Abstract
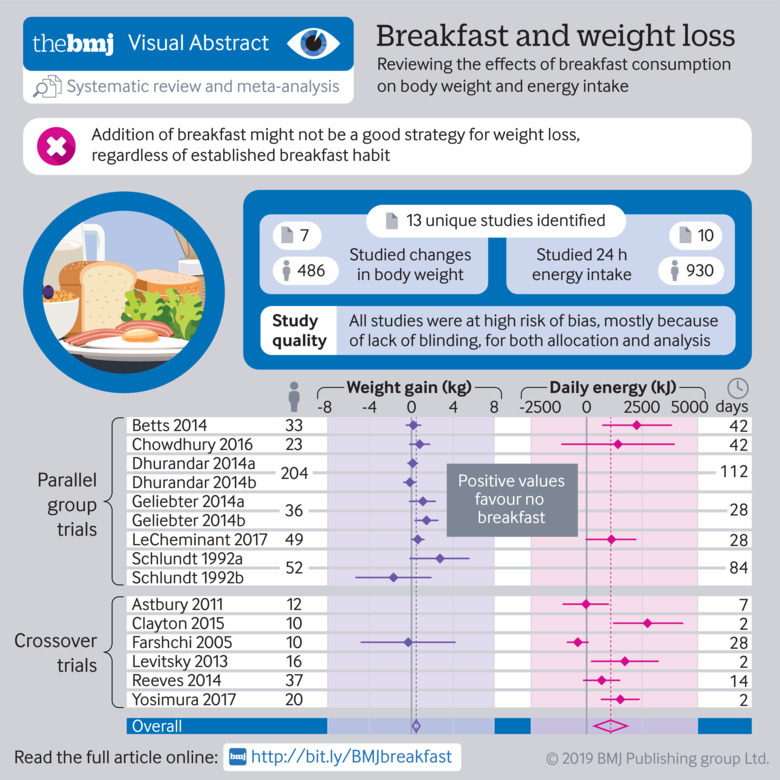
Objective
To examine the effect of regular breakfast consumption on weight change and energy intake in people living in high income countries.
Design
Systematic review and meta-analysis.
Data sources
PubMed, Ovid Medline, and CINAHL were searched for randomised controlled trials published between January 1990 and January 2018 investigating the effect of breakfast on weight or energy intake. ClinicalTrials.gov and the World Health Organization’s International Clinical Trials Registry Platform search portal were also searched in October 2018 to identify any registered yet unpublished or ongoing trials.
Eligibility criteria for selecting studies
Randomised controlled trials from high income countries in adults comparing breakfast consumption with no breakfast consumption that included a measure of body weight or energy intake. Two independent reviewers extracted the data and assessed the risk of bias of included studies. Random effects meta-analyses of the effect of breakfast consumption on weight and daily energy intake were performed.
Results
Of 13 included trials, seven examined the effect of eating breakfast on weight change, and 10 examined the effect on energy intake. Meta-analysis of the results found a small difference in weight favouring participants who skipped breakfast (mean difference 0.44 kg, 95% confidence interval 0.07 to 0.82), but there was some inconsistency across trial results (I2=43%). Participants assigned to breakfast had a higher total daily energy intake than those assigned to skip breakfast (mean difference 259.79 kcal/day, 78.87 to 440.71; 1 kcal=4.18 kJ), despite substantial inconsistency across trial results (I2=80%). All of the included trials were at high or unclear risk of bias in at least one domain and had only short term follow-ups (mean period seven weeks for weight, two weeks for energy intake). As the quality of the included studies was mostly low, the findings should be interpreted with caution.
Conclusion
This study suggests that the addition of breakfast might not be a good strategy for weight loss, regardless of established breakfast habit. Caution is needed when recommending breakfast for weight loss in adults, as it could have the opposite effect. Further randomised controlled trials of high quality are needed to examine the role of breakfast eating in the approach to weight management.
Study registration
PROSPERO registration number CRD42017057687.
Introduction
Obesity is considered to be one of the defining health issues of this time and is recognised as the most prevalent form of malnutrition worldwide, with rapidly increasing rates globally.1 The association of obesity with increased risk of chronic diseases (eg, cardiovascular disease, diabetes, and osteoarthritis) means that it is the major contributor to the global burden of disease.2 3 4 In high income countries, weight gain is rising in incidence across all population groups, thus efforts to manage the effects of this problem have been undertaken by government and public health organisations.
Although strategies aimed at prevention and management of obesity must be multifactorial, many international dietary recommendations suggest the regular inclusion of breakfast for weight management and as a protective factor against obesity (table 1). These recommendations are often derived from the presumption that skipping breakfast leads to energy overcompensation later in the day.11 Furthermore, it is postulated that the satiating properties of food over the course of the day decline12 and, therefore, eating earlier in the day could promote greater satiety than eating later in the day. However, despite this common recommendation for weight control by both health professionals13 14 and the lay community,15 16 17 most of these recommendations are based on the findings of observational studies.18 19 20 21 These concepts have potential for selection bias and confounding, because those individuals who eat breakfast might differ from those who do not in several ways, including socioeconomic status and the adoption of other health related behaviours such as the consumption of a healthy diet. A recent study has challenged the presumption of breakfast and weight control by examining the findings of two randomised controlled trials that showed no effect on weight.22 Additionally, recent results from several randomised controlled trials do not generally support a beneficial effect of breakfast eating on weight loss.23 24 Recommending regular breakfast consumption could adversely affect weight control by adding calories to diets, especially in older people with established eating behaviours, because past food habits are important predictors of current food habits.25
Table 1.
International recommendations for breakfast in 2010-18
| Country | Source | Recommendation |
|---|---|---|
| United Kingdom5 6 | British Dietetic Association (2016) and Eatwell Guide (2016): https://www.bda.uk.com/foodfacts/healthy_breakfast, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/742750/Eatwell_Guide_booklet_2018v4.pdf | “Skipping breakfast won’t help you lose weight. You could miss out on essential nutrients and you may end up snacking more throughout the day because you feel hungry.” |
| Australia7 | Dieticians Association of Australia (2013): https://daa.asn.au/resource/breakfast-cereals-and-body-weight-fact-sheet/ | “Research shows that consuming breakfast regularly is associated with lower levels of overweight and obesity. Breakfast fills you up, meaning you are less likely to experience hunger pangs throughout day and resort to snacking on high energy, high fat foods.” |
| United States8 | Academy of Nutrition and Dietetics: adult weight management (2014): https://www.andeal.org/vault/pq132.pdf | “The majority of observational research reported that breakfast consumption is associated with a lower BMI and decreased obesity risk, while omitting breakfast is associated with a higher BMI and increased obesity risk. Several studies suggest that cereal-based breakfasts are associated with lower BMI, while breakfasts that are very high in energy are associated with higher BMI” |
| Ireland9 | Food Safety Authority of Ireland: scientific recommendations for healthy eating guidelines (2011), p58: https://www.fsai.ie/recommendationsforhealthyeatingguidelinesinireland.html | “[When watching weight] Never skip meals; breakfast is especially important” |
| New Zealand10 | Food and nutrition guidelines for healthy children and young people (2015): www.health.govt.nz/publication/food-and-nutrition-guidelines-healthy-children-and-young-people-aged-2-18-years-background-paper | “Breakfast consumption is associated with a range of positive outcomes, including better nutrient intake and a healthy body weight.” |
BMI=body mass index.
Thus, the aims of this review were to examine the evidence from randomised controlled clinical trials of the effect of regular breakfast consumption on weight change (weight loss/weight gain), and daily energy intake in people living in high income countries.
Methods
Our systematic review was reported in accordance with the 2009 PRISMA statement.26 Our review protocol was registered with PROSPERO in February 2017 (registration number CRD42017057687).
Search strategy
We searched for articles indexed in PubMed, Ovid Medline, and CINAHL that were published between January 1990 and January 2018 (search strategy available in supplementary table 1). The search was limited to adult human studies published in the English language. The reference lists of recent reviews and included studies were screened for additional references. We also searched ClinicalTrials.gov and the World Health Organization’s International Clinical Trials Registry Platform search portal in October 2018 to identify any registered yet unpublished or ongoing randomised controlled trials. In both trials registers, we used only one search term: “breakfast.”
Study selection, inclusion and exclusion criteria
We included randomised controlled trials in adults that compared breakfast consumption with no breakfast consumption or skipping breakfast and included a measure of either self reported or measured body weight or energy intake. Studies had to have reported at least one of these primary outcomes. Owing to the varying nature of breakfast definitions, only studies that defined breakfast according to content or timing were included. We excluded studies if they compared breakfast content without assessing the role of breakfast on weight management, change in weight, or energy intake. Moreover, studies conducted in children or adolescents, or in populations with comorbidities other than overweight or obesity such as diabetes or binge eating disorder, were also excluded. We set a 28 year search limit because eating patterns more than 30 years ago are likely to have changed considerably from patterns in the past few decades, in accordance with natural changes in population dietary patterns.27 We chose to include studies conducted in high income country settings as defined by the World Bank definition of high income,28 because dietary habits vary immensely across resource limited settings.
KS did the search while SMH adjudicated. Two authors (KS and Cate Lombard) independently screened all titles and abstracts and retrieved the full text of any article considered definitely or possibly eligible. Both authors then reviewed the full text articles against the eligibility criteria. Any disagreement between the two authors was resolved by discussion.
Data extraction
Data on the characteristics of the included studies were extracted independently by pairs of reviewers (KS and YW or HJH), including (1) study design, study population, number of participants, mean age and percentage of female participants; (2) intervention details; (3) energy consumption; (4) outcome measures and weight measurement; and (5) study results for weight loss and energy intake. A third reviewer (SMH or MJP) checked the extracted data for any errors. If data were not available in numerical format, we estimated it from figures using WebPlotDigitizer.29
Risk of bias assessment
Pairs of authors (KS and MJP or MM) independently assessed the risk of bias of each included trial. Any disagreements were discussed between the two authors, and another author (FMC) gave a final judgment if no consensus could be reached. Trials were assessed using Cochrane’s tool for assessing risk of bias in randomised trials.30 The tool includes the following domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. We rated each domain as low risk, unclear risk, or high risk of bias. We classified the overall risk of bias as low if all domains were at low risk of bias, as high if at least one domain was at high risk of bias, or as unclear if at least one domain was at unclear risk of bias and no domain was at high risk. This rule is specified by the Cochrane tool for assessing risk of bias in randomised controlled trials, because any source of bias in a trial is problematic and there is a paucity of empirical research to prioritise one domain over the other.30
Data analysis
Results for all outcomes were expressed as mean differences with 95% confidence intervals, calculated from either end of treatment values or change from baseline values. Across the trials, results for weight were always presented in kilograms, whereas results for total daily energy intake were presented as kilocalories per day, kilojoules per day, or megajoules per day. Where required, we converted means and standard deviations for total daily energy intake into kilocalories per day (kcal/day; 1 kcal=4.18 kJ=0.00418 MJ).
We included several crossover trials that did not present results of a paired analysis, and that did not report correlations between baseline and end of study data, thereby ignoring within-person variation. We reanalysed the data from these studies assuming different correlation coefficients when estimating the standard error of the mean difference, using formulas provided in the Cochrane Handbook for Systematic Reviews of Interventions.31 We included in meta-analyses the results based on the most conservative approach, assuming a correlation coefficient of 0.3, and conducted sensitivity analyses assuming the following correlation coefficients: 0.5, 0.7, and 0.9. For any multiarm trials identified (eg, comparing breakfast A v breakfast B v no breakfast), we included each pairwise comparison in the meta-analysis (that is, breakfast A v no breakfast, and breakfast B v no breakfast) by dividing the control group sample size in half.
We synthesised estimates of mean difference using a random effects meta-analysis model, based on the assumption that clinical and methodological heterogeneity was likely to exist and to have an effect on the results. We used the DerSimonian and Laird method of moments estimator to estimate the between-study variance, and calculated 95% confidence intervals using the Wald type method.32 Statistical inconsistency was quantified by use of the I2 statistic.33 We generated contour enhanced funnel plots to investigate small study effects (the tendency for intervention effects estimated in smaller studies to differ from those estimated in larger studies, which can result from reporting biases, methodological or clinical heterogeneity, or other factors).34 All analyses were conducted using the metan and confunnel packages in Stata version 14.35
Patient and public involvement
Although this research contained no direct patient or public involvement, the research question was informed by work with a consumer organisation identifying patient needs in musculoskeletal disease36 and an audit of consumer with knee and hip pain to identify health beliefs in weight management.37
Results
Search results
The search of the three electronic databases identified 1868 records with 604 articles remaining after the removal of duplicates. Of these, 552 articles were excluded after screening titles and then abstracts, because these studies did not meet selection criteria (eg, did not include breakfast intake as an intervention, did not focus on adult participants, or were reviews or conference papers). Of the 52 retrieved articles, 39 studies were excluded after full text review because they were not a randomised controlled trial, weight or energy intake was not measured as an outcome, and the intervention was not breakfast consumption. Thus 13 trials were identified as eligible for inclusion in the review (fig 1).23 24 38 39 40 41 42 43 44 45 46 47 48 From our searches of trials registers, we identified five ongoing trials that are potentially eligible for inclusion in a future update of our review (register numbers NCT03134014, NCT02093572, NCT03257059, NCT03146442, and NCT03031132). Seven trials examined the relation between breakfast consumption or omission and changes in body weight (n=486), and 10 trials examined the effect of breakfast consumption on 24 hour energy intake (n=930).
Fig 1.
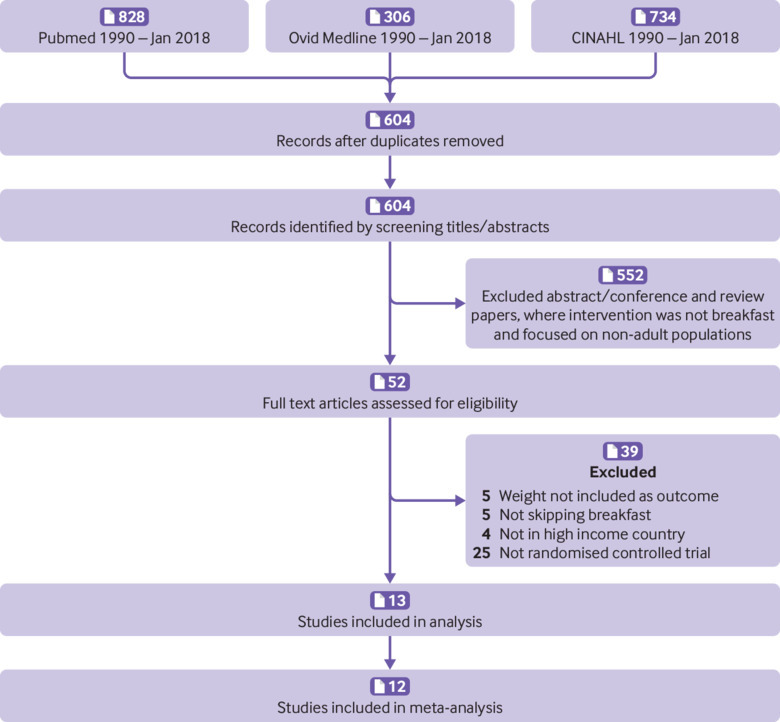
PRISMA flow diagram of included articles
Characteristics of included trials
The characteristics of the included trials are presented in table 2. Most trials were carried out in the United States24 41 43 44 46 47 and the United Kingdom.23 38 39 40 42 45 One trial was from Japan.48 Five trials included participants specifically with overweight or obesity23 41 43 46 47; the remaining trials included people with any weight range, including normal body weight, overweight, and obesity.24 38 39 40 42 44 45 48 Most of the included participants were community based,23 24 39 40 41 43 45 46 47 48 with the exception of two trials that included hospital workers38 42 and one trial that included university students.44
Table 2.
General characteristics of included studies
| Author (country, year of publication) | Baseline participant characteristics | Intervention group | Control group | Assessment of exposure | Outcome measures | Duration of study | |||
|---|---|---|---|---|---|---|---|---|---|
| No of participants | Population (BMI; mean (SD)) | Age (years; mean (SD)*) | |||||||
| Astbury (UK, 2011)38 | 12 (0% female) | Healthy hospital workers (students and staff; 23.5 (1.7)) | 23.4 (7.3) | Breakfast arm: participants were asked to consume Rice Krispies (Kelloggs) and semi-skimmed milk at 7 45 am. After 150 min, a liquid pre-load meal was given. Lunch meal was provided 90 min later. | No breakfast arm: only pre-load and lunch meal provided. | Direct visual monitoring | Energy intake | 7 days | |
| Betts (UK, 2014)39 | 33 (64% female) | Healthy normal and overweight community dwelling adults (24.4 (22)) |
36 (11) | Breakfast: energy intake of >700 kcal before 11 am daily, with at least half consumed within 2 hours of waking. | No breakfast arm: plain water only until noon daily. | Self administered intake | Weight loss in kg, energy intake | 6 weeks | |
| Chowdhury (UK, 2016)23 | 23 (65% female) | Healthy obese community dwellers (33 (4.9)) |
44 (10) | Breakfast arm: energy intake ≥700 kcal before 11 am daily, with at least half consumed within 2 hours of waking. | No breakfast arm: fasting until noon each day | 7 day food diary | Weight loss in kg, energy intake | 6 weeks | |
| Clayton (UK, 2015)40 | 10 (0% female) | Healthy active community dwellers who regularly consume breakfast (23.5 (3.2)) |
22 (3) | Breakfast arm: participants consumed a standardised breakfast of 25% estimated daily energy requirements, breakfast consisted of crisped rice cereal, semi-skimmed milk, white bread, butter, strawberry jam, and orange juice. After 4.5 hours, ad libitum lunch was provided, and then after 11 hours, ad libitum dinner | No breakfast arm: participants ingested water (624 mL) to match water contained in the breakfast group, and nothing else until lunch. | Direct visual monitoring | Energy intake | 2×24 h | |
| Dhurandhar (US, 2014)49 | 204 (82.6% female) | Healthy overweight and obese adult community dwellers | 42 (11.2) | Intervention in two groups—habitual breakfast skippers and breakfast eaters. Breakfast arm: received the same pamphlet and instructions for participants to consume breakfast before 10 am every day, accompanied with healthy breakfast food suggestions. | No breakfast arm: received the same pamphlet with instructions for participants not to consume any kJ before 11 am every day (water, 0 kJ beverages allowed). | 7 day food diary | Weight loss in kg | 16 weeks | |
| Farshchi (UK, 2005)42 | 10 (100% female) | Lean healthy hospital workers (medical students and clinicians; 23.2 (1.6)) | 25.5 (5.7) | Participants allocated to two intervention arms, differing by timing of standardised meal consumption. Breakfast arm: received bran cereal between 7 and 8 am, and a chocolate covered cookie between 10 30 and 11 am. | No breakfast arm: received a chocolate covered cookie between 10 30 and 11 am, and bran cereal between 12 and 12 30 am. | Direct visual monitoring | Weight loss in kg, energy intake | 2×14 days | |
| Geliebter (US, 2014)43 |
36 (50% female) | Healthy overweight adult community dwellers (32 (4.7)) | 33 (7.5) | Oat porridge arm: oat porridge made with whole milk served with 200 mL of decaffeinated coffee. Frosted cornflake arm: Kellogg’s Frosted Flakes served with low fat milk with 200 mL of decaffeinated coffee. | No breakfast arm (control): 350 mL of water with 200 mL of decaffeinated coffee. | Direct visual monitoring | Weight loss in kg | 4 weeks | |
| LeCheminant (US, 2017)24 | 49 (100% female) | Healthy women who did not regularly consume breakfast aged 18-55 years | Not reported | Breakfast arm: energy intake ≥15% of their total energy intake within 1.5 hours of waking, and finished by 8 30 am. | No breakfast arm: fasting until 11 30 am each day. | 7 day food diary | Weight loss in kg, energy intake | 4 weeks | |
| Levitsky study 2 (US, 2013)44 | 16 (81% female) | Healthy university students (24.1 (2.2)) | 24.0 (2.8) | Two groups matched by body weight. Breakfast arm: ad libitum breakfast from 8 45 am, followed by lunch, snacks, and dinner as above. |
No breakfast arm: no food or drink before 11 am. Lunch, snacks, and dinner served buffet style from 11 am and 5 pm, respectively. | Direct visual monitoring | Energy intake | 2×24 hours | |
| Reeves (UK, 2014)45 | 37 (57% female) | Healthy adult community dwellers (group 1, normal weight, 21.31 (1.79); group 2, overweight, 29.63 (5.32)) | Group 1, 29.5 (7.9); group 2, 36.2 (16.3) |
Intervention in two groups—normal weight and overweight. Breakfast arm: first meal to be consumed within 1 hour of waking. | No breakfast arm: no meals to be consumed before midday. | 7 day food diary | Energy intake | 2×7 days | |
| Schlundt (US, 1992)46 | 52 (100% female) | Community dwelling obese women (30.6 (0.5)) | 18-55 years | Intervention in two groups—habitual breakfast skippers and breakfast eaters. Breakfast arm: received weight loss instructions to consume three meals per day, including breakfast. | No breakfast arm: received weight loss instructions to consume only two meals per day, lunch and dinner. | 7 day food diary | Weight loss in kg | 12 weeks | |
| Thomas (US, 2015)47 | 18 (100% female) | Healthy overweight women who either regularly omitted or consumed breakfast (median 30.2 (IQR 28.6-33.7)) |
Median 29 (IQR 27-32) | Breakfast arm: 250 mL water plus wheat flakes plus milk, scrambled eggs, and orange juice. | No breakfast arm: 250 mL water only | Direct visual monitoring | Energy intake | 2×8 hours | |
| Yoshimura (Japan, 2017)48 | 20 (100% female) | Healthy, habitual breakfast eating women | 21.8 (0.9) | Breakfast arm: 30% daily energy intake. | No breakfast arm: water only until noon. | Self administered intake | Energy intake | 2×24 hours | |
BMI=body mass index; IQR=interquartile range; SD=standard deviation; UK=United Kingdom; US=United States. 1 kcal=4.18 kJ=0.00418 MJ.
Unless stated otherwise.
Assessment of intervention: breakfast eating
We saw methodological variations across the trials with regards to the breakfast consumption intervention. Six trials collected data on breakfast consumption by direct monitoring of breakfast intake at laboratory visits,38 40 42 43 44 47 with the remaining seven studies using self administered intake in the form of seven day food diaries or other recall methods.23 24 39 41 45 46 48 Weight and energy intake were measured objectively at study visits in 11 studies23 24 38 39 40 41 42 43 44 46 47; the remaining two studies measured outcomes through participant self report.45 48 Duration of intervention ranged from two42 to 16 weeks41 when examining the effect on weight loss (with some trials also looking at energy intake). Trials exclusively looking at caloric consumption to examine the effect on total daily energy intake ranged in duration from two 24 hour periods39 43 or two 8 hour periods47 up to six weeks.23 24 38 39 40 41 42 43 44 45 46 47
Risk of bias across studies
Full details of the risk of bias assessment for clinical trials are provided in table 3. Among the 13 randomised controlled trials, the main issues were a high risk of bias due to lack of blinding of participants and study personnel and lack of blinding of outcome assessment. Information about random sequence generation and allocation concealment was unclear for most trials. A summary of the proportion of trials that were at low, unclear, and high bias for each domain is shown in figure 2.
Table 3.
Risk of bias assessment in randomised controlled trials
| Author (year) | Sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessors | Incomplete outcome data | Selective reporting | Other bias | Overall risk of bias | |
|---|---|---|---|---|---|---|---|---|---|
| Subjective outcomes | Objective outcomes | ||||||||
| Astbury 2011 | Unclear risk | Unclear risk | High risk | High risk | Not applicable | Low risk | Unclear risk | Low risk | High risk |
| Betts 2014 | Low risk | Low risk | High risk | High risk | Not applicable | Low risk | Low risk | Low risk | High risk |
| Chowdhury 2016 | Low risk | Low risk | High risk | High risk | Not applicable | Low risk | Low risk | Low risk | High risk |
| Clayton 2015 | Unclear risk | Unclear risk | High risk | High risk | Unclear risk | Unclear risk | Unclear risk | Low risk | High risk |
| Dhurandhar 2014 | Low risk | Low risk | High risk | Low risk | Not applicable | Low risk | Unclear risk | Low risk | High risk |
| Farshchi 2005 | Unclear risk | Unclear risk | High risk | High risk | Unclear risk | Unclear risk | Unclear risk | Low risk | High risk |
| Geliebter 2014 | Unclear risk | Unclear risk | High risk | High risk | Low risk | High risk | Unclear risk | Low risk | High risk |
| LeCheminant 2017 | Unclear risk | Unclear risk | High risk | High risk | Unclear risk | Low risk | Unclear risk | Low risk | High risk |
| Levitsky 2013 (study 2) | Unclear risk | Unclear risk | High risk | High risk | Unclear risk | Unclear risk | Unclear risk | Low risk | High risk |
| Reeves 2014 | Unclear risk | Unclear risk | High risk | High risk | Not applicable | Unclear risk | Unclear risk | Low risk | High risk |
| Schlundt 1992 | Unclear risk | Unclear risk | High risk | High risk | Unclear risk | Low risk | Unclear risk | Low risk | High risk |
| Thomas 2015 | Low risk | Unclear risk | High risk | High risk | Unclear risk | Unclear risk | Unclear risk | Low risk | High risk |
| Yoshimura 2017 | Unclear risk | Unclear risk | High risk | High risk | Unclear risk | Low risk | Low risk | Low risk | High risk |
Fig 2.
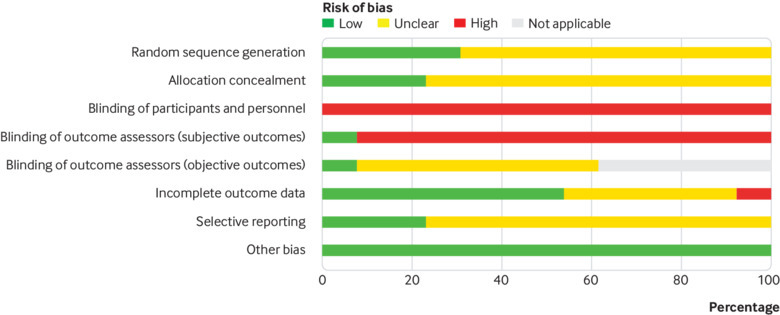
Review authors’ judgments about each risk of bias item, presented as percentages across all included studies. Grey area in the blinding of outcome assessment (objective outcomes) indicates that the domain was not applicable because some trials did not measure any eligible objective outcomes.
Breakfast eating and weight change
Breakfast eating and weight change (kg) was examined in seven studies.23 24 39 41 42 43 46 Two studies examined this effect further by separating experimental groups into habitual breakfast eaters or skippers at baseline41 46; we included both subgroups in the meta-analysis and observed that the mean differences did not significantly differ statistically and were not noticeably different from results in other trials. A random effects meta-analysis of the results revealed that at the end of the trials (mean follow-up seven weeks, range 2-16), there was a small difference in weight favouring participants who skipped breakfast (mean difference 0.44 kg; 95% confidence interval 0.07 to 0.82; fig 3), although there was some inconsistency across trial results (I2=43%). Based on visual inspection of the forest plot, the heterogeneity of results did not appear to be related to the timing of outcome assessment.
Fig 3.
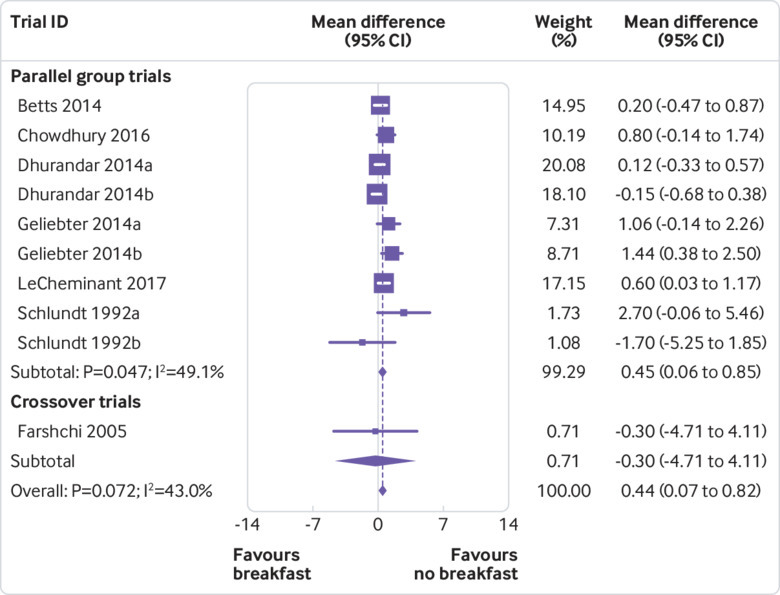
Random effects meta-analysis of the mean difference in weight (kg), based on breakfast consumption or no breakfast consumption. Data for Dhurandhar 2014a are based on the subset of participants who identified as breakfast eaters in general, whereas data for Dhurandhar 2014b are based on the subset of participants who identified as breakfast skippers in general. Data for Geliebter 2014a are based on the comparison of cornflakes with no breakfast, whereas data for Geliebter 2014b are based on the comparison of porridge with no breakfast (sample size for the no breakfast group was halved in each comparison to avoid double counting). Data for Schlundt 1992a are based on the subset of participants who identified as breakfast eaters in general, whereas data for Schlundt 1992b are based on the subset of participants who identified as breakfast skippers in general
We did not detect any evidence that results of smaller trials were systematically different from those of larger trials (fig 4), and our search of trial registers did not identify any registered yet unpublished trials that are missing from this meta-analysis. Furthermore, we conducted a subgroup analysis based on baseline body mass index and found that the effect of breakfast on weight did not differ between trials including participants with normal weight or overweight24 39 42 (mean difference 0.42 kg, 95% confidence interval −0.01 to 0.85) and trials including participants with overweight or obesity23 41 43 46 (0.54 kg, −0.03 to 1.11; supplementary figure 1).
Fig 4.
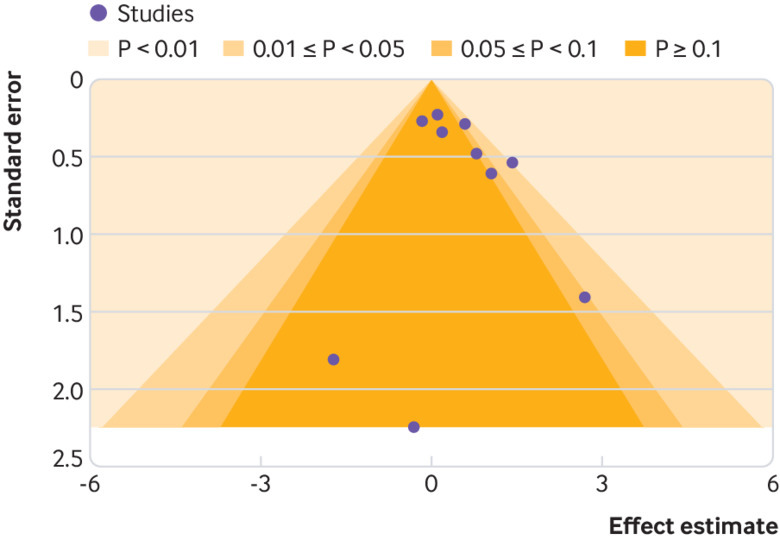
Contour enhanced funnel plot for random effects meta-analysis of mean difference in weight (kg), based on breakfast consumption or no breakfast consumption
Breakfast eating and energy intake
Energy intakes were reported according to breakfast consumption in 10 studies.23 24 38 39 40 42 44 45 47 48 In a random effects meta-analysis of nine studies with usable outcome data, we observed that at the end of the trials (mean follow-up two weeks, range 24 hours to six weeks), participants who were assigned to eat breakfast had a higher total daily energy intake than those assigned to skip breakfast (mean difference 259.79 kcal/day; 95% confidence interval 78.87 to 440.71; fig 5). Thus, breakfast skippers did not compensate their energy intake later in the day. However, we did detect substantial inconsistency across trial results (I2=80%). Based on visual inspection of the forest plot, the heterogeneity of results did not appear to be related to the timing of outcome assessment. Of two studies with markedly different results (both found less total energy intake in the breakfast eating group), both were conducted in populations of hospital workers and students.38 42 Given that health workers (particularly doctors and medical students) are generally more health conscious,50 this factor could have influenced the inconsistent results. We observed some asymmetry in a contour enhanced funnel plot (fig 6). However, reporting biases are unlikely to fully explain this asymmetry, because we suspect that small trials with statistically significant results in favour of eating breakfast would not be disadvantaged in being published given such results are consistent with dietary guidelines. In addition, our search of trials registers did not identify any registered yet unpublished trials that are missing from this meta-analysis.
Fig 5.
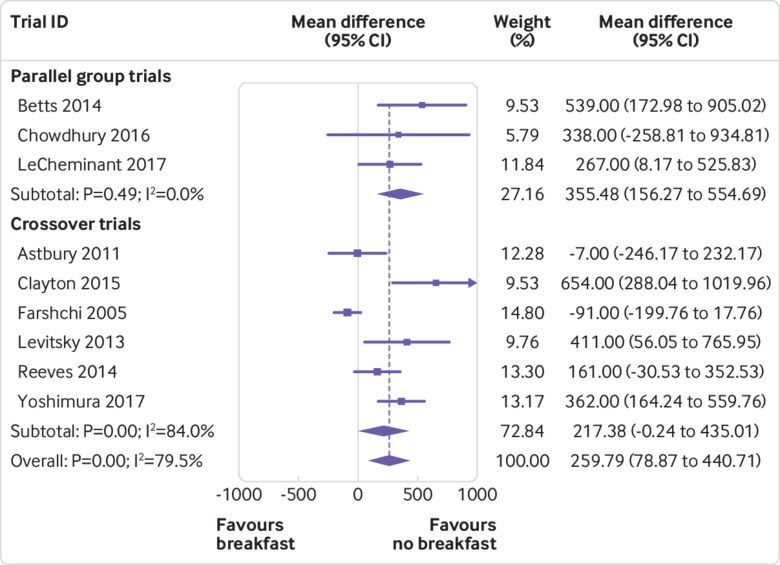
Random effects meta-analysis of the mean difference in total daily energy intake (kcal/day), based on breakfast consumption or no breakfast consumption. 1 kcal=4.18 kJ=0.00418 MJ
Fig 6.
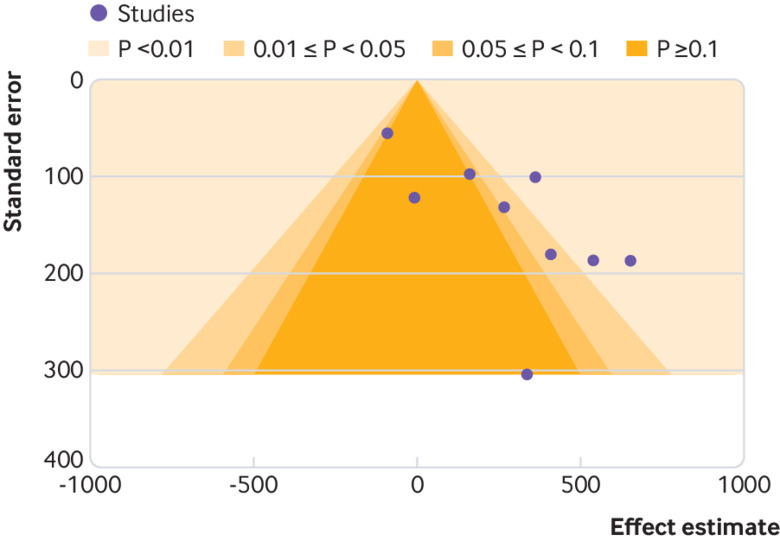
Contour enhanced funnel plot for the random effects meta-analysis of the mean difference in total daily energy intake (kcal/day), based on breakfast consumption or no breakfast consumption. 1 kcal=4.18 kJ=0.00418 MJ
Furthermore, we performed a subgroup analysis excluding the study that recruited only participants with obesity23 and found that it did not have a major impact on the effect of breakfast in regard to total daily energy intake (mean difference 255.89 kcal/day, 95% confidence interval 66.69 to 445.08). To explore whether cultural differences explained our result, we excluded the study conducted in Japan48 and examined studies conducted in the UK and US with regard to the effect of breakfast on calorie intake. We found a minor change in the mean difference (244.61 kcal/day, 49.67 to 439.54). One trial47 could not be included in the meta-analysis of total energy intake because only medians and interquartile ranges were reported; the authors found a higher total energy intake in the breakfast group (median 2516 kcal/day, interquartile range 2363-3324) than in the no breakfast group (2344 kcal/day, 1913-2777) at eight hours’ follow-up. The meta-analysis results for both outcomes were robust in sensitivity analyses assuming different correlation coefficients when estimating the standard error of the mean difference in crossover trials (supplementary table 2).
Discussion
This systematic review of randomised controlled trials examining weight change in adults consuming or skipping breakfast found no evidence to support the notion that breakfast consumption promotes weight loss or that skipping breakfast leads to weight gain. Furthermore, there was evidence to show that breakfast consumption increased total daily energy intake compared with skipping breakfast, with no evidence that skipping breakfast was associated with increased total daily caloric intake. The results were similar when we performed subgroup analyses based on country of origin and baseline body mass index. This review questions the recommendation for breakfast consumption in guidelines aimed at weight loss in adults and has identified a potential concern that the additional calorie intake might actually result in weight gain.
Principal findings
Meta-analysis of the randomised controlled trials did not demonstrate weight loss in participants who consumed breakfast compared with those who did not. Much of the previous support for a positive association between breakfast eating and healthy weight has come from observational studies.20 51 52 However, there are data to suggest that these findings on regular breakfast consumption in observational studies are reflective of a wider healthy lifestyle, in that individuals who are more health conscious and of higher socioeconomic status are more likely to eat breakfast as part of making healthy food choices.52 53 This notion is supported in a 2007 cohort study, which noted that participants who consumed breakfast were also more likely to have lower alcohol intake and higher fibre intake.52 Thus, the discordance between findings from the randomised controlled trials and observational studies are likely to reflect residual confounding by socioeconomic factors and healthy lifestyles and highlight the importance of controlled trials to reduce such confounding.
We also found that total daily energy intake was higher in groups consuming breakfast than in those skipping breakfast, regardless of whether the participants were habitual breakfast consumers or habitual breakfast skippers. Of the nine studies examining calorie intake, four included only habitual breakfast eaters38 40 42 48; one included only non-habitual breakfast eaters,24 three included both,23 39 44 and one included both but examined each separately.45 The trials in habitual breakfast eaters showed that total daily energy intake was lower in the skipping breakfast phase than in the eating breakfast phase.38 40 45 48 The three trials of both habitual and non-habitual breakfast eaters found that daily calorie intake was higher in the breakfast eating arm than in the breakfast skipping arm,23 39 44 while the two trials conducted in only non-habitual breakfast eaters found that the breakfast eating group consumed more daily calories than the breakfast skipping group.24 45
It has been hypothesised that the consumption of calories at breakfast could assist in weight loss due to the efficient metabolising of calories early in the day, leading to prevention of overconsumption later in the day.54 Four of the included studies examined the metabolic rates among the breakfast consumer group and breakfast skipper group and found no significant difference in metabolic rates between the two groups.23 39 42 47 Two of the studies included in this systematic review examined diet induced thermogenesis.23 39 One of the studies, conducted in lean women, found only a small increase in diet induced thermogenesis in the breakfast consumer group (breakfast v non-breakfast, mean 221 (standard deviation 49) kcal/day v 180 (39) kcal/day; P=0.01).39 However, in the other study conducted in women with obesity, researchers found no difference in diet induced thermogenesis (breakfast v non-breakfast, mean 1221 (standard deviation 261) kcal/day v 949 (709) kcal/day; P=0.3).23
Furthermore, a number of the included randomised controlled trials examined a range of hormones involved with appetite regulation and energy balance, including fasting concentrations of leptin,23 39 ghrelin,23 38 39 40 47 glucagon,23 38 39 adiponectin,23 39 glucose,23 38 40 42 47 insulin,23 38 40 42 47 and HOMA-IR (homeostatic model assessment of insulin resistance).23 In most trials, the levels of leptin,23 39 ghrelin,23 39 47 glucagon,23 38 39 adiponectin,23 39 glucose,23 38 39 40 47 insulin,23 38 39 40 47 and HOMA-IR23 did not differ significantly between the intervention and control groups. Taken together, the data do not support the assumption that omitting breakfast might lead to overconsumption of calories later in the day.55 Instead, they suggest that skipping breakfast might be an effective means to reduce total daily energy intake, and that skipping breakfast does not cause greater appetite in the afternoon.
It has been suggested that those who eat breakfast are subsequently more active and therefore have more energy expenditure than those who do not consume breakfast.56 Five of the included studies reported on whether level of physical activity changed after consuming or not consuming breakfast.23 24 39 47 48 Three studies reported no significant difference in physical activity between breakfast consumers and breakfast non-consumers.23 24 47 Two studies found that breakfast consumption was associated with increased physical activity, particularly during the morning.39 48 However, total thermogenesis from daily physical activity was not significantly higher in breakfast consumers than in breakfast non-consumers.
Quality of evidence
We consider the quality of the body of evidence to be low for several reasons. All of the included trials were at high or unclear risk of bias in at least one risk of bias domain and had only short term follow-up; more conclusive results could be drawn with more rigorously conducted trials. We also saw substantial heterogeneity among the trial results for energy intake. This heterogeneity could in part reflect the different populations being examined. For example, the patient populations examined varied from community based populations23 39 40 41 43 45 46 to hospital workers and students.38 42 We focused on high income countries, because dietary habits vary immensely among resource limited settings. However, as obesity is increasingly identified as a public health issue in low and middle income countries,57 it will be important to examine the effect of breakfast consumption in these populations to determine whether it differs in settings where malnutrition might coexist with overnutrition.
Most of the trials included in this systematic review were conducted in the UK23 38 39 40 42 45 or in the US.24 41 43 44 46 47 These populations might differ from those in other high income countries such as Argentina, South Korea, or Saudi Arabia, which do not necessarily follow the same western dietary patterns. However, in this meta-analysis, the types of breakfasts varied across the included studies and tended to focus on healthy options. Thus, although no studies have been performed in other populations, it is likely that if breakfast were to be added to the routine of those individuals who are not habitual breakfast consumers, the results would be similar.
Limitations
This review had several limitations. Firstly, our search strategy could have omitted abstracts that did not state weight or energy intake as an included outcome. This omission could have affected the number of studies included in the analysis, because researchers might have chosen not to report these results owing to the findings being non-significant. Furthermore, the trials included in this review lasted from 24 hours to 16 weeks. Although the difference in calorie intake between breakfast consumers and breakfast skippers was about 260 kcal/day, which could lead to increases in body weight over time, these timeframes make it difficult to draw conclusions about energy intake and change in weight. Longer duration studies are needed to investigate the long term effect of adding or omitting breakfast. In addition, we had to impute missing standard errors of the mean difference for all crossover trials, because paired analyses were not available in any of the included papers. However, results were robust in sensitivity analyses imputing different standard errors.
Conclusions and future implications
As the quality of the included studies was mostly low, the findings should be interpreted with caution. Currently, the available evidence does not support modification of diets in adults to include the consumption of breakfast as a good strategy to lose weight. We also found that overall, modifying diets to include breakfast consumption was associated with an increase in total daily calories. While breakfast has been advocated as the most important meal of the day in the media since 1917,55 58 there is a paucity of evidence to support breakfast consumption as a strategy to achieve weight loss, including in adults with overweight or obesity. Although eating breakfast regularly could have other important effects, such as improved concentration and attentiveness levels in childhood,59 60 caution is needed when recommending breakfast for weight loss in adults, as it could have the opposite effect. Further high quality randomised controlled trials are needed to substantiate whether those individuals seeking to lose weight should skip or consume breakfast and the role of breakfast eating in an overall weight management approach.
What is already known in this topic
Many observational studies have suggested that regular breakfast consumption is associated with low body mass index and is a protective factor against weight gain
Evidence from randomised controlled trials of breakfast consumption has been inconsistent
What this study adds
Modification of diets to include consumption of breakfast might not be a good strategy for weight loss, regardless of established breakfast habit
Caution is needed when recommending breakfast for weight loss in adults, as it could have the opposite effect
As the quality of the included studies was mostly low, the findings should be interpreted with caution; more high quality trials of longer duration are needed to examine the role of breakfast eating in an overall weight management approach
Acknowledgments
We thank our colleague, the late Cate Lombard (Monash Centre for Health Research and Implementation; Monash University Department of Nutrition and Dietetics), who provided her insights and expertise to this manuscript, which greatly assisted the research. Personal disclosures: KS and FMC do not consume breakfast; HJH eats breakfast occasionally; and SMH, MJP, YW, and MM eat breakfast daily.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary material
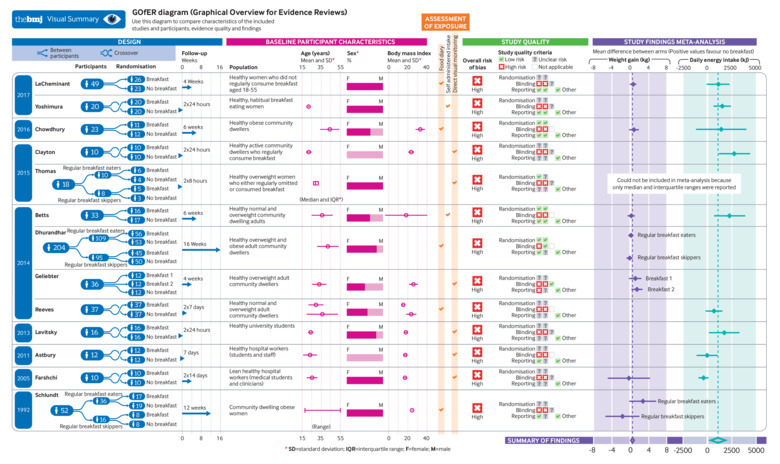
Infographic: Visual summary of trial and participant characteristics
Contributors: KS and SMH share joint first authorship. FMC and CL were involved in designing the study. KS and SMH were involved in searching the database. KS and CL screened citations for inclusion. KS, MJP, and MM were involved in risk of bias analysis. KS, YW, and HJH were involved in extracting data and interpretation. MJP analysed the data. KS, FC, MJP and SMH drafted the manuscript. FMC is study guarantor. All authors reviewed the final manuscript and agreed to be accountable for all aspects of the work and approved the final manuscript for submission. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This study did not receive any specific funding. SMH is supported by an early career fellowship from the National Health and Medical Research Council (NHMRC; No 1142198); YW is the recipient of NHMRC career development fellowships (clinical level 1, No 1065464); MJP is a recipient of an NHMRC early career fellowship (No 1088535).
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required.
Data sharing: The data and statistical analysis code for this paper are available on the Open Science Framework: https://osf.io/sqgn9/.
FMC affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1. NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627-42. 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Peeters A, Backholer K. Is the health burden associated with obesity changing? Am J Epidemiol 2012;176:840-5. 10.1093/aje/kws328 [DOI] [PubMed] [Google Scholar]
- 3. Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377:557-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806-14. 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.British Dietetic Association. Healthy breakfast. 2016. https://www.bda.uk.com/foodfacts/healthy_breakfast
- 6.Public Health England. The Eatwell Guide Booklet. 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/742750/Eatwell_Guide_booklet_2018v4.pdf
- 7.Council NHaMR. Dietary guidelines for all Australians. 2013. https://daa.asn.au/resource/breakfast-cereals-and-body-weight-fact-sheet/
- 8.Academy of Nutrition and Dietetics. Adult weight management (AWM) guideline. 2014. https://www.andeal.org/vault/pq132.pdf
- 9.Food Safety Authority of Ireland. Scientific recommendations for healthy eating guidelines. 2011. https://www.fsai.ie/recommendationsforhealthyeatingguidelinesinireland.html
- 10.New Zealand Ministry of Health. 2012. Food and nutrition guidelines for healthy children and young people (aged 2-18 years): a background paper. Partially revised February 2015. Wellington: Ministry of Health. https://www.health.govt.nz/publication/food-and-nutrition-guidelines-healthy-children-and-young-people-aged-2-18-years-background-paper
- 11. Garaulet M, Gómez-Abellán P. Timing of food intake and obesity: a novel association. Physiol Behav 2014;134:44-50. 10.1016/j.physbeh.2014.01.001 [DOI] [PubMed] [Google Scholar]
- 12. de Castro JM. When, how much and what foods are eaten are related to total daily food intake. Br J Nutr 2009;102:1228-37. 10.1017/S0007114509371640 [DOI] [PubMed] [Google Scholar]
- 13.Association of UK Dietitians. Healthy breakfast fact sheet. 2016. https://www.bda.uk.com/foodfacts/breakfast.pdf
- 14.Academy of Nutrition and Dietetics. 5 tips to kick bad eating habits to the curb. 2016. https://www.andeal.org/vault/pq132.pdf
- 15.Halpert T. 3 breakfast rules to follow to lose weight. Time Magazine. 2015. http://time.com/3667174/weight-loss-breakfast-rules/
- 16.Lerche Davis J. Lose weight: eat breakfast. 2010. https://www.webmd.com/diet/obesity/lose-weight-eat-breakfast
- 17.Haywood S. Breakfast and weight loss. www.weightloss.com.au/diet/diet-articles/breakfast-and-weight-loss.html
- 18. Bjørnarå HB, Vik FN, Brug J, et al. The association of breakfast skipping and television viewing at breakfast with weight status among parents of 10-12-year-olds in eight European countries; the ENERGY (EuropeaN Energy balance Research to prevent excessive weight Gain among Youth) cross-sectional study. Public Health Nutr 2014;17:906-14. 10.1017/S136898001300061X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cho S, Dietrich M, Brown CJ, Clark CA, Block G. The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr 2003;22:296-302. 10.1080/07315724.2003.10719307 [DOI] [PubMed] [Google Scholar]
- 20. O’Neil CE, Nicklas TA, Fulgoni VL., 3rd Nutrient intake, diet quality, and weight/adiposity parameters in breakfast patterns compared with no breakfast in adults: National Health and Nutrition Examination Survey 2001-2008. J Acad Nutr Diet 2014;114(suppl):S27-43. 10.1016/j.jand.2014.08.021 [DOI] [PubMed] [Google Scholar]
- 21. Purslow LR, Sandhu MS, Forouhi N, et al. Energy intake at breakfast and weight change: prospective study of 6,764 middle-aged men and women. Am J Epidemiol 2008;167:188-92. 10.1093/aje/kwm309 [DOI] [PubMed] [Google Scholar]
- 22. Casazza K, Fontaine KR, Astrup A, et al. Myths, presumptions, and facts about obesity. N Engl J Med 2013;368:446-54. 10.1056/NEJMsa1208051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chowdhury EA, Richardson JD, Holman GD, Tsintzas K, Thompson D, Betts JA. The causal role of breakfast in energy balance and health: a randomized controlled trial in obese adults. Am J Clin Nutr 2016;103:747-56. 10.3945/ajcn.115.122044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. LeCheminant GM, LeCheminant JD, Tucker LA, Bailey BW. A randomized controlled trial to study the effects of breakfast on energy intake, physical activity, and body fat in women who are nonhabitual breakfast eaters. Appetite 2017;112:44-51. 10.1016/j.appet.2016.12.041 [DOI] [PubMed] [Google Scholar]
- 25. Kvaavik E, Lien N, Tell GS, Klepp KI. Psychosocial predictors of eating habits among adults in their mid-30s: the Oslo Youth Study follow-up 1991-1999. Int J Behav Nutr Phys Act 2005;2:9. 10.1186/1479-5868-2-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264-9, W64. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 27. Kant AK, Graubard BI. 40-year trends in meal and snack eating behaviors of American adults. J Acad Nutr Diet 2015;115:50-63. 10.1016/j.jand.2014.06.354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. WorldBank Country classification - World Bank country and lending groups. Vol 2018 World Bank, 2018. [Google Scholar]
- 29. WebPlotDigitizer 2018 https://automeris.io/WebPlotDigitizer/
- 30. Higgins JP, Altman DG, Gøtzsche PC, et al. Cochrane Bias Methods Group. Cochrane Statistical Methods Group The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JPT, Green S, eds. Cochrane Handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). http://handbook-5-1.cochrane.org/
- 32. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 33. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 35.StataCorp. Stata statistical software. Release 14. 2015.
- 36.Wluka A, Cicuttini F, Renzaho A, et al. Understanding the needs of consumers with musculoskeletal conditions. Consumers’ perceived needs of health information, health services and other non-medical services: a systematic scoping review. 2016. https://researchmgt.monash.edu/ws/portalfiles/portal/239469465/238254946_oa.pdf
- 37. Ekram AR, Cicuttini FM, Teichtahl AJ, et al. Weight satisfaction, management strategies and health beliefs in knee osteoarthritis patients attending an outpatient clinic. Intern Med J 2016;46:435-42. 10.1111/imj.13007 [DOI] [PubMed] [Google Scholar]
- 38. Astbury NM, Taylor MA, Macdonald IA. Breakfast consumption affects appetite, energy intake, and the metabolic and endocrine responses to foods consumed later in the day in male habitual breakfast eaters. J Nutr 2011;141:1381-9. 10.3945/jn.110.128645 [DOI] [PubMed] [Google Scholar]
- 39. Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr 2014;100:539-47. 10.3945/ajcn.114.083402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Clayton DJ, Barutcu A, Machin C, Stensel DJ, James LJ. Effect of breakfast omission on energy intake and evening exercise performance. Med Sci Sports Exerc 2015;47:2645-52. 10.1249/MSS.0000000000000702 [DOI] [PubMed] [Google Scholar]
- 41. Dhurandhar EJ, Dawson J, Alcorn A, et al. The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr 2014;100:507-13. 10.3945/ajcn.114.089573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr 2005;81:388-96. 10.1093/ajcn.81.2.388 [DOI] [PubMed] [Google Scholar]
- 43. Geliebter A, Astbury NM, Aviram-Friedman R, Yahav E, Hashim S. Skipping breakfast leads to weight loss but also elevated cholesterol compared with consuming daily breakfasts of oat porridge or frosted cornflakes in overweight individuals: a randomised controlled trial. J Nutr Sci 2014;3:e56. 10.1017/jns.2014.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Levitsky DA, Pacanowski CR. Effect of skipping breakfast on subsequent energy intake. Physiol Behav 2013;119:9-16. 10.1016/j.physbeh.2013.05.006 [DOI] [PubMed] [Google Scholar]
- 45. Reeves S, Huber JW, Halsey LG, Horabady-Farahani Y, Ijadi M, Smith T. Experimental manipulation of breakfast in normal and overweight/obese participants is associated with changes to nutrient and energy intake consumption patterns. Physiol Behav 2014;133:130-5. 10.1016/j.physbeh.2014.05.015 [DOI] [PubMed] [Google Scholar]
- 46. Schlundt DG, Hill JO, Sbrocco T, Pope-Cordle J, Sharp T. The role of breakfast in the treatment of obesity: a randomized clinical trial. Am J Clin Nutr 1992;55:645-51. 10.1093/ajcn/55.3.645 [DOI] [PubMed] [Google Scholar]
- 47. Thomas EA, Higgins J, Bessesen DH, McNair B, Cornier MA. Usual breakfast eating habits affect response to breakfast skipping in overweight women. Obesity (Silver Spring) 2015;23:750-9. 10.1002/oby.21049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yoshimura E, Hatamoto Y, Yonekura S, Tanaka H. Skipping breakfast reduces energy intake and physical activity in healthy women who are habitual breakfast eaters: A randomized crossover trial. Physiol Behav 2017;174:89-94. 10.1016/j.physbeh.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 49. Dhurandhar EJ, Dawson J, Alcorn A, et al. The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr 2014;100:507-13. 10.3945/ajcn.114.089573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Christen WG, Gaziano JM, Hennekens CH. Design of Physicians’ Health Study II--a randomized trial of beta-carotene, vitamins E and C, and multivitamins, in prevention of cancer, cardiovascular disease, and eye disease, and review of results of completed trials. Ann Epidemiol 2000;10:125-34. 10.1016/S1047-2797(99)00042-3 [DOI] [PubMed] [Google Scholar]
- 51. Song WO, Chun OK, Obayashi S, Cho S, Chung CE. Is consumption of breakfast associated with body mass index in US adults? J Am Diet Assoc 2005;105:1373-82. 10.1016/j.jada.2005.06.002 [DOI] [PubMed] [Google Scholar]
- 52. van der Heijden AA, Hu FB, Rimm EB, van Dam RM. A prospective study of breakfast consumption and weight gain among U.S. men. Obesity (Silver Spring) 2007;15:2463-9. 10.1038/oby.2007.292 [DOI] [PubMed] [Google Scholar]
- 53. Vereecken C, Dupuy M, Rasmussen M, et al. HBSC Eating & Dieting Focus Group Breakfast consumption and its socio-demographic and lifestyle correlates in schoolchildren in 41 countries participating in the HBSC study. Int J Public Health 2009;54(Suppl 2):180-90. 10.1007/s00038-009-5409-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bo S, Fadda M, Castiglione A, et al. Is the timing of caloric intake associated with variation in diet-induced thermogenesis and in the metabolic pattern? A randomized cross-over study. Int J Obes (Lond) 2015;39:1689-95. 10.1038/ijo.2015.138 [DOI] [PubMed] [Google Scholar]
- 55.Nutrition Australia. Breakfast. 2014. www.nutritionaustralia.org/national/resource/breakfast
- 56. Corder K, van Sluijs EMF, Ridgway CL, et al. Breakfast consumption and physical activity in adolescents: daily associations and hourly patterns. Am J Clin Nutr 2014;99:361-8. 10.3945/ajcn.111.027607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012;70:3-21. 10.1111/j.1753-4887.2011.00456.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cooper LF. Good Health. Good Health Publishing Company, 1917:52;389. [Google Scholar]
- 59. Murphy JM, Pagano ME, Nachmani J, Sperling P, Kane S, Kleinman RE. The relationship of school breakfast to psychosocial and academic functioning: cross-sectional and longitudinal observations in an inner-city school sample. Arch Pediatr Adolesc Med 1998;152:899-907. 10.1001/archpedi.152.9.899 [DOI] [PubMed] [Google Scholar]
- 60. Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 2005;105:743-60, quiz 761-2. 10.1016/j.jada.2005.02.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary material
Infographic: Visual summary of trial and participant characteristics


