Abstract
Objective
To assess whether exposure-based internet-delivered cognitive–behavioural therapy (internet-CBT) is a cost-effective treatment for adolescents with irritable bowel syndrome (IBS) compared with a waitlist control, from a societal perspective, based on data from a randomised trial.
Design
Within-trial cost-effectiveness analysis.
Setting
Participants were recruited from the whole of Sweden via primary, secondary and tertiary care clinics reached through news media and advertising.
Participants
Adolescents (aged 13–17) with a diagnosis of IBS.
Interventions
Participants were randomised to either an exposure-based internet-CBT, including 10 weekly modules for adolescents and five modules for parents, or a waitlist.
Outcome measures
The main health outcome was the quality-adjusted life-year (QALY) estimated by mapping Pediatric Quality-of-Life Inventory (PedsQL) scores onto EQ-5D-3L utilities. The secondary outcome was the point improvement on the PedsQL scale. Data on health outcomes and resource use were collected at baseline and 10 weeks post-treatment. Resource use was measured using the Trimbos and Institute of Medical Technology Assessment Cost Questionnaire for Psychiatry (TIC-P). Incremental cost-effectiveness ratios (ICER) were calculated as the difference in average costs by the difference in average outcomes between groups.
Results
The base-case results showed that internet-CBT costs were on average US$170.24 (95% CI 63.14 to 315.04) more per participant than the waitlist. Adolescents in the internet-CBT group showed small QALY gains (0.0031; 95% CI 0.0003 to 0.0061), and an average improvement of 5.647 points (95% CI 1.82 to 9.46) on the PedsQL compared with the waitlist. Internet-CBT yielded an ICER of $54 916/QALY gained and a probability of cost-effectiveness of 74% given the Swedish willingness-to-pay threshold. The ICER for the outcome PedsQL was US$85.29/point improvement.
Conclusions
Offering internet-CBT to adolescents with IBS improves health-related quality of life and generates small QALY gains at a higher cost than a waitlist control. Internet-CBT is thus likely to be cost-effective given the strong efficacy evidence, small QALY gains and low cost.
Trial registration number
NCT02306369; Results.
Keywords: adolescents, cognitive-behaviour therapy, cost-effectiveness, irritable bowel syndrome
Strengths and limitations of this study.
This study is the first to investigate the cost-effectiveness of exposure-based internet-delivered cognitive– behavioural therapy (internet-CBT) for adolescents with irritable bowel syndrome (IBS).
Efforts were made to use mapping techniques to map PedsQL scores onto EQ-5D-3L utilities, thus estimate quality-adjusted life-years.
Results are limited by a short time horizon and lack of a multiattribute utility instrument sensitive to dimensions impacted by IBS in adolescents.
Further research investigating the cost-effectiveness of internet-CBT versus a face-to-face delivery to adolescents with IBS is recommended.
Introduction
Irritable bowel syndrome (IBS) is a functional bowel disorder characterised by abdominal pain or discomfort and stool irregularities.1 It is the most frequently reported functional abdominal pain disorder in the paediatric population,2 impacting about 8% of children and adolescents. IBS in the young population often persists into adulthood, and is associated with disability,3 symptoms of anxiety and reduced quality of life.4 IBS has a substantial economic impact on healthcare systems and families. A study on children with IBS in the Netherlands estimated an annual cost of US$3151.30 per child in current prices, including costs for healthcare and support at school, travel and out-of-pocket costs and productivity losses of parents.5 Healthcare costs (inpatient and outpatient care) accounted for 57.7% of the total costs, and parental productivity losses for 22.2%.
There is evidence supporting the effectiveness of cognitive–behavioural therapy (CBT) in reducing symptoms and improving mental health and quality of life in patients with IBS,6 7 but CBT treatments are poorly disseminated.8 Internet-delivered CBT (internet-CBT) increases treatment accessibility.9 In exposure-based CBT, participants provoke IBS symptoms and approach feared situations in order to decrease symptom-related fear and avoidance.9 10
The efficacy of exposure-based internet-CBT in the management of IBS symptoms has been investigated in several studies, and has shown positive effects when targeting adult populations.11–13 Only one study has been published to date targeting a paediatric population,14 and has also shown notable benefits. Evidence of effectiveness of such interventions is needed, but it is also important to investigate their cost-effectiveness. This information can together support decision-making on the allocation of public resources to providing such treatments to children and adolescents with IBS. As such, evidence on cost-effectiveness is needed to determine whether spending these resources is good value for money. Few studies to date have investigated the short-term cost-effectiveness of exposure-based internet-CBT targeting IBS in adult samples,15 16 and no studies have investigated its cost-effectiveness in a paediatric population. A previous randomised controlled trial (RCT) investigated the effectiveness of exposure-based internet-CBT for adolescents with IBS compared with a waitlist control,14 and showed that the treatment effectively reduced IBS symptoms and improved quality of life. We aimed to assess whether exposure-based internet-CBT is also cost-effective for adolescents with IBS compared with a waitlist control, over a trial period of 10 weeks, from a societal perspective.
Methods
Study design
This within-trial economic evaluation used data collected as part of an efficacy RCT. Details of the trial and results have been published elsewhere.14 In summary, participants needed a confirmed diagnosis of IBS, according to the Rome III criteria,17 from their treating physician and to be aged ≥13 and <18 years old to be included in the study. Participants were excluded if they had ongoing psychological treatment or severe psychological or psychiatric distress, and had been absent from school for more than 2 days/week during the previous month. The adolescent and at least one parent had to be able to read and write, have basic computer skills and internet access. Participants were recruited nationwide in Sweden via primary, secondary and tertiary care clinics reached through news media and advertising.
Interventions
Participants were consecutively randomised at baseline by an independent party to either an exposure-based internet-CBT or a waitlist. A total of 101 adolescents were included and randomised, 47 to internet-CBT and 54 to a waitlist. The internet-CBT was based on a treatment protocol for IBS in adults,12 and was previously evaluated for an adolescent population.18 It was a web-based and therapist-supported intervention that involved both the adolescents and their parents. The treatment consisted of exposure exercises with the aim to reduce fear and avoidance by, for instance, eating symptom-provoking foods and avoiding symptom-reducing behaviour such as resting. Reduced fear and avoidance in turn lead to reductions in overall symptom levels.19 20 The modules targeting parents mainly focused on the role of parents in encouraging adolescents to engage in the exercises. The internet-CBT treatment lasted 10 weeks and included 10 weekly modules for adolescents and five modules for parents. Mean (SD) number of completed modules for adolescents was 8.5 (2.1) and for parents 4.3 (1.0). Each family was randomised to a therapist (psychologist) who provided support throughout the study. During the period of 10 weeks, both intervention and waitlist groups were allowed to initiate other treatments elsewhere. Participants in the waitlist were crossed over to the internet-CBT condition after the post-treatment assessment.
Resource use and costs
Costs were collected from a societal perspective and comprised direct medical costs accruing to adolescents and indirect costs accruing to both adolescents and their parents. Direct medical costs included intervention costs, and costs associated with healthcare resources and medication used by the adolescents. Indirect costs comprised productivity losses associated with absenteeism and reduced efficiency at school by adolescents, and productivity losses associated with absenteeism and reduced efficiency in performing both paid work and unpaid housework by parents. Data were collected at baseline and 10 weeks (post-treatment) using an adapted version of the Trimbos and Institute of Medical Technology Assessment Cost Questionnaire for Psychiatry (TIC-P),21 a widely used health service receipt inventory, where both adolescents and their parents reported their use of resources in the preceding 4 weeks.
Intervention costs included salaried time for therapists to give support to families throughout the intervention and the cost for maintenance of the online platform. Therapist time consisted of time spent to provide feedback, help with assignments and remind participants to log on the platform. Therapist time for each family (one adolescent and one parent) was multiplied by the hourly wage rate for a psychologist to obtain total therapist time. Mean therapist time over the treatment period was 3.1 hours (SD: 1.4). Costs of supervision of therapists were excluded as we assumed the intervention to be operating under steady-state conditions, that is, fully implemented and operating with therapists fully trained and adherent to the principles of the intervention.
Healthcare resource use was costed using national Swedish tariffs, and medication costed using market prices. Productivity losses for both adolescents and parents were estimated using the human capital method.22 Productivity losses due to absenteeism from school were estimated by multiplying the number of days not at school due to illness by the estimated daily cost of a child in high school education.23 Productivity losses due to absenteeism from paid work were the product of the number of days off from work by parents due to the adolescent’s illness by the average hourly wage rate in Sweden.24 Losses due to absenteeism from unpaid work were the product of the number of days not performing unpaid work by the estimated hourly cost of leisure time.25 Productivity losses related to reduced efficiency at school, and in performing both paid and unpaid work were estimated in the same fashion as the productivity losses due to absenteeism, but additionally multiplied by a weighed score representing how the illness impacted the participants’ productivity.26 Costs associated with healthcare resource and medication use were estimated by multiplying frequencies of services used by unit costs. Total costs over the trial period were estimated using a conservative approach and corresponded to the costs at 10 weeks post-treatment (relative to the costs incurred in the preceding month). Unit costs and sources are presented in table 1. Resources were collected alongside the original trial, costed in 2016 Swedish krona (SEK) and converted to 2016 US$ using purchasing power parities for gross domestic product.27 No discounting was applied as all cost and outcome data were collected over a period of 10 weeks.
Table 1.
Unit costs used in the costing of resources in 2016 US$
| Resource item | Unit cost (US$) | Source |
| Health and healthcare use (per visit) | ||
| General practitioner | 204.15 | Stockholm County Council |
| General practitioner (phone consultation) | 73.72 | Sweden’s municipalities and counties |
| Nurse, counsellor, physiotherapist, dietitian, psychologist community health/private practice, alternative/complementary medicine* | 68.05 | Sweden’s municipalities and counties |
| Specialist practitioner | 376.77 | Sweden’s municipalities and counties |
| Psychologist at CAMHS† | 335.49 | Stockholm County Council |
| Medical technology staff | 104.91 | Västerbotten County Council |
| Others | 68.05 | Own estimates |
| Medication | ||
| Pharmaceuticals (eg, laxatives, analgesics) | Individual product prices | Dental and Pharmaceutical Benefits Agency of Sweden |
| Prescription-free medication (dietary supplements) | Individual product prices | Market price from Swedish pharmacy chain (www.apoteket.se) |
| Productivity losses | ||
| Cost per child/day at school | 73.77 | Own estimate based on Swedish National Agency for Education |
| Average wage/hour in Sweden‡ | 30.56 | Statistics Sweden |
| Average care of sick child in Sweden | 24.44 | Statistics Sweden |
| Cost of leisure time/hour* | 10.69 | 35% of average wage/hour in Sweden by Johannesson et al 25 |
| Intervention cost | ||
| Online platform maintenance cost (per adolescent) | 69.61 | Project documentation |
| i-CBT therapist average wage (per hour)‡ | 34.56 | Statistics Sweden |
*For example, reflexology, chiropractor.
†Unit cost for a hospital-based CAMHS psychologist.
‡Includes social fees of 31.42%. All costs uprated to 2016 US$.
CAMHS, Child and Adolescent Mental Health Services; i-CBT, internet-delivered cognitive–behavioural therapy.
Health outcomes
The primary health outcome for this study was the quality-adjusted life-year (QALY), and the secondary outcome was health-related quality of life (HRQoL) measured by the child self-report version of the 23-item Pediatric Quality-of-Life Inventory Version 4.0 Generic Core Scales (PedsQL)28 and reported as point improvement. The PedsQL comprises four dimensions: physical, emotional, social and school. It is one of the most frequently used instruments in paediatric health research. Scores for each item vary between 0 and 100, with higher scores representing higher HRQoL. The PedsQL does not allow the derivation of utilities for the estimation of QALYs, thus we have used a mapping algorithm to predict EQ-5D-Y-3L (youth version) health utilities from the PedsQL scores.29 The EQ-5D30 is the most widely used generic preference-based instrument to measure health outcomes.31 The EQ-5D-3L measures change in HRQoL by asking participants to rate their level of problems (no problems, moderate problems or severe problems) on five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. These ratings define health states which have previously been assigned preference weights. Utility valuations range from no problems (value=1.0) to severe or extreme impairment (value=−0.594). The mapping algorithm used in the current study was derived from the Ordinary Least Squares (OLS) 5 regression model in the paper by Khan et al 29, as this reported the smallest errors for the 0.8–1 category of the EQ-5D-Y utility score range, predicting more accurately at the upper end of this measure. The algorithm is as follows:
EQ-5D-Y-3L utility score = −0.428496 + 0.009127 * PedsQL Physical Functioning + 0.006611 * PedsQL Emotional Functioning + 0.005705 * PedsQL Social Functioning + 0.006011 * PedsQL School Functioning + 0.000020 * PedsQL Physical Functioning Squared − 0.000048 * PedsQL Emotional Functioning Squared + 0.000011 * PedsQL Social Functioning Squared − 0.000017 * PedsQL School Functioning Squared − 0.000004 * PedsQL Physical Functioning × Emotional Functioning − 0.000055 * PedsQL Physical Functioning × Social Functioning − 0.000066 * PedsQL Physical Functioning × School Functioning − 0.000009 * PedsQL Emotional Functioning × Social Functioning + 0.000059 * PedsQL EmotionalFunctioning × School Functioning − 0.000027 * PedsQL Social Functioning × School Functioning.
QALYs were calculated over the 10-week period using the area under the curve method, which multiplies utilities by time,32 and were adjusted for baseline utility.33 The QALY is a useful outcome measure that can be used across different medical areas, thus enabling comparability across various interventions in economic decision-making.
Statistical analyses
The trial was originally powered to detect differences between the groups on the clinical endpoints, such as the PedsQL, and hence not powered to test the cost-effectiveness hypotheses. The base-case analyses were performed following the intention-to-treat (ITT) principle. All participants who completed a baseline assessment were included (internet-CBT=47, waitlist=54). We used adolescent reports for resources pertaining to adolescents, and parent reports for resources pertaining to parents. However, information on healthcare resource use by adolescents was extracted from the parent reports because they were more comprehensive. The base-case analyses included only healthcare resource and medication use directly related to IBS. The relevant healthcare and medication items were selected based on expert opinion. Only one parent per child was included, and where both parents completed the questionnaire, the mother was selected as the primary reporter. Baseline differences in costs were assessed using Wilcoxon rank-sum tests, and baseline differences in PedsQL scores were assessed using t-tests. Differences in PedsQL scores between the internet-CBT and the waitlist over time were analysed using linear mixed models with restricted maximum likelihood estimates. Multiple imputation by predictive mean matching using chained equations, which assumes that data were missing at random, was employed to reduce bias from missing responses in cost and outcome data.34 Generalised linear models (GLM) with appropriate distributions and link functions were used to analyse differences in both costs and QALYs between groups. All models were adjusted for baseline values.35 Data management and costing were performed using Excel 2016, while statistical analyses were performed in STATA V.15 and figures produced in R studio V.3.4.3.
Cost-effectiveness analysis
Two types of analyses were conducted: a cost-utility analysis using QALYs as the primary outcome, and a cost-effectiveness analysis using point improvement on the PedsQL scale as a secondary outcome. A willingness-to-pay (WTP) threshold of 700 000 SEK per additional QALY gained (approximately US$80 000) was used as a benchmark for cost-effectiveness.36
Non-parametric bootstrapping with 5000 iterations was carried out to deal with uncertainty around the cost and outcome data.37 The bootstrap estimates, pairing up differences in costs with differences in outcomes, were used to calculate incremental cost-effectiveness ratios (ICER), given as the difference in average cost per participant between the internet-CBT and the waitlist divided by the difference in average health outcomes. The bootstrapped ICERs were graphically represented on cost-effectiveness planes. A cost-effectiveness plane is a cloud of the 5000 bootstrapped incremental costs and effects across four quadrants, where each quadrant has a decision implication. The bootstrapped estimates were also used to generate cost-effectiveness acceptability curves (CEACs), where the probability of internet-CBT being cost-effective was calculated over different ceiling ratios that a decision-maker would be willing to pay for an additional health effect. A range of sensitivity analyses was conducted to assess the impact of different assumptions on the study results. The following scenarios were considered: (1) analysis using complete cases (analysis of the cases with complete cost and QALY data at the 10-week follow-up); (2) assuming a healthcare perspective (using only the costs associated with the use of healthcare resources in the analysis); (3) assuming a 20% increase in intervention cost, to account for costs of supervision of intervention therapists in a scenario where the intervention has not been fully implemented; and (4) including all resources used during the trial (not limited to those directly related to IBS).
Patient and public involvement
The study was approved by the Regional Ethical Review Board in Stockholm in December 2011 and is registered on ClinicalTrials.gov (registration number NCT02033161). Parents and adolescents gave written informed consent for participation in the study at the inclusion interview for the original randomised trial. There are no plans to disseminate the results of the current study to study participants. For further information on patient involvement see ref 14.
Results
Resource use and costs
Total and mean resource use by adolescents and their parents in both conditions are detailed in table 2. On average, adolescents in the internet-CBT group consumed more healthcare-related resources and medication and were less efficient at school than adolescents in the waitlist. However, parents of adolescents in the waitlist reported being more absent and less efficient when performing paid and unpaid work compared with internet-CBT. Table 3 describes the total average costs per participant for both conditions. Small differences in total costs between groups at baseline were observed although not statistically significant; w=1086, p=0.272. Participants in the internet-CBT group showed a slightly more marked reduction in the different cost items over time than participants in the waitlist, however, this difference became negligible when assessing the incremental cost differences between the groups at post-treatment, while controlling for baseline cost estimates. Costs associated with intervention delivery (therapist time and online platform maintenance) contributed the most to the total cost. The average cost per participant to deliver the intervention internet-CBT was US$178.36 (SD=US$46.70). The total mean societal costs were significantly greater in the internet-CBT group compared with the waitlist. The estimate from the base-case analysis using multiple imputation for costs analysed using GLMs revealed an incremental mean difference in total mean societal costs of US$163.81 (95% CI 48.85 to 332.55, p=0.002). The bootstrapped estimate was US$170.24 (95% CI 63.14 to 315.04).
Table 2.
Frequency and average use of resources by adolescents and their parents in the trial
| Resource item | Baseline | Post-treatment | ||||||
| i-CBT | Waitlist | i-CBT | Waitlist | |||||
| (n=47) | (n=54) | (n=47) | (n=54) | |||||
| n | Mean | n | Mean | n | Mean | n | Mean | |
| Healthcare (visits) | ||||||||
| General practitioner | 20 | 0.426 | 24 | 0.44 | 9 | 0.19 | 7 | 0.13 |
| General practitioner (telephone consultation) | – | – | – | – | 0 | 0 | 1 | 0.02 |
| Nurse | 4 | 0.09 | 10 | 0.19 | 4.5 | 0.10 | 4 | 0.07 |
| Counsellor | 5.5 | 0.12 | 5 | 0.09 | 2 | 0.04 | 2 | 0.04 |
| Physiotherapist | 9 | 0.19 | 2 | 0.04 | 8 | 0.17 | 4 | 0.07 |
| Specialist practitioner in gastroenterology | 21 | 0.45 | 14 | 0.26 | 1 | 0.02 | 6 | 0.11 |
| Other medical practitioner* | 6 | 0.13 | 1 | 0.02 | 2 | 0.04 | 0 | 0 |
| Alternative/complementary medicine (eg, reflexology, chiropractor) | 1 | 0.02 | 0 | 0.00 | 2.5 | 0.05 | 0 | 0.00 |
| Psychologist community health/private practice | 1 | 0.02 | 1 | 0.02 | 0 | 0 | 0 | 0 |
| Psychologist at CAMHS | 4 | 0.09 | 4 | 0.07 | 3 | 0.06 | 1 | 0.02 |
| Dietitian | 3 | 0.06 | 7 | 0.13 | 2 | 0.04 | 1 | 0.02 |
| Medication (units) | 1207 | 25.67 | 1265 | 23.43 | 391 | 8.89 | 694.50 | 13.89 |
| Productivity losses at school (adolescents) | ||||||||
| School absence (days) | 163 | 3.47 | 145 | 2.69 | 84 | 1.79 | 102 | 1.89 |
| Reduced efficiency at school (days) | 268 | 5.70 | 208 | 3.85 | 166 | 3.53 | 115 | 2.13 |
| Productivity losses at work (parents) | ||||||||
| Absence from paid work (hours) | 0 | 0 | 46.60 | 0.88 | 0 | 0 | 24.00 | 0.50 |
| Reduced efficiency at work (hours) | 298.96 | 6.36 | 291.76 | 5.40 | 106.28 | 2.26 | 251.65 | 4.66 |
| Productivity losses unpaid housework (parents) | ||||||||
| Absence from unpaid housework (hours) | 6.43 | 0.14 | 14.00 | 0.26 | 1.14 | 0.03 | 14.29 | 0.30 |
| Reduced efficiency unpaid housework (hours) | 57.54 | 1.22 | 33.26 | 0.63 | 10.69 | 0.25 | 12.46 | 0.26 |
*Paediatrician, emergency services practitioner.
CAMHS, Child and Adolescent Mental Health Services; i-CBT, internet-delivered cognitive–behavioural therapy.
Table 3.
Total costs per participant for internet-CBT and waitlist at baseline and post-treatment (10 weeks) in 2016 US$ (imputed estimates)
| Baseline | Post-treatment | Incremental difference post-treatment (i-CBT–waitlist) | P value for difference | |||
| i-CBT | Waitlist | i-CBT | Waitlist | |||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | 95% CI* | ||
| i-CBT intervention cost | ||||||
| Online platform maintenance | – (–) | – (–) | 69.61 (–) | – (–) | 69.61 (–) | – |
| Therapist time cost | – (–) | – (–) | 108.75 (46.7) | – (–) | 108.75 (96.15 to 121.35) | 0.00 |
| Total intervention cost | – (–) | – (–) | 178.36 (46.7) | – (–) | 178.36 (165.75 to 190.96) | 0.00 |
| Adolescents | ||||||
| Healthcare costs | ||||||
| Healthcare resources | 359.49 (89.68) | 243.71 (49.16) | 112.44 (35.85) | 84.33 (26.88) | 5.53 (−28.18 to 81.25176) | 0.82 |
| Medication | 10.21 (3.23) | 4.02 (0.94) | 1.31 (0.59) | 1.63 (0.53) | −2.47 (−3.91 to 120.74) | 0.61 |
| Total healthcare cost† | 369.7 (89.56) | 247.73 (49.12) | 113.75 (35.81) | 85.97 (26.95) | 9.76 (−23.44 to 87.66) | 0.67 |
| Productivity loss at school | ||||||
| School absence | 242.11 (53.17) | 188.52 (30.71) | 136.19 (38.47) | 149.17 (34.26) | 10.56 (−49.17 to 63.47) | 0.71 |
| Reduced efficiency at school | 281.83 (50.42) | 192.61 (37.89) | 161.15 (40.02) | 91.47 (20.3) | −0.17 (−24.01 to 42.81) | 0.99 |
| Total productivity loss at school | 523.94 (92.78) | 381.13 (56.32) | 297.34 (66.71) | 240.64 (42.49) | −4.84 (−53.44 to 72.12) | 0.88 |
| Parents | ||||||
| Productivity loss paid work | ||||||
| Absence from paid work | 0 (0) | 20.97 (17.67) | 0 (0) | 13.04 (13.04) | −11.16 (−11.16 to 0) | 0.99 |
| Reduced efficiency at work | 220.75 (94.28) | 149.22 (68.44) | 81.07 (41.78) | 95.37 (67.57) | −112.75 (−158.55 to 283.06) | 0.29 |
| Total productivity loss paid work | 220.75 (94.28) | 170.19 (69.67) | 81.07 (41.78) | 108.41 (72.87) | −122.88 (−138.93 to 318.94) | 0.21 |
| Productivity loss unpaid housework | ||||||
| Absence from unpaid housework | 1.76 (1.42) | 3.33 (3.33) | 0.31 (0.31) | 3.4 (2.78) | −0.37 (−0.63 to 3.47) | 0.53 |
| Reduced efficiency unpaid housework | 15.78 (9.36) | 7.9 (6) | 2.93 (1.75) | 2.96 (2.03) | 0.4 (−0.98 to 9.52) | 0.77 |
| Total productivity loss unpaid housework | 17.54 (9.39) | 11.23 (7.71) | 3.24 (1.98) | 6.36 (4.75) | 0.55 (−1.38 to 12.8) | 0.77 |
|
Total societal costs
Trial estimate Bootstrapped estimate |
1131.93 (237.4) – |
810.28 (135.94) – |
671.24 (93.71) – |
441.37 (114.73) – |
163.81 (48.85 to 332.55) 170.24 (63.14 to 315.04) |
0.002 |
| Health outcomes | ||||||
| PedsQL | 71.28 (14.96) | 74.90 (13.42) | 77.03 (14.10) | 74.39 (14.61) | 5.647 (1.82 to 9.46) | 0.005 |
| EQ-5D-Y-3L utilities Trial estimate Bootstrapped estimate |
0.7976 (0.0198) – |
0.8269 (0.0161) – |
0.8361 (0.0175) – |
0.8292 (0.0156) – |
0.0032 (0.0001 to 0.0063)‡ 0.0031 (0.0003 to 0.0061)‡ |
0.043 |
*Mean incremental costs and 95% CI estimated using generalised linear models adjusted for baseline estimates.
†Does not include intervention cost.
‡Values correspond to difference in total quality-adjusted life-year (QALY) gains over the trial period, estimated using the area under the curve method.
i-CBT, internet-delivered cognitive–behavioural therapy.
Health outcomes
The estimate from the base-case analysis using multiple imputation for QALYs analysed using GLMs revealed that adolescents in the internet-CBT group gained 0.0032 QALYs (95% CI 0.0001 to 0.0063, p=0.043) over the treatment period compared with adolescents oi the waitlist. The bootstrapped estimate was 0.0031 QALYs (95% CI 0.0003 to 0.0061). Adolescents in the internet-CBT group showed an average improvement of 5.647 points on the PedsQL scale compared with the waitlist over the treatment period, with a significant time*group interaction (mean=5.647, SE=1.972, t=2.864, p=0.005).
Cost-effectiveness analysis
Figure 1 shows a cost-effectiveness plane with the bootstrapped replications of the joint incremental costs and incremental QALYs of internet-CBT compared with the waitlist from a societal perspective. Most observations fall into the north-east quadrant of the plane, showing internet-CBT entails larger benefits and larger costs than the waitlist. The ICER resulting from the incremental difference in mean costs between both groups divided by the incremental difference in mean QALYs was estimated at US$54 916 per additional QALY. The CEAC in figure 2 shows that the probability of internet-CBT being cost-effective is approximately 74% given the Swedish WTP threshold of approximately US$80 000 per additional QALY (figure 2).
Figure 1.
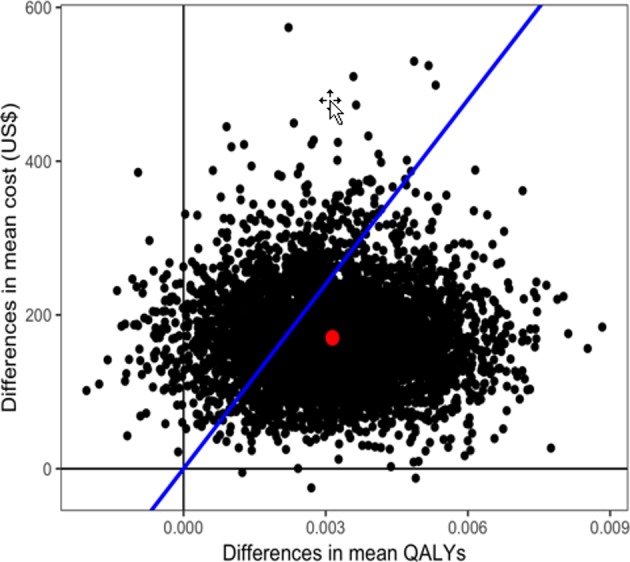
Cost-effectiveness plane of the differences in mean costs and differences in mean quality-adjusted life-years (QALY) between exposure-based internet-delivered cognitive–behavioural therapy (internet-CBT) and the waitlist.
Figure 2.
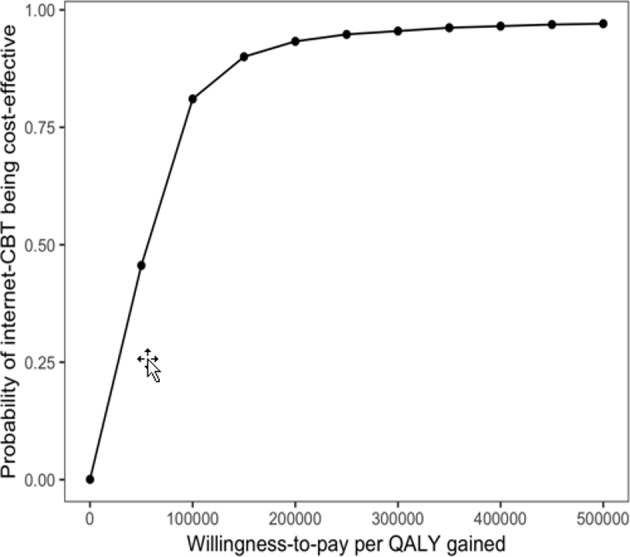
Cost-effectiveness acceptability curve showing the probability that exposure-based internet-delivered cognitive–behavioural therapy (internet-CBT) is cost-effective for different willingness-to-pay values. QALY, quality-adjusted life-year.
The ICER for the outcome PedsQL was estimated at US$85.29 per one point improvement on the PedsQL scale, with most bootstrapped iterations falling on the north-east quadrant of the plane as well (see online supplementary figure 1). At a WTP value of approximately US$50 and above for one point improvement on the PedsQL scale, internet-CBT has a greater probability of being a cost-effective option. The probability of internet-CBT being cost-effective was close to 100% at a WTP value of US$175 for one point improvement on the PedsQL (see online supplementary figure 2).
bmjopen-2018-023881supp001.pdf (295.8KB, pdf)
The sensitivity analysis including participants with complete cost and QALY data showed slightly higher QALY gains and lower costs compared with the base-case ITT analysis with the imputed data set, hence a higher probability of cost-effectiveness of 81%. Taking a healthcare perspective in the analysis also increased the probability of cost-effectiveness by reducing the mean difference in costs. Increasing intervention costs by 20% and including all resources used during the trial (not limited to those directly related to IBS) increased mean incremental costs between groups and decreased the probability of cost-effectiveness (table 4).
Table 4.
Results of the base-case analysis and sensitivity analyses
| Bootstrapped estimates | ||||
| Analysis | Difference mean QALYs (95% CI)* | Difference mean costs (US$) (95% CI)* | ICER (95% CI) | Probability internet-CBT cost-effective† $80 000/QALY (%) |
| 1. Base-case analysis (societal perspective)‡ | 0.0031 (0.0003 to 0.0061) | 170.24 (63.14 to 315.04) | 54 916 | 74 |
| 2. Complete cases | 0.0038 (0.0001 to 0.0075) | 164.01 (55.92 to 301.37) | 42 945 | 81 |
| 3. Healthcare perspective | 0.0031 (0.0003 to 0.0061) | 149.99 (100.39 to 219.74) | 48 384 | 81 |
| 4. 20% increase in treatment cost | 0.0031 (0.0003 to 0.0061) | 194.38 (85.69 to 343.16) | 62 703 | 68 |
| 5. All resources | 0.0031 (0.0003 to 0.0061) | 184.45 (69.52 to 344.26) | 59 500 | 71 |
*Bootstrapped estimates and CI.
†Probability of internet-CBT being cost-effective estimated by non-parametric bootstrapping.
‡Cost and outcome variables imputed using multiple imputation by chained equations.
ICER, incremental cost-effectiveness ratio; internet-CBT, internet-delivered cognitive–behavioural therapy; QALY, quality-adjusted life-year.
Discussion
This within-trial economic evaluation investigated the cost-effectiveness of internet-CBT delivered to adolescents with IBS compared with a waitlist control based on a prior efficacy trial. The base-case cost-utility analysis with imputed data showed that internet-CBT resulted in greater costs and small QALY gains compared with the waitlist control, with a 74% probability of being cost-effective given the Swedish WTP threshold. These results suggest that internet-CBT is likely to be cost-effective. The cost-effectiveness analysis based on the secondary outcome PedsQL demonstrated that internet-CBT also improved HRQoL at greater costs than the waitlist. However, we are not able to determine the societal WTP value for a one point improvement on the PedsQL scale. It is up to decision-makers to decide how much they are willing to invest in internet-CBT treatment given the outcomes generated.
The findings from this study are not directly in concordance with the findings from other studies evaluating exposure-based internet-CBT on IBS symptoms, although with adult populations.15 16 In the studies from Andersson et al 15 and Ljotsson et al,16 internet-CBT generated health gains and resulted in cost savings, with very high probability of cost-effectiveness, whereas in the present study internet-CBT resulted in slightly higher costs than the waitlist. One should keep in mind the more accentuated reduction in costs over time for participants in the internet-CBT group compared with participants in the waitlist. This reduction became, however, negligible when assessing the incremental differences between the groups at post-treatment, possibly due to the high costs in each group at baseline. Although all three studies used very similar methodologies, they had different populations and different outcome measures, thus not being directly comparable. Importantly, the version of TIC-P used in the current study to collect resource use information was originally developed and validated for use in adult populations, and later translated into Swedish for the purpose of this study. Thus, the questions included may not be the most adequate for the collection of information in younger subjects. Additionally, productivity losses are not the same for adults and children and adolescents. Even though a day of school absence generates an estimated cost, it is far less costly than an adult’s productivity loss when not working. IBS in adults may directly impact work ability and measurable productivity loss, and IBS in children may impact their parents’ work ability as they may need to take parental leave to stay home with their child. However, parents to older children in adolescence rarely need to stay home if the child stays home from school. Furthermore, adolescents with a school absence larger than 40% were excluded from the RCT for ethical reasons, as a high degree of school absenteeism needs more intense interventions than the internet-delivered treatment could provide. A decision leading to less room for improvement on this particular variable. This could explain the cost savings accruing in the studies by Andersson et al 15 and Ljotsson et al.16
Methodological considerations and recommendations
This study is the first to investigate the cost-effectiveness of exposure-based internet-CBT for adolescents with IBS and adds to the knowledge on interventions to manage symptomatology related to IBS in this group of patients. This economic evaluation was not planned alongside the design of the initial efficacy trial, thus not all data required for a more comprehensive cost-effectiveness analysis were available. In particular, the study lacks the presence of a multiattribute utility instrument sensitive enough to capture the impacts of IBS on different dimensions of adolescents’ quality of life.37 To tackle this issue, we used a published mapping algorithm to derive EQ-5D-3L utilities from PedsQL scores from the original trial, and thus estimated QALYs. A caveat to this is that the EQ-5D-3L is prone to ceiling and floor effects, however the mapping model chosen demonstrated to predict more accurately at the upper end of this measure.29
One important limitation is the short time horizon of this evaluation that is limited to a 10-week period. Such a time horizon gives only an indicative of the short-term impacts of the intervention, thus recurring to decision modelling techniques may be needed to extrapolate results over a longer time frame.
Further research is needed to address the issues with outcome measurement and extension of time horizon so that all appropriate impacts of the intervention can be fully captured. Internet-delivered psychotherapeutic interventions, such as this intervention, have great potential of being cost-effective when proven effective in improving health and quality of life of their target population. Their low intervention cost compared with other interventions that entail higher running costs is likely a very attractive feature to decision-makers. Internet-CBT has been proven effective targeting different mental health conditions, and has shown similar effect sizes to those of face-to-face interventions.38 A recent study by Lenhard et al 39 demonstrated that internet-CBT is cost-effective and can generate savings when treating adolescents with obsessive-compulsive disorder. Further research investigating the cost-effectiveness of internet-CBT versus a face-to-face delivery to a group of adolescents with IBS is recommended.
Conclusions
The findings demonstrated that internet-CBT improves HRQoL and generates small QALY gains at a higher cost than a waitlist control. Internet-CBT for adolescents with IBS is likely to be cost-effective given the strong efficacy evidence, QALY gains and low cost; however, full economic evaluations employing relevant preference-based quality-of-life instruments, and longer time horizons are needed to provide stronger evidence for decision-making against other competitive alternatives.
Supplementary Material
Footnotes
Patient consent for publication: Not required.
Contributors: MB, OO, EH, ES and BL designed the trial. MB, OO, ML, EH, FL, ES and BL contributed to data collection. FS, RS and IF were the trial health economists and conceived the economic evaluation. FS and RS analysed the data. FS drafted the manuscript. All authors contributed to data interpretation and approved the final manuscript.
Funding: This study was supported by grants from the Jan and Dan Olsson Foundation (4-1559/2013), the Swedish Research Council (521-2013-2846), the Kempe-Carlgren Foundation, the Ruth and Richard Julin Foundation (2012Juli0048), the Majblomman Foundation, the Ishizu Matsumurais Donation, the Bengt Ihre Foundation (SLS-331861), the Bengt Ihre Research Fellowship in Gastroenterology, the Swedish Society of Medicine (SLS331681, SLS-410501), the Stockholm County Council (ALF) and the Swedish Research Council for Health, Working Life and Welfare (2014-4052). Financial support was also provided through the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet (20130129).
Disclaimer: None of the funding bodies had any influence on study design, implementation, data analysis or interpretation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data requests should be made to the corresponding author.
References
- 1. Enck P, Aziz Q, Barbara G, et al. . Irritable bowel syndrome. Nat Rev Dis Primers 2016;2:16014 10.1038/nrdp.2016.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Korterink JJ, Diederen K, Benninga MA, et al. . Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PLoS One 2015;10:e0126982 10.1371/journal.pone.0126982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chitkara DK, van Tilburg MA, Blois-Martin N, et al. . Early life risk factors that contribute to irritable bowel syndrome in adults: a systematic review. Am J Gastroenterol 2008;103:765–74. 10.1111/j.1572-0241.2007.01722.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ballou S, Keefer L. The impact of irritable bowel syndrome on daily functioning: Characterizing and understanding daily consequences of IBS. Neurogastroenterol Motil 2017;29:e12982 10.1111/nmo.12982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hoekman DR, Rutten JM, Vlieger AM, et al. . Annual costs of care for pediatric irritable bowel syndrome, functional abdominal pain, and functional abdominal pain syndrome. J Pediatr 2015;167:1103–8. 10.1016/j.jpeds.2015.07.058 [DOI] [PubMed] [Google Scholar]
- 6. Laird KT, Tanner-Smith EE, Russell AC, et al. . Short-term and long-term efficacy of psychological therapies for irritable bowel syndrome: A systematic review and meta-analysis. Clin Gastroenterol Hepatol 2016;14:937–47. 10.1016/j.cgh.2015.11.020 [DOI] [PubMed] [Google Scholar]
- 7. Altayar O, Sharma V, Prokop LJ, et al. . Psychological therapies in patients with irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Gastroenterol Res Pract 2015;2015:1–19. 10.1155/2015/549308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shafran R, Clark DM, Fairburn CG, et al. . Mind the gap: Improving the dissemination of CBT. Behav Res Ther 2009;47:902–9. 10.1016/j.brat.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 9. Kinsinger SW. Cognitive-behavioral therapy for patients with irritable bowel syndrome: current insights. Psychol Res Behav Manag 2017;10:231–7. 10.2147/PRBM.S120817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Labus JS, Mayer EA, Chang L, et al. . The central role of gastrointestinal-specific anxiety in irritable bowel syndrome: further validation of the visceral sensitivity index. Psychosom Med 2007;69:89–98. 10.1097/PSY.0b013e31802e2f24 [DOI] [PubMed] [Google Scholar]
- 11. Ljótsson B, Hesser H, Andersson E, et al. . Provoking symptoms to relieve symptoms: a randomized controlled dismantling study of exposure therapy in irritable bowel syndrome. Behav Res Ther 2014;55:27–39. 10.1016/j.brat.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 12. Ljótsson B, Falk L, Vesterlund AW, et al. . Internet-delivered exposure and mindfulness based therapy for irritable bowel syndrome--a randomized controlled trial. Behav Res Ther 2010;48:531–9. 10.1016/j.brat.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 13. Craske MG, Wolitzky-Taylor KB, Labus J, et al. . A cognitive-behavioral treatment for irritable bowel syndrome using interoceptive exposure to visceral sensations. Behav Res Ther 2011;49(6-7):413–21. 10.1016/j.brat.2011.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bonnert M, Olén O, Lalouni M, et al. . Internet-delivered cognitive behavior therapy for adolescents with irritable bowel syndrome: A randomized controlled trial. Am J Gastroenterol 2017;112:152–62. 10.1038/ajg.2016.503 [DOI] [PubMed] [Google Scholar]
- 15. Andersson E, Ljótsson B, Smit F, et al. . Cost-effectiveness of internet-based cognitive behavior therapy for irritable bowel syndrome: results from a randomized controlled trial. BMC Public Health 2011;11:215 10.1186/1471-2458-11-215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ljótsson B, Andersson G, Andersson E, et al. . Acceptability, effectiveness, and cost-effectiveness of internet-based exposure treatment for irritable bowel syndrome in a clinical sample: a randomized controlled trial. BMC Gastroenterol 2011;11:110 10.1186/1471-230X-11-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Caplan A, Walker L, Rasquin A. Development and preliminary validation of the questionnaire on pediatric gastrointestinal symptoms to assess functional gastrointestinal disorders in children and adolescents. J Pediatr Gastroenterol Nutr 2005;41:296–304. 10.1097/01.mpg.0000172748.64103.33 [DOI] [PubMed] [Google Scholar]
- 18. Bonnert M, Ljótsson B, Hedman E, et al. . Internet-delivered cognitive behavior therapy for adolescents with functional gastrointestinal disorders — An open trial. Internet Interv 2014;1:141–8. 10.1016/j.invent.2014.07.002 [DOI] [Google Scholar]
- 19. Hesser H, Hedman-Lagerlöf E, Andersson E, et al. . How does exposure therapy work? A comparison between generic and gastrointestinal anxiety-specific mediators in a dismantling study of exposure therapy for irritable bowel syndrome. J Consult Clin Psychol 2018;86:254–67. 10.1037/ccp0000273 [DOI] [PubMed] [Google Scholar]
- 20. Ljótsson B, Hesser H, Andersson E, et al. . Mechanisms of change in an exposure-based treatment for irritable bowel syndrome. J Consult Clin Psychol 2013;81:1113–26. 10.1037/a0033439 [DOI] [PubMed] [Google Scholar]
- 21. Bouwmans C, De Jong K, Timman R, et al. . Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv Res 2013;13:217 10.1186/1472-6963-13-217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Koopmanschap MA, Rutten FF. A practical guide for calculating indirect costs of disease. Pharmacoeconomics 1996;10:460–6. 10.2165/00019053-199610050-00003 [DOI] [PubMed] [Google Scholar]
- 23. The Swedish National Agency for Education. Costs in school 2014;2014. [Google Scholar]
- 24. Statistics Sweden [Statistiska centralbyrån]. Lönedatabasen [Salary database]. 2016. http://www.scb.se/ (Accessed 3 Apr 2012).
- 25. Johannesson M, Borgquist L, Elenstål A, et al. . Tidskostnad och reskostnad för behamdling av hypertoni vid en vårdcentral (Time cost and travel cost of hypertension treatment in primary health care). University L, : Mimeo, 1990. [Google Scholar]
- 26. Kigozi J, Jowett S, Lewis M, et al. . The estimation and inclusion of presenteeism costs in applied economic evaluation: A systematic review. Value Health 2017;20:496–506. 10.1016/j.jval.2016.12.006 [DOI] [PubMed] [Google Scholar]
- 27. Organisation for Economic Co-operation and Development. Purchasing power parities. 2016. http://eppi.ioe.ac.uk/costconversion/ (Accessed 22 Aug 2017).
- 28. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800–12. 10.1097/00005650-200108000-00006 [DOI] [PubMed] [Google Scholar]
- 29. Khan KA, Petrou S, Rivero-Arias O, et al. . Mapping EQ-5D utility scores from the PedsQL™ generic core scales. Pharmacoeconomics 2014;32:693–706. 10.1007/s40273-014-0153-y [DOI] [PubMed] [Google Scholar]
- 30. EuroQol G. EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–208. [DOI] [PubMed] [Google Scholar]
- 31. Räsänen P, Roine E, Sintonen H, et al. . Use of quality-adjusted life years for the estimation of effectiveness of health care: A systematic literature review. Int J Technol Assess Health Care 2006;22:235–41. 10.1017/S0266462306051051 [DOI] [PubMed] [Google Scholar]
- 32. Matthews JN, Altman DG, Campbell MJ, et al. . Analysis of serial measurements in medical research. BMJ 1990;300:230–5. 10.1136/bmj.300.6719.230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487–96. 10.1002/hec.944 [DOI] [PubMed] [Google Scholar]
- 34. Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods 2002;7:147–77. 10.1037/1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- 35. Barber J, Thompson S. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy 2004;9:197–204. 10.1258/1355819042250249 [DOI] [PubMed] [Google Scholar]
- 36. Svensson M, Nilsson FO, Arnberg K. Reimbursement decisions for pharmaceuticals in sweden: The impact of disease severity and cost effectiveness. Pharmacoeconomics 2015;33:1229–36. 10.1007/s40273-015-0307-6 [DOI] [PubMed] [Google Scholar]
- 37. Drummond MF, Sculpher MJ, Claxton K, et al. . Methods for the Economic Evaluation of Health Care Programmes. Fourth Edition: Oxford Oxford University Press, 2015. [Google Scholar]
- 38. Hedman E, Ljótsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res 2012;12:745–64. 10.1586/erp.12.67 [DOI] [PubMed] [Google Scholar]
- 39. Lenhard F, Ssegonja R, Andersson E, et al. . Cost-effectiveness of therapist-guided internet-delivered cognitive behaviour therapy for paediatric obsessive-compulsive disorder: results from a randomised controlled trial. BMJ Open 2017;7:e015246 10.1136/bmjopen-2016-015246 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-023881supp001.pdf (295.8KB, pdf)


