Abstract
Objectives
Cardiorenal syndrome (CRS) is the combination of acute heart failure syndrome (AHF) and renal dysfunction (creatinine clearance (CrCl) ≤60 mL/min). Real-life data were used to compare the management and outcome of AHF with and without renal dysfunction.
Design
Prospective, multicentre.
Setting
Twenty-six academic, community and regional hospitals in France.
Participants
507 patients with AHF were assessed in two groups according to renal function: group 1 (patients with CRS (CrCl ≤60 mL/min): n=335) and group 2 (patients with AHF with normal renal function (CrCl >60 mL/min): n=172).
Results
Differences were observed (group 1 vs group 2) at admission for the incidence of chronic heart failure (56.42% vs 47.67%), use of furosemide (60.9% vs 52.91%), insulin (15.52% vs 9.3%) and amiodarone (14.33% vs 4.65%); additionally, more patients in group 1 carried a defibrillator (4.78% vs 0%), had ≥2 hospitalisations in the last year (15.52% vs 5.81%) and were under the care of a cardiologist (72.24% vs 61.63%). Clinical signs were broadly similar in each group. Brain-type natriuretic peptide (BNP) and BNP prohormone were higher in group 1 than group 2 (1157.5 vs 534 ng/L and 5120 vs 2513 ng/mL), and more patients in group 1 were positive for troponin (58.2% vs 44.19%), had cardiomegaly (51.04% vs 37.21%) and interstitial opacities (60.3% vs 47.67%). The only difference in emergency treatment was the use of nitrates, (higher in group 1 (21.9% vs 12.21%)). In-hospital mortality and the percentage of patients still hospitalised after 30 days were similar between groups, but the median stay was longer in group 1 (8 days vs 6 days).
Conclusions
Renal impairment in AHF should not limit the use of loop diuretics and/or vasodilators, but early assessment of pulmonary congestion and close monitoring of the efficacy of conventional therapies is encouraged to allow rapid and appropriate implementation of alternative therapies if necessary.
Keywords: acute heart Failure, ahf, cardio-renal syndrome, crs, real-life, renal dysfunction
Strengths and limitations of this study.
A large-scale, prospective, real-life study for the management and outcome of patients with cardiorenal syndrome compared with patients with acute heart failure without renal dysfunction.
Only two groups were included (ie, patients with or without kidney dysfunction), rather than for each stage of chronic kidney disease although the creatinine clearance cut-off (60 mL/min) is commonly used.
Glomerular filtration rate was calculated using three different methods.
Glomerular filtration rate estimations were performed by local laboratories for each centre (ie, a real-life situation).
There was no clearance monitoring after hospital discharge.
Background
Heart failure (HF) has an incidence of approximately 2% in adults in developed countries1 and mainly affects elderly patients, who may have multiple comorbidities. One such comorbidity, impaired renal function, has been shown to be a stronger predictor of mortality than impaired cardiac function2 3 and can be present in 50% of patients treated for acute HF (AHF).4 The prognostic importance of the association of renal dysfunction (creatinine clearance (CrCl) ≤60 mL/min) and AHF (cardiorenal syndrome (CRS)) has only been demonstrated recently. This represents a complex pathophysiological condition that has been classified into five stages.5 6 It is worth noting that this is a mechanistic classification and the patients’ clinical management must consider the full clinical presentation.
Even moderate degrees of renal insufficiency are independently associated with an increased risk of mortality from any cause in patients with HF.7 As such, CRS can lead to hesitancy among some clinicians to implement appropriate treatments for HF, such as diuretics, due to the effect that these may have to worsen the renal insufficiency. However, additional prospective research is needed and current recommendations are to maintain such treatments in patients with CRS,8 9 although the emergency physician should make an appropriate risk:benefit assessment for each patient.
In this context, a subanalysis was conducted using real-life data from the Description de la Filière de Soins dans les Syndromes d’Insuffisance Cardiaque Aigue (DeFSSICA study), a large-scale, prospective study that was conducted in patients with suspected dyspnoea of cardiac origin in emergency departments (EDs) throughout France.10 The aim of this subanalysis was to compare the management and outcome of patients with CRS to patients with AHF without renal dysfunction in France using novel real-life data, based on the hypothesis that patients with CRS and AHF would have the same outcome if the management of CRS was based on that for patients with AHF without renal dysfunction.
Methods
Study design
This was a prospective, multicentre study in patients presenting with suspected HF dyspnoea in 26 EDs in academic, community and regional hospitals (the DeFSSICA study) for which the rationale and design are reported elsewhere.10 Written information regarding the objectives of the survey was provided to all patients prior to their inclusion according to French law. Each participating physician presented the study to the patient and/or the patient’s family. The patient and/or the patient’s family could choose for the patient to withdraw from the study at any time. The study did not affect the patient–physician relationship or the patient’s care and follow-up.
Patient involvement
The research question was based on the prognostic importance of CRS and a need for real-life data on the management and outcome of patients with CRS. Patients were not involved in the design, recruitment and conduct of the study, and there is no plan to disseminate the results specifically to the patients who provided data used in this analysis.
Selection of participants
In the DeFSSICA survey, patients >18 years of age with dyspnoea compatible with AHF, defined as dyspnoea associated with peripheral oedema and/or pulmonary crackles and/or excessive weight gain and/or use of furosemide, were eligible for inclusion after ED admission and prior to chest X-ray and laboratory tests. Patient enrolment occurred between 16 June 2014 and 7 July 2014.
In this analysis, only patients with known CrCl were included and were divided into those with CrCl ≤60 mL/min, that is, renal dysfunction (group 1) and those with CrCl >60 mL/min, that is, normal renal function (group 2). Glomerular filtration rate (GFR) was calculated using either the Cockroft-Gault (9 centres), modification of diet in renal disease study (12 centres) or Chronic Kidney Disease (CKD) Epidemiology Collaboration equations (14 centres) (8 centres used two methods and 18 centres used one method).11 12
Study assessments
Patients’ baseline characteristics, medical history, social factors, in-hospital diagnostic tests and treatment, destination after ED discharge, in-hospital mortality and length of stay were recorded by emergency physicians in a case report form, which was structured according to the progress of care. Cardiac sonographic evaluations were performed at the discretion of the emergency physician. Abnormal chest X-ray was defined by the presence of cardiomegaly and/or alveolar oedema and/or interstitial opacity, and/or pleural effusion. The choice of treatment was at the emergency physician’s discretion and according to his/her usual practice. A final diagnosis of AHF was made by the emergency physician using a combination of a clinical history, abnormal chest X-ray, elevated brain-type natriuretic peptide (BNP) or BNP prohormone (pro-BNP), and echocardiographic signs.
Although it was not possible to impose any randomisation or blinding since this was an observational study, any potential bias in the study assessments was minimised by the provision of standard instructions to all participating physicians.
Data were entered into a secure database located at the Réseau Cardiologie Urgence (Cardiovascular Emergency Network) Coordination Centre.
Statistical analysis
Medians and IQRs are provided for continuous variables, and numbers and percentages for qualitative variables. Comparative analyses were performed using the χ2 or Fisher’s exact test for binary variables and the Wilcoxon test for analysis of variance for continuous variables.13 The 5% level was used to identify differences between groups that were of statistical significance (p<0.05). Statistical evaluations were performed using R Statistical Software (V.3.4.1).
Results
Patient disposition and prevalence of CRS
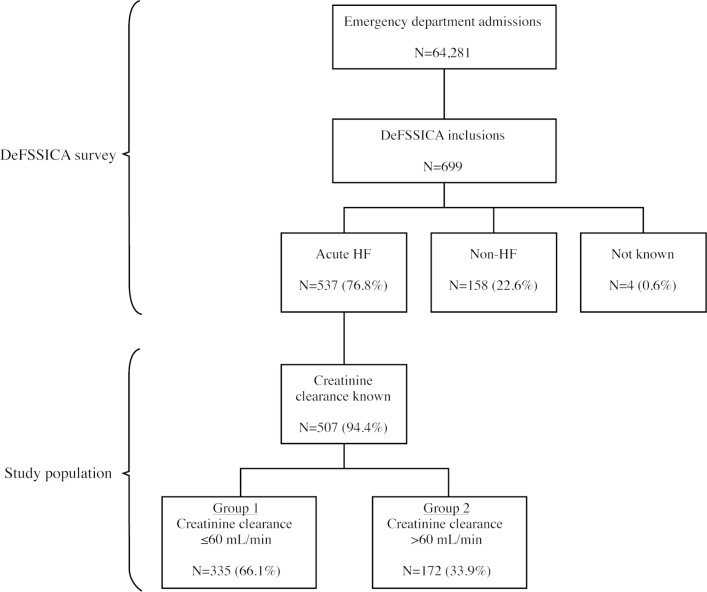
A total of 64 281 ED consultations took place during the survey period and 699 patients with dyspnoea of cardiac origin were included in DeFSSICA study. Of these, 537 patients were identified as having AHF, of whom only those with known CrCl (n=507) were included in this analysis.
Patients in group 1 (n=335 (66.1%)) had renal dysfunction (CrCl ≤60 mL/min) and comprised the population with CRS. In this group, 99 patients (29.6%) had severe renal dysfunction (stage 4 or 5: CrCl: <30 mL/min) and 120 (35.8%) had a known history of chronic renal failure. All patients in group 2 (n=172 (33.9%)) had normal renal function (CrCl >60 mL/min).
Patient disposition is presented in figure 1.
Figure 1.
Patient disposition. DeFSSICA, Description de la Filière de Soins dans les Syndromes d’Insuffisance Cardiaque Aigue; HF, heart failure.
Baseline characteristics
The baseline characteristics of patients in group 1 and group 2 are shown in table 1. There was no difference between group 1 and group 2 in age (median (IQR): 84 (88–79) years and 82 (75–88) years; p=0.09) or sex distribution (42.99% male in group 1 and 44.19% male in group 2; p=0.87).
Table 1.
Baseline characteristics of patients with confirmed AHF syndrome
| All patients with AHF (n=507) |
Group 1 (n=335) |
Group 2 (n=172) |
P value | |
| Age, year | 83 (77; 88) | 84 (78; 89) | 82 (75; 88) | 0.09 |
| Men | 220 (43.39%) | 144 (42.99%) | 76 (44.19%) | 0.87 |
| Comorbidities | ||||
| Hypertension | 353 (69.63%) | 234 (69.85%) | 119 (69.19%) | 0.79 |
| Chronic HF | 271 (53.45%) | 189 (56.42%) | 82 (47.67%) | <0.05 |
| Atrial fibrillation | 223 (43.98%) | 151 (45.07%) | 72 (41.86%) | 0.43 |
| Coronary heart disease | 150 (29.59%) | 98 (29.25%) | 52 (30.23%) | 1.00 |
| Diabetes type I | 14 (2.76%) | 12 (3.58%) | 2 (1.16%) | 0.26 |
| Diabetes type II | 132 (26.04%) | 93 (27.76%) | 39 (22.67%) | 0.20 |
| Chronic renal failure | 114 (22.49%) | 108 (32.24%) | 6 (3.49%) | <0.01 |
| Chronic respiratory failure | 87 (17.16%) | 60 (17.91%) | 27 (15.7%) | 0.46 |
| Known valvular disease | 95 (18.74%) | 70 (20.9%) | 25 (14.53%) | 0.07 |
| Priori medications | ||||
| Furosemide | 295 (58.19%) | 204 (60.9%) | 91 (52.91%) | <0.05 |
| ACEI/ARB | 225 (44.38%) | 153 (45.67%) | 72 (41.86%) | 0.30 |
| β-blocker | 214 (42.21%) | 147 (43.88%) | 67 (38.95%) | 0.20 |
| Anticoagulant | 221 (43.59%) | 151 (45.07%) | 70 (40.7%) | 0.24 |
| Aspirin | 155 (30.57%) | 110 (32.84%) | 45 (26.16%) | 0.08 |
| Other antiplatelet | 56 (11.05%) | 37 (11.04%) | 19 (11.05%) | 0.73 |
| Oral antidiabetic | 66 (13.02%) | 47 (14.03%) | 19 (11.05%) | 0.22 |
| Insulin | 68 (13.41%) | 52 (15.52%) | 16 (9.3%) | 0.03 |
| Amiodarone | 56 (11.05%) | 48 (14.33%) | 8 (4.65%) | <0.01 |
| Aldosterone antagonist | 38 (7.5%) | 26 (7.76%) | 12 (6.98%) | 0.48 |
| Digoxin | 38 (7.5%) | 18 (5.37%) | 20 (11.63%) | 0.10 |
| Thiazidine | 32 (6.31%) | 21 (6.27%) | 11 (6.4%) | 0.70 |
| None | 28 (5.52%) | 14 (4.18%) | 14 (8.14%) | 0.38 |
| Unknown | 13 (2.56%) | 7 (2.09%) | 6 (3.49%) | 1.00 |
| Prior hospitalisation for HF during past year | ||||
| 0 | 287 (56.61%) | 180 (53.73%) | 107 (62.21%) | 0.14 |
| 1 | 130 (25.64%) | 83 (24.78%) | 47 (27.33%) | 0.86 |
| ≥2 | 62 (12.23%) | 52 (15.52%) | 10 (5.81%) | <0.01 |
| Followed by a cardiologist | 348 (68.64% | 242 (72.24%) | 106 (61.63%) | 0.02 |
| Residence | ||||
| At home | 423 (83.43%) | 287 (85.67%) | 136 (79.07%) | 0.06 |
| Retirement institution | 74 (14.6%) | 43 (12.84%) | 31 (18.02%) | 0.18 |
| Other institution | 8 (1.58%) | 4 (1.19%) | 4 (2.33%) | 0.75 |
| Self-sufficient | 258 (50.89%) | 162 (48.36%) | 96 (55.81%) | 0.19 |
| Home assistance | ||||
| Housekeeper | 151 (29.78%) | 111 (33.13%) | 40 (23.26%) | 0.02 |
| Family support | 121 (23.87%) | 87 (25.97%) | 34 (19.77%) | 0.10 |
| Nurse | 134 (26.43%) | 98 (29.25%) | 36 (20.93%) | 0.04 |
| Known cognitive impairment | 83 (16.37%) | 49 (14.63%) | 34 (19.77%) | 0.26 |
| Bedridden | 45 (8.88%) | 25 (7.46%) | 20 (11.63%) | 0.28 |
Data are median (IQR) age or number (%) of patients.
Group 1: patients with CRS; group 2: patients with normal renal function.
ACEI, ACE inhibitor; AHF, acute heart failure; ARB, angiotensin II receptor blocker; CRS, cardiorenal syndrome; HF, heart failure.
As well as the higher incidence of chronic renal failure in group 1, patients with CRS were more likely to have chronic HF (56.42% in group 1 vs 47.67% in group 2; p<0.05). There was no difference in the incidence of any other comorbidity between groups. Patients in group 1 were more likely than patients in group 2 to receive furosemide (60.9% vs 52.91%; p<0.05), insulin (15.52% vs 9.3%; p=0.03) and amiodarone (14.33% vs 4.65%; p<0.01), but there were no other differences between groups for medications. Additionally, patients in group 1 were more likely to have been hospitalised for HF at least twice during the last year (15.52% vs 8.81%; p<0.01), and to be under the care of a cardiologist (72.24% vs 61.63%; p=0.02). The incidence of patients carrying a defibrillator and of pacemakers (single, dual or triple) are not presented since the sample sizes were small (n=16 and n=17, n=36 and n=6, respectively) and so the data were not considered sufficiently robust. Patients in group 1 were more likely to have a housekeeper (31.13% vs 23.26%; p=0.02) and nurse (29.25% vs 20.93%; p=0.04), but there was no difference between groups regarding family support, known cognitive impairment or the incidence of being bedridden.
Hospitalisation and clinical status
Although there were few statistically significant differences between groups in hospitalisation and clinical status parameters (table 2), there was a consistent trend towards more congestion in group 1, including higher levels of dyspnoea, more pulmonary infiltrates on chest X-ray, higher BNP and pro-BNP (table 3 and below).
Table 2.
Hospitalisation route and clinical status of patients with confirmed AHF syndrome
| All patients with AHF (n=507) |
Group 1 (n=335) |
Group 2 (n=172) |
P value | |
| Means of transport | ||||
| Personal | 232 (45.76%) | 157 (46.87%) | 75 (43.6%) | 0.50 |
| Ambulance | 89 (17.55%) | 56 (16.72%) | 33 (19.19%) | 0.63 |
| Firemen | 55 (10.85%) | 34 (10.15%) | 21 (12.21%) | 0.65 |
| MICU | 40 (7.89%) | 29 (8.66%) | 11 (6.4%) | 0.41 |
| Interhospital transfer | 6 (1.18%) | 5 (1.49%) | 1 (0.58%) | 0.48 |
| Clinical signs | ||||
| Warm extremities | 390 (76.92%) | 257 (76.72%) | 133 (77.33%) | 0.23 |
| Cold extremities | 61 (12.03%) | 45 (13.43%) | 16 (9.3%) | 0.97 |
| Signs of right heart failure | 216 (42.6%) | 144 (42.99%) | 72 (41.86%) | 0.69 |
| Inspiratory retraction | 146 (28.8%) | 107 (31.94%) | 39 (22.67%) | 0.02 |
| Inability to speak | 42 (8.28%) | 25 (7.46%) | 17 (9.88%) | 0.54 |
| First recorded vital signs | ||||
| Heart failure, beats/min | 85 (71; 102) | 85 (72; 102) | 85 (72; 104.25) | 0.49 |
| SBP, mm Hg | 140 (121; 160) | 140 (121; 160) | 140 (124; 162) | 0.11 |
| DBP, mm Hg | 76 (65; 90) | 75 (63.5; 89) | 78 (67.75; 92.25) | 0.03 |
| SBP <100 mm Hg | 34 (6.71%) | 27 (8.06%) | 7 (4.07%) | 0.13 |
| Respiratory rate, breaths/min | 25 (20, 30) | 26 (20, 30) | 24 (20, 29) | 0.16 |
| Pulse oximetry, % | 94 (90; 96.25) | 94 (90; 97) | 94 (89; 96) | 0.72 |
| GCS <15 | 48 (9.47%) | 31 (9.25%) | 17 (9.88%) | 0.94 |
| Temperature >37°C | 13 (2.56%) | 12 (3.58%) | 1 (0.58%) | 0.37 |
| Killip status | ||||
| 1 | 128 (25.25%) | 76 (22.69%) | 52 (30.23%) | 0.26 |
| 2 | 269 (53.06%) | 181 (54.03%) | 88 (51.16%) | 0.30 |
| 3 | 84 (16.57%) | 60 (17.91%) | 24 (13.95%) | 0.11 |
| Signs of shock | 15 (2.96%) | 8 (2.39%) | 7 (4.07%) | 0.89 |
Data are median (IQR) beats/minute, median (IQR) mm Hg, median (IQR) breaths/minute, median (IQR) % or number (%) of patients.
Group 1: patients with CRS; group 2: patients with normal renal function.
AHF, acute heart failure; CRS, cardiorenal syndrome; DBP, diastolic blood pressure; GCS, Glasgow Coma Scale; MICU, mobile intensive care unit; SBP, systolic blood pressure.
Table 3.
Biological and diagnosis tests of patients with confirmed AHF syndrome
| All patients with AHF (n=507) |
Group 1 (n=335) |
Group 2 (n=172) |
P value | |
| Biological analysis | ||||
| Performed | 507 (100%) | 335 (100%) | 172 (100%) | |
| Sodium, mmol/L | 138 (135; 141) | 138 (135; 141) | 139 (135; 141) | 0.40 |
| Potassium, mmol/L | 4 (4, 5) | 4 (4, 5) | 4 (4, 5) | 0.89 |
| Creatinine clearance, mL/min | 50 (35; 69.05) | 40 (29; 49.9) | 78.5 (67; 91) | <0.01 |
| Creatinine clearance <30 mL/min | 89 (17.55%) | 89 (26.57%) | 0 (0%) | <0.01 |
| Haemoglobin, g/L | 130 (110, 140) | 120 (110, 130) | 130 (130, 140) | 0.06 |
| Troponin positive | 271 (53.45%) | 195 (58.21%) | 76 (44.19%) | <0.01 |
| BNP, ng/L | 991 (507.5; 2443.5) | 1157.5 (569.25; 2680.5) | 534 (291; 1292) | <0.01 |
| Pro-BNP, ng/L | 4025 (1729; 8863) | 5120 (2520; 12 399.75) | 2513 (1146.5; 5376.5) | <0.01 |
| ECG | ||||
| Performed | 500 (98.61%) | 329 (98.20%) | 171 (99.41%) | |
| Sinusal | 220 (44%) | 145 (43.28%) | 75 (43.6%) | 0.92 |
| Atrial fibrillation | 213 (42.01) | 139 (41.49%) | 74 (43.02%) | 1.00 |
| Driven | 44 (8.8%) | 33 (9.85%) | 11 (6.4%) | 0.19 |
| AVB | 21 (4.14%) | 14 (4.18%) | 7 (4.07%) | 0.86 |
| LBBB | 86 (17.2%) | 64 (19.1%) | 22 (12.79%) | <0.05 |
| RBBB | 59 (11.8%) | 34 (10.15%) | 25 (14.53%) | 0.43 |
| Repolarisation disorder | 101 (20.2%) | 73 (21.79%) | 28 (16.28%) | 0.09 |
| Chest X-ray | ||||
| Performed | 481 (94.87%) | 318 (94.92%) | 163 (94.76%) | |
| Normal | 24 (4.73%) | 11 (3.28%) | 13 (7.56%) | 0.20 |
| Cardiomegaly | 235 (48.86%) | 171 (51.04%) | 64 (37.21%) | 0.01 |
| Interstitial opacities | 284 (59.04%) | 202 (60.3%) | 82 (47.67%) | 0.02 |
| Alveolar opacities | 108 (22.45%) | 64 (19.1%) | 44 (25.58%) | 0.05 |
Data are median (IQR) mmol/L, median (IQR) mL/min, median (IQR) g/dL, median (IQR) ng/L or number (%) of patients.
Group 1: patients with CRS; group 2: patients with normal renal function.
AHF, acute heart failure; AVB, atrioventricular block; BNP, brain natriuretic peptide; CRS, cardiorenal syndrome; LBBB, left bundle branch block; RBBB, right bundle branch block.
There were no significant differences between groups in their means of transport to the ED (most commonly by personal means (45.76% overall)), Killip status (most patients in each group had a Killip status of 2 (53.06% overall) and signs of cardiogenic shock (2.96% overall).
Early management and diagnosis
At admission, blood samples from all patients underwent biological analysis (table 3). As well as the differences between groups for CrCl, significant differences were observed for BNP, which was 2.2-fold higher in group 1 than group 2 (1157.5 ng/L vs 534 ng/L; p<0.01) and pro-BNP, which was twofold higher in group 1 than group 2 (5120 ng/L vs 2513 ng/L; p<0.01). Additionally, troponin was more likely to be positive in patients in group 1 than group 2 (58.21% vs 44.19%; p<0.01). There were no differences between groups for sodium, potassium or haemoglobin.
Most patients underwent under an ECG (98.61% overall) chest X-ray (94.87% overall). Patients in group 1 were more likely than those in group 2 to have left bundle branch block (19.1% vs 12.79%; p<0.05), cardiomegaly (51.04% vs 37.21%; p=0.01) and interstitial opacities (60.3% vs 47.67%; p=0.02).
Echography was only performed for 82 patients and so the data were not considered sufficiently robust for inclusion in the analysis.
Emergency treatments
Patients in group 1 were more likely than group 2 to receive emergency treatment of nitrates (21.19% vs 12.21%; p<0.01), but there were no group differences in other emergency measures (furosemide, oxygen, anticoagulant, continuous positive airway pressure, non-invasive ventilation, antiarrhythmics, ionotropic agents, tracheal intubation) (table 4). Overall 6.31% of patients received no emergency treatment, with no difference between groups.
Table 4.
Emergency treatment of patients with confirmed AHF syndrome
| All patients with AHF (n=507) |
Group 1 (n=335) |
Group 2 (n=172) |
P value | |
| Furosemide | 376 (74.16%) | 252 (75.22%) | 124 (72.09%) | 0.26 |
| Oxygen | 337 (66.47%) | 225 (67.16%) | 112 (65.12%) | 0.43 |
| Nitrates | 92 (18.15%) | 71 (21.19%) | 21 (12.21%) | 0.01 |
| Anticoagulant | 37 (7.3%) | 22 (6.57%) | 15 (8.72%) | 1.00 |
| CPAP | 8 (1.58%) | 6 (1.79%) | 2 (1.16%) | 0.24 |
| NIV | 45 (8.88%) | 30 (8.96%) | 15 (8.72%) | 0.58 |
| Antiarrhythmics | 23 (4.54%) | 15 (4.48%) | 8 (4.65%) | 0.60 |
| Ionotropic agents | 3 (0.59%) | 3 (0.9%) | 0 (0%) | 0.11 |
| Tracheal intubation | 1 (0.2%) | 1 (0.3%) | 0 (0%) | 0.20 |
| None | 32 (6.31%) | 17 (5.07%) | 15 (8.72%) | 0.58 |
Data are number (%) of patients.
Group 1: patients with CRS; group 2: patients with normal renal function.
AHF, acute heart failure; CPAP, continuous positive airway pressure; CRS, cardiorenal syndrome; NIV, non-invasive ventilation.
Outcomes
Precipitating factors were not determined in 42.21% of cases overall, with no overall difference between groups (table 5). The most common determined precipitating factors were an infection (25.25% overall), arrhythmia (15.19% overall) and hypertension (10.65% overall). Diabetes decompensation was considered to be the precipitating factor for AHF in 2.99% of patients in group 1 but none in group 2 (p=0.01). There were no other group differences in precipitating factors.
Table 5.
Outcomes of patients with confirmed AHF syndrome
| All patients with AHF (n=507) |
Group 1 (n=335) |
Group 2 (n=172) |
P value | |
| Precipitating factors | ||||
| Unknown | 214 (42.21%) | 138 (41.19%) | 76 (44.19%) | 0.82 |
| Infection | 128 (25.25%) | 84 (25.07%) | 44 (25.58%) | 0.89 |
| Rhythm disorder | 77 (15.19%) | 47 (14.03%) | 30 (17.44%) | 0.67 |
| Hypertension | 54 (10.65%) | 39 (11.64%) | 15 (8.72%) | 0.19 |
| Non-adherence to treatment | 30 (5.92%) | 17 (5.07%) | 13 (7.56%) | 0.92 |
| Acute coronary syndrome | 21 (4.14%) | 15 (4.48%) | 6 (3.49%) | 0.32 |
| Eating disorder | 20 (3.94%) | 14 (4.18%) | 6 (3.49%) | 0.39 |
| Diabetes decompensation | 10 (1.97%) | 10 (2.99%) | 0 (0%) | 0.01 |
| Discharge destination | ||||
| Cardiology | 142 (28.01%) | 100 (29.85%) | 42 (24.42%) | 0.33 |
| Geriatric medicine | 61 (12.03%) | 34 (10.15%) | 27 (15.7%) | 0.06 |
| Other medical unit | 99 (19.53%) | 67 (20%) | 32 (18.6%) | 0.98 |
| CICU | 62 (12.23%) | 42 (12.54%) | 20 (11.63%) | 1.00 |
| Resuscitation unit | 16 (3.16%) | 11 (3.28%) | 5 (2.91%) | 0.98 |
| ED hospitalisation unit | 74 (14.6%) | 48 (14.33%) | 26 (15.12%) | 0.72 |
| Back home | 26 (5.13%) | 14 (4.18%) | 12 (6.98%) | 0.14 |
| Other | 24 (4.73%) | 18 (5.37%) | 6 (3.49%) | 0.78 |
| Destination considered appropriate | 382 (75.35%) | 246 (73.43%) | 136 (79.07%) | 0.13 |
| Outcome | ||||
| In-hospital mortality | 30 (5.92%) | 24 (7.16%) | 6 (3.49%) | 0.97 |
| Still hospitalised at 30 days | 32 (6.31%) | 20 (5.97%) | 12 (6.98%) | 1.00 |
| Length of stay, days | 7 (4; 13) | 8 (4; 13) | 6 (3; 12) | 0.03 |
Data are number (%) of patients or median (IQR) days.
Group 1: patients with CRS; group 2: patients with normal renal function.
AHF, acute heart failure; CICU, cardiac intesive care unit; CRS, cardiorenal syndrome; ED, emergency department.
There was no difference between groups in discharge destination (which was most often cardiology (28.01% overall)), and the discharge destination was deemed appropriate for a similar number of patients in each group (75.35% overall).
Neither in-hospital mortality (5.92% overall) nor the percentage of patients still hospitalised at 30 days (6.31% overall) was significantly different between group 1 and group 2. However, the median length of stay was 2 days longer in group 1 than in group 2 (8 days vs 6 days; p=0.03) (table 5).
Discussion
The DeFSSICA study was a large-scale, prospective, real-life study conducted following the admission of patients with AHF to EDs throughout France. As such, the data are primarily applicable to the French population, although wider extrapolation is possible due to coherences with similar studies in other geographical regions. The overall DeFSSICA study data are presented elsewhere10 and the present subanalysis reports real-life data from subgroups of patients with AHF with or without concomitant renal dysfunction, based on a CrCl threshold of 60 mL/min. The results show that AHF admissions to EDs are often associated with renal impairment, with almost two-thirds of AHF admissions having CrCl ≤60 mL/min. This prevalence is comparable to published data from France,14 Italy,15 16 Poland,17 Spain,18 19 Taiwan20 and the USA,21–23 as well as from pan-European24 25 and wider international studies.26 In these studies,14–26 the prevalence of renal impairment on the admission of patients with AHF ranged from 54.5% to 64%, including 12.4% to 27.4% of patients with severe renal insufficiency. Patients with a history of chronic renal failure ranged from 21.4% to 32.5%, which is also comparable to the findings of the DeFSSICA survey. However, it should be noted that impaired cardiac function leads to reduced renal perfusion, which could be in addition to an underlying chronic renal insufficiency. Additionally, increased abdominal pressure at admission that can result from ascites can lead to renal vein compression and reduced GFR at admission, which could also result in elevated serum creatinine. It is likely, therefore, that a proportion of acute kidney injury diagnosed at admission based on serum creatinine could be due to temporary changes in perfusion pressures rather than kidney damage per se; these functional reductions in GFR would be expected to recover once a normal haemodynamic function is restored. While it is therefore important to consider the use of biomarkers to provide a more precise assessment of kidney function than serum creatinine,27 28 it is also important to note that the evidence supporting the preferential use of novel biomarkers rather than serum creatinine to detect acute kidney injury can be inconsistent and remains an area for further research.29–32
The overall baseline characteristics, clinical status, biological and diagnostic tests, emergency treatment, and outcome of the patients included in this subanalysis was similar to the overall population in the DeFSSICA study; however, some differences were observed between patients with AHF with and without renal dysfunction, including a trend towards more congestion in patients with CRS. As would be expected due to reduced kidney excretion,33 and as described elsewhere,34–37 BNP and pro-BNP levels were higher in patients with CRS than in patients with AHF with normal renal function and the percentage of troponin-positive patients was also higher in the CRS group. These biomarkers probably reflect the congestion status and remain formally recommended for the management of patients with AHF, especially for their prognostic value. The appropriate use of loop diuretics and/or vasodilators38 in the CRS group, as well as in the AHF group without renal dysfunction, may explain in part the similar intrahospital mortality rate in each group and the similar proportion of patients with AHF with and without renal dysfunction who were still in hospital 30 days after ED admission. Importantly, therefore, the prognosis of patients with CRS was not significantly different using loop diuretics and/or nitrates to those without renal dysfunction. As such, it appears that the correct congestive assessment is vital in this complex clinical situation with concomitant failures in two organs.
Recent publications suggest that appropriate, fast-acting decongesting therapies, as recommended by international guidelines, improve the prognosis for patients with AHF as long as such therapies are introduced early, even if renal impairment develops at the same time.8 Furthermore, it appears that renal impairment in patients with AHF does not have an adverse impact on patient prognosis provided that the congestion is improved. Renal function should be assessed according to the level of patient congestion, and so tools for the assessment of congestion such as the BNP or pro-BNP biomarkers,39 lung ultrasound B-lines (38) or the assessment of the dimensions and compliance of the inferior vena cava are vital. Additionally, haemoconcentration monitoring can be useful for monitoring congestion and significantly improves the short-term outcome of patients with AHF40 and several routinely assessed biological parameters, for example, serum protein, albumin, haemoglobin and haematocrit have been proposed as surrogate markers.41 Furthermore, formulae have been developed to indirectly estimate plasma volume using haemoglobin and/or haematocrit data.42 43 Further research is needed to establish the ability of novel biomarkers such as urinary angiotensinogen,44 neutrophil gelatinase-associated lipocalin,45 46 kidney injury molecule-1,47 interleukin-18,48 49 N-acetyl-β-d-glucosaminidase,50 cystatine C51 52 or a combination of some or all of these could also be used to improve clinical decision-making and therapy. The assessment of diuresis and natriuresis, which reflect both glomerular and tubular function, could offer a strategy to achieve decongestion.50 53 54 Ferreira et al 55 and Palazzuoli et al 56 showed that the lack of a diuretic response is a more important prognostic factor than the use of loop diuretics. This suggests a new diagnostic challenge, that is to assess the patient’s response to diuretics.57–60 However, despite some proposals to define diuretic resistance (eg, persistent congestion despite adequate and escalating doses of diuretic with >80 mg furosemide/day, amount of sodium excreted as a percentage of filtered load <0.2%, failure to excrete ≥90 mmol of sodium within 72 hours of a 160 mg oral furosemide dose given two times daily) and the means of evaluation (eg, weight loss per unit of 40 mg furosemide (or equivalent), net fluid loss/mg of loop diuretic (40 mg of furosemide or equivalent) during hospitalisation, natriuretic response to furosemide),61 there is currently no consensus for commonly accepted standards. Additionally, it is important that any alteration of GFR should be interpreted in the context of the deterioration of the clinical situation.
Another alternative therapy in CRS is the use of mineralocorticoid antagonists. These have been associated with an improvement in both congestion62 63 and mortality in patients with HF,64 65 although the Aldosterone Targeted Neurohormonal Combined with Natriuresis Therapy in Heart Failure (ATHENA-HF) trial results are less conclusive.66 Combined therapies have also been evaluated, including hypotonic saline serum in combination with diuretic therapy to improve diuresis67 68 and mannitol in combination with furosemide,61 although their benefit in diuretic-resistant patients is not confirmed. The addition of metolazone to furosemide could be of interest because of its capacity to produce diuresis even in patients with low GFR.69 70 In a meta-analysis, Wang et al showed that tolvaptan, an oral vasopressin V2-receptor antagonist, may also represent an alternative therapy in worsening renal function (WRF).71 Several studies have shown that tolvaptan can decrease WRF in patients treated with furosemide.72 73 Finally, venous ultrafiltration allows controlled hydrosodic depletion by subtracting isotonic fluid, compared with diuretics that allow the subtraction of hypotonic fluid. Other studies suggest that the effectiveness of ultrafiltration is associated with a reduction in inflammatory cytokines.74 These and other approaches in patients with cardiac insufficiency and resistance to diuretics have recently been reviewed.61
The CRS analysis using data from the DeFSSICA survey has some limitations. First, only two groups have been analysed (ie, patients with or without renal dysfunction), whereas CKD is characterised by five stages.5 However, as noted earlier, this is a mechanistic classification and in the present analysis the use of the CrCl threshold of 60 mL/min, which is commonly used to define renal dysfunction,2 37 75–77 is considered to be satisfactory, especially since the small number of patients would not allow a thorough analysis for five subcategories. However, the pathophysiology of WRF in AHF is complex78 and using a spot measurement of serum creatinine to classify CRS has limitations. This approach does not allow the separation of patients with acute and chronic CRS: in the present study, 35.8% of patients included in the CRS group had a history of chronic renal failure and so may not have suffered any acute change in renal function, whereas patients with acute changes in serum creatinine compared with their own baseline but not fulfilling the <60 mL/min criterion would not have been included in the CRS group. That said, the presence of renal failure on admission remains strongly associated with a poor prognosis irrespective of the anterior renal status and despite the lack of WRF in the first 5 days.79 While the choice of a CrCl threshold of 30 mL/min could have led to a greater chance of obtaining a significant difference between groups in terms of outcome, we based our analysis on the 60 mL/min cut-off since it is more widely used. Second, since the data used are observational, it was not possible to impose any randomisation or blinding, and the number of patients in each group was not balanced. Third, GFR assessments were performed by local laboratories for each centre, rather than standardised at a single centre, and repeated measures of GFR could have improved their accuracy and comparability. The use of different formulae to evaluate CrCl in a chronic disease state and an acute context without knowledge of the baseline value reflects the real-life situation. While potentially problematic, with the possibility of some incorrect classification of CKD, numerous previous studies of the impact of renal failure in AHF have used a similar approach.2 37 75 Finally, it was not possible to subclassify different types of CRS in this analysis since Kidney Disease Improving Global Outcomes data were not collected, although as described earlier the small number of patients would not have allowed a thorough analysis for each subcategory.
Conclusion
These real-life data suggested that patients with CRS have the same outcome as patients with AHF without renal dysfunction when the treatment of the former group is modelled on that for the latter group. This finding should not limit the use of loop diuretics and/or vasodilators as long as the patients present congestion as assessed using biomarkers and ultrasound. The use of diuretic treatment should be based on a more rapid diagnosis of congestion and evaluation of an inadequate response to diuretics, allowing the rapid and appropriate implementation of alternative therapies if necessary.
Supplementary Material
Acknowledgments
The authors thank the emergency physicians and cardiologists and patients who participated in this survey at the following centers: CHU Toulouse, CHU Rouen, CHU Clermont Ferrand, CHU Nancy, CHR Metz-Thionville-Hôpital de Mercy, Hôpital Lariboisière-Paris, CHR Annecy Genevois, CHU Lyon-Hôp, Edouard Herriot, CHRU de Lille, Chu De Caen, CHU Nice-Hôpital Saint-Roch, CHU de Grenoble, Hôpital Bicêtre-Paris, Hôpital St Louis Paris, CH I Meulan, CH d’Avignon, CH Jacques Lacarin–Vichy, CH d’Aix En Provence, CH Fleyriat – Bourg En Bresse, CH Bourgoin Jallieu, CHU de Saint Etienne, CH du Forez Montbrison-Feurs, CH de Firminy, CH Villefranche-Sur-Saône, CHU De Brest, CH Henri Mondor, CH de Vienne.
The authors also thank the RESCUe Network for the practical implementation of this survey and statistical analysis and Novartis France for its financial support.
Footnotes
Contributors: SM-S, NP, SC, ME, DS, EB-C, SL, PH, TC and CEK conceived the study, designed the trial and obtained research funding. TC and CEK supervised the conduct of the trial and data collection. NP, SC, DS and TC undertook recruitment of participating centers and patients. LF managed the data, including quality control, provided statistical advice and analysed the data. DdR, LF, AB, AG, KT, TC and CEK drafted the manuscript, and all authors contributed substantially to its revision. All authors reviewed and approved the final version of the manuscript and are accountable for its content.
Funding: Andrew Lane (Lane Medical Writing), funded by the RESCUe network, provided professional medical writing assistance in the preparation and development of the manuscript in accordance with the European Medical Writers Association guidelines and Good Publication Practice.
Competing interests: CEK has received grants from Novartis (other than this work), Daiichy Sankyo and Boehringer Ingleheim. NP report has acted as a paid consultant for Vygon SA. SC reports personal fees from Novartis (other than this work). LF is an employee of RESCUe Network.
Patient consent: Not required.
Ethics approval: The study received approval from the National Commission for Liberties and Data Protection (Commission Nationale de l’Informatique et des Libertés) (number DR-2014–543) and the Advisory Committee on the Treatment of Information in the field of Health Research (Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le Domaine de la Santé) (number 14–291).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The database supporting the results presented in this article can be shared on reasonable request.
References
- 1. Sayago-Silva I, García-López F, Segovia-Cubero J. Epidemiology of heart failure in Spain over the last 20 years. Rev Esp Cardiol 2013;66:649–56. 10.1016/j.rec.2013.03.012 [DOI] [PubMed] [Google Scholar]
- 2. Ferreira JP, Girerd N, Pellicori P, et al. Renal function estimation and Cockroft-Gault formulas for predicting cardiovascular mortality in population-based, cardiovascular risk, heart failure and post-myocardial infarction cohorts: The Heart ‘OMics’ in AGEing (HOMAGE) and the high-risk myocardial infarction database initiatives. BMC Med 2016;14:181 10.1186/s12916-016-0731-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hillege HL, Girbes AR, de Kam PJ, et al. Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation 2000;102:203–10. 10.1161/01.CIR.102.2.203 [DOI] [PubMed] [Google Scholar]
- 4. Damman K, Valente MA, Voors AA, et al. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J 2014;35:455–69. 10.1093/eurheartj/eht386 [DOI] [PubMed] [Google Scholar]
- 5. Ronco C, Haapio M, House AA, et al. Cardiorenal syndrome. J Am Coll Cardiol 2008;52:1527–39. 10.1016/j.jacc.2008.07.051 [DOI] [PubMed] [Google Scholar]
- 6. Ronco C, House AA, Haapio M. Cardiorenal syndrome: refining the definition of a complex symbiosis gone wrong. Intensive Care Med 2008;34:957–62. 10.1007/s00134-008-1017-8 [DOI] [PubMed] [Google Scholar]
- 7. Dries DL, Exner DV, Domanski MJ, et al. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol 2000;35:681–9. 10.1016/S0735-1097(99)00608-7 [DOI] [PubMed] [Google Scholar]
- 8. Hanberg JS, Tang WHW, Wilson FP, et al. An exploratory analysis of the competing effects of aggressive decongestion and high-dose loop diuretic therapy in the DOSE trial. Int J Cardiol 2017;241:277–82. 10.1016/j.ijcard.2017.03.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Testani JM, Ter Maaten JM. Decongestion in acute heart failure: does the end justify the Means? JACC Heart Fail 2016;4:589–90. 10.1016/j.jchf.2016.03.024 [DOI] [PubMed] [Google Scholar]
- 10. Chouihed T, Manzo-Silberman S, Peschanski N, et al. Management of suspected acute heart failure dyspnea in the emergency department: results from the French prospective multicenter DeFSSICA survey. Scand J Trauma Resusc Emerg Med 2016;24:112 10.1186/s13049-016-0300-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Diseases NIoDaDK. Estimating glomerular filtration rate (GFR). Secondary Estimating glomerular filtration rate (GFR). 2015. https://www.niddk.nih.gov/health-information/health-communication-programs/nkdep/lab-evaluation/gfr/estimating/Pages/estimating.aspx
- 12. Botev R, Mallié JP, Couchoud C, et al. Estimating glomerular filtration rate: Cockcroft-Gault and Modification of Diet in Renal Disease formulas compared to renal inulin clearance. Clin J Am Soc Nephrol 2009;4:899–906. 10.2215/CJN.05371008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ancelle T. Statistique Epidémiologique. 3rd ed Paris: Maloine, 2011. [Google Scholar]
- 14. Logeart D, Isnard R, Resche-Rigon M, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail 2013;15:465–76. 10.1093/eurjhf/hfs189 [DOI] [PubMed] [Google Scholar]
- 15. Oliva F, Mortara A, Cacciatore G, et al. Acute heart failure patient profiles, management and in-hospital outcome: results of the Italian Registry on Heart Failure Outcome. Eur J Heart Fail 2012;14:1208–17. 10.1093/eurjhf/hfs117 [DOI] [PubMed] [Google Scholar]
- 16. Tavazzi L, Maggioni AP, Lucci D, et al. Nationwide survey on acute heart failure in cardiology ward services in Italy. Eur Heart J 2006;27:1207–15. 10.1093/eurheartj/ehi845 [DOI] [PubMed] [Google Scholar]
- 17. Straburzyńska-Migaj E, Kałużna-Oleksy M, Maggioni AP, et al. Patients with heart failure and concomitant chronic obstructive pulmonary disease participating in the Heart Failure Pilot Survey (ESC-HF Pilot) - Polish population. Arch Med Sci 2015;11:743–50. 10.5114/aoms.2014.47878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Conde-Martel A, Formiga F, Pérez-Bocanegra C, et al. Clinical characteristics and one-year survival in heart failure patients more than 85 years of age compared with younger. Eur J Intern Med 2013;24:339–45. 10.1016/j.ejim.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 19. Llorens P, Escoda R, Miró Ò, et al. [Characteristics and clinical course of patients with acute heart failure and the therapeutic measures applied in Spanish emergency departments: based on the EAHFE registry (Epidemiology of Acute Heart Failure in Emergency Departments)]. Emergencias 2015;27:11–22. [PubMed] [Google Scholar]
- 20. Chang HY, Wang CC, Wu YW, et al. One-Year Outcomes of Acute Decompensated Systolic Heart Failure in Taiwan: Lessons from TSOC-HFrEF Registry. Acta Cardiol Sin 2017;33:127–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abraham WT, Fonarow GC, Albert NM, et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: insights from the organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE-HF). J Am Coll Cardiol 2008;52:347–56. 10.1016/j.jacc.2008.04.028 [DOI] [PubMed] [Google Scholar]
- 22. Adams KF, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the united states: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J 2005;149:209–16. 10.1016/j.ahj.2004.08.005 [DOI] [PubMed] [Google Scholar]
- 23. Diercks DB, Fonarow GC, Kirk JD, et al. Risk stratification in women enrolled in the Acute Decompensated Heart Failure National Registry Emergency Module (ADHERE-EM). Acad Emerg Med 2008;15:151–8. 10.1111/j.1553-2712.2008.00030.x [DOI] [PubMed] [Google Scholar]
- 24. Cleland JG, Swedberg K, Follath F, et al. The EuroHeart Failure survey programme- a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J 2003;24:442–63. 10.1016/S0195-668X(02)00823-0 [DOI] [PubMed] [Google Scholar]
- 25. Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J 2006;27:2725–36. 10.1093/eurheartj/ehl193 [DOI] [PubMed] [Google Scholar]
- 26. Follath F, Yilmaz MB, Delgado JF, et al. Clinical presentation, management and outcomes in the Acute Heart Failure Global Survey of Standard Treatment (ALARM-HF). Intensive Care Med 2011;37:619–26. 10.1007/s00134-010-2113-0 [DOI] [PubMed] [Google Scholar]
- 27. Molitoris BA, Levin A, Warnock DG, et al. Improving outcomes of acute kidney injury: report of an initiative. Nat Clin Pract Nephrol 2007;3:439–42. 10.1038/ncpneph0551 [DOI] [PubMed] [Google Scholar]
- 28. Waikar SS, Bonventre JV. Creatinine kinetics and the definition of acute kidney injury. J Am Soc Nephrol 2009;20:672–9. 10.1681/ASN.2008070669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Breidthardt T, Sabti Z, Ziller R, et al. Diagnostic and prognostic value of cystatin C in acute heart failure. Clin Biochem 2017;50:1007–13. 10.1016/j.clinbiochem.2017.07.016 [DOI] [PubMed] [Google Scholar]
- 30. Breidthardt T, Socrates T, Drexler B, et al. Plasma neutrophil gelatinase-associated lipocalin for the prediction of acute kidney injury in acute heart failure. Crit Care 2012;16:R2 10.1186/cc10600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Maisel AS, Wettersten N, van Veldhuisen DJ, et al. Neutrophil Gelatinase-Associated Lipocalin for acute kidney injury during acute heart failure hospitalizations: The AKINESIS Study. J Am Coll Cardiol 2016;68:1420–31. 10.1016/j.jacc.2016.06.055 [DOI] [PubMed] [Google Scholar]
- 32. Meersch M, Schmidt C, Hoffmeier A, et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med 2017;43:1551–61. 10.1007/s00134-016-4670-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tuegel C, Bansal N. Heart failure in patients with kidney disease. Heart 2017;103:1848–53. 10.1136/heartjnl-2016-310794 [DOI] [PubMed] [Google Scholar]
- 34. Anwaruddin S, Lloyd-Jones DM, Baggish A, et al. Renal function, congestive heart failure, and amino-terminal pro-brain natriuretic peptide measurement: results from the ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) Study. J Am Coll Cardiol 2006;47:91–7. 10.1016/j.jacc.2005.08.051 [DOI] [PubMed] [Google Scholar]
- 35. Wu AH, Jaffe AS, Apple FS, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: use of cardiac troponin and B-type natriuretic peptide or N-terminal proB-type natriuretic peptide for etiologies other than acute coronary syndromes and heart failure. Clin Chem 2007;53:2086–96. 10.1373/clinchem.2007.095679 [DOI] [PubMed] [Google Scholar]
- 36. Lamb EJ, Vickery S, Price CP. Amino-terminal pro-brain natriuretic peptide to diagnose congestive heart failure in patients with impaired kidney function. J Am Coll Cardiol 2006;48:1060–1. 10.1016/j.jacc.2006.06.019 [DOI] [PubMed] [Google Scholar]
- 37. Vickery S, Price CP, John RI, et al. B-type natriuretic peptide (BNP) and amino-terminal proBNP in patients with CKD: relationship to renal function and left ventricular hypertrophy. Am J Kidney Dis 2005;46:610–20. 10.1053/j.ajkd.2005.06.017 [DOI] [PubMed] [Google Scholar]
- 38. Peacock WF, Emerman C, Costanzo MR, et al. Early vasoactive drugs improve heart failure outcomes. Congest Heart Fail 2009;15:256–64. 10.1111/j.1751-7133.2009.00112.x [DOI] [PubMed] [Google Scholar]
- 39. Gargani L, Frassi F, Soldati G, et al. Ultrasound lung comets for the differential diagnosis of acute cardiogenic dyspnoea: a comparison with natriuretic peptides. Eur J Heart Fail 2008;10:70–7. 10.1016/j.ejheart.2007.10.009 [DOI] [PubMed] [Google Scholar]
- 40. Breidthardt T, Weidmann ZM, Twerenbold R, et al. Impact of haemoconcentration during acute heart failure therapy on mortality and its relationship with worsening renal function. Eur J Heart Fail 2017;19:226–36. 10.1002/ejhf.667 [DOI] [PubMed] [Google Scholar]
- 41. Girerd N, Seronde MF, Coiro S, et al. Integrative assessment of congestion in heart failure throughout the patient journey. JACC Heart Fail 2018;6:273–85. 10.1016/j.jchf.2017.09.023 [DOI] [PubMed] [Google Scholar]
- 42. Mentz RJ, Kjeldsen K, Rossi GP, et al. Decongestion in acute heart failure. Eur J Heart Fail 2014;16:471–82. 10.1002/ejhf.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Duarte K, Monnez JM, Albuisson E, et al. Prognostic value of estimated plasma volume in heart failure. JACC Heart Fail 2015;3:886–93. 10.1016/j.jchf.2015.06.014 [DOI] [PubMed] [Google Scholar]
- 44. Yang X, Chen C, Tian J, et al. Urinary angiotensinogen level predicts AKI in Acute decompensated heart failure: a prospective, two-stage study. J Am Soc Nephrol 2015;26:2032–41. 10.1681/ASN.2014040408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Elsharawy S, Raslan L, Morsy S, et al. Plasma neutrophil gelatinase-associated lipocalin as a marker for the prediction of worsening renal function in children hospitalized for acute heart failure. Saudi J Kidney Dis Transpl 2016;27:49–54. 10.4103/1319-2442.174071 [DOI] [PubMed] [Google Scholar]
- 46. Ito M, Doi K, Takahashi M, et al. Plasma neutrophil gelatinase-associated lipocalin predicts major adverse cardiovascular events after cardiac care unit discharge. J Cardiol 2016;67:184–91. 10.1016/j.jjcc.2015.05.010 [DOI] [PubMed] [Google Scholar]
- 47. Medić B, Rovčanin B, Basta Jovanović G, et al. Kidney Injury Molecule-1 and cardiovascular diseases: from basic science to clinical practice. Biomed Res Int 2015;2015:1–10. 10.1155/2015/854070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Springer-Verlag. Les biomarqueurs en médécine d’urgence [French]. 1 ed. Paris: Springer-Verlag, 2012. [Google Scholar]
- 49. Taub PR, Borden KC, Fard A, et al. Role of biomarkers in the diagnosis and prognosis of acute kidney injury in patients with cardiorenal syndrome. Expert Rev Cardiovasc Ther 2012;10:657–67. 10.1586/erc.12.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Verbrugge FH, Dupont M, Steels P, et al. The kidney in congestive heart failure: ‘are natriuresis, sodium, and diuretics really the good, the bad and the ugly?’. Eur J Heart Fail 2014;16:133–42. 10.1002/ejhf.35 [DOI] [PubMed] [Google Scholar]
- 51. Lassus JP, Harjola VP, Peuhkurinen K, et al. Cystatin C, NT-proBNP, and inflammatory markers in acute heart failure: insights into the cardiorenal syndrome. Biomarkers 2011;16:302–10. 10.3109/1354750X.2011.555822 [DOI] [PubMed] [Google Scholar]
- 52. Legrand M, De Berardinis B, Gaggin HK, et al. Evidence of uncoupling between renal dysfunction and injury in cardiorenal syndrome: insights from the BIONICS study. PLoS One 2014;9:e112313 10.1371/journal.pone.0112313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Metra M, Davison B, Bettari L, et al. Is worsening renal function an ominous prognostic sign in patients with acute heart failure? The role of congestion and its interaction with renal function. Circ Heart Fail 2012;5:54–62. 10.1161/CIRCHEARTFAILURE.111.963413 [DOI] [PubMed] [Google Scholar]
- 54. Mullens W, Verbrugge FH, Nijst P, et al. Renal sodium avidity in heart failure: from pathophysiology to treatment strategies. Eur Heart J 2017;38:1872–82. 10.1093/eurheartj/ehx035 [DOI] [PubMed] [Google Scholar]
- 55. Ferreira JP, Girerd N, Bettencourt Medeiros P, et al. Lack of diuretic efficiency (but not low diuresis) early in an acutely decompensated heart failure episode is associated with increased 180-day mortality. Cardiorenal Med 2017;7:137–49. 10.1159/000455903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Palazzuoli A, Testani JM, Ruocco G, et al. Different diuretic dose and response in acute decompensated heart failure: clinical characteristics and prognostic significance. Int J Cardiol 2016;224:213–9. 10.1016/j.ijcard.2016.09.005 [DOI] [PubMed] [Google Scholar]
- 57. Damman K, Testani JM. The kidney in heart failure: an update. Eur Heart J 2015;36:1437–44. 10.1093/eurheartj/ehv010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hoorn EJ, Ellison DH. Diuretic resistance. American Journal of Kidney Diseases 2017;69:136–42. 10.1053/j.ajkd.2016.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ray EC, Boyd-Shiwarski CR, Kleyman TR. Why diuretics fail failing hearts. J Am Soc Nephrol 2017;28:3137–8. 10.1681/ASN.2017070797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Valente MA, Voors AA, Damman K, et al. Diuretic response in acute heart failure: clinical characteristics and prognostic significance. Eur Heart J 2014;35:1284–93. 10.1093/eurheartj/ehu065 [DOI] [PubMed] [Google Scholar]
- 61. ter Maaten JM, Valente MA, Damman K, et al. Diuretic response in acute heart failure-pathophysiology, evaluation, and therapy. Nat Rev Cardiol 2015;12:184–92. 10.1038/nrcardio.2014.215 [DOI] [PubMed] [Google Scholar]
- 62. Bansal S, Lindenfeld J, Schrier RW. Sodium retention in heart failure and cirrhosis: potential role of natriuretic doses of mineralocorticoid antagonist? Circ Heart Fail 2009;2:370–6. 10.1161/CIRCHEARTFAILURE.108.821199 [DOI] [PubMed] [Google Scholar]
- 63. Hensen J, Abraham WT, Dürr JA, et al. Aldosterone in congestive heart failure: analysis of determinants and role in sodium retention. Am J Nephrol 1991;11:441–6. 10.1159/000168356 [DOI] [PubMed] [Google Scholar]
- 64. RALES. Effectiveness of spironolactone added to an angiotensin-converting enzyme inhibitor and a loop diuretic for severe chronic congestive heart failure (the Randomized Aldactone Evaluation Study [RALES]). Am J Cardiol 1996;78:902–7. 10.1016/S0002-9149(96)00465-1 [DOI] [PubMed] [Google Scholar]
- 65. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med 1999;341:709–17. 10.1056/NEJM199909023411001 [DOI] [PubMed] [Google Scholar]
- 66. Butler J, Anstrom KJ, Felker GM, et al. Efficacy and safety of spironolactone in acute heart failure: the athena-hf randomized clinical trial. JAMA Cardiol 2017;2:950–8. 10.1001/jamacardio.2017.2198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Licata G, Di Pasquale P, Parrinello G, et al. Effects of high-dose furosemide and small-volume hypertonic saline solution infusion in comparison with a high dose of furosemide as bolus in refractory congestive heart failure: long-term effects. Am Heart J 2003;145:459–66. 10.1067/mhj.2003.166 [DOI] [PubMed] [Google Scholar]
- 68. Paterna S, Di Pasquale P, Parrinello G, et al. Changes in brain natriuretic peptide levels and bioelectrical impedance measurements after treatment with high-dose furosemide and hypertonic saline solution versus high-dose furosemide alone in refractory congestive heart failure: a double-blind study. J Am Coll Cardiol 2005;45:1997–2003. 10.1016/j.jacc.2005.01.059 [DOI] [PubMed] [Google Scholar]
- 69. Ng TM, Konopka E, Hyderi AF, et al. Comparison of bumetanide- and metolazone-based diuretic regimens to furosemide in acute heart failure. J Cardiovasc Pharmacol Ther 2013;18:345–53. 10.1177/1074248413482755 [DOI] [PubMed] [Google Scholar]
- 70. Tilstone WJ, Dargie H, Dargie EN, et al. Pharmacokinetics of metolazone in normal subjects and in patients with cardiac or renal failure. Clin Pharmacol Ther 1974;16:322–9. 10.1002/cpt1974162322 [DOI] [PubMed] [Google Scholar]
- 71. Wang C, Xiong B, Cai L. Effects of Tolvaptan in patients with acute heart failure: a systematic review and meta-analysis. BMC Cardiovasc Disord 2017;17:164 10.1186/s12872-017-0598-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Jujo K, Saito K, Ishida I, et al. Randomized pilot trial comparing tolvaptan with furosemide on renal and neurohumoral effects in acute heart failure. ESC Heart Fail 2016;3:177–88. 10.1002/ehf2.12088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kimura K, Momose T, Hasegawa T, et al. Early administration of tolvaptan preserves renal function in elderly patients with acute decompensated heart failure. J Cardiol 2016;67:399–405. 10.1016/j.jjcc.2015.09.020 [DOI] [PubMed] [Google Scholar]
- 74. Torina AG, Silveira-Filho LM, Vilarinho KA, et al. Use of modified ultrafiltration in adults undergoing coronary artery bypass grafting is associated with inflammatory modulation and less postoperative blood loss: a randomized and controlled study. J Thorac Cardiovasc Surg 2012;144:663–70. 10.1016/j.jtcvs.2012.04.012 [DOI] [PubMed] [Google Scholar]
- 75. Chew DP, Astley C, Molloy D, et al. Morbidity, mortality and economic burden of renal impairment in cardiac intensive care. Intern Med J 2006;36:185–92. 10.1111/j.1445-5994.2006.01012.x [DOI] [PubMed] [Google Scholar]
- 76. Schaub JA, Coca SG, Moledina DG, et al. Amino-Terminal Pro-B-Type Natriuretic Peptide for Diagnosis and Prognosis in Patients With Renal Dysfunction: a systematic review and meta-analysis. JACC Heart Fail 2015;3:977–89. 10.1016/j.jchf.2015.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Tsutamoto T, Kawahara C, Yamaji M, et al. Relationship between renal function and serum cardiac troponin T in patients with chronic heart failure. Eur J Heart Fail 2009;11:653–8. 10.1093/eurjhf/hfp072 [DOI] [PubMed] [Google Scholar]
- 78. Aronson D, Abassi Z, Allon E, et al. Fluid loss, venous congestion, and worsening renal function in acute decompensated heart failure. Eur J Heart Fail 2013;15:637–43. 10.1093/eurjhf/hft036 [DOI] [PubMed] [Google Scholar]
- 79. Shirakabe A, Hata N, Kobayashi N, et al. Worsening renal function definition is insufficient for evaluating acute renal failure in acute heart failure. ESC Heart Fail 2018;5:322–31. 10.1002/ehf2.12264 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.