Abstract
Objective:
For chronic depression, the effectiveness of brief psychotherapy has been limited. This study is the first comparing the effectiveness of long-term cognitive-behavioural therapy (CBT) and long-term psychoanalytic therapy (PAT) of chronically depressed patients and the effects of preferential or randomized allocation.
Methods:
A total of 252 adults met the inclusion criteria (aged 21-60 years, major depression, dysthymia, double depression for at least 24 months, Quick Inventory of Depressive Symptoms [QIDS] >9, Beck Depression Inventory II [BDI] >17, informed consent, not meeting exclusion criteria). Main outcome measures were depression self-rating (BDI) and rating (clinician-rated QIDS [QIDS-C]) by independent, treatment-blinded clinicians. Full remission rates (BDI ≤12, QIDS-C ≤5) were calculated. An independent center for data management and biostatistics analyzed the treatment effects and differences using linear mixed models (multilevel models and hierarchical models).
Results:
The average BDI declined from 32.1 points by 12.1 points over the first year and 17.2 points over 3 years. BDI overall mean effect sizes increased from d = 1.17 after 1 year to d = 1.83 after 3 years. BDI remission rates increased from 34% after 1 year to 45% after 3 years. QIDS-C overall effect sizes increased from d = 1.56 to d = 2.08, and remission rates rose from 39% after 1 year to 61% after 3 years. We found no significant differences between PAT and CBT or between preferential and randomized allocation.
Conclusions:
Psychoanalytic as well as cognitive-behavioural long-term treatments lead to significant and sustained improvements of depressive symptoms of chronically depressed patients exceeding effect sizes of other international outcome studies.
Keywords: chronic, treatment-resistant depression, psychoanalytic psychotherapy, cognitive-behavioural therapy, long-term psychotherapy, remission, outcome
Abstract
Objectif :
L’efficacité d’une brève thérapie est limitée pour la dépression chronique. Cette étude est la première qui compare l’efficacité de la thérapie cognitivo-comportementale (TCC) à long terme et des thérapies psychanalytiques (TPA) à long terme chez des patients chroniquement déprimés, et les effets d’une allocation préférentielle et randomisée.
Méthodes :
Un total de 252 adultes satisfaisait aux critères d’inclusion (âge 21-60 ans, dépression majeure, dysthymie, double dépression pendant au moins 24 mois, QIDS >9, BDI >17, consentement éclairé, ne pas satisfaire aux critères d’exclusion). Les principales mesures des résultats étaient l’auto-évaluation de la dépression (BDI) et l’évaluation (QIDS-C) par des cliniciens indépendants, à l’insu du traitement. Les taux de rémission complète (BDI ≤12, QIDS-C ≤5) ont été calculés. Un centre indépendant de gestion des données et des biostatistiques a analysé les effets et les différences des traitements à l’aide de modèles linéaires mixtes (modèles multi-niveau et hiérarchiques).
Résultats :
La moyenne de la BDI a baissé de 32,1 points à 12,1 points durant la première année, et de 17,2 points sur 3 ans. La moyenne de l’ampleur de l’effet de la BGI générale est passée de d = 1,17 après 1 an à d = 1,83 après 3 ans. Les taux de rémission de la BDI ont augmenté de 34% après 1 an à 45% après 3 ans. L’ampleur de l’effet de la QIDS-C générale a augmenté de d = 1,56 à d = 2,08, et les taux de rémission se sont accrus de 39% après 1 an à 61% après 3 ans. Nous n’avons pas constaté de différences significatives entre la TPA et la TCC ou entre l’allocation préférentielle et randomisée.
Conclusions :
Les traitements psychanalytiques et cognitivo-comportementaux à long terme entraînent des améliorations significatives et soutenues des symptômes dépressifs de patients chroniquement déprimés qui excèdent l’ampleur de l’effet d’autres études de résultats internationales.
Clinical Implications
In the first controlled trial comparing the outcome of long-term psychoanalytic and cognitive-behavioural treatments for chronically depressed patients either with randomized or with preferred allocation, psychoanalytical and cognitive-behavioural therapies achieve similar outcomes on a symptomatic level.
Chronically depressed patients achieve sustained improvement of symptoms and remission up to 61% by long-term psychotherapy after 3 years of treatment. This finding is of interest for clinicians, patients, and insurance companies, implying that chronically depressed patients benefit from long-term psychotherapies.
No differences were found between randomized and preferential assignments regarding symptomatic outcome.
Further mediator and moderator analyses of the data will offer information about which long-term treatment may best treat chronically depressed patients.
Limitations
Due to the fact that two-thirds of patients had a clear treatment preference, the randomization arm was not sufficiently powered for an equivalent trial. Therefore, the missing statistical difference between the outcome of preferred and randomized patients might be due to lack of power.
Due to ethical reasons, medication could not be homogenized in this group of severely ill patients. While we compared the percentage of patients on medication between treatment modalities, the influence of medication on therapy outcome could not be studied in our design.
Due to ethical considerations, a nontreatment control group was not feasible. Only differential treatment effects of psychoanalytic therapy and cognitive-behavioural therapy long-term therapies can be compared.
Reimbursement of long-term treatments is provided in Germany but only in few other countries. Therefore, one could argue that our results could not be generalized to other countries.
Depression is a chronic or recurrent disorder1 that is difficult to treat and often treatment resistant. It remains one of the major challenges for mental health care, contributing to the suffering of individuals and their families, as well as to enormous mental health costs.1 In many randomized controlled trials (RCTs), cognitive-behaviour therapy (CBT) has been established as an effective treatment for acute unipolar depression.2 Short-term psychodynamic psychotherapy (PAT) was found equally effective compared to CBT3 and other psychotherapies.4 For chronic depression, the effects of short-term psychotherapy have been limited, and relapse rates were high.5,6 Positive long-term effects of long-term psychoanalytic treatments in complex mental disorders have been shown in several studies.7,8 In a recent study8 comparing long-term psychoanalytic therapy with treatment as usual, PAT showed a delayed therapeutic effect (not before 24 months after intake) and later (up to 42 months) turned out superior to the control condition. Until now, no RCT studies have compared long-term PAT and CBT directly. Based on their theoretical rationales, PAT or CBT differ in therapeutic aims, treatment intensity, frequency, and number of sessions. It is an open question about which group of chronically depressed patients benefits from which form of long-term treatment (PAT or CBT).8–11
We expected that many of the chronically depressed patients had already undergone several psychotherapeutic treatments with limited success and thus have preferences for another treatment. Therefore, we decided to give them the option to be allocated randomly or according to their treatment preference. A meta-analysis12 of 35 studies previously found that patients who were matched to their preferred treatment were less likely to drop out and showed greater improvement. Patients with strong preferences may refuse randomization, limiting the external validity of an RCT.13,14
This report will determine the short-term and long-term outcomes of PAT and CBT in reducing depressive symptoms, compare the remission rates of PAT and CBT over 3 years, and assess the influence of preferential treatment assignment.
We hypothesized that both treatments lead to lasting effects, that PAT starts more slowly but achieves more stable effects, and that remission rates will increase in both treatments.9 Antidepressant medication at the beginning of psychotherapies was documented and controlled statistically.
Methods
Study Design and Participants
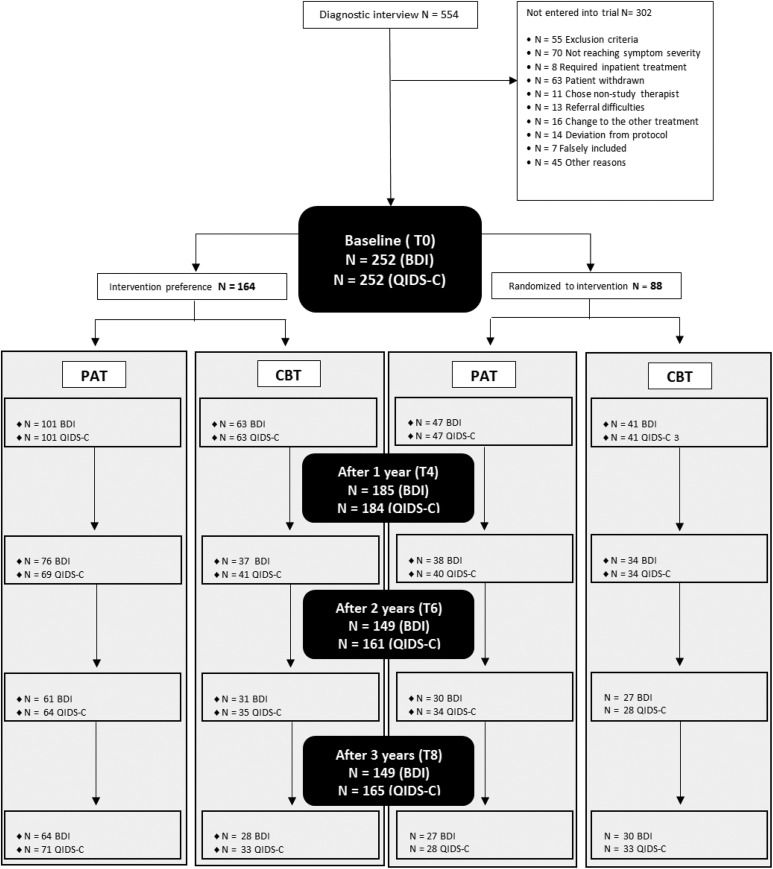
The Outcomes of Longterm Psychotherapies of Chronically Depressed Patients (LAC) study is a multicenter, controlled, single-blind 4-arm trial with a preference and a randomized section (see Figure 1).9 After being given a written general description of both forms of psychotherapy, patients were asked if they have a preference for 1 specific treatment (PAT or CBT). Patients were assigned according to preference or randomly allocated if they articulated no specific preference.
Figure 1.
Study design and patient flow diagram. BDI, Beck Depression Inventory II; CBT, cognitive-behavioural therapy; PAT, psychoanalytical therapy; QIDS-C, clinician-rated Quick Inventory of Depressive Symptoms Inventory of Depressive Symptoms. Inclusion of patients into the trial required checking of exclusion and inclusion criteria and informed consent on behalf of the patient. However, as described above in the CONSORT diagram, a number of patients did not comply with the study protocol and were therefore excluded: assigned to treatment (n = 292), chose nonstudy therapists (n = 11), referral difficulties (n = 13), and changed to other treatments (n = 16).
In 4 study centers (Frankfurt a.M., Mainz, Berlin, and Hamburg), we included patients between 21 and 60 years of age with chronic depression who gave written informed consent to study participation.9 Patients had to be depressed for more than 1 year and meet diagnostic criteria of major depressive episode or dysthymia. Their current depression severity had to meet a Beck Depression Inventory II (BDI–self-report15; score above 17) and a clinician-rated Quick Inventory of Depressive Symptoms (QIDS-C16; score of more than 9 points).9 Patients with antidepressant medication were included if they were on a stable dosage for more than 4 weeks. The study was registered (Clinical Trial Register ISRCTN91956346) and approved by the Ethics Committee of the State of Rhineland-Palatinate, Mainz, Germany (Ref: 837.124.075659).
Interventions
PAT for depression is well described.8,17–20 To ensure homogeneity, all study PAT therapists participated in training workshops based on the empirically validated PAT manual for treatment of chronic depression.21 Therapists were taught to uncover and modify the unconscious idiosyncratic fantasies and conflicts due to developmental deficits and traumatizations underlying chronic depression. The unconscious mental functioning (e.g., as manifested in dreams, current object relationships, fantasies leading into psychic retreat) is observed and worked through in the ‘here and now’ of the transference relationship, aiming to change the psychic structure.21,22 Participating psychoanalysts (n = 73) were state licensed and had at least 3 years of clinical practice.
CBT for depression is based on the work of Beck et al. and Lewinsohn et al., as adapted and integrated in a nationally widely used and well-accepted treatment protocol by Hautzinger.23,24 In general, CBT therapists used 5 modules (problem analysis, goals, psychoeducation, rationale for treatment; behavioural activation, increasing pleasant activities; cognitive interventions to restructure basic assumptions, schemata; social skill training, problem solving, stress management; maintenance, relapse prevention). State-licensed CBT therapists (n = 44) with at least 3 years of clinical practice participated in training workshops.
Adherence to Treatment Protocol
Adherence was measured by the Comparative Psychotherapy Process Scale (CPPS)25 based on randomly selected audiotapes of therapies distinguishing between psychoanalytic and cognitive-behavioural treatments. A total of 137 therapy sessions (89 PAT, 48 CBT) were assessed by 3 independent raters. The average interrater reliability was satisfactorily high (intraclass correlation coefficient [ICC] >.85). The 2 psychotherapies could be distinguished clearly. Each item characterizing psychodynamic-interpersonal therapy was scored higher in PAT compared to CBT with moderate effect sizes (.35-.74); the same was true for higher ratings of cognitive-behavioural items in CBT versus PAT (moderate to large effect sizes, .3-.84).
Allegiance
Researchers and therapists had a psychoanalytic or cognitive-behavioural background. An independent group of statisticians without allegiance to either treatment provided randomization lists and did the final analyses.
Outcome Measures
Main outcome measures were the BDI15 and the short form of the QIDS (QIDS-C).16 Full remission rates were based on BDI and QIDS-C cutoff scores.15,16 All patients were diagnosed by the Structured Clinical Interview for DSM-IV (SCID I and II) and followed over the 3-year study period by the Longitudinal Follow-up Evaluation (LIFE).26 All ratings (QIDS-C) were conducted by independent, trained clinicians blinded to treatment. Interrater reliability for the QIDS-C ratings was high (Pearson correlation r = .95; confidence interval [CI], 0.889 to 0.999). Additional secondary outcome measures and predictors encompass structural change, social adaptation, quality of social relationships, and therapeutic alliance.9
Randomization
Patients consenting to be randomized were coded by the respective study site and assigned by the independent statistic center, which generated separate random allocation sequences for the study sites.
Sample Size Calculation
Sample size calculation was based on meta-analyses with comparable interventions, patient groups, and outcome measures.27 A study comparing PAT and CBT directly was not available. Therefore, we used meta-analysis data comparing psychotherapies and antidepressant medication in depressed outpatients to extrapolate a probable effect size of d = 0.50 between treatments.28 To detect this difference at α = 0.025 (two-tailed) with a power of 0.80, a minimum number of 60 patients per cell or a total of 240 patients were required.
Data Analysis
To analyze the time course of BDI and QIDS-C scores in the 4 treatment groups, 2 linear mixed models were estimated with the software package lme4 in R.29–31 The dependent variables were the BDI and QIDS-C scores of the patients 1, 2, and 3 years after treatment start (time points T4, T6, T8). The time points of observation and the treatment group of the patient (CBT, PAT, randomized, preference) were included as categorical independent variables. To estimate different time courses in the 4 treatment groups, interaction terms of time points and treatment groups were included into the model. To control for psychopharmacological medication at baseline, a 3-categorical independent variable was included specifying whether or not a patient took antidepressant medication or if no information was available. In addition, a linear effect for the mean-centered baseline score of each patient (BDI/QIDS-C score before treatment start) and a patient-specific Gaussian random intercept were included into the models to account for depression severity before treatment and the repeated measurements of each patient. Effects of categorical independent variables were estimated using effect coding.
To test for differences between time points, between treatment groups, and for different time courses in the treatment groups, we performed 3 approximate F tests for each of the 2 models. We used Kenward-Rogers’s approach implemented in the R software package pbkrtest29 to derive the degrees of freedom of the corresponding test statistics. To test for a general trend in expected scores over time and for overall differences in the expected scores of the 4 treatment groups, a linear mixed model was fitted with the respective covariate included (in addition to the baseline score, random intercept, and medication covariate) and tested against the (nested) baseline model without the respective covariate. To test for different time courses in the treatment groups, the full model (including the interaction of time point and treatment group) was tested against the model including only the main time and treatment effects.
In the main analysis, missing data were assumed to be missing at random. In addition, we performed a sensitivity analysis by repeating the analysis on data in which missing BDI/QIDS-C scores were imputed based on the last available score of the respective participant (last value carried forward).
Given the limitations of the sample sizes for detecting differences between treatments, we also computed 95% confidence intervals of the estimated group differences 1 and 3 years after treatment start to further illustrate the results and quantify uncertainty in estimation.
Results
Trial Flow and Baseline Characteristics
A total of 554 patients were interviewed. Of those, 252 patients were included into the study. Typical for a naturalistic treatment setting, treatment ended upon mutual agreement of therapist and patient. Figure 1 shows the numbers of participants included, reasons for exclusion, and the available main outcome assessments, BDI and QIDS, at baseline (T0) and after 1 (T4), 2 (T6), and 3 years (T8), separately for each treatment arm. Based on the total sample of 252 study patients, at least 1 outcome criterion (BDI or QIDS) was available for 73.4% after 1 year, 63.9% after 2 years, and 65.5% after 3 years.
Table 1 summarizes baseline demographic and clinical characteristics of all study subjects. The patient sample had chronic depression of high current symptom severity (BDI, 32.1 points; QIDS-C, 14.3 points). These scores correspond to percent rank above 75 in large samples of depressed patients.15,26 Most had long sick leaves from work due to depression during the past year. More than 70% had had previous psychotherapies, some even 4 and more treatments. More than one-third of our sample had been admitted to inpatient psychotherapy, and 36% were on antidepressant medication. According to the DSM-IV, 58.3% fulfilled major depression (MDE) criteria, 12.3% had dysthymia, and 29.4% were diagnosed with double depression.
Table 1.
Social and Medical Characteristic of Study Participants: Analyzed (n = 221) vs. Dropouts (n = 31).
| Variable | Total (N = 252) | Analyzed (n = 221) | Dropout (n = 31) | t/χ2 | P Value |
|---|---|---|---|---|---|
| Age, mean, y | 40.62 | 40.43 | 42.00 | –0.768 | 0.443 |
| BDI score, mean (SD) | 32.12 (7.97) | 31.84 (7.78) | 34.09 (9.12) | –1.482 | 0.140 |
| QIDS-C score, mean (SD) | 14.28 (3.05) | 14.23 (3.04) | 14.261 (3.13) | –.653 | 0.514 |
| Sex, n (%) | 0.140 | 0.709 | |||
| Men | 82 (32.5) | 71 (32.1) | 11 (35.5) | ||
| Women | 170 (67.5) | 150 (67.9) | 20 (64.5) | ||
| Job status, n (%) | 241 | 212 | 29 | 2.544 | 0.467 |
| Full- or part-time work | 168 (66.67) | 148 (66.97) | 20 (64.52) | ||
| Not working | 30 (11.90) | 28 (12.67) | 2 (6.45) | ||
| In school/training | 12 (4.76) | 11 (4.98) | 1 (3.23) | ||
| Unemployed | 31 (12.30) | 25 (11.31) | 6 (19.35) | ||
| Education, n (%) | 245 | 215 | 30 | 8.704 | 0.013 |
| Lower secondary or middle school | 75 (29.76) | 62 (24.60) | 13 (41.94) | ||
| High school | 166 (65.87) | 151 (68.33) | 15 (48.39) | ||
| Did not graduate/other | 4 (1.59) | 2 (0.09) | 2 (6.45) | ||
| Marital status, n (%) | 244 | 214 | 30 | 2.52 | 0.882 |
| Single | 146 (57.94) | 129 (58.37) | 17 (54.84) | ||
| Married | 64 (25.39) | 55 (24.89) | 9 (29.03) | ||
| Separated | 34 (13.49) | 30 (13.57) | 4 (12.90) | ||
| Work disability (12 months), n (%) | 237 | 208 | 29 | 4.913 | 0.178 |
| None | 101 (40.08) | 92 (41.63) | 9 (29.03) | ||
| 1-4 weeks | 46 (18.25) | 42 (19.0) | 4 (12.90) | ||
| 5-12 weeks | 43 (17.06) | 34 (15.38) | 9 (29.03) | ||
| >13 weeks | 47 (18.65) | 40 (18.09) | 7 (22.58) | ||
| Diagnosis, n (%) | 1.137 | 0.566 | |||
| Double depression | 74 (29.37) | 64 (28.96) | 10 (32.26) | ||
| Dysthymia | 31 (12.30) | 29 (13.12) | 2 (6.45) | ||
| (Recurring) major depressive episode | 147 (58.33) | 128 (57.92) | 19 (61.29) | ||
| Previous outpatient treatments, n (%) | 243 | 213 | 30 | 14.147 | 0.001 |
| None | 67 (26.59) | 61 (27.60) | 6 (19.35) | ||
| 1 | 63 (25.0) | 62 (28.05) | 1 (3.23) | ||
| 2 or more | 113 (44.84) | 90 (40.72) | 23 (74.19) | ||
| Antidepressant medication, n (%) | 228 | 203 | 25 | 4.804 | 0.091 |
| Yes | 107 (42.46) | 93 (42.08) | 14 (45.16) | ||
| No | 121 (48.02) | 110 (49.77) | 11 (35.48) |
BDI, Beck Depression Inventory II; QIDS-C, clinician-rated Quick Inventory of Depressive Symptoms.
Primary Outcome
Table 2 presents the change scores of the main outcome criteria at the different time points of the trial, separately for the 4 treatment arms. BDI/QIDS-C scores at 1, 2, and 3 years were subtracted from the baseline scores. Effect sizes (Cohen’s d) were estimated based on mean change scores divided by the square roots of scores’ pooled variances (at the respective time point and baseline). Full remission rates (cutoffs: BDI ≤12, QIDS-C ≤5) and numbers of participants with full data at each time point are also reported.
Table 2.
Changes of Patients’ Self-Ratings (BDI) and Expert (QIDS-C) Ratings.
| PREF CBT | PREF PAT | RAND CBT | RAND PAT | Total | |
|---|---|---|---|---|---|
| BDI | |||||
| Baseline | |||||
| Score, mean (SD) | 32.0 (7.8) | 31.2 (7.8) | 32.6 (7.0) | 33.9 (9.2) | 32.1 (8.0) |
| n | 63 | 101 | 41 | 47 | 252 |
| Year 1 (t4) | |||||
| Difference, mean (SD) | 14.4 (12.1) | 10.7 (11.1) | 12.6 (13.3) | 12.0 (12.7) | 12.1 (12.0) |
| Cohen’s d | 1.58 | 1.09 | 1.20 | 1.00 | 1.17 |
| Remission, % | 38 | 28 | 47 | 32 | 34 |
| n | 37 | 76 | 34 | 38 | 185 |
| Year 2 (t6) | |||||
| Difference, mean (SD) | 15.2 (9.7) | 13.9 (12.7) | 11.9 (12.2) | 15.2 (12.7) | 14.1 (12.0) |
| Cohen’s d | 1.77 | 1.38 | 1.03 | 1.39 | 1.38 |
| Remission, % | 45 | 38 | 33 | 33 | 38 |
| n | 31 | 61 | 27 | 30 | 149 |
| Year 3 (t8) | |||||
| Difference, mean (SD) | 17.2 (10.7) | 15.8 (10.9) | 17.5 (12.4) | 20.1 (11.9) | 17.2 (11.4) |
| Cohen’s d | 2.43 | 1.62 | 1.85 | 1.89 | 1.83 |
| Remission, % | 43 | 44 | 50 | 44 | 45 |
| n | 28 | 64 | 30 | 27 | 149 |
| QIDS-C | |||||
| Baseline | |||||
| Score, mean (SD) | 14.1 (3.0) | 14.3 (3.0) | 13.3 (2.6) | 15.2 (3.4) | 14.3 (3.1) |
| n | 63 | 101 | 41 | 47 | 252 |
| Year 1 (t4) | |||||
| Difference, mean (SD) | 7.1 (4.0) | 5.7 (4.4) | 6.6 (4.8) | 6.8 (4.9) | 6.4 (4.5) |
| Cohen’s d | 1.90 | 1.46 | 1.92 | 1.39 | 1.56 |
| Remission, % | 54 | 33 | 41 | 33 | 39 |
| n | 41 | 69 | 34 | 40 | 184 |
| Year 2 (t6) | |||||
| Difference, mean (SD) | 7.8 (4.5) | 8.0 (4.4) | 6.9 (5.9) | 8.6 (4.9) | 7.9 (4.8) |
| Cohen’s d | 2.12 | 2.45 | 1.62 | 1.94 | 2.07 |
| Remission, % | 57 | 44 | 46 | 44 | 47 |
| n | 35 | 64 | 28 | 34 | 161 |
| Year 3 (t8) | |||||
| Difference, mean (SD) | 7.0 (5.5) | 8.0 (5.1) | 9.7 (3.7) | 10.4 (5.9) | 8.5 (5.2) |
| Cohen’s d | 1.69 | 1.85 | 3.43 | 2.38 | 2.08 |
| Remission, % | 52 | 55 | 79 | 68 | 61 |
| n | 33 | 71 | 33 | 28 | 165 |
BDI, Beck Depression Inventory II; CBT, cognitive-behavioural therapy; PAT, psychoanalytic therapy; PREF, preference arm; QIDS-C, clinician-rated Quick Inventory of Depressive Symptoms; RAND, randomization arm. Shown are mean baseline scores and standard deviations, as well as means and standard deviations of difference scores compared to baseline for participants 1, 2, and 3 years after baseline (‘improvement’ on BDI/QIDS-C scale). Effect sizes (Cohen’s d) were estimated by subtracting patients’ scores (1, 2, 3 years) from their baseline scores, divided by the square root of pooled variance. Remission rates (BDI ≤12, QIDS-C ≤5) and number of participants with full data at each time point are also reported.
Table 3.
Estimated Coefficients of the Linear Mixed Models of the Primary Outcome Measures BDI and QIDS-C.19,20
| Estimate | SE | t Value | Significances | |
|---|---|---|---|---|
| BDI | ||||
| Intercept | 16.72 | 1.01 | 16.63 | |
| Baseline score | 0.52 | 0.09 | 5.74 | |
| 1 year (T4) | 2.42 | 0.50 | 4.86 | F(2, 301.3) = 18.5, P ≤ 0.001a |
| 2 years (T6) | 0.06 | 0.53 | 0.12 | |
| 3 years (T8) | –2.48 | 0.53 | –4.70 | |
| PREF CBT | –0.68 | 1.29 | –0.53 | F(3, 198.3) = 0.68, p = 0.56b |
| PREF PAT | 1.54 | 1.06 | 1.45 | |
| RAND CBT | –0.27 | 1.38 | –0.20 | |
| RAND PAT | –0.58 | 1.32 | –0.44 | |
| No medication T0 | –1.14 | 1.14 | –1.00 | |
| Medication T0 | 2.78 | 1.15 | 2.41 | |
| Missing medication T0 | –1.64 | 1.77 | –0.93 | |
| PREF CBT T4 | –1.14 | 0.91 | –1.26 | F(6, 296.2) = 0.88, p = 0.51c |
| PREF PAT T4 | 0.46 | 0.71 | 0.65 | |
| RAND CBT T4 | –0.18 | 0.90 | –0.20 | |
| RAND PAT T4 | 0.86 | 0.91 | 0.94 | |
| PREF CBT T6 | –0.84 | 0.96 | –0.88 | |
| PREF PAT T6 | –0.36 | 0.76 | –0.48 | |
| RAND CBT T6 | 1.02 | 0.96 | 1.06 | |
| RAND PAT T6 | 0.19 | 0.95 | 0.20 | |
| PREF CBT T8 | 1.98 | 0.97 | 2.04 | |
| PREF PAT T8 | –0.10 | 0.76 | –0.13 | |
| RAND CBT T8 | –0.84 | 0.93 | –0.89 | |
| RAND PAT T8 | –1.05 | 0.98 | –1.07 | |
| QIDS-C | ||||
| Intercept | 6.81 | 0.39 | 17.68 | |
| Baseline score | 0.50 | 0.09 | 5.33 | |
| 1 year (T4) | 1.07 | 0.22 | 4.92 | F(2, 326.5) = 16.3, P ≤ 0.001a |
| 2 years (T6) | –0.12 | 0.22 | –0.53 | |
| 3 years (T8) | –0.95 | 0.22 | –4.24 | |
| PREF CBT | 0.19 | 0.49 | 0.38 | F(3, 203.8) = 0.62, p = 0.60b |
| PREF PAT | 0.56 | 0.42 | 1.34 | |
| RAND CBT | –0.43 | 0.54 | –0.79 | |
| RAND PAT | –0.32 | 0.53 | –0.60 | |
| No medication T0 | –0.91 | 0.44 | –2.09 | |
| Medication T0 | 0.37 | 0.45 | 0.82 | |
| Missing medication T0 | 0.54 | 0.67 | 0.80 | |
| PREF CBT T4 | –1.17 | 0.39 | –2.97 | F(6, 318.4) = 3.67, p = 0.0015c |
| PREF PAT T4 | 0.37 | 0.32 | 1.17 | |
| RAND CBT T4 | 0.04 | 0.40 | 0.09 | |
| RAND PAT T4 | 0.76 | 0.39 | 1.95 | |
| PREF CBT T6 | –0.34 | 0.39 | –0.86 | |
| PREF PAT T6 | –0.52 | 0.32 | –1.59 | |
| RAND CBT T6 | 1.02 | 0.42 | 2.45 | |
| RAND PAT T6 | –0.16 | 0.40 | –0.41 | |
| PREF CBT T8 | 1.51 | 0.41 | 3.71 | |
| PREF PAT T8 | 0.14 | 0.32 | 0.45 | |
| RAND CBT T8 | –1.06 | 0.40 | –2.63 | |
| RAND PAT T8 | –0.59 | 0.42 | –1.42 |
BDI, Beck Depression Inventory II; CBT, cognitive-behavioural therapy; PAT, psychoanalytic therapy; PREF, preference arm; QIDS-C, clinician-rated Quick Inventory of Depressive Symptoms; RAND, randomization arm. Shown are the estimated coefficients of the additive mixed models with the dependent variables BDI-II and QIDS-C scores, the estimated standard errors, t values, and the significance of approximate F tests of a model, including the corresponding covariate/parameters against the smaller nested model. The model includes the baseline score as a continuous covariate, time, treatment group, medication, and the interaction between time and treatment. Effect coding has been used, so the coefficients of time and treatment group indicate differences from the overall mean on the respective outcome scales. Estimated random intercept standard deviations were 8.5 (BDI-II) and 3.3 (QIDS-C); residual standard deviations were 7.2 (BDI-II) and 3.2 (QIDS-C).
a Refers to the effect of time.
b Refers the effect of therapy group.
c Refers to the interaction of time and treatment group.
Over the first year, the average (total) BDI declined from 32.1 by 12.1 points and 17.2 points after 3 years. BDI overall mean effect sizes increased from d = 1.17 after 1 year to d = 1.83 after 3 years. Full remission rates for BDI increased from 34% to 45% after 3 years. The average QIDS-C declined by 6.4 points over the first year and by 8.5 points over 3 years. The QIDS-C overall effect sizes increased from d = 1.56 to d = 2.08, and full remission rates rose from 39% after 1 year to 61% after 3 years.
As expected, BDI scores decreased over the 3 years. The corresponding test of the time covariate rejects the null hypotheses of no differences in expected BDI scores at the 3 different time points (P ≤ 0.001). We found no differences of BDI scores between the 4 study groups. No differences in expected values for the treatment groups over all time points were found, and we found no interaction between time points and treatment groups. Medication at baseline was controlled as a covariate.
Consistent with these findings, QIDS-C scores decreased over the 3 years. For the QIDS-C scores, the null hypotheses of no time differences over all treatment groups could be rejected as well (P ≤ 0.001). There were no structural differences between the treatment groups over all time points. However, a significant effect was found regarding the interaction between time points and treatment groups (P ≤ 0.01). Again, medication at baseline was controlled as a covariate.
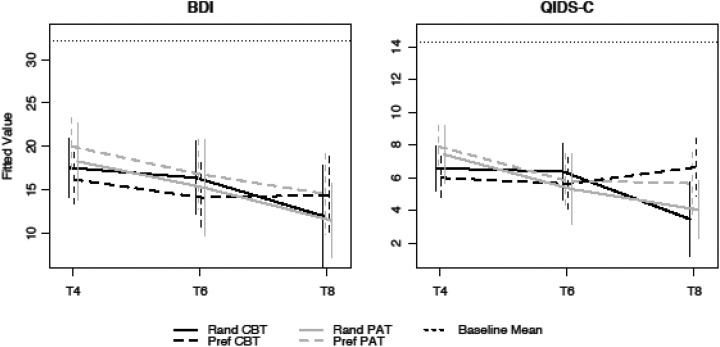
These findings are illustrated by Figure 2, depicting the course of change in the 4 treatment groups based on expected values and 95% confidence intervals. Against the mean baseline scores (dotted line on top of Figure 2), there were strong declines of expected BDI and QIDS-C scores to T4, which further declined to T8. As the figure indicates, the interaction between treatment group and time of QIDS-C was due to an increase of symptoms in the preference CBT arm and a further decrease of symptoms in the randomized CBT arm at T8. This corresponds to the difference of effect sizes calculated for CBT preference (d = 1.69) and CBT randomization (d = 3.43) at T8 (see Table 2).
Figure 2.
Estimated means and 95% confidence intervals over time in the 4 treatment groups against the mean baseline scores of BDI and QIDS-C. Estimated values of BDI/QIDS-C in the 4 different treatment groups (CBT, PAT, preference, randomization) after year 1 (T4), after year 2 (T6), and after year 3 (T8) for patients with mean baseline score and no baseline medication, associated 95% confidence intervals, and the mean baseline level. BDI, Beck Depression Inventory II; CBT, cognitive-behavioural therapy; PAT, psychoanalytic therapy.
The 95% confidence intervals of score differences between treatment groups at time points T4 and T8 are presented in the Supplemental Table S1. The sensitivity analyses (Suppl. Table S2) showed similar results as the main analysis. Based on the linear mixed models, there were no substantial differences between treatment groups. The interaction effect of treatment groups and time points was not significant for the models estimated by data with last value carried forward imputation.
Treatment Intensity
PAT and CBT offer different treatment intensities and durations due to their divergent conceptualizations of chronic depression. One major aim of PAT is to achieve so-called “structural changes” as a presupposition for sustaining change in patients, which can be observed in long follow-ups.4,7,18,22,32,33 According to this rationale, structural changes need longer and more intensive treatment. Our data showed that PAT had a mean (SD) of 80.4 (27.8) sessions during the first year of treatment, and CBT had a mean (SD) of 32.5 (9.0) therapy sessions. Over the 3 years, PAT had an average of 234 sessions, while CBT had an average of 57 sessions. PAT patients were in treatment for up to 36 months, while the last CBT patients ended treatment after 15 months.
Discussion
To our knowledge, this is the first controlled trial comparing the outcome of long-term psychoanalytic and cognitive-behavioural treatments for chronically depressed patients either with randomized or with preferred allocation. As expected, both treatments were associated with similar rates of symptom reduction and remission after 1 year. Remission rates increased to 45% (based on BDI) and 61% (based on QIDS-C) after 3 years. Exceeding previously reported remission rates of shorter treatments,8,10 our findings indicate a benefit of long-term treatments for chronically depressed patients.
Sustained improvement of the depressive symptoms has great relevance for these severely ill patients who have enormously high relapse rates.1,5,7 Preventing relapses of the chronically depressed is also significant for their families, reducing intergenerational transmission of depression and saving costs.7,32–35
Contrary to our expectation, being treated by the preferred psychotherapy did not result in better outcome than randomly assigned psychotherapy. Clearly, patients were reluctant to be randomized. After being educated about both psychotherapies offered in this trial, about two-thirds of our sample had articulated treatment preferences and were assigned accordingly. We thus consider this effect a possible statistical artefact due to the underpowered CBT randomization arm.
We took great care to conduct an outcome study relevant for clinical practice. Therefore, treatments were delivered under regular clinical conditions in outpatient settings and in private practice, performed by experienced psychotherapists, and reimbursed by health insurance. Thus, our study achieved high external validity under the conditions of regular psychotherapeutic care in Germany.
Reimbursement of long-term treatments offered the unique chance to investigate long-term treatment and to follow patients over 3 years after the beginning of outpatient treatment. Another follow-up after 5 years is ongoing.
PAT and CBT offered different intensities and durations of treatment due to their divergent theoretical conceptualizations of chronic depression and of the treatment process.7,8,17,23,36 To determine if improvements were due to common factors such as contact over time with the therapist or specific factors associated with each treatment modality (e.g., structural change in PAT), we will identify moderator and mediator variables for successful outcome of PAT and CBT, respectively. We have included a comprehensive set of secondary outcome criteria such as structural change, social adaptation, quality of social relationships, and therapeutic alliance to be used in such analyses.9 Future analyses will also scrutinize subgroups of chronically depressed patients who improved more in PAT or in CBT and how they differ from patients with less favorable outcomes. This will offer important insights into the relevant question about which chronically depressed patients need which kind and amount of treatment.18,37 Our findings may be taken to indicate that chronically depressed patients prefer psychoanalytic treatments obviously associated with higher direct treatment costs. Full analyses of direct and indirect costs of both treatments still need to be done.
To consider the clinical implications for working with this “difficult-to-treat” group of patients, we have taken great care to characterize our patients according to different dimensions of mental functioning beyond symptoms. As reported elsewhere,38 about 80% of our patients have had severe and cumulative childhood trauma, particularly emotional neglect, leading to maladaptive behaviour that may require long-term treatments to reduce relapses.
From a psychoanalytical perspective, chronically depressed patients have pathological self- and object-representations connected to unbearable emotions experienced during trauma (despair, helplessness, hopelessness), breakdown of mentalizing capabilities, and loss of basic feelings of self-agency and trust in helpful others. Modifying structural deficits in the self-object representations takes time and an intensive working through in the ‘corrective’ emotional relationship to the psychotherapist to reestablish some basic ‘epistemic trust’.36 Such ‘structural changes’ might be one reason why several studies reported that psychoanalytic treatments have a delayed therapeutic effect.4,5,8,19–21,32,33,39
From a cognitive-behavioural perspective, we need to understand by what mechanisms deeply ingrained maladaptive behaviour patterns are influenced by less intensive intervention. The mechanism of change should differ between CBT and PAT. Sustained changes can be achieved by more confronting, active, focused interventions.22 This should make it possible to take a step closer to answering such questions.
Limitations
Our naturalistic, controlled trial with 4 arms, 2 different active treatments, and 2 kinds of allocation suffers from several shortcomings, limiting our conclusions. First, we powered our design to detect treatment differences of an effect size of 0.5. Due to unavailable previous studies, we might have overestimated this difference and therefore underpowered our design. Concerning the randomization arm, we would have needed a larger sample. With only about 40 subjects in each cell of the randomization arms, we cannot reliably detect the unexpectedly small differences between preferred and randomized treatments. Not finding a significant difference between preferential and randomized allocation may therefore be a matter of statistical power. Second, the complexity of the design, recruitment of difficult-to-treat patients, and the long duration of the trial led to a considerable proportion of missing data at single time points. Differential attrition rates (e.g., in the CBT preferential arm) may have been due to different local conditions and commitments. However, by our statistical mixed-model analysis approach, we handled missing data, including all available assessments. The missing at random assumption could be problematic. Different imputation techniques could have led to slightly different results. Furthermore, we conducted a sensitivity analysis using the last available assessment for missing data. Third, we could not thoroughly control the effect of antidepressant medication over the duration of study time. Due to ethical reasons, medication could not be withheld in this group of severely ill patients. Only baseline medication was taken into account in our analyses.27,40,41 Fourth, in principle, the study would have been enhanced by adding a “treatment-as-usual” group in the design. However, given their high rates of previous treatments, we would have expected this group of patients to take up medication or CBT or PAT therapy in a treatment-as-usual arm.
Despite these limitations, the conclusion of this study is that psychoanalytic long-term psychotherapy as well as cognitive-behavioural long-term psychotherapeutic treatments help chronically depressed patients to achieve a sustained reduction of depressive symptoms and to substantially improve the remission rates. These are important findings for treating these “difficult-to-treat” patients in clinical practice on a global level.
Supplemental Material
Supplemental Material, 780340_Supplemental_Table_1 for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry
Supplemental Material
Supplemental Material, 780340_Supplemental_Table_2 for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry
Supplemental Material
Supplemental Material, 780340_Supplemental_Table_3 for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry
Supplemental Material
Supplemental Material, 780340_Supplemental_Table_3_English for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry
Acknowledgements
We thank all patients who participated, the study therapists and research assistants, interns, students, and members of the administrative teams of the participating institutions. The supporting institutions did not have any influence on the study realization or the data analyses.
Authors’ Note: Marianne Leuzinger-Bohleber and Martin Hautzinger share first authorship; Bernhard Rüger and Manfred Beutel share last authorship. Data are archived at the Department of Psychosomatic Medicine, University Medical Center of Mainz. Researchers interested in conducting meta-analyses may contact first and last authors (project leaders).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Deutsche Gesellschaft für Psychoanalyse, Psychotherapie, Psychosomatik und Tiefenpsychologie (DGPT); the Heidehof Foundation; the German Research Foundation (several conference supports); and a specific support of the Operationalized Psychodynamic Diagnostics (OPD) by Dr. M. von der Tann. Institutional supports also have been given by the participating Institutes and Universities.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet. 2007;370(9590):851–858. [DOI] [PubMed] [Google Scholar]
- 2. Lynch D, Laws KR, McKenna PJ. Cognitive behavioural therapy for major psychiatric disorder: does it really work? a meta-analytical review of well-controlled trials. Psycholo Med. 2010;40(1):9–24. [DOI] [PubMed] [Google Scholar]
- 3. Gibbons MBC, Gallop R, Thompson D, et al. Comparing effectiveness of cognitive therapy and dynamic psychotherapy for major depressive disorder in a community mental health setting: a randomized clinical noninferiority trial. JAMA Psychiatry. 2016;73(9):904–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Driessen E, Cuijpers P, de Maat SC, et al. The efficacy of short-term psychodynamic psychotherapy for depression: a meta-analysis. Clin Psychol Rev. 2010;30(1):25–36. [DOI] [PubMed] [Google Scholar]
- 5. Steinert C, Hofmann M, Kruse J, et al. Relapse rates after psychotherapy for depression—stable long-term effects? A meta-analysis. J Affect Disord. 2014;168:107–118. [DOI] [PubMed] [Google Scholar]
- 6. Cuipers P, Huibers MJH, Furukawa TA. The need for research on treatments of chronic depression. JAMA Psychiatry. 2017;74(3):242–243. [DOI] [PubMed] [Google Scholar]
- 7. Leuzinger-Bohleber M, Stuhr U, Rüger B, et al. How to study the quality of psychoanalytic treatments’ and their long-term effects on patient’s well-being: a representative, multi-perspective follow-up study. Int J Psychoanal. 2003;84(Pt 2):263–290. [DOI] [PubMed] [Google Scholar]
- 8. Fonagy P, Rost F, Carlyle JA, et al. Pragmatic randomized controlled trial of long-term psychoanalytic psychotherapy for treatment-resistant depression: the Tavistock Adult Depression Study (TADS). World Psychiatry. 2015;14(3):312–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beutel ME, Leuzinger-Bohleber M, Rüger B, et al. Psychoanalytic and cognitive-behavior therapy of chronic depression: study protocol for a randomized controlled trial. Trials. 2012;13:117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schramm E, Kriston L, Zobel I, et al. Effect of disorder-specific vs nonspecific psychotherapy for chronic depression. a randomized clinical trial. JAMA Psychiatry. 2017;74(3):233–242. [DOI] [PubMed] [Google Scholar]
- 11. Leichsenring F, Rabung S. Long-term psychodynamic psychotherapy in complex mental disorders: update of a meta-analysis. Br J Psychiatry. 2011;199(1):15–22. [DOI] [PubMed] [Google Scholar]
- 12. Long Q, Lin RJ. Causal inference in hybrid intervention trials: involving treatment choice. JASA. 2008;103(482):474–484. [Google Scholar]
- 13. Swift JK, Callahan JL, Vollmer B. Preferences. J Clin Psychol. 2011;67(2):155–165. [DOI] [PubMed] [Google Scholar]
- 14. Rawlins M. De testimonio: on the evidence for decision about the use of therapeutic interventions. Clin Med. 2008;8(6):579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hautzinger M, Keller F, Kühner C. Beck Depressions Inventar (BDI 2) Frankfurt a.M, Germany: Harcourt Test Service; 2006. [Google Scholar]
- 16. Rush AJ, Trivedi MH, Ibrahim HM. The 16-item Quick Inventory of Depressive Symptomatology (QIDS) clinical rating (QIDS-C) and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. [DOI] [PubMed] [Google Scholar]
- 17. Shedler J. The efficacy of psychodynamic psychotherapy. Am Psychol. 2010;65(2):98–109. [DOI] [PubMed] [Google Scholar]
- 18. Leuzinger-Bohleber M. Working with severely traumatized, chronically depressed analysands. Int J Psychoanal. 2015;96(3):611–636. [DOI] [PubMed] [Google Scholar]
- 19. Bleichmar H. Rethinking pathological mourning: multiple types and therapeutic approaches. Psychoanal Q. 2010;79(1):71–94. [DOI] [PubMed] [Google Scholar]
- 20. De Maat S, de Jonghe F, de Kraker R, et al. The current state of the empirical evidence for psychoanalysis: a meta-analytic approach. Harv Rev Psychiatry. 2013;21(3):107–137. [DOI] [PubMed] [Google Scholar]
- 21. Taylor D. Tavistock-manual der psychoanalytischen psychotherapie. Psyche Zeitschrift für Psychoanal. 2010;64:833–861. [Google Scholar]
- 22. Lane R, Ryan L, Nadel L, et al. Memory reconsolidation, emotional arousal, and the process of change in psychotherapy: new insights from brain science. Behav Brain Sci. 2015;38:e1. [DOI] [PubMed] [Google Scholar]
- 23. Hautzinger M. Cognitive behavior therapy of depression. 7th ed Stuttgart, Germany: Beltz Edition; 2013. [Google Scholar]
- 24. Trivedi RB, Nieuwsma JA, Williams JW., Jr Examination of the utility of psychotherapy for patients with treatment resistant depression: a systematic review. J Gen Intern Med. 2011;26(6):643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hilsenroth MJ, Ackerman SJ, Blagys MD, et al. Short-term psychodynamic psychotherapy for depression: an examination of statistical, clinically significant, and technique-specific change. J Nerv Ment Dis. 2003;191(6):349–357. [DOI] [PubMed] [Google Scholar]
- 26. Keller MB, Lavori PW. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540–548. [DOI] [PubMed] [Google Scholar]
- 27. Spijker J, van Straten A, Bockting CL, et al. Psychotherapy, anti-depressants, and their combination for chronic major depressive disorder: a systematic review. Can J Psychiatry. 2013;58(7):386–392. [DOI] [PubMed] [Google Scholar]
- 28. Thase ME, Greenhouse JB, Frank E, et al. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch Gen Psychiatry. 1997;54(11):1009–1015. [DOI] [PubMed] [Google Scholar]
- 29. Halekoh U, Højsgaard SA, Kenward R. Approximation and parametric bootstrap methods for tests in linear mixed models—the R package pbkrtest. J Statist Softw. 2014;59(9):1–30. [Google Scholar]
- 30. R Core Team. A language and environment for statistical computing Vienna, Austria: R Core Team; 2017. [Google Scholar]
- 31. Bates D, Mächler M, Bolker B, et al. Fitting linear mixed-effects models using lme4. J Statist Softw. 2015;67(1):1–48. [Google Scholar]
- 32. Monsen J, Odland T, Faugli A, et al. Personality disorders and psychosocial changes after intensive psychotherapy: a prospective follow-up study of an outpatient psychotherapy project, 5 years after end of treatment. Scand J Psychol. 1995;36(3):256–268. [DOI] [PubMed] [Google Scholar]
- 33. Knekt P, Lindfors O, Laaksonen MA, et al. ; Helsinki Psychotherapy Study Group. Quasi-experimental study on the effectiveness of psychoanalysis, long-term and short-term psychotherapy on psychiatric symptoms, work ability and functional capacity during a 5-year follow-up. J Affect Disord. 2011;13(1-2):37–47. [DOI] [PubMed] [Google Scholar]
- 34. Andrews G. Reducing the burden of depression. Can J Psychiatry. 2008;53(7):420–427. [DOI] [PubMed] [Google Scholar]
- 35. Beecham JK, Knapp MRJ. Costing psychiatric interventions In: Thornicroft G, Brewin C, Wing JK, eds. Measuring mental health needs. London: Gaskell/Royal College of Psychiatrists; 1992:163–183. [Google Scholar]
- 36. Fonagy P. The effectiveness of psychodynamic psychotherapies: an update. World Psychiatry. 2015;14(2):137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Milton J. Psychoanalysis and cognitive behaviour therapy-rival paradigms or common ground? Int J Psychoanal. 2001;82(Pt 3):431–447. [DOI] [PubMed] [Google Scholar]
- 38. Negele A, Kaufhold J, Leuzinger-Bohleber M. Childhood trauma from a patient and a psychoanalyst perspective: linking chronic depression to relational multiple trauma. Psychoanal Psychoth. 2016;30(4):300–328. [Google Scholar]
- 39. Corveleyn J, Luyten P, Blatt SJ, eds. The theory and treatment of depression: towards a dynamic interactionism model. Vol. 5 London: Routledge; 2013. [Google Scholar]
- 40. Fonagy P, Luyten P, Allison E. Epistemic petrification and the restoration of epistemic trust: a new conceptualization of borderline personality disorder and its psychosocial treatment. J Personal Disord. 2015;29(5);575–609. [DOI] [PubMed] [Google Scholar]
- 41. Huhn M, Tardy M, Spineli LM, et al. Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders: a systematic overview of meta-analyses. JAMA Psychiatry. 2014;71(6):706–715. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, 780340_Supplemental_Table_1 for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry
Supplemental Material, 780340_Supplemental_Table_2 for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry
Supplemental Material, 780340_Supplemental_Table_3 for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry
Supplemental Material, 780340_Supplemental_Table_3_English for Outcome of Psychoanalytic and Cognitive-Behavioural Long-Term Therapy with Chronically Depressed Patients: A Controlled Trial with Preferential and Randomized Allocation by Marianne Leuzinger-Bohleber, Martin Hautzinger, Georg Fiedler, Wolfram Keller, Ulrich Bahrke, Lisa Kallenbach, Johannes Kaufhold, Mareike Ernst, Alexa Negele, Margerete Schoett, Helmut Küchenhoff, Felix Günther, Bernhard Rüger, and Manfred Beutel in The Canadian Journal of Psychiatry