Abstract
Background & Aims
Functional luminal imaging probe (FLIP) panometry provides a comprehensive evaluation of esophageal functional at the time of endoscopy, including assessment of esophageal distensibility and distension-induced esophageal contractility. However, the few and inconsistent findings from healthy individuals pose challenges to application of FLIP to research and clinical practice. We performed FLIP panometry in asymptomatic volunteers.
Methods
We performed a prospective study of 20 asymptomatic volunteers (ages, 23–44; 14 female) who were evaluated with 16-cm FLIP positioned across the esophagogastric junction (EGJ) and distal esophagus (and in 8 subjects also repositioned at the proximal esophagus) during sedated upper endoscopy. FLIP data were analyzed with a customized MATLAB program that generated FLIP panometry plots and calculated the EGJ-distensibility index (DI) and distensibility plateaus (DP) of distal and proximal esophageal body. Distension-induced esophageal contractility was also assessed.
Results
The median EGJ-DI was 5.8 mm2/mmHg (interquartile range [IQR] 4.9 – 6.7 mm2/mmHg); all 20 subjects had an EGJ-DI > 2.8 mm2/mmHg. The median DP values from all subjects tested were 20.2 (IQR 19.8 – 20.8) mm at the distal body, 21.1 (IQR 20.3 – 22.9) mm at the proximal body, and >18 mm at both locations. Repetitive antegrade contractions (RACs) were observed in all 20 subjects; in 19/20 (95%) subjects, the RAC pattern persisted for ≥10 consecutive, antegrade contractions.
Conclusions
Normal parameters of FLIP panometry are EGJ-DI > 2.8 mm2/mmHg; DP > 18 mm, and antegrade contractions that occur in a repetitive pattern (RACs) – these can be used as normal findings for esophageal distensibility and distension-induced contractility. These values can be used in comparative studies of esophageal diseases, such as achalasia and eosinophilic esophagitis, and will facilitate application of FLIP panometry to clinical practice.
Keywords: manometry, motility, peristalsis, impedance
Introduction
The functional luminal imaging probe (FLIP) utilizes high-resolution impedance planimetry to measure luminal dimensions during controlled, volumetric distension. Distensive pressure is also measured to assess its relationship with luminal dimensions, i.e. distensibility.1 Furthermore, esophageal contractility can be elicited by FLIP distension, evident by occluding and non-occluding contractions along the FLIP probe that can be visualized when diameter changes are depicted as a function of time via FLIP topography.2, 3
When paired with the distensive pressure assessment (FLIP panometry; Figure 1), FLIP provides a comprehensive evaluation involving esophageal distensibility and motility. FLIP has demonstrated its potential as a valuable tool in the evaluation of esophageal function when applied to esophageal diseases associated with abnormalities of esophagogastric junction (EGJ) function (e.g. achalasia) and mechanical properties of the esophageal body (e.g. eosinophilic esophagitis, EoE).1, 4–7 However, inconsistent testing protocols (and thus substantial variability in reported measures) are reported among EGJ distensibiltiy measures and the normative distension-associated contractility experience is based upon a small cohort of 10 subjects.2, 4, 8 Thus, expanding FLIP panometry to clinical research and clinical practice was limited by the lack of reliable normative data.5
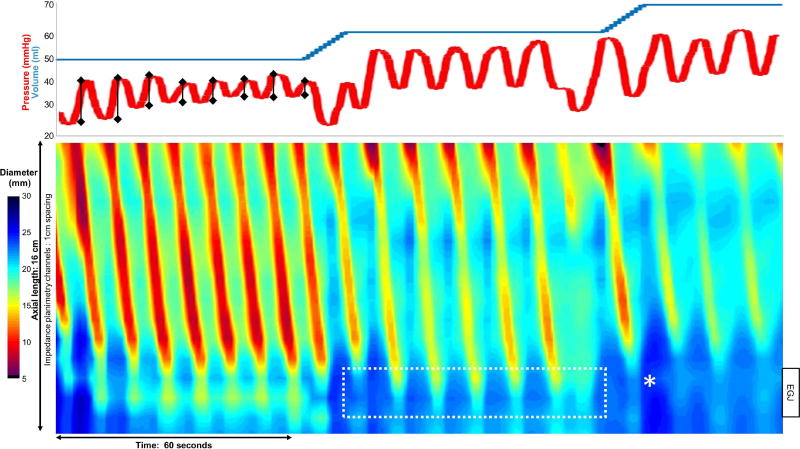
Figure 1. FLIP panometry.
A portion of a FLIP study is displayed with diameter (color-coded) by time FLIP topography plot (bottom) and corresponding intra-balloon pressure (top; red) and distension volume (top, blue). The EGJ-distensibility index (DI) was calculated during the 60-ml fill volume within the EGJ region (dashed white box) and measured 6.7 mm2/mmHg. In this subject, the maximum EGJ diameter (white *) occurred during a contraction at the 70-ml fill volume. The contraction-associated pressure amplitude (vertical black lines) were assessed during the 50ml fill volume. Figure used with permission from the Esophageal Center at Northwestern.
Therefore, the aim of this study was to evaluate distensibility of the EGJ and esophageal body and features of distension-induced contractility among asymptomatic volunteers to generate comprehensive normative values of FLIP panometry. These values will aid refinement of diagnostic criteria and aid future studies involving esophageal disease states.
Methods
Subjects
Healthy, asymptomatic (i.e. free of esophageal symptoms including dysphagia, heartburn, and chest pain), adult volunteers were enrolled. Potential subjects were excluded for previous diagnosis of esophageal, autoimmune, or eating disorders. Additional exclusion criteria included use of antacids or proton pump inhibitors, body mass index (BMI) > 30 kg/m2, or a history of tobacco use or alcohol abuse. The study protocol was approved by the Northwestern University Institutional Review Board. Informed consent was obtained from all subjects. Subjects were paid for their participation.
Study protocol
Evaluation was completed after a minimum 6-hour fast. Subjects underwent upper endoscopy in the left lateral decubitus position. Conscious sedation with 5–10 mg midazolam and 100–200 mcg fentanyl was administered during the procedure.
The 16-cm FLIP (EndoFLIP® EF-322N; Medtronic, Inc, Shoreview, MN) was calibrated to atmospheric pressure prior to trans-oral probe placement.2 With the endoscope withdrawn, the FLIP was positioned within the esophagus such that 1–3 impedance sensors were observed beyond the EGJ with this positioning maintained throughout the FLIP study. Stepwise 5-ml (n = 8) or 10-ml (n = 12) balloon distensions beginning with 20 ml and increasing to target volume of 70 ml were then performed; each stepwise distension volume was maintained for 30–60 seconds. In 8 subjects the proximal esophagus was evaluated by partially withdrawing the FLIP catheter while filled to 30ml until consistent narrowing was observed in the first 1–2 channels, indicative of positioning at the upper esophageal sphincter (UES). 5-ml stepwise distensions from 30 ml increasing to target volume of 50 ml (30-seconds per stepwise volume) were then performed.
High-resolution manometry (HRM) studies consisting of ten 5-ml, liquid swallows in supine position were completed using a solid-state assembly with 36 circumferential pressure sensors at 1-cm intervals and 18 impedance segments at 2-cm intervals (Medtronic, Inc). 24-hour ambulatory impedance-pH studies were performed in 18/20 (90%) subjects with a catheter containing 2 antimony pH electrodes positioned at 5 cm above the EGJ and 10 cm below the EGJ (Sandhill Scientific, Inc, Highlands Ranch, CO).
Data analysis
FLIP data including distension volume, intra-balloon pressure, and 16 channels of luminal diameter were exported to MATLAB (The Math Works, Natick, MA, USA) for analysis using a customized program as previously described.1, 2, 8, 9 The program identified the EGJ-midline by searching for the minimal diameter of the distal impedance planimetry channels. The EGJ-distensibility index (DI) was then calculated by dividing the median EGJ-midline cross-sectional area (CSA) by the median intra-balloon pressure over the duration of the 60-ml distension volume: median CSA/ median pressure = EGJ-DI in mm2/mmHg.1, 8 The maximum EGJ diameter achieved over the entire span of the FLIP study (i.e. 20 – 70 ml fill volumes) was also identified.
A distensibility plateau (DP) of the distal esophageal body was generated from the 8-cm region from 3 to 10 cm above the EGJ midline.9, 10 A distensibility plateau (DP) of the proximal esophageal body was generated similarly, but from a 12-cm region from 2 to 13 cm below the UES midline. The maximal diameters achieved at each impedance planimetry channel during each incremental (5 or 10-ml) distension volume were identified.9 The narrowest of these maximally-achieved diameters for each distension volume were then plotted by the nadir intra-balloon pressure at each distension volume and the esophageal body diameter-pressure relationship was then modeled with a polynomial regression technique to derive the DP.
Esophageal body contractions were identified by a transient decrease of ≥ 5 mm in the luminal diameter in ≥ 3 adjacent impedance planimetry channels. Antegrade contractions were categorized based on a tangent line placed at the onset of contraction. Contractions were further categorized as repetitive if ≥ 3 contractions of similar directionality occurred consecutively at a consistent time interval. Contractions were also categorized as occluding if they achieved a minimal esophageal diameter < 6mm or non-occluding if they did not.2, 3, 8 Finally, the contraction-associated pressure amplitude, i.e. the pressure change from nadir to peak pressures (Figure 1), generated by each contraction during the 60 seconds following the time the FLIP study achieved the 50ml fill volume was quantified. We chose to focus on the 50 ml fill volume as this provided a sufficient fill volume to distend the EGJ (and thus allow contraction-associated pressure transmission to the distally-located pressure sensor) and 60 seconds provided a reasonable, but sufficient, time frame to assess multiple contractions per subject.
Manometry studies were analyzed and esophageal motility diagnoses were determined according to the Chicago Classification v3.0.11 pH-impedance studies were analyzed using dedicated software. The total acid exposure time (AET) was calculated as the percentage of time (after exclusion of meal periods) that the pH was < 4 in the distal esophagus when associated with reflux events detected with impedance.
Statistical analysis
Intra-subject comparisons were made using paired t-test or Wilcoxon Rank Sum test and groups were compared using t-test or Mann-Whitney U tests, depending on data distribution. Bivariate correlation was evaluated with Pearson’s correlation coefficient. Analyses assumed a 5% level of statistical significance.
Results
Subjects
22 asymptomatic volunteers were evaluated, but one was excluded due to a technical limitation and another due to frequent retching during the endoscopy/FLIP that limited interpretation, thus 20 subjects, mean age 30 (range 23 – 44) years, 14 (70%) females, were included. Endoscopic examinations were normal in all 20 subjects. Sedation dosages were an average (range) of 9 (7–10) mg midazolam and 193 (150 – 200) mcg fentanyl.
Distensibility of the EGJ
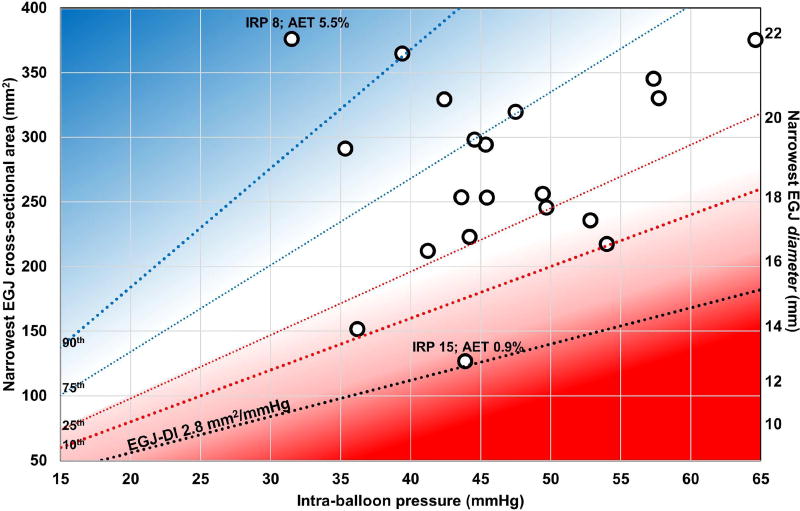
The median (interquartile range, IQR) EGJ-DI was 5.8 (4.9 – 6.7) mm2/mmHg; (Table 1). An EGJ-DI > 2.8 mm2/mmHg was observed in all 20 subjects (100%).1, 3, 6 At the 60-ml fill volume, the median (IQR) for the median narrowest EGJ CSA was 274 (226 – 330) mm2 (which corresponds to diameters of 18.7, 17.0 – 20.5 mm) and the median (IQR) median intra-balloon pressure was 45 (42 – 52) mmHg (Figure 2). The median (IQR; range) maximum intra-balloon pressure achieved was 71 (62 – 86; 54 – 94) mmHg. The median (IQR) maximum EGJ diameter was 24.3 (22.0 – 28.9) mm with associated median (IQR) pressures of 63 (47 – 71) mmHg. In all subjects, the maximum EGJ diameter was achieved during an antegrade contraction, as in Figure 1. A maximum EGJ diameter > 18 mm was achieved in all 20 subjects and ≥ 20 mm in 19/20 (95%) subjects.
Table 1.
Normative values of FLIP panometry.
| Median | 10th –90th percentile |
Threshold | n (%) meeting threshold |
|
|---|---|---|---|---|
| EGJ-DI, 60ml (mm2/mmHg) | 5.8 | 4.0 – 9.2 | > 2.8 | 20 (100) |
| Maximum EGJ diameter (mm) | 24.3 | 20.1 – 30.7 | ≥ 18 | 20 (100) |
| Distensibility plateau, distal body (mm) | 20.2 | 19.4 – 21.4 | ≥ 18 | 20 (100) |
| Distensibility plateau, proximal body (mm) | 21.2 | 19.8 – 24.9* | ≥ 18 | 8 (100) |
| Antegrade contractions | -- | Present | 20 (100) | |
| Repetitive antegrade contraction (RAC) pattern | -- | Present | 20 (100) | |
| Repetitive retrograde contraction (RRC) pattern | -- | Absent | 20 (100) | |
| Antegrade contractions (AC) characteristics | ||||
| Lumen occlusion | -- | -- | At distension volumes 40–60 ml | 14 (70) |
| Contraction-associated pressure amplitude (mmHg)† | 21.2 | 13 – 33 | 10 – 35 | 19 (95) |
| Duration of RAC pattern (number of ACs) | 24 | 12 – 32 | ≥ 10 | 19 (95) |
| RAC pattern cessation | -- | -- | Absent | 17 (85) |
range.
- median value per subject among antegrade contractions occurring during 60-seconds after achieving the 50ml fill volume.
EGJ-DI – esophagogastric junction distensibility index.
Figure 2. Esophagogastric junction (EGJ) distensibility.
Values reflect medians obtained during the 60ml fill volume for each subject. The median integrated relaxation pressure (IRP) in mmHg and 24-hour acid exposure time (AET) for the two subjects at the ranges of EGJ- distensibility index (DI) values are included. Potential for EGJ outlet obstruction is reflected by the intensity of red shading in the lower quartile, particularly below an EGJ-DI of 2.8 mm2/mmHg (black dotted line), while susceptibility to gastroesophageal reflux may be predicted by patients falling in the upper quartile (blue). Figure used with permission from the Esophageal Center at Northwestern.
Distensibility of the esophageal body
The median (IQR) DP of the distal esophageal body was 20.2 (19.8 – 20.8) mm and of the proximal esophageal body (n = 8) was 21.1 (20.3 – 22.9) mm. All 20 subjects had a distal DP > 19 mm and all 8 of those that had proximal esophageal evaluation had a proximal DP > 19 mm. The DP of the distal esophagus did not differ (P = 0.395) between subjects tested with 5 or 10 ml stepwise distension increments.
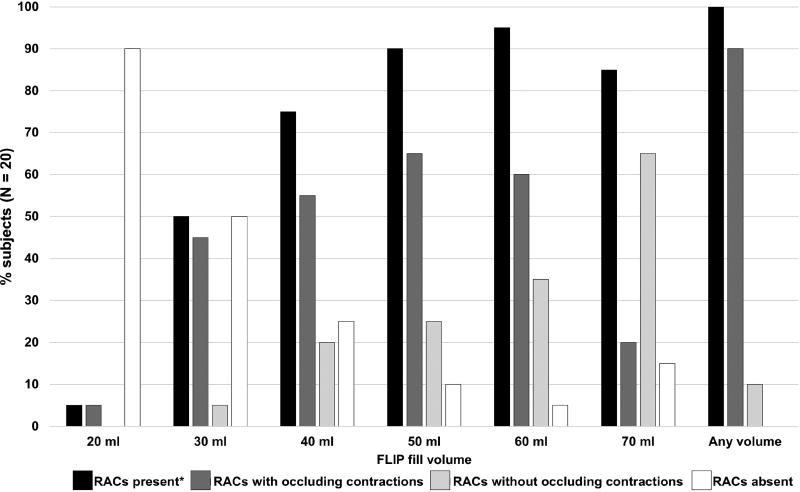
Distension-induced contractility
Antegrade contractions were observed in all 20 subjects. All 20 subjects had at least a single occluding contraction. Every subject had contractions that spanned from the first impedance planimetry channel to the EGJ, thus involving 10–12 cm of continuous axial esophageal length. In all 20 subjects, antegrade contractions occurred in a repetitive pattern, typically with antegrade contractions occurring every 6 – 10 seconds. Thus, repetitive, antegrade contractions (RACs) were observed in all 20 subjects (Figure 3).
Figure 3. Repetitive antegrade contractions (RACs).
The frequencies (%) of RAC presence and occlusion status (i.e. achieving a narrowest diameter < 6 mm) by distension volume are displayed. *Either with occluding or non-occluding contractions.
As RACs were a consistently observed pattern, characteristics associated with the RACs were further qualified and quantified. The presence and occlusion-status of RACs are displayed in Figure 3 and Supplementary Figure. The onset of RACs occurred at a median (IQR) volume 40 (30 – 44) ml and a median (IQR) pressure of 22 (16 – 27) mmHg. After onset, antegrade contractions continued in the RAC pattern through completion of the 70ml fill volume in 17/20 (85%) of subjects. The median (IQR) number of antegrade contractions during a consistent RAC pattern was 24 (18 – 30) contractions spanning a median (IQR) duration of 239 (191 – 258) seconds, recognizing that the duration of the RAC pattern was dependent on the duration of the FLIP study protocol in subjects that did not exhibit RAC cessation (Table 1).
Subjects had a median (IQR) 7 (6 – 8) antegrade contractions that occurred in the 60 seconds after achieving the 50 ml fill volume; thus in total, the contraction-associated pressure amplitudes associated with 127 contractions were assessed among the cohort. Among all 127 antegrade contractions, the median (IQR; 5th–95th percentiles) contraction-associated pressure amplitude was 20.8 (14.5 – 26.2; 9.0 – 40.7) mmHg. When examining the median values within each subject, the median (IQR) median contraction-associated pressure amplitude was 21.2 (15.9 – 29.2) mmHg; Table 1. Subjects with occluding antegrade contractions during the 50-ml fill volume (n = 13) had a greater median contraction-associated pressure amplitude than the subjects that had only non-occluding contractions at the 50-ml fill volume, median (IQRs) 23.3 (20.0 – 31.1) mmHg vs 17.6 (14.9 – 20.4) mmHg; P = 0.019.
High resolution manometry, esophageal acid exposure, and association with FLIP
The median (IQR) integrated relaxation pressure (IRP) was 12.1 (9.0 – 14.3) mmHg; 2 (10%) subjects had a median IRP > 15 mmHg. The median (IQR) basal EGJ pressure (end-expiratory) was 15 (10.3 – 22.3) mmHg. The motility diagnosis based on the 10 supine swallows was normal motility in 17 (85%), ineffective esophageal motility (IEM) in 1 (5%), and EGJ outflow obstruction in 2 (10%). The peristaltic pattern was normal in both subjects with EGJ outflow obstruction.
The 24-hour AET was a median (IQR) 0.65% (0.3 – 1.6). One subject had an AET of 5.5%, while the remaining 17/18 (94%) that completed 24-hr pH-impedance had AETs ≤2.6%.
Observations among the subjects not meeting criteria for normal motility on HRM include the two subjects with EGJ outflow obstruction on HRM (median IRPs of 16 and 18 mmHg) had EDJ-DIs of 4.2 and 5.1 mm2/mmHg, respectively, (Supplementary Figure). The subject with IEM was one of only three subjects from this cohort that did not have an occluding contraction at a distension volume of 40-ml or more. Other descriptive observations associated with outlying values include the subject with the lowest EGJ-DI (2.9 mm2/mmHg) had a median IRP of 15 mmHg, and was thus considered normal motility on HRM while the subject with the highest EGJ-DI (11.9 mm2/mmHg) was the subject with an AET of 5.5% (Figure 2).
Discussion
This study described the esophageal response to volumetric distention in 20 asymptomatic normal subjects and generated normative data focused on EGJ distensibility, esophageal body distensibility and the contractile response to sustained volumetric distention. Focusing on EGJ-DI as the primary metric of EGJ opening function, our results support a previously defined cutoff for normal of 2.8 mm2/mmHg as 100% of our asymptomatic normal subjects exceeded this threshold.1, 3, 6 Similarly, our findings of esophageal body distensibility revealed that the normal values for both the proximal and distal esophagus was greater than 18 mm, which supports previous data suggesting that a DP greater than 17 mm was associated with lower rates of dysphagia and food impaction among patients with EoE.7 Last, we were able to reproduce our previous findings that the RAC pattern was the normal contractile response to sustained volume distention and we described qualitative and quantitative measures to parametrize this physiologic response.2, 3, 8 These findings will provide a useful foundation for further research and describing motor abnormalities in patients with esophageal symptoms.
Previous studies reporting normal values of FLIP primarily included EGJ parameters, but with substantial variability in values reported between studies. This variability was likely related to differences in FLIP study techniques that included different FLIP catheters (6.4, 8, or 16 cm in length), different test settings (awake, endoscopic with conscious sedation, or intra-operative under general anesthesia), and differing pressure references (atmospheric or gastric).4 The largest cohort described included 50 patients without esophageal symptoms that were studied with an 8-cm FLIP catheter while under general anesthesia resulting in a median (IQR) EGJ-DI of 1.2 (0.8 – 2.2) mm2/mmHg at the 40-ml fill volume.12 However, several other studies utilizing the 8-cm FLIP catheter demonstrated an EGJ-DI threshold of of 2.7 – 2.9 mm2/mmHg distinguished achalasia from asymptomatic controls and further, this threshold carried an association with treatment outcomes in achalasia.1, 6, 13 Similarly, our previous studies that included 10 asymptomatic subjects evaluated with the 16-cm FLIP observed 2.8 mm2/mmHg as the lower range of normal.8 Utilization of this threshold detected abnormally low EGJ-DI in 94% (101/108) of patients with an HRM-defined EGJ outflow obstruction (i.e. median IRP > 15 mmHg), including 97% (68/70) of patients with achalasia.3 The present study lends additional support for an EGJ-DI mm2/mmHg threshold of 2.8 mm2/mmHg, being exceeded in all 20 subjects. Further, we also report the maximum EGJ diameter achieved, which may provide complementary information to the EGJ-DI. In total, when pooling data from the current study with the previous 10 subjects studied with 16-cm FLIP via a similar protocol, 30/30 (100%) had an EGJ-DI > 2.8 mm2/mmHg and 28/30 (93%) achieved a maximal EGJ diameter ≥ 18 mm (Supplementary Table).3, 8
Additionally, our earlier work describing esophageal motility with FLIP panometry reported the normal response to sustained esophageal distension from the 10 subject cohort, in which antegrade contractions were observed in all 10 subjects and ≥ 3 consecutive antegrade contractions at a consistent time interval (RACs) were observed in 80%.2, 3, 8 However, the subjects in this initial cohort did not uniformly complete manometry to verify normal esophageal motility. Among the current cohort in which 19/20 (95%) had normal peristaltic function on HRM, all 20 asymptomatic subjects demonstrated a RAC pattern, supporting this observation as the normal response to sustained volumetric distension. Further, repetitive retrograde contractions (RRCs), a pattern associated with type 3 achalasia and spastic motor function among patients with post-fundoplication dysphagia, was not observed among this cohort during this testing protocol, nor the historic cohort of controls, thus lending further support that RRCs representing an abnormal motility finding.3, 8, 14 While the overall homogeneity within this normative cohort limits comparisons within this cohort beyond several descriptive observations of outlying features, we again support an association of esophageal motility findings with FLIP panometry performed during conscious sedation and HRM.3 In fact, our a-priori concept of normal esophageal motility on FLIP (i.e. EGJ-DI > 2.8 mm2/mmHg with RACs) was observed in all 20 subjects; a classification of “normal motility” on HRM was observed in 17/20 (85%).11
The current study provides expanded observations of characteristics associated with the normal contractile response to sustained esophageal distension. Here, we observed that the RAC pattern most commonly occurred at the 40-ml, 50-ml, and/or 60-ml fill volume, usually with occluding contractions. Further, the RAC pattern typically persisted for >10 consecutive contractions, often persisted through the remaining duration of the testing protocol, as opposed to spontaneously fatiguing. Further, we quantified the pressure-amplitudes generated by antegrade contractions, which may provide supplementary functional information regarding the effectiveness of contractions: this contraction-associated pressure amplitude reflects the vigor of the antegrade contraction, as well as the patency of the EGJ. Thus, while presence of the RAC pattern has carried an association with normal motility on HRM and esophageal acid exposure, the ‘normal’ contractile response appears to be more robust than solely the presence of three or more consecutive antegrade contractions.2, 3, 15 Therefore, application of added characteristics to quantify vigor of the contractile response to esophageal distension facilitate identification of weak or hyper-contractile responses when falling outside of normal limits (Table 1). While specific thresholds will be refined by future studies evaluating esophageal disease states, a weak contractile response may be considered with reduced duration or cessation of the RAC pattern or inability for antegrade contractions to occlude the lumen at fill volumes ≥40 ml. On the flip side, a hypercontractile response may be suggested by occluding contractions at the 70ml fill volume or contraction-associated pressures amplitudes > 35 mmHg.
Additionally, we report distensibility assessment of the distal esophageal body and EGJ and also an expanded FLIP technique to evaluate the proximal esophageal body. Using the EGJ and UES as anatomic landmarks provides confirmation of appropriate positioning throughout the FLIP study while evaluating the majority of the esophageal body; the possibility remains for overlap or a short segment missed in the mid-esophagus. Thus, this technique can facilitate evaluation for stenosis along the length of the esophagus among patients with EoE. Further, as we did not observe a difference in distal esophageal body distensibily measures between subjects using 5 or 10 ml incremental volumes, omission of the 5-ml incremental fill volumes would improve efficiency of the FLIP study, without apparent sacrifice in functional information. Evaluation in an EoE cohort will help substantiate this claim.
While the normative results from this study will yield improved comparisons for future studies with esophageal disease states, there are several limitations worth considering. Effects on esophageal motility associated with opiates and benzodiazepines have been reported, thus concerns have been voiced about the potential effects of sedating agents on the esophageal motility impression when assessed at the time of sedated endoscopy.3, 14, 16 By evaluating this asymptomatic cohort with FLIP panometry during conscious sedation, our data supports that our FLIP findings are associated with normal manometry and will serve as a reliable reference for patients studied under similar conditions. Although we have not observed significant differences in FLIP parameters among clinical FLIP studies performed using propofol, further study remains needed to clarify the potential effects of sedating agents.3, 14 Generalizability of our results may be limited by the sample size (although the consistency of results within this cohort was reassuring), as well as by relatively young age and low BMI of our cohort. Generalizability of our FLIP panometry analysis techniques with the reliance on customized MATLAB software may also pose a limitation. However, broader application may be facilitated by recent commercial availability of the real-time FLIP topography display (Medtronic, Inc), particularly through its depiction of the contractile-response to distension. Application to clinical practice will hopefully be further improved by incorporation of our paradigms into analysis software associated with this evolving technology.
In conclusion, we evaluated 20 asymptomatic volunteers with FLIP panometry during upper endoscopy and provide further support that normal EGJ distensibilty can be defined by an EGJ-DI > 2.8 mm2/mmHg and a maximum EGJ diameter of > 18 mm, normal esophageal body distensibility can be defined by DPs of > 18 mm at the distal and proximal esophageal body, and that RACs represent the normal contractile response to sustained, esophageal distension. Although future studies evaluating esophageal disease states remains needed to further validate the clinical utility of esophageal distensibility and distension-induced motility evaluation, these values enhance the normative reference to aid application of FLIP panometry in scientific and clinical evaluation of esophageal disease.
Supplementary Material
What you need to know.
Background
The functional luminal imaging probe (FLIP) provides a promising esophageal evaluation including esophageal distensibility and contractile response to distension, though its application to research and clinical practice was limited by a lack of consistent, normative data.
Findings
All 20 asymptomatic subjects had an esophagogastric junction distensibility index > 2.8 mm2/mmHg, maximum EGJ diameter > 18mm, distal esophageal body distensibility plateau > 18mm, and exhibited a pattern of repetitive antegrade contractions in response to distension.
Implications for patient care
FLIP parameters falling outside these normative ranges supports identification of functional abnormalities in the esophageal response to distention in patients evaluated with a similar FLIP technique.
Acknowledgments
Grant support: This work was supported by R01 DK079902 (JEP) from the Public Health service and Scleroderma Research Foundation grants (MH).
Dustin A. Carlson, Zhiyue Lin, Peter J. Kahrilas, and John E. Pandolfino hold shared intellectual property rights and ownership surrounding FLIP panometry systems, methods, and apparatus with Medtronic Inc.
John E. Pandolfino: Crospon, Inc (stock options), Given Imaging (Consultant, Grant, Speaking), Sandhill Scientific (Consulting, Speaking), Takeda (Speaking), Astra Zeneca (Speaking), Medtronic (Speaking. Consulting), Torax (Speaking, Consulting), Ironwood (Consulting), Impleo (Grant).
Abbreviations
- AET
acid exposure time
- BMI
body mass index
- CSA
cross-sectional area
- DI
distensibility index
- DP
distensibility plateau
- EoE
eosinophilic esophagitis
- EGJ
esophagogastric junction
- FLIP
functional lumen imaging probe
- HRM
High-resolution manometry
- IRP
integrated relaxation pressure
- IQR
interquartile range
- RACs
Repetitive antegrade contractions
- RRCs
repetitive retrograde contractions
- UES
upper esophageal sphincter
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest:
Wenjun Kou, Monique Hinchcliff, Sophia Falmagne, Jacqueline Prescott1, Emily Dorian: None.
Author contributions: DAC contributed to study concept and design, data analysis, data interpretation, drafting of the manuscript, and approval of the final version. WK and ZL contributed to data analysis and approved the final version. MH contributed to study concept, obtaining funding, and approval of the final version. AT contributed to recruitment of subjects, data acquisition, and approval of the final version. SF, JP, and ED contributed to data analysis and approval of the final version PJK contributed to editing the manuscript critically and approval of the final version. JEP contributed to study concept, obtaining funding, and approval of the final version.
References
- 1.Pandolfino JE, de Ruigh A, Nicodeme F, et al. Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil. 2013;25(6):496–501. doi: 10.1111/nmo.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carlson DA, Lin Z, Rogers MC, et al. Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil. 2015;27(7):981–9. doi: 10.1111/nmo.12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlson DA, Kahrilas PJ, Lin Z, et al. Evaluation of Esophageal Motility Utilizing the Functional Lumen Imaging Probe. Am J Gastroenterol. 2016;111(12):1726–35. doi: 10.1038/ajg.2016.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carlson DA. Functional lumen imaging probe: The FLIP side of esophageal disease. Curr Opin Gastroenterol. 2016;32(4):310–8. doi: 10.1097/MOG.0000000000000272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirano I, Pandolfino JE, Boeckxstaens GE. Functional Lumen Imaging Probe for the Management of Esophageal Disorders: Expert Review From the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15(3):325–34. doi: 10.1016/j.cgh.2016.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rohof WO, Hirsch DP, Kessing BF, et al. Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology. 2012;143(2):328–35. doi: 10.1053/j.gastro.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 7.Nicodeme F, Hirano I, Chen J, et al. Esophageal distensibility as a measure of disease severity in patients with eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2013;11(9):1101–7. e1. doi: 10.1016/j.cgh.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carlson DA, Lin Z, Kahrilas PJ, et al. The Functional Lumen Imaging Probe Detects Esophageal Contractility Not Observed With Manometry in Patients With Achalasia. Gastroenterology. 2015;149(7):1742–51. doi: 10.1053/j.gastro.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlson DA, Lin Z, Hirano I, et al. Evaluation of esophageal distensibility in eosinophilic esophagitis: an update and comparison of functional lumen imaging probe analytic methods. Neurogastroenterol Motil. 2016;28(12):1844–53. doi: 10.1111/nmo.12888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwiatek MA, Hirano I, Kahrilas PJ, et al. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology. 2011;140(1):82–90. doi: 10.1053/j.gastro.2010.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74. doi: 10.1111/nmo.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nathanson LK, Brunott N, Cavallucci D. Adult esophagogastric junction distensibility during general anesthesia assessed with an endoscopic functional luminal imaging probe (EndoFLIP(R)) Surg Endosc. 2012;26(4):1051–5. doi: 10.1007/s00464-011-1996-3. [DOI] [PubMed] [Google Scholar]
- 13.Smeets FG, Masclee AA, Keszthelyi D, et al. Esophagogastric junction distensibility in the management of achalasia patients: relation to treatment outcome. Neurogastroenterol Motil. 2015;27(10):1495–503. doi: 10.1111/nmo.12651. [DOI] [PubMed] [Google Scholar]
- 14.Carlson DA, Kahrilas PJ, Ritter K, et al. Mechanisms of repetitive retrograde contractions in response to sustained esophageal distension: a study evaluating patients with postfundoplication dysphagia. Am J Physiol Gastrointest Liver Physiol. 2018;314(3):G334–G40. doi: 10.1152/ajpgi.00368.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carlson DA, Kathpalia P, Craft J, et al. The relationship between esophageal acid exposure and the esophageal response to volumetric distention. Neurogastroenterol Motil. 2017 doi: 10.1111/nmo.13240. epub Nov 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ratuapli SK, Crowell MD, DiBaise JK, et al. Opioid-Induced Esophageal Dysfunction (OIED) in Patients on Chronic Opioids. Am J Gastroenterol. 2015;110(7):979–84. doi: 10.1038/ajg.2015.154. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.