Abstract
Background
Nonspecific low back pain (NSLBP) accounts for a large proportion of low back pain cases. The present study aimed to investigate the effect of the whole-body vibration (WBV) exercise on lumbar proprioception in NSLBP patients. It was hypothesized that WBV exercise enhances lumbar proprioception.
Material/Methods
Forty-two patients with NSLBP performed an exercise program 3 times a week for a total of 12 weeks of WBV. The lumbar proprioception was measured by joint position sense. Outcomes were lumbar angle deviation and visual analogue scale (VAS) score.
Results
After the 12-week WBV exercise, lumbar flexion angle deviation was reduced from 3.65±2.26° to 1.90±1.07° (P=0.0001), and extension angle deviation was reduced from 3.06±1.85° to 1.61±0.75° (P=0.0001), significantly lower than baseline. After participating in the 12-week WBV exercise, a significant pain reduction was observed (P=0.0001). Men in the whole group (n=32) indicated significantly lower angle deviations in flexion and extension, whereas women (n=10) indicated significantly lower flexion angle deviation (P=0.037), and no significant difference was found in extension angle deviation (P=0.052). However, by subdividing the entire group (n=42) into poor and good proprioceptive groups, WBV exercise presented significant enhancement of lumbar proprioceptive ability in the poor flexion proprioception subgroup, poor extension proprioception subgroup, and good extension proprioception subgroup (each P=0.0001), but not in the subgroup with good flexion proprioceptive ability (P=0.165).
Conclusions
Lumbar flexion and extension proprioception as measured by joint position sense was significantly enhanced and pain was significantly reduced after 12-week WBV exercise in NSLBP patients. However, the patients with good flexion proprioceptive ability had limited proprioceptive enhancement.
MeSH Keywords: Chronic Pain, Low Back Pain, Proprioception, Exercise, Vibration
Background
Low back pain (LBP), as a symptom rather than a disease, like headache and dizziness [1], is one of the most prevalent and expensive musculoskeletal conditions [2]. LBP is a leading cause of years lived with disability, which increased by 54% between 1990 and 2015, with the biggest increase seen in low-income and middle-income countries [3]. The prevalence increased by 18% from 2006 to 2016 [4], and its lifetime prevalence was reported to be 84% [5]. Nonspecific low back pain (NSLBP) accounts for a large proportion of LBP cases (commonly cited as 90%) [6], which is LBP with an unrecognizable, unknown specific pathology (e.g., radicular syndrome, cauda equina syndrome, fracture, infection, osteoporosis, structural deformity, inflammatory disorder, or tumor) [1]. The pathogenesis of NSLBP is not fully understood [5]. Clinicians and patients were recommended by the American College of Physicians to select nonpharmacologic treatment [7] with exercise [8], multidisciplinary rehabilitation [9], electrical therapies [10], and magnetic therapy [11] to reduce pain and its consequences.
NSLBP patients showed an impaired proprioception compared with healthy controls [12–14]. Proprioceptive sense, by definition, is a result of the central processing by the central nervous system of afferent information about joint position, joint force, and joint movement from various mechanoreceptors in muscle spindles, Golgi tendon organ, and the fibrous membrane in joint capsules [15]. Proprioception has been shown to be a key component of motor control and joint stability during daily activities [16], and also coordinates movement and affects injury risk during sports [17]. Lumbar instability also restricts muscle strength, endurance, and flexibility [18] and makes recurrence of LBP more likely [19]. Hence, impaired proprioception affects normal coordinated movement. Decreased lumbar proprioception may lead to higher sports injury risk, an increase in pain intensity, and lumbar disability. A negative correlation between lumbar proprioception and pain was described in our previous study [20].
In recent years, whole-body vibration (WBV) exercise has increased in popularity in pain relief and physical performance in various clinical populations [21–24]. Conditions that have been studied include anterior cruciate ligament reconstruction [25], osteoporosis [26], fibromyalgia syndrome [27], overweight/obesity [28], cerebral palsy [29], post-stroke [30], and chronic NSLBP [31]. WBV requires the individual to perform static or steadily controlled exercises on an oscillating platform [32,33]. WBV improves muscle function through increased reflexive activity from the stimulation of the muscle spindle system [25] and also from increased corticomotor excitability [34]. This mechanism has also been suggested to reduce LBP, which has been previously shown to be associated with reduced lumbar segmental stabilization muscle activity. WBV increases reflexive activity and subsequently strengthens lumbar segmental muscles to alleviate LBP [35,36]. WBV with high vibration levels increase the risk of LBP [37], but frequencies below 20 Hz induces muscle relaxation and alleviates LBP caused by paravertebral muscle spasm [38]. Some additional benefits of WBV exercise are decreased heart rate and blood pressure [28,39], as well as improved cardiac autonomic function [40] and anti-inflammatory status [41]. These benefits assist overall health to mitigate the risk of LBP. Another appealing characteristic of WBV exercise is its suitability for someone unable to perform strenuous exercise modalities.
Proprioception is one of several objective measures used to determine the effectiveness of WBV exercise on NSLBP. Although proprioceptive sense plays an essential part in joint stability and injury prevention [42], few studies have investigated the effect of WBV exercise on lumbar proprioception among NSLBP patients, and the effect of WBV exercise on other segment proprioception is also unclear. Several studies demonstrated that a single session of WBV does not influence knee joint proprioception [43] and lumbar repositioning ability [44] in normal individuals. However, Myung-Sook et al. found that 3 weeks of WBV training was effective in improving ankle joint position sense (JPS) in children with cerebral palsy [29]. Hence, WBV exercise may have positive effects on proprioception after several weeks of training. Regarding the effect of WBV exercise in NSLBP patients, WBV training was reported to have significant positive effects on functional capacity (evaluating by the Roland and Morris disability questionnaire score, the Oswestry Disability Index, and the quality of life questionnaire SF-36) [45], balance ability, and pain of NSLBP patients [46]. However, research on the effect of WBV exercise on lumbar proprioception is lacking. The positive influence of WBV exercise on lumbar proprioception and alleviation of pain would be beneficial for NSLBP patients. NSLBP patients with poor proprioception might also benefit from the WBV training program.
The purpose of the present study was to determine the effect of WBV exercise on lumbar proprioception and pain control in NSLBP patients. We hypothesized that WBV exercise would enhance lumbar proprioception and reduce pain, and that patients with poor proprioceptive sense would get more clinical benefit from WBV exercise.
Material and Methods
The study had a one-group pretest-posttest design and was approved by the Ethics Committee of the Shanghai University of Sports, China, and by the Chinese Clinical Trial Registry (registry number ChiCTR-TRC-13003708). All participants signed written informed consent.
Sample size
GPower 3.1.9.2 was used for power calculation. Previous studies reported effect sizes (Cohen’s d) of −0.85 by investigating WBV effects on VAS in elderly individuals [47]. Therefore, to conduct a paired-samples t test, with an alpha of 0.05 (2-tailed), power of 0.9, and an effect size of 0.85, the estimated sample size was 17 participants. With an attrition rate of 20%, the sample size required for the study was 21 participants.
Participants
A total of 42 individuals participated in this study. All subjects underwent x-ray and MRI to exclude specific low back pain, and the clinician performed lumbar function tests assessing lumbar flexion, extension, and rotation. Inclusion criteria were: 18–35 years of age, low back pain persisting for approximately 12 weeks or longer, and at least 3 episodes. Exclusion criteria were: taking analgesic and/or anti-inflammatory agent, previous major trauma and/or surgery of the spine, serious spinal pathology (vertebral fracture, inflammatory arthropathy, spondylolisthesis, rheumatic diseases, cauda equina syndrome, tumor or cancer), cardiovascular and/or neurological disorders, insufficiently treated hypertension, acute inflammation of the musculoskeletal system, and pregnancy. The doctor excluded specific low back pain patients by taking their history, performing a physical examination, and laboratory testing. Participants were asked not to change their daily lifestyle and or to perform additional physical therapy during the study period.
Procedure
This was a longitudinal study investigating the effect of WBV exercise in NSLBP patients (Figure 1). Each participant performed exercises 3 times a week for a total of 12 weeks, and the sessions could not be performed on consecutive days. Each training session consisted of 5 min of warm-up, 18 min of WBV, and 5 min of cool-down exercises. Lumbar joint position sense (an indirect measurement of proprioception) and the visual analogue scale (VAS) scores were recorded before and 12 weeks after WBV exercise.
Figure 1.
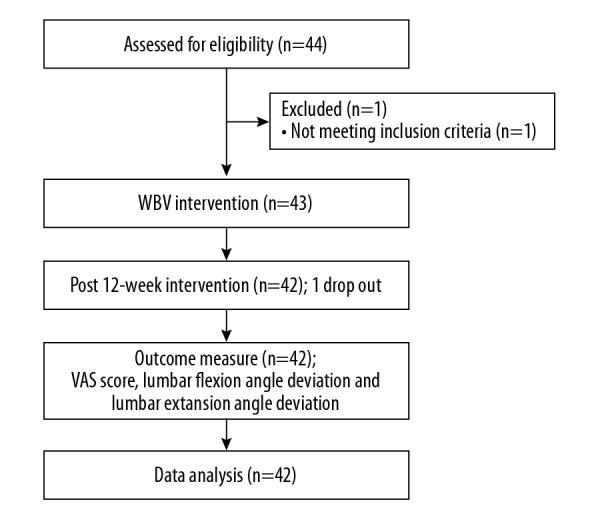
Flowchart of the study. WBV, whole-body vibration; VAS, visual analogue scale, was used to assess pain intensity.
Intervention
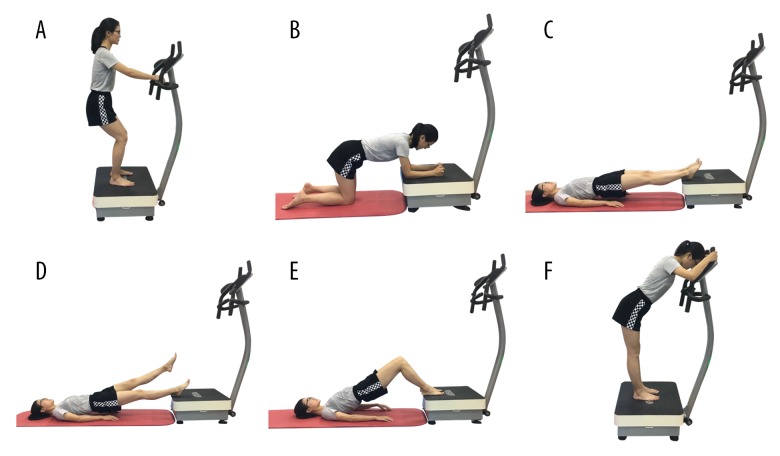
All exercises were performed on a vertical vibration instrument (AV001; BODYGREEN, Taiwan, China). Participants were asked to take off their shoes to avoid slowing vibrations on the human body. WBV exercise contains 6 exercise postures: squat, kneeling, bridge, bridge with leg lift, bridge and knee flex, and back release. Postures were maintained for 60 s, except for squat, which was maintained for 90 s, and repeated twice with 30 s of rest. In clinical practice, these postures are widely used and are safe for patients with LBP. The vibration frequency was 9 Hz, and the amplitude was 2 mm. Figure 2 and Table 1 display more detailed information about the WBV exercise protocol. WBV exercises were completed under the supervision of registered physical therapists.
Figure 2.
Training program for whole-body vibration exercise. Training program included: (A) squat, (B) kneeling, (C) bridge, (D) bridge with leg lift, (E) bridge and knee flex, and (F) back release.
Table 1.
Parameters and intensity of whole-body vibration exercise.
| Exercise program | Each time (s) | Repetitions (n) | Frequency (Hz) | Rest interval (s) | WBV total time (s) |
|---|---|---|---|---|---|
| Squat | 90 | 2 | 9 | 30 | 180 |
| Kneeling | 60 | 2 | 9 | 30 | 120 |
| Bridge | 60 | 2 | 9 | 30 | 180 |
| Bridge with leg lift | 60 | 2 | 9 | 30 | 120 |
| Bridge and knee flex | 60 | 2 | 9 | 30 | 120 |
| Back release | 60 | 2 | 9 | 30 | 180 |
Measurement
Lumbar joint position sense
Lumbar joint position sense (JPS), an indirect measure of proprioceptive sense, was evaluated before the WBV exercise and after the 12-week WBV exercise by using Con-Trex Multi-Joint System (CMV AG, Dübendorf, Switzerland).
In the measurement setup, participants stood in neutral position, and were asked to wear a blinder and earplugs to remove visual and auditory disturbance. From the starting neutral standing position, the trunk of the participant was passively flexed to a random predetermined target angle in constant-velocity mode. Participants were instructed to relax their bodies and avoid any active muscle contraction when bending the trunk to the target angle. Participants maintained the target angle for 3 s to memorize the position. Then, the participants returned passively to the starting position. Subsequently, a hand-held trigger was given to participants and were instructed to return to the target position from the neutral position. Upon pressing the pause button on the trigger, the investigator recorded the actual angle. The process was repeated for total of 6 times in series (3 times for lumbar flexion and 3 times for lumbar extension). The absolute error angles, which deviated from the actual angle to the target angle, were calculated and taken as an average for lumbar flexion and extension, which is also the angle deviation. The larger value of absolute error value angle indicated inferiority in lumbar joint position sense, thereby indicating worse proprioceptive acuity.
Before this study, we did a pilot study to determine the reliability of the Con-Trex Multi-Joint lumbar testing system. Twenty-five NSLBP patients participated in the pilot study. All subjects’ lumbar proprioception was tested by the above procedures, and performed the same test after 2 days. The re-test reliability was calculated by intraclass correlation coefficient (ICC). ICC value ranges between 0 and 1 and can be interpreted as excellent: ≥0.75, good: 0.60–0.74, fair: 0.40–0.59, or poor: <0.4 [48]. We found the above procedures had good reliability (flexion angle deviation: 3.33±1.82° for first test, 3.22±1.22° for re-test, ICC=0.766; extension angle deviation: 2.78±1.47° for first test, 3.08±0.78° for re-test, ICC=0.719) [49].
Pain intensity
The visual analogue scale (VAS) was used to assess pain intensity, which used a 100-mm horizontal line marked from 0 to 10 from left to right, in which “0” meant no pain and “10” meant the worst pain imaginable. Participants specify their pain intensity by indicating a position between 2 end-points along a continuous line. The minimal clinically important difference (MCID), identified as a change of 2 or more points [50], was also used to evaluate the therapeutic effect after 12-week WBV training.
Statistical analysis
Microsoft Excel 2016 and SPSS 20.0 were used for data logging and statistical analysis. Demographic data were collected for descriptive statistics, which are described as mean ± standard deviation (SD).
The paired-samples t test was used to compare lumbar angle deviations and VAS scores before and after WBV exercise. The changes in lumbar angle deviations and VAS score were also calculated, and a negative difference meant that the participant had improvement in proprioception and pain intensity after WBV intervention. Then, using the baseline lumbar angle deviation value as the reference value, the group of 42 participants were divided into 2 proprioceptive subgroups (good and poor). In the good proprioceptive subgroup, participant whose lumbar angle deviations were below the group mean before WBV exercise were included. Participants whose lumbar angle deviation above the group mean were included in the poor proprioceptive subgroup. The same analysis via paired-samples t test was utilized for the 2 subgroups. The same approach was used for VAS subgroups. The good VAS subgroup included participants with VAS scores lower than the group mean before WBV exercise, and the poor VAS subgroup contained participants with higher VAS score. The level of significance was set at 0.05. Treatment effect was calculated by comparing the differences in outcome measured over the 12-week training program.
Lastly, odds ratio and the corresponding 95% confidence intervals were estimated to assess the differences between subgroups for perceived benefit of WBV exercise (gender, pain intensity, and lumbar proprioception above the MCID). In addition, chi-square tests were also used to determine whether there was a difference between the subgroups in the proportion of participants reporting perceived benefits.
Results
Forty-two NSLBP patients aged 18–34 years old (average age 21.6±3.0 years old; 32 males and 10 females) voluntary participated in this study. Other baseline demographic and clinical characteristics of participants are shown in Table 2.
Table 2.
Demographic and clinical characteristics of participants (n=42).
| Men (n=32) | Women (n=10) | Total (n=42) | |
|---|---|---|---|
| Age (y) | 21.9±3.2 | 20.5±2.0 | 21.6±3.0 |
| Height (cm) | 171.50±6.53 | 173.90±6.57 | 172.07±6.54 |
| Weight (kg) | 67.75±10.66 | 67.20±12.50 | 67.62±10.96 |
| BMI (kg/m2) | 22.91±2.41 | 22.14±3.33 | 22.73±2.64 |
| Time since first experience with NSLBP (mo) | 9.2±3.6 | 6.8±1.87 | 8.6±3.4 |
| VAS-baseline | 4.47±1.27 | 5.10±0.99 | 4.62±1.23 |
| Flexion angle deviation-baseline | 3.79±2.37 | 3.18±1.90 | 3.65±2.26 |
| Extension angle deviation- baseline | 3.21±1.94 | 2.57±1.52 | 3.06±1.85 |
BMI – body mass index (calculated as weight in kilograms divided by height in meters squared); NSLBP – nonspecific low back pain; VAS – visual analogue scale. Values are expressed as mean ±SD.
Proprioception
After the 12-week WBV exercise program, lumbar flexion angle deviation was reduced from 3.65±2.26° to 1.90±1.07° (P=0.0001) and extension angle deviation was reduced from 3.06±1.85° to 1.61±0.75° (P=0.0001), which were significantly lower than baseline (Table 3).
Table 3.
Comparison of lumbar angle deviation and VAS score between baseline and after 12-week WBV exercise.
| Baseline | 12 weeks | Mean change from baseline to 12 weeks (95% CI) | % change | P value# | Effect size | |
|---|---|---|---|---|---|---|
| Whole group (n=42) | ||||||
| Flexion angle deviation (°) | 3.65±2.26 | 1.90±1.07 | −1.75 (−2.48 to −1.01) | −26.4±57.5 | 0.0001* | 0.75 |
| Subgroup <3.65° (good flexion proprioception; n=23) (°) | 2.10±0.88 | 1.76±0.89 | −0.34 (−0.82 to 0.15) | 0.6±61.3 | 0.165 | 0.30 |
| Subgroup >3.65° (poor flexion proprioception; n=19) (°) | 5.52±1.98 | 2.06±1.26 | −3.45 (−4.57 to −2.34) | −59.1±29.5 | 0.0001* | 1.49 |
| Men (flexion proprioception; n=32) (°) | 3.79±2.37 | 1.98±1.11 | −1.81 (−2.70 to −0.92) | −30.0±48.4 | 0.0001* | 0.73 |
| Women (flexion proprioception; n=10) (°) | 3.18±1.90 | 1.63±0.92 | −1.54 (−2.97 to −0.12) | −14.9±82.4 | 0.037* | 1.77 |
| Extension angle deviation (°) | 3.06±1.85 | 1.61±0.75 | −1.44 (−1.98 to −0.90) | −35.9±27.9 | 0.0001* | 0.83 |
| Subgroup <3.06° (good extension proprioception; n=26) (°) | 1.90±0.74 | 1.46±0.67 | −0.43 (−0.62 to −0.25) | −21.7±20.2 | 0.0001* | 0.93 |
| Subgroup >3.06° (poor extension proprioception; n=16) (°) | 4.94±1.52 | 1.86±0.84 | −3.08 (−4.05 to −2.12) | −58.9±23.1 | 0.0001* | 1.70 |
| Men (extension proprioception; n=32) (°) | 3.21±1.94 | 1.64±0.73 | −1.56 (−2.22 to −0.91) | −37.4±27.5 | 0.0001* | 0.86 |
| Women (extension proprioception; n=10) (°) | 2.57±1.52 | 1.52±0.87 | −1.05 (−2.12 to 0.01) | −31.1±30.1 | 0.052 | 0.71 |
| VAS | 4.62±1.23 | 3.00±1.38 | −1.62 (−2.14 to −1.10) | −28.3±47.9 | 0.0001* | 0.96 |
| Subgroup <4.62 (good VAS; n=21) | 3.67±0.73 | 2.86±1.11 | −0.81 (−1.43 to −0.188) | −13.1±57.8 | 0.013* | 0.59 |
| Subgroup >4.62 (poor VAS; n=21) | 5.57±0.81 | 3.14±1.62 | −2.43 (−3.16 to −1.70) | −43.6±29.8 | 0.0001* | 1.52 |
| Men (VAS; n=32) | 4.47±1.27 | 3.03±1.12 | −1.44 (−2.02 to −0.85) | −23.3±50.6 | 0.0001* | 0.88 |
| Women (VAS; n=10) | 5.10±0.99 | 2.90±2.08 | −2.20 (−3.50 to −0.90) | −44.5±35.5 | 0.004* | 1.21 |
VAS – visual analogue scale; Values are expressed as mean ±SD;
analyzed by the paired-sample t test;
significant at P<0.05.
The whole group was subdivided into good or poor flexion proprioceptive groups according to baseline values. A total of 19 participants showing flexion angle deviations above 3.65° (group mean value) were included in the poor flexion proprioceptive group, and 23 participants showing lumbar flexion angle deviations below 3.65° were included in the good flexion proprioceptive group. For the subgroup with poor flexion proprioception, the difference in lumbar flexion angle deviation significantly decreased after WBV intervention (P=0.0001). No significant difference was found in the good flexion proprioceptive group (P=0.165). For extension proprioception, 16 participants were included in the poor extension proprioceptive group (extension angle deviations above the group mean value of 3.06°), and 26 participants were included in the good extension proprioceptive group. Both subgroups showed significant improvement in extension proprioception after WBV exercise (poor extension proprioceptive group: P=0.0001, good extension proprioceptive group: P=0.0001).
After WBV exercise, men in the whole group (n=32) had significantly lower flexion and extension angle deviations (flexion angle deviation: P=0.0001, extension angle deviation: P=0.0001) after intervention. However, women (n=10) had significant lower flexion angle deviation (P=0.037), but showed no significant difference in extension angle deviation (P=0.052).
VAS
At baseline, the mean VAS value was 4.62±1.23, and participants had significant pain reduction after the 12-week WBV exercise program (VAS value: 3.00±1.38, P=0.0001). The poor VAS subgroup, containing 21 participants, had VAS values that were higher than the group mean value of 4.62. Correspondingly, 21 participants were in the good VAS group. For both subgroups, WBV exercise significantly reduced VAS scores (poor VAS: P=0.0001, good VAS: P=0.013). At baseline, the mean VAS value was 4.47±1.27 for males in the whole group (n=32) and 5.10±0.99 for women (n=10). After the 12-week WBV exercise program, the mean VAS value was significantly reduced to 3.03±1.12 for men (P=0.0001) and 2.90±2.08 for women (P=0.004) (Table 3).
MCID in gender, proprioception, and pain intensity
Participants with poor VAS reported significantly greater benefits from WBV exercise compared to participants with good VAS (P=0.001). No significant differences between subgroups were found for gender, flexion proprioception, or extension proprioception, in relation to the proportion of participants who attained MCID (Table 4).
Table 4.
Number and proportion of participants having a minimal clinically important change in gender, proprioception, and pain intensity after 12-week intervention.
| Subgroups | MCID | Odds ratio (CI 95%) | P value# | |
|---|---|---|---|---|
| Benefit; n (%) | No benefit; n (%) | |||
| Gender | 0.221 (0.040 to 1.205) | 0.066 | ||
| Men | 15 (46.9%) | 17 (53.1%) | ||
| Women | 8 (80.0%) | 2 (20.0%) | ||
| Flexion proprioception | 0.793 (0.233 to 2.699) | 0.711 | ||
| Good flexion proprioception | 12 (52.2%) | 11 (47.8%) | ||
| Poor flexion proprioception | 11 (57.9%) | 8 (42.1%) | ||
| Extension proprioception | 0.907 (0.259 to 3.177) | 0.879 | ||
| Good extension proprioception | 14 (53.8%) | 12 (46.2%) | ||
| Poor extension proprioception | 9 (56.2%) | 7 (43.8%) | ||
| Pain intensity | 0.094 (0.022 to 0.398) | 0.001* | ||
| Good VAS | 6 (28.6%) | 15 (71.4%) | ||
| Poor VAS | 17 (81.0%) | 4 (19.0%) | ||
MCID – minimal clinically importance difference, identified as a change of 2 or more VAS points to evaluate the therapeutic effect after 12-week whole-body vibration training; VAS – visual analogue scale; CI – confidence interval;
significant at P<0.05;
analyzed by chi-squared test.
Discussion
WBV, which is a noninvasive intervention, has become an increasingly popular treatment for LBP. To investigate whether the proprioceptive performance of NSLBP patients can be improved by WBV exercise, the effect of WBV exercise on lumbar proprioception and pain control in NSLBP patients was examined. The present findings showed a significant difference in lumbar angle deviation change and VAS change after WBV exercise (flexion proprioception: P=0.0001, extension proprioception: P=0.0001, VAS: P=0.001). These results provide a possible explanation as to why a 12-week WBV program relieved pain and improved function for patients with chronic nonspecific low back pain in previous studies [47,51,52]. These positive effects might be an increase in proprioception of the lumbopelvic area, which improved the outcome of muscle co-ordination.
Categorizing the data at baseline into good and poor flexion proprioception revealed that WBV exercise significantly decreased the lumbar flexion angle deviation of NSLBP participants whose lumbar flexion angle deviation value was more than 3.65° (P=0.0001). WBV improved the flexion performance of those NSLBP patients classified into the poor flexion proprioception group (n=19). Conversely, WBV had no noticeable effect on flexion proprioception of participants with good flexion proprioception (n=23, lumbar flexion angle deviation was less than 3.65°). The findings of Hosp et al. [53] and Callaghan et al. [54] indirectly support these observations, as they demonstrated that healthy participants whose knee proprioception was graded as good did not benefit from the intervention.
In our previous cross-sectional study, we found that decreased lumbar muscle strength, endurance, and lumbar proprioception of the lumbar vertebra lead to an increase in pain intensity and lumbar disability [20]. Therefore, we hypothesized that patients with poor proprioceptive sense might have more clinical benefit from performing WBV exercises. Clinical benefit was measured by minimal clinically important difference (MCID), defined as a change of 2 or more VAS points [50] after the intervention. However, results of the present study do not confirm this hypothesis. No significant differences between subgroups were found in flexion proprioception or extension proprioception in relation to the proportion of participants who attained MCID. However, an increased proportion of participants with poor VAS perceived a benefit in their clinical symptoms after the 12-week WBV intervention. Combined with the above results showing that WBV exercise decreased lumbar angle deviation significantly for NSLBP patients with poor proprioception, this finding indicated that NSLBP patients with severe pain and poor proprioception might be more suitable for WBV intervention.
Considering the gender factor, WBV showed a demonstrable effect on flexion proprioception but not extension proprioception for women in the whole group. Correspondingly, WBV showed a demonstrable effect on proprioception for men in both flexion and extension in the whole group (both P=0.0001). Few studies have reported on gender differences for NSLBP patients in lumbar proprioception based on WBV intervention. Ye et al. found that women were less sensitive than men in lumbar extensor endurance for WBV exposure [55]. Lumbar muscles in women have a higher proportion of cross-sectional area of type I fibers than men (73% and 56%, respectively) [56]. Type Iα afferent activities increased after vibration training, and type II afferents were also sensitive to vibration, especially when muscle contraction occurs. Because recruitment of type Iα afferents would precede that of type II afferents with somatosensory and perceptual stimulations, type II afferent fibers were used as elements to activate proprioception [57]. Women had a higher proportion of type Iα afferents fibers. Consequently, WBV training for women with NSLBP induced lower activations of type II afferent fibers, thereby resulting in relatively less improvement in proprioception. This is in line with the current findings.
Recently, a number of studies have reported that the LBP incidence in children and young adults is similar to that in adults [58–61], and even the lifetime prevalence rates increase with the age of the subjects [62]. Physically heavy work at a young age [63], psychological distress during childhood [64], and abdominal obesity [65] have been found to be the main risk factor for low back pain, not only during childhood, but also in early adulthood. Lifestyle-factors such as smoking, alcohol consumption, and overweight are was positively associated with LBP [66].
A meta-analysis of surgical versus nonsurgical treatment of chronic low back pain (CLBP) suggested that nonsurgical treatment was slightly more effective, feasible, and safe [67]. Nonsurgical physical therapies like low-level laser therapy [68], magnetic therapy [11], electrical therapies [10], extracorporeal shockwave therapy [69], and high-intensity laser therapy [70] have a favorable effect on self-reported pain and functional limitations on NSLBP. These results are in line with our study, but no previous study has reported on the effect of proprioception on the lumbopelvic area.
The present study contains certain limitations. First of all, our age range was narrow and the sample was small. All participants were young individuals, and the average age was 21.6 years old (range: 18–34 years old). Thus, these results did not represent the condition of the entire population. Furthermore, proprioceptive senses included position sense, motion perception, and vibration sensation; however, this study only tested position reproduction, particularly position sense. Given that the sense of joint movement and vibration was difficult to quantify under the conditions in the present study, the effort to improve accuracy and comprehensiveness of proprioceptive sensation testing is another important research field. Our findings are based on a single-group pre-post test design without a control group, which increases the risk of bias, and the lack of follow-up observations is another limitation. Future studies involving a control group and long-term follow-up observation are needed to ensure that the improvements we demonstrated are due to the whole-body vibration exercise, thereby strengthening the validity and credibility our study findings. Furthermore, it would be useful to evaluate the effect on lumbopelvic proprioception and pain control of different training approaches.
Conclusions
Lumbar flexion and extension proprioception, as measured by joint position sense, were enhanced significantly, and pain was also significantly reduced in NSLBP patients after completing the 12-week WBV exercise program. However, patients with good flexion proprioceptive ability had limited proprioceptive enhancement.
Abbreviations
- NSLBP
nonspecific low back pain
- WBV
whole-body vibration
- VAS
visual analogue scale
- LBP
low back pain
- JPS
joint position sense
- ChiCTR
Chinese Clinical Trial Registry
- ICC
intraclass correlation coefficient
- MCID
the minimal clinically important difference
- SD
standard deviation
- CLBP
chronic low back pain
- MCE
motor control exercise
Footnotes
Source of support: The National Natural Science Foundation of China (81501956, 81871844); Fok Ying-Tong Education Foundation of China (161092); Shanghai Municipal Commission of Health and Family Planning (201840346); Shanghai Key Lab of Human Performance (Shanghai University of Sport) (no: 11DZ2261100); “Shu Guang” project supported by Shanghai Municipal Education Commission and Shanghai Education Development Foundation
Conflicts of interest
None.
References
- 1.Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet (London, England) 2017;389(10070):736–47. doi: 10.1016/S0140-6736(16)30970-9. [DOI] [PubMed] [Google Scholar]
- 2.Luedtke K, Rushton A, Wright C, et al. Effectiveness of transcranial direct current stimulation preceding cognitive behavioural management for chronic low back pain: Sham controlled double blinded randomised controlled trial. BMJ. 2015;350(apr16 1):h1640. doi: 10.1136/bmj.h1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet (London, England) 2018;391(10137):2356–67. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 4.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England) 2017;390:1211–59. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet (London, England) 2012;379:482–91. doi: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 6.Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332:1430–34. doi: 10.1136/bmj.332.7555.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline From the American College of Physicians. Ann Intern Med. 2017;166(7):514–30. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 8.Shiri R, Coggon D, Falah-Hassani K. Exercise for the prevention of low back pain: systematic review and meta-analysis of controlled trials. Am J Epidemiol. 2018;187(5):1093–101. doi: 10.1093/aje/kwx337. [DOI] [PubMed] [Google Scholar]
- 9.Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: A systematic review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2017;166(7):493–505. doi: 10.7326/M16-2459. [DOI] [PubMed] [Google Scholar]
- 10.Rajfur J, Pasternok M, Rajfur K, et al. Efficacy of selected electrical therapies on chronic low back pain: A comparative clinical pilot study. Med Sci Monit. 2017;23:85–100. doi: 10.12659/MSM.899461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taradaj J, Ozon M, Dymarek R, et al. Impact of selected magnetic fields on the therapeutic effect in patients with lumbar discopathy: A prospective, randomized, single-blinded, and placebo-controlled clinical trial. Adv Clin Exp Med. 2018;27(5):649–66. doi: 10.17219/acem/68690. [DOI] [PubMed] [Google Scholar]
- 12.Lee AS, Cholewicki J, Reeves NP, et al. Comparison of trunk proprioception between patients with low back pain and healthy controls. Arch Phys Med Rehabil. 2010;91(9):1327–31. doi: 10.1016/j.apmr.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Willigenburg NW, Kingma I, Hoozemans MJ, van Dieen JH. Precision control of trunk movement in low back pain patients. Hum Mov Sci. 2013;32(1):228–39. doi: 10.1016/j.humov.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Janssens L, McConnell AK, Pijnenburg M, et al. Inspiratory muscle training affects proprioceptive use and low back pain. Med Sci Sports Exerc. 2015;47(1):12–19. doi: 10.1249/MSS.0000000000000385. [DOI] [PubMed] [Google Scholar]
- 15.Riemann BL, Lephart SM. The sensorimotor system, Part I: The physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71–79. [PMC free article] [PubMed] [Google Scholar]
- 16.Salles JI, Velasques B, Cossich V, et al. Strength training and shoulder proprioception. J Athl Train. 2015;50(3):277–80. doi: 10.4085/1062-6050-49.3.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: A systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2014;48(11):871–77. doi: 10.1136/bjsports-2013-092538. [DOI] [PubMed] [Google Scholar]
- 18.Cho HY, Kim EH, Kim J. Effects of the CORE exercise program on pain and active range of motion in patients with chronic low back pain. J Phys Ther Sci. 2014;26(8):1237–40. doi: 10.1589/jpts.26.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bae CR, Jin Y, Yoon BC, et al. Effects of assisted sit-up exercise compared to core stabilization exercise on patients with non-specific low back pain: A randomized controlled trial. J Back Musculoskelet Rehabil. :2018. doi: 10.3233/BMR-170997. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Hu H, Zheng Y, Wang X, et al. Correlations between lumbar neuromuscular function and pain, lumbar disability in patients with nonspecific low back pain: A cross-sectional study. Medicine. 2017;96(36):e7991. doi: 10.1097/MD.0000000000007991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matutellorente Á, Gonzálezagüero A, Gómezcabello A, et al. Effect of whole-body vibration therapy on health-related physical fitness in children and adolescents with disabilities: A systematic review. J Adolesc Health. 2014;54(4):385–96. doi: 10.1016/j.jadohealth.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Lai CC, Tu YK, Wang TG, et al. Effects of resistance training, endurance training and whole-body vibration on lean body mass, muscle strength and physical performance in older people: A systematic review and network meta-analysis. Age Ageing. 2018;47(3):367–73. doi: 10.1093/ageing/afy009. [DOI] [PubMed] [Google Scholar]
- 23.Kurt C, Pekunlu E. Acute effect of whole body vibration on isometric strength, squat jump, and flexibility in well-trained combat athletes. Biol Sport. 2015;32(2):115–22. doi: 10.5604/20831862.1134558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee J, Lee K, Song C. Determining the posture and vibration frequency that maximize pelvic floor muscle activity during whole-body vibration. Med Sci Monit. 2016;22:4030–36. doi: 10.12659/MSM.898011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pamukoff DN, Pietrosimone B, Ryan ED, et al. Whole-body vibration improves early rate of torque development in individuals with anterior cruciate ligament reconstruction. J Strength Cond Res. 2017;31(11):2992–3000. doi: 10.1519/JSC.0000000000001740. [DOI] [PubMed] [Google Scholar]
- 26.Pamukoff DN, Pietrosimone B, Lewek MD, et al. Whole-body and local muscle vibration immediately improve quadriceps function in individuals with anterior cruciate ligament reconstruction. Arch Phys Med Rehabil. 2016;97(7):1121–29. doi: 10.1016/j.apmr.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 27.Alentorn-Geli E, Padilla J, Moras G, et al. Six weeks of whole-body vibration exercise improves pain and fatigue in women with fibromyalgia. J Altern Complement Med. 2008;14(8):975–81. doi: 10.1089/acm.2008.0050. [DOI] [PubMed] [Google Scholar]
- 28.Figueroa A, Gil R, Wong A, et al. Whole-body vibration training reduces arterial stiffness, blood pressure and sympathovagal balance in young overweight/obese women. Hypertens Res. 2012;35(6):667–72. doi: 10.1038/hr.2012.15. [DOI] [PubMed] [Google Scholar]
- 29.Ko MS, Sim YJ, Kim DH, Jeon HS. Effects of three weeks of whole-body vibration training on joint-position sense, balance, and gait in children with cerebral palsy: A randomized controlled study. Physiother Can. 2016;68(2):99–105. doi: 10.3138/ptc.2014-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi W, Han D, Kim J, Lee S. Whole-body vibration combined with treadmill training improves walking performance in post-stroke patients: a randomized controlled trial. Med Sci Monit. 2017;23:4918–25. doi: 10.12659/MSM.904474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palmer KT, Harris CE, Griffin MJ, et al. Case-control study of low-back pain referred for magnetic resonance imaging, with special focus on whole-body vibration. Scand J Work Environ Health. 2008;34(5):364–73. doi: 10.5271/sjweh.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chung P, Liu C, Wang H, et al. Various performance-enhancing effects from the same intensity of whole-body vibration training. J Sport Health Sci. 2017;6(3):333–39. doi: 10.1016/j.jshs.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang WW, Chou LW, Chen WH, et al. Dual-frequency whole body vibration enhances vertical jumping and change-of-direction ability in rugby players. J Sport Health Sci. 2017;6(3):346–51. doi: 10.1016/j.jshs.2015.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pamukoff DN, Pietrosimone B, Lewek MD, et al. Immediate effect of vibratory stimuli on quadriceps function in healthy adults. Muscle Nerve. 2016;54(3):469–78. doi: 10.1002/mus.25081. [DOI] [PubMed] [Google Scholar]
- 35.Perraton L, Machotka Z, Kumar S. Whole-body vibration to treat low back pain: Fact or fad? Physiother Can. 2011;63(1):88–93. doi: 10.3138/ptc.2009.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang X-Q, Pi Y-L, Chen P-J, et al. Whole body vibration exercise for chronic low back pain: Study protocol for a single-blind randomized controlled trial. Trials. 2014;15:104. doi: 10.1186/1745-6215-15-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burstrom L, Nilsson T, Wahlstrom J. Whole-body vibration and the risk of low back pain and sciatica: A systematic review and meta-analysis. Int Arch Occup Environ Health. 2015;88(4):403–18. doi: 10.1007/s00420-014-0971-4. [DOI] [PubMed] [Google Scholar]
- 38.Rittweger J, Mutschelknauss M, Felsenberg D. Acute changes in neuromuscular excitability after exhaustive whole body vibration exercise as compared to exhaustion by squatting exercise. Clin Physiol Funct Imaging. 2003;23(2):81–86. doi: 10.1046/j.1475-097x.2003.00473.x. [DOI] [PubMed] [Google Scholar]
- 39.Figueroa A, Kalfon R, Madzima TA, Wong A. Whole-body vibration exercise training reduces arterial stiffness in postmenopausal women with prehypertension and hypertension. Menopause (New York, NY) 2014;21(2):131–36. doi: 10.1097/GME.0b013e318294528c. [DOI] [PubMed] [Google Scholar]
- 40.Alam MM, Khan AA, Farooq M. Effect of whole-body vibration on neuromuscular performance: A literature review. Work (Reading, Mass) 2018;59(4):571–83. doi: 10.3233/WOR-182699. [DOI] [PubMed] [Google Scholar]
- 41.Simao AP, Avelar NC, Tossige-Gomes R, et al. Functional performance and inflammatory cytokines after squat exercises and whole-body vibration in elderly individuals with knee osteoarthritis. Arch Phys Med Rehabil. 2012;93(10):1692–700. doi: 10.1016/j.apmr.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 42.Riva D, Bianchi R, Rocca F, Mamo C. Proprioceptive training and injury prevention in a professional men’s basketball team: A six-year prospective study. J Strength Cond Res. 2016;30(2):461–75. doi: 10.1519/JSC.0000000000001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hannah R, Minshull C, Folland JP. Whole-body vibration does not influence knee joint neuromuscular function or proprioception. Scand J Med Sci Sports. 2013;23(1):96–104. doi: 10.1111/j.1600-0838.2011.01361.x. [DOI] [PubMed] [Google Scholar]
- 44.Lee TY, Chow DH. Effects of whole body vibration on spinal proprioception in normal individuals. Conf Proc IEEE Eng Med Biol Soc. 2013;2013:4989–92. doi: 10.1109/EMBC.2013.6610668. [DOI] [PubMed] [Google Scholar]
- 45.Kaeding TS, Karch A, Schwarz R, et al. Whole-body vibration training as a workplace-based sports activity for employees with chronic low-back pain. Scand J Med Sci Sports. 2017;27(12):2027–39. doi: 10.1111/sms.12852. [DOI] [PubMed] [Google Scholar]
- 46.Yang J, Seo D. The effects of whole body vibration on static balance, spinal curvature, pain, and disability of patients with low back pain. J Phys Ther Sci. 2015;27(3):805–8. doi: 10.1589/jpts.27.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.del Pozo-Cruz B, Hernández Mocholí MA, Adsuar JC, et al. Effects of whole body vibration therapy on main outcome measures for chronic non-specific low back pain: a single-blind randomized controlled trial. J Rehabil Med. 2011;43(8):689–94. doi: 10.2340/16501977-0830. [DOI] [PubMed] [Google Scholar]
- 48.Cicchetti DV. Multiple comparison methods: Establishing guidelines for their valid application in neuropsychological research. J Clin Exp Neuropsychol. 1994;16(1):155–61. doi: 10.1080/01688639408402625. [DOI] [PubMed] [Google Scholar]
- 49.Chen B. Effect of whole body vibration for neuromuscular function in patients with chronic nonspecific low back pain [master’s thesis] Shanghia University of Sport; 2016. [Google Scholar]
- 50.Pires D, Cruz EB, Caeiro C. Aquatic exercise and pain neurophysiology education versus aquatic exercise alone for patients with chronic low back pain: A randomized controlled trial. Clin Rehabil. 2015;29(6):538–47. doi: 10.1177/0269215514549033. [DOI] [PubMed] [Google Scholar]
- 51.Kaeding TS, Karch A, Schwarz R, et al. Whole-body vibration training as a workplace-based sports activity for employees with chronic low-back pain. Scand J Med Sci Sports. 2017;27(12):2027–39. doi: 10.1111/sms.12852. [DOI] [PubMed] [Google Scholar]
- 52.Rittweger J, Just K, Kautzsch K, et al. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: A randomized controlled trial. Spine. 2002;27(17):1829–34. doi: 10.1097/00007632-200209010-00003. [DOI] [PubMed] [Google Scholar]
- 53.Hosp S, Bottoni G, Heinrich D, et al. A pilot study of the effect of Kinesiology tape on knee proprioception after physical activity in healthy women. J Sci Med Sport. 2015;18(6):709–13. doi: 10.1016/j.jsams.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 54.Callaghan MJ, Selfe J, Bagley PJ, Oldham JA. The effects of patellar taping on knee joint proprioception. J Athl Train. 2002;37(1):19–24. [PMC free article] [PubMed] [Google Scholar]
- 55.Ye J, Ng G, Yuen K. Acute effects of whole-body vibration on trunk muscle functioning in young healthy adults. J Strength Cond Res. 2014;28(10):2872–79. doi: 10.1519/JSC.0000000000000479. [DOI] [PubMed] [Google Scholar]
- 56.Thorstensson A, Carlson H. Fibre types in human lumbar back muscles. Acta Physiol Scand. 1987;131(2):195–202. doi: 10.1111/j.1748-1716.1987.tb08226.x. [DOI] [PubMed] [Google Scholar]
- 57.Cordo P, Gurfinkel VS, Bevan L, Kerr GK. Proprioceptive consequences of tendon vibration during movement. J Neurophysiol. 1995;74(4):1675–88. doi: 10.1152/jn.1995.74.4.1675. [DOI] [PubMed] [Google Scholar]
- 58.Trevelyan FC, Legg SJ. Risk factors associated with back pain in New Zealand school children. Ergonomics. 2011;54(3):257–62. doi: 10.1080/00140139.2010.547608. [DOI] [PubMed] [Google Scholar]
- 59.Murphy S, Buckle P, Stubbs D. A cross-sectional study of self-reported back and neck pain among English schoolchildren and associated physical and psychological risk factors. Appl Ergon. 2007;38(6):797–804. doi: 10.1016/j.apergo.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 60.Watson KD, Papageorgiou AC, Jones GT, et al. Low back pain in schoolchildren: occurrence and characteristics. Pain. 2002;97(1–2):87–92. doi: 10.1016/s0304-3959(02)00008-8. [DOI] [PubMed] [Google Scholar]
- 61.Coenen P, Smith A, Paananen M, et al. Trajectories of low back pain from adolescence to young adulthood. Arthritis Care Res (Hoboken) 2017;69(3):403–12. doi: 10.1002/acr.22949. [DOI] [PubMed] [Google Scholar]
- 62.Calvo-Munoz I, Gomez-Conesa A, Sanchez-Meca J. Prevalence of low back pain in children and adolescents: A meta-analysis. BMC Pediatrics. 2013;13:14. doi: 10.1186/1471-2431-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lallukka T, Viikari-Juntura E, Viikari J, et al. Early work-related physical exposures and low back pain in midlife: The Cardiovascular Risk in Young Finns Study. Occup Environ Med. 2017;74(3):163–68. doi: 10.1136/oemed-2016-103727. [DOI] [PubMed] [Google Scholar]
- 64.Kanchiku T, Suzuki H, Imajo Y, et al. Psychogenic low-back pain and hysterical paralysis in adolescence. Clin Spine Surg. 2017;30(8):E1122–25. doi: 10.1097/BSD.0000000000000264. [DOI] [PubMed] [Google Scholar]
- 65.Shiri R, Solovieva S, Husgafvel-Pursiainen K, et al. The association between obesity and the prevalence of low back pain in young adults: The Cardiovascular Risk in Young Finns Study. Am J Epidemiol. 2008;167(9):1110–19. doi: 10.1093/aje/kwn007. [DOI] [PubMed] [Google Scholar]
- 66.Hestbaek L, Leboeuf-Yde C, Kyvik KO. Are lifestyle-factors in adolescence predictors for adult low back pain? A cross-sectional and prospective study of young twins. BMC Musculoskeletal Disord. 2006;7:27. doi: 10.1186/1471-2474-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang L, Guo Q, Lu X, Ni B. Surgical versus nonsurgical treatment of chronic low back pain: A meta-analysis based on current evidence. J Back Musculoskelet Rehabil. 2016;29(3):393–401. doi: 10.3233/BMR-150632. [DOI] [PubMed] [Google Scholar]
- 68.Huang Z, Ma J, Chen J, et al. The effectiveness of low-level laser therapy for nonspecific chronic low back pain: A systematic review and meta-analysis. Arthritis Res Ther. 2015;17:360. doi: 10.1186/s13075-015-0882-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Notarnicola A, Maccagnano G, Gallone MF, et al. Extracorporeal shockwave therapy versus exercise program in patients with low back pain: Short-term results of a randomised controlled trial. J Biol Regul Homeost Agents. 2018;32(2):385–89. [PubMed] [Google Scholar]
- 70.Choi H-W, Lee J, Lee S, et al. Effects of high intensity laser therapy on pain and function of patients with chronic back pain. J Phys Ther Sci. 2017;29(6):1079–81. doi: 10.1589/jpts.29.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]