitation benefits, and sickness absences. No GDP calculation was made due to the lack of reliable data on RA. The available data show that GDP per capita in Poland in 2014 was at the level of $ 14 411.495 (with a dollar exchange rate of PLN 4.14, it is about PLN 59 663.60) [12]. Indirect costs generate very large social expenditures. About 12% of sickness absences are associated with rheumatic diseases [12]. The estimated social costs of lost productivity, that is abstinence, and informal care, measured by the human capital method, amount to approximately PLN 2 778 million [5].
However, it is important to note that data may be understated due to limitations in access to ZUS and KRUS (Agricultural Social Insurance Fund) data. In the meantime, ZUS expenses related to RA amount to about PLN 211 million per year [13, 14]. Among the group of diseases of unknown etiology, which are characterized by chronic inflammation and lack of a proper immune response, ZUS allocates the highest benefits for RA. The report „Move to Work” (M2W) shows that the highest annual costs per working person associated with overall loss of productivity are generated by RA patients – approximately PLN 29 700 [14].
Looking at the results of research conducted under the „RA: Join the Fight” campaign, these costs should not be surprising. As many as 47% of respondents considered that RA had a negative impact on their careers or their ability to work [13]. According to ZUS data, in 2011, as a result of sickness absences, patients with RA missed 555 thousand work days, in 2012 – 561 thousand days [13, 14], in 2013 – about 552 thousand days, and in 2014 – 574 thousand days [15].
It is estimated that after 2 years after the diagnosis of RA, every third patient is unable to perform professional activity. After ten years, this number increases to 50% [16]. The persistent disease progression in RA patients generates not only higher direct costs, but also higher indirect costs. Becoming disabled is the worst possible scenario, so it is important to have a well-functioning system that will provide the right treatment and keep the patients in professional activity. One should consider the best solutions that would increase the availability of biological treatment in Poland. It is not enough to change the criteria of the therapeutic program, but also the availability of new therapies for patients must be increased.
Conclusions
Therefore, given the Polish financial conditions, the best solution now is to reduce the prices of biological medications. This is possible through the introduction of biosimilar medications that, when placed on the market, reduce the price of the original medication, as is currently the case with Remicade and Enbrel. The introduction of Inflectra and Remsima, as well as Benepali and Erelzi, has reduced the price base of original medications to similar levels of treatment with biosimilar medications. The wider use of biological treatment would also reduce indirect costs.
Footnotes
The authors of this publication had no research support. The rights revenue was paid by Stowarzyszenie Zbiorowego Zarządzania Prawami Autorskimi Twórców Dzieł Naukowych i Technicznych KOPIPOL of Kielce from fees collected pursuant to Article 20 and Article 201 of the Copyright and Neighbouring Rights Act.
Wynagrodzenie autorskie sfinansowane zostało przez Stowarzyszenie Zbiorowego Zarządzania Prawami Autorskimi Twórców Dzieł Naukowych i Technicznych KOPIPOL z siedzibą w Kielcach z opłat uzyskanych na podstawie art. 20 oraz art. 20ą ustawy o prawie autorskim i prawach pokrewnych.
Sławomir Jeka has conducted lectures during conferences, conventions and business meetings in cooperation with pharmaceutical companies Pfizer, MSD, Sandoz, Roche, Eli Lilly, UCB, Abbvie, Astra Zeneca, Novartis.
The other authors declare no conflict of interest.
References
- 1.Felson D, Anderson J, Boers M, et al. American College of Rheumatology preliminary definitions of improvement in rheumatoid arthritis. Arthritis Rheum. 1995;38:727–735. doi: 10.1002/art.1780380602. [DOI] [PubMed] [Google Scholar]
- 2.Kobelt G, Kasteng F. Access to innovative treatments in rheumatoid arthritis in Europe. A report prepared for the European Federation Of Pharmaceutical Industry Associations (EFPIA) 2009:1–92. [Google Scholar]
- 3.Orlewska E, Wiland P. Access to biologic treatment for rheumatoid arthritis in Central and Eastern European (CEE) countries. Med Sci Monit. 2011;17:1–13. doi: 10.12659/MSM.881697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruszkowski J, Leśniowska J, Gierczyński J, et al. Koszty pośrednie i bezpośrednie leczenia reumatoidalnego zapalenia stawów w Polsce. Farmakoekonomika. 2009;13:3–9. [Google Scholar]
- 5.Wałdysiuk M. Mulitmedial presentation: Koszty pośrednie w ocenie technologii medycznych. Metodyka i rekomendacje dla Polski (Indirect costs in medical technology assessment. Methodology and recommendations for Poland) Krynica-Zdrój: XXIII Economic Forum; 2014. [Google Scholar]
- 6.Głuszko P, Filipowicz-Sosnowska A, Tłustochowicz W. Reumatoidalne zapalenie stawów. Reumatologia. 2012;50:83–90. [Google Scholar]
- 7.Moreland LW, Schiff MH, Baumgartner SW, et al. Etanercept therapy in rheumatoid arthritis. A randomized, controlled trail. Ann Intern Med. 1999;130:478–486. doi: 10.7326/0003-4819-130-6-199903160-00004. [DOI] [PubMed] [Google Scholar]
- 8.Stajszczyk M. Leczenie biologiczne w chorobach reumatycznych w Polsce w 2013 r. Warszawa: Polskie Towarzystwo Reumatologiczne; 2013. Raport; pp. 1–20. [Google Scholar]
- 9.Koligat D, Paczkowska A, Leszczyński P, et al. Analiza kosztów farmakoterapii u pacjentów z reumatoidalnym zapaleniem stawów leczonych biologicznymi lekami modyfikującymi przebieg choroby. Now Lek. 2013;82:394–398. [Google Scholar]
- 10.Koligat D. Katedra i Zakład Farmakoekonomiki i Farmacji Społecznej Uniwersytetu Medycznego im. Poznań: Karola Marcinkowskiego w Poznaniu; 2014. Kalkulacja kosztów leczenia oraz ocena jakości życia pacjentów z reumatoidalnym zapaleniem stawów. [Google Scholar]
- 11.Report on biological treatment Porównajmy się z innymi krajami (Let’s compare ourselves with other countries): http://www.rynekzdrowia.pl/Serwis-Reumatologia/Raport-nt-leczenia-biologicznegoPorownajmy-sie-z-innymi-krajami,136600,1011.html (access from 26.04.2018)
- 12.Kotarba-Kańczugowska M, Kucharski K, Linder-Kopiecka I, et al. JA PACJENT! Perspektywa Organizacji Pacjenckich na Stan Opieki Reumatologicznej w Polsce. Warszawa: Raport Organizacji Pacjenckich; 2014. pp. 115–118. http://zzsk.org.pl/documents/JaPacjentRaportStanuReumatologii2014.pdf (access from 26.04.2018) [Google Scholar]
- 13.Wróbel P. Chorzy mają głos. Rynek Zdrowia. 2013;9:22–26. [Google Scholar]
- 14.Bebrysz M, Fedyna M, Rutkowski J, et al. Przewlekłe choroby zapalne mediowane immunologicznie – ocena kosztów pośrednich w Polsce. Kraków: Central and Eastern European Society of Technology Assessment in Health Care; 2014. pp. 29–58. [Google Scholar]
- 15.Bogusławski S. Reumatoidalne zapalenie stawów. Wydatki na leczenie RZS w Polsce. Warszawa: Sequence HC Partners Sp. z o.o.; 2015. pp. 2–8. [Google Scholar]
- 16.Zheltoukhova K, Bevan S, Reich A. Zdolni do pracy? Choroby układu mięśniowo-szkieletowego a rynek pracy w Polsce. London: The Work Foundation; 2011. pp. 1–116. [Google Scholar]