Abstract
Purpose:
To improve persistence of adoptively transferred T cell receptor (TCR)-engineered T cells and durable clinical responses, we designed a clinical trial to transplant genetically-modified hematopoietic stem cells (HSCs) together with adoptive cell transfer (ACT) of T cells both engineered to express an NY-ESO-1 TCR. Here, we report the preclinical studies performed to enable an investigational new drug (IND) application.
Experimental design:
HSCs transduced with a lentiviral vector expressing NY-ESO-1 TCR and the PET reporter/suicide gene HSV1-sr39TK and T cells transduced with a retroviral vector expressing NY-ESO-1 TCR were co-administered to myelodepleted HLA-A2/Kb mice within a formal GLP-compliant study to demonstrate safety, persistence and HSC differentiation into all blood lineages. Non-GLP experiments included assessment of transgene immunogenicity and in vitro viral insertion safety studies. Furthermore, GMP-compliant cell production qualification runs were performed to establish the manufacturing protocols for clinical use.
Results:
TCR genetically-modified and ex vivo cultured HSCs differentiated into all blood subsets in vivo after HSC transplantation, and co-administration of TCR-transduced T cells did not result in increased toxicity. The expression of NY-ESO-1 TCR and sr39TK transgenes did not have a detrimental effect on gene-modified HSCs differentiation to all blood cell lineages. There was no evidence of genotoxicity induced by the lentiviral vector. GMP batches of clinical-grade transgenic cells produced during qualification runs had adequate stability and functionality.
Conclusion:
Co-administration of HSCs and T cells expressing an NY-ESO-1 TCR is safe in preclinical models. The results presented in this manuscript led to the U.S. FDA approval of IND 17471.
Keywords: NY-ESO-1 TCR, adoptive cell therapy, genetically modified hematopoietic stem cells, safety, gene therapy investigational new drug (IND) application
Introduction
Adoptive transfer of T cells genetically modified to express tumor-specific T cell receptors (TCR) has shown remarkable antitumor efficacy in several clinical trials (1–7). However, durable long-term clinical responses have been more challenging to maintain (4,6), while engraftment and persistence of the modified T cells have been associated with better antitumor responses (4,5,8).
To improve the persistence of the TCR-expressing T cells, we propose to use genetically modified hematopoietic stem cells (HSCs) as a source for constant endogenous renewal of TCR-engineered T cells. The use of genetically modified HSCs was first shown to be efficacious in primary immunodeficiencies, where the transplantation of genetically modified HSCs demonstrated long-term correction of the disease (9–11). Regarding its use in cancer immunotherapy, it has been previously shown in murine and humanized murine models that transplantation of HSCs engineered to express a tumor-specific TCR results in the output of functional T cells with the defined specificity after proper thymic selection. The newly generated T cells showed antitumor activity, and were able to differentiate into memory T cells after antigen stimulation (12–18). The endogenously produced TCR-engineered T cells demonstrated allelic exclusion, a process in which the TCR transgenic chains inhibit the expression of the endogenous TCR chains, thereby avoiding TCR mispairing and consequently reducing the potential toxicity of the therapy (19).
To test the approach of TCR genetic engineering of HSCs in the clinic, we designed a clinical trial of double cell therapy co-administering HSCs and T cells both genetically modified to express an NY-ESO-1 TCR. We propose to use two TCR-engineered cell therapies because we anticipate that the TCR-engineered HSCs will endogenously differentiate into fully active mature T cells with a long delay in their appearance in the periphery, as new T cells reaching peripheral circulation must undergo a thymic selection process which takes one to three months (20,21). In this clinical trial, TCR-engineered mature lymphocytes and TCR-engineered HSCs will be co-administered to patients with NY-ESO-1-positive advanced cancers after a myelo- and lymphodepleting conditioning regimen. We hypothesize that the TCR-engineered mature lymphocytes will expand in vivo and provide the first wave of transient antitumor activity. This will serve as a bridge until the second wave of TCR-transgenic cells arising from the bone marrow-engrafted gene-modified HSCs has gone through the T lymphocyte maturation process and partially repopulated peripheral tissues (Supplemental Figure 1).
We propose to use the NY-ESO-1 TCR for this clinical trial since the toxicities observed in adoptive T cell therapy clinical trials using this TCR were not dose-limiting and unrelated to the TCR recognizing its cognate antigen, which in adult life is presented by the cancer cells and absent in most normal somatic cells (3,5,6). NY-ESO-1 is a cancer-testis antigen expressed at high homogeneous levels in synovial sarcoma, with lower frequency of expression in melanoma and multiple myeloma, and at even lower levels in other cancers (22–24). The NY-ESO-1 TCR used in this work recognizes the SLLMWITQC NY-ESO-1 epitope in the context of HLA-A*0201 and contains a two amino acid substitution in the third complementary determining region that increases its affinity for peptide-MHC complexes (25).
Herein we report on preclinical studies performed to demonstrate the safety and feasibility of the approach. These studies led to the investigational new drug (IND) application approval for a new clinical trial that is being conducted at UCLA (NCT03240861). Based on the previous experience with adoptive T cell transfer using the NY-ESO-1 TCR, the major safety concerns were focused on the transplantation with lentivirally modified HSCs and the untested effects of the co-administration of the HSCs and T cells both expressing the same NY-ESO-1 TCR. The preclinical studies performed to justify the safety of our approach adressed: i) the ability of the genetically modified and ex vivo cultured Lin- cells to differentiate into all blood lineages; ii) the effect of the co-administration of genetically modified Lin- cells and T cells on the engraftment and proliferation of the T cells and the engraftment and differentiation of the HSCs; iii) the immunogenicity of the NY-ESO-1 TCR and the sr39TK transgenes caused by their expression in the various hematopoietic cells; iv) the potential genotoxicity induced by the lentiviral vector integration in the Lin- cells; and v) the ability of the sr39TK suicide gene to ablate transduced stem cell progeny in case of a serious adverse event. To test the feasibility of the clinical trial, we validated the HSC cell product manufacturing process and demonstrated the stability and functionality of the final product. The data presented on the manuscript is focused on the approach-specific studies. Detailed information on the viral vector manufacturing, lot release criteria and optimization of the gene modified cell manufacturing can be found in the Supplemental Data Section.
Materials and Methods
Bone marrow transplantation (BMT) experiments:
All animal experiments were performed under the UCLA Animal Research Committee protocol #2013–095 that was previously approved by the IACUC. Lin- cells were isolated from the bone marrow of HLA-A2/Kb transgenic mice (26), pre-stimulated with cytokines, transduced with previously validated lentiviral vectors LV-NY-ESO-1 TCR/sr39TK, LV-NY-ESO-1 TCR, or LV-empty and cultured in vitro. For the co-administration experiments, T cells were isolated from spleens from HLA-A2/Kb transgenic mice, activated with CD3/28 and IL-2 stimulation, transduced with the RV-NY-ESO-1 TCR and expanded in vitro. The methods and reagents to manufacture and validate both cell products are described in the supplemental materials. Transduced Lin- cells alone or together with transduced T cells were administered systemically to 8- to 12-week-old HLA-A2/Kb mice that had received total body irradiation with 900cGy the day prior to cell administration. A detailed description of the cell testing performed prior to administration and the cell doses can be found in the supplemental material and methods. Five days or three months after the BMT, mice were euthanized and hematology, serum chemistry, complete histopathology survey, lentivirus and retrovirus vector copy number (VCN) in the blood, spleen and bone marrow and TCR expression and phenotype analysis in the bone marrow and spleen were performed. A detailed explanation of these procedures can be found in the supplemental material and methods.
In vitro immortalization assays:
Lin- cells from C57BL/6J (Jackson Laboratories, Bar Harbor, ME) mice were transduced with the LV-NY-ESO-1 TCR/sr39TK vector or the retrovirus SF91-eGFP-WPRE, expanded and seeded at limiting dilution. The growth of transformed clones was measured. This procedure is detailed in the supplemental material and methods.
LV-NYESO TCR/sr39TK Peripheral Blood Stem Cells (PBSC) manufacturing and stability evaluation:
The CD34+ cell population was enriched using the CliniMACS®CD34 reagent system, pre-stimulated overnight and transduced with LV-NYESO TCR/sr39TK vector supernatant at a final multiplicity of infection (MOI) of 50 (two transduction cycles of 25 MOI each). After 18±6 hours from the first transduction, cells were harvested, formulated in cryopreservation solution and cryopreserved using a controlled-rate freezer. The cell product was tested for sterility, endotoxin levels, mycoplasma contamination, clonogenic potential and transduction efficiency. Long-term stability of the cryopreserved cell product was evaluated 30±7, 90±7 and 180±10 days post-cryopreservation. The post-thaw stability of the cell product was tested over a 48-hour period. See supplemental material for further details.
Statistical analysis:
Described in the supplemental materials.
Results
Generation of clinical-grade lentiviral and retroviral vectors expressing NY-ESO-1 TCR
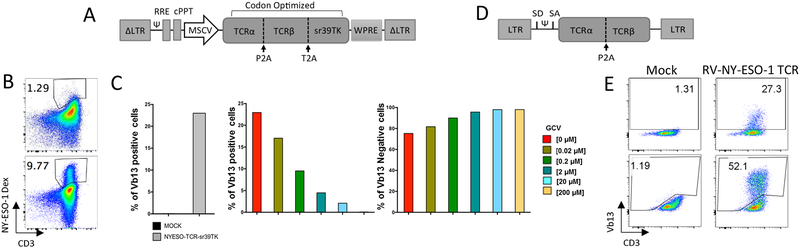
The lentiviral vector used in this clinical trial, LV-NY-ESO-1 TCR/sr39TK (RRL-MSCV-optNYESO-optsr39TK-WPRE, Figure 1A), expresses the alpha and beta chains of the NY-ESO-1 TCR and the sr39TK suicide/PET reporter gene linked by a 2A self-cleavage peptide, and has been previously described in preclinical studies (17). The expression of the transgenes is driven by the murine stem cell virus (MSCV) promoter derived from the MSCV retrovirus long terminal repeat (LTR). Both genes had been codon-optimized to improve expression in mammalian cells. This vector was produced at Good Manufacturing Practice (GMP) grade at the Indiana University Vector Production Facility (IU VPF). To have enough vector for all of the IND-enabling studies and product manufacture optimization, a first manufacture of a 20-liter preparation without full lot release testing was labeled as GMP-comparable lot and was used for the majority of the preclinical studies. A second GMP production of 60 liters that was tested and met all of the lot release criteria (Supplemental Tables 1 and 2) was used for preclinical studies of cell product manufacturing and functionality, and will be used for clinical product manufacturing. To characterize the functionality of the lentiviral vector, we measured: i) the expression of the NY-ESO-1 TCR on the cell surface by dextramer staining in transduced human PBMCs (Figure 1B); and ii) the sr39TK suicide gene function in transduced human CD34+ peripheral blood stem cells (PBSC). Following treatment of human CD34+ PBSC with increasing doses of ganciclovir in vitro, the number of NY-ESO-1 TCR-positive cells (Vβ13+ cells) decreased while the number of TCR-negative cells remained constant (Figure 1C).
Figure 1. Lentiviral and retroviral vector characterization.
A. LV-NY-ESO-1 TCR/sr39TK (RRL-MSCV-optNYESO-optsr39TK-WPRE) self-inactivating third-generation lentiviral vector scheme. B. NY-ESO-1 TCR expression in human PBMCs three days after transduction. Percentage of NY-ESO-1 TCR and CD3 expression were measured by flow cytometry with NYESO-1(157–162) dextramer and anti-CD3 antibody in mock-transduced (top panel) and transduced (bottom panel) PBMCs. C. In vitro sr39TK functionality in hCD34+. Mock-transduced or LV-NY-ESO-1 TCR/sr39TK-transduced human CD34+ cells were treated with 0, 0.02, 0.2, 2, 20 or 200μM ganciclovir (GCV) for 48 days. Left, TCR expression (measured by Vβ13 staining) in cells not treated with GCV. Percentage of Vβ13+ (center) and Vβ13- cells (right) in the transduced CD34+ cells after GCV treatment at the indicated concentrations. Vβ13 expression was measure by flow cytometry D. RV-NY-ESO-1 TCR (MSGV1-A2aB-1G4A-LY3H10) gamma-retroviral vector scheme. E. NY-ESO-1 TCR expression in murine T cells from HLA-A2/Kb mice two days after transduction. Surface (top panels) and total (surface + intracellular, bottom panels) TCR expression was measured by Vβ13 TCR beta chain and surface CD3 staining detected by flow cytometry. Abbreviations: Ψ, packaging signal; cPPT, central polypurine tract; LTR, long terminal repeat; MSCV, murine stem cell virus promoter; RRE, Rev response element; SA, splicing acceptor; SD, splicing donor; WPRE, woodchuck hepatitis virus posttranslational response element.
To genetically engineer the peripheral T cells for short-term anti-tumor activity while awaiting the emergence of TCR transgenic T cells from the transplanted HSCs, a preparation of 18 liters of GMP-grade retroviral vector expressing the NY-ESO-1 TCR chains, RV-NY-ESO-1 TCR (MSGV1-A2ab-1G4A-Ly3H10), was made at the IU VPF. The vector met all of the release criteria (Supplemental Table 3). This retroviral vector is a splicing-optimized MSCV-derived vector expressing the alpha and the beta chains of the NY-ESO-1 TCR linked by a P2A self-cleavage peptide (a kind gift from Dr. Steven A. Rosenberg and Dr. Paul Robbins, Figure 1D). For the studies in mice presented in this manuscript, we pseudotyped the clinical vector with an ecotropic envelope, and a 3-liter GMP-comparable batch was produced at the IU VPF. For the GMP-comparable vector, only partial lot release testing was performed (Supplemental Table 4). To demonstrate the functionality of the ecotropic RV-NY-ESO-1 TCR retroviral vector, we transduced murine T cells from HLA-A2/Kb mice and measured the expression of extracellular and surface NY-ESO-1 TCR staining for the beta chain of the TCR (Vβ13 staining, Figure 1E).
Preparation for a Good Laboratory Practice (GLP) study in an academic setting
To formally test if the co-administration of both cell products is safe, it was necessary to set up all of the conditions required to conduct a complete toxicology study under GLP conditions in compliance with 21 CFR Part 58. As GLP studies require exclusively dedicated facilities, a new laboratory space was set up with certified and calibrated equipment, with continuous automated monitoring of all the equipment and a tracking system in place to assure that the raw materials, test articles and specimens were adequately preserved. One-hundred-twelve standard operating procedures (SOPs) were generated that captured all of the intended procedures for the study, including the specifics of the scientific protocols, facility and equipment management, personnel training and GLP procedures. All of the personnel involved in the study were qualified to perform their assignments, and curricula vitae, job descriptions and training records were maintained to document their proficiency. The study required 32 personnel with job descriptions previously defined and recorded (see organizational chart in Supplemental Figure 2). All personnel were required to undergo documented training to conduct GLP studies and to perform the procedures for which they were responsible. In addition, all personnel were required to demonstrate proficiency using the pertinent SOPs according to their job descriptions. Prior to study initiation, the identity, purity and potency of the test articles were verified, acceptance criteria for the manufactured cells were established, and the study protocol was approved by the study director, the test facility management and the sponsor. This documentation was included in the IND later submitted to the FDA. Before the beginning of the study, a master schedule was generated and distributed to all personnel involved in the study. Sterility testing, blood and serum analysis and histopathology analysis were outsourced to GLP-compliant contract research organizations. The study included a full histopathological analysis performed by an ACVP board-certified veterinary pathologist. All raw data were signed by the study personnel performing the activity, reviewed by the study director or designee and archived. Any deviation from the SOPs, study protocol or GLP regulations was summarized in a deviation report, and its impact on the study data addressed by the study director and archived with the study documentation. All of the data generated in the study were included in a final study report that was submitted to the FDA in support of the IND application. All of the study raw data, specimens and test articles will be archived for 5 years after submission of the IND to the FDA. Finally, an independent Quality Assurance Unit audited all of the experimental portions of the study, the facilities, the SOPs, the study records and the GLP report and generated a Quality Assurance statement that was included in the final study report.
Establishment of a suitable syngeneic mouse model for the GLP testing of dual TCR-engineered cell therapy
Fully immunocompetent HLA-A2/Kb transgenic mice express a chimeric MHC class I complex that includes the human HLA-A2.1 α1 and α2 domains, allowing their cells to present the same epitopes as HLA-A2.1 subjects, and maintain the murine α3 domain, permitting murine CD8 co-receptor engagement (26). To manufacture the T cell products, T cells from HLA-A2/Kb mice were activated, transduced with the RV-NY-ESO-1 TCR vector and expanded ex vivo. For the HSC product, lineage-negative (Lin-) progenitor stem cells were purified from the bone marrow of HLA-A2/Kb mice, pre-stimulated with cytokines and transduced with the LV-NY-ESO-1 TCR/sr39TK vector. Both cell types were co-administered by tail vein injection to myelodepleted HLA-A2/Kb mice that had previously received a lethal dose of total body irradiation (TBI, 900 cGy). We performed twelve pilot studies to establish the best conditions for bone marrow transplantation (BMT) in this model. The main conclusions from these pilot studies were: i) TBI at 900cGy is myelodepleting and lethal without BMT (Supplemental Figure 3A); ii) specific animal care procedures had an important role, in particular having long acclimatization periods in the animal facility before treatment, preventive antibiotic treatment, and supplementary hydration and nutritional gel diet during the post-irradiation recovery; iii) culture of Lin- cells for a short time, 48 hours, was important for HSCs engraftment, progeny persistence and survival (Supplemental Figure 3B); iv) doses from 0.5–2 × 106 short culture (48 hours) Lin- cells showed no differences in engraftment and survival (Supplemental Figure 3C); and v) increasing the retrovirus vector copy number (VCN) in T cells was not toxic (Supplemental Figure 3D).
GLP toxicity study demonstrating that co-administration of TCR-engineered Lin- cells and T cells is safe and does not affect the engraftment and differentiation of progeny cells
The formal GLP-compliant toxicity study design is described in detail in the study protocol (Supplemental Materials section 4). This study included a total of 110 mice divided into five groups (Supplemental Table 5). The number of mice had been prospectively defined by power calculation based on the assumptions made after interpreting the pilot studies (see study protocol in the Supplemental Materials section 4). TCR-transduced Lin- cells and TCR-transduced T cells (cohort E) were co-administered to myelodepleted HLA-A2/Kb mice and compared with control groups of mice receiving mock-transduced Lin- cells and mock-transduced T cells (cohort B), transduced Lin- cells and mock-transduced T cells (cohort C), mock-transduced Lin- cells and transduced T cells (cohort D), or untreated control mice (cohort A). Different cohorts of mice were euthanized at five days or three months after BMT to allow analyses of toxicity without interfering with the overall survival endpoint (Supplemental Table 5). Prior to the study start, we established acceptance criteria for the cell manufacture, and planned to not proceed with any batches of cells that did not meet the criteria. The criteria included cell purity, viability, VCN, mycoplasma, sterility, endotoxin, cell mix homogeneity and stability during administration (Supplemental Table 6).
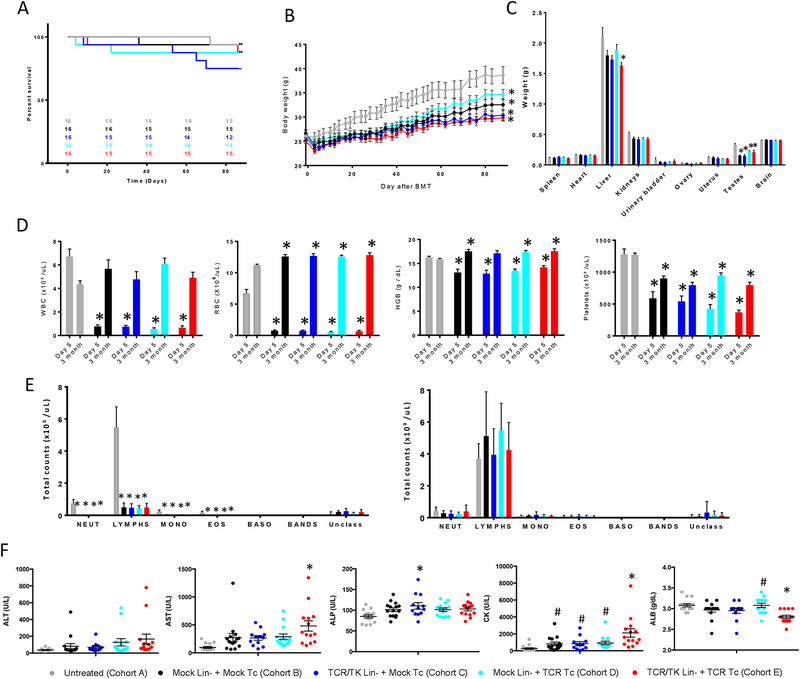
After BMT and T cell administration, mice were followed for three months. No differences in overall survival were observed among cohorts (log-rank test p-value 0.48, Figure 2A). A statistically significant decrease in total body weight was observed in all cohorts receiving TBI and BMT compared to the untreated mice, but it was independent of the expression of the NY-ESO-1 TCR and sr39TK transgenes (Figure 2B, Supplemental Figure 4).
Figure 2. Co-administration of Lin- cells and T cells expressing NY-ESO-1 TCR does not have a negative impact on survival, body and organ weights, blood cell reconstitution and serum chemistry parameters three months after BMT.
TCR engineered Lin- cells and T cells were co-administered to myelodepleted 8- to 12-week-old HLA-A2/Kb mice by intravenous injection. Mice from each cohort were euthanized at day 5 (n=6) or 3 months (n=12–15) after BMT. A. Kaplan-Meier survival curve (Log-rank test p = 0.48). Numbers in the graph indicate survivor count at each time point. B. Total body weight. * p<0.05 vs untreated controls (cohort A), pair-wise comparisons of least-squares means in a linear model framework with Tukey-Kramer adjustment within each time point; considered significant only if 5 or more consecutive measurements were significantly different. C. Organ weights at 3 months after BMT. D. Hematology at day 5 and 3 months after BMT. WBC, White Blood Cells; RBC, Red Blood Cells; HGB, Hemoglobin. E. White Blood Cell differential count at day 5 (left) and 3 months (right) after BMT. Neut, neutrophils; Lymphs, lymphocytes; Mono, monocytes; Eos, eosinophils; Baso, basophils; Bands, Band cells; Unclass, Unclassified cells. F. Serum chemistry at 3 months after BMT. ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase, serum; CK, creatine kinase; ALB, Albumin. Mean ±SEM is plotted. * p<0.05 vs cohort A, # p<0.05 compared to cohort E (receiving transduced Lin- and transduced T cells), pair-wise comparisons of least-squares means in a linear model framework with Tukey-Kramer adjustment within each time point.
Overall, the clinical observations, gross pathology and histopathology from the 10 animals that died or were euthanized before the end of the study did not identify toxicities that could be attributed to a specific treatment leading to increased mortality of a specific cohort. Lack of engraftment together with intestine necrosis was observed in the three mice that died within the first two weeks after BMT: one in cohort C (transduced Lin- cells and mock T cells), one in cohort D (mock Lin- cells and transduced T cells) and one in cohort E (transduced Lin- cells and transduced T cells). Necrotic intestines and cecal torsions associated with irradiation sickness were also observed in two additional mice from cohort C (transduced Lin- cells and mock T cells) that died at day 64 and 69 after BMT. Urethral obstruction and urinary bladder distension were observed in one mouse from cohort C that died at day 52 after BMT (transduced Lin- cells and mock T cells) and one from cohort D that died at day 21 after BMT (mock Lin- cells and transduced T cells). Additionally, one mouse from cohort A (untreated) died at day 71 presenting an atypical enlargement of the heart. No significant findings were identified in one mouse from cohort B (mock Lin- cells and mock T cells) that died at day 35 and one from cohort E (transduced Lin- cells and transduced T cells) that died at day 85. We performed a full necropsy for all of the mice euthanized at the study end, three months after treatment. The necropsy included organ weights (Figure 2C) and histopathology of all protocol-specified collected tissues (Supplemental Table 7). A marked reduction in testes weight was observed in all cohorts receiving TBI, consistent with germ cell ablation identified by histopathology analysis. No other consistent microscopic findings associated with a treatment or with irradiation were identified.
Complete blood cell counts (CBC) at day 5 after BMT showed that mice receiving TBI were lymphodepeleted and presented with statistically significant decreases in red blood cell and platelet counts (Figure 2D and E, Supplemental Figure 4C). TBI caused a sharp reduction in splenocyte and bone marrow cell counts, with a decrease in spleen weight that was recovered three months after BMT (Supplemental Figure 5). At three months after BMT, mice from all cohorts had reconstituted all blood cell compartments. All white blood cell lineages had recovered completely (Figure 2D and E), and red blood cell parameters (RBC, hemoglobin and hematocrit) were slightly increased in irradiated mice while platelets were not completely recovered relative to untreated mice (Figure 2D and Supplemental Figure 4). Serum chemistry analysis at three months after BMT showed a slight decrease in albumin levels in the co-administration group (cohort E). Liver function tests and creatinine kinase activities were highly variable and in general increased in all cohorts receiving BMT (Figure 2 F and Supplemental Figure 6). However, there was no evidence of hepatocyte or muscle damage in tissue sections or the clinical observations. Altogether, these data demonstrate that the co-administration of Lin- cells and T cells expressing an NY-ESO-1 TCR is safe and does not increase toxicity beyond those related to the BMT procedure.
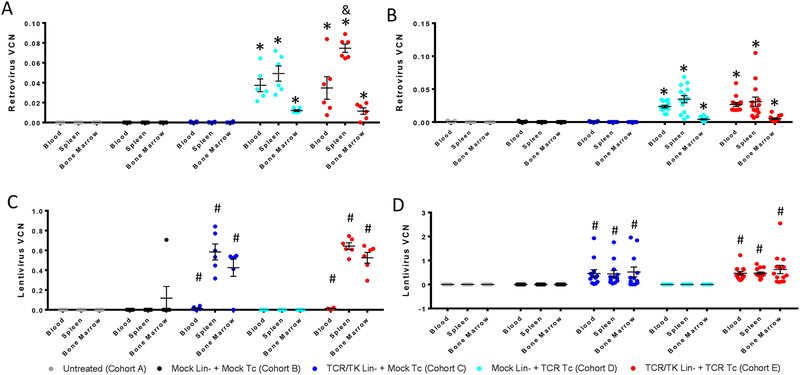
To assess the engraftment and persistence of the T cells and Lin- cells expressing the NY-ESO-1 TCR, we quantified the VCN using droplet digital PCR (ddPCR) with primers specific for the inserted retroviral and lentiviral vectors. We demonstrated the presence of transduced T cells at five days and three months after treatment in blood, spleen and bone marrow cells with no statistical difference between the groups receiving mock transduced Lin- cells or NY-ESO-1/sr39TK-transduced Lin- cells together with the transduced T cells (Figure 3A and B). Similarly, we quantified the engraftment of the transduced Lin- cells and the persistence of their progeny five days and three months after treatment in blood, spleen and bone marrow. No statistically significant differences were identified among the cohorts receiving transduced Lin- cells together with mock-transduced T cells or with NY-ESO-1 TCR-transduced T cells (Figure 3C and D).
Figure 3. Co-administration of Lin- cells and T cells expressing an NY-ESO-1 TCR does not have a negative impact on stem cell and T cell engraftment and progeny persistence.
Retrovirus vector copy number (VCN) in the blood, spleen and bone marrow at 5 days (n=6) (A) and 3 months (n=12–15) (B) after BMT. Lentivirus VCN in the blood, spleen and bone marrow at 5 days (n=6) (C) and 3 months (n=12–15) (D) after BMT. Individual values and mean ±SEM are plotted. * p<0.05 vs cohorts A, B and C; # p<0.05 vs Cohorts A, B and D; & p<0.05 vs Cohorts D; pair-wise comparisons of least-squares means in a linear model framework with Tukey-Kramer adjustment.
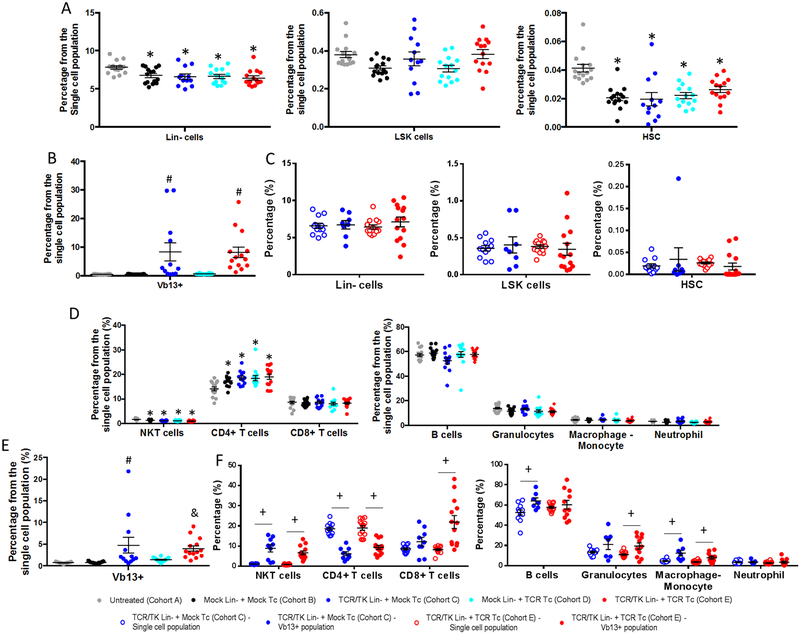
Finally, to study the differentiation of the Lin- cells, we performed an extensive phenotype characterization of the bone marrow cells and splenocytes three months after BMT. In the bone marrow, there were no differences in the frequencies of HSCs and precursor populations, Lin-, LSK (Lin-, ScaI+, cKit+) and HSCs (LSK, CD150+ CD48-), among the cohorts receiving BMT, although the frequency of Lin- and HSCs populations was decreased compared to untreated mice (Figure 4A and Supplemental Figure 7). Intracellular expression of the NY-ESO-1 TCR by clonotypic Vβ13 staining was observed in mice receiving BMT with TCR-transduced Lin- cells independently of the T cells received (Figure 4B and Supplemental Figure 7). Interestingly, there were no differences in the frequencies of the Lin-, LSK and HSCs cells between the total bone marrow and the Vβ13+ population (Figure 4C and Supplemental Figure 7). Similarly, phenotypic characterization in the spleen showed no differences in NKT cells, CD4+ T cells, CD8+ T cells, B cells, granulocytes, neutrophils and monocytes/macrophages among all cohorts receiving BMT, although there was a decrease in the NKT cell population and an increase in the CD4+ T cell population when compared to the untreated mice (Figure 4D and Supplemental Figure 7). Intracellular NY-ESO-1 TCR was expressed in the cohorts receiving transduced Lin- cells independent of the T cells received (Figure 4E and Supplemental Figure 7). The NY-ESO-1 TCR-positive cells displayed an increase in CD8+ T cells, NKT and macrophages and a decrease in CD4+ T cells compared to the total splenocyte population (Figure 4F and Supplemental Figure 7).
Figure 4. The expression of NY-ESO-1 TCR in Lin- cells and their co-administration with T cells expressing an NY-ESO-1 TCR does not have a negative impact on hematopoietic lineage differentiation.
Bone marrow cells and splenocyte phenotype characterization 3 months after BMT. TCR and cell surface markers were assessed by flow cytometry. A. Percentage of Lin- (left panel), LSK (Lin- ScaI+ cKit+, middle panel) and HSC (LSK CD150+ CD48-, right panel) cells in bone marrow. B. Percentage of NY-ESO-1 TCR-expressing cells in the bone marrow, detected by intracellular Vβ13 staining. C. Comparison of the frequency of Lin- (right), LSK (middle) and HSC (left) cells in the total bone marrow population (open circles) and the Vβ13+ population (closed circles). D. Percentages of NKT cells, CD4+ T cells, CD8+ T cells (left panel), B cells, granulocytes, macrophages and neutrophils (right panel) in the total splenocyte population, E. Percentage of NY-ESO-1 TCR-expressing cells in the splenocytes, detected by intracellular Vβ13 staining. F. Comparison of the frequency of NKT cells, CD4+T cells, CD8+ T cells (left panel), B cells, granulocytes, macrophages and neutrophils (right panel) in the total splenocyte population (open circles) and the Vβ13+ population (closed circles). Individual values and mean ±SEM are plotted (n=12–15). * p<0.05 vs cohort A; # p<0.05 vs Cohort A, B and D; & p<0.05 vs Cohort A and B; + p<0.05; pair-wise comparisons of least-squares means in a linear model framework with Tukey-Kramer adjustment.
Lack of immunogenicity due to the expression of NY-ESO-1 TCR and sr39TK by Lin- cells progeny after BMT in myelodepleted mice
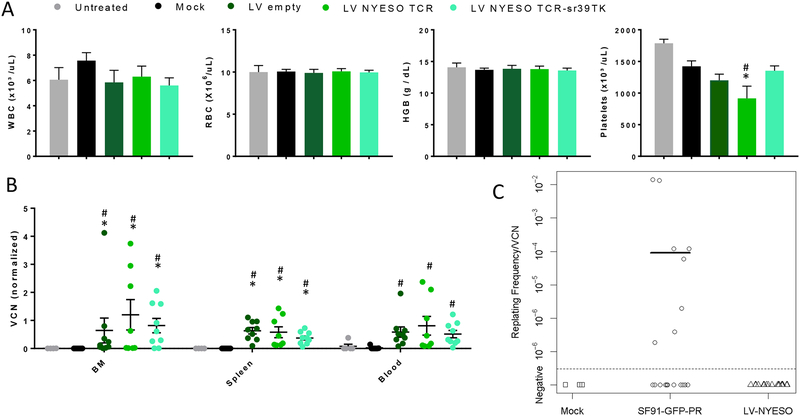
To test if the expression of the NY-ESO-1 TCR and the sr39TK in the hematopoietic cell progeny after BMT in myelodepleted hosts is immunogenic, we performed BMT experiments with Lin- cells transduced with the lentiviral vectors expressing the NY-ESO-1 TCR and the sr39TK, the NY-ESO-1 TCR alone, or an empty vector using the same animal model described above. We demonstrated that after the BMT, engraftment was observed in mice from all cohorts with no difference in survival (Supplemental Figure 8A). The peripheral blood cell populations were reconstituted three months after BMT, and no significant differences were observed among cohorts in the white cell and red blood cell populations (Figure 5A and Supplemental Figure 8B). As seen in the co-administration experiment, at three months the platelets had not completely recovered to the level of untreated control mice (Figure 5A). To test the potential immunogenicity of the transgenes, we assessed the engraftment and persistence of modified Lin- cells progeny by VCN quantification using primers designed within the lentivirus packaging signal to be able to detect the three lentiviruses. If the transgenes were immunogenic, then we would anticipate that cells expressing NY-ESO-1 TCR and sr39TK would not persist long term. As the engraftment and persistence of the transduced stem cell progeny in the bone marrow, spleen and blood were not affected by the expression of the transgenes (Figure 5B), we concluded that expression of the NY-ESO-1 TCR and sr39TK was not immunogenic three months after autologous BMT in this immunocompetent mouse model.
Figure 5. Lack of immunogenicity and genotoxicity of the LV-NY-ESO-1 TCR/sr39TK vector.
Lin- cells transduced with either a LV-NY-ESO-1 TCR/sr39TK, LV-NY-ESO-1 TCR or LV-empty vector were transplanted into myelodepleted HLA-A2/Kb mice. Mice were euthanized at three months after BMT. A. Hematology at 3 months after BMT (n=5–9). WBC, White Blood Cells; RBC, Red Blood Cells; HGB, Hemoglobin. * p<0.05 vs untreated and # p<0.05 vs Mock-transduced. Pair-wise Comparison with Tukey-Kramer. B. Lentivirus VCN in the bone marrow, spleen and blood at three months after BMT. The VCN is normalized with the VCN value of the transplanted cells. Mean ±SEM are plotted (n=6–9). *p<0.05 vs untreated and # p<0.05 vs Mock-transduced. Pair-wise multiple comparison analysis using the Dwass, Steel, Critchlow-Fligner method. C. In vitro immortalization assay. Replating frequency/VCN ratio for mock transduced Lin- cells (n=3), Lin- cells transduced with SF91-eGFP-RRE (n=20) and Lin- cells transduced with the LV-NY-ESO-1 TCR/sr39TK (n=17). Fisher’s exact test (two-sided), p-value = 0.004, and Wilcoxon rank-sum test (two sided), p-value = 0.004, between the SF91-eGFP-RRE transduced group and the LV-NYESO-1 TCR/sr39TK group.
Lack of genotoxicity of the LV-NY-ESO-1 TCR/sr39TK vector in murine Lin- cells
To assess the potential genotoxicity of the lentiviral vector in Lin- cells, we performed an in vitro immortalization (IVIM) experiment (27). Briefly, Lin- stem cells from C57BL/6J mice were purified and either mock-transduced, transduced with the retroviral vector SF91-eGFP-WPRE (28), or transduced with the LV-NY-ESO-1 TCR/sr39TK lentiviral vector. The retrovirus SF91-eGFP-WPRE is known to be oncogenic and to integrate preferentially close to cancer-related genes (27,29,30), thereby serving as a positive control for the IVIM experiment. The Lin- cells were cultured in bulk for two weeks and then seeded in limiting dilution and cultured for an additional two weeks. At the end of the expansion, the replating frequency/VCN ratio was measured. Transformation occurred in eight out of the 20 independent assays performed with the cells transduced with the positive control vector, SF91-eGFP-WPRE. In contrast, no growth was observed in the mock-transduced Lin- cells (n=3) or the Lin- cells transduced with LV-NY-ESO-1 TCR/sr39TK (n=17) (Figure 5C). These data demonstrated lack of genotoxicity of the vector proposed for use in our clinical trial by the IVIM assay.
Human PBSC product manufacturing validation, functionality and stability of the final product
For the chemistry, manufacturing and controls (CMC) section of the IND, we performed five manufacturing validation runs together with their lot release testing. Three of the validation runs were performed using the GMP-compliant clinical-grade vectors. We purchased granulocyte-colony stimulating factor (G-CSF)-mobilized peripheral blood leukapheresis products obtained from healthy human donors and enriched them for CD34+ PBSC using a clinical grade magnetic sorting system. Analysis of five enrichment procedures demonstrated mean CD34+ fraction purity of 96% and viability of 92%. Following enrichment, the cells were stimulated for approximately 18 hours in X-Vivo 15 media supplemented with rhSCF, rhTPO, rhFLT3L and rhIL-3 and transduced with the lentiviral vector encoding NY-ESO-1 TCR and sr39TK for an additional 18 hours. Following the transduction, the PBSC were harvested and cryopreserved; average cell viability was 95%. An aliquot evaluated for bacterial, fungal, and mycoplasmal contamination using both organism-specific cultures and multiple histological stains demonstrated no infections. Endotoxin levels were ≤ 5 EU/Kg of body weight. We assessed the transduction efficiency of PBSC with the LV-NY-ESO-1 TCR/sr39TK vector by VCN with an average of 0.3. The percentage of cells expressing NY-ESO-1 TCR (by Vβ13 staining) was 24%, and the percentage of colony-forming units (CFU) positive for Psi (Ψ) sequence was 33%. These results show the feasibility of the manufacturing procedure and were used to establish the lot release acceptance criteria for the clinical trial batches (See Supplemental Table 8 summarizing the cell product specifications for all of the qualification runs and Supplemental Material Section 5 containing the CMC section of the approved IND).
To study the effect of gene-modification on PBSC functionality, we compared the clonogenic potential of PBSC product to that of freshly isolated peripheral blood CD34+ cells and untransduced CD34+ cells cultured under the same conditions. The clonogenic potential of peripheral blood CD34+ cells was similar between the groups as established by percentage of CFU per total cells plated. The average percentage of CFUs was 39±11%, 48±6% and 51±11% (n=5, p=0.1), respectively, in the unstimulated, untransduced and transduced PBSC final product. Finally, we showed that the transduced and in vitro-cultured stem cells were able to differentiate in vitro in artificial thymic organoids into functional T cells expressing the NY-ESO TCR (Supplemental Figure 9), as previously described by Seet and co-workers (31).
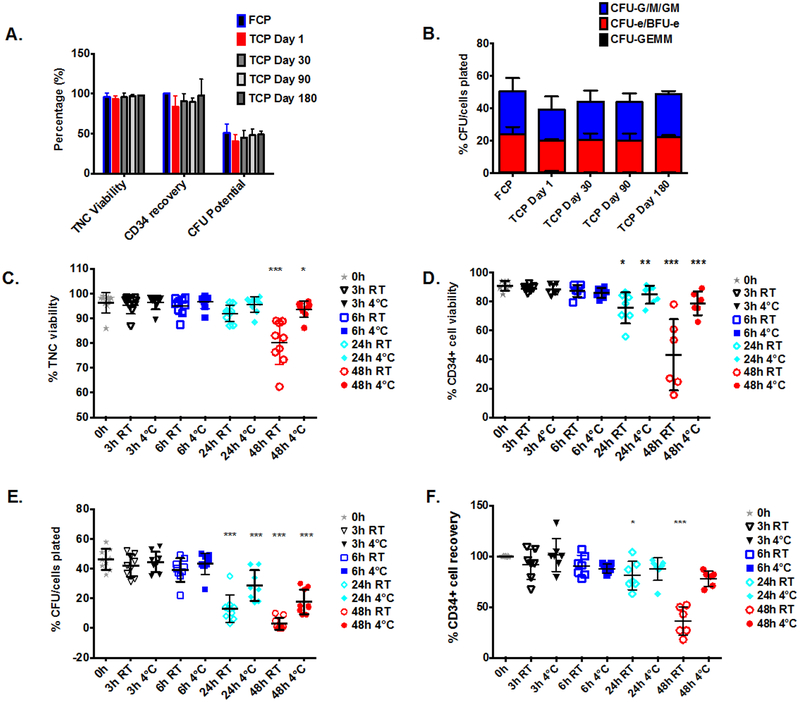
To measure the stability of the TCR-transduced HSCs product, we confirmed that the total cell viability, CD34 recovery and clonogenic potential as well as the CFU subtype distribution were not affected after 1, 3 and 6 months post-cryopreservation (Figures 6A and B). See Supplemental Table 9 and supplemental material section 6 for the detailed description of the stability evaluation for the LV-NYESO TCR/sr39TK PBSC product. In addition, we evaluated the post-thaw stability of the PBSC product after 3, 6, 24 and 48 hours. The cells were split and stored at either ambient room temperature (RT) or 4–8°C. Based on the results of CD34+ cell viability and clonogenic potential, we concluded that the PBSC product should be stable for up to 6 hours post-thawing. Although no significant changes in total cell viability were observed (Figure 6C) the number of viable CD34+ cells in the cell product was significantly decreased in both storage conditions after 24h (Figure 6D). The percent CFU per total cells plated significantly decreased after 24 hours in both storage conditions, from 46% to 13% (RT) and 29% (4–8°C) (Figure 6E). The average recovery of CD34+ cells after 24h in storage at RT decreased to 81%, whereas no significant change in recovered CD34+ cells was observed while stored at 4–8°C (Figure 6F).
Figure 6. PBSC product stability.
An aliquot of cryopreserved PBSC product was recovered at different time points post-cryopreservation: Thawed Cell Product (TCP Day 1, n=2), 30 days (TCP Day 30, n=5), 90 days (TCP Day 90, n=3) and 180 days (TCP Day 180, n=2) after cryopreservation (panels A and B). The stability parameters of the recovered PBSC product stored at RT or 4–8°C were analyzed after 3, 6, 24 and 48h post-thaw and compared to those at 0h, (n=9), (Panels C – F). A. Total nucleated cells (TNC) viability (by trypan blue exclusion), CD34 recovery (by ISCHAGE method) and the percentage of TNCs that grew into hematopoietic colonies when cultured in MethoCult complete medium for 14 days (CFU potential) was assessed at different time points after the cryopreservation. There was no significant difference between the examined time points and fresh cell product (FCP) (p=0.17, p=0.31 and p=0.45 for TNC viability, CD34 recovery and CFU potential, respectively). Data are presented as mean±SD. B. The percentages of CFU-G/M/GM (colony-forming unit-granulocyte/-macrophage/-granulocyte and macrophage), CFU-e/BFU-e (colony-forming unit-erythroid/Burst-forming unit erythroid) and CFU-GEMM (colony-forming unit granulocyte, erythrocyte, monocyte, megakaryocyte) colonies after 14 days culture in MethoCult complete medium. Colonies were scored with the aid of a Zeiss Vert.A1 inverted microscope. Results are expressed as the percentage of CFU subtype per total cells plated. There were no statistically significant differences in the percentage of CFU-G/M/GM (p=0.24), CFU-e/BFU-e (p=0.68) and CFU-GEMM (p=0.52) between different time points and fresh CP. C. Percentage of viable TNC in the PBSC product at 0, 3, 6, 24 and 48h post thaw established by trypan blue exclusion essay. D. Percentage of viable CD34+ at 0, 3, 6, 24 and 48h post-thaw assessed by flow cytometry (ISCHAGE method). E. Percentage of CD34 recovery at the different time points post thawing calculated by dividing “the number of CD34+ cells/ml at 0h” by the “number of CD34+ cells/ml at 3, 6, 24 and 48h time points” and multiplying by 100%. F. Clonogenic potential of the PBSC product 0, 3, 6, 24 and 48h post thaw measured by the percentage of TNCs that grew into hematopoietic colonies. The horizontal bars show averaged values (*p<0.05, **p<0.01 and ***p<0.001 when compared to the 0h time point, by Tukey-Kramer test).
Discussion
The IND-enabling studies presented herein were performed based on the written requirements from FDA reviewers discussed at a pre-IND meeting. The safety concerns regarding the proposed clinical trial were mainly focused on the effect of ex vivo modification of HSCs with lentiviral vectors on genotoxicity and stem cell differentiation and the effect of the co-administration with TCR-transduced T cells. Our studies demonstrate that neither of these concerns were evident in preclinical models. Accordingly, the proposed clinical trial has subsequently been approved by the FDA to proceed to patient accrual.
We have previously shown that human CD34+ cells transduced with the same lentiviral vector and ex vivo-cultured were able to engraft in myelodepleted neonatal NSG HLA-A2.1 mice and differentiate into B cells and functional T cells (17). In these experiments, we have also demonstrated that the modified HSCs and their progeny could be tracked using PET/CT scan and could be completely ablated following ganciclovir treatment (17). We also have demonstrated that human CD34+ cells transduced with the LV-NY-ESO-1 TCR vector were able to differentiate in vitro in artificial thymic organoids to functional T cells with tumor antigen-specific cytotoxicity and near-complete lack of endogenous TCR Vβ expression due to allelic exclusion (31). In the current studies using immunocompentent mouse models, we have established that co-administration of genetically modified Lin- cells and T cells does not affect the engraftment and persistence of T cells and the engraftment, differentiation and progeny persistence of the Lin- cells. Based on these new results, we conclude that the expression of NY-ESO-1 TCR and sr39TK do not alter the differentiation of the Lin- cells or the persistence of their progeny, supporting the lack of immunogenicity of these transgenes after BMT in myelodepleted mice. Overall, these data indicate that co-administration of TCR-engineered T cells and TCR-engineered HSCs represents a viable means of obtaining cells capable of mounting both an immediate and a prolonged tumor-targeted immune response.
A concern regarding the HSCT with lentivirally transduced HSCs is the potential genotoxicity of the vector caused by its integration close to cancer-related genes leading to clonal expansion, a process termed insertional mutagenesis. This concern arises from previous clinical trials using gamma-retroviral vectors that preferentially integrate near oncogenes (LMO2, MDS1-EVI1, PRDM16, SETBP1, CCND2 among others) and deregulate their expression due to the strong viral promoters located in their LTRs; this phenomenon led to the development of leukemia and myelodysplasia in the first gene therapy clinical trials using gene-modified HSCs (32–35). More recently, clinical trials of HSCT with HSCs genetically modified with self-inactivating (SIN) lentiviral vectors have proven the safety of this approach, showing high polyclonality and no expansion of clones with integrations near cancer-related genes previously associated with insertional mutagenesis (36–40). In the current clinical trial, we plan to use a SIN-lentiviral vector with an MSCV promoter derived from the MPSV murine gamma-retrovirus (41) to drive the expression of the transgenes. There is no prior clinical experience with this lentiviral vector. However, clinical trials using SIN-lentiviral vectors with the closely related MND promoter derived from the MPSV murine gamma-retrovirus (42) to drive the expression of the ABCD1 gene have shown safety and lack of clonal expansion of the modified cells (43,44). Interestingly, Biffi et al. compared the integration profile of different lentiviruses in human HSCs engrafted in immunodeficient mice and showed that integration clustered in megabase-wide chromosomal regions of high lentiviral vector integration density demonstrating the bias toward specific genomic regions rather than by oncogenic selection (37). In line with these data, we demonstrated that the transduction of murine Lin- cells with our vector does not lead to transformation in vitro in contrast with the gamma-retroviral vector used as a positive control.
T cells are a self-renewing population, but we and others have previously shown that the their persistence is limited and associated to increased antitumor responses (4,5,8). HSC gene therapy holds great promise for immunotherapy due to the long-term persistence of the modified cells. Similar to the clinical trial proposed in this manuscript, the use of TCR genetically engineered HSCs has been proposed for HIV-1 therapy (45,46) in which feasibility has been shown in preclinical models. In line with this, cancer therapy and HIV-1 therapy approaches using chimeric antigen receptors (CARs) (47–49) and iNKT cell receptors (50) have been proposed in preclinical studies. These studies demonstrate the ability of HSCs to differentiate into functional T cells or invariant natural killer T (iNKT) cells expressing the selected antigen-specific receptor and show antitumor activity or functional antiviral response to limit HIV-1 replication. The co-administration of T cells together with HSCs is key to allow the HSCs to engraft and generate new functional T cells and at the same time provide a therapeutic effect, especially in patients with advanced disease.
Supplementary Material
Translational relevance.
TCR-engineered adoptive T cell transfer has shown a high frequency of transient antitumor responses in several clinical trials but has been followed by a high relapse rate. Persistence and continuous functionality of the engineered T cells are thought to be an important component to achieve long-term responses. We propose a clinical trial to co-administer genetically modified T cells and hematopoietic stem cells (HSCs) expressing an NY-ESO-1 TCR to generate a source for constant renewal of TCR-engineered T cells. The clinical trial proposed here will serve as a proof-of-concept to demonstrate the feasibility and efficacy of gene-modified stem cell therapy to genetically redirect the immune response to cancer.
Acknowledgements
This work was funded by the California Institute for Regenerative Medicine (A.R.), National Cancer Institute grants P01 CA168585 and R35 CA197633 (A.R.), the PhaseOne Foundation (A.R.), the Caltech/UCLA Joint Center for Translational Medicine (David Baltimore, O.N.W., A.R.), the Ressler Family Fund, the Grimaldi Family Fund, the Samuels Family Fund and the Garcia-Corsini Family Fund (A.R.). A.R. and O.N.W. are members of the Parker Institute for Cancer Immunotherapy.
We would like to acknowledge the support of the California Institute for Regenerative Medicine (CIRM), the UCLA Broad Stem Cell Research Center and the CIRM Alpha Stem Cell Clinic at UCLA. The National Gene Vector Biorepository (NGVB, funded by a P40 grant from the NHLBI 9P40HL116242 (K.C.)) provided cells and plasmids available in their repository and archive the test articles and specimens generated in the GLP studies. Flow cytometry was performed in the UCLA Jonsson Comprehensive Cancer Center (JCCC) and Center for AIDS Research Flow Cytometry Core Facility, which is supported by NIH awards CA-16042 and AI-28697, and the JCCC, the UCLA AIDS Institute, and the David Geffen School of Medicine at UCLA. We thank Dr. Stephen T. Smale for his role as Test Facility Management in the GLP study, Dr. Richard C. Koya and Dr. Thinle Chodon for their support in the early stages of the project, all Division of Laboratory Animal Medicine (DLAM) personnel for their support with the animal work and GLP implementation and Justin Tran for his help with the logistics of the project.
The NY-ESO TCR used in this study is covered by patents including US 8,143,376 and is used under license from Adaptimmune Limited. As of 7th September 2017, GlaxoSmithKline plc (LSE:GSK) (NYSE:GSK) has exercised its option under a collaboration and license agreement signed in 2014 to exclusively license the right to research, develop, and commercialize Adaptimmune’s NY-ESO SPEAR T-cell therapy program.
Financial support: CIRM, NIH-NCI, the PhaseOne Foundation, the Caltech/UCLA Joint Center for Translational Medicine, the Ressler Family Fund, the Grimaldi Family Fund, the Samuels Family Fund and the Garcia-Corsini Family Fund.
Footnotes
The authors have no conflict of interests on this work
References
- 1.Morgan RA, Dudley ME, Wunderlich JR, Hughes MS, Yang JC, Sherry RM, et al. Cancer regression in patients after transfer of genetically engineered lymphocytes. Science. 2006;314:126–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson LA, Morgan RA, Dudley ME, Cassard L, Yang JC, Hughes MS, et al. Gene therapy with human and mouse T-cell receptors mediates cancer regression and targets normal tissues expressing cognate antigen. Blood. 2009;114:535–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robbins PF, Morgan RA, Feldman SA, Yang JC, Sherry RM, Dudley ME, et al. Tumor regression in patients with metastatic synovial cell sarcoma and melanoma using genetically engineered lymphocytes reactive with NY-ESO-1. J Clin Oncol. 2011;29:917–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chodon T, Comin-Anduix B, Chmielowski B, Koya RC, Wu Z, Auerbach M, et al. Adoptive transfer of MART-1 T-cell receptor transgenic lymphocytes and dendritic cell vaccination in patients with metastatic melanoma. Clin Cancer Res. 2014;20:2457–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rapoport AP, Stadtmauer EA, Binder-Scholl GK, Goloubeva O, Vogl DT, Lacey SF, et al. NY-ESO-1-specific TCR-engineered T cells mediate sustained antigen-specific antitumor effects in myeloma. Nat Med. 2015;21:914–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robbins PF, Kassim SH, Tran TLN, Crystal JS, Morgan RA, Feldman SA, et al. A pilot trial using lymphocytes genetically engineered with an NY-ESO-1-reactive T cell receptor: Long term follow up and correlates with response. Clin Cancer Res. 2015;21:1019–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu Y-C, Parker LL, Lu T, Zheng Z, Toomey MA, White DE, et al. Treatment of Patients With Metastatic Cancer Using a Major Histocompatibility Complex Class II–Restricted T-Cell Receptor Targeting the Cancer Germline Antigen MAGE-A3. J Clin Oncol. 2017; 35(29):3322–3329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenberg S a Yang JC, Sherry RM Kammula US, Marybeth S, Phan GQ, et al. Durable Complete Responses in Heavily Pretreated Patients with Metastatic Melanoma Using T Cell Transfer Immunotherapy. Clin Cancer Res. 2011;17:4550–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bordignon C, Notarangelo LD, Nobili N, Ferrari G, Casorati G, Panina P, et al. Gene Therapy in Peripheral Blood Lymphocytes and Bone Marrow for ADA-Immunodeficient Patients. Science. 1995;270:470–5. [DOI] [PubMed] [Google Scholar]
- 10.Kohn DB, Weinberg KI, Nolta JA, Heiss LN, Lenarsky C, Crooks GM, et al. Engraftment of gene–modified umbilical cord blood cells in neonates with adenosine deaminase deficiency. Nat Med. 1995;1:1017–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aiuti A, Slavin S, Aker M, Ficara F, Deola S, Mortellaro A, et al. Correction of ADA-SCID by stem cell gene therapy combined with nonmyeloablative conditioning. Science. 2002;296:2410–3. [DOI] [PubMed] [Google Scholar]
- 12.Yang L, Qin X-F, Baltimore D, Van Parijs L. Generation of functional antigen-specific T cells in defined genetic backgrounds by retrovirus-mediated expression of TCR cDNAs in hematopoietic precursor cells. Proc Natl Acad Sci U S A. 2002;99:6204–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang L, Baltimore D. Long-term in vivo provision of antigen-specific T cell immunity by programming hematopoietic stem cells. Proc Natl Acad Sci U S A. 2005;102:4518–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ha SP, Klemen ND, Kinnebrew GH, Brandmaier AG, Marsh J, Hangoc G, et al. Transplantation of mouse HSCs genetically modified to express a CD4-restricted TCR results in long-term immunity that destroys tumors and initiates spontaneous autoimmunity. J Clin Invest. 2010;120:4273–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vatakis DN, Koya RC, Nixon CC, Wei L, Kim SG, Avancena P, et al. Antitumor activity from antigen-specific CD8 T cells generated in vivo from genetically engineered human hematopoietic stem cells. Proc Natl Acad Sci U S A. 2011;108:E1408–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vatakis DN, Arumugam B, Kim SG, Bristol G, Yang O, Zack JA. Introduction of exogenous T-cell receptors into human hematopoietic progenitors results in exclusion of endogenous T-cell receptor expression. Mol Ther. 2013; 21(5):1055–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gschweng EH, McCracken MN, Kaufman ML, Ho M, Hollis RP, Wang X, et al. HSV-sr39TK positron emission tomography and suicide gene elimination of human hematopoietic stem cells and their progeny in humanized mice. Cancer Res. 2014;74:5173–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stärck L, Popp K, Pircher H, Uckert W. Immunotherapy with TCR-Redirected T Cells: Comparison of TCR-Transduced and TCR-Engineered Hematopoietic Stem Cell − Derived T Cells. J Immunol. 2014;192:206–13. [DOI] [PubMed] [Google Scholar]
- 19.Giannoni F, Hardee CL, Wherley J, Gschweng E, Senadheera S, Kaufman ML, et al. Allelic exclusion and peripheral reconstitution by TCR transgenic T cells arising from transduced human hematopoietic stem/progenitor cells. Mol Ther. 2013; 21(5):1044–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nolte A, Buhmann R, Emmerich B, Schendel D, Hallek M. Reconstitution of the cellular immune response after autologous peripheral blood stem cell transplantation in patients with non-Hodgkin’s lymphoma. Br J Haematol. 2000;108:415–23. [DOI] [PubMed] [Google Scholar]
- 21.Rueff J, Medinger M, Heim D, Passweg J, Stern M. Lymphocyte subset recovery and outcome after autologous hematopoietic stem cell transplantation for plasma cell myeloma. Biol Blood Marrow Transplant. 2014;20:896–9. [DOI] [PubMed] [Google Scholar]
- 22.Lai JP, Robbins PF, Raffeld M, Aung PP, Tsokos M, Rosenberg SA, et al. NY-ESO-1 expression in synovial sarcoma and other mesenchymal tumors: Significance for NY-ESO-1-based targeted therapy and differential diagnosis. Mod Pathol. 2012;25:854–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aung PP, Liu Y-C, Ballester LY, Robbins PF, Rosenberg SA, Lee C-CR. Expression of New York esophageal squamous cell carcinoma-1 in primary and metastatic melanoma. Hum Pathol. 2014;45:259–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park TS, Groh EM, Patel K, Kerkar SP, Lee CCR, Rosenberg SA. Expression of MAGE-A and NY-ESO-1 in Primary and Metastatic Cancers. J Immunother. 2016;39:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robbins PF, Li YF, El-Gamil M, Zhao Y, Wargo JA, Zheng Z, et al. Single and Dual Amino Acid Substitutions in TCR CDRs Can Enhance Antigen-Specific T Cell Functions. J Immunol. 2008;180:6116–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vitiello a, Marchesini D, Furze J, Sherman L a, Chesnut RW. Analysis of the HLA-restricted influenza-specific cytotoxic T lymphocyte response in transgenic mice carrying a chimeric human-mouse class I major histocompatibility complex. J Exp Med. 1991;173:1007–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Modlich U, Bohne J, Schmidt M, Von Kalle C, Knöss S, Schambach A, et al. Cell-culture assays reveal the importance of retroviral vector design for insertional genotoxicity. Blood. 2006;108:2545–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schambach A, Mueller D, Galla M, Verstegen MMA, Wagemaker G, Loew R, et al. Overcoming promoter competition in packaging cells improves production of self-inactivating retroviral vectors. Gene Ther. 2006;13:1524–33. [DOI] [PubMed] [Google Scholar]
- 29.Zychlinski D, Schambach A, Modlich U, Maetzig T, Meyer J, Grassman E, et al. Physiological promoters reduce the genotoxic risk of integrating gene vectors. Mol Ther. 2008;16:718–25. [DOI] [PubMed] [Google Scholar]
- 30.Modlich U, Navarro S, Zychlinski D, Maetzig T, Knoess S, Brugman MH, et al. Insertional transformation of hematopoietic cells by self-inactivating lentiviral and gammaretroviral vectors. Mol Ther. 2009;17:1919–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seet CS, He C, Bethune MT, Li S, Chick B, Gschweng EH, et al. Generation of mature T cells from human hematopoietic stem and progenitor cells in artificial thymic organoids. Nat Methods. 2017;14:521–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hacein-Bey-Abina S, Von Kalle C, Schmidt M, McCormack MP, Wulffraat N, Leboulch P, et al. LMO2-Associated Clonal T Cell Proliferation in Two Patients after Gene Therapy for SCID-X1. Science. 2003;302:415–9. [DOI] [PubMed] [Google Scholar]
- 33.Ott MG, Schmidt M, Schwarzwaelder K, Stein S, Siler U, Koehl U, et al. Correction of X-linked chronic granulomatous disease by gene therapy, augmented by insertional activation of MDS1-EVI1, PRDM16 or SETBP1. Nat Med. 2006;12:401–9. [DOI] [PubMed] [Google Scholar]
- 34.Deichmann A, Hacein-bey-abina S, Schmidt M, Garrigue A, Brugman MH, Hu J, et al. Vector integration is non random and clustered and influences the fate of lympropoiesis in SCID-X1 gene therapy. J Clin Invest. 2007;117:2225–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Howe SJ, Mansour MR, Schwarzwaelder K, Bartholomae C, Hubank M, Kempski H, et al. Insertional mutagenesis combined with acquired somatic mutations causes leukemogenesis following gene therapy of SCID-X1 patients. J Clin Invest. 2008;118:3143–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aiuti A, Biasco L, Scaramuzza S, Ferrua F, Cicalese MP, Baricordi C, et al. Lentiviral hematopoietic stem cell gene therapy in patients with wiskott-aldrich syndrome. Science. 2013;341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Biffi A, Montini E, Lorioli L, Cesani M, Fumagalli F, Plati T, et al. Lentiviral Hematopoietic Stem Cell Gene Therapy Benefits Metachromatic Leukodystrophy. Science. 2013;341:1233158–1233158. [DOI] [PubMed] [Google Scholar]
- 38.Hacein-Bey Abina S, Gaspar HB, Blondeau J, Caccavelli L, Charrier S, Buckland K, et al. Outcomes Following Gene Therapy in Patients With Severe Wiskott-Aldrich Syndrome. JAMA. 2015;313:1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Ravin SS, Wu X, Moir S, Anaya-O’Brien S, Kwatemaa N, Littel P, et al. Lentiviral hematopoietic stem cell gene therapy for X-linked severe combined immunodeficiency. Sci Transl Med. 2016;8, 335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ribeil J-A, Hacein-Bey-Abina S, Payen E, Magnani A, Semeraro M, Magrin E, et al. Gene Therapy in a Patient with Sickle Cell Disease. N Engl J Med. 2017;376:848–55. [DOI] [PubMed] [Google Scholar]
- 41.Grez M, Akgun E, Hilberg F, Ostertag W. Embryonic stem cell virus, a recombinant murine retrovirus with expression in embryonic stem cells. Proc Natl Acad Sci U S A. 1990;87:9202–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Challita PM, Skelton D, el-Khoueiry a, Yu XJ, Weinberg K, Kohn DB. Multiple modifications in cis elements of the long terminal repeat of retroviral vectors lead to increased expression and decreased DNA methylation in embryonic carcinoma cells. J Virol. 1995;69:748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cartier N, Hacein-Bey-Abina S, Bartholomae CC, Veres G, Schmidt M, Kutschera I, et al. Hematopoietic stem cell gene therapy with a lentiviral vector in X-linked adrenoleukodystrophy. Science. 2009;326:818–23. [DOI] [PubMed] [Google Scholar]
- 44.Eichler F, Duncan C, Musolino PL, Orchard PJ, De Oliveira S, Thrasher AJ, et al. Hematopoietic Stem-Cell Gene Therapy for Cerebral Adrenoleukodystrophy. N Engl J Med. 2017;NEJMoa1700554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kitchen SG, Bennett M, Galic Z, Kim J, Xu Q, Young A, et al. Engineering antigen-specific T cells from genetically modified human hematopoietic stem cells in immunodeficient mice. PLoS One. 2009;4:e8208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kitchen SG, Levin BR, Bristol G, Rezek V, Kim S, Aguilera-Sandoval C, et al. In vivo suppression of HIV by antigen specific T cells derived from engineered hematopoietic stem cells. PLoS Pathog. 2012;8:e1002649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.De Oliveira SN, Ryan C, Giannoni F, Hardee CL, Tremcinska I, Katebian B, et al. Modification of Hematopoietic Stem/Progenitor Cells with CD19-Specific Chimeric Antigen Receptors as a Novel Approach for Cancer Immunotherapy. Hum Gene Ther. 2013;24:824–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhen A, Kamata M, Rezek V, Rick J, Levin B, Kasparian S, et al. HIV-specific Immunity Derived from Chimeric Antigen Receptor-engineered Stem Cells. Mol Ther. 2015;23:1358–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Larson SM, Truscott LC, Chiou T-T, Patel A, Kao R, Tu A, et al. Pre-clinical development of gene modification of hematopoietic stem cells with chimeric antigen receptors for cancer immunotherapy. Hum Vaccin Immunother. Taylor & Francis; 2017;13:00–00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith DJ, Liu S, Ji S, Li B, McLaughlin J, Cheng D, et al. Genetic engineering of hematopoietic stem cells to generate invariant natural killer T cells. Proc Natl Acad Sci. 2015;112:1523–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.