Abstract
Objective
In this meta-analysis, we aim to investigate the neonatal mortality in hospitalized Chinese population in the recent 20 years in China, which may provide basis for decreasing the neonatal mortality.
Methods
The merged mortality was estimated based on the random effect model, and subgroup analysis was performed for the gender, publication year, gestational age, and birth weight. Sensitivity analysis was utilized to evaluate the effects of research type and research quality on the effects.
Results
The neonatal mortality in eastern China was lower than that of the central and western China (2.3% versus 2.9; 2.3% versus 26.%). The mortality in neonates with a gestational age of 28-32 weeks (0.6%) was significantly higher than that of <28 weeks (0.1%), 32-37 weeks (0.3%), 37-42 weeks (0.4%), and >42 weeks (0.1%). The mortality in those with a body weight of 1.0-2.5 kg (0.3%) was significantly higher than that of 2.5-4.0 kg (0.2%) and >4.0 kg (0.0%). Sensitivity analysis revealed that the findings of meta-analysis were stable. The major causes for neonatal death included asphyxia, respiratory distress syndrome, and infection.
Conclusions
The hospitalized neonatal mortality showed a tendency of decrease, which differed based on gender, region, gestational age, and birth weight.
1. Introduction
Neonatal mortality is an important index for evaluating the perinatal healthcare of a region or even a nation [1]. There are about 3 million neonatal deaths worldwide, which accounts for about 43% in the children aged less than 5 yrs old. The majority is reported from the developing countries [2]. Neonatal period, a time range of 28 days after birth including an early stage (0-7 days) and advanced stage (8-28 days), shows the highest mortality worldwide [3]. Although great stride has been achieved in controlling the childhood mortality aged < 5 yrs, the decrease of neonatal mortality shows a tendency of slow decline. Moreover, in a recent survey, about half of the children aged <5 yrs are neonates [4]. In a survey, the Chinese neonatal death accounts for about 6.4% among the neonatal death worldwide [5]. Nowadays, the total death rate in the neonates is on a decreasing trend with the advances of technical development and social progress; however, in China mainland, neonatal mortality surpassed about 60% of the mortality in children aged < 5yrs [6], among which the mortality was high in the hospitalized cases. It has been reported that neonatal death is associated with the financial status and medical technique [4]. Indeed, there are differences in the medical technique in different regions of China, which triggers variation in the neonatal death. To date, there are some disputes on the neonatal mortality during hospitalization among different studies [7].
In this study, we did this meta-analysis to evaluate the neonatal mortality during the hospitalization in China mainland. Besides, subgroup analysis was performed to investigate the differences in study time, age, region, gestational age, and birth weight.
2. Materials and Methods
2.1. Strategies
We searched the articles published between 2000 and 2017 by Chinese authors or institutions. The studies published before June 2018 were considered to be eligible for the study. The articles were searched from PubMed, EMBASE database, and three Chinese medical databases including CNKI database, VIP database, and Wanfang databases. The following key words were used for the searching strategy: (death) OR (death rate)] AND (newborn OR neonatal) AND (hospital OR in hospital) AND (China OR Chinese). The articles were manually checked for the information of neonatal mortality. Besides, manual search was performed after reading these articles.
2.2. Eligibility
Articles meeting the following criteria were eligible for this study: (i) research studies performed in Chinese neonates involving qualified samples; (ii) studies reporting the mortality of neonates; (iii) reporting the number of live birth and mortality of neonates in a qualified form. The exclusion criteria were as follows: (i) studies based on samples collected from neonates with specific diseases that could not represent the neonatal population; (ii) not reporting complete information; (iii) repeated articles.
2.3. Data Collection
The articles were reviewed by two qualified researchers. The data were collected by two independent researchers. In cases of any disputes, a deep communication was performed until consensus. Epidata 3.02 software was utilized for the data entry. For each eligible article, the following information was collected including title, publication year, author information, region, study duration, and number of live births and mortality.
2.4. Article Quality Evaluation
The article quality was evaluated using the standards proposed by Agency for Healthcare Research and Quality (QHRQ). The standards used in the cross-sectional study included 11 aspects, including data source, research setting, participants, variables, data, bias, sample size, quantitative variables, statistical analysis, and follow-up [8].
2.5. Statistical Analysis
The data were merged using the generic inverse variance model proposed by Sutton et al. Subgroup analysis was performed to analyze the publication year, region, gender, gestational age, birth weight, and neonatal mortality. According to the previous description, we classified the China mainland into three regions (i.e., eastern, central, and western regions). On this basis, we did the sensitivity analysis for the article qualities, to analyze the effects on meta-analysis. The forest plot was drawn using Stata 11.0 software, together with determination of the heterogeneity and publication bias.
3. Results
3.1. Data Characteristics
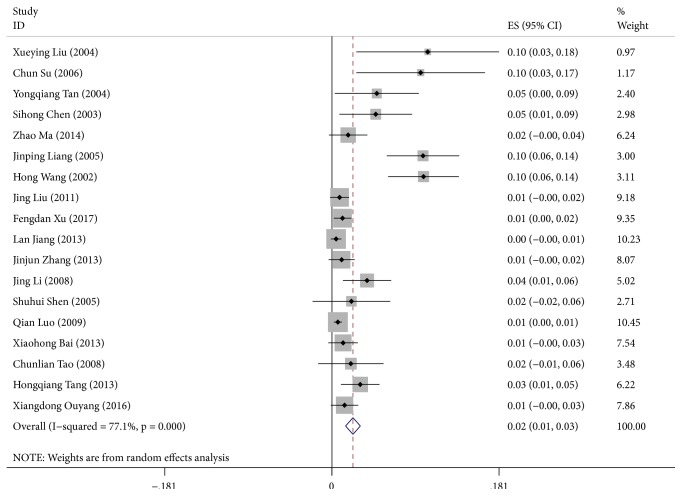
A total of 3462 articles were obtained after research. Finally, 18 eligible articles [9–26] involving 488,604 cases were obtained after detailed exclusion (Figure 1). The time range of the studies was between 2000 and 2017. There were 4571 neonatal deaths. The sample volume showed large variances (580-201,115, median: 7030, Table 1).
Figure 1.
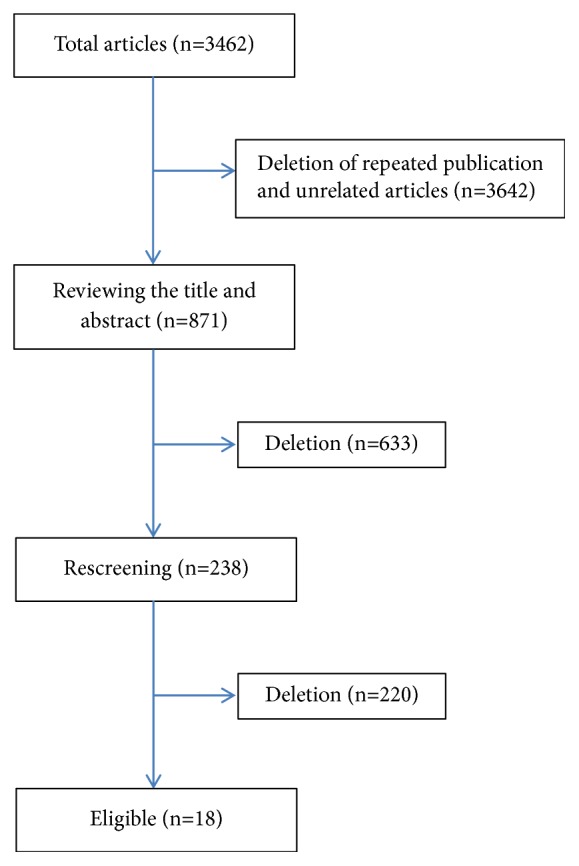
Study flowchart.
Table 1.
Characteristics of eligible studies.
| Author | Year | Study duration | Region | Live birth (n) | Death toll (n) | Mortality | Top five reasons for death |
|---|---|---|---|---|---|---|---|
| Liu et al [9] | 2004 | 1997-2003 | Guangdong Province | 580 | 60 | 0.103 | Asphyxia/intracranial hemorrhage/pneumonia/birth defect/RDS |
| Su et al [10] | 2006 | 1997~2005 | Guangdong Province | 720 | 69 | 0.095 | Premature birth/asphyxia/intracranial hemorrhage/pneumorrhagia/RDS |
| Tan et al [11] | 2004 | 1993~2002 | Shanghai | 1775 | 86 | 0.048 | Not available |
| Chen et al [12] | 2003 | 1995~2002 | Guangdong Province | 2367 | 112 | 0.047 | Asphyxia/premature birth/infection/intracranial hemorrhage/scleredema |
| Ma et al [13] | 2014 | 2003-2012 | Guangxi Province | 8788 | 154 | 0.017 | birth defect/septicemia/RDS/asphyxia/bilirubin cerebropathy |
| Liang et al [14] | 2005 | 1998~2004 | Jiangxi Province | 2265 | 223 | 0.098 | Asphyxia/intracranial hemorrhage/RDS/septicemia/scleredema |
| Wang et al [15] | 2002 | 1995-2000 | Sichuang Province | 2376 | 235 | 0.098 | Asphyxia/intracranial hemorrhage/RDS/septicemia/scleredema |
| Liu et al [16] | 2011 | 2007-2009 | Liaoning Province | 36861 | 305 | 0.008 | Premature birth/birth defect/asphyxia/pneumonia/RDS |
| Xu et al [17] | 2017 | 2008-2014 | Beijing | 41910 | 480 | 0.011 | Infection/birth defect/RDS/asphyxia/pneumorrhagia |
| Jiang et al [18] | 2013 | 1990-2010 | Jilin Province | 119327 | 537 | 0.004 | Asphyxia/RDS/birth defect/pneumorrhagia/intracranial hemorrhage |
| Zhang et al [19] | 2013 | 2003-2012 | Jiangsu Province | 19158 | 201 | 0.010 | RDS/birth defect/asphyxia/pneumonia/septicemia |
| Li et al [20] | 2008 | 2000-2007 | Shanghai | 5459 | 207 | 0.037 | Birth defect/RDS/septicemia/pneumonia/asphyxia |
| Shen et al [21] | 2005 | 1992-2001 | Hunan Province | 2138 | 45 | 0.021 | Pneumonia/asphyxia/intracranial hemorrhage/septicemia/tetanus |
| Luo et al [22] | 2009 | 2005-2008 | Chongqing Province | 201115 | 1297 | 0.006 | Asphyxia/premature birth/birth defect/pneumonia/accidental death |
| Bai et al [23] | 2013 | 2007-2011 | Sichuan Province | 14909 | 180 | 0.012 | Pneumonia/asphyxia/birth defect/septicemia/RDS |
| Tao et al [24] | 2008 | 2003-2007 | Guangdong Province | 3034 | 62 | 0.020 | RDS/asphyxia/birth defect/pneumonia/septicemia |
| Tang et al [25] | 2013 | 2008-2012 | Shaanxi Province | 8602 | 263 | 0.030 | Birth defect/RDS/asphyxia/pneumonia/pneumorrhagia |
| Ouyang et al [26] | 2016 | 2010-2014 | Hunan Province | 17220 | 235 | 0.013 | Asphyxia/birth defect/RDS/intracranial hemorrhage/septicemia |
3.2. Methodology Quality Control
A quality score of 4-6 was achieved for the 18 articles. In most studies, the application of variables was clear, and the sample volume was adequate. The major problem for these articles was not mentioning the reasons for data missing and the potential influences. Most of the articles did not report the 95% confidential interval of the neonatal mortality.
3.3. Merge of Effect Size
There was significant heterogeneity in this study (I2=77.10%, P<0.001); therefore, the random effect model was used for the merging of effect size. According to the forest plot, the neonatal mortality was 2.3% after mergence (CI: 1.5%-3.1%). Subgroup analysis indicated that the neonatal mortality between 2010 and 2017 was significantly lower than that between 2000 and 2009 (Figure 2). The neonatal mortality of male was higher than that of female. Meanwhile, the neonatal mortality in eastern China was lower than that of the central and western China. The neonatal mortality was the lowest in the full-term newborn infants and those with normal birth weight. The mortality in the neonates with a gestational age of 28-32 weeks and a body weight of 1.0-2.5 kg was higher than the other counterparts, with a ratio of 0.6% and 0.3%, respectively (Table 2).
Figure 2.
Forest plot for the neonatal mortality in hospital cases.
Table 2.
Subgroup analysis for the neonatal mortality.
| Variables | Article (n) | Mortality | 95% CI | I 2 | Publication bias | |
|---|---|---|---|---|---|---|
| Begg's test p | Egger's test p | |||||
| Year | ||||||
| 2000~2009 | 10 | 0.053 | (0.026, 0.079) | 86.30% | 0.531 | 0.001 |
| 2010~2017 | 8 | 0.010 | (0.005, 0.014) | 12.90% | 0.013 | 0.003 |
| Gender | ||||||
| Male | 18 | 0.013 | (0.008, 0.018) | 66.60% | 0.000 | 0.450 |
| Female | 18 | 0.005 | (0.002, 0.007) | 22.40% | 0.000 | 0.763 |
| Region | ||||||
| Eastern China | 10 | 0.023 | (0.110, 0.034) | 56.60% | 0.016 | 0.010 |
| Central China | 3 | 0.029 | (0.005, 0.053) | 88.90% | 0.042 | 0.063 |
| Western China | 5 | 0.026 | (0.004, 0.049) | 87.10% | 0.042 | 0.194 |
| Gestational age | ||||||
| <28 weeks | 18 | 0.001 | (-0.005, 0.007) | 0.00% | 0.085 | 0.170 |
| 28~32 weeks | 18 | 0.006 | (-0.000, 0.011) | 0.00% | 0.020 | 0.368 |
| 32~37 weeks | 18 | 0.003 | (0.000, 0.006) | 0.00% | 0.000 | 0.577 |
| 37~42 weeks | 18 | 0.004 | (0.002, 0.007) | 0.00% | 0.009 | 0.994 |
| >42 weeks | 18 | 0.001 | (-0.004, 0.006) | 0.00% | 0.074 | 0.746 |
| Birth weight | ||||||
| <1000g | 18 | 0.001 | (-0.003, 0.005) | 0.00% | 0.300 | 0.605 |
| 1000~1500g | 18 | 0.003 | (-0.001, 0.007) | 0.00% | 0.002 | 0.699 |
| 1500~2500g | 18 | 0.003 | (-0.000, 0.005) | 0.00% | 0.000 | 0.263 |
| 2500~4000g | 18 | 0.002 | (0.001, 0.003) | 0.00% | 0.005 | 0.619 |
| >4000g | 18 | 0.000 | (-0.003, 0.004) | 0.00% | 0.005 | 0.277 |
3.4. Sensitivity and Publication Bias
Sensitivity analysis was performed by gradual exclusion of each study. No significant changes were noticed in the merged mortality. These indicated the results for this meta-analysis were stable. Funnel plot revealed the neonatal mortality (Figure 3). The sample size was comparatively low, which resulted in bias to some extent. Begg test indicated a test statistic of 3.48 (P<0.01). Egger test statistic was -0.59 (P>0.01). This implied that there might be publication bias.
Figure 3.
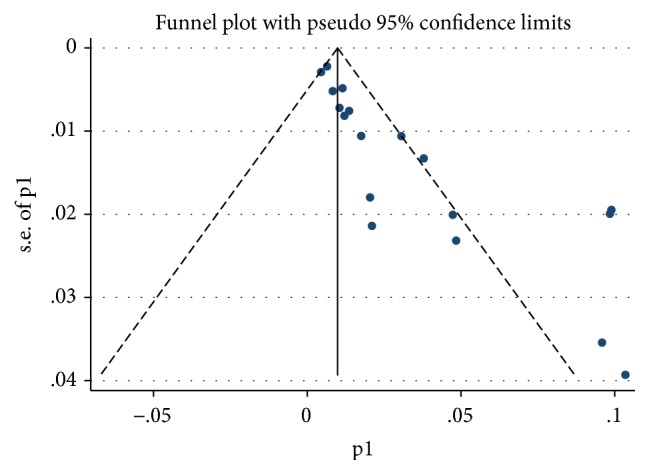
Funnel plot with pseudo 95% CI.
4. Discussion
Nowadays, more and more attention has been paid to the meta-analysis as it provides high quality evidence. In this meta-analysis, we analyzed the neonatal mortality in Chinese population. Our study contributed to the neonatal researches.
In the recent twenty years, the neonatal mortality decreased from 5.3% (2000-2009) to 1.0% (2010-2017). The merged mortality was 2.3%. According to a recent survey by WHO in 2016, the neonatal mortality dropped from 2.35% in 2008 to 1.92% in 2015, in which the mortality dropped from 0.12% in 2008 to 0.09% in 2015 in Japan, from 0.43% in 2008 to 0.36% in 2015 in US, and from 1.01% in 2008 to 0.55% in 2015 in China [27]. The merged mortality was significantly higher than that reported by WHO. This may be related to the fact that most cases included in this study were neonates in hospital, as well as differences in region, hospital conditions, and sources. In total, the neonatal mortality was higher than that of the developed countries. In this study, the neonatal mortality of male was higher than that of the female, which was in line with the previous study in US [28, 29]. As mentioned in the survey in China mainland in 2010, the neonatal mortality of female was higher than that of the male [30]. As previously described, the risk of death in the neonates born in the regions with high financial income and adequate medical sources was lower, and the mortality may be different in different regions [31, 32], which were in line with our data. The variation in the neonatal death in the eastern and western China is mainly associated with the economic levels in these regions. Our data indicated that neonates with a birth weight of 1.0-2.5 kg and a gestational age of 28-32 weeks showed the highest mortality, which was consistent with the previous description [33, 34]. The prevalence of complications in the neonates was significantly higher than that of the full-term infants, which was mainly associated with low gestational age and birth weight and incomplete organ function that resulted in asphyxia, respiratory distress syndrome, and hemorrhagic disease. On this basis, it is necessary to pay attention to the development of organs, in order to avoid complications. Our data showed that the subgroup mortality in the neonates with a gestational age of <28 weeks and a body weight of <1 kg was the lowest. This may be related to the fact that most of the families gave up the treatment due to financial considerations. The outcome for these cases was death in most cases. This information was not included in the analysis as loss to follow-up.
Among the 18 studies, 17 reported the potential causes for mortality. We selected the top 5 factors from each study; the major causes for mortality were asphyxia, infection/pneumonia, septicaemia, and neonatal respiratory distress syndrome. Similarly, Bale et al. reported these factors were also responsible for neonatal mortality in most developing countries [35]. Besides, in the developing countries, the major causes for neonatal death include asphyxia, preterm labor, and severe infection, accounting for about 70% of the neonatal deaths [35]. In a recent survey aimed to generate high quality data about the burden, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-Saharan Africa, the most common causes of neonatal deaths were perinatal asphyxia (40% in south Asia; 34% in sub-Saharan Africa) and severe neonatal infections (35%, in south Asia; 37% in sub-Saharan Africa), followed by complications of preterm birth (19% in south Asia; 24% in sub-Saharan Africa) [36]. In the developed regions, the prime cause for neonatal death is birth defect, followed by preterm labor, sudden death, perinatal complications, and injuries [37–39].
In the developing countries, the lower medical techniques are mainly responsible for the neonatal death. Carlo et al. reported the early neonatal mortality rates decreasing from 11.5 deaths per 1000 live births to 6.8 deaths per 1000 live births after Essential Newborn Care (ENC) training, because of decreases in rates of deaths attributable to birth asphyxia and infection [40]. Late-stage neonatal death in hospital is mainly related to infectious diseases, such as pneumonia and septicemia. Therefore, for the long-term hospitalized neonates, close monitoring should be given to induce the incidence of nosocomial infection such as appropriate application of antibiotics and paying attention to the breast feeding [41].
Sensitivity analysis demonstrated that there might be effects of article quality and research types on the study findings of this study. In future, high quality prospective studies are required to accurately calculate the neonatal mortality. In this study, there is indeed publication bias, and large sample sizes studies are needed to further investigate the neonatal mortality.
There are some limitations for the meta-analysis. The final sample size was not large, and severe mixed factors were available, which may lead to selection bias and information bias. In addition, we only performed subgroup analysis to the gender, gestational age, birth weight, publication year, and region. Neonatal mortality may be related to the treatment options and social or environmental factors, but these factors were not included in the subgroup analysis. We can not exclude the heterogeneity through subgroup analysis. Moreover, there might be differences in the index expression in different articles, which may cause effects on the findings.
In summary, our meta-analysis indicates that the neonatal mortality in hospitalized Chinese population is on a trend of decrease, which demonstrates differences in terms of gender, region, gestational age, and body weight. The major causes responsible for neonatal mortality include asphyxia, RDS, infection, and birth defect. In future, large sample size, multicentered prospective studies are required to obtain the accurate proportion of neonatal mortality.
Acknowledgments
This work was supported by the Research Fund of Fujian Provincial Maternity and Children's Hospital: YCXM 18-22.
Data Availability
All the data were available upon appropriate request.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.Kochanek K. D., Kirmeyer S. E., Martin J. A., Strobino D. M., Guyer B. Annual summary of vital statistics: 2009. Pediatrics. 2012;129(2):338–348. doi: 10.1542/peds.2011-3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blencowe H., Cousens S. Review: addressing the challenge of neonatal mortality. Tropical Medicine & International Health. 2013;18(3):303–312. doi: 10.1111/tmi.12048. [DOI] [PubMed] [Google Scholar]
- 3.Patel R. M., Kandefer S., Walsh M. C., et al. Causes and Timing of Death in Extremely Premature Infants from 2000 through 2011. The New England Journal of Medicine. 2015;372(4):331–340. doi: 10.1056/NEJMoa1403489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu L., Johnson H., Cousens S. Global, regional and national causes of child mortality: an update systematic analysis for 2010 with time trends since 2000. The Lancet. 2012;379(9832):2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 5.Oestergaard M. Z., Inoue M., Yoshida S. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: a systematic analysis of progress, projections, and priorities. PLoS Medicine. 2011;8(8) doi: 10.1371/journal.pmed.1001080.e1001080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang H., Liddell C. A., Coates M. M. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014;384(9947):956–979. doi: 10.1016/S0140-6736(14)61632-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ananth C. V., Goldenberg R. L., Friedman A. M., Vintzileos A. M. Association of Temporal Changes in Gestational Age With Perinatal Mortality in the United States, 2007-2015. JAMA Pediatrics. 2018;172(7):627–634. doi: 10.1001/jamapediatrics.2018.0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engineer L. D., Winters B. D., Weston C. M., et al. Hospital characteristics and the agency for healthcare research and quality inpatient quality indicators: A systematic review. Journal for Healthcare Quality. 2016;38(5):304–313. doi: 10.1097/JHQ.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 9.Xy L. Neonatal death analysis in 60 cases. Xian Dai Yi Xue. 2004;4(9):30–31. [Google Scholar]
- 10.Su C., Lin Y. Q., Zb X. Neonatal death in 69 cases. Zhong Yuan Yi Kan. 2006;33(11):52–53. [Google Scholar]
- 11.Tan Y. Q., Xu J. P., Lw Y. Neonatal death analysis in 86 cases. Zhong Hua Wei Chan Yi Xue Za Zhi. 2004;7(2):126–127. [Google Scholar]
- 12.Chen S. H., Zhang X. H., L M. Neonatal death analysis in 112 hospitalized cases. He Bei Yi Xue. 2003;9(01):55–57. [Google Scholar]
- 13.Ma Z., Li M., D W. Neonatal death analysis in 154 hospitalized cases. Guang Xi Yi Ke Da Xue Xue Bao. 2014;31(4):657–660. [Google Scholar]
- 14.Liang J. P., Yang R. L., Ml H. Neonatal death analysis in 223 cases. Zhong Guo Fu You Bao Jian. 2005;20(22):2292–2293. [Google Scholar]
- 15.Wang H., Li W. Neonatal death analysis in 235 cases. Xiao Er Ji Jiu Yi Xue. 2002;9(01):30–31. [Google Scholar]
- 16.Liu J. Neonatal death analysis in 305 cases. Dang Dai Yi Xue. 2011;17(19):92–93. [Google Scholar]
- 17.Xu F. D., Kong X. Y., Zc F. Neonatal mortality and death in 480 cases. Zhong Guo Dang Dai Er Ke Za Zhi. 2017;19(02):153–158. doi: 10.7499/j.issn.1008-8830.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang L. Dynamic statistical analysis in 537 hospitalized neonates. Zhong Guo Fu You Bao Jian. 2013;28(28):2716–2763. [Google Scholar]
- 19.Zhang J. J., Wang J. X. Neonatal death analysis between 2003 and 2012. Zhong Guo Fu You Bao Jian. 2013;28(17):4663–4665. [Google Scholar]
- 20.Li J., Sun J. H. Neonatal death analysis in 207 cases. Zhong Guo Er Tong Bao Jian Za Zhi. 2008;16(04):445–446. [Google Scholar]
- 21.Shen S. H., Dg H. Neonatal death analysis in 45 cases. Zhong Guo Re Dai Yi Xue. 2005;5(01):174–175. [Google Scholar]
- 22.Luo X. N., Xj Z. Neonatal death analysis in Chongqing City between 2005 and 2008 in 1297 cases. Chong Qiong Yi Xue. 2009;38(24):3084–3086. [Google Scholar]
- 23.Bai X. H., Xiong Y., Ds Z. Neonatal death analysis in 180 hospitalized cases. Zhong Guo Xin Sheng Er Ke Za Zhi. 2013;28(02):88–91. [Google Scholar]
- 24.Tao C. L., Xu X., Hy C. Neonatal death analysis between 2003 and 2007. Zhong Hua Quan Ke Yi Xue. 2008;6(09):960–961. [Google Scholar]
- 25.Tang H. Q., Jiang Y., HQ L. Neonatal death analysis in 263 cases. Zhong Guo Er Tong Bao Jian Za Zhi. 2013;21(11):1220–1222. [Google Scholar]
- 26.Ouyang X. D., Zhang J. Neonatal death analysis in 235 cases. Zhong Guo Xian Dai Yi Sheng. 2014;54(11):35–38. [Google Scholar]
- 27.WHO. Newborns: Reducing Mortality [EB/OL] 2018. http://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality. [Google Scholar]
- 28.Speights J. S. B., Goldfarb S. S., Wells B. A., Beitsch L., Levine R. S., Rust G. State-level progress in reducing the black-white infant mortality gap, United States, 1999-2013. American Journal of Public Health. 2017;107(5):775–782. doi: 10.2105/AJPH.2017.303689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Balsara S. L., Faerber J. A., Spinner N. B., Feudtner C. Pediatric mortality in males versus females in the United States, 1999-2008. Pediatrics. 2013;132(4):631–638. doi: 10.1542/peds.2013-0339. [DOI] [PubMed] [Google Scholar]
- 30. http://www.nhfpc.gov.cn/zwgkzt/pgb/201104/51512.shtml.
- 31.Travasso C. Neonatal mortality almost halved in India between 1990 and 2012. BMJ. 2014;349 doi: 10.1136/bmj.g5772.g5772 [DOI] [PubMed] [Google Scholar]
- 32.Khadka K. B., Lieberman L. S., Giedraitis V., Bhatta L., Pandey G. The socio-economic determinants of infant mortality in Nepal: Analysis of Nepal Demographic Health Survey, 2011. BMC Pediatrics. 2015;15(152) doi: 10.1186/s12887-015-0468-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Altman M., Bonamy A.-K. E., Wikström A.-K., Cnattingius S. Cause-specific infant mortality in a population-based Swedish study of term and post-term births: The contribution of gestational age and birth weight. BMJ Open. 2012;2(4) doi: 10.1136/bmjopen-2012-001152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pulver L. S., Guest-Warnick G., Stoddard G. J., Byington C. L., Young P. C. Weight for gestational age affects the mortality of late preterm infants. Pediatrics. 2009;123(6):e1072–e1077. doi: 10.1542/peds.2008-3288. [DOI] [PubMed] [Google Scholar]
- 35.Institute of Medicine Committee on Improving Birth O. In: Improving Birth Outcomes: Meeting the Challenge in the Developing World. Bale J. R., Stoll B. J., Lucas A. O., editors. Washington (DC), USA: National Academies Press; 2003. [PubMed] [Google Scholar]
- 36.The Alliance for Maternal and Newborn Health Improvement (AMANHI) Mortality Study Group. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-Saharan Africa: a multi-country prospective cohort study. Lancet Glob Health. 2018;6(12):e1297–e1308. doi: 10.1016/S2214-109X(18)30385-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seske L. M., Muglia L. J., Hall E. S., Bove K. E., Greenberg J. M. Infant mortality, cause of death, and vital records reporting in Ohio, United States. Maternal and Child Health Journal. 2017;21(4):727–733. doi: 10.1007/s10995-016-2159-x. [DOI] [PubMed] [Google Scholar]
- 38.Mathews T. J., Driscoll A. K. Trends in infant mortality in the United States, 2005-2014. NCHS Data Brief. 2017;(279):1–8. [PubMed] [Google Scholar]
- 39.Chen A., Oster E., Williams H. Why is Infant Mortality Higher in the US than in Europe? American Economic Journal. 2016;8(2):89–124. doi: 10.1257/pol.20140224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carlo W. A., McClure E. M., Chomba E., et al. Newborn care training of midwives and neonatal and perinatal mortality rates in a developing country. Pediatrics. 2010;126(5):e1064–e1071. doi: 10.1542/peds.2009-3464. [DOI] [PubMed] [Google Scholar]
- 41.Carlo W. A., Goudar S. S., Jehan I., et al. High mortality rates for very low birth weight infants in developing countries despite training. Pediatrics. 2010;126(5):e1072–e1080. doi: 10.1542/peds.2010-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data were available upon appropriate request.