Chronic obstructive pulmonary disease (COPD) is associated with substantial morbidity. A severe exacerbation necessitating hospitalization is a sentinel event in the life course of patients with COPD. Each exacerbation is followed by a prolonged period of pulmonary and systemic inflammation, worsened symptoms, functional limitation, skeletal muscle dysfunction, frailty, and debility. In the long run, these severe exacerbations are associated with a greater decline in lung function, and the 2-year survival rate after hospitalization is only 50% (1). Currently available inhaled medications are associated with a modest reduction in exacerbation frequency and an even smaller effect on hospitalizations (2).
Now imagine that a new therapy is brought to the market that results in a significant improvement in respiratory quality of life, with a change in the St. George’s Respiratory Questionnaire score of 7 units, a change in the 6-minute walk distance of 44 m, improvement in dyspnea, and a 56% reduction in hospitalizations (3, 4). The therapy is also considerably more cost effective than existing inhaled therapies (5). This therapy would be an immediate blockbuster! Such a therapy, however, already exists, is supported by Medicare, and is recommended by every major respiratory society for patients with COPD. It is the often-underappreciated cousin of pharmacotherapy, pulmonary rehabilitation (PR). Despite the many established benefits, patients who present with stable COPD but debilitating symptoms are infrequently offered PR. Indeed, it is not uncommon for patients with severe COPD to go a lifetime having never even heard of PR. In a national survey of patients with COPD and a high symptom burden, 57% were not aware of PR (6).
Multiple recent studies underscore the post-hospital discharge vulnerability of patients to decompensation and rehospitalization. To arrest the downward spiral in pulmonary and skeletal muscle function experienced after a severe exacerbation, the initiation of PR is recommended soon after hospital discharge (7). Recent studies have also highlighted the very poor referral rates for PR after hospitalization, with rates as low as 10% (8), and it is not surprising that even fewer patients eventually receive PR.
In a study presented in this issue of AnnalsATS, Spitzer and colleagues (pp. 99–106) analyzed 223,832 individuals who had been hospitalized for a COPD exacerbation, using a Medicare administrative claims database in a single calendar year, and determined that only 1.9% received PR within 6 months of hospital discharge (9). This number increased marginally to 2.7% when follow-up was extended to 12 months after hospitalization. The authors found striking disparities in rehabilitation participation by age, sex, race, and socioeconomic status. Those who lived 10 miles or more from a rehabilitation center were considerably less likely to receive PR, and half the patients lived within 5 miles of a rehabilitation provider. Those with prior hospitalizations, and thus the very patients expected to benefit the most, were less likely to receive PR. These sobering data are a stark reminder that we need to do more to improve our abysmal record of referral and enrollment in a therapy with proven benefits.
There are a few limitations to the study that should be considered. First, because of the design of the study and the use of administrative data, it is not possible to determine whether the low participation in PR was due to poor referral rates or the inability or refusal of patients to enroll. Previous studies suggest it is very likely a combination of these factors. Second, by excluding patients who had previously received PR, the authors did not account for those who may not have been referred due to exhaustion of lifetime limits on the number of sessions covered by payers. This, though, would only have further reduced the documented rate of referrals.
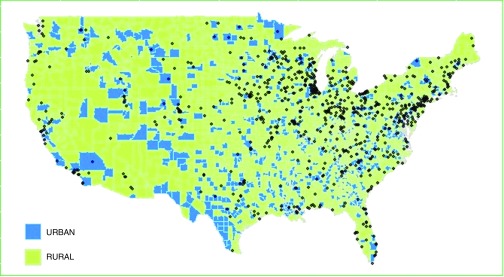
There are three major reasons for the poor uptake of PR for COPD in the community, both after hospitalization and during the chronic stable phase: availability, accessibility, and attrition—the three A’s. There are only 831 PR centers in the United States to serve a population of 24 million patients with COPD, and 561 (67.5%) of these are certified by the American Association of Cardiovascular and Pulmonary Rehabilitation. Thus, there is only one certified PR center per 43,000 patients with COPD. Based on 2010 census data, and categorizing geographical areas into urbanized areas (population of 50,000 or more), urban clusters (population of 2,500 to <50,000), and rural areas (population of <2,500), the majority of PR centers are located in urban areas (Figure 1). These data point to a stark inequity in availability of care, with vast swathes of the country being without PR centers. Accessibility is an additional factor, and a number of studies have shown that distance to the PR center and lack of transportation are major reasons for patients not enrolling or dropping out (10–12). Results from the National Emphysema Treatment Trial (NETT) showed that participants who lived more than 36 miles from a PR center were 51% less likely to be adherent than those who lived less than 6 miles away (11), and a commute time of more than 30 minutes more than doubled the risk of poor attendance (13). Once the patient is enrolled, distance becomes especially critical for continued adherence, as PR involves recurrent sessions over 3 months, unlike other clinic visits that are spaced farther apart temporally. Other barriers include living alone and a lack of social support. Medical factors, such as hospitalizations and a high degree of baseline respiratory morbidity, including poor quality of life, dyspnea, and poor exercise tolerance, also impact enrollment and adherence (10, 14). In addition, economic factors such as parking fees, copays, and insurance coverage that limits PR to 36 sessions over a lifetime likely influence enrollment and adherence to PR.
Figure 1.
Distribution of pulmonary rehabilitation centers (black diamonds) across the United States, stratified by location in urban and rural areas.
So, what is the way forward? A multipronged strategy is necessary to address the three A’s. First, respiratory professional societies, PR experts, healthcare providers, and patients with COPD should make a stronger and more vocal case with payers and health policy makers about the benefits and cost-effectiveness of PR. Quality metrics and perhaps financial incentives can be created to enhance referral and uptake of PR. Referral to PR can be incorporated into existing COPD bundles to reduce rehospitalizations. Second, payers should be petitioned to relax the lifetime limits on the number of PR sessions, as these limits adversely affect referral and enrollment practices. It is increasingly evident that patients with any stage of COPD benefit from PR, and PR should not be reserved for those with severe disease alone (15). Allowance should be made for repeated sessions of PR as needed when a patient’s clinical situation changes. Maintenance PR has also been shown to reduce hospitalization rates in addition to improving quality of life (16), but is currently not reimbursed. Third, efforts should be made to reduce the financial disincentives for sustainability of PR centers so that we can address their geographically inequitable distribution. In this regard, it is pertinent to note that the Centers for Medicare and Medicaid Services recently decreased reimbursement for PR substantially. Fourth, we should invest in novel and alternative methods for delivering PR that move away from the traditional center-based delivery of PR but have equivalent benefits. Such approaches include home-based PR under supervision, interactive web-based PR, and telehealth PR via videoconferencing (17–19). Fifth, we should explore other modes of exercise that do not require center-based equipment, such as tai chi and yoga, and hence are likely to be more durable (20). Finally, efforts to reduce attrition should be made with increased use of self-management and education programs that can be incentivized financially. The status quo is not acceptable, and it is time we brought our A game to this issue.
Supplementary Material
Footnotes
Supported by National Institutes of Health grant K23HL133438.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Connors AF, Jr, Dawson NV, Thomas C, Harrell FE, Jr, Desbiens N, Fulkerson WJ, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments) Am J Respir Crit Care Med. 1996;154:959–967. doi: 10.1164/ajrccm.154.4.8887592. [DOI] [PubMed] [Google Scholar]
- 2.Puhan MA, Bachmann LM, Kleijnen J, Ter Riet G, Kessels AG. Inhaled drugs to reduce exacerbations in patients with chronic obstructive pulmonary disease: a network meta-analysis. BMC Med. 2009;7:2. doi: 10.1186/1741-7015-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005305. doi: 10.1002/14651858.CD005305.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2:CD003793. doi: 10.1002/14651858.CD003793.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zoumot Z, Jordan S, Hopkinson NS. Emphysema: time to say farewell to therapeutic nihilism. Thorax. 2014;69:973–975. doi: 10.1136/thoraxjnl-2014-205667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barr RG, Celli BR, Martinez FJ, Ries AL, Rennard SI, Reilly JJ, Jr, et al. Physician and patient perceptions in COPD: the COPD resource network needs assessment survey. Am J Med. 2005;118:1415. doi: 10.1016/j.amjmed.2005.07.059. [DOI] [PubMed] [Google Scholar]
- 7.Wedzicha JA (ERS Co-Chair), Miravitlles M, Hurst JR, Calverley PMA, Albert RK, Anzueto A, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline Eur Respir J 201749pii: 1600791. [DOI] [PubMed] [Google Scholar]
- 8.Jones SE, Green SA, Clark AL, Dickson MJ, Nolan AM, Moloney C, et al. Pulmonary rehabilitation following hospitalisation for acute exacerbation of COPD: referrals, uptake and adherence. Thorax. 2014;69:181–182. doi: 10.1136/thoraxjnl-2013-204227. [DOI] [PubMed] [Google Scholar]
- 9.Spitzer KA, Stefan MS, Priya A, Pack QR, Pekow PS, Lagu T, et al. Participation in pulmonary rehabilitation after hospitalization for chronic obstructive pulmonary disease among Medicare beneficiaries Ann Am Thorac Soc 20191699–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8:89–99. doi: 10.1177/1479972310393756. [DOI] [PubMed] [Google Scholar]
- 11.Fan VS, Giardino ND, Blough DK, Kaplan RM, Ramsey SD Nett Research Group. Costs of pulmonary rehabilitation and predictors of adherence in the National Emphysema Treatment Trial. COPD. 2008;5:105–116. doi: 10.1080/15412550801941190. [DOI] [PubMed] [Google Scholar]
- 12.Brown AT, Hitchcock J, Schumann C, Wells JM, Dransfield MT, Bhatt SP. Determinants of successful completion of pulmonary rehabilitation in COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:391–397. doi: 10.2147/COPD.S100254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sabit R, Griffiths TL, Watkins AJ, Evans W, Bolton CE, Shale DJ, et al. Predictors of poor attendance at an outpatient pulmonary rehabilitation programme. Respir Med. 2008;102:819–824. doi: 10.1016/j.rmed.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 14.Fischer MJ, Scharloo M, Abbink JJ, van ’t Hul AJ, van Ranst D, Rudolphus A, et al. Drop-out and attendance in pulmonary rehabilitation: the role of clinical and psychosocial variables. Respir Med. 2009;103:1564–1571. doi: 10.1016/j.rmed.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 15.Schroff P, Hitchcock J, Schumann C, Wells JM, Dransfield MT, Bhatt SP. Pulmonary rehabilitation improves outcomes in chronic obstructive pulmonary disease independent of disease burden. Ann Am Thorac Soc. 2017;14:26–32. doi: 10.1513/AnnalsATS.201607-551OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jenkins AR, Gowler H, Curtis F, Holden NS, Bridle C, Jones AW. Efficacy of supervised maintenance exercise following pulmonary rehabilitation on health care use: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:257–273. doi: 10.2147/COPD.S150650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vasilopoulou M, Papaioannou AI, Kaltsakas G, Louvaris Z, Chynkiamis N, Spetsioti S, et al. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur Respir J. 2017;49:pii: 1602129. doi: 10.1183/13993003.02129-2016. [DOI] [PubMed] [Google Scholar]
- 18.Chaplin E, Hewitt S, Apps L, Bankart J, Pulikottil-Jacob R, Boyce S, et al. Interactive web-based pulmonary rehabilitation programme: a randomised controlled feasibility trial. BMJ Open. 2017;7:e013682. doi: 10.1136/bmjopen-2016-013682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhatt SP, Sanders JG, Anderson EM, Baugh D, Givens TH, Schumann CD, et al. Telehealth exercise intervention reduces COPD readmissions. Am J Respir Crit Care Med. 2018;197:A4545. doi: 10.1164/rccm.201902-0314LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polkey MI, Qiu ZH, Zhou L, Zhu MD, Wu YX, Chen YY, et al. Tai chi and pulmonary rehabilitation compared for treatment-naive patients with COPD: a randomized controlled trial. Chest. 2018;153:1116–1124. doi: 10.1016/j.chest.2018.01.053. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.