Despite significant strides in our ability to treat cardiac disease over the past half a century, heart disease remains the leading cause of death, and acute cardiac events such as acute myocardial infarction (AMI) and sudden cardiac death (SCD) account for a majority of these. There remains a significant need to predict who will develop an acute cardiac event, and when and how to intervene in a person at high risk.
Patients often have warning symptoms in the days to week before an AMI or SCD.1, 2 Constructive use of this information, especially with ongoing innovations in communication and wireless technologies, could potentially be used to predict and prevent such events. Warning signs differ from acute symptoms in that they are experienced before the actual event. In addition to angina and respiratory complaints, they frequently involve generalized fatigue, anxiety, and influenza-like symptoms. However, they can be nonspecific, and there is likely to be significant overlap between those that precede AMI, SCD, or even non-cardiac conditions. The mere presence of prodromal symptoms has been shown to improve survival in both AMI and SCD. Lower mortality rates were noted in Canadian women with AMI who had previously reported prodromal symptoms to a health care provider (risk-adjusted mortality, 8.7% vs 11.1%), but were not different among men.1 In the population-based Oregon Sudden Unexpected Death Study (SUDS), at least 50% of individuals who experienced SCD had warning symptoms in the 4 weeks preceding their lethal event.2 Those who called 911 immediately following their symptoms were significantly more likely to survive to hospital discharge in comparison with those for whom 911 was contacted during a later time period.
It is possible that warning signs correlate with prognosis after AMI or SCD because patients with warning signs call for help and subsequently receive earlier treatment. In cases with sufficient time between onset of prodrome and the acute event, it might be possible to avert cardiac arrest or AMI in patients with clear warning signs if they are acted on. Their non-specific nature, however, poses a challenge to this notion, because asking every patient with a warning sign to seek early care would certainly over-burden the emergency response and advance cardiac care systems. One solution may be to combine information about these symptoms with individual clinical risk profiles and with smartphone or wearable generated real-time physiological measures to identify those at highest risk for an acute cardiac event. No mobile application (app) has been previously described or designed that combines acute cardiac disease symptom tracking with other known acute cardiac disease risk factors. The heart failure community, however, has developed several symptom-tracking commercial apps designed to support patients managing heart failure symptoms that have been shown to be well liked and usable among a wide range of demographics and could serve as a model for the development of a warning signs/symptoms-tracking app.3 One example of an app with demonstrated effectiveness is Heart Failure Storylines from Self Care Catalysts Inc (http://www.hfsa.org/patient/patient-tools/patient-app/) developed in partnership with the Heart Failure Society of America. On this platform, patients with heart failure record symptoms and severity, current mood, medication use, and vital signs into the program. The app tracks these data and attempts to detect potential correlations between symptoms and time periods. Users also have the option to input data from other health and fitness apps and email this information to their friends or family.
Several companies make smartphone-based electrocardiographic capture systems for arrhythmia screening and have the capacity to facilitate early transmission of information to health care providers. One of these platforms, AliveCor (www.alivecor.com), enables users to record a single-lead ECG on their smartphone. The device includes 2 electrodes and attaches directly to the back of a patient’s mobile phone or its case. A 30-second real-time ECG equivalent to lead I on a 12-lead ECG is recorded by activating the app and placing at least one finger from each hand onto the electrodes. The user can also annotate the recorded ECG with symptom data. Their personal data and recorded ECGs are then stored on a secure server that can be accessed online by the patient or by a health care professional via AliveCor’s website. Although there are early data that show promise with single-lead smartphone systems, more development is required in this area, including advancement to multiple-lead systems.
A group in Australia has developed a model for an app that could be used for recognition of impending AMI, entitled heart attack self-test.4 In their schema, a user first inputs personal health and demographic data into the proposed mobile app. At the onset of symptoms, the patient starts the program and is asked to answer several yes or no questions including, “Do you feel discomfort around your chest?” and “Do you feel dizzy, weak, or anxious?” Based on their replies and the personal data and medical history stored in the system, the proposed app determines the degree of risk of AMI and, if elevated, the program has the capacity to directly dial 911. If the answers indicate that the user is at a low risk or the user declines calling emergency medical services, the app asks the user to obtain an ECG recording. The app then analyzes the ECG, and, if the ECG is concerning for AMI, the device either urges the user to dial 911 or alerts emergency medical services automatically. 4 This app is not available commercially.
A mobile app designed to identify individuals at highest risk for acute cardiac disease (Figure) would potentially combine user-input warning sign symptom data with demographic data, physiological measures such as heart rate and blood pressure from biometric sensors, and a smartphone-generated ECG to generate a risk score for impending acute cardiac disease. This score would facilitate an individualized recommendation for whether a person should seek emergent, urgent, or nonurgent evaluation by medical personnel. Specific abnormal ECG markers have been correlated with increased risk of SCD. 5 These ECG markers could potentially be extracted from smartphone-based electrocardiographic capture systems to refine the risk profile of a patient with prodromal symptoms. The goal would be the encouragement of individuals with prodromal symptoms who are at highest risk for AMI or SCD to seek early care before actual plaque rupture or cardiac arrest occurs. Care must be taken to balance encouragement of patients at highest risk to seek care while avoiding false positives that may result in unnecessary health care evaluation. Such a paradigm shift will require significant further investigation in carefully designed prospective observational studies to evaluate effectiveness, followed by randomized clinical trials in patients at increased risk of acute cardiac disease.
Central Illustration.
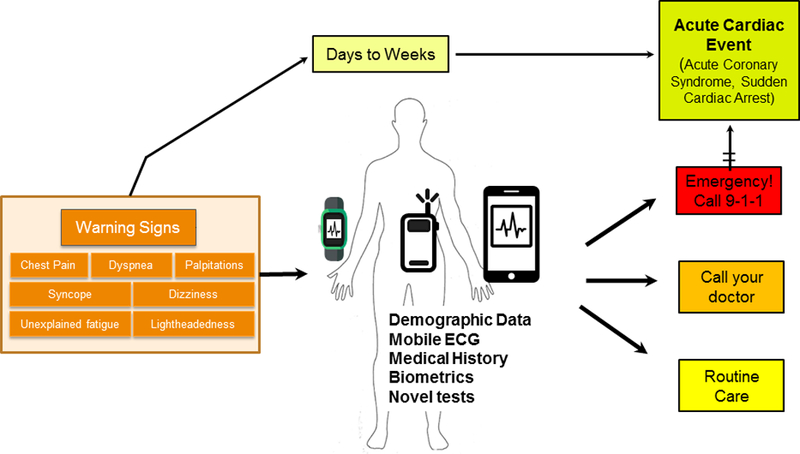
The concept for A mobile app designed to identify individuals at highest risk for an acute cardiac event. A smartphone-based platform would combine user-inputted warning signs/symptoms data with demographic data, physiologic measures such as heart rate and blood pressure from biometric sensors, and a smartphone-generated ECG to generate a risk score for impending acute cardiac disease. Novel platforms for noninvasive monitoring of biomarkers could be integrated, once these are developed and validated. This could provide an individualized recommendation for whether an individual should seek emergent, urgent, or non-urgent evaluation by medical personnel.
Acknowledgments
Sources of Funding: Funded by the National Institutes of Health, National Heart, Lung, and Blood Inssitute (NHLBI) grants R01HL122492 and R01HL126938 to Dr Chugh. Dr Chugh holds the Pauline and Harold Price Chair in Cardiac Electrophysiology at Cedars-Sinai Health System, Los Angeles.
Footnotes
Disclosures: The authors have no relationships with industry.
References
- 1.Graham MM, Westerhout CM, Kaul P, Norris CM and Armstrong PW. Sex differences in patients seeking medical attention for prodromal symptoms before an acute coronary event. Am Heart J. 2008;156:1210–1216 e1. [DOI] [PubMed] [Google Scholar]
- 2.Marijon E, Uy-Evanado A, Dumas F, Karam N, Reinier K, Teodorescu C, Narayanan K, Gunson K, Jui J, Jouven X and Chugh SS. Warning Symptoms Are Associated With Survival From Sudden Cardiac Arrest. Ann Intern Med. 2016;164:23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masterson Creber RM, Maurer MS, Reading M, Hiraldo G, Hickey KT and Iribarren S. Review and Analysis of Existing Mobile Phone Apps to Support Heart Failure Symptom Monitoring and Self-Care Management Using the Mobile Application Rating Scale (MARS). JMIR mHealth and uHealth. 2016;4:e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leijdekkers P, Gay V. A Self-Test to Detect a Heart Attack Using a Mobile Phone and Wearable Sensors. 21st IEEE International Symposium on Computer-Based Medical Systems. 2008:93–98. [Google Scholar]
- 5.Aro AL, Reinier K, Rusinaru C, Uy-Evanado A, Darouian N, Phan D, Mack WJ, Jui J, Soliman EZ, Tereshchenko LG and Chugh SS. Electrical risk score beyond the left ventricular ejection fraction: prediction of sudden cardiac death in the Oregon Sudden Unexpected Death Study and the Atherosclerosis Risk in Communities Study. Eur Heart J. 2017;38:3017–3025. [DOI] [PMC free article] [PubMed] [Google Scholar]


