Abstract
Gut fungi may influence the course of Clostridium difficile infection either positively or negatively for the host. Fungi are not prominent in the mouse gut, and C. albicans, the major human gastrointestinal commensal yeast, is in low abundance or absent in mice. Bifidobacterium is one of the probiotics that may attenuate the severity of C. difficile infection. Inflammatory synergy between C. albicans and C. difficile, in gut, may provide a state that more closely resembles human infection and be more suitable for testing probiotic effects. We performed fecal mycobiota analysis and administered C. albicans at 1 day prior to C. difficile dosing. Fecal eukaryotic 18S rDNA analysis demonstrated the presence of Ascomycota, specifically, Candida spp., after oral antibiotics, despite negative fecal fungal culture. C. albicans administration enhanced the severity of the C. difficile infection model as determined by mortality rate, weight loss, gut leakage (FITC-dextran assay), and serum and intestinal tissue cytokines. This occurred without increased fecal C. difficile or bacteremia, in comparison with C. difficile gavage alone. Candida lysate with C. difficile increased IL-8 production from HT-29 and Caco-2 human intestinal epithelial cell-lines. Bifidobacterium attenuated the disease severity of the C. difficile plus Candida model. The reduced severity was associated with decreased Candida burdens in feces. In conclusion, gut C. albicans worsened C. difficile infection, possibly through exacerbation of inflammation. Hence, a mouse model of Clostridium difficile infection with C. albicans present in the gut may better model the human patient condition. Gut fungal mycobiome investigation in patients with C. difficile is warranted and may suggest therapeutic targets.
Introduction
Clostridium difficile, an anaerobic spore-forming gram-positive bacterium, is the most common cause of nosocomial antibiotic-associated diarrhea of patients in long term care facilities world-wide [1, 2]. C. difficile-associated infection is also the most common hospital-acquired diarrhea worldwide [1]. Gut microbiota alteration due to antibiotic administration diminishes pathogen colonization resistance and is a well-known risk factor for C. difficile infection [2, 3]. Interestingly, C. difficile-induced GI leakage is characterized by i) spontaneous bacteremia deriving from the intestinal microbiota [4], ii) fluorescein isothiocyanate-dextran (FITC-dextran) translocation and iii) elevated serum (1→3)-β-D-glucan (BG) without fungemia [5]. The detection of dextran, a carbohydrate molecule that is not absorbed through the intestine, in serum after oral administration, is a standard gut leakage measurement method [6]. BG is a polyglucoside that is a major component of the fungal cell wall [7]. Spontaneous BG elevation in serum, in the absence of invasive fungal disease or iatrogenic contamination, is also an indirect indicator of gut leakage [5, 8]. C. difficile toxins are responsible for intestinal barrier damage through the disruption of actin cytoskeleton and tight junctions of gut epithelial cells, thus potentiating the translocation of BG [9]. Further, prolonged antibiotic administration, an important risk factor for C. difficile infection, has been shown to induce the overgrowth of Candida spp. (a ubiquitous human GI commensal organism), potentially enhancing the burden of translocatable BG [2, 3, 10, 11]. Although Candida overgrowth is well studied in humans, Candida spp. are not the predominant fungi in the murine GI tract [12]. Yamaguchi et al. demonstrated that Candida albicans in mouse feces was detectable only after a specific mouse chow administration [11]. We also demonstrated that fecal Candida is undetectable in mice without oral administration [8, 13]. Interestingly, Candida colonization has been demonstrated to alter the course of several mouse models of sepsis and food allergy [8, 13, 14]. Accordingly, Candida presence in mouse gut might have an impact on several animal models, especially with respect to intestinal inflammation, and the Candida colonization mouse model might more closely resemble human patient conditions. Based upon the role of C. difficile in enhancing intestinal permeability, and the role of BG as a pro-inflammatory pathogen-associated molecular pattern (PAMP) with pro-inflammatory synergy with other PAMPS [15, 16], we investigated the role of introduced C. albicans, and derivatives, upon the course and symptom severity of murine C. difficile infection.
Materials and methods
Animals
The animal care and use protocol followed that of the National Institutes of Health (NIH) USA (#85–23, revised 1985). The animal protocols number SST 07/2560 were approved by the Institutional Animal Care and Use Committee of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand. Male, C57BL/6 mice at 8-week-old (National Laboratory Animal Center, Nakhornpathom, Thailand) were used. A total of 96 mice were randomized into several groups including 92 mice for the survival studies and experiments and 12 mice for the microbiome analysis.
Fecal mycobiome analysis
Because i) the enhancement of gut Candida colonization by oral antibiotics in patients is well-known [10], ii) Candida spp. are not the predominant fungi in mouse feces [11] and iii) data on fungal colonization in mouse are sparse, we analyzed the mycobiota in feces of antibiotic-administered mice. Antibiotic cocktail (0.5 ml) containing gentamicin (3.5 mg/kg), colistin (4.2mg/kg), metronidazole (21.5mg/kg) and vancomycin (4.5mg/kg) (Sigma Aldrich, St. Louis, MO, USA) was administered twice a day for 3 days (D-6 to D-4) and feces were collected on D-1 (Fig 1). For fecal collection, mice were sacrificed and all visible feces from cecum to rectum were collected and mixed together. Feces from 3 mice (0.25g per mouse) were combined before microbiota analysis. The antibiotic-administered group (6 mice) was divided into ATB#1 and #2 and the control group (6 mice) was divided into control#1 and #2. Of note, mice in the same groups were housed in different cages because co-housing might induce similar gut microbiota within the same cage [17].
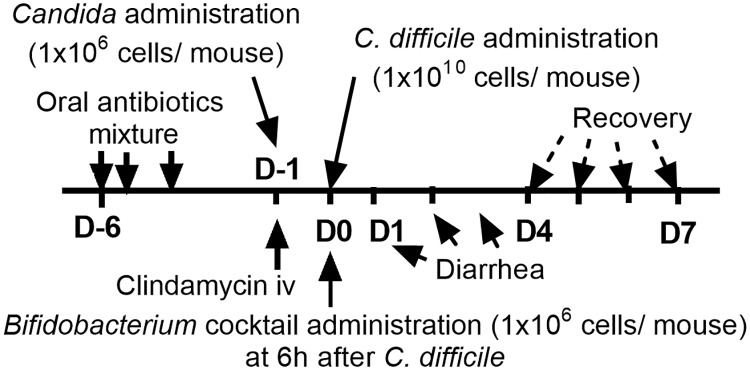
Fig 1. Timeline of the experiment.
The timeline of the C. difficile-infection mouse model is shown. C. difficile-infected mice developed diarrhea at D1-D3 and were recovered, or dead, after D4.
Subsequently, feces from each group (0.25g) were processed for metagenomic DNA extractions with 3 independent extractions per sample. Total nucleic acid was extracted using a Power DNA Isolation Kit (MoBio, Carlsbad, CA, USA). Agarose gel electrophoresis and nanodrop spectrophotometry were used to assess metagenomic DNA quality. Universal eukaryotic 1391F (forward, 5'-GTACACACCGCCCGTC-3') and EukBr (reverse, 5'-TGATCCTTCTGCAGGTTCACCTAC-3'), with appended 5' Illumina adapter and 3' Golay barcode sequences, were used for 18S rRNA gene library construction [16]. Each 25-μl PCR reaction comprised 1×EmeraldAmp1 GT PCR Master Mix (TaKaRa), 0.2μM of each primer, and 75 ng of the metagenomic DNA. Independent triplicate polymerase chain reactions (PCRs) were performed and pooled to prevent stochastic PCR bias. The 18S rDNA amplicons of 258 basepairs (bp) were purified from agarose gel, using the GenepHlow™ Gel Extraction Kit (Geneaid Biotech Ltd., New Taipei City, Taiwan), and quantified by Picogreen (Invitrogen, Eugene, Oregon, USA). Each sample (240 ng) was pooled for Miseq300 platform sequencing (Illumina, San Diego, CA, USA), using the sequencing primers and index sequence described [17]. Mothur’s standard operating procedures for MiSeq platform were used for the quality screening of the raw sequences [18] then aligned and assigned taxa (operational taxonomic unit, OTU) based on a default parameter [18]. Samples were normalized to an equal sampling depth (N = 118121 reads per sample) following Mothur’s computational method [18].
Clostridium difficile infection mouse model and Bifidobacterium cocktail administration
The Clostridium difficile mouse model was set up as previously published [5, 18]. Briefly, 0.5 ml of the antibiotic cocktail was orally administered twice a day for 3 days (Fig 1). At Day 2 after last dose of oral antibiotics (D-1) mouse feces were collected for fecal eukaryotic 18S rDNA analysis (mycobiome) (detail above). In another group of these mice, a single dose of clindamycin (10 mg/kg) was administered intra-peritoneally. Candida albicans ATCC 90028 (Fisher Scientific, Waltham, MA, USA) was cultured overnight on Sabouraud dextrose broth (SDB) (Thermo Scientific, Hampshire, UK), counted by hemocytometer and orally administered 6h later. To select the dose of the Candida-administration, C. albicans at 1x104-1010 CFU were gavaged at D-1. Then mouse feces and blood (through tail vein nicking) were collected daily for 3 days starting at 6h after gavage (D-1) to D1 (see Fig 1) to determine fungi in blood and feces by culture (detail below). For fecal collection, the individual mice were placed in a metabolic cage (Hatteras Instrument, Cary, NC, USA) for a few hours. Then Candida at a dose of 1x106 CFU was administered (selected due to positive fecal fungal culture in the absence of candidemia at least 3 days after the administration). Subsequently, 0.5 ml of C. difficile 1×1010 CFU/ml (ATCC BAA1870, Manassas, VA, USA) in NSS or NSS alone was administered orally at D0 (Fig 1). The control group received oral and intra-peritoneal antibiotics but no organism challenge. In addition, a combination of Bifidobacterium adolescentis-B24 (BA-B24) and Bifidobacterium catenulatum-NB38 (BC-NB38), in a ratio of 1:1 in a total dose at 1x106 cell/ mouse, was orally administered at 6h after C. difficile gavage, to test the effects of the probiotic (Fig 1).
Humane endpoints were used to euthanize mice in distressed condition. The criteria for euthanasia included inability to maintain standing position, hunched position, agonal breathing, weight loss more than 15% and impaired mobility after a stimulation [19]. Mice were monitored daily and mice meeting the criteria were euthanized by cardiac puncture under isoflurane anesthesia. All mice were sacrificed at 7 days post-C. difficile infection.
Gut leakage measurement
Intestinal epithelial permeability (gut leakage), in the model, was determined by serum fluorescein isothiocyanate-dextran (FITC-dextran) and elevation of serum BG without fungemia, as described previously [5, 20]. Briefly, FITC-dextran (molecular weight 4.4 kDa, Sigma, St. Louis, MO, USA) at 0.1 ml/ gram (of 25 mg/ml solution) was orally gavaged at D1 (24h after C. difficile administration) and blood was collected 3h later, through cardiac puncture, under isoflurane, for serum FITC-dextran detection. Blood was allowed to clot, centrifuged, and serum was kept at -80°C until analyzed. Serum BG was analyzed with Fungitell (Associates of Cape Cod, Inc., East Falmouth, MA, USA) and values beyond the lower and upper range of the standard curve at <31 and >500 pg/ml were recorded as 0 and 523 pg/ml, respectively. Serum FITC-dextran was measured by the fluorospectrometry (NanoDrop 3300; Thermo Scientific, Wilmington, DE, USA) with the excitation and emission wavelength at 485 and 523 nm, respectively, against a standard curve of serially diluted FITC-dextran in phosphate buffer solution (PBS).
Mouse sample analysis
For quantitative bacterial analysis, blood (25μl) was spread directly onto blood agar plates (Oxoid, Hampshire, UK), incubated at 37°C and bacterial colonies were enumerated at 24-48h. In parallel, macrophage inflammatory protein 2 (MIP-2), keratinocyte chemoattractant (KC), tumor necrosis factor (TNF)-α and interleukin (IL)-1β, the pathogenesis associated cytokines of C. difficile infection [2], were measured in serum with ELISA assays (PeproTech, NJ, USA). All assays were performed according to the manufacturer’s protocol. For the fungal burden in blood, blood (50 μl), in serial dilution, was directly plated on Sabouraud Dextrose Agar (SDA) with 0.1% chloramphenicol (Thermo Scientific, Hampshire, UK) and Sabouraud Dextrose Broth (SDB) with 0.05 g/l chloramphenicol (Thermo Scientific), then kept at 35°C for 72h before Candida colony enumeration. In addition, the colons of the mice were collected at sacrifice, weighed, homogenized with PBS and used for tissue cytokine analysis (MIP-2, KC, TNF-α and IL-1β) as biomarkers of local inflammatory responses.
Fecal collection and analysis
At sacrifice, all visible feces from cecum to rectum were mixed with PBS in a ratio of 1μg/ 1μl before plating directly onto SDA with 0.1% chloramphenicol (Thermo Scientific) to determine fecal fungal burdens. The plates were incubated at 35°C, for 72h, before fungal colony enumeration. In parallel, fecal fungal identification by polymerase chain reaction (PCR) was also performed. Genomic DNA was extracted from the sample by High Pure PCR Template Preparation Kit (Roche, USA) and quantified by NanoDrop™ 1000 Spectrophotometer (Thermo Scientific). The DNA was amplified in the internal transcribed spacers (ITS1 and ITS2) and fungal taxa were identified by the 5.8S rRNA region of fungal universal primer (kit1 and kit4 i-Taq™ DNA polymerase; iNtRON Biotechnology, Korea).
In addition, the fecal burdens of C. difficile in the mice were quantified using quantitative real-time PCR. The C. difficile toxin B (tcdB)-specific primers tcdB-F [5'-GG AAAAGAGAATGGTTTTATTAA-3'] and tcdB-R [5'-ATCTTTAGTTATAA CTTTGACATCTTT-3'] were from the conserved 5 region of tcdB and generated a 160-bp fragment, as previously described [21]. The standard curve was created by the LightCycler software using 10-fold serial dilution (1 copy number −109 copies number) per 5 μl of plasmid. The profiling standard curve was indicated as a graph of crossing point (Cp) vs. bacterial copy number. The PCR reaction was performed in a 20 μl mixture containing 4 μl of Faststart DNA LightCycler®FastStart DNA MasterPLUSSYBR Green I (Roche, Germany), 9 μl of nuclease-free water, 1 μl of each 10μM primer, and 5 μl of plasmid template. The PCR reaction was performed as follows: 45 cycles of 95°C for 10s, 55°C for 10s, 72°C for 25s with LightCycler® 2.0 instrument (Roche, Germany). The amplified product was measured by a SYBR green fluorescent signal using LightCycler® FastStart DNA MasterPLUSSYBR Green I (Roche, Germany). C. difficile quantification was calculated using the standard curve and shown as bacterial copy number.
Induction of IL-8 production from human intestinal epithelial cells and dectin-1 inhibition
Human colorectal adenocarcinoma cells from the American Type Culture Collection (Manassas, VA, USA) (HT-29 and Caco-2; ATCC HTB-38 and ATCC HTB-37, respectively) were maintained in McCoy’s 5a modified medium supplemented with 10% (v/v) heat-inactivated FBS and Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 20% (v/v) heat-inactivated FBS, respectively at 37°C under 5% CO2 and sub-cultured before performing the co-culture assay. For sub-culture, 5x104 cells/well were plated in a 96-well plate. A preparation of heat-killed C. albicans was used as representative of fungal molecule exposure following a previously published protocol with some modifications [8]. Briefly, C. albicans at 5x105 or 1x106 cells/ ml (intestinal cells: C. albicans: ratio at 1:5 and 1:10, respectively) were killed by heating at 65°C for 30 minutes and sonication (the power setting: pulse on 20 Sec with Amplitude 40%, pulse off 5 Sec, and total processing time 60 min) with a High Intensity Ultrasonic Processor (VC/VCX 130, 500,750). Additionally, live C. difficile in the ratio of 100:1 (bacteria: intestinal cells) were incubated with the cells. The total volume was adjusted by PBS addition to 200 μl/ well. Supernatant was collected at 24h of incubation and cytokines were measured by ELISA (R&D Systems, Minneapolis, MN). Because lipopolysaccharide (LPS) and (1→3)-β-D-glucan (BG) are major cell wall molecules of gram negative bacteria and fungi, respectively, both components were incubated with the intestinal cells to further explore combinatorial effects. Hence, LPS (Escherichia coli 026:B6; Sigma-Aldrich) at 100 ng/ml and/ or BG (Pachyman, Megazyme, Bray, Ireland) at 1 μg/ml, alone and in combination, were incubated with the intestinal cells, followed the above-described procedure. In addition, we hypothesized that a synergistic response of intestinal cells against C. difficile and Candida might, at least in part, go through dectin-1 (a potent receptor of BG found on immune system lineage cells). Accordingly, a dectin-1 blocker, 1, 3/1, 6-β-glucan from Saccharomyces cerevisiae, a competitive inhibitor of dectin-1 (WGP Soluble (tlrl-wgps), Invivogen, San Diego, CA, USA), at 1 μg/ml was incubated for 1 h before certain of the above-described cell stimulation experiments.
Because of the anti-inflammatory property of conditioned medium from some probiotics [22, 23], we tested this potential effect of Bifidobacterium spp. against C. difficile. Bifidobacterium-conditioned media (BCM) were prepared as previously described with modification [24]. Briefly, Bifidobacterium adolescentis-B24 (BA-B24) and Bifidobacterium catenulatum-NB38 (BC-NB38), inoculated at an optical density of 0.1 at 600 nanometers (OD600) was incubated anaerobically for 48h. Supernatants were collected by centrifugation at 4000 xg for 10 min at 4°C, filtered using a 0.22 μm membrane filter (Minisart, Sartorius Stedim Biotech GmbH, Goettingen, Germany) and 500 μL of supernatants were concentrated by speed vacuum drying at 40°C for 3h (Savant instruments, Farmingdale, NY). Residues, concentrated to near dryness, were re-suspended in an equal volume of McCoy’s 5a modified medium or DMEM medium as Bifidobacterium culture media (BCM) and stored at -20°C until further use.
HT-29 and Caco-2 cells (5.0 x 104 cells/well) were pre-cultured in 96 wells plate for 24h. The culture supernatant was replaced with fresh medium containing either (5% vol/vol) BCM of BA-B24 or BC-NB38. Then, C. difficile were added, at the ratio of bacteria: intestinal cells of 100:1, and the mixed cultures were incubated with and without BCM for 24h. IL-8 concentrations in culture supernatants were determined using the Quantikine Human IL-8 Immunoassay Kit (R&D Systems, Minneapolis, MN).
Statistical analysis
Mean ±standard error (SE) was used for the data presentation and the differences between groups were examined for statistical significance by one-way analysis of variance (ANOVA) followed by Tukey’s test for the comparisons of multiple groups. Survival analysis and time course analysis were performed by log-rank test with Bonferroni correction and repeated measure ANOVA, respectively. All statistical analyses were performed with SPSS 11.5 software (SPSS, IL, USA). A P-value < 0.05 was considered to be statistically significant.
Results
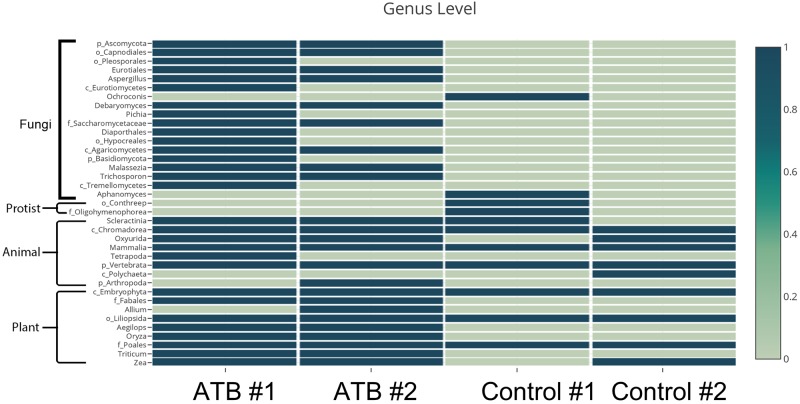
Oral antibiotics enhanced fungal colonization in mouse gut; A mycobiota analysis
Conventional culture and polymerase chain reaction (PCR) for fungal identification were performed upon mouse feces after the oral antibiotic cocktail (at D1 of the model; Fig 1). These were negative in all mice (data not shown). Surprisingly, the 18S rDNA analysis revealed several groups of fungi after antibiotic administration but very few in the control group suggesting increased sensitivity of 18S rDNA analysis over regular PCR. Fungi, in the phyla Ascomycota (eg. Aspergillus and Pichia) and Basidiomycota (eg. Trichosporon) were presented in mouse feces after antibiotic treatment but not in control (Fig 2). Increased 18S rDNA of plant and animal origin was observed in the antibiotic-treated mice, presumably due incomplete digestion of chow. In contrast, Candida spp. in human feces is easily demonstrated by culture (data not shown). Because the scarcity of C. albicans in mouse gut compared with human might influence the mouse model illness severity, we administered C. albicans in the Clostridium difficile model.
Fig 2. Fecal microbiome analysis.
The 18S rDNA analysis of mouse feces, with and without antibiotic administration (ATB and Control, respectively) was analyzed (combined feces from 3 mice in each group).
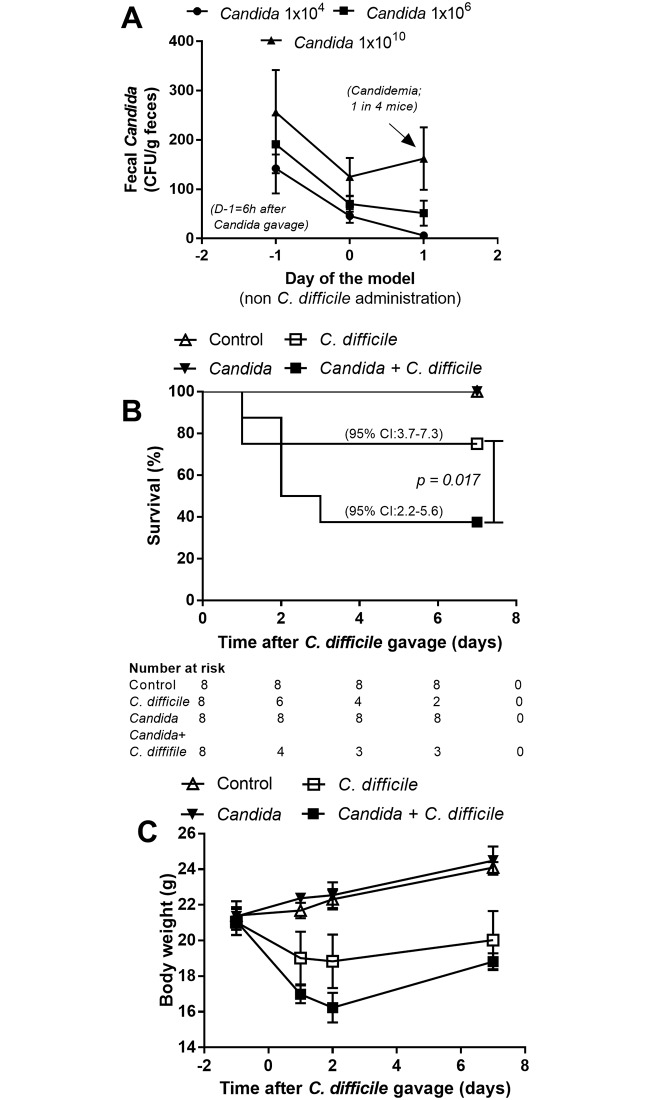
Candida albicans administration enhanced the severity of the Clostridium difficile infection model
The dose of administered Candida could have a variable impact upon the natural course of C. difficile infection. Accordingly, to optimize, we orally administered C. albicans in several doses (1x104-1x1010 CFU) and measured fungi in feces and blood. Recoverable Candida was present in feces as early as 6h after the oral administration, but without significant differences in fungal burdens among the dosage groups (Fig 3A). However, fecal fungi were undetectable in 3 of 4 mice, with a dose of 1x104 CFU, and spontaneous candidemia was demonstrated in 1 of 4 mice at 3 days after fungal administration at a dose of 1x1010 CFU/mouse (Fig 3A). Accordingly, C. albicans dosing at 1x106 CFU was selected for use in all further experiments based upon its providing the most consistent fecal fungi levels, absent candidemia, in comparison with other doses.
Fig 3. Candida albicans dose determination.
To determine the appropriate dose of C. albicans, fecal fungi and fungemia were analyzed after the administration of C. albicans at several dose levels, without C. difficile gavage (n = 4/group) (A). The severity of the C. difficile-infection mouse model and control (non-C. difficile) with and without C. albicans administration (1x106 CFU) as determined by survival analysis (n = 8/group) (B) and weight loss (n = 6-8/time point, except for D7 of Candida + C. difficile group; n = 3) (C) are shown. 95%CI, 95% confidence interval.
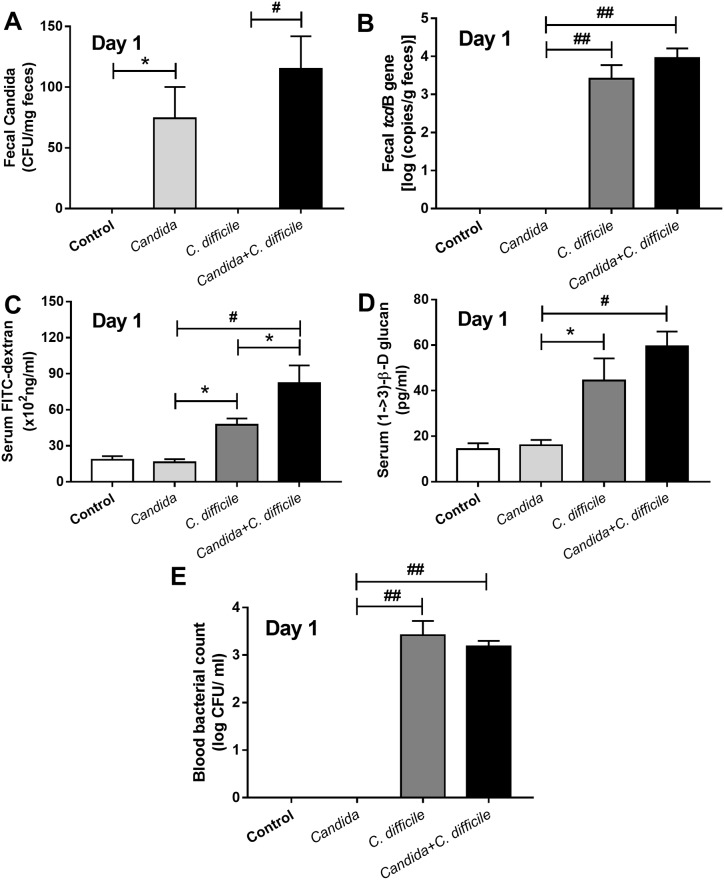
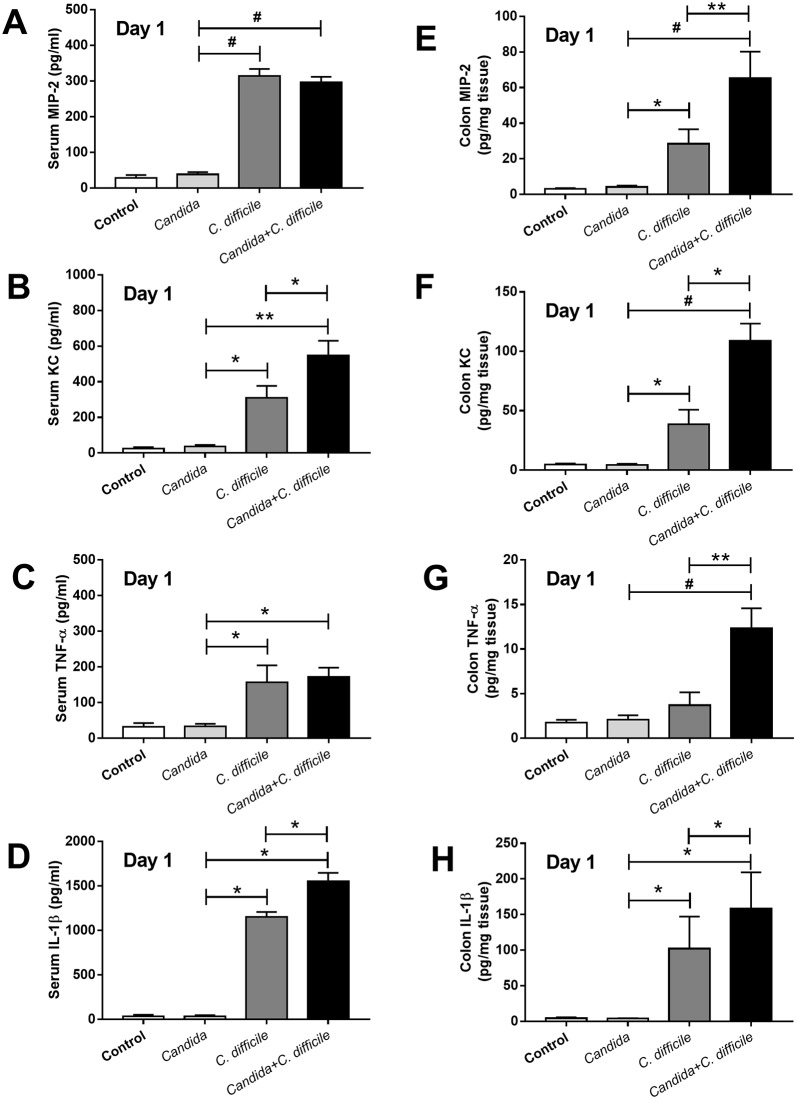
The C. difficile model with Candida administration, as compared with C. difficile gavage alone, was more severe as demonstrated by i) reduced survival rate (from 75% into 38%, respectively) and ii) enhanced generalized bowel edema, 75% of C. difficile +Candida mice and 25% of C. difficile mice, respectively (Fig 3B and S1 Fig), but without a difference in weight loss (Fig 3C). D7 weight was not compared due to the marked mortality difference between the groups. In addition, no direct impact of co-exposure upon the respective populations of C. albicans and C. difficile was observed in the model. Neither fecal Candida nor microbial burden (Clostridium toxin B gene burden) in feces was increased with the co-administration (Fig 4A and 4B). Although Candida alone did not cause gut leakage, Candida enhanced C difficile induced gut leakage as determined by FITC-dextran assay but not by serum BG and bacteremia (Fig 4C–4E). In addition, culturable candidemia was undetectable in all mice (data not shown). In addition, in comparison with C. difficile infection alone, the Candida + C. difficile model showed an increase in only some serum cytokines (serum KC and IL-1β) (Fig 5A–5D). In contrast, a broader spectrum of increased, but localized, inflammatory cytokines (MIP-2, KC, TNF-α and IL-1β) appeared in colon tissue (Fig 5E–5H).
Fig 4. Impact of Candida gavage upon Clostridium difficile model.
To determine the impact of gavaged Candida in the C. difficile mouse model, fecal Candida (A), fecal C. difficile toxin B (B), gut leakage by FITC-dextran assay and serum (1→3)-β-D-glucan (BG) (C, D) and bacteremia (E), were measured (n = 6-8/group). *, p<0.05; #, p< 0.01; ##, p< 0.001.
Fig 5. Inflammatory responses in the model.
The systemic and local inflammatory responses as determined by several inflammatory cytokines in serum and colon tissue, respectively, in C. difficile-infection mouse model and control (non-C. difficile) with and without C. albicans administration are presented (n = 6-8/group) (A-H). *, p<0.05; **, p<0.01; #, p<0.001; MIP-2, macrophage inflammatory protein 2; KC, keratinocyte chemoattractant; TNF-α, tumor necrosis factor-α; IL-1β, interleukin-1β.
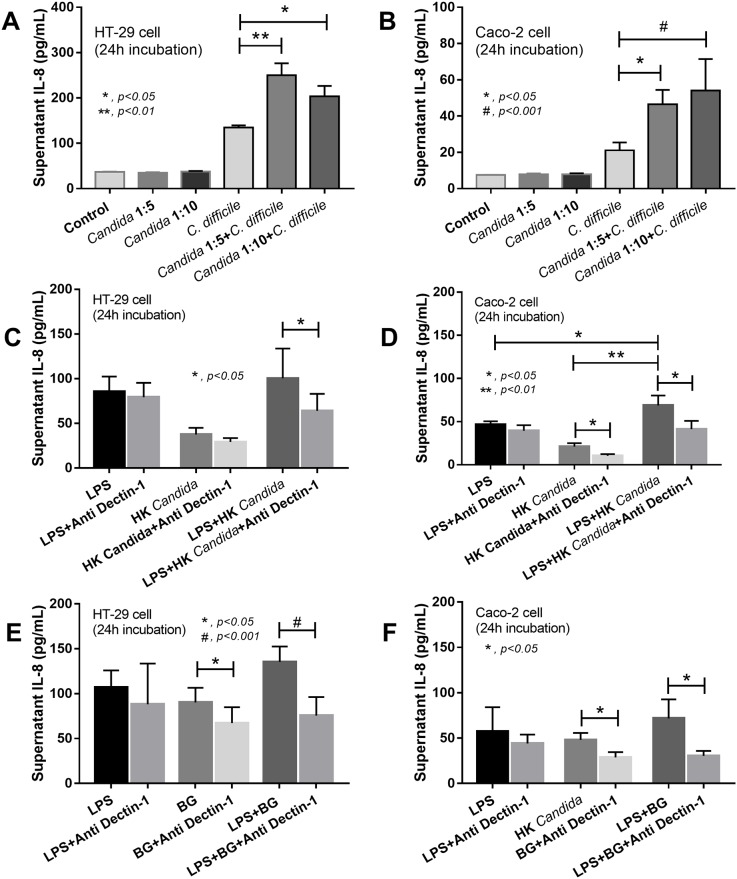
Candida albicans induced pro-inflammatory cytokine production in human intestinal cell-lines
As intestinal epithelial inflammation is one of the important mechanisms responsible for gut leakage, we investigated whether the cell lysate of C. albicans could induce IL-8, an important pro-inflammatory chemokine [25]. Candida lysate together with C. difficile, but not Candida lysate alone, strongly enhanced IL-8 production from the intestinal cells compared with C. difficile alone. However, the enhancement by Candida lysate with C. difficile was not dose-dependent, in the range tested (Fig 6A and 6B). The Candida enhancement of C. difficile-related inflammatory stimulus might reflect cell wall beta-glucan (BG) interaction with the dectin-1 receptor in the host or on cells in culture [26]). The response to co-stimulation with LPS and heat-killed Candida declined with the addition of dectin-1 beta-glucan. However, only Candida-related stimulation (Caco-2 cell only), but not LPS stimulation, was inhibited (Fig 6C and 6D). There was an additive response as demonstrated by higher supernatant IL-8 in LPS + Candida than with LPS alone in Caco-2 cells (Fig 6D). Likewise, in LPS with BG incubation, dectin-1 blocker again reduced the intensity of the co-stimulation and attenuated the reaction of BG alone (but not the reaction of LPS alone) (Fig 6E and 6F). There was no additive response with regard to IL-8 elicitation with LPS+BG compared to LPS stimulus alone (Fig 6E and 6F).
Fig 6. Stimulations of HT-29 and Caco-2 cell-lines.
IL-8 cytokine levels in the culture supernatants of human intestinal epithelial cell lines (HT-29 and Caco-2 cell) after activation by C. difficile or phosphate buffer solution (PBS) as control, with and without the cell lysate of heat-killed C. albicans at the ratio of intestinal cells: C. albicans at 1:5 or 1:10 (see Method) are presented (A, B). In addition, lipopolysaccharide (LPS) alone or with heat-killed C. albicans or (1→3)-β-D-glucan (BG), with and without dectin-1 blocker, were used toward HT-29 and Caco-2 cells (C-F) (independent experiments were performed in triplicate) *, p<0.05; **, p<0.01; #, p<0.001.
Bifidobacterium cocktail effectively attenuated the C. difficile plus Candida model severity
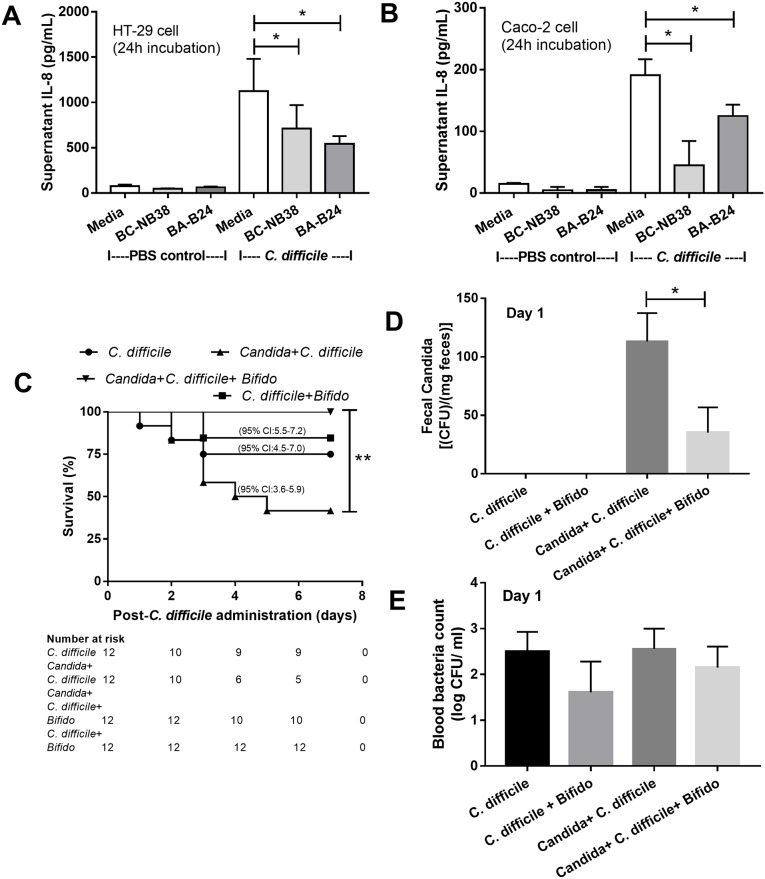
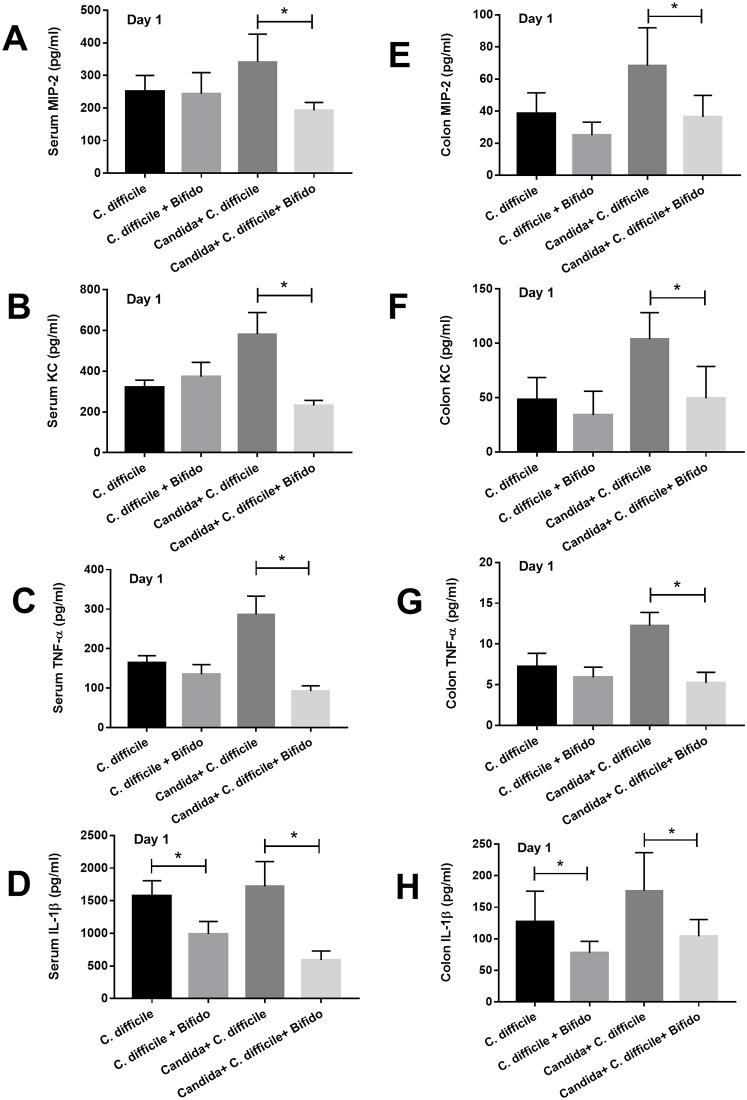
We tested the effectiveness of Bifidobacterium both in vitro with the intestinal cell lines and in vivo, in the two models. First, the cytokine elicitation attenuation properties of the conditioned media from Bifidobacterium adolescentis-B24 (BA-B24) and Bifidobacterium catenulatum-NB38 (BC-NB38) were demonstrated by the decrease in IL-8 production of the C. difficile-activated intestinal cells (HT-29 and Caco-2) (Fig 7A and 7B). Second, the administration of both strains in combination (Bifidobacterium cocktail) improved the survival rate in the C. difficile model with Candida but not the model without Candida (Fig 7C). Likewise, the cocktail significantly attenuated fecal fungal burdens, but not blood bacterial burdens (Fig 7D and 7E). The probiotics also attenuated all cytokines (MIP-2, KC, TNF-α and IL-1β) either in serum or colon in C. difficile model with Candida but reduced only IL-1β (in serum and colon) in the model without Candida (Fig 8A–8H).
Fig 7. The in vitro effect of the probiotic.
IL-8 cytokine levels in the supernatants of human intestinal epithelial cell lines (HT-29 and Caco-2 cell) after activation by C. difficile or phosphate buffer solution (PBS) control, with and without Bifidobacterium adolescentis-B24 (BA-B24) and Bifidobacterium catenulatum-NB38 (BC-NB38), are presented (A, B) (independent experiments were done in triplicate); Survival analysis (C) (n = 12/ group); fecal fungal burdens (D); and blood bacterial count (E) were measured to determine the effect of Bifidobacterium cocktail (Bifido; see Methods) against C. difficile with and without C. albicans administration (n = 5-7/group for D-E). *, p<0.05; **, p< 0.02.
Fig 8. The in vivo effect of the probiotic.
The systemic and local inflammatory responses as determined by several inflammatory cytokines in serum and colon, respectively, after the administration of Bifidobacterium cocktail (Bifido; see Method) in C. difficile-infection with and without C. albicans are presented (n = 6-8/group) (A-H). *, p<0.05; MIP-2, macrophage inflammatory protein 2; KC, keratinocyte chemoattractant; TNF-α, tumor necrosis factor-α; IL-1β, interleukin-1β.
Discussion
Candida albicans is not a prevalent gastrointestinal microorganism in mouse. Oral challenge with Candida exacerbated several markers used to characterize the severity of the course of a C. difficile infection in a murine model. Oral-administration of C. albicans prior to C. difficile administration enhanced the disease severity through increased gut inflammation. Given that gut Candida spp. are commensal organisms in humans and are observed to experience large increases in number under the influence of a wide variety of antibiotics, the murine model of C. difficile with C. albicans might more closely resemble human conditions.
Although antibiotic-induced bacterial dysbiosis in gut is well-known [27–29], the impact of antibiotics upon gut fungi is still an emerging area of study [30]. Mouse gut fungi are undetectable by conventional mouse feces culture [8, 11, 13] but are easily identified in human [10, 31]. Antibiotic effects upon gut levels of Ascomycota (Candida, Aspergillus and Pichia [32, 33]), Basidiomycota (Tricosporon [34]), and Ochroconis and Aphanomyces, a dematiaceous fungus and a water mold [35, 36], respectively, have been observed. Pichia, a group with some species re-classified as Candida [33, 37], were detectable after antibiotic administration despite being undetectable in normal controls.
It is important to consider the role of intestinal fungi in models of gut inflammation as fungi are present in humans and they may be beneficial or detrimental. While gut fungi attenuate the severity of colitis in dextran sulfate solution model possibly through competition with gut pathogenic bacteria [38], C. albicans in gut worsen sepsis severity [8, 13]. This may occur, in part, through increased gut permeability as evidenced by translocation of BG, a major molecular of fungal cell wall [8, 13]. Because of the low abundance of C. albicans in mouse gut, a C. difficile murine model with C. albicans might be a better representative translational model.
Here, we demonstrated that an optimal dose of C. albicans, enough to be detectable in feces by culture for a few days (but in the absence of candidemia), increased the severity of the C. difficile infection model. This may be partly due to increased gut-pathogen burdens (C. albicans + C. difficile) that directly amplified enterocyte inflammation and enhanced gut-translocation of pathogens, PAMPs, or other microbially-derived moeities. Candida gavage alone did not induce gut leakage (as indicated by lack of translocation of FITC-dextran, serum BG and bacteremia) and did not amplify the burdens of C. difficile in gut. In contrast, C. difficile is a well-known organism that directly degrades gut tight-junctions [5, 39]. Tellingly, Candida administration along with C. difficile, in comparison with C. difficile alone, enhanced gut leakage as determined by FITC-dextran (molecular weight; MW 4.4 kDa) although the leakage possibly did not permit larger molecules such as BG (MW 30–300 kDa) to translocate [40]). In addition, co-exposure to Candida and C. difficile increased local inflammatory responses as demonstrated by more elevated cytokine levels from gut specimens and corroborated by in vitro experiments on intestinal cell-lines. Candida or BG (a major fungal molecule) also enhanced the response of LPS against the intestinal cell-lines, presumably through dectin-1 activation. Dectin-1 blockage neutralized this effect. Thus, the in vitro observations suggest that introduction of Candida into the gut enhances the enterocyte response towards both C. difficile and, potentially, various gut-predominant Gram-negative bacteria, in part, through BG-related inflammatory responses. These data support the conclusion that the C. difficile mouse model with Candida is different from the conventional model with C. difficile alone.
To assess potential translational utility of this model, Bifidobacterium were tested for a probiotic effect. Bifidobacterium attenuated the severity of the C. difficile with Candida model demonstrating improved survival. However, only a limited effectiveness in the model without Candida was observed. The probiotic attenuated the C. difficile + Candida model through decreased fecal fungal burdens, but not reduced clostridium toxin in feces, suggesting that a therapeutic strategy focusing on fungal reduction might be useful in C. difficile infection. Gut-derived BG-induced hepatic inflammation has also been observed [41]. Additional studies of fungal burden characterization in C. difficile infection as well as gut fungal burden mitigation are warranted.
Conclusions
The presence of C. albicans in gut enhanced the severity of a murine C. difficile infection model, through the enhancement of intestinal inflammation. This work informs pre-clinical model development for the study of C. difficile infection and suggests translational research approaches.
Supporting information
(TIF)
Acknowledgments
The authors thank Dr. Wasan Punyaseang, a statistician of the research affairs, Faculty of medicine, Chulalongkorn University, Bangkok, Thailand, for his guidance of the statistical analysis.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by Thailand Government Fund (RSA-6080023 to AL) and Thailand Research Fund (RES_61_202_30_022 to AL) and grant for International Research Integration, Chula Research Scholar, Ratchadaphisek Somphot Endowment Fund (2017), Chulalongkorn University (760001-HR to AL). WP was supported by Ratchadaphisek Somphot Fund for Postdoctoral Fellowship, Chulalongkorn University. MF received salary from Cape Cod Inc. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Evans CT, Safdar N. Current Trends in the Epidemiology and Outcomes of Clostridium difficile Infection. Clin Infect Dis. 2015;60 Suppl 2:S66–71. 10.1093/cid/civ140 [DOI] [PubMed] [Google Scholar]
- 2.Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;372(16):1539–48. 10.1056/NEJMra1403772 [DOI] [PubMed] [Google Scholar]
- 3.Kelly CP, Pothoulakis C, LaMont JT. Clostridium difficile colitis. N Engl J Med. 1994;330(4):257–62. 10.1056/NEJM199401273300406 [DOI] [PubMed] [Google Scholar]
- 4.Libby DB, Bearman G. Bacteremia due to Clostridium difficile—review of the literature. Int J Infect Dis. 2009;13(5):e305–9. 10.1016/j.ijid.2009.01.014 [DOI] [PubMed] [Google Scholar]
- 5.Leelahavanichkul A, Panpetch W, Worasilchai N, Somparn P, Chancharoenthana W, Nilgate S, et al. Evaluation of gastrointestinal leakage using serum (1—>3)-beta-D-glucan in a Clostridium difficile murine model. FEMS Microbiol Lett. 2016;363(18). 10.1093/femsle/fnw204 [DOI] [PubMed] [Google Scholar]
- 6.Arrieta MC, Bistritz L, Meddings JB. Alterations in intestinal permeability. Gut. 2006;55(10):1512–20. 10.1136/gut.2005.085373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zekovic DB, Kwiatkowski S, Vrvic MM, Jakovljevic D, Moran CA. Natural and modified (1—>3)-beta-D-glucans in health promotion and disease alleviation. Crit Rev Biotechnol. 2005;25(4):205–30. 10.1080/07388550500376166 [DOI] [PubMed] [Google Scholar]
- 8.Panpetch W, Somboonna N, Bulan DE, Issara-Amphorn J, Worasilchai N, Finkelman M, et al. Gastrointestinal Colonization of Candida Albicans Increases Serum (1—>3)-beta-D-Glucan, without Candidemia, and Worsens Cecal Ligation and Puncture Sepsis in Murine Model. Shock. 2017. 10.1097/SHK.0000000000000896 [DOI] [PubMed] [Google Scholar]
- 9.Voth DE, Ballard JD. Clostridium difficile toxins: mechanism of action and role in disease. Clin Microbiol Rev. 2005;18(2):247–63. 10.1128/CMR.18.2.247-263.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Samonis G, Anastassiadou H, Dassiou M, Tselentis Y, Bodey GP. Effects of broad-spectrum antibiotics on colonization of gastrointestinal tracts of mice by Candida albicans. Antimicrob Agents Chemother. 1994;38(3):602–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamaguchi N, Sonoyama K, Kikuchi H, Nagura T, Aritsuka T, Kawabata J. Gastric colonization of Candida albicans differs in mice fed commercial and purified diets. J Nutr. 2005;135(1):109–15. 10.1093/jn/135.1.109 [DOI] [PubMed] [Google Scholar]
- 12.Koh AY. Murine models of Candida gastrointestinal colonization and dissemination. Eukaryot Cell. 2013;12(11):1416–22. 10.1128/EC.00196-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panpetch W, Somboonna N, Bulan DE, Issara-Amphorn J, Finkelman M, Worasilchai N, et al. Oral administration of live- or heat-killed Candida albicans worsened cecal ligation and puncture sepsis in a murine model possibly due to an increased serum (1—>3)-beta-D-glucan. PLoS One. 2017;12(7):e0181439 10.1371/journal.pone.0181439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamaguchi N, Sugita R, Miki A, Takemura N, Kawabata J, Watanabe J, et al. Gastrointestinal Candida colonisation promotes sensitisation against food antigens by affecting the mucosal barrier in mice. Gut. 2006;55(7):954–60. 10.1136/gut.2005.084954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ballou ER, Avelar GM, Childers DS, Mackie J, Bain JM, Wagener J, et al. Lactate signalling regulates fungal beta-glucan masking and immune evasion. Nat Microbiol. 2016;2:16238 10.1038/nmicrobiol.2016.238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kikkert R, Bulder I, de Groot ER, Aarden LA, Finkelman MA. Potentiation of Toll-like receptor-induced cytokine production by (1—>3)-beta-D-glucans: implications for the monocyte activation test. J Endotoxin Res. 2007;13(3):140–9. Epub 2007/07/11. 10.1177/0968051907080024 [DOI] [PubMed] [Google Scholar]
- 17.Laukens D, Brinkman BM, Raes J, De Vos M, Vandenabeele P. Heterogeneity of the gut microbiome in mice: guidelines for optimizing experimental design. FEMS Microbiol Rev. 2016;40(1):117–32. 10.1093/femsre/fuv036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hutton ML, Mackin KE, Chakravorty A, Lyras D. Small animal models for the study of Clostridium difficile disease pathogenesis. FEMS Microbiol Lett. 2014;352(2):140–9. 10.1111/1574-6968.12367 [DOI] [PubMed] [Google Scholar]
- 19.Nemzek JA, Xiao HY, Minard AE, Bolgos GL, Remick DG. Humane endpoints in shock research. Shock. 2004;21(1):17–25. Epub 2003/12/17. 10.1097/01.shk.0000101667.49265.fd [DOI] [PubMed] [Google Scholar]
- 20.Issara-Amphorn J, Surawut S, Worasilchai N, Thim-Uam A, Finkelman M, Chindamporn A, et al. The Synergy of Endotoxin and (1—>3)-beta-D-Glucan, from Gut Translocation, Worsens Sepsis Severity in a Lupus Model of Fc Gamma Receptor IIb-Deficient Mice. J Innate Immun. 2018;10(3):189–201. 10.1159/000486321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lemee L, Dhalluin A, Testelin S, Mattrat MA, Maillard K, Lemeland JF, et al. Multiplex PCR targeting tpi (triose phosphate isomerase), tcdA (Toxin A), and tcdB (Toxin B) genes for toxigenic culture of Clostridium difficile. J Clin Microbiol. 2004;42(12):5710–4. 10.1128/JCM.42.12.5710-5714.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boonma P, Spinler JK, Venable SF, Versalovic J, Tumwasorn S. Lactobacillus rhamnosus L34 and Lactobacillus casei L39 suppress Clostridium difficile-induced IL-8 production by colonic epithelial cells. BMC Microbiol. 2014;14:177 10.1186/1471-2180-14-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panpetch W, Chancharoenthana W, Bootdee K, Nilgate S, Finkelman M, Tumwasorn S, et al. Lactobacillus rhamnosus L34 Attenuates Gut Translocation-Induced Bacterial Sepsis in Murine Models of Leaky Gut. Infect Immun. 2018;86(1). 10.1128/IAI.00700-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Panpetch W, Spinler JK, Versalovic J, Tumwasorn S. Characterization of Lactobacillus salivarius strains B37 and B60 capable of inhibiting IL-8 production in Helicobacter pylori-stimulated gastric epithelial cells. BMC Microbiol. 2016;16(1):242 10.1186/s12866-016-0861-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zlotnik A, Yoshie O. Chemokines: a new classification system and their role in immunity. Immunity. 2000;12(2):121–7. [DOI] [PubMed] [Google Scholar]
- 26.Tsoni SV, Brown GD. beta-Glucans and dectin-1. Ann N Y Acad Sci. 2008;1143:45–60. 10.1196/annals.1443.019 [DOI] [PubMed] [Google Scholar]
- 27.Francino MP. Antibiotics and the Human Gut Microbiome: Dysbioses and Accumulation of Resistances. Front Microbiol. 2015;6:1543 10.3389/fmicb.2015.01543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iizumi T, Taniguchi T, Yamazaki W, Vilmen G, Alekseyenko AV, Gao Z, et al. Effect of antibiotic pre-treatment and pathogen challenge on the intestinal microbiota in mice. Gut Pathog. 2016;8:60 10.1186/s13099-016-0143-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15(1):73 10.1186/s12967-017-1175-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hill DA, Hoffmann C, Abt MC, Du Y, Kobuley D, Kirn TJ, et al. Metagenomic analyses reveal antibiotic-induced temporal and spatial changes in intestinal microbiota with associated alterations in immune cell homeostasis. Mucosal Immunol. 2010;3(2):148–58. 10.1038/mi.2009.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumamoto CA. Inflammation and gastrointestinal Candida colonization. Curr Opin Microbiol. 2011;14(4):386–91. 10.1016/j.mib.2011.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.BERBEE ML. The phylogeny of plant and animal pathogens in the Ascomycota. Physiological and Molecular Plant Pathology. 2001;59:165–87. [Google Scholar]
- 33.Guitard J, Atanasova R, Brossas JY, Meyer I, Gits M, Marinach C, et al. Candida inconspicua and Candida norvegensis: new insights into identification in relation to sexual reproduction and genome organization. J Clin Microbiol. 2015;53(5):1655–61. 10.1128/JCM.02913-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Colombo AL, Padovan AC, Chaves GM. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin Microbiol Rev. 2011;24(4):682–700. 10.1128/CMR.00003-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Giraldo A, Sutton DA, Samerpitak K, de Hoog GS, Wiederhold NP, Guarro J, et al. Occurrence of Ochroconis and Verruconis species in clinical specimens from the United States. J Clin Microbiol. 2014;52(12):4189–201. 10.1128/JCM.02027-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaulin E, Jacquet C, Bottin A, Dumas B. Root rot disease of legumes caused by Aphanomyces euteiches. Mol Plant Pathol. 2007;8(5):539–48. 10.1111/j.1364-3703.2007.00413.x [DOI] [PubMed] [Google Scholar]
- 37.Guitard J, Angoulvant A, Letscher-Bru V, L’Ollivier C, Cornet M, Dalle F, et al. Invasive infections due to Candida norvegensis and Candida inconspicua: report of 12 cases and review of the literature. Med Mycol. 2013;51(8):795–9. Epub 2013/07/17. 10.3109/13693786.2013.807444 [DOI] [PubMed] [Google Scholar]
- 38.Qiu X, Zhang F, Yang X, Wu N, Jiang W, Li X, et al. Changes in the composition of intestinal fungi and their role in mice with dextran sulfate sodium-induced colitis. Sci Rep. 2015;5:10416 10.1038/srep10416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hecht G, Pothoulakis C, LaMont JT, Madara JL. Clostridium difficile toxin A perturbs cytoskeletal structure and tight junction permeability of cultured human intestinal epithelial monolayers. J Clin Invest. 1988;82(5):1516–24. Epub 1988/11/01. 10.1172/JCI113760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Finkelman M THDamoβ-D-gwLal-brIYS, Castranova V (eds). Toxicity of 1–>3-Beta-glucan, Glucans as a Marker of Fungal exposure. London: Taylor & Francis, 2005, 179–97. [Google Scholar]
- 41.Yang AM, Inamine T, Hochrath K, Chen P, Wang L, Llorente C, et al. Intestinal fungi contribute to development of alcoholic liver disease. J Clin Invest. 2017;127(7):2829–41. Epub 2017/05/23. 10.1172/JCI90562 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.