Abstract
Approximately 1.8 million young adults aged 18 to 25 had a Cannabis Use Disorder (CUD) in the past year. Unfortunately, engaging young adults in treatment is very challenging. Creative approaches to treat cannabis disorders such as integrating mobile technology with evidence-based treatments are warranted. In light of these challenges, we developed a text message-delivered version of Peer Network Counseling (PNC-txt), which is a substance use intervention that focuses on peer relations. PNC-txt engages participants in 16 automated, personalized text interactions over 4 weeks. We conducted a randomized controlled trial to test the efficacy of PNC-txt against a waitlist control group with 30 treatment seeking young adults (ages 18–25) who met DSM-5 criteria for CUD. Self-report and urine analyses were used to test outcomes at the three-month follow-up. The PNC-txt group significantly reduced their cannabis use related problems as well as cannabis cravings, compared to the control group. PNC-txt participants also had a significantly greater percentage with urines negative for cannabis metabolites compared to controls. Moderation analysis showed that CUD severity level moderated treatment, suggesting that PNC-txt is more effective for participants with medium and high levels of CUD severity. All effect sizes ranged from medium to large. Results from this pilot trial are promising and warrant further research on PNC-txt for addressing cannabis use disorder.
Keywords: Cannabis Use Disorder, Young Adults, Text messages, Peer Network Counseling
1. Introduction
Young adulthood is a particularly critical developmental period with rates of substance use more than doubling between early adolescence and young adulthood (Johnson et al., 2018). Recent data from the Monitoring the Future (MTF) survey indicate that more than a third (35.3%) of young adults ages 19 to 28 report cannabis use in the past year - the highest levels recorded in three decades (Schulenberg et al., 2017). Even more concerning, approximately one in thirteen young adults (7.6%) are now daily cannabis users (using 20 or more times per month) - the highest levels ever recorded since the inception of MTF (Schulenberg et al., 2017). Over 5% or approximately 1.8 million young adults aged 18 to 25, had a Cannabis Use Disorder (CUD) in the past year (SAMHSA, 2016). Unfortunately, young adults rarely seek help or recognize a need for substance use treatment (Caldeira et al., 2009). Among college students cannabis use is associated with poorer academic performance (Arria, Caldeira, Bugbee, Vincent, & O’Grady, 2015; Suerken et al., 2016) and discontinuous enrollment/drop-out (Arria et al., 2013). Cannabis use has been associated with both traffic and non-traffic injuries (Barrio et al., 2012; Li et al., 2012). Frequent and sustained cannabis use has also been prospectively associated with functional impairment due to injury, illness, and emotional problems, lower health-related quality of life, and greater psychiatric symptoms (Caldeira, O’Grady, Vincent, & Arria, 2012).
Cannabis use varies by current educational status for young adults. Past 30-day cannabis use among young adults who are enrolled fulltime in college and their non-college enrolled peers in 2016 was 22% and 30% respectively. Non-college enrolled young adults are using cannabis daily at a rate more than twice (12.8%) that of their college-enrolled peers (4.9%) (Schulenberg et al., 2017). Both of these young adult populations should be studied as both have unique challenges and perceived barriers to treatment engagement (SAMHSA, 2015).
1.1. Barriers to Treating Cannabis Use Disorders in Young Adults
Effectively addressing Cannabis Use Disorders is challenging. The cost of treatment, difficulty in accessing treatment facilities, and stigma associated with seeking help, prevent many young adults from engaging in treatment (Perron et al., 2009). Stigmatization by peers may prevent treatment engagement for young adults, as they are particularly sensitive to peer perceptions surrounding this issue. In a national study, 37% of college students feared social stigma attached to substance abuse, which kept them from seeking help; only 6% of students who met criteria for alcohol or drug disorder sought help (CASA, 2007). Finally, dependent upon the cannabis use culture where young adults finds themselves, acknowledging that their use of cannabis has contributed to significant social, educational or career, and emotional problems is often difficult, and many do not recognize a need for treatment (Calderia et al., 2009). This type of self-awareness is a critical step towards seeking treatment and is often accompanied with a sustained pattern of negative events such as a disturbed social relations or doing poorly in school or work. This critical decision point is common among those who struggle with substances of abuse, where the individual has to see enough down-side of their behavior to instigate treatment seeking. Thus, intervention modalities that can deliver treatments while minimizing the associated barriers are vital to engaging more young adults in substance use treatment. Technology-based programs have been identified as a useful tool in engaging young adults, particularly those not enrolled in college who may be difficult to find (SAMHSA, 2015).
1.2. Integrating Text Messages into CUD Treatment
Compared to other age groups, young adults ages 18 to 24 are the most active in their use of text messaging, sending and receiving 128 texts per day and 3,853 per month (Burke, 2016). A small but growing literature has integrated text-based interventions into substance use treatment. Most of these studies have targeted tobacco and alcohol use. The content, frequency and duration of these interventions has been wide ranging, and many studies have not reported sufficient detail to fully understand or replicate findings. In a meta-analysis of text-delivered alcohol and tobacco programs for adolescents and young adults, interventions ranged from a single text message reflecting the amount of money spent on alcohol to more complicated designs based on cognitive behavioral theory and motivation frameworks with texts sent over several weeks to many months (Mason, Ola, Zaharakis, & Zhang, 2015a).Yet, the limited evidence available so far is promising. For example, Gonzales and colleagues (2016) found that young adults in treatment for a drug use disorder who were randomized to a mobile texting aftercare intervention fared better than the usual-care control group. To date, we are aware of only one study that has tested a text message- based intervention specifically for cannabis use among young adults (Shrier, Rhoads, Burke, Walls, & Blood, 2014); however, this intervention was not tested as a free-standing intervention but rather as a supplement to two in-person counseling sessions. The intervention used a motivational interviewing approach and was tailored using baseline assessments. For two weeks post- counseling sessions, participants were sent supportive texts if they reported use, desire to use, or being in the presence of a trigger during randomly sent ecological momentary assessments (Shrier et al., 2014). Participants also received a text message after completing daily diary surveys.
Text-based interventions can circumvent several barriers to treatment, including stigma, cost, and access, and there is evidence that they are an acceptable mode of treatment among young adults (e.g., Gonzales et al., 2016). While research on text-message interventions is still in the early stages, results thus far provide initial evidence of effect sizes, most often within the small range (Mason et al., 2015a). However, given the ability of text message interventions to circumvent treatment barriers and reach large populations more easily than traditional in-person interventions, smaller effect sizes may still be useful in impacting treatment outcomes with greater numbers of patients. Advances in technology now allow for the easy personalization of text messages, thereby offering the opportunity to provide tailored text-based interventions. Given these results and the limited number of rigorous trials in the extant literature, developing text-based interventions for CUD appears to be justified.
1.3. Peer Context as Target in Young Adult Treatment
Extensive research has shown that peer context is a very robust predictor of cannabis use (Pollard, Tucker, de la Haye, Green, & Kennedy, 2014). For example, a recent study demonstrated that when actual friends’ cannabis use increased, personal cannabis increased (Deutsch, Chernyavskiy, Steinley, & Slutske, 2015). In contrast, research has found that peer prosocial behaviors stimulate or activate internal motivation of index participants as well as through “conformity training” where peers approve of each other’s prosocial behaviors and disapprove of antisocial behaviors (Exner-Cortens, 2014; Mrug & McCray, 2013). Peers provide an important route for exposure to cannabis, with almost 80% of 18 to 22 year olds reporting that they have at least one friend who uses cannabis (Schulenberg et al., 2017). Addressing the peer context as a clinical target for reducing cannabis use among young adults has a scientific premise.
1.3.1. Peer Network Counseling Rationale and Structure
Given the above review, interventions that target the importance of peer context with young adults and utilize text messaging would be a promising approach for substance use disorder treatment. One such intervention is Peer Network Counseling (PNC). PNC is a brief (20 minutes) substance use in-person intervention that uniquely focuses on peer relations as the primary mechanism for behavioral change. PNC has been tested in five clinical trials with over 400 adolescents and young adults (Mason, Pate, Drapkin, & Sozinho, 2011; Mason, Benotsch, Way, Kim, & Snipes, 2014; Mason et al., 2015b; Mason, et al., 2016). PNC is a peer-focused substance use intervention that applies Motivational Interviewing (MI) (Miller & Rollnick, 2013) principles, but uses a relational framework in addressing risk behaviors, focusing on the interpersonal and environmental interactions that the participant encounters. PNC introduces the construct “peer network health” (a summative index of participants’ peers’ pro-social and risk-enhancing behaviors) to participants in order to activate reflection on peers and places to meet their personal goals regarding substance use. Table 1 provides a summary of PNC component parts, duration, and approach.
Table 1.
Peer Network Counseling Parts, Approach, and Components.
| Part | Time | Approach & MI spirit | Intervention Components |
|---|---|---|---|
| 1 | 4 days | Rapport building MI engagement |
Participants describe their experience with cannabis use Participants discuss likes and dislikes about cannabis use |
| 2 | 4 days | Presenting feedback MI acceptance |
Participants’ cannabis use is compared to national norms Participants reflect on their goals in light of current use |
| 3 | 4 days | Presenting information & feedback MI acceptance |
Peer network health risk & protection is reviewed Participants are asked to reflect on their peer network |
| 4 | 4 days | Summarize & encourage change talk MI encouragement |
Session is summarized, change talk & action plan encouraged Participants reflect on making adjustments to peer network & behaviors |
Prior to the PNC intervention, participants complete an assessment of their cannabis use and close peers’ risk and protective behaviors, as well as values and plans related to cannabis use. These data are then used to provide personalized feedback during the in-person intervention session. PNC is structured into four component parts: (a) rapport building and presentation of cannabis use feedback, (b) discussion of cannabis use likes/dislikes, goals, and discrepancies, (c) introduction of peer relations information and feedback, and (d) change talk and action plans. Participants are provided the opportunity to critically examine the composition of their close peer networks as well as temporal and place-based considerations (e.g., amount of time spent at particular locations).
1.3.2. Adapting PNC into PNC-txt
We initially began PNC-Text Message Version (PNC-txt) using a dosage of 30 texts delivered over five days and had promising results in increasing readiness to change problematic alcohol use with young adults (Mason, et al., 2014) and in reducing tobacco use with adolescents (Mason et al., 2016). However, our meta-analysis on text-based interventions revealed a dose response between outcomes and the number of texts and the length of interventions (r=0.69, p<0.01; Mason et al., 2015b). The first author systematically examined each of the four parts of PNC and translated the hypothesized active ingredients into four weeks of text messages. Each week of PNC-txt corresponds to each component part of PNC. PNC-txt delivers 112 texts over 4 weeks, allowing enough time to cover PNC components in detail, but not burdening participants. The total estimated time to complete PNC-txt is approximately 20 minutes. This dosage is in-line with typical text interventions (Mason et al., 2015b). See Table 2 for examples of the PNC-txt intervention.
Table 2.
Examples of PNC-txt.
| Text Number | Text Message |
|---|---|
| Text 1 | Hi SUBJECT NAME, Before we start, how would you rate your craving for SMK right now (0=none-10=intense) Txt back: 0–10 |
| Text 2 | Thx NAME. We appreciate your honesty. One more before we start, have you used SMK in the past 24 hours? Txt back; yes or no |
| Text 3 | Thx NAME. Let’s talk about your peer network. Based on your survey your network seems Kind of Unhealthy. What do you think of this? Txt back: surprise, seems right, concerned |
| Text 4 | Thx, we appreciate it. Let’s focus on Peer Nick-Name, who seems Pretty healthy. You both hang out at the Gym, you get Lots of Support & Some Encouragement. Txt: yes/no |
| Text 5 | Thanks NAME. Some people spend more time with certain friends at certain places to make changes. Do you think you might try this? Text: yes, unsure, no |
| Text 6 | Most of us have not looked at our friends this way. Its odd cause we can have mixed feelings about SMKing & friends. You’re doing great on this stuff! Text: ok |
| Text 7 | Thx a lot NAME. Small changes like who you hang with and where really helps. That ends today’s texts. Need more support? Txt: BOOST. This is not being read immediately, if this is a crisis call 911 |
Note. a) Bolded text indicates where responses are automatically populated based on participants’ baseline data via the TextIt program.
b) If any response is NO, we send this message: OK, this is what we have from your survey. What is the correct answer? Txt answer. We then use that answer and continue the program.
In our review of the literature, we found no studies to date that have explicitly tested text- delivered treatment for CUD. Therefore, the purpose of the present pilot study is to test the efficacy of text-message delivered Peer Network Counseling (PNC-txt) with young adults meeting DSM-5 criteria for Cannabis Use Disorder. We hypothesized that young adults in the PNC-txt condition would exhibit reduced cannabis use, cannabis problems, and cannabis craving. We also hypothesized that CUD severity would moderate the association between treatment condition and cannabis use and cannabis problems. We hypothesized that the PNC-txt group would produce more urines negative for cannabis metabolites compared to the wait-list control group. Finally, we hypothesized that the PNC-txt group would reduce peer risk and increase peer protection based on the Peer Network Health measure.
2. Methods
2.1. Recruitment.
All procedures were approved by the Virginia Commonwealth University (VCU) Institutional Review Board and a Certificate of Confidentiality was obtained from the National Institutes of Health. Participants were treatment-seeking cannabis users ages 18 to 25 who met criteria for a diagnosis of CUD. Participants were recruited by flyers, Craiglist postings, and informational notices posted on media display boards around the VCU campus and VCU Medical Center. Recruitment proceeded between March and May 2016. All data collection was completed by September 2016.
The current study is a secondary analysis of a parent study which examined the feasibility and efficacy of PNC with 45 young adults. The parent study was a three-arm trial: PNC-in-person, PNC-txt, and waitlist control and was not published. Both PNC versions reduced cannabis use, but there was no significant condition X time effect. Because of this null finding and our interest in m-health interventions, we selected 30 cases to analyze the efficacy of PNC-txt compared to controls. There were no significant demographic differences between the full sample (n=45) and the subgroup sample (n=30). The subgroup was 60%White, 27% Black, and 13% Other, Mage = 20.8 years, age range: 18–25. The sample was split evenly between male and female. The majority (66.7%) of participants were enrolled in college.
2.2. Procedures.
Prior to enrollment into the trial, participants were screened for eligibility. Inclusion criteria were: 18 to 25 years old, presence of a CUD (Cannabis Use Disorder Identification Test - Revised [CUDIT-R], Adamson et al., 2010, and Cannabis Use Disorder Diagnostic Interview ([CUDDI], Mason & Zaharakis, 2016); absence of an AUD (Alcohol Use Disorder Identification Test [AUDIT]; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001), and urine drug screen positive for the cannabis metabolite. Exclusion criteria were: substance use treatment within past 90 days, not having a smart phone, unwilling to commit to a three month study, not fluent in English, unable to consent. Trained research staff conducted telephone and in person screening. Verbal consent was obtained prior to completing the CUDIT and AUDIT by phone, and signed consent was obtained prior to completing the CUDDI and urine drug screen for all participants. Participants completed all screening procedures prior to completing the baseline assessment. Participants were then randomized to either PNC-txt or waitlist control group. The control group received no intervention for three months. At the end of the study, they received the PNC-txt intervention. During the four weeks of the study, both conditions responded to two Ecological Momentary Assessment (EMA) survey questions regarding: 1) their cannabis use for the current day and 2) momentary cravings via text messages. EMA texts were sent out every other day for four weeks, for a total of 16 EMAs. After three months, the waitlist control group participants received the PNC-txt intervention. At 1, 2, and 3 months, post baseline assessment, participants completed a follow-up survey online. Immediately following the 3-month survey, participants returned to the research offices to provide a second urine sample for drug screening. Figure 1 is a CONSORT diagram illustrating participant recruitment to final analyses, including those excluded at screening and those who dropped out during the trial. Participants were compensated for the baseline assessment ($25) and each of the follow-up assessments and EMA surveys ($30, $35, and $40 respectively) and received an additional payment for providing a urine sample at the final three- month assessment ($20) for a total of up to $150 over the course of the study. The majority of participants completed the 1-month (97%), 2-month (80%) and 3-month (87%) follow-up assessments.
Figure 1.
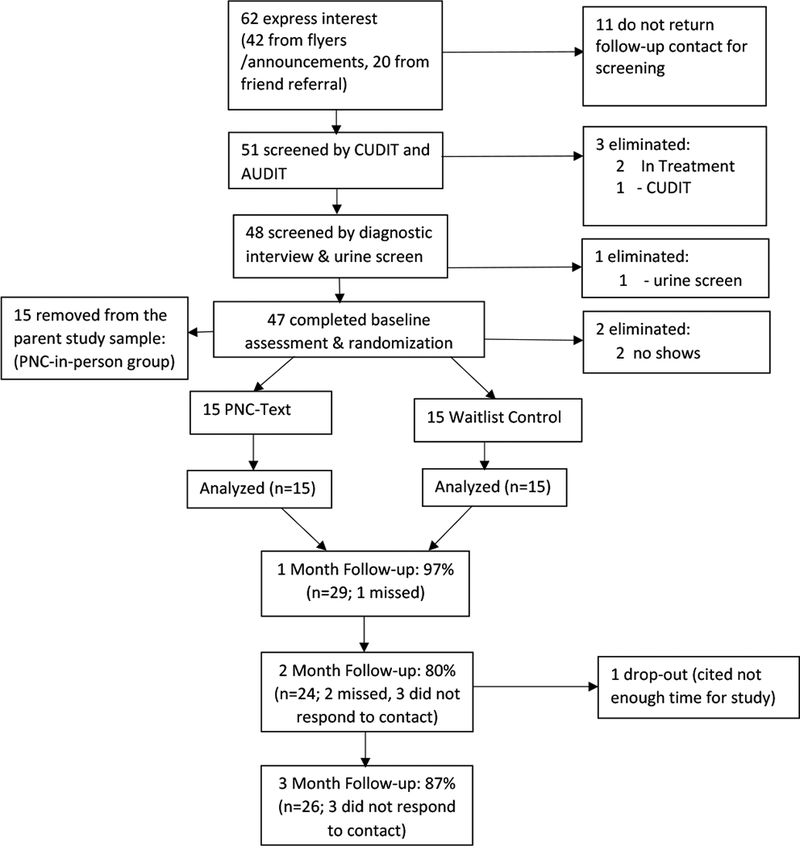
Consort diagram
2.3. How PNC-txt Works
PNC-txt began with two texts that asked about craving level and if the participant had used cannabis in the last 24 hours (See section D.4 Momentary Cannabis Use & Craving for details). The next five texts covered the intervention content, tapping the same constructs as the in-person intervention and providing tailored feedback from the participant’s survey. Instructions contained at the end of each text directed participants to reply back with either “ok” or with a response to a specific question or statement, such as responding with what they like about cannabis, in order to continue. In this way, the text interactions attempts to mimic the discussion between the counselor and participant that occurs in the in-person version of the intervention. Testing of the text intervention indicated that each day’s texts took approximately 1–2 minutes to complete. Thus, the text intervention offers approximately the same dose of interaction (~20 minutes) as the in-person intervention. Each intervention day ended with a closing text, alerting the participant that no further texts would follow and reminding them of the option to text “Boost” for additional support if desired. The “boost” option provided supportive messages as often as the participant would like. These are general messages provided to supplement the intervention, such as “Changing little things like spending less time in places that remind you of using can really help.”
An automated, web-based texting platform named TextIt (Nyaruka, 2016) was used to implement the intervention. The program automatically populated data from the participant’s baseline assessment into the text messages. Baseline data informed the normative feedback regarding their cannabis use by comparing their reported use to age-matched national data such as the National Survey on Drug Use and Health. For the peer network health feedback, we used the YASNA score to determine if their network was not-healthy, average, or healthy. These three categories were based on score values that were negative (not healthy), within 1 standard deviation of a 0 score (average), and scores above average (healthy).
In order to protect participants’ privacy, we used the term “SMK” to represent cannabis use. Participants were informed of this at enrollment, and also selected nick-names for their peers to protect privacy. Participants also were provided with a handout on privacy by the research assistant who reviewed ways for keeping the text messages private (e.g., blocking the text preview display on the phone’s home screen and setting a password on the phone). Further, participants were given the choice to receive the first text message of each day at either 6:00 PM or 9:00 PM. The research assistant showed the participant what the texts would look like and how to respond. Participants were encouraged to respond to the texts as soon as their schedule allowed, but not to respond while driving or in a setting where texting would be inappropriate (e.g., class). Participants were automatically sent a reminder text message to complete the intervention two-hours after receiving the first text of the day and again at 8:00 AM the following morning if still incomplete. If participants did not respond to these automatic reminders, a trained research assistant would contact the participant by personal text, email and/or phone call as an additional reminder to complete the intervention texts every other day.
2.4. Measures
Demographics.
Participants reported their age, sex, and race during the initial survey at enrollment.
Cannabis Use Disorder Screening.
During the initial phone contact participants were screened for likely CUD using the Cannabis Use Disorders Identification Test Revised (CUDIT- R; Adamson et al., 2010). Participants with CUDIT scores of at least 8 were included in the study. The CUDIT has favorable internal reliability (Cronbach’s alpha = .84).
Alcohol Use Disorder Screening.
At initial phone contact participants were screened for likely AUD using the Alcohol Use Disorders Identification Test (AUDIT; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). Participants with scores of 20 or greater were excluded from the study. We chose to exclude participants with AUD as alcohol and cannabis are the most frequently abused substances among adults and research has demonstrated that persons with comorbid AUD and CUD are a particularly vulnerable group whose cannabis use is more severe and associated with more problems that may require a greater intensity of clinical attention (Hayaki, Anderson, & Stein, 2016). The AUDIT has favorable internal reliability (Cronbach’s alpha = .80).
Urine Drug Test.
The CLIA Waived Integrated E-Z Split Key Cup II (TestCountry.com, 2016) was used to determine whether THC was present in the participant’s urine sample. A positive result for THC was required for inclusion in the study. The urine test used in this study also tested for cocaine and methamphetamine, however, positive screens on these drugs were not exclusionary. These combination test kits were used as they were more readily available than THC- only test kits. No samples were found to have evidence of cocaine or methamphetamine. Cutoff level for testing THC was 50 ng/mL. This cutoff level leads to a binary result of THC presence in the urine, but does not indicate the concentration of THC nor recency of use. Dependent upon frequency of use, THC may be detectable in urine for 30 days post-use (Redwood Toxicology Laboratory, 2018). The urine drug test was administered in-person at two timepoints - screening and immediately after the three-month follow-up.
Cannabis Use Disorder.
At enrollment into the study, CUD was confirmed using the Cannabis Use Disorder Diagnostic Interview (CUDDI; Mason & Zaharakis, 2016). We developed this instrument for this study based on the DSM-5 diagnostic criteria for CUD to confirm the disorder diagnosis and to characterize CUD severity. The CUDDI uses the 11 DSM-5 diagnostic criteria, each of which addresses multiple aspects of CUD symptoms (e.g., During the past 12 months: Have you thought about cutting down or controlling your cannabis use?). Each item was coded as no = 0, yes = 1. A total score was generated by summing each item producing a range of 0–11. Diagnostic and severity scores were interpreted following the DSM-5 CUD symptom count criteria: 0–1 = no CUD; 2–3 = mild CUD; 4–5 = moderate CUD; ≥6 = severe CUD. A score of at least 2 was necessary for inclusion into the trial. The CUDI measure has acceptable internal reliability (Cronbach’s alpha = .75).
Past 30-day Cannabis Use.
We assessed past 30-day frequency of cannabis use, as well as days abstinent, consecutive days abstinent, number of grams used, maximum grams used, and heavy use days using the Timeline Followback [TLFB,(Sobell & Sobell, 1996)] at baseline and each follow-up timepoint. The TLFB test-retest reliability ranges from .75 to .96.
Cannabis Problems.
We used the Marijuana Problem Index (MPI; White, Labouvie, & Papadaratsakis, 2005) to assess past 30-day frequency of problems related to cannabis use at baseline and each follow-up timepoint. The MPI is a 28-item measure that uses a 5-point frequency scale: 0 = never, 1 = 1–2 times, 2 = 3–5 times, 3 = 6–10 times, 4 = more than 10 times. A total score is produced by summing items and is interpreted as higher scores indicating more problems. The MPI has acceptable internal reliability (Cronbach’s alpha = .86).
Momentary Cannabis Use & Craving.
Via a text message ecological momentary assessment (EMA) survey, participants rated their momentary craving for cannabis and whether they had used cannabis in the past 24 hours. Participants were asked “Have you SMKed in the last 24 hours,” and “How would you rate your craving for SMK right now? (0=none - 10=intense)” and responded by texting yes or no and a number from 0 (no craving at all) to 10 (intense craving). The EMA texts were sent out 16 times (every other day for one month) between baseline and one- month follow-up. Participants were given the option of receiving the text message survey at 6:00 PM or 9:00 PM. Individual momentary assessment scores at each of the 16 assessments (range: 0–10) are a representation of overall craving (with higher scores interpreted as more intense cravings). These scores were used to model craving over time, as described in the analysis section.
Peer Network Health.
Peer network health data were gathered using the Young Adult Social Network Assessment (YASNA; Mason, Cheung, & Walker, 2004). The YASNA captures information on each subject’s three closest friends, which constitute their personal or egocentric friend network. These friends are whom participants indicated they spent the most time with in person, on average. Participants are asked if each friend uses cannabis, the frequency of use, if they have received offers to use cannabis, and if the participant and the friend co-participated in cannabis use. The YASNA also captures protective activities with their friends such as receiving instrumental and emotional support (help with school or transportation, or by talking through problems), prosocial encouragement (encouraging exercise, academic clubs, volunteering), and suggestions to reduce or not use cannabis. These items create a total score for each friend and then are summed for a total Peer Network Health score. The seven items are weighted and are based upon previous research that has shown, for example, that risk for substance use doubles with one substance user in a network, and risk for mental health problems increases three-fold with one daily substance user in a network (Mason et al., 2004). Assuming three peers per participant, total peer network health scores can range from −42 to 42. Higher scores indicate greater peer network health, and lower scores indicate increased behavioral risk. The YASNA has favorable internal reliability (Cronbach’s alpha = .84) and is positively correlated with days abstinent from cannabis (.622) and negatively with intentions to use in the next 30 days (−.786).
Treatment Satisfaction.
We assessed the PNC-txt group satisfaction at the one-month follow-up (immediately after the end of the PNC-txt intervention) with 10 items covering relevance and helpfulness, as well as comprehension, frequency and amount of texts. Items were rated on a 1 to 5 scale (Strongly Disagree to Strongly Agree), with 5 being most positive response. A mean score was computed across all items, as well as for each individual item. The treatment satisfaction measure has favorable internal reliability (Cronbach’s alpha = .96).
2.5. Statistical Analyses
We calculated descriptive statistics on all key variables used in our models. To determine the effect of the intervention, a general linear repeated measures model was used to examine follow-up assessments (Time 2, 3, 4), and baseline (Time 1) scores on two outcome variables: past 30-day cannabis use and cannabis problems. We conducted a repeated measures analysis of covariance, controlling for race, gender, age, and baseline CUD severity level to examine treatment condition X time interactions. We obtained effect sizes using the Partial Eta Squared statistic, allowing us to test intervention effectiveness compared to control and across time (baseline to 3-month follow-up). We conducted these same repeated measures procedures examining treatment condition x time interactions on the seven peer network health items. Next, we conducted a moderation test to determine if CUD severity level would moderate the relationship between treatment condition and cannabis problems. We employed the approach described by Hayes (2013) and the PROCESS SPSS computational tool (model 1). We used cannabis problems as the dependent variable, treatment condition as the predictor variable, and CUD severity level as the moderator. We then estimated the conditional effect of treatment condition on cannabis problems as a function of CUD severity, using an inferential test to interpret the interaction. This allows the moderation of treatment condition’s effect on cannabis problems to depend on three levels of CUD severity: 1 standard deviation (SD) below the mean, the mean, and 1 SD above the mean. We conducted a univariate analysis of variance to determine differences in the 3-month follow-up urine analysis (presence of cannabis metabolites) by condition.
Time-varying effect modeling (TVEM; Lanza, Vasilenko, Liu, Li, & Piper, 2014) was used to estimate time-varying PNC-txt effects on cannabis craving using the momentary craving item. TVEM analyses were conducted via the following steps. First, model coefficients (the intercept and slopes describing treatment effects on craving) were estimated as a function of time since the start of the intervention. Dummy variables were created to test the time-varying effects of PNC-txt on craving, with the wait-list condition serving as the reference group. These time- varying effects, represented by unstandardized regression coefficients and their 95% confidence intervals (CIs), were plotted, and treatment effects were declared significant on all days when the 95% CIs did not overlap with 0. Second, trajectories illustrating time-varying levels (and 95% confidence intervals) of craving since the start of the study were generated for PNC-txt by recentering the time-varying effect model. The SAS software 9.4 and the SAS macro %TVEM_normal (TVEM SAS, V 3.1.1, 2017) was used to estimate the model. The macro as well as detailed technical information is available free for download at www.methodology.psu.edu. Missing items for self-reported measures across all three months ranged from 0 to 9. Little’s Missing Completely At Random (MCAR) test was subsequently conducted (X2 (3) = 26.9, p = 0.194), indicating no systematic missingness. A total of 23 missing items across all measures and all participants were found. No differences were found between original and the imputed data. A power analysis revealed that using a repeated measure F-test and conservatively assuming a small effect size (.22), the sample of 30 would have .80 power to detect differences between the two groups. Missing data were handled using multiple imputation procedures (i.e., expectation maximization algorithm) in SPSS V. 21 No differences were found between original and the imputed data.
3. Results
3.1. Characteristics, Texting Delivery & Engagement Results.
Table 3 provides descriptive demographic statistics and baseline scores of key variables by condition. The PNC-txt messages were sent to the correct recipient at the correct time and delivered the correct message with 100% accuracy. PNC-txt participants completed 99.4% of all responses to the intervention. Approximately one-third (30%) of PNC-txt participants utilized at least one boost message. The PNC-txt group treatment satisfaction was 3.5 (SD =1.18). Examination of individual items showed that participants most highly endorsed that the texts made them think about their cannabis use, the ease of understanding the texts, and the amount of texts. Table 6 provides descriptive statistics on the treatment satisfaction measure.
Table 3.
Descriptive statistics and baseline scores by condition (N=30).
| PNC-Text (n = 15) | Control (n = 15) | |
|---|---|---|
| Age [mean (sd)] | 20.7 (2.1) | 20.8 (2.8) |
| Female (%) | 46.7 | 53.3 |
| Race1 | ||
| African American (%) | 26.7 | 26.7 |
| White (%) | 60.0 | 60.0 |
| Employment | ||
| Part-time (%) | 38.4 | 38.4 |
| Full-time (%) | 15.3 | 15.3 |
| Enrolled in College (%) | 60 | 73.3 |
| Current Residence | ||
| With Family (%) | 20 | 26.6 |
| On Campus (%) | 20 | 13.4 |
| Without Family (%) | 60 | 60 |
| Parent College Graduate (%) | 53.3 | 66.6 |
| Cannabis Use Disorder Test | 22.9 (4.2) | 21.8 (4.1) |
| Alcohol Use Disorder Test | 8.07 (3.8) | 7.86 (4.9) |
| CUD Severity Level | 9.46 (1.4) | 9.26 (1.3) |
| Past 30 Days Cannabis Use | 23.4 (6) | 23.5 (6) |
| Past 30 Days Cannabis Problems | 36.2 (14.7) | 41.7 (13.4) |
Other races are not reported as these were a small percentage of the sample.
There were no significant differences between groups on all baseline variables.
Table 6.
Treatment Satisfaction Results.
| Item | M | SD |
|---|---|---|
| Were relevant to my marijuana use. | 3.29 | 1.20 |
| Were easy to understand. | 4.29 | 1.27 |
| Were the right amount each day (not too many or too few). | 4.00 | 1.36 |
| Came to me at the right times. | 3.50 | 1.16 |
| Were helpful to my marijuana treatment. | 3.36 | 1.34 |
| Were the right amount each week. | 3.64 | 1.28 |
| Made me think about my marijuana use. | 4.00 | 1.13 |
| Were the right amount to 4 weeks. | 3.67 | 1.18 |
| Made me think about my peers. | 3.40 | 1.55 |
| Gave me some helpful ideas to consider. | 3.73 | 1.22 |
3.2. Cannabis Use and Problems Results.
Table 4 presents the adjusted group means (adjusted for CUD severity score) and standard deviations from baseline to 3-month follow-up on past 30-day cannabis use and cannabis problems. We hypothesized that PNC-txt would reduce past 30-day cannabis use and cannabis problems. The results from the first model on past 30-day cannabis use indicated no significant condition X time interaction, F (3, 22) = 0.447, p = 0.72, eta2 = 0.057. To examine this null finding further, we examined days abstinent, number of grams used, and largest number of grams used in the past 30 days. We found no statistical difference in these outcomes.
Table 4.
Adjusted group means and standard deviations from baseline to 3-month follow-up on cannabis use outcomes
| Outcomes | Adjusted PNC-txt means (SD) | Adjusted Control means (SD) | Eta2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 1 month | 2 month | 3 month | Baseline | 1 month | 2 month | 3 month | ||
| Past 30-day cannabis use | 23.4 (6.0) | 20.4 (9.8) | 14.7 (12.2) | 17.6 (10.8) | 23.5 (6.0) | 22.3 (5.2) | 17.3 (9.1) | 17.7 (10.3) | 0.057 |
| Past 30 day cannabis problems | 36.2 (14.7) | 36,2 (14.0) | 14.2 (11.3) | 12.2 (8.4) | 41.7 (13.4) | 43.0 (12.1) | 33.3 (18.4) | 25.6 (19.3) | 0.221* |
| Negative Urine | 0% | 44% | 0% | 7% | 0.15* | ||||
p < 0.05
The second model testing the effect of treatment condition on cannabis problems was found to be significant, F (3, 22) = 3.258, p = 0.04, eta2 = 0.308, producing a large effect size. Figure 2 provides a visualization of the second model on cannabis problems. Over the 4-weeks of treatment the PNC-txt group reported increased problems, leaving both groups essentially at the same point at the 1-month follow-up time-point. The PNC-txt group then showed a steep reduction in problems throughout the remainder of the study compared to the control group. This pattern may be indicative of a strong effect of PNC-txt on cannabis problems.
Figure 2.
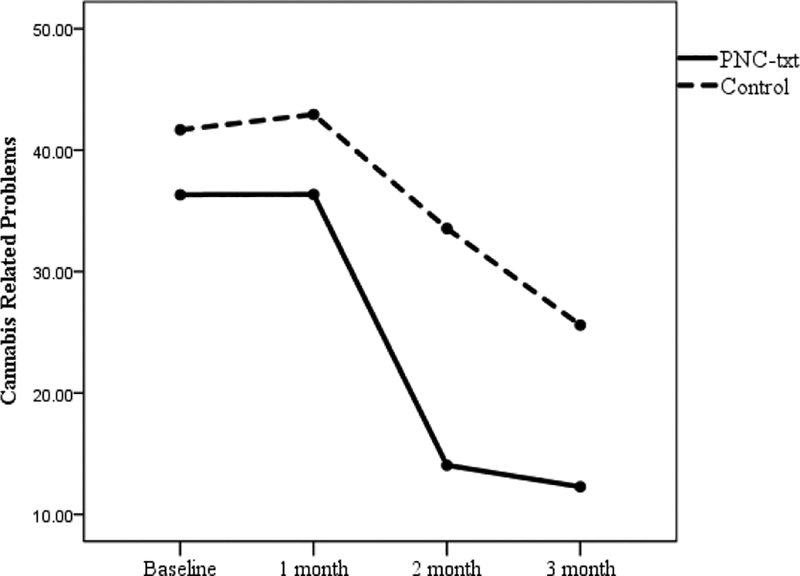
PNC-txt treatment effects on cannabis problems.
Analysis of individual items on the Marijuana Problem Index suggest that the intervention may have most benefited several problem areas. Participants in the treatment group reported significantly fewer days missing school or work or attending school or work while under the influence of cannabis, as well as reductions in problems related to school or work. Treatment participants reported fewer problems with memory and clear thinking. Mental health problems were also significantly reduced, comprising fewer problems with feeling unmotivated, loss of interest, overly nervous, and “going crazy.” Finally, PNC-text appears to have reduced problems related to CUD symptoms, including less problems with tolerance and withdrawal symptoms, as well as less difficulty in trying to control or cut down on use. Interpersonal problems, such as getting into fights with family or friends, saying or doing mean things, and causing shame or embarrassments to others appeared not to have been affected by the intervention.
3.3. Moderation Results.
We hypothesized that if the association between treatment condition and cannabis use and problems were significant, CUD severity would moderate these relationships. Specifically, we expected that reductions in treatment outcomes would be associated with higher levels of CUD severity, based on our previous research that indicated PNC is more effective with heavy cannabis use participants (Mason et al., 2016). Because only cannabis problems were found to be significant, we conducted the moderation analysis on this outcome. Supporting our second hypothesis, the association between treatment condition and cannabis problems was significantly moderated by CUD severity (p < 0.05). The conditional effect analysis revealed that the moderating effect of treatment condition on cannabis problems was observed when CUD severity was high (b = −24.5, SE = 7.22, p = 0.002) and moderate (b = −13.7, SE = 4.94, p = 0.010), but not low (b = −2.9, SE = 7.03, p = 0.683). In examining the effects further, it appears that the cases classified as high severity got nearly double the effect relative to cases with moderate severity (high = −24.5, moderate = −13.7).
3.4. Cannabis Craving Results.
Figure 3 shows the time-varying effect of PNC-txt on participants’ cannabis craving. The PNC-txt condition significantly reduced cannabis craving during the first 24 days of the intervention, where the 95% CI for the treatment effect does not include 0 (represented by the straight horizontal line). The PNC-txt effect was already apparent during the first few days post-intervention, and increased steadily during the first week, peaking on day 8, when participants in PNC-txt group showed craving levels that were 2.6 units lower than participants in the control group. Afterward, the PNC-Text effect slowly began to dissipate, until it became nonsignificant on day 25.
Figure 3.
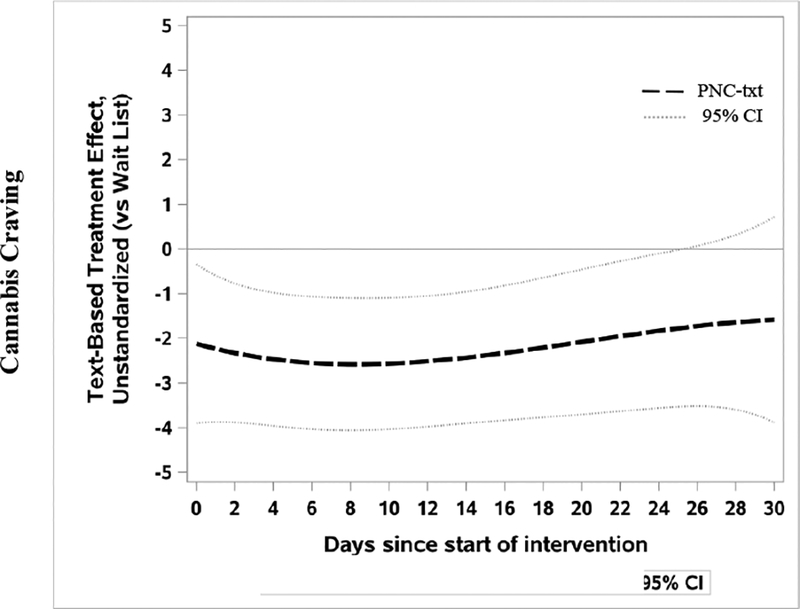
Time-varying effect of PNC-txt versus control on cannabis craving. Treatment effects are significant (p < 0.05) at all times when the 95% CI does not overlap with 0, represented by the horizontal lines.
3.5. Urine Analysis Results.
Finally, we used a univariate analysis of variance to test the 3-month follow-up of the presence of cannabis metabolites in participant urine specimen by condition. We hypothesized that PNC-txt participants would reduce positive cannabis metabolites specimens compared to controls. Results supported this hypothesis, showing that the PNC-txt group produced significantly more urines negative for cannabis metabolites compared to the control group, Sum of Squares = 0.683, F (1, 27) = 5.054, p = 0.03, eta2 = 0.158.
3.6. Peer Network Health Results.
Table 5 presents the adjusted group means and standard deviations from baseline to 3- month follow-up on the seven peer network health items. Participants in the PNC-txt group significantly reduced the number of cannabis users in their networks, F (3, 22) = 2.93, p = 0.04, eta2 = 0.12, reduced the frequency of peer cannabis use, F (3, 22) = 2.69, p = 0.05, eta2 = 0.10, and increased peer instrumental and emotional support, F (3, 22) = 3.54,p = 0.03, eta2 = 0.32, compared to the control group. Thus, PNC-txt may influence two peer network health dimensions in the hypothesized direction: reduction of peers who use cannabis (and the amount used) and increasing support.
Table 5.
Peer Network Health Items by Condition.
| Outcomes | Adjusted PNC-txt means (SD) | Adjusted Control means (SD) | Eta2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 1 month | 2 month | 3 month | Baseline | 1 month | 2 month | 3 month | ||
| Number of users in network | 2.66 (.61) | 2.53 (.63) | 2.2 (.86) | 2.1 (.89) | 2.07 (.82) | 2.32 (.72) | 2.25 (.64) | 2.21 (.80) | .10* |
| Frequency of use in network | −7.8 (1.0) | −6.7 (1.1) | −7.4 (.94) | −7.12 (1.4) | −7.8 (.98) | −6.7 (1.1) | −7.4 (.94) | −7.2 (1.1) | .33** |
| Offers to use | −14.4 (5.1) | −11.0 (7.3) | −11.6 (5.4) | −12.6 (7.6) | −11.0 (7.3) | −12.9 (4.8) | −10.3 (8.1) | −9.4 (6.9) | .13 |
| Use with friend | −9.8 (3.3) | −8.5 (4.9) | −7.3 (4.5) | −7.7 (4.3) | −9.8 (2.9) | −8.1 (4.8) | −7.2 (4.8) | 5.7 (4.5) | .12 |
| Asked to reduce or not use | −14.2 (5.1) | −11.0 (7.3) | −11.6 (5.4) | −12.6 (7.6) | −11.0 (7.3) | −12.9 (4.8) | −10.9 (6.8) | −9.4 (6.9) | .05 |
| Support | 3.8 (4.8) | 6.0 (5.5) | 4.8 (5.4) | 4.8 (5.9) | 6.8 (5.0) | 6.6 (4.8) | 4.8 (5.4) | 4.8 (5.9) | .12* |
| Prosocial Encouragement | 1.5 (1.0) | 1.7 (.88) | 1.8 (1.0) | 1.7 (.96) | 1.4 (1.1) | 1.7 (.88) | 1.0 (.97) | 1.2 (.96) | .05 |
p <.05;
p <.01
4. Discussion
The findings from this small trial provide preliminary evidence that PNC-txt may be efficacious in reducing cannabis related problems for those with moderate and high levels of CUD severity, in reducing cannabis craving, and in reducing positive cannabis metabolites specimen results among young adults. Based on our review of the literature, this study is the only published randomized clinical trial testing a stand-alone text message-based intervention to treat cannabis use among young adults. In addition, these findings suggest that PNC-txt may be efficacious in reducing risk behavior and increasing protective behaviors within a young adult’s close peer group.
Our results extend those of Shrier and colleagues (2014) in finding evidence for the effectiveness of a text message intervention in reducing cannabis related problems, without additional in-person counseling. To do this, we used tailored text messages customized based on baseline assessments, as Shrier et al. did, but covered a wider range of content over a longer period of time (4 weeks). Further, our intervention offered this expanded set of messages to all participants, regardless of whether they momentarily reported use, craving or triggers. Like Shrier and colleagues, we found that our intervention improved treatment outcomes, with our results demonstrating reductions in cannabis use related problems. In addition, our intervention appears to have reduced cannabis craving and improved participants’ peer networks through the reduction of the amount of cannabis used and by increasing support.
The null result regarding days used cannabis may have occurred for multiple reasons. First, there may be no difference in treatment effects between conditions either due to actual effects or due to the study being under-powered. Second, we have seen in our previous work that PNC-txt can produce both initial effects as well as a secondary effect that occurs approximately 3.5 months into a study (Mason, Mennis, Way, Lanza, Russell, & Zaharakis, 2015). It is not unreasonable to speculate that given more time, the current study results may mirror previous findings. However, this is an empirical question that future research should address.
The reduction of cannabis related problems is a promising finding and may be evidence of a harm-reduction effect, common with brief interventions. As can be seen in figure 2, the PNC-txt group reported more problems during the 4-weeks of their treatment. This may be due to the treatment raising awareness of these problems. After the treatment period, the PNC-txt group sharply reduces problems over the next two months, producing a steeper reduction relative to controls. Our use of a covariance adjustment that included CUD severity into the model provides reasonable confidence in this result (Pocock, Assmann, Enos, & Kasten, 2002). The potential to reduce cannabis related problems is promising as is the finding that CUD severity level moderates PNC-txt. This finding supports our previous work with the PNC-in-person version, which demonstrated improved treatment effects with adolescents who were heavy users of cannabis (Mason et al., 2016c). These results may have been influenced by seaonality, as recruitment occurred near the end of a semester (March to May), the reporting of problems could be decreased due to reduced academic workload and the anticipation of summer.
Exploratory examination of specific problem types revealed that PNC-txt may be most effective in reducing problems related to fulfilling responsibilities associated with school and work, improving memory and cognitive ability, lessening symptoms of depression and anxiety, and decreasing symptoms of dependence. The intervention did not appear to improve interpersonal problems related to relationships with family and friends. These findings suggest that the intervention may have reduced cannabis use, though the study is underpowered to detect this finding. Reductions in use would likely lead to improved psychosocial functioning, as these results suggest. In contrast, interpersonal problems may be more entrenched behavior patterns that are unlikely to change due to a brief intervention. Importantly, these results suggest that the intervention can improve academic and job performance and decrease mental health problems, areas that are especially salient to young adults who are in a developmental stage in which mental health symptoms peak. Future refinements of this intervention may benefit from additional assessment of these problem areas and content aimed at reducing these problems, such as encouragement to attend school or work without being under the influence of cannabis or suggestions for ways to manage anxiety and depression through positive social support.
The reduction of cannabis craving during the PNC-txt intervention is an important finding because during these four weeks the control group was essentially an ‘active control group.’ Controls were responding every other day to texts about their use and craving perhaps stimulating reflection and behavior change. Recall that all participants were treatment seeking, who had sufficient motivation to enroll and complete the trial. Thus, the assessment effect may be particularly evident in this control group, as they wanted to receive treatment, but had to wait 90 days. Given this potential assessment effect, the reduction of craving during this period provides more confidence in PNC-txt, by demonstrating the reduction of craving is likely associated with the content of PNC-txt, and not just the act of receiving and responding to neutral text messages.
The finding that PNC-txt produced significantly more urines negative for cannabis metabolites provides evidence that this group actually used less cannabis than controls at 3- months. In reconciling this result to the past 30-days used outcome, it could be that the control group reported using less than they actually did use. Another explanation is that the control group did reduce their use early in the study, but the PNC-txt group used less during the last month of the study, and therefore produced more urines negative for cannabis metabolites. Regardless, this finding provides encouragement that PNC-txt is a promising, cost-effective treatment for CUD.
This study also provides initial evidence that participants in the PNC-txt group improved their peer network health as theorized. Reducing the number of cannabis users in one’s network and reducing the frequency of peer cannabis use, are demonstrable adjustments to participants’ peer network. PNC-txt participants also increased the support that they received from their peer network. This would fit with PNC-txt’s clinical goal of increasing reflection on the benefits of particular peers, such that peer behaviors are actually changing or there is increased awareness of the support that already exists. These findings could mean that PNC-txt participants actually changed the composition of their peer network, or it could be interpreted as a positive contagion effect, where peers modify their cannabis use and support based on the participants’ behaviors. Future research with larger samples should examine the peer network health mechanisms of specific behavioral change.
Overall, participants of the treatment intervention rated PNC-text positively. Comprehension and amount of texts were rated highest, as was that the texts encouraged reflection on participants’ use. While still positive, the relevancy and helpfulness of texts were rated lowest, as was the intervention’s ability to encourage reflection on peers. These data can inform future study of the active ingredients of the intervention. Refinements should continue to test different amounts of texts delivered increase to expand these results.
Results of this study need to be tempered by the following limitations. First, the sample size was small and thus analyses were underpowered and may be less stable compared to a larger sample. Second, we did not collect urine samples at months 1 and 2, as this is a task that is very challenging with an outpatient sample. Third, the follow-up period was 3 months instead of 6 to 12 months. Fourth, we did not assess other forms of treatment- therapy or 12-step support during the follow-up period. We excluded those with treatment history within 90 days of the start of the study, but did not assess this at follow-up. Fifth, the participants were ‘treatment seeking’ and therefore results may not replicate among more general pools of young adults with CUD or among those who may not be seeking treatment. Finally, we did not submit our hypotheses a priori to clinicaltrials.gov, e.g., because this study was an initial feasibility trial. These limitations are common features of pilot studies and can be addressed in future research.
5. Conclusion
In all, this small pilot trial provides initial evidence that PNC-txt may be a promising approach to treating young adults with CUD . It is reasonable to continue this line of research with both young adults and adolescents who have moderate to severe levels of CUD. Lessons learned from the current study could provide guidance to improve future efforts. Specifically, areas for future research are 1) testing the amount of texts 2) capturing qualitative data to improve content, 3) testing creative approaches for participants who want more than the texts provide, and 4), addressing polysubstance use. As polysubstance use is common, finding novel ways to address an underlying behavioral pattern could reveal a common treatment approach that would be very relevant to this population, and 5) collecting qualitative data to inform the ongoing text development. These type of data could provide insight into what makes the best text messages and messaging. This encouraging platform for intervention has potential to provide needed, cost-effective treatment to populations struggling with their cannabis use.
Footnotes
Disclosure:
All authors have not conflicts of interest with the research presented in this manuscript.
References
- Adamson SJ, Kay-Lambkin FJ, Baker AL, Lewin TJ, Thornton L, Kelly BJ, & Sellman JD (2010). An improved brief measure of cannabis misuse: The Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug and alcohol dependence, 110(1), 137–143. doi: 10.1016/j.drugalcdep.2010.02.017. [DOI] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, Bugbee BA, Vincent KB, & O’Grady KE (2015). The academic consequences of marijuana use during college. Psychology of Addictive Behaviors, 29(3), 564. doi: 10.1037/adb0000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Garnier-Dykstra LM, Caldeira KM, Vincent KB, Winick ER, & O’Grady KE (2013). Drug use patterns and continuous enrollment in college: Results from a longitudinal study. Journal of Studies on Alcohol and Drugs, 74(1), 71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Barrio G, Jiménez-Mejías E, Pulido J, Lardelli-Claret P, Bravo MJ, & de la Fuente L (2012). Association between cannabis use and non-traffic injuries. Accident Analysis & Prevention, 47, 172–176. doi: 10.1016/j.aap.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, & Olfson M (2008). Mental health of college students and their non-college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Archives of general psychiatry, 65(12), 1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke K (2016, May 18). How many texts do people send every day? [Web log post]. Retrieved from https://www.textrequest.com/blog/many-texts-people-send-per-day/
- Caldeira KM, Kasperski SJ, Sharma E, Vincent KB, O’ Grady KE, Wish ED, & Arria AM (2009). College students rarely seek help despite serious substance use problems. Journal of Substance Abuse Treatment, 37(4), 368–378. doi: 10.1016/j.jsat.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldeira KM, O’Grady KE, Vincent KB, & Arria AM (2012). Marijuana use trajectories during the post-college transition: Health outcomes in young adulthood. Drug and Alcohol Dependence, 125(3), 267–275. doi: 10.1016/j.drugalcdep.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASAColumbia. (2007). Wasting the best and the brightest: Substance abuse at America’s colleges and universities. New York (US): Columbia University National Center on Addiction and Substance Abuse (CASA). [Google Scholar]
- Deutsch AR, Chernyavskiy P, Steinley D, & Slutske WS (2015). Measuring peer socialization for adolescent substance use: A comparison of perceived and actual friends’ substance use effects. Journal of Studies on Alcohol and Drugs, 76, 267–277. 10.15288/jsad.2015.76.267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Exner-Cortens D (2014). Theory and teen dating violence victimization: Considering adolescent development. Developmental Review, 34(2), 168–188. doi: 10.1016/j.dr.2014.03.001. [DOI] [Google Scholar]
- Gonzales R, Hernandez M, Murphy DA, & Ang A (2016). Youth recovery outcomes at 6 and 9 months following participation in a mobile texting recovery support aftercare pilot study. The American journal on addictions, 25(1), 62–68. doi: 10.1111/ajad.12322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayaki J, Anderson BJ, & Stein MD (2016). Dual cannabis and alcohol use disorders in young adults: Problems magnified. Substance abuse, 37, 579–583. doi: 10.1080/08897077.2016.1176613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis. NY, NY: Guilford. [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2018). Monitoring the Future national survey results on drug use: 1975–2017: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Lanza ST, Vasilenko SA, Liu X, Li R, & Piper ME (2014). Advancing the understanding of craving during smoking cessation attempts: A demonstration of the time-varying effect model. Nicotine & Tobacco Research, 16, S127–S134. doi: 10.1093/ntr/ntt128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, & Li G (2012). Marijuana use and motor vehicle crashes. Epidemiologic Reviews, 34(1), 65–72. doi: 10.1093/epirev/mxr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason M, Benotsch EG, Way T, Kim H, & Snipes D (2014). Text messaging to increase readiness to change alcohol use in college students. The Journal of Primary Prevention, 35(1), 47–52. doi: 10.1007/s10935-013-0329-9. [DOI] [PubMed] [Google Scholar]
- Mason M, Cheung I, & Walker L (2004). Substance use, social networks, and the geography of urban adolescents. Substance use & misuse, 39(10–12), 1751–1777. doi: 10.1081/JA-200033222. [DOI] [PubMed] [Google Scholar]
- Mason MJ, Light J, Campbell L, Keyser-Marcus L, Crewe S, Way T, Saunders H, King L, Zaharakis N, & McHenry C (2015b). Peer network counseling with urban adolescents: A randomized controlled trial with moderate substance users. Journal of Substance Abuse Treatment, 58, 16–24. doi: 10.1016/j.jsat.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason M, Mennis J, Way T, Lanza S, Russell M, & Zaharakis N (2015c). Time-varying effects of a text-based smoking cessation intervention for urban adolescents. Drug and Alcohol Dependence, 157, 99–105. 10.1016/j.drugalcdep.2015.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason M, Mennis J, Way T, Zaharakis N, Campbell LF, Benotsch EG, & King L (2016a). Text message delivered peer network counseling for adolescent smokers: A randomized controlled trial. The Journal of Primary Prevention, 37(5), 403–420. doi: 10.1007/s10935-016-0439-2. [DOI] [PubMed] [Google Scholar]
- Mason M, Ola B, Zaharakis N, & Zhang J (2015a). Text messaging interventions for adolescent and young adult substance use: A meta-analysis. Prevention Science, 16, 181–188. 10.1007/s11121-014-0498-7 [DOI] [PubMed] [Google Scholar]
- Mason M, Pate P, Drapkin M, & Sozinho K (2011). Motivational interviewing integrated with a social network intervention for female adolescents: A randomized pilot study in urban primary care. Journal of Substance Abuse Treatment, 41(2), 148–155. doi: 10.1016/j.jsat.2011.02.009. [DOI] [PubMed] [Google Scholar]
- Mason MJ, Sabo R, & Zaharakis NM (2016c). Peer network counseling as brief treatment for urban adolescent heavy cannabis users. Journal of Studies on Alcohol and Drugs, 78(1), 152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason MJ & Zaharakis NM (2016b). Cannabis Use Disorder Diagnostic Interview.Unpublished instrument. [Google Scholar]
- Miller WR, & Rollnick S (2013). Motivational interviewing: Helping people change. New York: Guilford Press. [Google Scholar]
- Mrug S, & McCray R (2013). Parental and peer disapproval of alcohol use and its relationship to adolescent drinking: Age, gender and racial differences. Psychology of Addictive Behavior, 27(3), 604–614. doi: 10.1037/a0031064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyaruka Ltd. (2016). TextIt. Available at https://textit.in/.
- Perron BE, Mowbray OP, Glass JE, Delva J, Vaughn MG, & Howard MO (2009). Differences in service utilization and barriers among Blacks, Hispanics, and Whites with drug use disorders. Substance Abuse Treatment, Prevention, and Policy, 4, 3. doi: 10.1186/1747-597X-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pocock S, Assmann S, Enos L, & Kasten L (2002). Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Statistics in Medicine, 21, 2917–2930. doi: 10.1002/sim.1296 [DOI] [PubMed] [Google Scholar]
- Pollard MS, Tucker JS, de la Haye K, Green HD, & Kennedy DP (2014). A prospective study of marijuana use change and cessation among adolescents. Drug and Alcohol Dependence, 144, 134–140. doi: 10.1016/j.drugalcdep.2014.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redwood Toxicology Laboratory (2018). Marijuana Drug Information. Retrieved from https://www.redwoodtoxicology.com/resources/drug_info/marijuana.
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA & Patrick ME (2017). Monitoring the Future national survey results on drug use, 1975–2016: Volume II, College students and adults ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Shrier LA, Rhoads A, Burke P, Walls C, & Blood EA (2014). Real-time, contextual intervention using mobile technology to reduce marijuana use among youth: A pilot study. Addictive Behaviors, 39(1), 173–180. doi: 10.1016/j.addbeh.2013.09.028. [DOI] [PubMed] [Google Scholar]
- Smith A (Sept. 19, 2011). Americans and text messaging. Retrieved from http://pewinternet.org/Reports/2011/Cell-Phone-Texting-2011.aspx
- Sobell LC, Sobell MB (1996) Alcohol Timeline Followback (TLFP) Users’ Manual. Addiction Research Foundation, Toronto, Canada. [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] (2015). Reaching and Engaging Non-College Young Adults in Prevention Efforts. Retrieved from https://www.samhsa.gov/capt/sites/default/files/resources/reaching-noncollege-young-adults.pdf.
- Substance Abuse and Mental Health Services Administration (2016). 2015 National survey on drug use and health: Detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Suerken CK, Reboussin BA, Egan KL, Sutfin EL, Wagoner KG, Spangler J, & Wolfson M (2016). Marijuana use trajectories and academic outcomes among college students. Drug and Alcohol Dependence, 162, 137–145. doi: 10.1016/j.drugalcdep.2016.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TestCountry.com. (2016). CLIA Waived Integrated E-Z Split Key Cup II. Retrieved: 10.16.17 at TestCountry.com
- TVEM SAS Macro (Version 3.1.1) [Software]. (2017). University Park: The Methodology Center, Penn State. Retrieved from http://methodology.psu.edu
- White HR, Labouvie EW, & Papadaratsakis V (2005). Changes in substance use during the transition to adulthood: A comparison of college students and their noncollege age peers. Journal of Drug Issues, 35, 281–306. doi: 10.1177/002204260503500204. [DOI] [Google Scholar]


