Abstract
Objectives
The aim of this study was to explore the effects of laser acupuncture on improvement of recovery and muscle performance in delayed muscle soreness (DOMS) when applied before exercise.
Methods
This randomized, blinded, and controlled study included healthy participants (n = 40) who were randomized into laser acupuncture and placebo groups. Laser acupuncture was applied to the Tianquan (PC2) and Chihtseh acupoints (LU5) at a dose of 36 J and energy density of 9.7 J/cm2 before inducing DOMS. The placebo group received sham laser acupuncture with no laser output. Visual analog scale (VAS), proprioception, pressure pain threshold (PPT), arm circumference, and muscle strength were observed at the baseline and 24, 48, 72, and 96 h after induction of DOMS.
Results
Significant changes in the VAS (F4, 43.96 = 31.47; p = 0.001), PPT (F4, 1.35 = 35.07; p = 0.001), normalized arm circumference (F4, 0.001 = 3.87; p = 0.005), and normalized muscle strength (F4, 0.31 = 24.99; p = 0.001) were observed within the groups over time (p < 0.05), but there were no significant differences between the two groups (p > 0.05). Normalized arm circumference was significantly different between the two groups at 48 and 72 h after induction of DOMS (p < 0.05).
Conclusion
Photobiomodulation therapy on Tianquan (PC2) and Chihtseh acupoints (LU5) before the exercise did not significantly decrease DOMS and increase muscle performance. Laser acupuncture as a supplemental therapy seemed to have no effect on DOMS prevention.
1. Introduction
Delayed muscle soreness (DOMS) is observed after sport in elite athletes, and it may also affect the general population [1]. It is a myogenic condition often caused 24 to 72 h after performing exercises that overload the muscles. DOMS is not inflammatory in nature [1]. The symptoms of DOMS, which include pain, muscle tenderness, and loss of joint range of motions, are alleviated over time [2]. However, accompanying symptoms, such as muscular discomfort, often affect the sports performance and training schedule of the athlete [2]. The previous study of Cheung et al. revealed that DOMS could increase the risk of injuries when the affected individual returns to the sport after recovery [3]. Therefore, the development of effective preventions that can help prevent DOMS may prove beneficial for athletes.
Acupuncture is a supplemental therapy in traditional Chinese medicine. It involves the use of needles that are placed on acupuncture points, which alters the qi and blood circulation along the meridians, thus exerting its therapeutic effects [4]. Acupuncture points commonly are located in a tender point or muscular pain site, and qi occurs to transmit energy through meridians by acupuncture [5]. The study of Hübscher et al. reported that acupuncture for DOMS resulted in reducing pain and increasing muscle strength when applied on acupuncture points of Yanglingquan (GB34), Tianfu (LU3), Chize (LU5), Quchi (LI11), Xuehai (SP10), and ah-shi (tender points) [6]. The needle acupuncture is manipulated to create a de-qi sensation, and participants could feel soreness, numbness, heaviness, and distension around the acupuncture point [5]. It could activate the meridian, but the effects of acupuncture vary significantly based on the physician's technology [7]. Based on the theory of traditional Chinese medicine for musculoskeletal diseases, disharmony between ying and wei causes muscle soreness and tightness in DOMS. In clinic practice, the signs of asthenia in renal yin and yang and loss of renal qi can be treated with acupuncture by focusing on the pericardium meridians of hand-Jueyin and hand-Shaoyin. The acupuncture points, that is, Tianquan (PC2) and Chihtseh (LU5) acupoints, were chosen as they corresponded with the injured areas on the biceps muscle tendon. Through transmitting qi through the specific meridians, the active energy may improve the muscle fatigue recovery. It could be an advanced treatment that acupuncture also may be used before exercise to enhance the muscle recovery ability and prevent sports injury.
Fleckenstein et al. indicated that acupuncture was not effective in the treatment of symptoms after inducing DOMS [8]. The biases of physicians' technique and non-quantifiable dose could affect the effects of acupuncture. Laser acupuncture, which uses low-level lasers on the acupuncture points to activate the meridians, has several advantages such as noninvasiveness and safety and the ability to quantify the dose and apply the same amount repeatedly in order to achieve the desired therapeutic effect [9]. The systematic review of Law et al. provided moderate evidence of the use of laser acupuncture for the management of musculoskeletal pain, using an appropriate treatment dosage [10]. Laser acupuncture could provide quantifiable dosages to stimulate acupuncture points and to explore the analgesic effect as a result of the laser biostimulation [9]. However, there is a dearth of studies exploring the effect of laser acupuncture on DOMS. Laser biostimulation is also called photobiomodulation and could be used on injured muscle tissue. Laser light could irradiate on muscle tissue to increase mitochondrial activity. Cytochrome c oxidase absorbed photons to increase adenosine triphosphate and provide energy source for muscle tissue recovery. Lopes-Martins et al. used the output power of 2.5 mW and wavelength of 655 nm on fatigued tibial anterior muscle. It was the first study of laser biostimulation in rats and was used to prove the effect on decreasing muscle damage after high intense exercise in animal study [11]. The studies of Leal Junior et al. are the first randomized controlled trials to investigative the effects of photobiomodulation on DOMS [12, 13].
Some systematic review studies indicated preexercise photobiomodulation could provide ergogenic effect on recovery and muscle performance of DOMS [14, 15]. The evidences on preexercise photobiomodulation to prevent muscle injury and improve recovery were proved. The development of supplemental therapies for DOMS prevention has also shown an increasing trend over the past few decades. Laser acupuncture is a quantitative treatment, and also have advantages of safety and convenient. The use of laser acupuncture before the development of DOMS may prove beneficial for the prevention of sports injuries and provide additional protection during exercise. Some studies have found that the use of photobiomodulation therapy on muscles with DOMS before exercise could reduce pain and decrease creatine kinase levels in athletes [16–19]. However, to the best of our knowledge, no studies have been conducted on the effect of laser acupuncture before exercise, and its effects on decrease of DOMS and increase of muscle performance. Therefore, the aim of the present study was to explore the effects of laser acupuncture before the induction of DOMS, and changes in the visual analog scale (VAS), proprioception, pressure pain threshold (PPT), arm circumference, and muscle strength were examined 24, 48, 72, and 96 h after DOMS induction.
2. Methods
This randomized and triple blinded controlled trial was approved by the Institutional Review Board of China Medical University and Hospital (No. CMUH106-REC1-090). Informed consent was obtained from the participants in this study. Based on the study by Hübscher et al. [6], a significant difference of 1.6 in VAS was detected, and statistical power of 80% and α level of 0.05 were calculated. The sample size was estimated at 20 in each group by G∗Power software (version 3.1.9.2; Heinrich-Heine-Universität, Düsseldorf, Germany). The participants in the present study comprised healthy college students belonging to the sports team at Ming Chuan University, Taiwan. Healthy individuals were included in this study, whereas the exclusion criteria included the following: presence of muscle soreness and tenderness, acupuncture within a period of 1 week, and the use of any drugs or medication for musculoskeletal conditions. Each participant completed six visits. The first visit was used to collect demographic data, and baseline assessments were performed in both groups before the laser acupuncture. Subsequent visits were used to assess the VAS, proprioception, PPT, arm circumference, and muscle strength, in order to ascertain the changes in DOMS symptoms 24, 48, 72, and 96 h after the induction of DOMS procedure.
The recruited participants were divided into laser acupuncture and placebo groups. A simple drawing of lots (A or B) was used to determine the grouping, and an assistant, who was not involved in this experiment, handled the randomization procedure. The laser instruments were classified as active (A lot) and nonlaser (B lot) output modes, and the appearance and mode of operation were similar. The laser instruments were applied by one therapist. The exercise for inducing DOMS and subsequent assessments were implemented by an athletic trainer. The outcome data were calculated and analyzed by an analyst. The participants, physical therapist, technician, and analyst were all blinded to the type of laser instrument used.
2.1. Laser Acupuncture
Laser acupuncture was performed before DOMS induction using the laser instrument, Painless Light PL-830 (Advanced Chips & Products Crop., USA) at an output frequency of 10 Hz, a wavelength of 830 nm, a total output power of 60 mW, a dose of 36 J, and energy density of 9.7 J/cm2 (Table 1). The laser was irradiated directly onto the Tianquan acupoint (PC2) and Chihtseh acupoint (LU5) on each arm. Tianquan acupoint (PC2) is located between the short and long heads of the proximal humeral biceps muscle, and it is an acupoint for the pericardium meridian of hand-Jueyin. Chihtseh acupoint (LU5) is located at the distal tendon of the humeral biceps muscle, and it is an acupoint for the heart meridian of hand-Shaoyin [20]. Each acupuncture point was irradiated for 10 min. Participants in the placebo group underwent the same procedures as those in the laser acupuncture group, but the laser instrument was placed on the points without any laser output.
Table 1.
The instrument parameters of photobiomodulation therapy.
| Parameters | Value |
|---|---|
| Laser mode | 830 nm |
| Pulse frequency | 10 Hz |
| Pulse width | 0.75 ms |
| Peak power | 8 W |
| Treatment time per point | 10 min |
| Energy | 60 mW |
| Energy density | 9.7 J/cm2 |
| Number of treated points | 2 acupoints |
| Total energy | 36 J |
2.2. Induction Procedure
A dumbbell was used for free-weight training to induce DOMS in the nondominant arm. Prior to induction, the participants were asked to perform one round of the elbow-flexor stretching exercise for 60 s. The recruited participants were seated on a stable chair, and one repetition maximum in elbow flexion was determined as the maximum amount of muscle force. One repetition maximum of the elbow flexors is determined by lifting dumbbell in 0.5 kg increments, and the participants were encouraged to elicit the maximal weight. The weight of the dumbbell, at 75% one repetition maximum, was used to perform the eccentric muscle contraction exercise of the elbow flexor muscles. The participant was instructed to lift the weight and put it down as slowly as possible. Verbal encouragement was used to urge them to perform as many continuous exercises as possible. Repeated exercise procedures with 30 s rest intervals were between the procedures. The procedure continued until participants' subjective muscle exhaustion [21], and the period of exhaustive exercise was assessed and checked by the physical therapist.
2.3. Outcome Measures
The outcome assessments, including VAS, proprioception, pressure pain threshold, arm circumference, and muscle strength were evaluated by the same physical therapist, who had 10 years of clinical experience. The extractive data of outcome were blinded to be analyzed by another analyst.
2.4. Visual Analog Scale
Pain intensity of the biceps muscle during manual resisted isomeric test was evaluated using a VAS. The VAS involved a 10 cm horizontal line used to assess the intensity of muscle soreness. It determined the pain intensity and had high reliability (intraclass correlation coefficients = 0.97) [22]. The participants were seated with the elbow flexed at 90° and were instructed to perform an isometric elbow flexor contraction for 5 s and score the intensity of muscle soreness on the scale (0 cm “no pain” and 10 cm “extreme soreness”) [6].
2.5. Proprioception
Force sense is one kind of proprioception and is a high-reliable measure. At first, each participant was seated with the elbow in flexion at 90° and performed maximum voluntary isometric contraction against a handheld dynamometer (MicroFET3; Hoggan Health Industries Co., UT, USA). The elbow flexor muscles at 50% maximal voluntary isometric contraction for 3 s was determined as the target force [23]. This valid assessment is a force sense testing and has moderate test-retest reliability (intraclass correlation coefficients = 0.70) [23]. A handheld dynamometer was used to perform the exercises several times with visual feedback and then with 1 min rest intervals. The measurements were repeated three times, and the average of three trials (absolute error value) was calculated.
2.6. Pressure Pain Threshold
The minimum amount of force required to induce muscle pain was assessed by measuring the pressure pain threshold (PPT) using a pressure algometer (Wagner Pain Test™ Model FPK 40; Wagner Instrument, Greenwich, USA). The upper arm was marked with eight equidistant points at 4 cm intervals along the median line of the biceps muscle from the bicipital groove to the radial insertion. Manual pressure at a constant speed of 10 N/s was applied to the points through the head (diameter, 1 cm) of the pressure algometer, and it was stopped when the participant began to feel muscle tenderness [24]. The muscle tenderness is a valid and clinical physical evaluation for assessing the subjective muscle pain and has moderate test-retest reliability (intraclass correlation coefficients = 0.77) for the elbow region [25]. The average PPT of the eight assessed points was calculated for statistical analysis.
2.7. Arm Circumference
The participants were seated with their arms resting beside their trunks. Based on the eight equidistant points used to measure the PPT, a tape measure was used to measure the circumference of the arm at the point and was wrapped tightly around the bicep, and the measurement was recorded. The average value of each measured point was calculated. This assessment was valid for upper extremity edema of DOMS and had high reliability (intraclass correlation coefficients = 0.95) [26].
2.8. Muscle Strength
The isometric strength of the elbow flexor muscles was assessed using a digital muscle testing dynamometer (MicroFET3, Hoggan Health Industries Co., Utah, USA). The dynamometer was placed at the wrist to measure perpendicular force during the movement proceeds toward elbow flexion. The participant was seated with the elbow in flexion (90°), and the dynamometer sensor was contacted on 1 inch above styloid process of ulna on flexor surface. They were asked to perform maximal voluntary isometric contractions for 5 s [27]. The procedure was repeated three times with 1-minute rest intervals. This assessment had moderate test-retest reliability (intraclass correlation coefficients = 0.77) for elbow flexor muscle and was valid for muscle strength [28].
3. Statistical Analysis
Data were analyzed using SPSS Version 17 (SPSS Inc., Chicago, IL, USA). Descriptive statistics of the participants' demographic data, including age, height, weight, and body mass index, and baseline assessments of both groups, are presented as mean ± standard deviation. An independent t-test was used to compare the assessed variables between the two groups. Proprioception, arm circumference, and muscle strength were normalized against the baseline assessment values obtained before inducing DOMS. Two-way mixed analysis of variance (2 groups × 5 times) with repeated measures over time was used to compare the groups. Mauchly's sphericity test was used to validate the conditions and assumptions of applying the repeated-measures test. The Greenhouse–Geisser test was performed if the sphericity assumption did not hold, and the Bonferroni correction was used for multiple comparisons. The assessed variables are presented as mean ± standard error. A significance level of p < 0.05 was set for all the analyses.
4. Results
Forty participants were included (Figure 1) and were randomly divided into a laser acupuncture group (n = 20) and a placebo group (n = 20). All participants completed the study procedure with no dropouts and no adverse reactions reported. No significant differences in age, height, weight, or body mass index were observed between the two groups (p > 0.05; Table 2). Furthermore, no significant differences in baseline assessment values of force sense, arm circumference, or muscle strength (p > 0.05; Table 2) were noted between the two groups. All participants did not present with muscle soreness or tenderness before DOMS induction. Hence, the VAS was 0, and the upper limit PPT was set at 5 kg/cm2 for avoiding tissue bruising.
Figure 1.
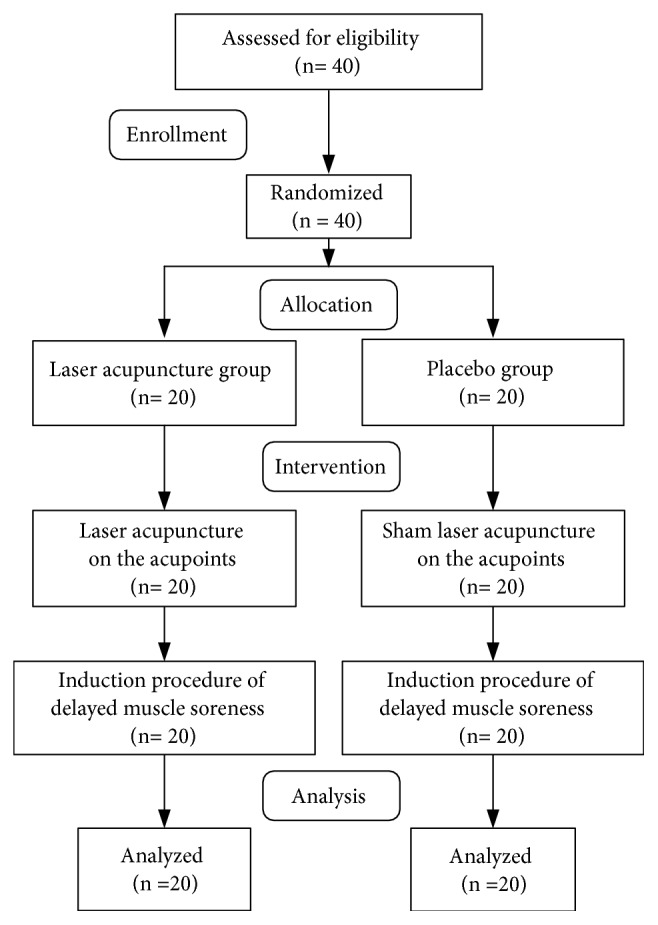
Flow chart of the present study.
Table 2.
Demographic characteristics of the recruited participants.
| Laser acupuncture group | Placebo group | P value | |
|---|---|---|---|
| (n=20) | (n=20) | ||
| Age (years) | 20.90±1.12 | 21.05±1.53 | 0.72 |
| Height (cm) | 165.96±7.34 | 164.56±6.56 | 0.53 |
| Weight (kg) | 59.62±7.87 | 61.23±6.91 | 0.49 |
| Body mass index (kg/m2) | 21.74±3.38 | 22.69±3.05 | 0.35 |
| VAS | 0 | 0 | 1 |
| Force sense (Ib) | 1.34±0.84 | 1.31±1.01 | 0.92 |
| PPT (kg/cm2) | 5 | 5 | 1 |
| Arm circumference (cm) | 29.02±3.65 | 29.18±3.46 | 0.89 |
| Muscle strength (Ib) | 47.62±14.22 | 47.83±13.54 | 0.96 |
VAS, visual analog scale; PPT, pressure pain threshold.
However, after induction of DOMS, the VAS was increased in both groups, with no significant differences observed between the two in subsequent assessments (p > 0.05; Figure 2 and Table 3). Maximum pain occurred at 48 h in both groups. A significant main effect for time (F4, 43.96 = 31.47; p = 0.001) was observed, but no significant main effects were noted for the group (F1, 0.41 = 0.09; p = 0.76) or group × time interactions (F4, 0.43 = 0.03; p = 0.99).
Figure 2.
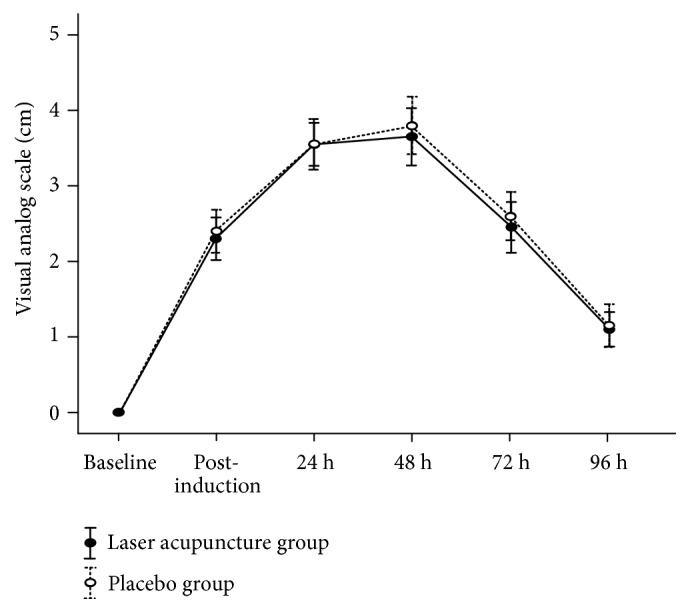
Visual analog scale (mean ± standard error) of muscle soreness from 2 groups at baseline, postinduction, and 24, 48, 72, and 96 h after inducing delayed muscle soreness.
Table 3.
Outcomes at baseline, postinduction, and 24, 48, 72, and 96 h after inducing delayed muscle soreness.
| Items | Groups | Postinduction | 24 h | 48 h | 72 h | 96 h |
|---|---|---|---|---|---|---|
| VAS | Laser acupuncture group | 2.28±1.07 | 3.51±1.52 | 3.67±1.01 | 2.43±1.43 | 1.09±0.84 |
| Placebo group | 2.37±0.94 | 3.53±1.01 | 3.81±1.65 | 2.56±1.83 | 1.21±0.58 | |
| Normalized force sense | Laser acupuncture group | 1.15±0.76 | 0.94±0.71 | 0.98±0.54 | 1.03±0.84 | 1.01±0.08 |
| Placebo group | 1.11±0.80 | 1.07±0.84 | 1.07±0.80 | 1.11±0.89 | 1.06±0.62 | |
| PPT | Laser acupuncture group | 1.15±0.31 | 0.78±0.36 | 0.67±0.27 | 0.78±0.31 | 1.01±0.37 |
| Placebo group | 1.14±0.37 | 0.79±0.31 | 0.69±0.37 | 0.84±0.42 | 1.02±0.30 | |
| Normalized arm circumference | Laser acupuncture group | 1.01±0.02 | 1.02±0.03 | 1.00±0.03 | 0.99±0.02 | 0.99±0.03 |
| Placebo group | 1.01±0.03 | 1.00±0.04 | 1.02±0.02∗ | 1.02±0.04∗ | 1.01±0.03 | |
| Normalized muscle strength | Laser acupuncture group | 0.72±0.78 | 0.77±0.13 | 0.83±0.22 | 0.87±0.17 | 0.94±0.31 |
| Placebo group | 0.71±0.13 | 0.74±0.09 | 0.82±0.22 | 0.86±0.13 | 0.95±0.17 |
∗p<0.05, laser acupuncture group versus placebo group
No significant main effects on normalized force sense were noted for the group (F1, 0.17 = 0.13; p = 0.71), time (F4, 0.72 = 0.18; p = 0.94), or group × time (F4, 0.39 = 0.10; p = 0.98). In both groups, normalized force sense was increased after the induction of DOMS, but no significant differences in values were observed in subsequent assessments (p > 0.05; Figure 3 and Table 3). The lowest normalized force sense was measured at 24 h, with the laser acupuncture group presenting lower 0.12 value of normalized force sense, when compared with the placebo group.
Figure 3.
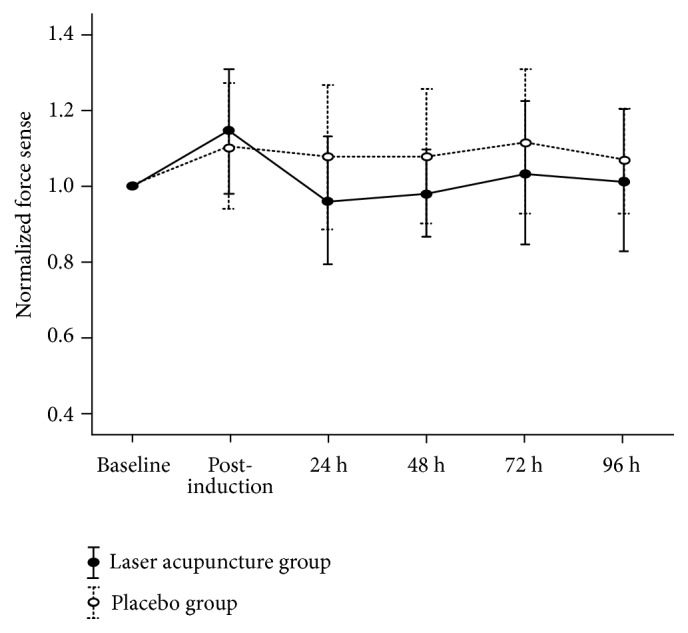
Normalized force sense (mean ± standard error) from 2 groups at baseline, postinduction, and 24, 48, 72, and 96 h after inducing delayed muscle soreness.
A significant main effect on PPT for time (F4, 1.35 = 35.07; p = 0.001) was observed, but not for group (F1, 0.01 = 0.29; p = 0.86) or group × time interactions (F4, 0.01 = 0.11; p = 0.98). Similar to the VAS, maximum PPT occurred 48 h after DOMS induction. In Figure 4 and Table 3, the laser acupuncture group exhibited lower 0.02 kg/m2 of PPT when compared with the placebo group.
Figure 4.
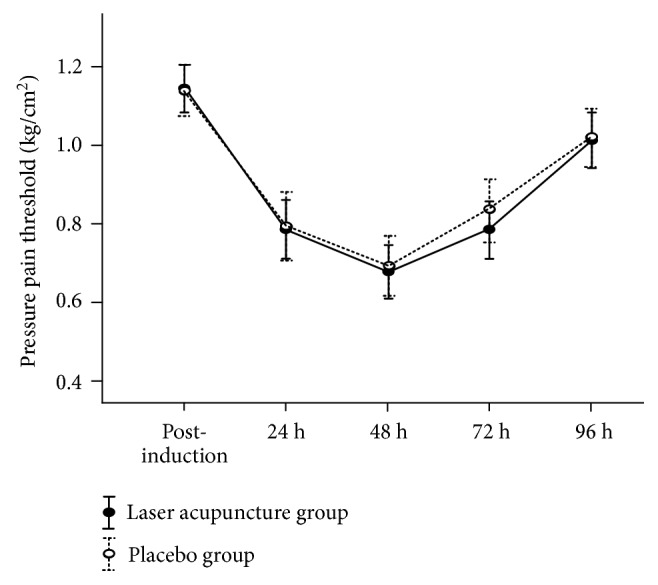
PPT (mean ± standard error) from 2 groups at postinduction and 24, 48, 72, and 96 h after inducing delayed muscle soreness.
No significant main effects on normalized arm circumference for group (F1, 0.01 = 1.79; p = 0.18) or group × time interactions (F4, 0.001 = 2.04; p = 0.09) were noted. Nevertheless, a significant main effect for time (F4, 0.001 = 3.87; p = 0.005) was observed. In addition, normalized arm circumference was highest at 48 h after DOMS induction, with significant differences at 48 and 72 h between the two groups (p = 0.04; Figure 5 and Table 3).
Figure 5.
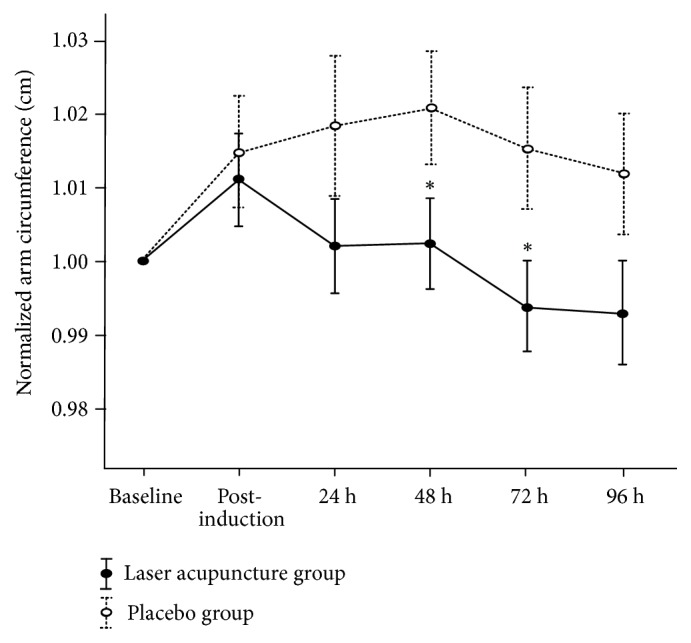
Normalized arm circumference (mean ± standard error) from 2 groups at baseline, postinduction, and 24, 48, 72, and 96 h after inducing delayed muscle soreness. ∗P < 0.05, significant difference between groups.
Similar to the arm circumference measurement values, no significant main effects on normalized muscle strength for group (F1, 0.001 = 0.01; p = 0.93) or group × time interactions (F4, 0.001 = 0.07; p = 0.98) were observed (Figure 6 and Table 3). A significant main effect for time (F4, 0.31 = 24.99; p = 0.001) was found. Normalized muscle strength demonstrated a gradual increase during the subsequent assessments, but no significant differences were observed between the two groups.
Figure 6.
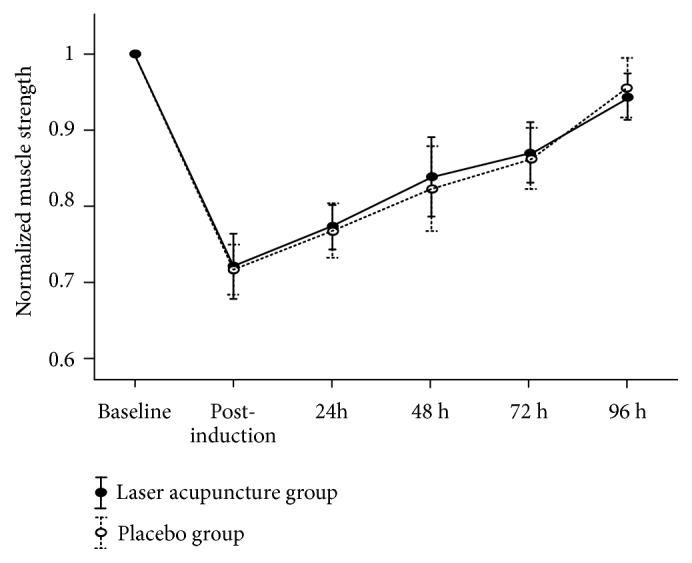
Normalized muscle strength (mean ± standard error) from 2 groups at baseline, postinduction, and 24, 48, 72, and 96 h after inducing delayed muscle soreness.
5. Discussion
The present study was focused on clinical outcomes, that is, VAS, proprioception (force sense), PPT, arm circumference, and muscle strength, and used low-level laser on the acupuncture points before DOMS induction. In both groups, decreased VAS and PPT occurred at 48 h after DOMS induction, and increased normalized muscle strength occurred at postinduction. But, there were no significant differences on VAS, PPT, normalized force sense, and normalized muscle strength at all assessment times between both groups. Only arm circumference was significantly decreased 48–72 h after induction in the laser group when compared with the sham laser group.
Traditional acupuncture involves the application of needles on acupuncture points for mechanical stimulation. By contrast, laser acupuncture causes photobiomodulation to activate neurophysiological pathways for analgesia (inhibition of spinal and supraspinal descending pathways) and modulate neurotransmitters [29]. Fleckenstein et al. were the first to compare the effects of laser acupuncture with verum acupuncture after the induction of DOMS [8]. Their results showed that laser acupuncture had no effects on the treatment of DOMS, because this treatment cannot penetrate into local deep muscle tissue. However, they indicated that the treatment mechanisms involved in traditional and laser acupuncture were presumed to be similar.
Leal Junior et al. are pioneers in this field and their series of studies had provided positive evidences on low-level laser for DOMS. Both low-level laser parameters (655 nm wavelength, 5 J; energy density of 500 J/cm2; 830 nm wavelength, energy density of 500 J/cm2) could decrease the increase of blood lactate level [12, 13]. In another study, low-level laser parameter (energy density: 1,428.57 J/cm2) could inhibit the increase of CK level and acceleration of lactate removal in athletes. These findings provided the basis for other studies [30]. Baroni et al. had applied low-level laser on quadriceps muscle before knee extensor eccentric exercise and then lowered lactate dehydrogenase and serum creatine kinase levels and enhanced the recovery of the damaged muscles which were found in biochemical analysis [17].
Hübscher et al. evaluated the effects of acupuncture on Chihtseh (LU5) acupoint and other accompanied acupoints in delayed-onset muscle soreness after exercise, and they reported an improvement in both the VAS and PPT after 48–72 h [6]. Barlas et al. also indicated that acupuncture on Chihtseh (LU5) acupoint and other accompanied acupoints exerted analgesic effects until 120 h, which were significantly higher than those in the placebo and control groups [31]. Unlike previous studies on the effect of acupuncture treatment on DOMS, our results of the present study indicated that laser acupuncture on Tianquan (PC2) and Chihtseh (LU5) acupoints before the induction of DOMS had no significant decrease in VAS and PPT to compare with control group. To the best of our knowledge, there are no reports on the effects of acupuncture or laser acupuncture before DOMS induction. It seemed that laser acupuncture had no effects on pain relief for prevention of DOMS occurring. Further studies evaluating the use of the appropriate acupuncture treatment method on various acupoints to prevent the occurrence of DOMS were suggested to explore.
Photobiomodulation therapy was used as the treatment tool. The therapeutic effects were dependent on laser irradiation parameters such as the applied wavelength, dosage, and pulses. Very high or very low values of the parameters could influence the treatment effects of the laser, which is “Arndt-Shultz law” [32]. Dos Reis et al. applied photobiomodulation therapy (830 nm) on quadriceps muscles before and after exercise, and they reported reduced levels of serum lactate and creatine kinase before the induction of DOMS [33]. In the systematic review study with meta-analysis, Vanin et al. investigated photobiomodulation therapy on the improvement of muscular performance and reduction of muscular fatigue. Their positive results were the wavelength (655-950 nm), energy dose (60-300 J), and maximal power output per diode (200 mW) [34]. In the present study, 830 nm laser acupuncture at a total energy of 9.7 J/cm2 and total energy of 36J was tried before DOMS induction. The pain and discomfort of DOMS successfully presented with at 48 h. Comparing with the placebo group, the pain was not lowered significantly during the subsequent assessment times in the laser acupuncture group. Insufficient energy of photobiomodulation therapy may be the source of problem in this study. Application of photobiomodulation therapy on muscle could increase the mitochondrial respiratory rate and adenosine triphosphate synthesis, thereby improving cellular metabolism and decreasing the accumulation of pain factors before muscle fatigue [8]. In the current study, the energy of the laser acupuncture was directed on the acupuncture points, but not on the affected muscles belly. Therefore, the local laser acupuncture could not exert significant bioenergetic effects at the cellular level. Laser acupuncture as a supplemental therapy for DOMS prevention may cause no effects on reducing the symptoms.
Athletes need to return to sports approximately 48 h after high intensity training, which is often accompanied with DOMS. Thus, the recovery of muscle performance including muscle strength and proprioception is essential [35]. Antonialli et al. used photobiomodulation therapy with doses of 10, 30, and 50 J on quadriceps muscle before the eccentric contraction protocol [36]. They found that 30 J dose significantly increased maximum voluntary contraction compared to placebo group. It seems that 30 J dose, 905 nm wavelength of laser pulsed 640 nm wavelength of red LEDs, and irradiated site (6 locations in muscle belly of quadriceps) represented an effect on increased muscle strength. However, in the current study, we found that 36 J dose and 830 nm wavelength of photobiomodulation on Tianquan (PC2) and Chihtseh acupoints (LU5) could not recover the muscle performance. Borges et al. indicated that photobiomodulation therapy applied immediately on the muscle after eccentric contraction exercise could promote the increase in muscle strength and improve the recovery time of the fatigued muscle [37]. During occurring muscle fatigue, loss in muscle strength was also accompanied by a disturbance in muscular proprioception [38]. Mesquita-Ferrari et al. confirmed that photobiomodulation therapy could decrease tumor necrosis factor-alpha (TNF-α) by modulating the expression of the cytokine [39]. TNF-α is a proinflammatory cytokine and can affect the muscle contraction force [40]. Therefore, photobiomodulation therapy could decrease muscle strength loss in DOMS. The results of the present study indicate that laser acupuncture did not provide better muscle strength recovery at 48 h, and the difference was not significant when compared with the sham laser acupuncture group. This may be attributed to the same reason that the laser acupuncture was not applied to the affected muscles, resulting in nonsignificant changes. In a previous animal study, Onda et al. noted that acupuncture could modulate messenger RNA expression levels of atrogin-1 and muscle RING-finger protein-1 (MuRF1) [41], leading to an increase in protein synthesis and decrease in degradation, thereby preventing skeletal muscle atrophy and muscle strength loss. Nonetheless, this mechanism was not proved in human study. A similar tendency was observed in the present study, wherein the outcome of muscle strength and proprioception in the laser acupuncture group was not better than that in the placebo group, and the difference was not statistically significant.
The arm circumference is increased due to exercise-induced muscle damage. The DOMS occurs because of structural damage to the micro contractile filaments in the muscle, resulting in pain and edema [42]. In the present study, the differences in arm circumference were significantly presented at 48 and 72 h between two groups, and this means that laser acupuncture could improve the recovery of edema. Lorenzini et al. indicated that laser acupuncture had an antiedema effect in an animal model of complete Freund's adjuvant-induced inflammatory pain [43]. This effect of laser acupuncture was also found in the subcutaneous tissues of osteoarthritic patients by sonographic examination [44]. The evidences of a decrease in reactive oxygen species [45] and improvements in antioxidant capacity and adenosine triphosphate synthesis also support the effect of low-level laser for DOMS [46]. However, the change of arm circumference is only one finding that supports that laser acupuncture before DOMS induction could decrease edema in the injured muscle. But, the physiological mechanism of laser acupuncture is still not clear to confirm this finding.
There are some limitations in the present study. First, the study design should have a nontreated group as a control group to investigate the psychological effect. Second, appropriate laser parameters and preventive acupuncture points on DOMS were still unclear. Usage of various laser acupuncture parameters and differential acupoints were suggested in future studies.
6. Practical Relevance
Photobiomodulation therapy on Tianquan (PC2) and Chihtseh acupoints (LU5) before the exercise cannot decrease DOMS and increase muscle performance. It seems that muscles may be preconditioned by photobiomodulation to improve the reduction of muscle edema.
7. Conclusion
Laser acupuncture applied on Tianquan (PC2) and Chihtseh (LU5) acupoints before the induction of DOMS significantly decreased the arm circumference at 48 and 72 h.
But it seemed to have no effects of the DOMS prevention on pain, proprioception, PPT, and muscle strength. Laser acupuncture as a supplemental therapy to reduce DOMS symptoms should be probed in future studies.
Acknowledgments
The authors would like to thank all of the Ming Chuan University students, especially Yi-Lu Tsai and Jyun-Pei Lin. They helped in the volunteers' recruitment and data collection and had contributed to this study.
Data Availability
The data used to support the findings of this study are included within the article.
Disclosure
No funder support was involved in the manuscript writing, editing, approval, or decision to publish.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Wen-Dien Chang was responsible of the initial outline, data interpretation, draft writing, revisions for intellectual content, and final approval; Jih-Huah Wu, draft writing, revisions for intellectual content, corresponding author, and final approval; Nai-Jen Chang, data interpretation and presentation, draft writing, and revisions for intellectual content; Chia-Lun Lee, data interpretation and presentation, draft writing, and revisions for intellectual content; Shuya Chen, data interpretation and presentation and revisions for intellectual content.
References
- 1.Lewis P. B., Ruby D., Bush-Joseph C. A. Muscle Soreness and Delayed-Onset Muscle Soreness. Clinics in Sports Medicine. 2012;31(2):255–262. doi: 10.1016/j.csm.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Keane K. M., Salicki R., Goodall S., Thomas K., Howatson G. Muscle damage response in female collegiate athletes after repeated sprint activity. The Journal of Strength and Conditioning Research. 2015;29(10):2802–2807. doi: 10.1519/JSC.0000000000000961. [DOI] [PubMed] [Google Scholar]
- 3.Cheung K., Hume P. A., Maxwell L. Delayed onset muscle soreness: treatment strategies and performance factors. Sports Medicine. 2003;33(2):145–164. doi: 10.2165/00007256-200333020-00005. [DOI] [PubMed] [Google Scholar]
- 4.Chae Y., Olausson H. The role of touch in acupuncture treatment. Acupuncture in Medicine. 2017;35(2) doi: 10.1136/acupmed-2016-011178. [DOI] [PubMed] [Google Scholar]
- 5.Longhurst J. C. Defining meridians: a modern basis of understanding. Journal of Acupuncture and Meridian Studies. 2010;3(2):67–74. doi: 10.1016/s2005-2901(10)60014-3. [DOI] [PubMed] [Google Scholar]
- 6.Hübscher M., Vogt L., Bernhörster M., Rosenhagen A., Banzer W. Effects of acupuncture on symptoms and muscle function in delayed-onset muscle soreness. The Journal of Alternative and Complementary Medicine. 2008;14(8):1011–1016. doi: 10.1089/acm.2008.0173. [DOI] [PubMed] [Google Scholar]
- 7.Irnich D., Salih N., Offenbächer M., Fleckenstein J. Is sham laser a valid control for acupuncture trials? Evidence-based Complementary and Alternative Medicine. 2011;2011:8. doi: 10.1093/ecam/neq009.485945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleckenstein J., Niederer D., Auerbach K., et al. No Effect of Acupuncture in the Relief of Delayed-Onset Muscle Soreness: Results of a Randomized Controlled Trial. Clinical Journal of Sport Medicine. 2016;26(6):471–477. doi: 10.1097/JSM.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 9.Lin M. L., Wu J. H., Lin C. W., Su C. T., Wu H. C., Shih Y. S., et al. Clinical effects of laser acupuncture plus Chinese cupping on the pain and plasma cortisol levels in patients with chronic nonspecific lower back pain: a randomized controlled trial. Evidence-based Complementary and Alternative Medicine. 2017;2017:7. doi: 10.1155/2017/3140403.3140403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Law D., McDonough S., Bleakley C., Baxter G. D., Tumilty S. Laser acupuncture for treating musculoskeletal pain: a systematic review with meta-analysis. Journal of Acupuncture and Meridian Studies. 2015;8(1):2–16. doi: 10.1016/j.jams.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Lopes-Martins R. Á. B., Marcos R. L., Leonardo P. S., et al. Effect of low-level laser (Ga-Al-As 655 nm) on skeletal muscle fatigue induced by electrical stimulation in rats. Journal of Applied Physiology. 2006;101(1):283–288. doi: 10.1152/japplphysiol.01318.2005. [DOI] [PubMed] [Google Scholar]
- 12.Leal E. C. P., Lopes-Martins R. Á. B., Dalan F., et al. Effect of 655-nm low-level laser therapy on exercise-induced skeletal muscle fatigue in humans. Photomedicine and Laser Surgery. 2008;26(5):419–424. doi: 10.1089/pho.2007.2160. [DOI] [PubMed] [Google Scholar]
- 13.Leal Junior E. C. P., Lopes-Martins R. Á. B., Vanin A. A., et al. Effect of 830 nm low-level laser therapy in exercise-induced skeletal muscle fatigue in humans. Lasers in Medical Science. 2009;24(3):425–431. doi: 10.1007/s10103-008-0592-9. [DOI] [PubMed] [Google Scholar]
- 14.Borsa P. A., Larkin K. A., True J. M. Does phototherapy enhance skeletal muscle contractile function and postexercise recovery? A systematic review. Journal of Athletic Training. 2013;48(1):57–67. doi: 10.4085/1062-6050-48.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leal-Junior E. C. P., Vanin A. A., Miranda E. F., de Carvalho P. D. T. C., Dal Corso S., Bjordal J. M. Effect of phototherapy (low-level laser therapy and light-emitting diode therapy) on exercise performance and markers of exercise recovery: a systematic review with meta-analysis. Lasers in Medical Science. 2015;30(2):925–939. doi: 10.1007/s10103-013-1465-4. [DOI] [PubMed] [Google Scholar]
- 16.Torres R., Ribeiro F., Alberto Duarte J., Cabri J. M. H. Evidence of the physiotherapeutic interventions used currently after exercise-induced muscle damage: Systematic review and meta-analysis. Physical Therapy in Sport. 2012;13(2):101–114. doi: 10.1016/j.ptsp.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 17.Baroni B. M., Leal Junior E. C. P., De Marchi T., Lopes A. L., Salvador M., Vaz M. A. Low level laser therapy before eccentric exercise reduces muscle damage markers in humans. European Journal of Applied Physiology. 2010;110(4):789–796. doi: 10.1007/s00421-010-1562-z. [DOI] [PubMed] [Google Scholar]
- 18.De Almeida P., Lopes-Martins R. Á. B., De Marchi T., et al. Red (660 nm) and infrared (830 nm) low-level laser therapy in skeletal muscle fatigue in humans: What is better? Lasers in Medical Science. 2012;27(2):453–458. doi: 10.1007/s10103-011-0957-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Marchi T., Leal E. C. P., Jr., Bortoli C., Tomazoni S. S., Lopes-Martins R. Á. B., Salvador M. Low-level laser therapy (LLLT) in human progressive-intensity running: Effects on exercise performance, skeletal muscle status, and oxidative stress. Lasers in Medical Science. 2012;27(1):231–236. doi: 10.1007/s10103-011-0955-5. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Y. H., Liu J., Li X. F., Jia C. S. Advances of studies on acupuncture and moxibustion for exercise-induced fatigue. Zhongguo Zhen Jiu. 2010;30(3):261–264. [PubMed] [Google Scholar]
- 21.Craig J. A., Barron J., Walsh D. M., Baxter G. D. Lack of effect of combined low intensity laser therapy/phototherapy (CLILT) on delayed onset muscle soreness in humans. Lasers in Surgery and Medicine. 1999;24(3):223–230. doi: 10.1002/(SICI)1096-9101(1999)24:3<223::AID-LSM7>3.0.CO;2-Y. doi: 10.1002/(SICI)1096-9101(1999)24:3<223::AID-LSM7>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 22.Bijur P. E., Silver W., Gallagher E. J. Reliability of the visual analog scale for measurement of acute pain. Academic Emergency Medicine. 2001;8(12):1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 23.Chang H.-Y., Chou K.-Y., Lin J.-J., Lin C.-F., Wang C.-H. Immediate effect of forearm Kinesio taping on maximal grip strength and force sense in healthy collegiate athletes. Physical Therapy in Sport. 2010;11(4):122–127. doi: 10.1016/j.ptsp.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Lau W. Y., Blazevich A. J., Newton M. J., Xuan Wu S. S., Nosaka K. Assessment of muscle pain induced by elbow-flexor eccentric exercise. Journal of Athletic Training. 2015;50(11):1140–1148. doi: 10.4085/1062-6050-50.11.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bisset L. M., Evans K., Tuttle N. Reliability of 2 protocols for assessing pressure pain threshold in healthy young adults. Journal of Manipulative and Physiological Therapeutics. 2015;38(4):282–287. doi: 10.1016/j.jmpt.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 26.Gulick D. T., Kimura I. F., Sitler M., Paolone A., Kelly J. D. Various treatment techniques on signs and symptoms of delayed onset muscle soreness. Journal of Athletic Training. 1996;31(2):145–152. [PMC free article] [PubMed] [Google Scholar]
- 27.Aufsesser P., Horvat M., Croce R. A critical examination of selected hand-held dynamometers to assess isometric muscle strength. Adapted Physical Activity Quarterly. 1996;13(2):153–165. doi: 10.1123/apaq.13.2.153. [DOI] [Google Scholar]
- 28.Surburg P. R., Suomi R., Poppy W. K. Validity and reliability of a hand-held dynamometer with two populations. Journal of Orthopaedic & Sports Physical Therapy. 1992;16(5):229–241. doi: 10.2519/jospt.1992.16.5.229. [DOI] [PubMed] [Google Scholar]
- 29.Kibar S., Konak H. E., Evcik D., Ay S. Laser Acupuncture Treatment Improves Pain and Functional Status in Patients with Subacromial Impingement Syndrome: A Randomized, Double-Blind, Sham-Controlled Study. Pain medicine (Malden, Mass.) 2017;18(5):980–987. doi: 10.1093/pm/pnw197. [DOI] [PubMed] [Google Scholar]
- 30.Leal Junior E. C. P., Lopes-Martins R. Á. B., Baroni B. M., et al. Effect of 830 nm low-level laser therapy applied before high-intensity exercises on skeletal muscle recovery in athletes. Lasers in Medical Science. 2009;24(6):857–863. doi: 10.1007/s10103-008-0633-4. [DOI] [PubMed] [Google Scholar]
- 31.Barlas P., Robinson J., Allen J., David Baxter G. Lack of effect of acupuncture upon signs and symptoms of delayed onset muscle soreness. Clinical Physiology. 2000;20(6):449–456. doi: 10.1046/j.1365-2281.2000.00280.x. [DOI] [PubMed] [Google Scholar]
- 32.Chang W.-D., Wu J.-H., Yang W.-J., Jiang J.-A. Therapeutic effects of low-level laser on lateral epicondylitis from differential interventions of chinese-western medicine: Systematic review. Photomedicine and Laser Surgery. 2010;28(3):327–336. doi: 10.1089/pho.2009.2558. [DOI] [PubMed] [Google Scholar]
- 33.Dos Reis F. A., Da Silva B. A. K., Laraia E. M. S., et al. Effects of pre-or post-exercise low-level laser therapy (830 nm) on skeletal muscle fatigue and biochemical markers of recovery in humans: Double-blind placebo-controlled trial. Photomedicine and Laser Surgery. 2014;32(2):106–112. doi: 10.1089/pho.2013.3617. [DOI] [PubMed] [Google Scholar]
- 34.Vanin A. A., Verhagen E., Barboza S. D., Costa L. O. P., Leal-Junior E. C. P. Photobiomodulation therapy for the improvement of muscular performance and reduction of muscular fatigue associated with exercise in healthy people: a systematic review and meta-analysis. Lasers in Medical Science. 2018;33(1):181–214. doi: 10.1007/s10103-017-2368-6. [DOI] [PubMed] [Google Scholar]
- 35.Jakeman J. R., Byrne C., Eston R. G. Lower limb compression garment improves recovery from exercise-induced muscle damage in young, active females. European Journal of Applied Physiology. 2010;109(6):1137–1144. doi: 10.1007/s00421-010-1464-0. [DOI] [PubMed] [Google Scholar]
- 36.Antonialli F. C., De Marchi T., Tomazoni S. S., et al. Phototherapy in skeletal muscle performance and recovery after exercise: effect of combination of super-pulsed laser and light-emitting diodes. Lasers in Medical Science. 2014;29(6):1967–1976. doi: 10.1007/s10103-014-1611-7. [DOI] [PubMed] [Google Scholar]
- 37.Borges L. S., Cerqueira M. S., Dos Santos Rocha J. A., et al. Light-emitting diode phototherapy improves muscle recovery after a damaging exercise. Lasers in Medical Science. 2014;29(3):1139–1144. doi: 10.1007/s10103-013-1486-z. [DOI] [PubMed] [Google Scholar]
- 38.Tsay A., Allen T. J., Leung M., Proske U. The fall in force after exercise disturbs position sense at the human forearm. Experimental Brain Research. 2012;222(4):415–425. doi: 10.1007/s00221-012-3228-z. [DOI] [PubMed] [Google Scholar]
- 39.Mesquita-Ferrari R. A., Martins M. D., Silva J. A., Jr., et al. Effects of low-level laser therapy on expression of TNF-α and TGF-β in skeletal muscle during the repair process. Lasers in Medical Science. 2011;26(3):335–340. doi: 10.1007/s10103-010-0850-5. [DOI] [PubMed] [Google Scholar]
- 40.Miles M. P., Andring J. M., Pearson S. D., et al. Diurnal variation, response to eccentric exercise, and association of inflammatory mediators with muscle damage variables. Journal of Applied Physiology. 2008;104(2):451–458. doi: 10.1152/japplphysiol.00572.2007. [DOI] [PubMed] [Google Scholar]
- 41.Onda A., Jiao Q., Nagano Y., et al. Acupuncture ameliorated skeletal muscle atrophy induced by hindlimb suspension in mice. Biochemical and Biophysical Research Communications. 2011;410(3):434–439. doi: 10.1016/j.bbrc.2011.05.152. [DOI] [PubMed] [Google Scholar]
- 42.MacIntyre D. L., Sorichter S., Mair J., Berg A., McKenzie D. C. Markers of inflammation and myofibrillar proteins following eccentric exercise in humans. European Journal of Applied Physiology. 2001;84(3):180–186. doi: 10.1007/s004210170002. [DOI] [PubMed] [Google Scholar]
- 43.Lorenzini L., Giuliani A., Giardino L., Calzà L. Laser acupuncture for acute inflammatory, visceral and neuropathic pain relief: An experimental study in the laboratory rat. Research in Veterinary Science. 2010;88(1):159–165. doi: 10.1016/j.rvsc.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 44.Baratto L., Capra R., Farinelli M., Monteforte P., Morasso P., Rovetta G. A new type of very low-power modulated laser: Soft-tissue changes induced in osteoarthritic patients revealed by sonography. International Journal of Clinical Pharmacology Research. 2000;20(1-2):13–16. [PubMed] [Google Scholar]
- 45.Hamblin M. R. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophysics. 2017;4(3):337–361. doi: 10.3934/biophy.2017.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Silveira P. C. L., Silva L. A. D., Fraga D. B., Freitas T. P., Streck E. L., Pinho R. Evaluation of mitochondrial respiratory chain activity in muscle healing by low-level laser therapy. Journal of Photochemistry and Photobiology B: Biology. 2009;95(2):89–92. doi: 10.1016/j.jphotobiol.2009.01.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.


