Abstract
Introduction
Vibration from a helicopter during aeromedical retrieval of divers may increase venous gas emboli (VGE) production, evolution or distribution, potentially worsening the patient’s condition.
Aim
To review the literature surrounding the helicopter transport of injured divers and establish if vibration contributes to increased VGE.
Method
A systematic literature search of key databases was conducted to identify articles investigating vibration and bubbles during helicopter retrieval of divers. Level of evidence was graded using the Oxford Centre for Evidence-Based Medicine guidelines. A modified quality assessment tool for studies with diverse designs (QATSDD) was used to assess the overall quality of evidence.
Results
Seven studies were included in the review. An in vitro research paper provided some evidence of bubble formation with gas supersaturation and vibration. Only one prospective intervention study was identified which examined the effect of vibration on VGE formation. Bubble duration was used to quantify VGE load with no difference found between the vibration and non-vibration time periods. This study was published in 1980 and technological advances since that time suggest cautious interpretation of the results. The remaining studies were retrospective chart reviews of helicopter retrieval of divers. Mode of transport, altitude exposure, oxygen and intravenous fluids use were examined.
Conclusion
There is some physical evidence that vibration leads to bubble formation although there is a paucity of research on the specific effects of helicopter vibration and VGE in divers. Technological advances have led to improved assessment of VGE in divers and will aid in further research.
Keywords: Transport, Scuba diving, Decompression sickness, Venous gas embolism (VGE), Vibration, Review article
Introduction
Although scuba diving is a relatively safe sport, 15 divers died in Australia in 2011[ 1] and 168 divers were treated for decompression illness (DCI), 33 of these in Queensland.[ 2] The possibility of a diver having DCI often necessitates retrieval for medical assessment and possible recompression. Retrieval options commonly include: water (dive boats, police, and coast guard), land (ambulance, private car, bus[ 3]) and air (rotary or fixed wing aircraft). Many factors are considered when deciding on the most appropriate retrieval platform: patient location and access, acuity, distance to definitive care, response time, speed, weather, time of day, altitude exposure, crew skill mix and platform availability.[ 4] Owing to dive site remoteness, helicopter aeromedical retrieval is often used for short-haul transport of divers. It has been suggested that the vibration associated with helicopter transport may cause increased bubble generation in divers potentially worsening DCI.[ 5 - 8]
DCI is a collective term encompassing the clinical consequences of two different pathophysiological processes: introduction of bubbles to the arterial circulation by pulmonary barotrauma (referred to as arterial gas embolism (AGE)); and formation of bubbles from inert gas (referred to as decompression sickness (DCS)). Both involve bubbles as presumed primary vectors of injury. There is potential difficulty in clinical distinction between them, and the modern trend in therapy is to treat both in the same manner.[ 9] These considerations provided the motivation for referring to them collectively as DCI with the nomenclature describing the clinical picture: acute/chronic, evolution, organ system involved, and degree of severity (e.g., acute, stable, mild neurological DCI).[ 10]
AGE occurs secondarily to pulmonary barotrauma, where expanding alveolar gas enters the systemic arterial circulation.[ 9] If these bubbles enter the cerebral circulation and cause central neurological symptoms it is called cerebral arterial gas embolism (CAGE). DCS, on the other hand, is presumably caused by the formation of bubbles in the extravascular space or within tissue capillaries primarily from dissolved inert gas. These capillary bubbles subsequently appear in the systemic veins as venous gas emboli (VGE). The in vivo formation of bubbles at levels of supersaturation that are vastly lower than predicted to be required for bubble formation in pure solutions suggests the existence of surfactant-stabilized gas micronuclei into which supersaturated gas diffuses to form larger bubbles.
The exact mechanism by which these bubbles cause the symptoms of DCS is not clear. Indeed, they do not always cause problems, but when in abundance are commonly held to be the inciting factors in DCS[ 9] with the probability of DCS correlated with the bubble load detected.[ 11] Bubble formation is generally accepted as an indicator of decompression stress and DCS risk in research where the generation of clinical DCS would be an unacceptable end point.[ 11]
Post-dive risk factors for increased bubble production and DCS include elevated temperature exposure, altitude exposure and exercise. Hot showers post-diving cause vasodilation and decreased inert gas solubility potentially leading to increased bubbles and possible DCS.[ 12] The decreased ambient pressure accompanying altitude exposure increases any tissue supersaturation which in turn will increase bubble formation. If bubbles were already present the decreased ambient pressure also promotes bubble growth.[ 13 , 14] VGE have been detected in some divers during a commercial flight 24 hours after completing their last dive, even though no pre-flight VGE were detected.[ 15] Exercise post-diving may cause small bubbles to grow and promote new bubbles by physical excitation of the tissues by the process of tribonucleation.[ 16] Tribonucleation is the process of bubble formation when solid surfaces immersed in a liquid are pulled apart.[ 17] It has been stated that vibration can lead to tribonucleation and, especially in supersaturated tissues, lead to increased gas bubble loads.[ 18 , 19] Pre-dive vibration at 35–40 Hz[ 20 , 21] and impact exercise[ 22] reduced bubble formation, presumably by dislodging pre-existing micronuclei from crevices or enhancing lymphatic elimination of gas nuclei.[ 20] Low frequency vibration[ 20] and movement[ 23] post-dive have been reported to increase VGE presumably by a similar mechanism of dislodging micronuclei that are growing as inert gas from the surrounding supersaturated tissue diffuses into them.
Low frequency vibration of this nature can be encountered during helicopter transport. It has been hypothesized that this may increase VGE generation, evolution or distribution in a diver, potentially worsening their condition.[ 5 - 8] We are not aware of any evidence that could guide the clinician regarding the related risks of helicopter retrieval of scuba divers. Therefore, the purpose of this report is to systematically review the literature surrounding helicopter transport of injured divers to find any evidence that vibration contributes to increased VGE formation and worsening DCS.
Methods
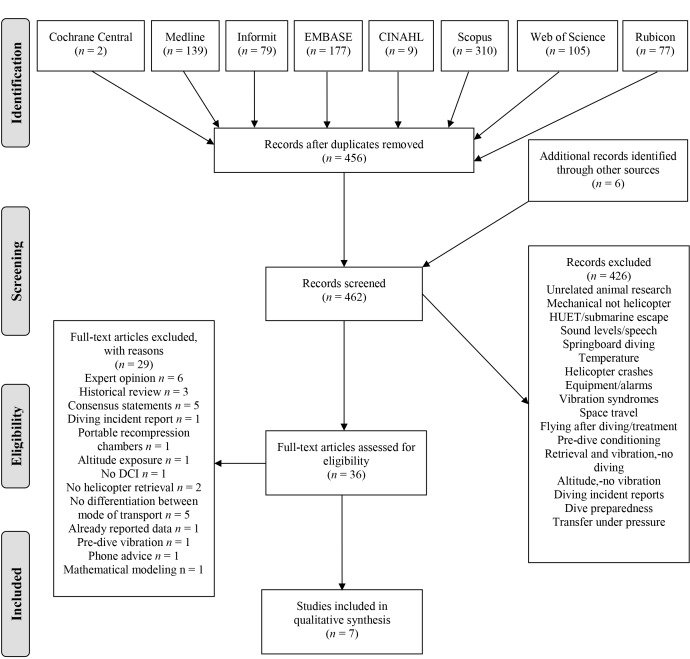
A systematic search of the literature was conducted to identify articles investigating vibration and bubble generation during helicopter retrieval of divers. Databases searched included MEDLINE, CINAHL, Informit, EMBASE, Scopus, Web of Science, Rubicon Foundation and Cochrane Central, with no date limits (i.e., from database inception to April 2018). Medical subject headings (MeSH) and key words used as search terms included: diving* OR scuba OR "self contained underwater breathing apparatus"; bends OR "caisson disease" OR "decompression sickness"; helicopter* OR "air ambulance" OR "emergency helicopter" OR "helicopter ambulance"; vibration AND "transportation of patients". Results of the search were exported to a reference managing database (EndNote X7). Preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines were followed Figure 1.[ 24] All authors participated in the development of the inclusion and exclusion criteria.
Figure 1.
PRISMA flow diagram
Titles and abstracts were screened and the full texts of potentially relevant articles were obtained for review. Inclusion criteria were helicopter retrieval, scuba divers, bubble production, and DCS. Owing to the limited number of articles on vibration and bubble formation, inclusion criteria were broadened to include articles that only presented data on helicopter retrieval of divers. Exclusion criteria for each stage of the review are listed in Figure 1. Exclusion in the initial screening (DFB) included articles pertaining to animals that dive, mechanical vibrations of platforms and equipment, helicopter underwater escape training, and syndromes from using equipment that vibrates such as a jack hammer. Full text review exclusions included articles with no data and only expert opinion, consensus statements, historical review of retrieval services and listing of patient presentations with no differentiation between modes of arrival.
Reference lists of identified publications were reviewed for additional relevant articles. All non-English language (Danish, French, German, Italian and Japanese) abstracts and relevant articles were translated. Two authors (DFB, MC) reviewed the literature; the content experts (SJM, PA, NWP) also being tasked to identify any further missing literature (none were found). The manuscript and tables were critically reviewed by all authors.
Included articles were evaluated and their initial level of evidence (LOE) was determined based on the reported research methodology utilized by the Oxford Centre for Evidence-Based Medicine.[ 25] A levels-of-evidence table guided the initial grading when assessing each study’s research question and methodology. The next step was to adjust the initial grade based on study quality, imprecision, indirectness, inconsistencies and effect size.[ 26] The grading of recommendations, assessment, development and evaluation (GRADE) approach was then used to upgrade or downgrade the initial LOE as appropriate.[ 26] The overall quality of evidence was assessed using the quality assessment tool for studies with diverse designs (QATSDD).[ 27] This tool allows for the comparison of studies with differing methodological research designs. Papers are graded on a scale of 0 to 3 for each criterion. The score is then summed and expressed as a percentage of the maximum possible score. Each individual paper is given a quality score and the percentage then allows for comparison across the differing methodologies within the same field of research.[ 27] An interpretation of the scores can then allow for classification into low (< 50%), medium (50–80%) or high (> 80%) quality evidence. The QATSDD tool was modified by excluding one criterion, "evidence of user involvement in design", as it did not appear relevant to the included studies. Two authors (DFB and MC) replicated and agreed on the grading.
Results
The combined searches initially identified 898 records with 456 records remaining after duplicates were removed (Figure 1). After initial screening, 36 full text articles were assessed for eligibility. Limited scientific literature was available on this topic, and only seven articles met the broadened inclusion criteria. Table 1 contains a summary of the seven relevant articles. Study characteristics including participants, study design, methods, results, author conclusions and study limitations are presented. The overall quality of clinical evidence was low with only one clinical article reaching a 50% score on the modified QATSDD assessment (Table 2). An in vitro research paper provided some evidence of bubble formation with gas saturation and vibration. Only one prospective intervention study was identified which examined the effect of vibration on VGE formation. The remaining studies were retrospective chart reviews of helicopter retrieval of divers. The articles have been categorised into three groups for comparison: bubbles and vibration, retrieval method comparison and helicopter retrieval only.
Table 1. Characteristics of studies included in systematic review; a LOE – level of evidence: Level 1 high (systematic review), Level 2 (randomized trial), Level 3 (cohort study), Level 4 (case-series), Level 5 low (Mechanism-based reasoning)25; b Type 2 DCS is considered more serious and includes central nervous system (CNS), inner ear and cardiorespiratory symptoms; AGE − arterial gas embolism; CAGE − cerebral arterial gas embolism; CNS − central nervous system; DCI − decompression illness; DCS − decompression sickness; Hz − hertz; HBO − hyperbaric oxygen; kPa − kilopascal; IV − intravenous; SANDHOG − San Diego Diving and Hyperbaric Organizations; VGE − venous gas emboli; W − watt .
| Study | LOE | Participants | Study design | Methods | Results |
| Bubbles and vibration | |||||
| Ikels[17] | 5 | Liquids of various viscosities | in vitro | Liquids of varying viscosity saturated with various gases (including nitrogen) at ambient pressure; bubble production observed during hypobaria and from steel ball rolled down a tube | High steel ball velocity facilitated bubble formation. Extreme hypobaria for bubbles to form in human blood. Hypobaria for bubble formation increased as Pgas↓. Hypobaria for bubble formation decreased as viscosity increased |
| Balldin[6] | 3 | 10 healthy male scuba divers 28 ± 7 years (y) (range 18 to 38 y) | Block randomized (1–5 vibrate/rest; 6–10 rest/vibrate) | 1. 250 kPa, 100 minutes (min), hyperbaric chamber; cycling (75 W), 2 min work/2 min rest; 2. 70 kPa, 120 min + vibration 15 Hz, 15 min on/off, seated "some further participants" vibrated @ 25 Hz Precordial Doppler | No significant difference in VGE detection |
| Retrieval method comparison | |||||
| Bennett[7] | 4 | 107–109 patients with DCI (clinical diagnosis) 78% male, average age 29 y | Retrospective consecutive case series | 2-year review; retrieval method; time of symptoms to treatment; 6-week follow up; 131 reviewed, 16 excluded – insufficient data or failure to follow up = 115 | Helicopter for intermediate distance, difficult access, worse injured, shorter time to treatment, no worse outcome |
| Bennett[4] | 4 | 133 patients with DCI (clinical diagnosis) No sex/age data | Retrospective consecutive case series | 2-year review; retrieval method; time of symptoms to treatment; 6-week follow up; 131 reviewed, 16 excluded – insufficient data or failure to follow up = 115 | Helicopter for intermediate distance, difficult access, worse injured, shorter time to treatment, no worse outcome |
| Helicopter retrieval of divers | |||||
| Cristina[8] | 4 | 25 male divers 24 DCS type 2b age 31 ± 8 y 1 AGE, age 35 y | Retrospective case series | 7 years of helicopter retrievals by the Italian military | 2.8% of missions for divers. 24 DCS type 2b, 1 AGE All treated with oxygen and IV fluids. No deterioration enroute, all flights < 300 metres, transport time 53 ± 9 min |
| Oode[30] | 4 | 28 patients with DCI (SANDHOG criteria[31]) 71% male, 45 ± 2 y | Retrospective consecutive case series | 4 years of transportation in physician-staffed helicopters 34 identified; 6 excluded due to cardiopulmonary arrest at scene | 0 deterioration, 20 no change, 8 improved during flight. All received oxygen; all but 1 received IV fluids; all flights < 300 metres |
| Reddick[13] | 5 | 6 males; average age 28 y | Retrospective case series | Cases of DCS over 18 months in altitude chamber participants | 5 pain and cutaneous DCS, 1 peripheral paraesthesia developed into CNS DCS; all transported by helicopter and received oxygen; 3 worsened in flight, all improved with lower altitude |
| Study | Conclusions | Limitations | |||
| Bubbles and vibration | |||||
| Ikels[17] | Tribonucleation may lead to bubble formation where surfaces rub across one another such as joints, small blood vessels expanding/contracting or muscle tendon insertion sites. | Blood is a complex liquid and was only used in initial decompression studies with no saturation or vibration. | |||
| Balldin[6] | Differences were inter-individual. Helicopter vibrations complex. No effect on release of VGE with vibration frequencies used. | Lack of allocation concealment and blinding; Wet (immersed) vs dry hyperbaric exposure not outlined; Timing of Doppler unable to be determined; No grading of Doppler signal, only length of time VGE heard; No blinded independent review of Doppler signals; Only used 15 and 25 Hz sitting in vibrating chair; Altitude as confounder, may obscure any increase with vibration. | |||
| Retrieval method comparison | |||||
| Bennett[7] | Early transfer of severe injury may outweigh or disguise risk of helicopter transport. | 8 patients with DCS via helicopter, 12 CAGE; Scoring by chart review; Number of HBO treatments not included, nor entry or discharge classification; Classification system not validated; Inconsistent data. | |||
| Bennett[4] | Retrieval of divers is complicated, consider physiology and retrieval system. No good outcome evidence to guide strategies. | Most of helicopter group CAGE, so not included in detailed analysis of time to treatment, altitude and recovery grade. Grading scale developed in previous study not used. No information on pre-treatment severity, pre-hospital treatment or number of HBO treatments; No follow-up. | |||
| Helicopter retrieval of divers | |||||
| Cristina[8] | Considerations for retrieval air speed and vibrations. | No number of HBO treatments or outcome at end of treatment; No retrieval method comparison group; No follow-up. | |||
| Oode[27] | Subjective improvement via helicopter if altitude < 300 metres + administration of O2 and fluids. | Unsure if any patients had CAGE; No details on patients requiring intubation (n = 4); Oxygen saturation improvement clinically insignificant; No analysis between groups with change in symptoms; No data on HBO treatment or follow up; No retrieval method comparison group. | |||
| Reddick[15] | No worsening of symptoms if helicopter stayed below 61 metres above ground level of the take-off point. Retrieval twice as fast air vs land. | Altitude exposure pre-DCS; Not divers; No retrieval method comparison group. | |||
Table 2. Quality of clinical evidence for systematic review of vibration and bubbles in divers; * QATSDD – quality assessment tool for studies with diverse designs; 0 = not at all; 1 = very slightly; 2 = moderately; 3 = complete; n/a − not applicable (in vitro study) .
| QATSDD* Criteria | Study | ||||||
| Ikels[17] | Balldin[6] | Bennett[7] | Bennett[4] | Cristina[8] | Oode[30] | Reddick[13] | |
| Explicit theoretical framework | 3 | 1 | 2 | 2 | 1 | 1 | 0 |
| Statement of aims/objectives in main body of report | 2 | 3 | 3 | 1 | 2 | 2 | 0 |
| Clear description of research setting | 3 | 2 | 3 | 1 | 3 | 3 | 1 |
| Evidence of sample size in terms of analysis | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Representative sample of target group of reasonable size | n/a | 1 | 2 | 1 | 3 | 1 | 1 |
| Description of procedure for data collection | 3 | 1 | 2 | 1 | 1 | 2 | 0 |
| Rationale for choice of data collection tool(s) | 3 | 0 | 2 | 0 | 0 | 0 | 0 |
| Detailed recruitment data | n/a | 0 | 2 | 1 | 2 | 2 | 1 |
| Statistical assessment of reliability and validity of measurement tool(s) (Quantitative only) | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fit between stated research question and method of data collection (Quantitative only) | 3 | 1 | 2 | 2 | 1 | 2 | 0 |
| Fit between research question and method of analysis (Quantitative only) | 3 | 0 | 1 | 1 | 0 | 2 | 0 |
| Good justification for analytical method selected | 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| Evidence of user involvement in design | Item not included in scoring as not relevant to included studies | ||||||
| Strengths and limitations critically discussed | 1 | 1 | 1 | 1 | 0 | 1 | 0 |
| Total score | 26/33 | 10/39 | 20/39 | 11/39 | 13/39 | 16/39 | 3/39 |
| % of maximum possible score | 79 | 26 | 51 | 28 | 33 | 41 | 8 |
BUBBLES AND VIBRATION
Preliminary in vitro research into tribonucleation was completed on human blood suggesting that significantly decreased pressure was required for bubbles to form.[ 17] Further studies were then completed using liquids of varying viscosities saturated with different gases. The liquids were examined for bubble generation under decreasing pressure and varying velocities of a steel ball rolling down the side of a test tube which acted as a vibration stimulus. High steel ball velocity increased bubble formation. The amount of decompression required for bubble formation was inversely proportional to the gas supersaturation, i.e., as the gas supersaturation decreased the amount of pressure reduction required for bubble formation increased.
This article was assessed as a medium quality of evidence with a modified QATSDD score of 79% (Table 2) and a LOE grade 5. Even though this was in vitro research, the study provides important insight into the physics of bubble generation. The addition of a mechanical stimulus to the combination of gas saturation and pressure reduction increased bubble production. Only preliminary work was completed on human blood with the more extensive research conducted on liquids of varying viscosities.
Only one prospective intervention study assessing VGE generation in divers exposed to vibration was found.[ 6] Healthy, young, male scuba divers were enrolled and exposed to 250 kPa for 100 min in a hyperbaric chamber with cycling for 2 min/2 min rest. Within five min of surfacing the divers were taken to 70 kPa (hypobaric) for two hours. During the hypobaric exposure the divers were vibrated for 15-min periods at 15 hertz (Hz) in a seated chair alternated with a 15-min period of non-vibration for a total of 120 min. VGE were detected using precordial Doppler with duration of bubble signal recorded in seconds (sec). All participants were then treated with oxygen (O2) at 220 kPa for 30 min. Results were reported as duration of bubbles in sec with no significant differences found between the vibrated and non-vibrated conditions.
This article was assessed as having a low quality of evidence with a modified QATSDD score of 26% (Table 2) and a LOE grade 3. This was a block randomized, quasi-crossover study with no allocation concealment or blinding of participants or adjudicators. Dry versus wet (immersed) hyperbaric exposure was not outlined. Participants sat in a vibration chair and were therefore not supine. Sitting would be an unusual position for a patient during helicopter retrieval and not the recommended position for optimal inert gas washout.[ 28] Helicopter vibration frequencies occur in a wide range of frequencies from 5 to 150 Hz.[ 29] Only 15 (peak 0.23 ĝz) and 25 (peak 0.64 ĝz) Hz exposures were performed. The peak accelerations used were much lower than peak helicopter accelerations quoted in the literature.[ 29] The exact timing of the Doppler scans was unclear with no grading scale used. There was no reporting of training of the Doppler technician, how the recordings were saved or whether there was independent blinded review of the recordings. Since this study, technological advances and reporting guidelines have substantially changed,[ 23] so the results require cautious interpretation. The main limitation is the use of altitude exposure to generate VGE. The altitude exposure, known to produce a great amount of bubbles, may have acted as a confounder and masked any difference in VGE generation between the vibration and non-vibration conditions.
RETRIEVAL METHOD COMPARISON
Two retrospective case series compared outcomes of injured divers treated at a hyperbaric facility stratified by retrieval mode. Retrieval modes included fixed and rotary wing aircraft, road ambulance or self-referral. Both studies were written by the same author and based in Sydney, Australia. Most helicopter retrievals were for divers with CAGE and not DCS.
The medical records of 131 consecutive divers who presented to The Prince Henry Hospital, Sydney, Australia for treatment of DCI over a two-year period were retrospectively reviewed.[ 7] Cases were classified by retrieval method, time of symptom onset to recompression and a six-week follow-up score designed for the study. Most of the patients were self-referrals. More than half (60%) of the helicopter retrieval group were diagnosed with CAGE, with two deaths in the CAGE group. The discharge scores for the DCS patients were similar for each retrieval mode. Patients retrieved via helicopter had a significantly shorter time to first recompression (4.9 hours (h) vs > 20 h road and fixed wing).
This was a pilot study[ 7] and was assessed as medium quality of evidence with a modified QATSDD score of 51% (Table 2) and a LOE grade 4. Only a very small number of the patients with DCS were transported by helicopter (7%). The discharge classification scoring system was designed for this study, not previously validated and completed by reviewing the medical records. The patients were followed up at six weeks. The author’s conclusion was that the speed of retrieval in the helicopter group and the presumed benefit of earlier recompression may possibly mask any increased risk from rotary wing retrieval.
A further retrospective study performed by the same author reviewed 133 cases treated in the same hyperbaric medicine unit.[ 4] Cases were analysed by transport platform, time to recompression, altitude stress and status at discharge. Helicopter retrievals (23 patients) were, again, predominantly for divers with CAGE and had markedly shorter average times to recompression (5 h vs > 20 h for road and fixed wing) and, therefore, were not included in further analysis. Altitude exposure was similar in the self-referral (200 metres, m), road (200 m) and rotary wing groups (150 m). Two cases were discussed in more detail to highlight the complexity of retrieval decisions.
This article[ 4] outlined retrieval options and considerations and was given a low quality of evidence modified QATSDD score of 28% (Table 2) and a LOE grade 4. Most patients retrieved by helicopter were diagnosed with CAGE so the author decided to omit them from the more in-depth analysis of time to recompression and symptom resolution. Even though the helicopter-retrieved patients were omitted from further analysis, their outcomes appear to be similar to the other retrieval modes. The grading scale developed in the previous study[ 7] was not used and discharge outcome was only classified as full or incomplete resolution with no follow up performed. Within the other retrieval modes there was no information on number of DCS versus CAGE cases in the cohort.
HELICOPTER RETRIEVAL OF DIVERS
This third group of articles were all retrospective chart reviews of DCI cases transported by helicopter. Their focus was on change in clinical condition during helicopter flight. The cases in one article were altitude chamber participants not scuba divers. This article was still included in the review as it was frequently referenced in other articles. All three articles were graded as low quality of evidence (Table 2).
Charts were retrospectively reviewed for a seven-year period of helicopter retrieval flights by the Italian Military search and rescue organization.[ 8] The authors extracted cases associated with diving injuries. Twenty-five cases were identified (2.8% of total missions) as involving divers, comprising 24 DCS and 1 CAGE. All divers were treated with 100% O2 and intravenous (IV) fluids en route. All flights were at altitudes of less than 300 m. Transport time was 53 ± 9 min (measure of variance not reported). There was no deterioration reported during any of the flights.
This article[ 8] was of a low quality of evidence based on the modified QATSDD score of 33% (Table 2) and a LOE score of 4. The retrieval service provided exceptional service with rapid transit times, low altitude flights, O2 and IV fluids for all patients. There were no data presented on pre-flight O2 or time from symptom onset to retrieval. No information was presented on injury severity or hyperbaric treatment. There was no comparison with other retrieval methods and no follow up.
The charts of 28 consecutive DCI patients retrieved via helicopter over a four-year period from Izu Peninsula, Japan were retrospectively reviewed.[ 30] Six divers who had cardiopulmonary arrest at the scene were excluded. Diagnosis of DCI was made using the San Diego diving and hyperbaric organizations (SANDHOG) criteria.[ 31] Patient demographics and dive characteristics were collected. Patients were classified by type of DCS: central nervous system (CNS), 'chokes', 'chokes'/'bends' and 'chokes'/CNS. All patients received O2 with delivery device and flow reported. All participants were transported in the supine position and all but one subject received IV fluids. All flights were below an altitude of 300 metres above sea level. Changes in vital signs, Glasgow coma scale (GCS) and change of subjective symptoms before and after the flights were compared. A statistically significant improvement in O2 saturation pre- and post-flight was found. Four patients required intubation but the timing of this intervention is unclear. No patient deteriorated en route, 20 did not change status and eight improved. Time from request for transfer and arrival at the medical facility was recorded.
This article examined the outcomes of patients diagnosed with DCI in a physician-staffed helicopter retrieval service.[ 30] The quality of evidence was low based on the modified QATSDD score of 41% (Table 2) and a LOE grade 4. Inconsistent use of the terms DCS and DCI make it difficult to determine if patients who surfaced suddenly were CAGE or CNS DCS. Duration of O2 therapy was stated to be similar in all patients with reference to a table that does not contain that data. The significant improvement stated for O2 saturation was clinically insignificant. There is no detail about the timing or indication for intubation in four patients. No follow up data on hospital treatment or outcome were reported. There was no comparison with other methods of retrieval. No analysis of the differences between the patients in relation to change in subjective symptoms was performed.
Six cases of altitude chamber participants with DCS occurring over an 18-month period were retrospectively reviewed.[ 13] A synopsis of each case was presented. All patients were retrieved by helicopter and received 100% O2 from diagnosis to delivery to the hyperbaric facility. Three of the patients had worsening of their symptoms during flight which all resolved on flying at lower altitudes. The article was given a very low level of evidence score based on the modified QATSDD score of 8% (Table 2) and a LOE grade 4. The author stated that aeromedical retrieval was twice as fast as ground transportation however no actual retrieval times by other modes were compared.
Discussion
It has been suggested that the vibration generated during helicopter retrieval of injured divers may lead to worsening of DCS due to an increase in inert gas bubbles.[ 5 - 8 , 18] Knowledge in this area is necessary to assist the clinician in deciding the possible risk of retrieving an ill or injured diver by a rotary wing platform. This systematic review confirms that there is no published research to help guide the retrieval decision-making process.
Physical evidence shows that vibration leads to bubble formation although there is limited published research on the specific effects of helicopter vibration and VGE in divers. Early in vitro research demonstrated that movement of an object in a nitrogen-saturated liquid could lead to bubble production.[ 17] The addition of a mechanical stimulus increased bubble formation more than increased gas saturation and pressure reduction alone. It is plausible that this process of tribonucleation could lead to VGE production in divers exposed to vibration.
An early study exposing healthy divers to vibration found no increase in VGE.[ 6] However we now understand that helicopter vibrations are much more complex than those simulated in this study with a wider range of frequencies and amplitudes.[ 29] The range of vibration frequency generated by a helicopter is 5 to 150 Hz,[ 29] while the two frequencies (15 and 25 Hz) used in this study were too close together to be classified as separate measurements. The peak accelerations used were significantly less than those experienced in a helicopter. The frequencies and amplitudes used in this study do not reflect actual measured helicopter vibrations and may not have been a strong enough stimulus for VGE generation.[ 29]
Divers are exposed to both altitude and vibration during helicopter retrieval. One of the included articles found that exposure to altitude during the helicopter retrieval of patients with DCS led to worsening symptoms.[ 13] Improvement in symptoms was seen in divers treated with O2, IV fluids and restricting the flying altitude to below 300 metres.[ 8 , 30] Positioning divers in areas with less vibration during aeromedical retrieval has been suggested with an acknowledgement of little evidence on which to base this recommendation.[ 18] The previous South Pacific Underwater Medicine Society (SPUMS) policy for initial management of injured or ill divers recommended O2 administration, IV fluids and to fly as low as possible with 300 metres considered the maximum.[ 32] However, the most recent consensus guidelines for the pre-hospital management of decompression illness suggests that flying at less than 150 metres above pick-up location is preferred, though no reference for this recommendation is given.[ 33]
Both AGE and DCS are caused by bubble generation although their mechanisms are significantly different and this limits the generalization of the CAGE outcomes to divers with DCS. The two retrospective articles comparing retrieval methods stated that most of the injured divers retrieved by helicopter were diagnosed with CAGE.[ 4 , 7] Another article used confusing nomenclature making it difficult to determine if the included patients had CAGE or DCS.[ 30] Patients with CAGE tend to be sicker and with symptom onset earlier than patients with DCS. Request for helicopter transport in these divers may be due to clinical urgency. Speed of retrieval may mask any increased risk from the rotary wing retrieval.[ 7] CAGE can occur in circumstances of lower inert gas load than serious DCS, meaning that patients may be at less risk of vibration-induced bubble formation if transported by helicopter.
FUTURE RESEARCH
Though the evidence is limited, these articles provide a framework for further research into this area. Technological advances have occurred allowing for better assessment of bubbles in divers.[ 23] Helicopter vibrations are complex,[ 29] but measurements of helicopter vibrations during a flight have been acquired.[ 29] This will lead to the ability to replicate and expose a diver to the position and vibrations encountered during actual aeromedical retrieval. Administration of O2 pre-vibration should be considered.[ 8 , 30 , 34] Altitude exposure should be eliminated so that the effect of vibration on bubble production can be isolated. Research into this area can lead to a better understanding of the effects of vibrations on divers and provide evidence to guide clinical decisions surrounding the risk/benefit of helicopter retrieval of injured divers.
LIMITATIONS
There is very little specific literature on bubble generation induced by vibration, and none during helicopter retrieval of divers. Studies identified were of diverse designs so the modified QATSDD tool was used to better compare the levels of evidence. The quality of evidence was low with most articles being retrospective reviews. Older investigative techniques were poorly described and therefore it was difficult to interpret the results.[ 6] Articles were of varying languages but translation allowed for their inclusion. There may be an element of selection bias as only articles found were reviewed. However, the Rubicon Foundation research repository was searched and provided access to some military research documents and many conference proceedings.
VGE are relatively easy to detect using ultrasonic methods by trained technicians and are often used as an outcome measurement in diving research.[ 35] Even though VGE may be responsible for some symptoms of DCS, they commonly occur after dives without DCS.[ 36] Nevertheless, higher VGE grades correlate with an increased risk of DCS.[ 37] Ultrasound techniques are only able to assess intravascular bubbles and therefore provide an incomplete picture of conditions in the whole body. Studies using VGE as a surrogate marker for DCS risk need to use paired comparisons and be well powered.[ 35]
CONCLUSIONS
There is some physical evidence that vibration leads to bubble formation although there is a paucity of research on the specific effects of helicopter vibration and VGE in divers. Technological advances have led to improved assessment of bubbles in divers and will aid in further research.
Footnotes
Acknowledgements
The authors thank the following people for their translation of non-English abstracts and articles: Gemma O'Kane (Japanese), Uli Orda (German), Ole Hyldegaard (Danish) and Costantino Balestra, Susanna Primavesi and Maëlle Barton (Italian). Special thanks to Dr Peter Grabau for his ongoing support into helicopter vibration measurement, simulator development and expertise in critically reviewing this manuscript. Professor Peter Leggat provided review of the final manuscript.
Funding
The Townsville Hospital and Health Service SERTA grant 2013_32.
Conflicts of interest:
Professors Simon Mitchell and Neal Pollock are members of the Editorial Board of Diving and Hyperbaric Medicine, but had no input into the peer review or decision-to-publish processes.
Contributor Information
Denise F Blake, Emergency Department, The Townsville Hospital, Townsville, Queensland, Australia; Marine Biology and Aquaculture, James Cook University, Townsville.
Melissa Crowe, Discipline of Sport and Exercise Science, James Cook University, Townsville.
Simon J Mitchell, Department of Anaesthesiology, University of Auckland, Auckland, New Zealand.
Peter Aitken, College of Public Health, Medical and Veterinary Sciences, James Cook University, Townsville; Health Disaster Management Unit, Queensland Health, Brisbane, Queensland.
Neal W Pollock, Department of Kinesiology, Faculty of Medicine, Université Laval, Québec, Canada; Service de médecine hyperbare, Centre de médecine de plongée du Québec, Levis, Québe.
References
- Lippmann J, Lawrence CL, Fock A, Jamieson S, Harris R, et al. Provisional report on diving-related fatalities in Australian waters in 2011 . Diving Hyperb Med. 2016;46:207. [PubMed] [Google Scholar]
- Hyperbaric Technicians and Nurses Association . Christchurch, New Zealand: 2012. Aug-25. Australian and New Zealand hyperbaric treatment data, 1 July 2011 – 30 June 2012. Proceedings of the 20th Annual Scientific Meeting on Diving and Hyperbaric Medicine . [Google Scholar]
- Griffiths D, Webb R, Shao H. Durham, NC: Divers Alert Network; 2005. [cited 2018 November 17]. Ground transportation of diving injuries in Townsville ; pp. 100–10. In: Mitchell SJ, Doolette DJ, Wachholz CJ, Vann RD, editors. Management of mild or marginal decompression illness in remote locations workshop proceedings . Available from: https://www.diversalertnetwork.org/files/RemoteWrkshpFinal05.pdf. [Google Scholar]
- Bennett M. Evacuation methods in diving injuries . SPUMS Journal. 1998;28:10–4. [Google Scholar]
- Acott C. Transportation of patients suffering from decompression sickness . SPUMS Journal. 1984;14:34–6. [Google Scholar]
- Balldin UI, Sporrong A. Vibration and decompression gas bubbles . Adv Physiol Sci. 1980;23(Suppl 6):S147–8. [PubMed] [Google Scholar]
- Bennett M. The retrieval of diving injuries in New South Wales: a retrospective review of two years practice.Evacuation methods in diving injuries . SPUMS Journal. 1995;25:142–7. [Google Scholar]
- Cristina G, Zarba Meli E, Di Padova M, Giacovazzo F, Aglietti A, Scorretti M. [Indications for the use of air transport in cases of dysbarism] . Gazz Med Ital Arch Sci Med. 1996;155:63–9. (Ita). [Google Scholar]
- Vann RD, Butler FK, Mitchell SJ, Moon RE. Decompression illness . Lancet. 2011;377(9760):153–164. doi: 10.1016/S0140-6736(10)61085-9. [DOI] [PubMed] [Google Scholar]
- Francis TJR. Annex A. Bethesda, MD: Undersea and Hyperbaric Medical Society; 1991. [cited 2018 November 17]. The classification of dysbarism . In: Francis TJR, Smith DJ, editors. Describing decompression illness: Proceedings of the 42nd workshop of the Undersea and Hyperbaric Medical Society . Available from: http://archive.rubicon-foundation.org/4499. [Google Scholar]
- Pollock NW. Use of ultrasound in decompression research . Diving Hyperb Med. 2007;37:68–72. [Google Scholar]
- Mekjavić IB, Kakitsuba N. Effect of peripheral temperature on the formation of venous gas bubbles . Undersea Biomed Res. 1989;16(5):391–401. [PubMed] [Google Scholar]
- Reddick EJ. Movement by helicopter of patients with decompression sickness . Aviat Space Environ Med. 1978;49:1229–1230. [PubMed] [Google Scholar]
- Lambertsen CJ. Bethesda, MD: Undersea and Hyperbaric Medical Society Inc; 1989. Feb 24, 1989. [cited 2018 November 17]. The pressure continuum: need for rational correlation and differentiation of the flying and diving environments ; pp. 1–9. In: Sheffield PJ, editor. Flying after diving. Proceedings of the 39th Undersea and Hyperbaric Medical Society Workshop . Available from: http://archive.rubicon-foundation.org/4256. [Google Scholar]
- Cialoni D, Pieri M, Balestra C, Marroni A. Flying after diving: should recommendations be reviewed? In-flight echocardiographic study in bubble-prone and bubble-resistant divers . Diving Hyperb Med. 2015;45:10–5. [PubMed] [Google Scholar]
- Pollock NW, Buteau D. Updates in decompression illness . Emerg Med Clin North Am. 2017;35:301–19. doi: 10.1016/j.emc.2016.12.002. [DOI] [PubMed] [Google Scholar]
- Ikels K. Production of gas bubbles in fluids by tribonucleation . [cited 2018 August];J Appl Physiol. 1970 28(4):524–527. Available from: http://tecvault.t101.ro/tribonucleation.pdf. [Google Scholar]
- Stephenson JC. Pathophysiology, treatment and aeromedical retrieval of SCUBA related DCI . J Mil Veterans Health. 2009;17(3):10–9. [Google Scholar]
- Evans C, Creaton A, Kennedy M, editors. Oxford, UK: Oxford University Press; 216. Retrieval medicine: diving and barotrauma ; pp. 430–2. [Google Scholar]
- Germonpré P, Pontier JM, Gempp E, Blatteau JE, Deneweth S, Lafère P, Marroni A, Balestra C. Pre-dive vibration effect on bubble formation after a 30-m dive requiring a decompression stop . Aviat Space Environ Med. 2009;80:1044–8. doi: 10.3357/asem.2588.2010. [DOI] [PubMed] [Google Scholar]
- Balestra C, Theunissen S, Papadopoulu V, Le Mener C, Germonpré MT, Guerrero F, Lafère P. Pre-dive whole-body vibration better reduces decompression-induced vascular gas emboli than oxygenation or a combination of both . Front Physiol. 2016;7:586. doi: 10.3389/fphys.2016.00586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurd KM, Thacker JC, Seddon FM, Gennser M, Loveman GA. The effect of pre-dive exercise timing, intensity and mode on post-decompression venous gas emboli . Diving Hyperb Med. 2011;41:183–8. [PubMed] [Google Scholar]
- Møllerløkken A, Blogg SL, Doolette DJ, Nishi RY, Pollock NW. Consensus guidelines for the use of ultrasound for diving research . Diving Hyperb Med. 2016;46:26–32. [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement . Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, et al. The Oxford 2011 levels of evidence. Oxford Centre for Evidence-Based Medicine . [cited 2018 October]; Available from: http://www.cebm.net/index.aspx?o=5653. [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz O, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations . BMJ. 2008;336:924–6. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool . J Eval Clin Pract. 2012;18:746–52. doi: 10.1111/j.1365-2753.2011.01662.x. [DOI] [PubMed] [Google Scholar]
- Balldin U. Effects of ambient temperature and body position on tissue nitrogen elimination in man . Aerosp Med. 1973;44:365–70. [PubMed] [Google Scholar]
- Grabau P. Townsville: James Cook University; 2016. [cited 2018 August]. The simulation of vibrations experienced by patients during helicopter winching and retrieval. PhD [dissertation] . Available from: http://www.researchonline.jcu.edu.au/44642/1/44642-grabau-2016-thesis.pdf. [Google Scholar]
- Oode Y, Yanagawa Y, Omori K, Osaka H, Ishikawa K, Tanaka H. Analysis of patients with decompression illness transported via physician-staffed emergency helicopters . J Emerg Trauma Shock. 2015;8:26–9. doi: 10.4103/0974-2700.145396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover I, Reed W, Neuman T. The SANDHOG criteria and its validation for the diagnosis of DCS arising from bounce diving . Undersea Hyperb Med. 2007;34:199–210. [PubMed] [Google Scholar]
- Gorman D, Richardson D, Davis M, Moon R, Francis J. The SPUMS policy on the initial management of diving injuries and illnesses . SPUMS Journal. 1997;27:193–6. [Google Scholar]
- Mitchell SJ, Bennett MH, Bryson P, Butler F, Doolette DJ, Holm JR, Kot J, Lafère F. Pre-hospital management of decompression illness: expert review of key principles and controversies . Diving Hyperb Med. 2018;48:45–55. doi: 10.28920/dhm48.1.45-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SJ, Doolette DJ, Wacholz CJ, Vann RD. Management of mild or marginal decompression illness in remote locations workshop proceedings . Diving Hyperb Med. 2006;36:152–5. [Google Scholar]
- Doolette DJ, Gault KA, Gutvik CR. Sample size requirement for comparison of decompression outcomes using ultrasonically detected venous gas emboli (VGE): power calculations using Monte Carlo resampling from real data . Diving Hyperb Med. 2014;44:14–9. [PubMed] [Google Scholar]
- Dunford RG, Vann RD, Gerth WA, Pieper CF, Huggins K, Wacholtz C, Bennett PB. The incidence of venous gas emboli in recreational diving . Undersea Hyperb Med. 2002;29:247–59. [PubMed] [Google Scholar]
- Eftedal OS, Lydersen S, Brubakk AO. The relationship between venous gas bubbles and adverse effects of decompression after air dives . Undersea Hyperb Med. 2007;34:99–105. [PubMed] [Google Scholar]