Abstract
Objective:
Fear of falling is an important problem among older adults, even those with relatively low rates of objective fall risk, who are often overlooked as targets for intervention.
Method:
We developed and pilot tested a new intervention, Activity, Balance, Learning, and Exposure (ABLE), in a sample of 10 older adults with excessive fear of falling. The ABLE intervention integrates exposure therapy and cognitive restructuring with a home safety evaluation and an exercise program and is conducted in the home. In this pilot project, ABLE was jointly conducted by a physical therapist and a psychologist with expertise in geriatric anxiety disorders.
Results:
The intervention was feasible and acceptable and resulted in decreases in fear and activity avoidance for most participants. One participant experienced an injurious fall.
Discussion:
We learned a number of important lessons resulting in modifications to the inclusion criteria, assessments, and intervention over the course of this pilot study. Results suggest that ABLE has promise for treating excessive fear of falling in the elderly and support testing the intervention in a larger randomized trial.
Keywords: falls, fall prevention, fear of falling, exposure therapy, exercise, cognitive-behavioral therapy
One in three adults aged 65 years and older fall each year, and the risk of falling increases with age (Tinetti et al., 1988). Approximately half of those who fall develop a fear of falling (Tinetti et al., 1988), but a significant proportion of older adults who have never fallen experience fear of falling as well (Tinetti et al., 1994). Prevalence estimates ranged from 20 to 39% in several large-scale studies of fear of falling in community-dwelling older adults (Arfken et al., 1994; Bertera and Bertera, 2008; Friedman et al., 2002; Lach, 2005); prevalence is higher in women and increases with age (Arfken et al., 1994; Denkinger et al., 2015). Fear of falling predicts future falls and is associated with depression, frailty, poor quality of life, and restriction in activity (Arfken et al., 1994; Friedman et al., 2002; Hadjistavropoulos et al., 2011). As many as two-thirds of older adults with fear of falling report related activity restriction, and those who limit activities are more likely to fall (Bertera and Bertera, 2008; Friedman et al., 2002; Zijlstra et al., 2007).
Falls and fear of falling are interrelated, and their combination can lead to a downward spiral of activity restriction, disability, future falls, and increasing anxiety related to falls (Arfken et al., 1994). However, even among older adults who have no history of falls, those with fear of falling have an almost fivefold risk of nursing home admission compared to those without fear of falling, indicating that fear of falling is a serious problem regardless of fall history (Cumming et al., 2000). In older adults with either high or low fall risk based on physiological measures, those with fear of falling had lower self-rated quality of life and higher rates of depression, neuroticism, and future falls than those without fear of falling (Delbaere et al., 2010). Thus, it is important to develop interventions that target fear of falling in addition to assessing objective risk profiles.
Research on interventions that aim to reduce fear of falling and increase activity in older adults is needed (Halvarsson et al., 2011; Zijlstra et al., 2007). Multi-component interventions that combine cognitive behavior therapy with balance training, exercise, and home safety assessments may be most effective at reducing fall rate and fear of falling in community-dwelling older adults (Freiberger et al., 2012; Gillespie et al., 2012; Zijlstra et al., 2007). Furthermore, home-based interventions are warranted to reach those individuals who are most fearful and thus may benefit the most from treatment (Tennstedt et al., 1998).
Activity, Balance, Learning, and Exposure (ABLE) is a new, home-based intervention that aims to treat older adults with excessive fear of falling. The ABLE intervention is a multi-component therapy designed to target fear and activity avoidance with exposure therapy and cognitive restructuring while also incorporating exercise and fall prevention education. Exposure therapy is an empirically supported treatment for fears and phobias (Hahlweg et al., 2001; Meuret et al., 2012), but to date the effectiveness of exposure therapy for fear of falling has not been evaluated.
The current study is an open-label pilot demonstration of the ABLE intervention with older adults with excessive fear of falling. We used an adaptive trial design that allowed for revisions to the manual and procedures as needed based on feedback from patients, interventionists, and investigators. The aims of this pilot study were to (1) establish the acceptability and tolerability of the new in-home ABLE intervention, (2) evaluate safety of the ABLE intervention, and (3) assess the feasibility of recruitment procedures and outcome measures for future research efforts.
Method
Participants
Participants were 10 older adults (nine females, one male) aged 71 to 94 years old (M = 80.7, SD = 8.0). All participants were Caucasian and non-Hispanic. Table 1 lists demographic and fall risk characteristics for each participant. Objective and subjective fall risk were calculated based on criteria from Lamb et al. (2008). Participants were classified as low, moderate, or high risk. Fear of falling was determined to be low, moderate, or high based on the Short Falls Efficacy Scale International as described in Delbaere et al. (2010).
Table 1.
Participant demographics
| Participant | Age | Gender | Education (years) | Falls (past year) | Objective fall risk | Subjective fall risk | Fear of falling |
|---|---|---|---|---|---|---|---|
| 1 | 94 | Female | 12 | 1 | Low | Moderate | High |
| 2 | 73 | Female | 12 | 5 | High | High | High |
| 3 | 79 | Female | 14 | 12 | High | High | High |
| 4 | 87 | Female | 12 | 0 | Moderate | Moderate | High |
| 5 | 71 | Male | 18 | 1 | High | Moderate | Moderate |
| 6 | 79 | Female | 18 | 0 | Low | Low | High |
| 7 | 72 | Female | 14 | 1 | Low | Moderate | High |
| 8 | 81 | Female | 12 | 0 | Moderate | Moderate | High |
| 9 | 79 | Female | 14 | 1 | Low | Moderate | High |
| 10 | 92 | Female | 12 | 1 | Low | Moderate | High |
Participants were recruited through senior health fairs, community presentations, and flyers distributed in the community. Recruitment took place for seven months, from December 2010 through June 2011. Inclusion criteria required that participants be 65 years of age or older and report moderate to severe fear of falling and distress or functional impairment because of fear of falling. Additionally, fear of falling had to be excessive relative to the participant’s physical health and functional limitations, as determined by a study physician. All participants were required to obtain approval to participate from their primary care physician.
Exclusion criteria included any medical condition that could interfere with study participation, dementia or cognitive impairment, lifetime diagnosis of bipolar disorder or psychotic disorder, current suicidal ideation, significant orthostasis (e.g. drop of more than 20 points in systolic or diastolic blood pressure from sitting to standing), alcohol or drug abuse within 6 months, or a history of osteoporotic fracture. Participants were also excluded if they were blind (e.g. corrected vision worse than 20/60 in both eyes), required assistance of another person to ambulate or transfer, or were in physical therapy or psychotherapy during the study period. Inclusion and exclusion criteria were selected to attempt to minimize risk for enrolled participants and to target those with more fear than would be appropriate given their fall risk history and current health and functioning.
Eligibility to participate in the study was assessed via an initial telephone screening and an intake evaluation performed by a study physician (DC), which included a physical exam, review of medical records and medications, and evaluation of activity restriction related to fear of falling. Individuals who were deemed ineligible after the intake evaluation received fall prevention education materials and were referred to appropriate outside services.
All participants gave written informed consent prior to enrollment and received monetary compensation for their participation. The study was approved by the University of California, San Diego Institutional Review Board.
Design
Participants completed in-home assessments at baseline, mid-treatment, and post-treatment. In addition, research assistants contacted participants by telephone at 2 and 6 weeks to assess fear and activity avoidance.
The ABLE intervention consisted of 8 weekly in-home sessions lasting approximately 1 h each. Sessions were jointly conducted by a licensed physical therapist (KJ) and licensed psychologist (JW). Each session was videotaped and reviewed by another PT co-investigator (SW) to provide feedback to the interventionists.
ABLE is an integration of an empirically supported fall prevention exercise program, a home safety evaluation, and exposure-based CBT (Table 2). Exercise has demonstrated efficacy in reducing fear of falling as well as preventing falls (Gillespie et al., 2012). The Otago Exercise Programme to Prevent Falls in Older Adults, an in-home, PT-delivered intervention, formed the exercise component of ABLE. The Otago Exercise Programme is a well-established, empirically supported intervention for fall prevention that as a standalone intervention comprises four home visits over an 8-week period, according to the following schedule: weeks 1, 2, 4, and 8 (Campbell et al., 1997; Campbell et al., 1999a; Campbell et al., 1999b; Robertson et al., 2001a; Robertson et al., 2001b).
Table 2.
ABLE intervention
| Session | Contents |
|---|---|
| 1 |
Introduction and exercise
|
| 2 |
Exercise and education
|
| 3 |
Home safety evaluation
|
| 4 |
Exercise and fear hierarchy
|
| 5 |
Exposure
|
| 6 |
Exposure and cognitive restructuring
|
| 7 |
Exposure and cognitive restructuring
|
| 8 |
Exercise and action plan
|
All Otago exercise sessions start with approximately 5 min of gentle warm-up with flexibility exercises. Strengthening exercises focus on five major lower limb muscle groups and include ankle cuff weights, starting at 1 pound and increasing as tolerated to as much as 5 pounds. The balance exercises are dynamic and designed to improve the recovery of balance in addition to helping maintain balance. Patients are instructed to practice the exercises three times a week on their own and to walk for up to 30 min twice a week at their usual pace.
The home safety assessment, conducted in week 3, has been demonstrated to reduce environmental hazards and falls among high-risk older adults (Gillespie et al., 2012; Wyman et al., 2007). The checklist used in ABLE includes specific recommendations for eliminating hazards (e.g. removing throw rugs, installing grab bars; Stay On Your Feet: Your Home Safety Checklist, New South Wales Department of Health, 2004). The therapist accompanied patients through their homes and helped them formulate a personalized action plan to address hazards.
Finally, ABLE also included a number of CBT elements, primarily delivered in weeks 5–7, with some elements covered in sessions 2, 4, and 8: (1) educating the patient about anxiety and the role of avoidance in maintaining it; (2) identifying specific triggers; (3) identifying avoidance behaviors; (4) creating a fear hierarchy; (5) performing exposure practice; (6) identifying negative thoughts and generating more realistic or helpful alternatives; and (7) dealing with setbacks.
Measures
Fear of falling, falls efficacy, and activity avoidance.
The Survey of Activities and Fear of Falling in the Elderly (SAFFE) is an 11-item scale that measures fear of falling and activity restriction (Lachman et al., 1998). Participants are asked if they currently partake in any of 11 items (e.g. “Do you currently walk several blocks outside?”) and then are asked a series of follow-up questions to determine to what extent, if any, the activity is restricted because of fear of falling. The SAFFE was administered at baseline and bi-weekly throughout the treatment phase.
In order to minimize participant burden while taking published recommendations for fear of falling measures into account, we also administered the 7-item Short Falls Efficacy Scale—International (FES-I; Kempen et al., 2008) at baseline and weeks 4 and 8. Each item lists a common activity (e.g. getting dressed or undressed), and the participant is asked to rate how concerned they are that they might fall while doing the activity on a 4-point scale. Total scores range from 7 (no concern about falling) to 28 (severe concern about falling).
The Activity Card Sort (ACS; Baum, 1995) was added mid-study as a patient-centered assessment of activity restriction. Participants choose five activities that they would like to be doing more often from a large set of photographs depicting older adults engaging in numerous activities. Participants were then queried at weeks 4 and 8 about the number of times they engaged in the activity during the past month.
Physical activity.
Physical activity was measured with the Physical Activities Scale for the Elderly (PASE; Washburn et al., 1993). The PASE is a brief self-report scale to assess activity level over a one-week period in adults aged 65 or older. Higher scores indicate higher levels of physical activity. The PASE was administered at baseline, week 4, and week 8.
Acceptability, tolerability, and safety.
The Credibility and Expectations for Improvement Scale (CEI; Devilly and Borkovec, 2000) is a 5-item questionnaire that was administered to participants over the phone after the first session to evaluate how much the participant expected to benefit from the treatment and how logical they felt the treatment was.
Client satisfaction was measured with the Client Satisfaction Questionnaire (CSQ; Attkisson and Zwick, 1982), which was administered at the end of treatment (Week 8). The CSQ is an 8-item self-report questionnaire that is widely used to evaluate patient satisfaction with health services. Scores range from 8 to 32 with higher scores indicating higher satisfaction.
Safety was assessed with a fall calendar to capture the number of falls that the patient experienced while they were in the study. A fall was defined as “including a slip or trip in which you lost your balance and landed on the floor, ground, or lower level” (Hauer et al., 2006). A study physician contacted any participant who fell to assess whether medical attention was needed and to evaluate appropriateness of continuing the intervention.
Mental health.
The Structured Clinical Interview for DSM-IV-TR Patient Edition (First et al., 2007) was used to evaluate participants for psychiatric disorders at baseline. Depression and anxiety symptoms were measured with the Hospital Anxiety and Depression Scale (Zigmond and Snaith, 1983), a 14-item measure with seven items assessing anxiety and seven items assessing depression according to a 4-point Likert scale. Scores of 8 or more on either scale are indicative of clinically significant symptoms. Agoraphobic avoidance was assessed using the 5-item agoraphobia subscale of the Fear Questionnaire (FQ; Marks and Mathews, 1979). Scores range from 0 to 40, with scores over 10 typically considered clinically significant. Post-traumatic Stress Disorder was assessed with a 6-item abbreviated form of the PTSD Checklist (Blanchard et al., 1996). Scores range from 6 to 30, with scores over 14 considered indicative of possible PTSD.
Quality of life and disability.
Quality of life was measured with the Quality of Life Inventory (Frisch et al., 1992). Scores range from 1 to 6, with higher scores indicating greater satisfaction with quality of life. The Short Physical Performance Battery (SPPB; Guralnik et al., 1994) was added mid-study to assess observed physical functioning, with scores ranging from 0 (worst performance) to 12 (best performance).
Results
Acceptability and tolerability
After the first session, participants rated the intervention as very logical (scores ranged from 8 to 10 out of a possible 10 on the CEI; n =8), and expected the program to be somewhat to very useful (scores ranged from 7 to 9 out of a possible 10 on the CEI; n = 8). Participants who completed the 8-week ABLE program reported that they were very satisfied with the intervention, as indicated by scores on the CSQ ranging from 30 to 32 out of a possible 32 (n = 7).
No participants dropped out because of voluntary attrition. Two participants were withdrawn before completing the intervention (one fell and broke her hip; one was too disabled to benefit). The patient with hip fracture was considered low risk for falling based on her medical status, and she had no prior history of falls; her fall occurred when she tripped over a crack in the sidewalk while walking near her home. After reviewing the incident, study consultants and the Data Safety Monitoring Board allowed the trial to continue. Of note, the patient herself requested to reenroll in the study after completing her rehabilitation. The remaining eight participants attended all eight sessions. Seven of them provided data on homework completion. Adherence ranged from 35% to 100%, with a median of 92.5%.
Fear of falling and activity avoidance
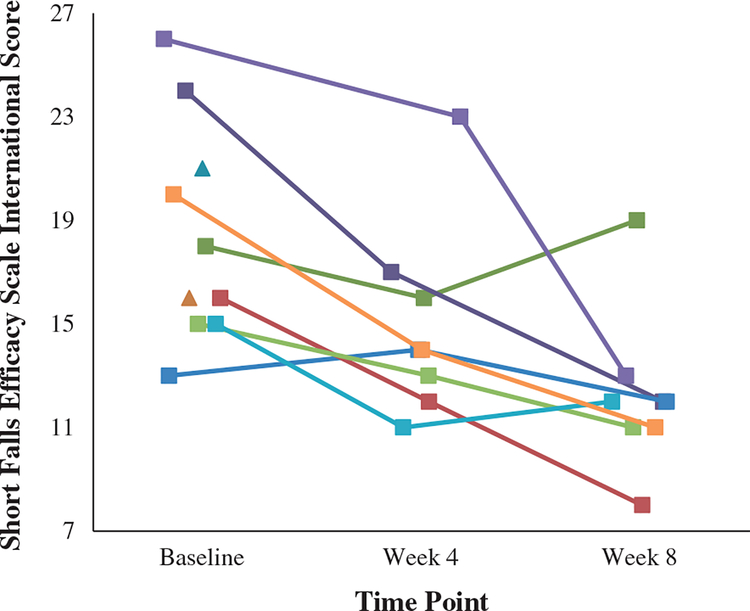
Scores on the SAFFE did not change significantly after the intervention. Scores on the Short FES-I declined from baseline to post-treatment for seven of the eight participants who completed the treatment (see Figure 1), with four participants experiencing a decrease of 30% or more. Across all eight participants, the decline (ΔM = −6.1, SD =5.1) was statistically significant t(7) = −3.37, p = 0.012.
Figure 1.
Participant scores on the Falls Efficacy Scale International indicating fear of falling at baseline, week 4, and week 8.
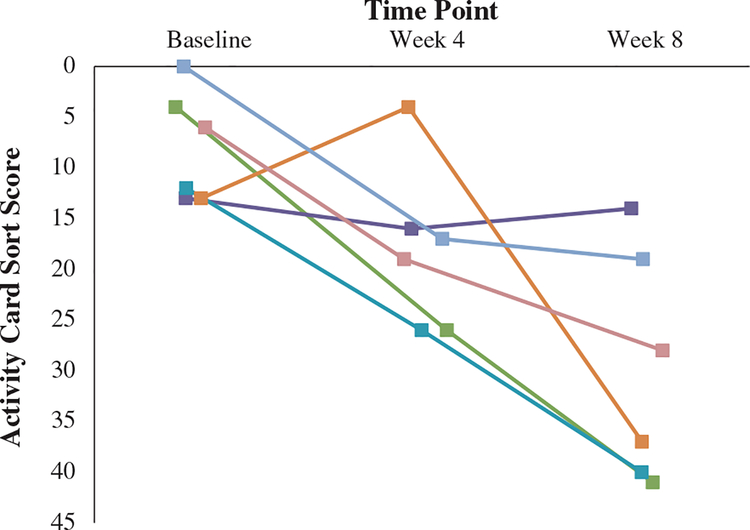
The ACS was added as a measure of activity restriction midway through the study. There was a statistically significant decrease in activity restriction for the six participants who completed the ACS at baseline and post-treatment [t(5)=−4.47, p=0.007], indicating that participants increased the number of times they participated in activities (ΔM=21.8, SD=12.0). Figure 2 displays the change in ACS scores for each of the six participants.
Figure 2.
Participant scores (n = 6) on the Activity Card Sort depicting the number of times that each participant engaged in their top five goal activities at baseline, week 4, and week 8. Downward-sloping lines correspond to higher levels of participation in activities (i.e. lower levels of avoidance).
Table 3 lists scores on the other assessment instruments for each participant at baseline and week 8. No other pre-post treatment effects were statistically significant.
Table 3.
Participant performance on outcome variables
| Measure | Participant | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| SAFFE—Avoidance | ||||||||||
| Baseline | 5 | 3 | 8 | 6 | 3 | 5 | 5 | 2 | 5 | 1 |
| Week 8 | 5 | 7 | --a | --a | 5 | --c | 0 | 0 | 7 | 0 |
| SAFFE—Fear | ||||||||||
| Baseline | 14 | 26 | 25 | 12 | 12 | 9 | 16 | 13 | 21 | 21 |
| Week 8 | 12 | 4 | --a | --a | 17 | --c | 7 | 7 | 10 | 10 |
| Physical Activities Scale for the Elderly | ||||||||||
| Baseline | 2 | 30 | 25 | 41 | 93 | 25 | 72 | 155 | 34 | 59 |
| Week 8 | 31 | 79 | --a | --a | 123 | 38 | 86 | 141 | 35 | 82 |
| Short Physical Performance Battery | ||||||||||
| Baseline | --b | --b | --b | --b | 4 | 9 | 10 | 7 | 8 | 3 |
| Week 8 | 7 | 6 | --a | --a | 4 | 8 | 10 | 9 | 7 | 9 |
| HADS—Anxiety | ||||||||||
| Baseline | 5 | 15 | 16 | 4 | 0 | 12 | 1 | 0 | 3 | 1 |
| Week 8 | 5 | 14 | --a | --a | 3 | 6 | 1 | 1 | 6 | 1 |
| HADS—Depression | ||||||||||
| Baseline | 2 | 18 | 11 | 2 | 3 | 8 | 2 | 1 | 3 | 4 |
| Week 8 | 5 | 16 | --a | --a | 2 | 6 | 1 | 2 | 7 | 8 |
| FQ—Agoraphobia | ||||||||||
| Baseline | 20 | 34 | 24 | N/A | 0 | 8 | 5 | 2 | 1 | 5 |
| Week 8 | 20 | 24 | —a | —a | 4 | 2 | 5 | 4 | 6 | 9 |
| PTSD Checklist (abbreviated form) | ||||||||||
| Baseline | 9 | 21 | 8 | 10 | 8 | 7 | 6 | 6 | 11 | 15 |
| Week 8 | 9 | 21 | —a | —a | 6 | 9 | 6 | 6 | 14 | 12 |
| Quality of Life Inventory | ||||||||||
| Baseline | —b | —b | —b | 5.1 | 4.3 | 1.9 | 3.4 | 4.2 | 2.9 | 2.8 |
| Week 8 | —b | 0.8 | —a | —a | 3.4 | 3.2 | 3.4 | 2.3 | 1.5 | 3.1 |
Note.SAFFE = Survey of Activities and Fear of Falling in the Elderly; HADS = Hospital Anxiety and Depression Scale; FQ = Fear Questionnaire; PTSD = Post Traumatic Stress Disorder.
Withdrawn from study participation prior to Week 8.
Measure added to study after time point.
Measure removed from study prior to time point.
Safety
Five participants reported one fall during the course of the project and one participant reported two falls. One major injury requiring hospitalization (i.e. hip fracture because of a fall) was reported, and the participant was subsequently withdrawn from the study because of inability to participate in the intervention activities. Two participants reported mild injuries or pain as a result of a fall, but did not require medical treatment. No other injuries or adverse events were recorded.
Discussion
Preliminary results from this open-label pilot study suggest that the ABLE intervention may be successful at improving falls efficacy and reducing activity avoidance because of fear of falling in older adults. Eight of 10 participants successfully completed the 8-week intervention. Satisfaction with the intervention was high overall. After completing the intervention, falls efficacy and activity restriction were improved for all but one participant, and most experienced significant improvement.
As a result of this pilot work, changes have been made to the eligibility criteria, assessments, and intervention based on feedback from participants and interventionists in preparation for the next phase of the research. For future investigations, the inclusion criteria will be revised to require severe levels of concern about falling based on a score of greater than 28 on the full 16-item FES-I, and low to moderate actual risk of falling based on criteria by Lamb et al. (2008). Requiring a discrepancy between objective and subjective fall risk will ensure that participants are excessively fearful rather than appropriately cautious. Second, the psychometric properties of the SAFFE were not satisfactory in this study. Specifically, we found ceiling effects in our sample, which was selected to be excessively fearful, i.e. with high levels of fear but relatively low levels of objective risk. Because no one scored lower than 9 (out of 11) activity restrictions, there was very little room for improvement. The FES-I has the further advantages of being self-reported rather than interviewer-administered and is recommended by the international fall research community as the “gold standard” measure of falls efficacy and related concepts such as fear of falling (Kempen et al., 2007; Zijlstra et al., 2007). Finally, the ACS was added midway through the study as a patient-centered measure of activity avoidance. Baseline and Week 8 ACS data were available for six participants, and indicated that the measure was sensitive to change in activity restriction across the 8-week intervention.
Two changes will be made to the exclusion criteria to improve participant safety. To exclude older adults who may be too frail or disabled to safely benefit from the intervention, potential participants will be excluded if they had a body mass index less than 17 or had 3 or more falls in the past year.
Several changes were also made to the ABLE intervention procedures as a result of this pilot study. Methods for safely getting up off the floor after a fall were added to the exercise protocol. Educating older adults on how and when it is safe to get off the floor after a fall is likely to improve confidence and fall-related self-efficacy. Some components of the ABLE intervention were determined to be unnecessary; these included more sessions for participants without caregivers.
Finally, in addition to the changes to the protocol for the next phase of the research, we learned several valuable things regarding the procedures and application of the intervention during this open-label pilot study. Procedures for training physical therapists in how to administer the exposure component were established and refined. We found that the home safety evaluation component required a full 60 min to complete, limiting the amount of other material that could be presented during session 3. The interventionists also learned that it was better to delay the discussion of fear and avoidance until after the first session in order to build rapport with the participant.
Limitations include the fact that this was an open-label pilot study. Randomized trials will be necessary to determine whether the ABLE intervention is superior to a control condition in reducing fear and avoidance in older adults with severe fear of falling. Second, the FES-I is actually a measure of falls efficacy, which is a somewhat distinct concept from fear of falling (Hadjistavropoulos et al., 2011). However, it is currently considered the “gold standard” measure in this field, leading to its use in the present study. Furthermore, participants were mostly female and all Caucasian; a more diverse sample should be recruited for future research efforts. Future research should also include at least a one year follow-up period in order to more thoroughly assess long-term effects on fear, avoidance, and falls.
It should be noted that although we used an exercise protocol that has demonstrated efficacy in reducing falls and fall risk, evidence suggests that a minimum dose of 50 h of exercise, substantially more than the 20 h included in ABLE, is recommended for this purpose (Shubert, 2011). This suggests that the ABLE intervention may not include a sufficiently intensive exercise component for individuals whose primary problem is actual fall risk, as opposed to excessive fear.
In conclusion, this open-label pilot study provides evidence that the ABLE intervention shows promise for individuals with high levels of concern about falling in the context of relatively low actual fall risk. The adaptive study design allowed for revisions to the protocol as needed to ensure that the intervention was administered safely and appropriately. Most of the participants experienced a significant improvement in symptoms of falls efficacy and avoidance after completing the ABLE intervention. Future studies will assess the efficacy of the multifactorial intervention in a larger, randomized trial.
Key points.
An intervention integrating exposure-based cognitive-behavioral therapy and exercise may reduce fear and avoidance among older adults with excessive fear of falling.
The intervention, delivered by a physical therapist and psychologist, is feasible, tolerable, and safe.
Randomized clinical trials are needed to determine whether the intervention is efficacious.
Acknowledgements
Research support from NIMH (R34 MH086668)
Footnotes
Conflict of interest
None declared.
References
- Arfken CL, Lach HW, Birge SJ, Miller JP. 1994. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Pub Health 84: 565–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attkisson CC, Zwick R. 1982. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Prog Plann 5: 233–237. [DOI] [PubMed] [Google Scholar]
- Baum CM. 1995. The contribution of occupation to function in persons with Alzheimer’s disease. J Occup Sci 2: 59–67. DOI: 10.1080/14427591.1995.9686396. [DOI] [Google Scholar]
- Bertera EM, Bertera RL. 2008. Fear of falling and activity avoidance in a national sample of older adults in the United States. Health Soc Work 33: 54–62. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. 1996. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 34: 669–673. [DOI] [PubMed] [Google Scholar]
- Campbell AJ, Robertson MC, Gardner MM, et al. 1997. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 315: 1065–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell AJ, Robertson MC, Gardner MM, et al. 1999a. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc 47: 850–853. [DOI] [PubMed] [Google Scholar]
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. 1999b. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing 28: 513–518. [DOI] [PubMed] [Google Scholar]
- Cumming RG, Salkeld G, Thomas M, Szonyi G. 2000. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol, Ser A: Med Sci 55: M299–305. [DOI] [PubMed] [Google Scholar]
- Delbaere K, Close JCT, Brodaty H, Sachdev P, Lord SR. 2010. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. BMJ 341:. DOI: 10.1136/bmj.c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denkinger MD, Lukas A, Nikolaus T, Hauer K. 2015. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry 23: 72–86. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, Borkovec TD. 2000. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 31: 73–86. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. 2007. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) Biometrics Research, New York State Psychiatric Institute: New York. [Google Scholar]
- Freiberger E, Häberle L, Spirduso WW, Zijlstra GA. 2012. Long-term effects of three multicomponent exercise interventions on physical performance and fall-related psychological outcomes in community-dwelling older adults: a randomized controlled trial. J Am Geriatr Soc 60: 437–446. DOI: 10.1111/j.1532-5415.2011.03859.x. [DOI] [PubMed] [Google Scholar]
- Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. 2002. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc 50: 1329–1335. [DOI] [PubMed] [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. 1992. Clinical validation of the Quality of Life Inventory: a measure of life satisfaction for use in treatment planning and outcome assessment. Psychol Assess 4: 92–101. [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, et al. 2012. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012(9):. DOI: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, et al. 1994. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol, Ser A: Med Sci 49: M85–94. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos T, Delbaere K, Fitzgerald TD. 2011. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health 23: 3–23. [DOI] [PubMed] [Google Scholar]
- Hahlweg K, Fiegenbaum W, Frank M, Schroeder B, von Witzleben I. 2001. Short-and long-term effectiveness of an empirically supported treatment for agoraphobia. J Consult Clin Psychol 69: 375–382. [DOI] [PubMed] [Google Scholar]
- Halvarsson A, Olsson E, Farén E, Pettersson A, Ståhle A. 2011. Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: a randomized controlled trial. Clin Rehabil 25: 1021–1031. DOI: 10.1177/0269215511411937. [DOI] [PubMed] [Google Scholar]
- Hauer K, Lamb SE, Jorstad EC, et al. 2006. Systematic review of definitions and methods of measuring falls in randomized controlled fall prevention trials. Age Aging 35: 5–10. [DOI] [PubMed] [Google Scholar]
- Kempen GI, Todd CJ, Van Haastregt JC, et al. 2007. Cross-cultural validation of the Falls Efficacy Scale International (FES-I) in older people: results from Germany, the Netherlands and the UK were satisfactory. Disabil Rehabil 29: 155–162. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, Yardley L, Van Haastregt JCM, et al. 2008. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 37: 45–50. DOI: 10.1093/ageing/afm157. [DOI] [PubMed] [Google Scholar]
- Lach HW. 2005. Incidence and risk factors for developing fear of falling in older adults. Pub Health Nurs 22: 45–52. DOI: 10.1111/j.0737-1209.2005.22107.x. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Howland J, Tennstedt S, et al. 1998. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE). J Gerontol Ser B: Psychol Sci 53: 43–50. [DOI] [PubMed] [Google Scholar]
- Lamb SE, McCabe C, Becker C, Fried LP, Guralnik JM. 2008. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: the Women’s Health and Aging Study. J Gerontol Ser A: Med Sci 63: 1082–1088. [DOI] [PubMed] [Google Scholar]
- Marks IM, Mathews AM. 1979. Brief standard self-rating for phobic patients. Behav Res Ther 17: 263–267. DOI: 10.1016/0005-7967(79)90041-X [DOI] [PubMed] [Google Scholar]
- Meuret AE, Wolitzky-Taylor KB, Twohig MP, Craske MG. 2012. Coping skills and exposure therapy in panic disorder and agoraphobia: latest advances and future directions. Behav Ther 43: 271–284. DOI: 10.1016/j.beth.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New South Wales Department of Health. Stay on your feet: your home safety checklist. Author, 2004.
- Robertson MC, Devlin N, Gardner MM, et al. 2001a. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ 322: 697–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson MC, Devlin N, Scuffham GMM, Buchner DM, Campbell AJ. 2001b. Economic evaluation of a community based exercise programme to prevent falls. J Epidemiol Community Health 55: 600–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shubert TE. 2011. Evidence-based exercise prescription for balance and falls prevention: a current review of the literature. J Geriatr Phys Ther 34: 100–108. [DOI] [PubMed] [Google Scholar]
- Tennstedt S, Howland J, Lachman M, et al. 1998. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol Ser B: Psychol Sci 53: 384–392. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. 1994. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol Ser A: Med Sci 49: M140–147. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. 1988. Risk factors for falls among elderly persons living in the community. NE J Med 319: 1701–1707. DOI: 10.1056/nejm198812293192604. [DOI] [PubMed] [Google Scholar]
- Washburn RA, Smith KW, Jette AM, Janney CA. 1993. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 46: 153–162. [DOI] [PubMed] [Google Scholar]
- Wyman JF, Croghan CF, Nachreiner NM, et al. 2007. Effectiveness of education and individualized counseling in reducing environmental hazards in the homes of community-dwelling older women. J Am Geriatr Soc 55: 1548–1556. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. 1983. The Hospital Anxiety and Depression Scale. ActaPsychiatr Scand 67: 361–370. [DOI] [PubMed] [Google Scholar]
- Zijlstra GA, van Haastregt JC, van Eijk JT, et al. 2007. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 36: 304–309. DOI: 10.1093/ageing/afm021. [DOI] [PubMed] [Google Scholar]
- Zijlstra GA, van Haastregt JC, van Rossum E, et al. 2007. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc 55: 603–615. DOI: 10.1111/j.1532-5415.2007.01148.x. [DOI] [PubMed] [Google Scholar]