Abstract
Many evidence-based interventions (EBIs) have been developed to prevent or treat major health conditions. However, many EBIs have exhibited limited adoption, reach, and sustainability when implemented in diverse community settings. This limitation is especially pronounced in low-resource settings that serve health disparity populations.
Often, practitioners identify problems with existing EBIs originally developed and tested with populations different from their target population and introduce needed adaptations to make the intervention more suitable. Although some EBIs have been extensively adapted for diverse populations and evaluated, most local adaptations to improve fit for health disparity populations are not well documented or evaluated. As a result, empirical evidence is often lacking regarding the potential effectiveness of specific adaptations practitioners may be considering.
We advocate an expansion in the emphasis of adaptation research from researcher-led interventions to research that informs practitioner-led adaptations. By presenting a research vision and strategies needed to build this area of science, we aim to inform research that facilitates successful adaptation and equitable implementation and delivery of EBIs that reduce health disparities.
Many evidence-based interventions (EBIs) exist to address a variety of health issues, but most have not been designed to maximize fit for health disparity populations (see the box on page S95 for definitions of terms used in this essay). Health disparity populations have been underrepresented in research testing the efficacy of interventions to improve health.3,4 Resulting problems with EBI relevance and implementation challenges with health disparity populations can have significant consequences. Low rates of EBI adoption or sustainability in settings that serve disadvantaged populations diminish the capacity of EBIs to reduce or eliminate health disparities by limiting access to these potentially helpful interventions. Moreover, adoption of EBIs for which advantaged populations show greater benefit may actually increase health disparities.5
Definitions of Terms Relevant for Planned Adaptations by Practitioners Serving Health Disparity Populations.
| Adaptation: modifications to content, format, or mode of delivery to an EBI in response to the needs and preferences of the target population or characteristics of the intervention setting to maintain or improve an EBI’s effectiveness. |
| Researcher-led adaptation: adaptation by researchers or originators of the EBI. |
| Ad hoc adaptation: adaptation by practitioners during intervention implementation or delivery. |
| Planned adaptation: adaptation by practitioners before intervention implementation. |
| Evidence-based interventions: tested prevention and treatment interventions, also identified as evidence-based practices, empirically supported treatments, and empirically validated treatments. EBIs address a variety of health conditions and may include singe or multilevel (e.g., individual, group, family, or community level) interventions. |
| Health disparity populations: socially or economically disadvantaged populations that have a demonstrated pattern of poorer health outcomes than do more advantaged populations. National Institutes of Health–designated health disparity populations include Blacks/African Americans, Hispanics/Latinos, Asians, American Indians/Alaska Natives, Native Hawaiians/other Pacific Islanders, socioeconomically disadvantaged populations, underserved rural populations, and sexual or gender minorities.1 |
| Practitioners: organizations or agencies that deliver EBIs, including health care systems, public health departments, social service agencies, criminal justice systems, schools, community-based organizations, and other service settings. |
| Science of intervention adaptation: the systematic examination through empirical observation or experimental manipulation of how adaptations to EBIs are originated and implemented, including evaluation of the efficacy and sustainability of the adapted EBI. Historically, the science of intervention adaptation has emphasized randomized controlled trials of adapted EBIs.2 |
Note. EBI = evidence-based intervention.
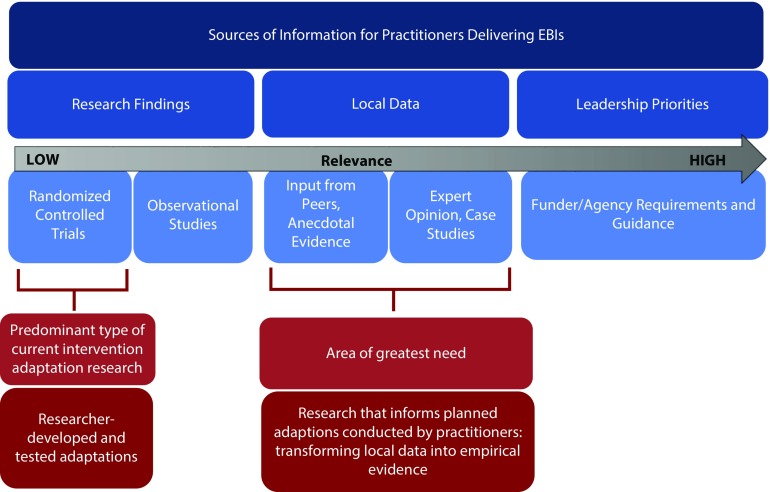
If EBIs are to reduce health disparities, they must be tailored to the needs and characteristics of the intended health disparity populations as well as the settings in which these populations receive services.6 Thus, intervention adaptation by practitioners who serve health disparity populations is often a necessary step in the EBI implementation process. Researchers can provide invaluable information to practitioners to inform what types of adaptations may be most effective. Unfortunately, a significant disconnect exists between the types of information that practitioners find useful and the predominant types of information that intervention adaptation researchers are producing. Studies examining how public health practitioners use research evidence find that funder and organization leadership priorities and guidance are of primary importance, and research evidence, particularly findings from an individual study, is much less likely to be used to inform decision-making.7,8 Practitioners also often consider local evidence, including stakeholder input and success stories in the organization or similar settings, as more relevant than research studies with questionable applicability or conflicting findings.8,9 This hierarchy of information according to the relevance and value for practitioners is depicted in Figure 1.
FIGURE 1—
The Mismatch Between Information Relevant to Practitioners and Information Generated by Researchers
By contrast, even though intervention adaptation research falls at the end of the translational research spectrum, which ranges from basic research to population-level health outcomes research,10 much intervention adaptation research is not necessarily geared toward informing the work of practitioners responsible for achieving those community- or population-level health outcomes. For example, the most common type of grant application related to intervention adaptation submitted to the National Institute on Minority Health and Health Disparities (NIMHD) involves the development and evaluation of EBIs adapted for a particular health disparity population, with the adaptation process led by researchers. Far less common are application submissions that characterize and evaluate adaptations of EBIs done in the field by community organizations or practitioners.
Thus, as depicted in Figure 1, we argue that much of current intervention adaptation research follows the existing research hierarchy, which places high value on methodologies with high internal validity, such as the randomized controlled trial, and lower value on methodologies that emphasize local context, such as case studies and the analysis of practice-based evidence.11 This evidence hierarchy is essentially the opposite for practitioners, for whom local context and relevance are of greater value. This apparent disconnect between what researchers are currently doing and what is most useful to practitioners is of heightened relevance for the adaptation of EBIs for health disparity populations, as EBIs may be less likely to be successful for these populations “out of the box” than for more advantaged populations. One way to address this disconnect is for researchers to conduct rigorous and systematic analysis of local data to generate empirical evidence relevant to a broad audience of practitioners.
We argue for enhancing the relevance of the growing science of intervention adaptation through research that informs evidence-based decision-making for practitioners adapting EBIs for health disparity populations. Specifically, we advocate an expansion of focus from researcher-developed and tested adaptations, a necessary and critical step that has facilitated the availability of EBIs for health disparity populations, to include research that informs planned adaptations conducted by practitioners. This topic emerged as a priority in the NIMHD science visioning process that brought together intervention researchers to identify strategies to further mature the field of health disparities research.
PLANNED ADAPTATIONS BY PROVIDERS
Researcher-led adaptations have been supported by a growing scientific literature that has identified frameworks12,13 to guide researchers developing and evaluating adapted interventions that maintain the original EBI’s core components, while being responsive to the needs of the new population.14 These adaptation models often involve a lengthy process that culminates in a clinical trial evaluating the effectiveness of the adapted intervention, a process that may take several months or years and external funding. Such models are likely to be of limited utility to practitioners because of the prolonged nature of the implementation and translation processes involved.8 Practitioners faced with the urgent and complex health needs of disparity populations are typically on a more compressed timeline regarding the selection and adaptation of EBIs.
By contrast, practitioners who observe significant problems with an original EBI may introduce ad hoc adaptive changes in content or format in response to emerging needs of participants. Typically, these ad hoc adaptations have not been well documented or assessed for their effectiveness in producing desired health outcomes. Thus, the beneficial or detrimental effects of these ad hoc adaptations are often unknown. Because of the limitations of ad hoc adaptations, planned adaptations, in which practitioners engage local stakeholders in the planning and modification of an EBI to meet local needs, may be more successful and sustainable.15
Although planned adaptations may be assessed as part of routine program evaluation by practitioners or funders, they have not typically been the focus of rigorous, systematic evaluation by researchers. However, generating evidence on planned adaptations and their effects on outcomes for health disparity populations could contribute substantially to the development of guidance to inform practice. For example, an agency planning to implement an EBI using licensed clinicians might conclude that using community health workers is more feasible for the setting and more culturally congruent for the target population. However, the agency may lack information about whether the intervention adapted in this way will retain its effectiveness, as some types of interventions may be more amenable to delivery by community health workers than are others. Although a variety of published frameworks exists to guide practitioners through the conceptual process to generate proposed adaptations,12,13 practitioners also need empirical data on the kinds of adaptations that are effective for certain populations and service delivery contexts. In the absence of systematic evidence on which to base their decisions on how to adapt, practitioners may have to rely on anecdotal evidence or case studies.16
We would like to emphasize that research to inform and evaluate planned evaluations by practitioners does not refer to research adaptations conducted in collaboration with practitioners or other community partners. This is already standard practice. Rather, we are advocating an expansion in emphasis from community-partnered researcher-led intervention adaptation studies to include community-partnered research to inform practitioner-led adaptations.
RESEARCH VISION FOR BUILDING THE EVIDENCE BASE
Because the original context in which an EBI was developed and the real-world needs of local health disparity communities can differ dramatically, EBIs often require extensive adaptations to intervention content and delivery.17 Important factors practitioners often consider for such adaptations include acceptability, practicality, feasibility, and integrability, which are defined and described in the box at the top of page S97. Adaptations addressing these factors to improve the fit of an EBI with a population or setting may lead to changes in modality (e.g., in-person vs Web based), level of intervention (e.g., family vs individual), setting (e.g., community based vs clinic based), personnel to deliver or support the intervention (e.g., community health worker vs licensed professional), or content (e.g., emphasis on wellness rather than illness) of EBIs.
Types of Adaptations Practitioners May Consider When Adapting Evidence-Based Interventions (EBIs) for Health disparity populations.
| Criterion | Definition | Examples |
| Acceptability | Compatibility of EBI content, approach, and theoretical model with culture, language, beliefs, and ecological context of population | Is the EBI suitable for the population in terms of culture, language, literacy level, and content? |
| Is the EBI sensitive to the values and illness or wellness experiences of the population? | ||
| Practicality | Appropriateness of EBI in terms of participant effort required and convenience; fit with participants’ life demands | Is the effort required to participate reasonable? |
| What core EBI elements are important to retain? | ||
| Can any EBI elements be shortened or omitted? | ||
| Feasibility | Appropriateness of EBI in terms of practitioner effort and skills required to deliver program; feasibility of delivery modes and formats | Can the EBI be delivered by community health workers or other peer professionals instead of health care professionals? |
| Is a group or individual format more feasible? | ||
| Are in-person, electronic, or written formats most appropriate or can they be combined? | ||
| Is the cost to deliver the program reasonable? | ||
| Integrability | Congruence of EBI with organization or system philosophy, mission, culture, and practices | Does the EBI help advance the mission of the organization? |
| Does the EBI provide added value to the system’s programmatic efforts? | ||
| Is the EBI compatible with the organizational culture of the setting? | ||
| Can the EBI be combined with or embedded within other services or programs? |
Practitioners may use a variety of approaches to identify appropriate strategies to improve the acceptability, practicality, feasibility, and integrability of an EBI, such as funder guidance, consultation with intervention developers, community input, and past experience. However, even if there is a strong conceptual rationale for making specific adaptations, little information may be available about whether such adaptations are likely to produce successful outcomes.
The following recommendations lay out a critical research agenda that can be used to provide empirically supported answers to key questions practitioners may have about adaptation decisions. This agenda, summarized in the box at the bottom of page S97, is organized around 2 distinct research activities: analysis of practice-based data and intervention studies.
Recommended Research Agenda to Build Evidence Base for Planned Evidence-Based Interventions (EBIs) Intervention Adaptations for Health disparity populations.
| Support systematic analysis of practice-based data to examine |
| • The incremental benefit of using adapted interventions vs the original EBI |
| • Effectiveness of different types of adaptations in varied contexts |
| • Utility of using published adaptation frameworks |
| • Success of community engagement strategies |
| • Impact of adapted interventions on health disparities |
| Conduct intervention studies to inform intervention adaptations by practitioners through |
| • Ascertaining critical intervention elements |
| • Cost–benefit analysis of adapted interventions |
| Build infrastructure needed to achieve this research vision, including |
| • Prioritization and funding for research |
| • Platforms housing archival data to inform EBI adaptations |
| • Training in research, reporting, and analysis related to adaptation of EBIs |
SYSTEMATIC ANALYSIS OF PRACTICE-BASED DATA
Although meta-analyses on the effectiveness of different types of adapted interventions, particularly cultural adaptations, have been conducted,18 these studies have examined only a small portion of the universe of adapted interventions that are implemented in practice.2,19 Because the vast majority of adaptations of EBI are not represented in the published scientific literature, data are lacking on the types of adaptations that have been undertaken in practice and their impact on intervention effectiveness and sustainability.20 This “in-the-field” practice-based evidence can generate more data points with respect to the multitude of EBIs, target populations, intervention settings, and specific adaptations than could ever be accomplished through randomized trials or meta-analyses of published studies. Analysis of practice-based data can also address the issue of the lack of relevance of research findings compared with local evidence—this approach offers the opportunity to aggregate locally collected data to enhance applicability to many more settings. Practice-based data can be particularly useful in understanding the incremental benefit of using adapted interventions over the original EBI, effectiveness of different types of adaptations in different contexts, the utility of using established adaptation frameworks, the success of different types of community engagement strategies, and the impact of adapted interventions on health disparities.
Adapted vs Original Interventions
Practice-based data can be used to assess the effectiveness of adapted EBIs for different health disparity populations relative to the original EBI. Meta-analyses and systematic reviews find that some culturally tailored interventions, particularly mental health interventions, appear to be more effective with racial/ethnic minorities than do those developed for a general or nonminority population.21 However, direct comparisons of tailored and nontailored interventions in the same research study are rare, and findings among studies that do provide direct comparisons are inconclusive.20,22 Some culturally adapted interventions demonstrate increased engagement of health disparity populations without a corresponding improvement in health outcomes.22 More common than direct comparison, adapted interventions are often compared with usual care or some other condition, indicating that the adapted intervention “works” but not necessarily that it works better than the original EBI. Analysis of practice-based data can determine whether intervention benefits are similar to those of the original EBI, information that is critical to help practitioners decide whether to adapt and what types of adaptation are necessary.
Effectiveness of Different Adaptations
Data about the types of adaptations undertaken in practice and their impact on intervention effectiveness and sustainability would be invaluable to practitioners faced with their own decision-making regarding adaptation. Such practice-based evidence from settings that serve health disparity populations could answer fundamental questions about the effects of specific types of planned adaptations undertaken to improve acceptability, practicality, feasibility, and integrability with respect to targeted health conditions or outcomes, service delivery systems, and population characteristics and preferences.
Utility of Published Adaptation Frameworks
In addition to a need for evidence about the effectiveness of specific intervention adaptations, evidence is also needed about the process of adaptation. Various intervention adaptation frameworks and strategies have now been published in the scientific literature.13 Many frameworks emphasize acceptability or practicality of EBI content or format more than feasibility and integrability. These additional dimensions are likely to require adaptation for use with health disparity populations. Therefore, analysis of the use of frameworks and strategies, the duration of the adaptation process, and the ultimate success of implementing the adaptation would help practitioners determine which frameworks may be most useful for their setting and populations. In addition, data from these planned adaptations can also provide empirical feedback for expanding and improving existing adaptation frameworks.
Success of Community Engagement Strategies
It is generally accepted that obtaining the perspectives, priorities, and preferences of the target communities and other stakeholders is essential to successful implementation and sustainability of EBIs.23 To build the evidence base in this area, research is needed to understand which engagement strategies may be most useful for obtaining stakeholder input about adaptation for health disparity populations under various circumstances. Information regarding the acceptability, cost, and utility of different community engagement strategies (e.g., town hall meetings, presentations to community organizations and advocacy groups, consumer focus groups, client interviews) could identify cost-effective methods for engaging communities in efforts to adapt EBIs.
Impact on Health Disparities
In the general population, studies have shown that local adaptations can maintain or increase an EBI’s effectiveness.24 However, the impact of adaptations made to EBIs on health disparities is largely unknown, as this metric is missing from most evaluations of intervention success.25 Most evaluations are limited to assessing improvement in health outcomes for a particular health disparity population rather than whether the intervention closed the gap in outcomes between health disparity populations and their more advantaged counterparts. This information is critical to practitioners and funders whose mission includes reducing or eliminating health disparities.
INTERVENTION STUDIES TO INFORM ADAPTATIONS
It is not possible for clinical trials evaluating individual adapted EBIs to provide sufficient evidence to inform practitioners across the full gamut of EBIs, service settings, and target populations.26 However, certain types of intervention studies can generate specific information that may be difficult or impossible to obtain from practice-based data. Two types of intervention research can build the evidence base for adaptation for health disparity populations: identification of critical intervention elements and cost effectiveness of adapted interventions.
Ascertaining Critical Components
Across adaptation frameworks, a common theme is the importance of retaining an EBI’s core elements. Identifying the theories underlying the approach and content of an EBI is important in clarifying the intervention’s intended effects for changing targeted outcomes. The assumption is that adaptations that do not retain the core theoretical components will lose effectiveness because the mechanisms of action are diminished. Whether all or some of these core components are necessary to achieve desired health outcomes remains an empirical question in addition to a conceptual one.
Multiphase optimization strategy (MOST) trials, which use a factorial design to randomly assign participants to different combinations of interventions or intervention components, can be used to determine which elements are critical to EBI effectiveness and which can be omitted without compromising intervention benefits.27 MOST designs have the advantage of allowing the testing of multiple intervention elements and combinations of elements without requiring large sample sizes that would be needed to compare complete interventions.27 Results from MOST designs also may be particularly useful to address feasibility and acceptability issues. Practitioners can use this information to make informed decisions regarding which elements of an EBI may be best suited to the resources and capacities of their organizations and the preferences of the target population.28
Similarly, Sequential Multiple Assignment Randomized Trial designs, in which interventions or intervention components are tested in sequential, randomly assigned stages, may also be useful to identify critical intervention elements.29 Particularly for resource-poor settings or target populations with limited time or ability to participate in lengthy multicomponent interventions, these designs may help to identify intervention decision rules, such as offering more costly or time-intensive components of an EBI only to those who do not benefit from less intensive components.
Cost–Benefit Analysis of Adapted Interventions
Cost considerations are critical to practitioners and funders when selecting and adapting EBIs. Adaptations that facilitate engagement of disadvantaged populations, such as greater frequency of contact with providers or the addition of community health workers, may increase the costs of an EBI. Alternatively, practitioners may consider adaptations to reduce the cost of an EBI to fit the available budget or resources, such as shortening the intervention or replacing licensed health care professionals with peer advisors or paraprofessionals to deliver the intervention. Cost-effectiveness analyses to examine the costs and benefits of EBIs and adaptations from individual, provider, payer, or societal perspectives offer unique information not likely to be available from practice-based data. These data can provide funders, implementers, and policymakers with needed information on the costs and resources necessary for adapting, implementing, and sustaining EBIs in various settings.
INFRASTRUCTURE TO ACHIEVE RESEARCH VISION
Advancing a research vision to inform evidence-based planned intervention adaptation for practitioners requires a paradigm shift to move beyond existing silos that separate intervention research, implementation research, service delivery, and program evaluation. Capacity building to promote links across these domains is needed in the areas of research prioritization and funding, data platforms, and training for practitioners and researchers.
Research Prioritization and Funding
As mentioned, the hierarchy of research evidence regarding health interventions has placed the individual-level randomized controlled trial at the highest level,11 with nonrandomized intervention designs and analysis of practice-based data falling lower in the hierarchy. To address the implementation gap between efficacy trials and adoption of EBIs in practice, the field of implementation science has introduced a series of alternative research designs to better evaluate intervention implementation and effectiveness in various practice settings and communities. Examples include benchmarking studies, which test adapted interventions by using rigorous pretest and posttest measures and comparing the effect sizes to that of the original EBI without the need for a new randomized controlled trial,30 and interrupted time-series analysis, which involves multiple assessments before and after intervention initiation.31 These and other alternative designs may be especially appropriate for conducting adaptation research because of their explicit focus on external validity and the heterogeneity of populations and settings in which interventions are delivered.32 To understand and promote the adoption of EBIs in diverse settings, it is critical that these alternative designs be accepted and adopted to provide relevant and valuable evidence that can inform practitioners.33
This needed prioritization is unlikely to happen in the absence of specifically targeted research initiatives, as the prevailing research hierarchy often makes it difficult for applications proposing implementation studies and analysis of practice-based evidence to fare well in peer review and receive funding. In the absence of grant funding, academic institutions are less likely to recognize this type of research as sufficient for faculty promotion or tenure.34 Research funders can lead the way by developing specific funding initiatives, providing guidance for maintaining rigor and reproducibility in such studies, and establishing peer review panels with appropriate training and expertise. More grant funding, in turn, can promote greater acceptance and endorsement of this research in academic and research institutions.
Platforms for Housing Archival Data
Chambers and Norton argue for a novel approach called the adaptome to better understand “the complexity of pathways that better characterize research-to-practice processes,”2(pS125) especially those that occur in practice settings and outside the research enterprise. The adaptome challenges the assumption that EBIs declared to be efficacious under randomized controlled trials are fully optimized and require no further changes. An adaptome data commons that archives data on various types of adaptations performed by both researchers and practitioners could serve as the basis for generating evidenced-based guidance on intervention adaptation for health disparity populations. EBI registries could feed into the adaptome data commons and could include channels for practitioners to submit feedback on their experiences with implementation of these EBIs, as well as findings from research studies, that could inform future designs, development, and implementation.35
The adaptome data commons could also create a useful classification system of distinct types of adaptations, such as the one developed by Stirman et al.36 to facilitate data archiving and retrieval. Potential categories of adaptations include adding, removing, substituting, or reordering intervention elements; shortening the length or number of sessions; and changing the delivery format (e.g., from in-person to online sessions), target population (e.g., individual to family intervention), intervention setting (e.g., clinic based to school based), or intervention personnel (e.g., licensed health care professional to community health worker). This classification system also could include methods of obtaining community and other stakeholder input, personnel, and other resources required to implement the adapted intervention, the effectiveness and sustainability of the adapted EBI, and the impact on reducing health disparities using common metrics.37
Federal agencies such as the National Institutes of Health could host the adaptome data commons. For example, NIMHD is currently developing an intervention portal to serve as a repository for interventions shown to improve minority health or reduce health disparities. This portal is part of HDPulse (https://hdpulse.nimhd.nih.gov), an ecosystem that provides access to health disparities–related data and resources to design, implement, and evaluate evidence-based programs. The adaptome data commons could be an extension to this portal or similar federally sponsored data repositories or intervention compendia.
The commons curators could enter data from the original EBI as adaptations are entered into the system. Efforts to populate the commons could be facilitated if government funders of service delivery (e.g., Centers for Disease Control and Prevention, Substance Abuse and Mental Health Services Administration, Health Resources and Services Administration, and state health departments) required submission of data into the system by the practitioners they support to deliver EBIs. Research funders could require grantees to submit data about research adaptations into this system. However, even if data entry into the system were entirely voluntary, invaluable information could still be obtained from practitioners invested in tailoring EBIs to best serve the needs of health disparity populations. As an example of a voluntary repository, the Third Mission Institute (Instituto Tercera Mision) in Puerto Rico has established a local commons-like repository of EBI information and data. This institute works in partnership with local community-based organizations (http://archivopbe.info/home) in archiving treatment and prevention protocols of local evidence-based information and analysis to support the efforts of practitioners.38
Once populated with data on adaptations by researchers and practitioners, the adaptome data commons could serve as a source of secondary data for subsequent analyses by researchers (e.g., to identify the types of EBIs originally developed for in-person delivery that could be successfully adapted to an online format). The published results from such analyses could be entered into the commons so that they are more accessible to practitioners. In addition, the data commons could offer practitioners the opportunity to search for specific examples of adaptations that have been successful in settings or populations similar to their own (e.g., to determine whether a particular smoking cessation EBI had ever been successfully adapted for use with a rural American Indian/Alaska Native population) and address a specific challenge that practitioners face in trying to find relevant information that is scattered across different sources and media.39
Training in Research, Reporting, and Analysis
To contribute to and use the adaptome data commons, practitioners could receive training on processes of adaptation that retain intervention effectiveness, the use of practice-based data to inform adaptation decision-making, and the collection and reporting on subsequent intervention adaptations. Training for adaptation researchers should include alternative research designs beyond traditional individual-level randomized controlled trials,32 as well as cost-effectiveness analysis. Training on systems science approaches may be particularly valuable in analyzing practice-based data to model the complexity and essential ingredients of successful real-world implementation.40 Research training also should include community-engaged and community-based participatory research methods, as well as the use of mixed methods designs to provide a detailed understanding of ways to incorporate cultural factors into the adaptation and implementation of EBIs.33
CONCLUSIONS
The adaptation of EBIs by practitioners is a common occurrence across service sectors and populations. Practitioners who serve health disparity populations are presented with particular challenges because they are often faced with a choice between adhering to an EBI’s content and format with high fidelity or making potentially significant adaptations to enhance acceptability, practicality, feasibility, and integrability—without knowing whether these adaptations will be successful in maintaining the EBI’s effectiveness. Researchers can help practitioners make empirically informed choices by building the evidence base on how and why certain adaptations work, for whom, and under what conditions, as well as how these adaptations may reduce health disparities. Expanding the science of intervention adaptation to build the evidence base for health disparity populations is necessary to promote health equity and improve the nation’s health.
ACKNOWLEDGMENTS
This work was supported in part by the following institutes and offices of the National Institutes of Health: the National Institute on Minority Health and Health Disparities (NIMHD), the National Institute on Drug Abuse, the Office of Research on Women’s Health, and the Office of Disease Prevention.
This work resulted from an NIMHD-led workshop, which included external experts, to address intervention science for health disparities research.
Note. The final content is the responsibility of the authors and does not necessarily represent the perspective of the US government.
CONFLICTS OF INTEREST
No conflicts of interest.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed because no human participants were involved.
REFERENCES
- 1.National Institute on Minority Health and Health Disparities. NIMHD research framework. 2017. Available at: https://www.nimhd.nih.gov/about/overview/research-framework.html. Accessed October 16, 2017.
- 2.Chambers DA, Norton WE. The adaptome: advancing the science of intervention adaptation. Am J Prev Med. 2016;51(4 suppl 2):S124–S131. doi: 10.1016/j.amepre.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weisz JR, Ng MY, Bearman SK. Odd couple? Reenvisioning the relation between science and practice in the dissemination-implementation era. Clin Psychol Sci. 2013;2(1):58–74. [Google Scholar]
- 4.Erves JC, Mayo-Gamble TL, Malin-Fair A et al. Needs, priorities, and recommendations for engaging underrepresented populations in clinical research: a community perspective. J Community Health. 2017;42(3):472–480. doi: 10.1007/s10900-016-0279-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lorenc T, Oliver K. Adverse effects of public health interventions: a conceptual framework. J Epidemiol Community Health. 2014;68(3):288–290. doi: 10.1136/jech-2013-203118. [DOI] [PubMed] [Google Scholar]
- 6.Padwa H, Teruya C, Tran E et al. The implementation of integrated behavioral health protocols in primary care settings in Project Care. J Subst Abuse Treat. 2016;62:74–83. doi: 10.1016/j.jsat.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Fields RP, Stamatakis KA, Duggan K, Brownson RC. Importance of scientific resources among local public health practitioners. Am J Public Health. 2015;105(suppl 2):S288–S294. doi: 10.2105/AJPH.2014.302323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Graaf P, Forrest LF, Adams J, Shucksmith J, White M. How do public health professionals view and engage with research? A qualitative interview study and stakeholder workshop engaging public health professionals and researchers. BMC Public Health. 2017;17(1):892. doi: 10.1186/s12889-017-4896-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atkins MS, Rusch D, Mehta TG, Lakind D. Future directions for dissemination and implementation science: aligning ecological theory and public health to close the research to practice gap. J Clin Child Adolesc Psychol. 2016;45(2):215–226. doi: 10.1080/15374416.2015.1050724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blumberg RS, Dittel B, Hafler D, von Herrath M, Nestle FO. Unraveling the autoimmune translational research process layer by layer. Nat Med. 2012;18(1):35–41. doi: 10.1038/nm.2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansen HF. Organisation of evidence-based knowledge production: evidence hierarchies and evidence typologies. Scand J Public Health. 2014;42(13 suppl):11–17. doi: 10.1177/1403494813516715. [DOI] [PubMed] [Google Scholar]
- 12.Castro FG, Yasui M. Advances in EBI development for diverse populations: towards a science of intervention adaptation. Prev Sci. 2017;18(6):623–629. doi: 10.1007/s11121-017-0809-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Domenech Rodriguez MM, Bernal G. Conceptual frameworks of cultural adaptation. In: Bernal G, Domenech Rodriguez MM, editors. Cultural Adaptations: Tools for Evidence-Based Practice With Diverse Populations. Washington, DC: APA Press; 2012. pp. 23–45. [Google Scholar]
- 14.Singla DR, Weobong B, Nadkarni A et al. Improving the scalability of psychological treatments in developing countries: an evaluation of peer-led therapy quality assessment in Goa, India. Behav Res Ther. 2014;60:53–59. doi: 10.1016/j.brat.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barrera M, Jr, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol. 2013;81(2):196–205. doi: 10.1037/a0027085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Milat AJ, King L, Newson R et al. Increasing the scale and adoption of population health interventions: experiences and perspectives of policy makers, practitioners, and researchers. Health Res Policy Syst. 2014;12:18. doi: 10.1186/1478-4505-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nápoles AM, Santoyo-Olsson J, Stewart AL. Methods for translating evidence-based behavioral interventions for health-disparity communities. Prev Chronic Dis. 2013;10:E193. doi: 10.5888/pcd10.130133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Mourik K, Crone MR, de Wolff MS, Reis R. Parent training programs for ethnic minorities: a meta-analysis of adaptations and effect. Prev Sci. 2017;18(1):95–105. doi: 10.1007/s11121-016-0733-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramanadhan S, Crisostomo J, Alexander-Molloy J et al. Perceptions of evidence-based programs among community-based organizations tackling health disparities: a qualitative study. Health Educ Res. 2012;27(4):717–728. doi: 10.1093/her/cyr088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stirman SW, Gamarra J, Bartlett BA, Calloway A, Gutner C. Empirical examinations of modifications and adaptations to evidence-based psychotherapies: methodologies, impact, and future directions. Clin Psychol (New York) 2017;24(4):396–420. doi: 10.1111/cpsp.12218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall GC, Ibaraki AY, Huang ER, Marti CN, Stice E. A meta-analysis of cultural adaptations of psychological interventions. Behav Ther. 2016;47(6):993–1014. doi: 10.1016/j.beth.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Davidson E, Bhopal R et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess. 2012;16(44):1–469. doi: 10.3310/hta16440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boothroyd RI, Flint AY, Lapiz AM, Lyons S, Jarboe KL, Aldridge WA. Active involved community partnerships: co-creating implementation infrastructure for getting to and sustaining social impact. Transl Behav Med. 2017;7(3):467–477. doi: 10.1007/s13142-017-0503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKleroy VS, Galbraith JS, Cummings B et al. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Educ Prev. 2006;18(4 suppl A):59–73. doi: 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- 25.Welch V, Tugwell P, Petticrew M et al. How effects on health equity are assessed in systematic reviews of interventions. Cochrane Database Syst Rev. 2010;12:MR000028. doi: 10.1002/14651858.MR000028.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacDonald M, Pauly B, Wong G et al. Supporting successful implementation of public health interventions: protocol for a realist synthesis. Syst Rev. 2016;5:54. doi: 10.1186/s13643-016-0229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Collins LM, Murphy SA, Nair VN, Strecher VJ. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med. 2005;30(1):65–73. doi: 10.1207/s15324796abm3001_8. [DOI] [PubMed] [Google Scholar]
- 28.Collins LM, Kugler KC, Gwadz MV. Optimization of multicomponent behavioral and biobehavioral interventions for the prevention and treatment of HIV/AIDS. AIDS Behav. 2016;20(suppl 1):S197–S214. doi: 10.1007/s10461-015-1145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent ehealth interventions. Am J Prev Med. 2007;32(5 suppl):S112–S118. doi: 10.1016/j.amepre.2007.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spilka MJ, Dobson KS. Promoting the internationalization of evidence-based practice: benchmarking as a strategy to evaluate culturally transported psychological treatments. Clin Psychol Sci Pract. 2015;22(1):58–75. [Google Scholar]
- 31.Bonell CP, Hargreaves J, Cousens S et al. Alternatives to randomisation in the evaluation of public health interventions: design challenges and solutions. J Epidemiol Community Health. 2011;65(7):582–587. doi: 10.1136/jech.2008.082602. [DOI] [PubMed] [Google Scholar]
- 32.Brown CH, Curran G, Palinkas LA et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. 2017;38:1–22. doi: 10.1146/annurev-publhealth-031816-044215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tucker JA, Roth DL. Extending the evidence hierarchy to enhance evidence-based practice for substance use disorders. Addiction. 2006;101(7):918–932. doi: 10.1111/j.1360-0443.2006.01396.x. [DOI] [PubMed] [Google Scholar]
- 34.Ammerman A, Smith TW, Calancie L. Practice-based evidence in public health: improving reach, relevance, and results. Annu Rev Public Health. 2014;35:47–63. doi: 10.1146/annurev-publhealth-032013-182458. [DOI] [PubMed] [Google Scholar]
- 35.Leviton LC. Generalizing about public health interventions: a mixed-methods approach to external validity. Annu Rev Public Health. 2017;38:371–391. doi: 10.1146/annurev-publhealth-031816-044509. [DOI] [PubMed] [Google Scholar]
- 36.Stirman SW, Miller CJ, Toder K, Calloway A. Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implement Sci. 2013;8:65. doi: 10.1186/1748-5908-8-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ng E, de Colombani P. Framework for selecting best practices in public health: a systematic literature review. J Public Health Res. 2015;4(3):577. doi: 10.4081/jphr.2015.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sardiñas LM, Padilla V, Aponte M et al. Identification de intervenciones para el desarollo positivo de la juventud. Rev Puertorriquena Psicol. 2017;28(1):14–32. [PMC free article] [PubMed] [Google Scholar]
- 39.Ford J, Korjonen H. Information needs of public health practitioners: a review of the literature. Health Info Libr J. 2012;29(4):260–273. doi: 10.1111/hir.12001. [DOI] [PubMed] [Google Scholar]
- 40.Green LW. Public health asks of systems science: to advance our evidence-based practice, can you help us get more practice-based evidence? Am J Public Health. 2006;96(3):406–409. doi: 10.2105/AJPH.2005.066035. [DOI] [PMC free article] [PubMed] [Google Scholar]