Short abstract
Objective
The aim of this study is to review the evidence for tailored eHealth weight-loss interventions, describing in detail: 1. how tailoring was implemented in these studies and 2. whether these tailored approaches were effective in producing weight loss compared with generic or inactive controls.
Methods
A systematic review was carried out. Five databases were searched up until 15 March, 2018, including: EBSCO, Science Direct, Pubmed, EMBASE and Web of Science, using combinations of the concepts ‘tailoring’, ‘eHealth’ and ‘overweight’.
Results
Eight articles relating to six interventions were accepted. Tailoring was carried out in a number of ways, based on, for example, anthropometric data, health-related behaviours (e.g. dietary intake, physical activity), goals (e.g. weight goal), theoretical determinants (e.g. confidence/willingness to change behaviours), psychosocial factors (e.g. social support) and participant location. Systems acquired data using strategies that ranged from online questionnaire administration, to the dynamic gathering of data from web-based diaries, websites, mobile applications and SMS messaging. Tailored interventions were more effective in supporting weight loss than generic or waitlist controls in four of the six articles. Effect sizes were very small to moderate, with evidence for fluctuations in effect sizes and differences of effect between tailoring and non-tailoring interventions, and between tailoring types, over time.
Conclusions
We contribute an enhanced understanding of the variety of methods used for the tailoring of eHealth interventions for weight loss and propose a model for categorising tailoring approaches.
Keywords: Tailoring, weight loss, eHealth, obesity, health behaviour change, systematic review, engagement, personalisation
Introduction
There is an urgent need to identify effective and scalable strategies to address what the World Health Organization terms ‘the obesity epidemic’. Indeed, the number of overweight and obese individuals has increased from 857 million in 1980 to 2.1 billion in 2013.1 However, we have yet to see strong evidence for a successful population-wide obesity intervention. In standard lifestyle interventions, behavioural therapy is delivered to participants by trained interventionists to support modification of diet and physical activity levels in an individual or group setting; it has been found to be effective in producing weight loss when compared with pharmacological strategies.2 This approach is resource-intensive, requiring significant input from both the patient and the interventionist, and can be costly to deliver, which poses a challenge for widespread translation of these approaches.3 Accessible and cost-effective interventions are necessary to bring about impact on a large scale. Two developments that appear promising for scalable, effective interventions are the use of eHealth tools in the delivery of interventions and tailoring of intervention content.
eHealth approaches to treating obesity
Research suggests that by delivering interventions via the Internet (eHealth), some of the cost and scalability problems of obesity interventions are mitigated.4,5 eHealth interventions can be deployed through websites, emails, text messages, monitoring devices, mobile applications, computer programmes, podcasts and personal digital assistants.5 eHealth systems can set individualised goals for users, monitor diet and physical activity behaviours, and respond to data with personalised guidance, among other behaviour-change strategies.
To establish the viability of these systems for large-scale impact, research into the implementation and outcomes of eHealth interventions is needed. Hutchesson et al.5 conducted a series of meta-analyses drawing on 88 eHealth weight loss or weight maintenance interventions. eHealth weight-loss interventions achieved modest weight-loss compared with no treatment (mean difference: –2.70 [–3.33, –2.08], p < 0.001; nine studies pooled in meta-analysis) or minimal treatment (mean difference: –1.40 [–1.98, –0.82], p < 0.001; 16 studies pooled in meta-analysis). Studies were found to be heterogeneous in both groups of pooled studies, I2 = 49%, p = 0.04 and (I2 = 72%, p < 0.001), respectively in terms of intervention strategy, technology usage and interaction style. eHealth interventions with extra features/behavioural components (e.g. self-monitoring, personalised feedback) or technologies (e.g. applications, texts or social networks) were more effective than standard eHealth programmes (drawing on either the Internet or podcasts only) (mean difference: 1.46 [0.80, 2.13], p < 0.001).5 Arem and Irwin6 also found the Internet-based weight-loss interventions included in their review to be heterogeneous. This was both in terms of the nature of the intervention (e.g. contact with participants, sample size and study duration) and their outcomes, with weight loss ranging from <1 kg to 4.9 kg. Crucially, since the interventions included in these reviews differed from each other in so many ways, it was impossible for the authors to make specific recommendations regarding which intervention components were necessary to bring about weight loss.
These effect sizes are modest in comparison with what may be achieved using traditional behavioural approaches. The modest weight losses demonstrated by the Hutchesson5 review are several times less than in-person interventions. For example, an in-person behavioural weight-loss intervention of 4–6 months of weekly group-based lifestyle counselling and intensive dietary restriction showed that participants lose on average 10.7 kg.7 These may be due in part to the varying intensity of behavioural-change strategies, personalisation strategies and supportive accountability provided by a human counsellor. To ascertain the effective components in these interventions, it is necessary to draw together the interventions that implement a common strategy.
A significant challenge to the wide-scale usage of eHealth interventions is that they typically suffer a steep decline in usage over the course of the intervention and have poor completion rates.4 Neve et al.8 highlight that use of eHealth technological components (both frequency and duration) may prove a useful metric to enable the establishment of an ‘optimal dose’ required for behaviour change. The review demonstrates that the higher the number of log-ins, self-monitoring occasions, chatroom attendances and bulletin board posts, resulted in greater weight loss, and this pattern was evident in the majority of studies included. Participant attrition is a key issue in assessing the efficacy of Internet-based interventions, as low levels of completion compromise the feasibility of implementing such interventions on a larger scale.
These findings provide promising support for the efficacy of eHealth interventions for weight loss.5,6 They confer an additional advantage over traditional methods, for example, in-person behavioural counselling in delivering weight-loss interventions in a cost-effective, effectual manner suited equally to the individual and at a scale needed to address the global obesity epidemic. Efforts to investigate specific strategies that are effective for weight loss, which address the issues of modest effects and low levels of engagement are needed. Delineating the precise strategies within eHealth efforts that are effective in bringing about the greatest decrease in weight requires a granulated examination and specification of the various components, modes of delivery, technological features and behavioural theory that inform these eHealth approaches, as well of usage of technological components as part of these efforts. Web-based weight-loss interventions have been reported as being less effective than face-to-face interventions,6,9 however, enhanced web-based interventions (e.g. more interactive and tailored) are more efficacious than basic, more generic interventions (e.g. purely informational).9 Web-based interventions may prove to be clinically effective and feasible if they can mimic some of the tools and strategies of the in-person interventions, while reaching a larger population.6 Enhancing web-based interventions through tailoring the eHealth interventions to characteristics of the user or patterns of behaviour is supported by a recent systematic review that evaluated web-based interventions for weight loss and maintenance.9
Tailoring as a strategy to enhance eHealth interventions
Tailoring is a process whereby the provision of information, advice and support is individualised to the user.10 Noar et al.11 explain that the process of tailoring involves an assessment of individual-level characteristics gathered by a person or self-administered (input: the basis for tailoring). This information then gets processed by either a human (human tailoring), or an expert system (computer tailoring) that uses algorithms to select content (i.e. text, images, recommendations and intervention messages) from an expert-developed database for the individual (tailoring process). Tailored material (output) is adapted using a variety of strategies to be delivered to the individual via multiple delivery modes.
Compared with non-tailored, generic materials, tailored health-messages command greater attention and are more likely to be read, elaborated upon, recalled and understood.12 As such, tailored health-messages are considered to be processed more deeply, contain less redundant information, and are perceived more positively by health consumers.13 Tailoring strategies can range from relatively simple, for example, employing the user’s name, to the more complex, for instance adapting content to personally relevant variables.14 Work has also been undertaken to draw together concrete definitions of tailoring strategies.13,15,16 Krebs et al.17 add to this by defining ‘dynamic tailoring’ as the assessment of intervention variables prior to each feedback and ‘static tailoring’ where one baseline assessment provides the basis of all subsequent feedback.
Impact of tailored approaches on health outcomes
While there is little evidence for the impact of tailored eHealth interventions for weight loss, evidence has accrued for the effectiveness of tailored web-based approaches to health interventions. For example, Lustria et al.10 conducted a meta-analysis to assess the impact of tailored web-based interventions targeting physical activity, nutrition, smoking/tobacco use, drinking, medication adherence (asthma management), stress management and faecal soiling (encopresis). Forty experimental and quasi-experimental studies were analysed and web-based tailored interventions effected significantly greater improvement in health outcomes compared with controls both at post-testing, d = 0.139 (95% CI = 0.111, 0.166, p < 0.001, k = 40) and at follow-up, d = 0.158 (95% CI = 0.124, 0.192, p < 0.001, k = 21). While these results are encouraging, (similarly to the eHealth reviews discussed earlier5,6) the authors identified that there was great variability in how tailoring was carried out among their included articles, including differences in intervention features, formats, and levels of interactivity.
A series of meta-analyses by Krebs et al.17 also assessed the effect of 88 computer-tailored interventions, using computer, print, or telephone communication channels that focused on four health behaviours: smoking cessation, physical activity, diet, and mammography screening. A significant, small effect size (Hedges’s g = 0.17) was found for tailored interventions, taking the average of the four health behaviours. This is encouraging evidence for tailoring as an approach to health behaviour change in general, but more specific approaches, honing in on one specific outcome may allow for in-depth conclusions to be drawn, considering that the determinants of health behaviour change interventions differ by outcome.
These studies provide support for tailoring as a strategy for use in health behaviour-change interventions, but we argue that previous research on tailored health interventions has focused primarily on understanding whether tailoring works, rather than focusing on how it works, or which approaches are most useful under which circumstances.12,15
The current study
Without meticulous description of intervention designs, the science and practice of tailoring within eHealth intervention design and implementation cannot be advanced. Previous work on tailoring has met with difficulty in differentiating the range of approaches to tailoring, differences in modality, intervention features and components.10 In addition, Harrington and Noar16 have called for improved reporting standards in tailored research.
The aim of the current paper was to review the evidence for tailored eHealth weight-loss interventions. We aim to describe in detail: 1. how tailoring was implemented in these studies and 2. whether these tailored approaches were effective in producing weight loss compared with generic or inactive controls. Specifically, we sought to identify what individual factors were assessed as part of the tailoring process, what tailoring strategies and eHealth tools were used, how engagement with eHealth interventions was conceptualised and whether tailoring increased this and, lastly, whether tailored approaches produced larger effect sizes than generic information and waitlist control approaches for weight loss.
Methods
Design
Systematic review of pre–post intervention trials with a control group, following Cochrane methodology and Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (see Appendix A).18 The review was registered with PROSPERO (CRD42017072901).19
A systematic review of tailored eHealth interventions for weight loss was carried out, with a title and abstract screening phase (Phase 1) and a full text screening phase (Phase 2).
Eligibility criteria
All papers that were deemed relevant at Phase 1 were included if they were quantitative peer-reviewed articles, published at any time, in the English language, with a pre-test–post-test intervention design (either randomised controlled trials (RCT) or pilot study) using a control comparison group (generic or inactive) approach. Interventions of any duration that aimed to bring about weight loss in overweight or obese (Body Mass Index (BMI) >25), free-living participants without specified clinical disease were included. Articles were required to have a stated tailored approach, which we operationalised as ‘if the intervention was personalised, and based on an assessment of individual characteristics’.20 The intervention was required to be behavioural in nature (e.g. aimed to change diet and physical activity), and delivered primarily via the Internet (Internet-based); in-person measurement of weight was permissible, as was briefing to randomisation group components. Articles were excluded if the intervention was not tailored at the individual level (e.g. generic in nature or tailored based on shared rather than individual characteristics, e.g. gender tailoring), not delivered online (e.g. delivered in-person), not aiming to change behaviours (e.g. pharmacological), and if the primary aim of the intervention was not specifically for weight loss; however, articles were included if there was more than one main aim, as long as weight loss was stated as one of the aims. Articles were excluded if they stated that the participants had a clinical population (e.g. type 2 Diabetes patients who may have been taking medication to control their condition), or if they were not published in the English language. Authors of studies that met the criteria but did not report the body weight of participants at baseline and follow-up (e.g. reported the BMI only) were contacted in an attempt to include them in the review.
Sources and Searching
Searches were run in December 2016 in five databases, including: EBSCO, Science Direct, Pubmed, EMBASE and Web of Science. Combinations of the concepts ‘tailoring’, ‘eHealth’ and ‘overweight’ were searched as part of the search strategy. For example, EBSCO search included the following combination: TI personalis* OR individualis* OR tailor* OR custom* AND AB (ehealth or e-health or website or web or web-based or website-based or online or Internet) AND SU (overweight or obesity or obese or weight management or weightloss or weight loss or diet* or physical activity). Searches were re-run on 15 March, 2018. An example of the search strategy is included in Supplemental material (Appendix B). Hand-searching was conducted of reference lists of included articles, systematic reviews and meta-analyses of eHealth interventions for weight loss, as well as in the Journal of Medical Internet Research.
Data extraction
Data extraction was conducted by KR. Fifty per cent of the extracted data were checked for accuracy by author SD and 50% by author CL. Two accepted articles had associated adjunctive articles, published separately but reporting details of the development of the tailored eHealth weight-loss intervention. Data from these articles were also included in the extraction and qualitative synthesis, in tandem with the original accepted article. The extracted information included participant information, intervention information and weight-loss outcomes. This included details on study setting; study population and participant demographics and baseline characteristics; details of the tailoring intervention and control conditions; study methodology; recruitment and study completion rates; outcomes and times of measurement; suggested mechanisms of intervention action; and information for assessment of the risk of bias. Specific to the process of tailoring, we identified the individual factors that were assessed as part of the tailoring process, how the assessment was conducted (e.g. what eHealth technology/modes of delivery were used), how often it occurred (e.g. static tailoring or dynamic), how the message output was devised, what specific tailoring and behavioural strategies were implemented, how engagement with the eHealth intervention was conceptualised and measured, whether tailoring increased this and, lastly, whether tailored approaches produced greater weight loss compared with generic or waitlist approaches. Authors were contacted for any missing information.
Data analysis
There were two components to data analysis: qualitative and quantitative synthesis. Qualitative synthesis involved examining how tailoring approaches were conducted within each intervention using information in each article’s intervention description and any corresponding intervention development articles.21,22 As part of this process, terms listed in Harrington and Noar16 were used to identify the tailoring strategies described. These included the following terms: ‘content-matching’ (adapting intervention content based on theoretical determinants), ‘feedback’ (providing messages to individuals about their psychological or behavioural states, which may involve description of objective data back to participant (‘descriptive feedback’), comparing their data to norms (‘comparative-normative feedback’), their previous states (‘comparative-progress feedback’) and providing an interpretation or judgement of their data (‘evaluative feedback’) and ‘personalisation’ where recognisable information relating to the participant is relayed to them, including the use of their name (‘identification’), telling participants that the intervention content has been created especially for them (‘raising expectation of customisation’) and framing messages in a context that is meaningful to them, e.g. through gender-, cultural- or ethnicity-related cues (‘contextualisation’).
Quantitative synthesis involved evaluating the effect of the tailored eHealth interventions on weight loss: effect sizes were calculated to estimate the difference between the intervention and control groups (both active and waitlist controls). Effect sizes for weight change at follow-up assessments were calculated based on the mean pre–post change in the treatment group minus the mean pre–post change in the control group, divided by the pooled pre-test standard deviation (SD).23 In one case, the post-test SD was used as a proxy where the pre-test SD was not reported.24 A pooled SD was calculated using Cohen’s25 formula, squaring the baseline SD of weight of the intervention group and adding the squared baseline SD for weight for the control group, and taking the square root of these. Effect sizes are therefore reported in SD units of change. Changes between the intervention and control were considered to be small (0.2 to <0.5); moderate (0.5 to <0.8) or large (>0.8).25
Quality appraisal
Quality of methodology was assessed by authors KR and SD using the Cochrane Collaboration’s tool for assessing risk of bias for RCTs.26 Bias was assessed as a judgement (high, low, or unclear) in the following domains of bias: selection, performance, detection, attrition, reporting and other bias. In this review, as the outcome of significance was weight, we included an assessment of measurement bias for weight as part of the quality review. Studies using self-reported weight, or using one-off (not averaged) weight measurements were considered to have an increased risk of measurement bias.
Results
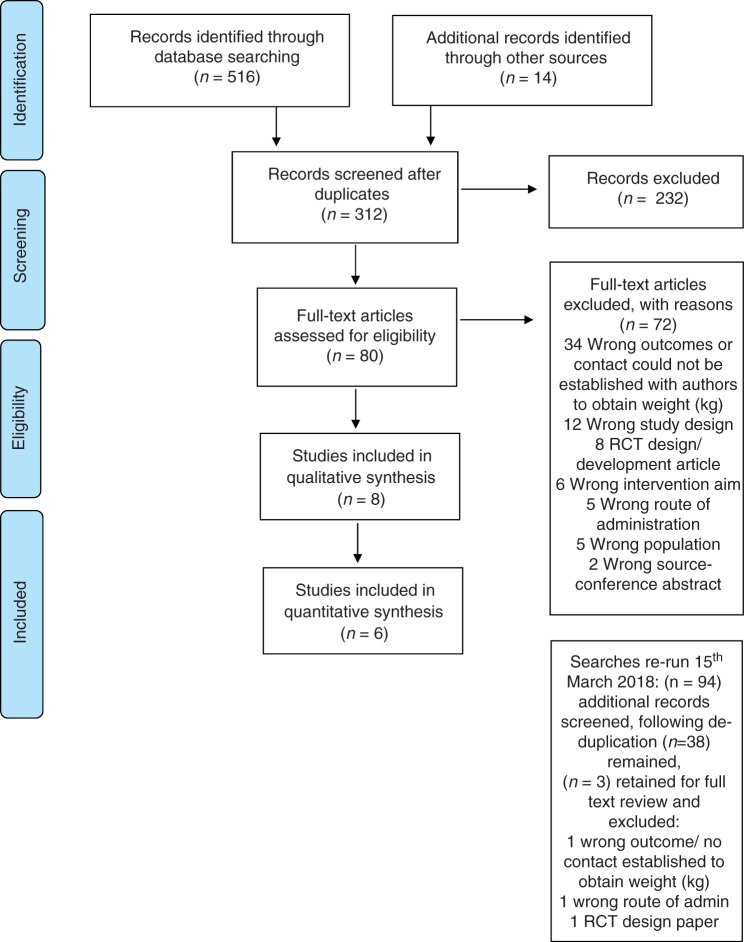
Initially 516 articles were captured in the searches and a further 14 records were identified from hand-searching reference lists of accepted articles and relevant systematic reviews.5,6,8 Following the removal of duplicates (N = 218), there were 312 articles for title and abstract screening, of which 80 were subjected to full text review. Searches were re-run in March 2018, which led to an additional three articles suitable for full text review.27–29 Articles were excluded due to relating to wrong outcomes (e.g. cardiovascular risk, BMI), wrong study design (e.g. review articles, face validity evaluations); being an RCT development article; wrong intervention aims (e.g. aiming to increase physical activity, diabetes prevention); wrong route of administrations (e.g. in-person), wrong population (e.g. those with diabetes mellitus) and wrong source (e.g. conference abstracts). A systematic review of tailored eHealth weight-loss interventions ultimately yielded a total of eight articles,21,22,24,30–34 describing six interventions. See the PRISMA flow diagram below (Figure 1).
Figure 1.
PRISMA flow diagram.
A summary of the included studies is presented in Table 1. There were 14 intervention arms, 2 interventions had three arms, and 4 interventions had two. There were N = 4356 participants (baseline), with 2243 assigned to the intervention groups, and 2113 assigned to the control groups. Participants were recruited from the general population (82.5%), university students (10.5%) and university staff (7%). The mean retention rate to final follow-up was 39.04%. The average age of participants was 37.11, SD = 7.54. Their mean BMI at baseline was 30.06, SD = 4.05. They were mostly female, 82.18% and Caucasian, 56.67%. Studies were published between 2006 and 2016. There were five RCTs30–34 and one randomised pilot study24 with the majority (N = 5) conducted in the USA24,30–33 and one in Europe.34 The intervention durations ranged from 5 weeks to 24 months, with the average length being 24.5 weeks. There was an average of 2.33 follow-ups where participants’ body weight data were collected. Four of the six studies measured weight objectively24,30,33,34 with two relying on self-report methods.31,32 Four out of these six studies compensated participants for taking part.24,30,33,34
Table 1.
Characteristics of eligible studies.
| First author and Year | Article aim | Country | Population (number, participant type, recruitment strategy) and BMI (M, SD) | Intervention (duration; number of follow-ups; retention to final weight measurement) | Comparison | Outcomes (primary and secondary, where stated in article) | Study design |
|---|---|---|---|---|---|---|---|
| Mouttapa et al. (2011) | To evaluate the impact of the Personal Nutrition Planner on dietary intake (dairy, fruit, vegetable intake) and weight loss | USA | 307 female university staff, recruited by email advertisement; BMI: M = 27.72; SD = 6.97 | 5-week duration; two follow-ups (6 weeks; 8 weeks); 85% retentionRegister on study website; fill in online Personal Nutrition Planner questionnaire; receive personalised dietary guidelines; participants self-selected a long-term goal (e.g. lose weight, reduce risk of chronic disease), and short-term action for next 7 days relevant to this. Opt out/in for weekly newsletter with personalised information relating to their goal | Waitlist control; completed three assessments at same time as intervention group evaluating dietary intake, weight | Dietary intake frequencies; weight loss; opinions of intervention (intervention group only) | Randomised control trial (RCT) |
| Tate et al. (2006) | To determine the short-term efficacy of a self-directed Internet weight-loss programme (compared with the same programme supplemented with behavioural counselling from either a computer-automated tailored system or from a human counsellor) | USA | 192 participants recruited from local newspaper; BMI: M = 32.7; SD = 3.5 | 6-month duration; 2 follow-ups (3 and 6 months); 80.7% retentionTwo active intervention groups: computer-automated feedback (CT), or human email counselling (HC)Both HC and CT groups: access to separate website with electronic diary and within group message board, extra weekly email prompting logging of behaviour and educational content (as per the diabetes prevention programme)HC only: weekly feedback via email from health counsellor – unstructured and based on clinical judgement (HCs had behavioural weight-loss experience and degrees in nutrition, psychology, health education, exercise physiology) including answering questions, behavioural feedback on progress towards goals, weight loss feedback, overcoming barriers and motivationCT only: automated feedback based on behaviours from past week – comparative-progress feedback for weight loss, comparative-feedback on calorie goals, consumed and burned compared with individualised diet and exercise goals, behavioural strategies for improving adherence to self-monitoring diet and exercise, overcoming barriers, and motivation or praise depending on logging frequency | Baseline: in-person group session for randomisation; education (principles of behavioural weight-loss, diet, exercise and behaviour change); orientation to website (differed by group), instruction on meal replacement usage (440 kcals – coupons given) with unstructured third meal, increase exercise to 30 mins walking per day, self-monitor diet and exercise; access to website, which provided somewhere to log weight and see graphs of weight, weekly email prompts to report weight, weekly weight loss tips via email, recipes, and a weight-loss e-buddy network system for comparison and peer support for weight loss via email | Weight loss (body weight change); secondary outcomes: dietary intake, exercise | RCT |
| Van Genugten et al. (2012)Design article: Van Genugten et al. (2010) | To evaluate the efficacy of the computer-tailored intervention in weight-related anthropometric measures and energy balance-related behaviours (physical activity; dietary intake) | Netherlands | 539 participants, recruited by local newspapers, flyers delivered door-to-door/in waiting rooms of GP’s/among the employees of four large companies;BMI: M = 28.04; SD = 1.94 | 2-month duration; 2 follow-ups (at 1 and 6 months); 57.8%Log-in name and a password received by email, for access to intervention website. Participants were asked to visit the websites at least three or four times during a 2-month period. They received email reminders to visit the intervention every 2 weeks. At 1 month and 6 months after the intervention period, participants were asked by email to fill out the online questionnaire again.The entire intervention could be finished in 90 minutes; The intervention consisted of four modules, each to be visited 1 week after the previous one and followed the steps of self-regulation.Module 1: weighing up pros and cons of weight gain prevention, identifying and setting a goal for one relevant change in DI or PA and making a plan for change. Participants were made aware of current levels of DI and PA and individualised feedback on their behaviour. Then, people could make a choice for what to change (guided goal-setting) and make a plan for where, when, and how to make that change (implementation plan). The second and third modules were focused around evaluation of progress towards behaviour change, and provided feedback on past week performance. If necessary, it supported adaptation of action and coping plans (when attempts to change behaviour were unsuccessful). The fourth module aimed at promoting sustained self-regulation of body weight without use of the programme. A tool to monitor and evaluate (changes in) body weight was provided, as well as a short guideline with sequences of actions for long-term WGP, reflecting on the self-regulatory skills that had been practised in the previous three modules, and provision of positive reinforcement to maintain behaviour. At the end, the participants signed a personalised contract, which included their personal behaviour goals, actions plans, weight status, etc. The modules were embedded in a website that also contained recipes, a peer-to-peer forum and links to useful websites, and was accessible through the Internet. | Log-in name and a password received by email for access to separate control website. Three web-based educational modules with general information on weight-gain prevention. The first module aimed to increase the motivation for weight management/ prevention. The second module provided information about possible behaviour changes. The third module provided general information about a healthy diet and safe physical activity | Anthropometric: (Body Mass Index, skin folds and waist circumference) and energy balance-related behaviours (physical activity; intake of fat, snacks and sweetened drinks) | RCT |
| Godino et al. (2016); Design article: Patrick et al. (2014) | To assess the efficacy of a 2-year social and mobile intervention designed to reduce weight by improving weight-related behaviours among college students | USA | 404 college students, recruited by print (e.g. newspapers, flyers, posters, magnets) and digital (e.g. emails, electronic bulletins, websites, and Facebook) advertisements; in-person student orientation events;BMI: M= 28.5; SD = 2.75 | 24-month duration; four follow-ups (at 6, 12, 18, 24 months); 84% retention.Access to range of six remote modes of delivery apps, social media networks, website, text/ emails and phone contact with health coaches. Intervention content was tailored to participants’ physical location (e.g. text to determine location and advice depending on answer) and social environment (e.g. whether using apps, Facebook, study website). ‘Tailoring information’ gathered at baseline via Facebook and apps captured participant information (preferred mode of delivery; physical activity and diet goals; preferred frequency and time of tracking, feedback and participation in goal review; health coaches issued feedback on performance and progress towards goals) | Active control: access given to an alternative website to intervention participants (asked to visit once per week) and were sent quarterly newsletters via email with generic health information (no specific behavioural strategies) | Weight (at 24 months) secondary: weight at 6,12,18 months; waist circumference (cm), arm circumference (cm), systolic blood pressure (mm Hg), diastolic blood pressure (mm Hg), heart rate (beats per min), and the level of engagement (ie, amount of use) of the intervention components, physical activity, sedentary behaviours, total dietary intake, eating behaviours relating to weight management, sugar-sweetened beverage consumption, eating away from home, quality of life, depression, self-esteem, body image, psychosocial constructs relating to physical activity and diet, social support and social network composition (Facebook data) | RCT |
| Napolitano et al. (2013) | To examine the feasibility, acceptability, and initial efficacy of a technology-based 8-week weight-loss intervention among college students | USA | 52 college students, recruited in-person and online through websites; BMI: M = 31.36; SD = 5.3 | 2-month duration; 2 follow-ups (at 4 and 8 weeks); 96% retention.(Facebook) + daily text messages with prompt to (a) monitor their behaviours; feedback on performance of self-monitoring (e.g. whether or not they monitored each behaviour, diet only, PAonly, both, or neither);(b) report their behaviours (e.g. text back their daily calories, PA, weight). Participant returns a text response of these, and receives immediate feedback by text (e.g. acknowledgement of submitting self-monitoring data); or (c) address high-risk habits identified at baseline (e.g. late night snacking, liquid calories).Weekly tailored feedback summary reports based on self-monitored PA, calorie and weight data received via text during the week were compiled into personalised reports that summarised progress (included text and visual feedback (graphs) of average weekly weight, calories and physical activity), as well as feedback on progress towards reaching one’s behavioural goals and progress in the skills training for the week, and provided encouragement; identification of support 'buddy' separate to the intervention programme, the buddy received a text when participant was excelling or doing poorly and asked to provide encouragement or support around self-monitoring compliance | Two control groups (active control and wait list control):Facebook group (active control): educational content (handouts/ podcasts);access to polls and healthy activity or eating event invitations (e.g. on-campus farmer’s market, group fitness class, and cycling event) messages via group post or messaging); goal setting for calorie intake based on weight, increase PA;wait list control | Weight loss; secondary: physical activity behaviour; goal setting and planning; physical activity self-efficacy; weight self-efficacy; adapted social support for diet and exercise; engagement/compliance; consumer satisfaction | Pilot RCT |
| Rothert et al. (2006) | To assess the efficacy of a web-based tailored behavioural weight management programme compared with web-based information-only weight management materials | USA | 2,862 Kaiser Permanente members, recruited by letters, newsletters and flyers; BMI: M = 32.05; SD = 3.85 | 6-week duration; 2 follow-ups (at 3 and 6 months); 20% retention.Register on study website and fill in baseline questionnaire (same for both conditions); within 24 hrs, access to respective website (tailored or information-only). The tailored condition employed a tailored expert system (TES) that used 'Balance', a 6-week self-help weight management programme devised on an algorithm using baseline assessment data and links between data elements. The Balance programme creates individually tailored weight management plans, which focus on a healthy diet, behavioural and social cues to eating, physical activity, better understanding of the relationship between food consumption and energy expenditure, calorie and fat consumption, attributions for previous weight management efforts, body image, and social support. Authors provided an example of the tailoring processes: participants who reported greater ability to change diet than physical activity received more dietary advice; specifically cited barriers and lack of efficacy were addressed with messages tailored to those issues. The web-based materials consisted of an initial guide followed by tailored action plans delivered at 1, 3, and 6 weeks into the programme. An email sent to the participants informed them of the availability of the follow-up tailored action plans. Follow-up materials were designed to reinforce dietary and physical activity improvements, address specific barriers and provide support and self-monitoring resources. Participants were allowed to return to any of the materials throughout the course of the study | Access to freely accessible website with weight loss/health information-only and a determination of whether participant was overweight. The programme included an overview and sections related to the importance of weight and weight management; definitions of a healthy weight; determinations of whether the participant is overweight; preparation for weight management; facts about weight-loss diets and programmes; and weight management strategies. Through a menu, the user had the option of selecting any section for viewing and reviewing. They could also view other health topics on the site of their choosing, such as diabetes or asthma. Using this programme, participants were able to create their own educational experience. As in the TES condition, participants were allowed to return to the site throughout the course of the study | Weight-loss percentage; secondary: process measures (whether the user read the information completely, found the information helpful, easy to understand, and personally relevant, and whether they would recommend the programme to others) | RCT |
Note: CT = computer tailoring; HT= human tailoring; PA= physical activity; M = mean; SD = standard deviation; SMS= short message service (text); NR= not reported.
There were two articles considered to be of low risk of bias, three of moderate quality, and one of high risk. Random sequence generation, allocation concealment and blinding of participants and personnel were judged to be adequate strategies in three articles, blinding of outcomes assessment was described in two articles. Five articles were deemed to be low risk in regards to reporting incomplete outcome data. Two articles had published protocols and thus were considered to have a low risk of bias for selective outcome reporting. Two articles relied upon participants’ self-reported weight for their analysis, and this was considered to have a high risk of bias in relation to the measurement and reporting of weight. One was considered to be low risk owing to the inclusion of two objective measurements of weight and taking the average. A summary of the risk of bias results is included in Figure 2.
Figure 2.
Risk of bias graph for quantitative articles (n = 6). (a) Summary of included articles using Cochrane’s Risk of Bias tool. (b) Summary of risk of bias across studies.
How was tailoring implemented?
There were six interventions included in the review, referring to 14 intervention arms, four articles compared computer tailoring to generic information control,24,32–34 or to waitlist control;24,31 one compared human tailoring (devised by human health counsellors) to generic information control;33 one used a combination of computer tailoring and human tailoring30 compared with a generic information control.
Computer tailoring, when feedback is delivered by a system, was implemented through a tailored website devised by Tailorbuilder34 and a tailored expert system.32
What was tailoring based on and how was it gathered? (Tailoring input)
Theoretical models of behaviour change are integral to tailoring and so any difference in theoretical components that provides the basis for the tailoring process may underlie any similarities or differences in intervention outcomes. Four out of six studies mentioned one or more theories that informed the development of the intervention: Social Cognitive Theory;31 Cognitive Behavioural Theory;33 Self-Regulation Theory, the Theory of Planned Behaviour, the Precaution Adoption Process Model;34 and Behaviour Change Theory comprising Social Cognitive Theory, Control Theory, Operant Conditioning, Ecological Theory, and Social Network Theory.30 Tailoring was based on anthropometric data and personal characteristics including age, height, weight, gender,31,32 family history and prior weight-loss experience;32 behaviours including dietary factors, e.g. calories, level of physical activity,24,30–32,34 theoretical concepts such as future weight goals,31,32,34 physical activity and diet goals,30 advantages and disadvantages of weight management, confidence and willingness to change behaviours,34 physical location,30 whether self-monitoring occurred;24 high-risk habits,24 health-related habits, barriers to physical activity; as well as a range of psychosocial characteristics around stress management, attitudes to overweight people, comfort eating, and sources of motivation to lose weight, among others32 (see Table 2 for further details).
Table 2.
Summary table of tailoring methods.
| Study author, year and title | Theory stated and behavioural principles | How tailoring conducted; when; how often | Tailoring based on … | Tailored output: type and mode of delivery | Engagement |
|---|---|---|---|---|---|
| Mouttapa et al., 2011The Personal Nutrition Planner: A 5-week, computer-tailored intervention for women | Social Cognitive TheoryEducation on diet and nutrition; goal setting (long- and short-term); self-efficacy (identifying short-term goal over next 7 days); provision of facilitators of diet change: shopping list; meal planner; recipe suggestions; advice for overcoming barriers | Static computer-tailoring via online questionnaire at baseline | Input 1: age, height, weight, sex, level of physical activity, and weight goals | Output 1: participants’ body mass index and estimated energy expenditure are calculated (evaluative feedback)Output 2: specific nutrition information using MyPyramid guidelines used to recommend amounts for all food groups and how nutrients in each food group benefit health (Content-matching); mode: website.Output 3: personalised newsletter based on their selection of long-term and short-term goals (content-matching, self-tailoring/customisation),mode: (if opt in) emailed newsletter | Not explicitly defined.Registration rate of intervention group to access intervention profile: 79%. Questionnaire for opinions of the intervention (not given to control) |
| Tate et al., 2006A randomised trial comparing human email counselling, computer-automated tailored counselling, and no counselling in an Internet weight-loss programme | Cognitive Behavioural TheoryEducation (principles of behavioural weight-loss: diet exercise and behaviour change); orientation to website (differed by group); instruction on meal replacement usage (440 kcals: coupons given) with unstructured third meal; increase exercise to 30 mins walking per day; self-monitor diet and exercise | Dynamic tailoring (weekly) via participants logging to a web-based diary Either computer-tailoring (CT) or human tailoring (HT), depending on intervention condition | Web-based diaries, including weekly weight, daily caloric intake, use of meal replacements and exercise | Human-tailoring group: weekly feedback – unstructured and based on clinical judgement (counsellors had behavioural weight-loss experience and degrees in nutrition, psychology, health education, exercise physiology) including answering questions, behavioural feedback on progress towards goals and weight loss (comparative-progress feedback; evaluative feedback), overcoming barriers and motivation.Mode: email.Computer tailoring: automated feedback based on behaviours from past week (comparative-progress feedback and evaluative feedback) for weight loss and calories consumed and burned compared with individualised diet and exercise goals, behavioural strategies for improving adherence to self-monitoring diet and exercise, overcoming barriers, and motivation or praise depending on logging frequency (evaluative feedback). Mode: website | Not explicitly defined. Log-in frequency and site component usage (number of weeks of online diary submission)Median no. of total log-ins to website. Control=34; CT=20; HT= 32.5 timesThose in the HT group submitted diaries for 17.2 weeks (SD=8.7) more than the CT group, 11.4 weeks (SD= 9.2), p<0.001Online diary submissions associated with greater weight loss for both active intervention groups (HT:r= –0.56; CT: r= –0.69, p <0.001) |
| Van Genugten et al., 2012Results from an online computer-tailored weight management intervention for overweight adults: randomised controlled trial | Self-Regulation Theory; Theory of Planned Behaviour; Precaution Adoption Process Model.Based on main steps for self-regulation for weight control: self-monitoring (weight, diet and PA), goal setting, action planning, evaluation, adaptation); aimed to support decision making/goal setting around behaviour change; comprised education about behaviour-health link; a review of current behaviours and feedback; social support and peer modelling; support intention formation; prompt cues; decisional balance; behavioural feedback; support for preparing and enacting behaviour change: action planning; analysing lapses in behaviours; relapse prevention; coping planning; behavioural contract | Dynamic computer-tailoring (asked to visit website every 2 weeks) Tailored website made using TailorBuilder software | Module 1: Input 1:assessments based on personal details and future weight goals; Input 2:assessment of personal advantages and disadvantages of weight-gain prevention; Input 3: assessment of confidence and willingness for weight-gain prevention; Input 4: assessment of diet and PA; Input 5: goal-setting tool and preparation tool.Modules 2 and 3: Input 1: assessment of weight and behaviours over past week; Input 2: assessment of high-risk situations in past or future; Input 3: when insufficient perceived behavioural control.Module 4: Input 1: assessment of weight; Input 2: asked to describe their personal rewards when goals are accomplished | Module 1:Output 1: graphs depicting weight history and predicted weight (comparative-progress feedback; evaluative feedback); tailored feedback on participants’ reasons for weight management and alternate views, instruction to consider both and reweigh pros and cons.Output 2: feedback decisional balance of advantages and disadvantages (descriptive feedback;content-matching); Output 3: if not confident to change behaviour receive a peer story; if not willing, anticipated regret (content-matching); Output 4: feedback on diet and PA and recommendations for change (evaluative feedback); Output 5: overall module output: summary and tailored plan.Modules 2 and 3: Output 1: factual and visual feedback on performance (comparative-progress feedback; evaluative feedback); if poor performance, decisional balance on old/new behaviours; if negative feelings reported about the person/their change, output was discussion of their feelings during failure and replacing them with positive feelings (descriptive feedback; content-matching); Output 2: guided, situation specific coping plan (content-matching); Output 3: option to change behaviour goal (self-tailoring/customisation); overall modules 2 and 3:Output 4: summary of coping plan.Module 4: Output 1: written and visual feedback on weight progress (comparative-progress feedback;); personalised normal weight range (evaluative feedback); Output 2: personal reward plan (personalisation); Output 3: overall module output: personalised certificate (identification).Mode: website | Not explicitly defined.Log-in data for each intervention moduleTailored vs control: Visited Module 1: 93.3% vs 81.5%; Module 2: 74.1% vs 66.7%; Module 3: 26.7% vs46.1%, Module 4: 15.2% (no generic Module 4)Process measures:(item-specific rating scale, summary of differences reported): Tailored group rated intervention as morepersonally relevant and novel than those receiving the generic information, ps<0.01, but read less of the information, p<0.001, and perceived the length of the information as less appropriate than those in the generic group p =0.01. There was no differenceamong groups in their ratings of usefulness of the information, attractiveness of the design, appreciation of the tool, whether they would recommend to others, and overall rating |
| Godino et al., 2016;Patrick et al., 2014Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): a 2-year, parallel-group, randomised, controlled trial | Abraham and Michie (2008) taxonomy of 26 behaviour change techniques (which they cite draws on: Social Cognitive Theory; Control Theory; and operant conditioning); Ecological Theory; Social Network Theory.Intention formation, goal setting, self-monitoring, feedback, and goal review; techniques to increase self-efficacy for diet and physical activity, relay the benefits of, and remove barriers to, healthy changes in physical activity and diet; blog posts that were educational; Patrick (2014) adds: social support and accountability (friends, participants, health coach via social network); formation of healthy social norms about health weight-related behaviour; location based support and prompts; problem solving | Dynamic tailoring (daily/weekly). Combination of computertailoring and human tailoring.Unclear specifically when and how due to flexible nature of intervention delivery: choice of six modes including Facebook, three study-designed mobile applications, text messaging, emails, a website with blog posts, and technology-mediated communication with a health coach (up to 10 brief (5–15 min) interactions) | Input 1: physical location; Input 2: physical activity and diet goals; preferred frequency/time of tracking, feedback and participation in goal review; Input 3: physical activity, diet and weight | Output 1: text relaying behaviour-change information according to where the participant was (e.g. at home or university-based exercise) (location-tailoring). Mode: text.Output 2: customisation of programme delivery according to preferences (self-tailoring/customisation).Output 3: Trend-setter app-issued automated feedback (comparative-progress); health coaches issued feedback on self-monitored physical activity, diet and weight-performance and progress towards goals and usage of intervention modes (e.g. apps and Facebook) (comparative-progress feedback; evaluative feedback; contextualisation of health messages by time of year).Mode: text, apps, Facebook, website, instant messenger, telephone call, or video call | Engagement operationalised as: sum of a participant’s recorded interactions on the study Facebook page (e.g. a post, comment, or like) and mobile apps (e.g. entry of the number of steps taken per day), text messages sent and replied to, and communication with the health coach between each study measurement.Intervention group: median (inter-quartile range) = 98 (9–265) interactions at 6 months, 76 (0–222) at 12 months, 41 (0–198) at 18 months, and 12 (0–161) at 24 months. Control: NR |
| Napolitano et al., 2013Using Facebook and text messaging to deliver a weight-loss programme to college students | None stated.Goal setting (weight-loss goal set with study staff member); self-monitoring (given advice on how, given tools including scales, book and pedometer, measuring utensils), and social support (via their selected non-study-related ‘buddy’ and daily text messages); educational content sent weekly via handout/ podcast, video demonstrations, one topic per week, topics of: self-monitoring and navigating campus; planning and nutrition; internal vs external hunger and eating triggers; physical activity; stress and distorted thinking; social support; special occasions, dining out and holidays; relapse prevention | Dynamic tailoring (daily/ weekly) Unclear how devised – appears to be automated/computer-tailored feedback (via daily text and weekly summary report) (‘messages were programmed at random intervals’ p. 26) | Input 1: whether they monitored (general and behaviour specific, e.g. diet and PA) on that day; Input 2: daily PA, calories, and weight; Input 3: baseline reported high-risk habits | Output 1: feedback on performance of self-monitoring (e.g. whether or not they monitored each behaviour, diet only, PA only, both, or neither) (descriptive feedback); Output 2: immediate feedback by text (e.g. acknowledgement of submitting self-monitoring data); (descriptive feedback); Output 3: advice on habits (e.g. late night snacking, liquid calories); Output 4: weekly tailored feedback summary reports (based on collated Input 2), which are compiled into personalised reports that summarised progress (included text and visual feedback (graphs) of average weekly weight, calories and physical activity), as well as feedback on progress towards reaching one’s behavioural goals and progress in the skills training for the week (evaluative feedback; comparative-progress feedback).Mode: SMS message, external link to secure page accessed via Facebook | Level of engagement was examined for the Facebook groups (intervention group and active control) by quantifying the number of times participants ‘liked’ a study-related post, posted a comment, and RSVP’d to an event. Active control: 4/17 participants 'liked’ study-related posts (M=1.25 likes each); 7/17 commented on study-related content at least once (M=3.05 posts per commenter); 15/17 responded to event invite (average RSVPs, M=6.54).Intervention group: 4/18 ‘liked’ study-related posts (M= 1 like each); 14/18 posted on study-related content at least once (M = 1.3 posts per commenter); 13/18 responded to event invitations (M=8.56 RSVPs of those who responded);79.7% of all general monitoring texts receiving a response |
| Rothert et al., 2006Web-based weight management programmes in an integrated health care setting: Arandomised, controlled trial | None stated.Social support (optional participant-nominated 'buddy' who received email prompts to provide support); educational content (initial guide); action plans (weeks 1, 3 and 6); positive reinforcement of dietary and physical activity improvements, address specific barriers, and provide support and self-monitoring resources | Static computer-tailoring algorithm (tailored expert system): Balance a self-help weight management programme developed by HealthMedia, Inc.) via baseline questionnaire | Input: demographic information; personal and family health history; former weight-loss experiences (including former use of specific weight-loss treatments and outcomes from weight-loss attempts); general self-care activities (including tobacco, physical examinations, flossing, seat belt use, and stress management); physical activity, ability to be physically active, and barriers to being physically active; perceived difficulty in controlling diet and physical activity; worry regarding body image; barriers to weight management; psychosocial stress and coping; general dietary preferences (e.g. consumption of alcoholic beverages, desserts, fast food, high-fat dairy products, fried food); foods typically consumed when stressed; weight-loss goals and motivation to lose weight; source of motivation (e.g. personal choice, pressure from others); a typological assessment of eating behaviour (e.g. whether the subject eats in response to certain emotions, restricts food intake, then eats because of hunger, etc.); attitudes regarding overweight individuals (e.g. that they lack willpower, are unattractive, cannot be physically fit, etc.); weight-related self-efficacy; weight-loss expectations (e.g. looking and feeling younger, reducing risk of disease, having clothes fit better, reassuring others, getting people to stop nagging them to lose weight, etc.); and perceived social support | Output 1: an individually tailored weight management plan in line with behavioural strategies, e.g.participants who reported greater ability to change diet than physical activity received more dietary advice; specifically cited barriers and lack of efficacy were addressed with messages tailored to those issues (content-matching).Output 2: tailored action plans delivered at 1, 3 and 6 weeks into the programme to reinforce initial plan (content-matching). Mode: website | Not explicitly defined. Process measures (% positive): tailored vs control Read information completely 82% vs 67%; materials helpful 75% vs 57%; information easy to understand 93% vs 82%; materials were personally relevant 78% vs 61%; would recommend programme to others 75% vs 59%, all ps =0.0001 |
Note: CT = computer tailoring; HT= human tailoring; PA = physical activity; M = mean; SD = standard deviation; SMS= short message service (text); NR= not reported.
Tailoring input, which provided the basis for the process of tailoring was gathered using online questionnaires at baseline,31,32 web-based diaries,33 via purpose-built tailored website,33 study-designed mobile applications,30 SMS messaging,29 Facebook, and emails from a remote health coach.30
Self-tailoring or ‘customisation’15 reflected personal preferences, and was based on desired features, e.g. whether they wanted a newsletter,31 their desired intervention mode of delivery,31 and how often users wanted feedback, tracking and goal reviews.30
How was tailoring conducted? Computer tailoring
Dynamic tailoring (based on dietary or physical activity behaviours or weight, self-monitoring status or location) was conducted through daily and/or weekly input24,30,33 or less regular input and based on theory, e.g. recommended every two weeks34 or a self-determined pattern of tracking and feedback.30 Static tailoring involved a process of distributing an online questionnaire at baseline.31,32
Two tailoring approaches were explicitly named and described: a tailored website34 and a tailored expert system.32
One intervention delivered computer-tailored feedback and human tailoring via health coaches who also delivered feedback,30 and whether or not participants received the intervention depended on the usage of these components. In the other instance, daily feedback appeared to be automated as messages were programmed and feedback was immediate, however it was not explicitly stated who or what devised the weekly personalised messages; an automated system appeared to have gathered daily behavioural data and this was provided to participants through a secure link delivered by Facebook message.24 The computer-tailored feedback in Tate and colleagues’ study33 was based on the participants’ responses and matched with a response from a bank of messages previously devised by experts; a series of decision rules ensured that automatically generated feedback was provided on the webpage.
As an example of an in-depth level of computer tailoring, Rothert et al.32 described the action of the tailored expert system in their intervention:
participants reporting a family history of a particular disease received information regarding the connection of obesity to this class of diseases; participants who reported greater ability to change diet than physical activity received more dietary advice; specifically cited barriers and lack of efficacy were addressed with messages tailored to those issues; psychosocial stress was compared with reported coping abilities and accompanied with tailored stress management advice; and participants who reported that overweight individuals lacked willpower were given messages attempting to change this perception to a more controllable, external attribution (p. 268).
Human tailoring
Tate et al.33 drew on human tailoring by human counsellors who had behavioural weight-loss experience and degrees in nutrition, psychology, health education, and exercise physiology. Feedback was based on their clinical judgement in interpreting the participants’ self-reported weekly weight, daily caloric intake, use of meal replacements and exercise, in their electronic, web-based diaries on the study website. The content of feedback for approaches involved comparative-progress feedback for weight, comparative-progress feedback on calorie goals consumed and burned compared with individualised diet and exercise goals, behavioural strategies for improving adherence to self-monitoring diet and exercise, overcoming barriers, and motivation or praise depending on logging frequency. This detail was not provided in the other study.21,30 Based on the description provided we determined that feedback was based on app usage, behaviours and progress to goals.
How tailored interventions were delivered
A range of modes were used in the delivery of tailored interventions. Websites were used in all studies.24,30–34 Two used SMS messages as well as Facebook.24,30 Two studies used humans to tailor information: one used health counsellors who contacted participants via email33 and one used health coaches who could instant message, telephone or video-call participants.30
Type of Tailored Strategies and Output
Tailoring strategies were identified from the descriptions in the articles. Content-matching,31,32,34 evaluative feedback,24,30,31,33,34 descriptive feedback,24,34 and comparative-progress feedback,24,30,33,34 identification,34 contextualisation,30 as well as self-tailoring (customisation)30,31,34 and personalisation34 were implemented by a range of eHealth systems. Location-tailoring was also used.30
Output typically consisted of feedback on weight loss, physical activity and diet (e.g. calories burned and consumed) compared with individualised diet and exercise goals.24,30,31,33,34 Visual graphs of progress, behavioural feedback, differential behaviour-change strategies, personalised certificates and personal reward plans were also delivered to participants.34 Output also included a personalised nutrition plan and newsletter around their goals.31 Feedback on behaviours such as daily self-monitoring also featured,24 as did a weight management plan with behavioural strategies (e.g. action plans) matched to the individual.32
Did tailoring work to increase engagement?
Four studies did not explicitly define engagement within the context of their intervention. As such, there was no consistent method of conceptualising and measuring engagement with eHealth interventions. Some studies reported usage metrics such as number of log-ins or use of eHealth features e.g. web-based behavioural diary,33 registration to a website,31 while others used process evaluations using subjective participant reports of amount of provided material read.32 One study drew on both online module visits and subjective process measures.34
Engagement was explicitly defined in Godino et al.27 and also in Napolitano et al.24 Godino et al.30 defined it as the sum of a participant’s recorded interactions on the study Facebook page (e.g. a post, comment, or like) and mobile apps (e.g. entry of the number of steps taken per day), text messages sent and replied to, and communication with the health coach between each study measurement. Napolitano et al. defined engagement as the number of times participants ‘liked’ a study-related post, posted a comment, and RSVP’d to an event.24 Tate and colleagues30 examined log-in frequency and number and use of online diary submissions, counting the number of weeks where behavioural diaries were submitted.
Two articles conducted a process evaluation, capturing participants’ subjective views of the intervention through self-report questionnaires.32,34 Rothert et al.32 reported that the tailored group responded more favourably than the information-only group for each item, including reading the intervention information completely; rating the materials as more helpful, more personally relevant, and easier to understand; and reporting that they would recommend programme to others, all ps = 0.0001. In research by van Genugten et al.34 the tailored intervention group also perceived the material to be more personally relevant, and found content to be more novel than those in the generic information group, ps < 0.01, but contrastingly reported that they read less of the information, p < 0.001. They perceived the length of the information as less appropriate than those in the generic group, p = 0.01. There was no difference among groups in their ratings of usefulness of the information, attractiveness of the design, appreciation of the tool, whether they would recommend it to others, and overall rating.
Did tailoring support weight loss compared with control conditions?
A summary of the intervention groups compared with the controls is provided in Table 3.
Table 3.
Summary table of results of included studies on weight loss.
| Baseline body weight (kg) |
Follow-up(months unless otherwise stated) |
Follow-up body weight (change in kg) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Int |
Control |
Int |
Control |
|||||||
| M | SD | M | SD | M | SD | M | SD | Effect size (d) | ||
| Mouttapa et al., 2011 | 71.7 | 17.43 | 74.91 | 21.42 | 6 weeks | ↓0.59 | 2.12 | ↓0.29 | 5.02 | –0.02 |
| Tate et al., 2006 | CT = 89; HT = 89 | CT = 13.2; HT = 13 | 88.3 | 13.9 | 3, 6 | 3 months: CT = ↓5.3; HT = ↓6.16 months: CT = ↓4.9; HT = ↓7.3 | 3 months: CT = 4.2; HT = 3.9 months: CT = 5.9; HT = 6.2 | 3 months: ↓2.86 months: ↓2.6 | 3 months: 3.5; 6 months: 5.7 | 3 months:CT vs C = –0.19**; HT vs C = –0.26**; (no dif CT vs HT)6 months: CT vs C = –0.17; HT vs C = –.35***(HT>CT) |
| van Genugten et al., 2012 | 83.39 | 11.49 | 83.34 | 10.61 | 1 (NR); 6 | ↓0.34 | 12.36 | ↓0.6 | 10.81 | 0.02 |
| Godino et al., 2016 | 76.5 | 12.7^ | 76.5 | 13.2^ | 6, 12, 18, 24 | 6 months = ↓1.1; 12 months = ↓1; 18 months = ↓0.3; 24 months = ↑0.3 | NR | 6 months = ↑0.3; 12 months = ↑0.3; 18 months = ↑0.4; 24 months = ↑1.1 | NR | 6 months: –0.11*12 months: –0.1**18 months: –0.05 24 months: –0.06 |
| Napolitano et al., 2013 | NR | NR | NR | NR | 1; 2 | 1 month = ↓1.72 months = ↓2.4 | 1 month = 1.6; 2 months = 2.5 | 1 month: AC = ↓0.46; C = ↑0.28; 2 months: AC = ↓0.63; C = ↓0.24 | 1 month:AC = 1.4; C = 1.72 months: AC = 2.4; C = 2.6 | ^^1 month: T vs AC = –0.5*; T vs C = –0.79***;2 months:T vs AC = –0.71*; T vs C = –0.86* |
| Rothert et al., 2006 | 92.2 | 14.4 | 92.5 | 14.3 | 3; 6 | 3 months = ↓2.6; 6 months = ↓2.8 | NR | 3 months = ↓1.4; 6 months = ↓1.1 | NR | 3 months = –0.1***; 6 months = –0.12*** |
Note: ^raw standard deviation reported; ^^ follow-up SD used to calculate effect size; *p < 0.05 **p < 0.01, ***p < 0.001. CT = computer tailored; C = control; HT = human tailoring; T = tailored intervention; AC = active control; NR = not reported.
Four out of six articles found positive effects for tailoring on weight loss when compared with generic or waitlist controls.24,30,32,33 Two articles found no difference between the intervention and control (waitlist31 and generic information34). Follow-up time points ranged widely from 1 month to 24 months.
The effect sizes denoting the mean difference in weight between intervention and the control groups ranged from −0.02 to −0.86 but in general are very small to small.25 In the only article that compared tailoring types, there was no difference between human tailoring and computer tailoring at 3-month follow-up; both resulted in statistically significant weight loss compared with the control group. However, at 6 months, human tailoring was still effective in producing weight loss compared with the control, but this was no longer the case for computer tailoring.33 Napolitano et al.24 found the largest effect between the tailored vs waitlist control conditions, d = −0.86, followed by the difference between the tailored and generic information, d = −0.71.
Godino et al.30 found a significant difference between groups at 6 month and 12 month follow-ups, with the tailored intervention resulting in 1.33 kg more weight loss than the general information control at both 6 and 12 months (p < 0.05), but there was no significant difference at 18 or 24 months, where ultimately the effect size at 24 months was −0.06. Rothert et al.32 found a significant difference between groups at 3 and 6 months, (mean weight loss for the tailored groups = 2.6 and 2.8 kg, respectively, ps < 0.001) favouring the intervention group, which used a tailored expert system.
Discussion
Summary of key findings
A systematic review of tailored eHealth weight-loss interventions was conducted on six interventions, outlined in eight published articles, to describe how tailoring was implemented, and whether it was effective in producing weight-loss. Tailored interventions were found to be more effective in supporting weight loss than generic or waitlist controls in four of the six articles. Effect sizes were very small to moderate, with evidence of fluctuations in effect sizes and differences of effect between tailored and non-tailored interventions, and between tailoring types, over time.
We note the diversity of approaches, input and technology used in tailored interventions; tailoring included a range of approaches including computer tailoring (using purpose-built tailored websites e.g. using TailorBuilder34 and tailored expert systems32), human tailoring (by remote trained health counsellors33) and a combination of the two techniques.30 Tailoring was based on a range of inputs, including anthropometric data (e.g. weight) and personal characteristics (e.g. age, prior weight-loss experience), behaviours (e.g. dietary intake, physical activity), goals (e.g. weight goal), theoretical determinants (e.g. confidence/willingness to change behaviours) psychosocial factors (e.g. stress management, social support) and location. A range of tailoring strategies was implemented, including evaluative- and comparative-progress feedback and content-matching, as outlined by Harrington and Noar.16
Tailoring input was gathered using a variety of technological modes and included static processes of data collection from online questionnaires at baseline.31,32 Dynamic processes also occurred where rolling input was gathered from web-based diaries,33 via a purpose-built tailored website,34 study-designed mobile applications30 and SMS messaging.24 Conceptualisation of engagement with tailored interventions was not uniformly defined. Our findings suggest that tailored materials were rated by participants as more personally relevant, more helpful, easier to understand, more likely to be recommended to others, and more novel than those in the generic information group.
The first goal of this review was to describe how tailoring was implemented in eHealth interventions. We have described a range of methods, inputs and technology used as part of tailored interventions. Previous reviews describing eHealth interventions have also found heterogeneity in approaches, so this was no surprise given the ubiquity of the Internet and the range of delivery options it affords.5,6 With this advance in delivery methods comes new opportunities for tailoring health information, and we have found that tailoring is being increasingly used in innovative ways. However, if we are to build the science of tailoring it is imperative that the strategies reported in existing tailoring specification efforts15,16 are used. In addition, the input or basis for tailoring should be specified as well as who/what devises tailoring output.
In this vein, our review has attempted to describe the range of tailoring approaches delivered by eHealth means. In Kreuter’s35 much cited original definition, tailoring is defined as the provision of individualised information, advice and support based on the participant’s known characteristics, behaviours or scores on relevant theoretical constructs. To aid the conceptualisation of tailoring in this context, we devised a model of tailoring depth, which we refer to as deep- and surface levels of tailoring (see Figure 3). This model is by no means exhaustive but we feel it is a step in the right direction in terms of differentiating between types of tailoring input to provide the basis for tailoring. It incorporates concepts discussed by Resnicow et al. in developing culturally sensitive public health interventions.36 These concepts include surface structures, in other words relating to observable or behavioural characteristics of a population, and deep structures, relating to psychosocial, cultural and historical factors of a target population. This model indicates the distinctions made when the process of tailoring is based on behaviours or observable factors and when it is based on theoretical constructs, and allows for a combination of these. This builds upon Morrison’s assertion that tailoring strategies can range from relatively simple e.g. employing the user’s name, to the more complex, e.g. adapting content to personally relevant variables.14 Deep-level tailoring refers to tailoring message content based on theoretical determinants of a specific health outcome, and the content that is delivered aims to modify these through strategies, for example like content-matching and evaluative feedback. In our review, input for deep-level tailoring was captured using a questionnaire at baseline (static tailoring).32 For example, participants who reported a greater ability to change their diet at baseline compared with those who reported greater ability to change their physical activity received more dietary advice.32 Deep-level tailoring was also conducted in a dynamic manner, gathering theory-based input via modules, using more than one assessment point, in order to ensure the intervention remained suitable to the needs of participants.34 This is referred to as ‘re-tailoring’ where new information from participants is obtained and feedback given at follow-up time points.37 It was recently found that participants disengage from eHealth interventions because they believe they are no longer relevant to them and their needs.38 As such, a more continuous process of adapting and delivering content to the individual may be a promising route.
Figure 3.
Model of tailoring depth.
Surface-level tailoring is a more concrete but simpler process, when tailoring is based on participants’ (ongoing) self-reported behavioural data, e.g. amount of physical exercise or dietary intake, and evaluative or comparative-progress feedback is delivered on this basis with the aim of keeping participants on-track with their behavioural goals. We suggest that this type of tailoring is no less important, but is conducted on the basis of behaviours or observable factors, typically relying on more frequent input (e.g. daily or weekly). This process aligns with self-regulation theory in that it enables the participant to learn to self-monitor and regulate their behaviour in line with their goals.39 There may be a fundamental difference in the mechanisms at play behind this tailoring approach compared with deep-level tailoring, but this will need to be tested empirically in future research.
Tailoring may initiate processes of behaviour change, and it is possible that these processes in turn influence the efficacy of, and engagement with tailored interventions. Dynamic processes of tailoring, including movement between surface and deep level, or by tailoring type (e.g. human or computer), must be examined in relation to the efficacy of the intervention. For example, in the only study to examine human vs computer tailoring, both of these groups were effective at 3-month follow-up, however at 6 months, the human-tailoring group had significantly greater weight loss than the control.33 This indicates the possibility that over time, the effects of tailoring will vary, and this variation may be related to an interaction on intervention-type by intervention-time. For example, at some intervention phases it may be more effective for a computer-tailored vs a human-tailored intervention to be implemented. This is linked to the suggestion that interactivity should be considered in developing effective eHealth interventions.9 This also highlights the concept of engagement, an under-considered factor in the research design or assessment of factors influencing intervention efficacy. We note that engagement was not explicitly defined in the majority of included studies (N = 4), and among those that did, it was conceptualised in a variety of ways mostly in relation to interaction with study-related content but also through process evaluations of the interventions.
This is in line with how engagement has been conceptualised in eHealth interventions – in terms of both participant experience and behaviours.40 Future efforts to examine tailoring in eHealth interventions should measure engagement both in terms of participants’ objective usage of intervention components (e.g. behavioural- through log-in metrics, usage data) and subjective experience (e.g. through process evaluations, participant interviews or surveys). This will enable an assessment of the extent to which tailoring (and indeed other intervention features and components) works the way it is theorised to (e.g. via mechanisms of increasing attention, increasing self-referential thinking15) and will provide a platform for future efforts to develop enhanced tailoring approaches addressing these mechanisms.
The second aim of the review was to establish whether tailored eHealth interventions result in weight loss compared with a generic control. Effect sizes were modest, comparable to other reviews in health behaviour change.10,17 However, it has been shown that modest weight loss (3–5% of pre-test body weight) is enough to have a beneficial health impact, e.g. reducing blood pressure, HbA1c, triglycerides and LDL cholesterol41 and so, even modest effects are desirable.
Four out of the six studies found beneficial effects for the tailored arm of eHealth weight-loss interventions. The two studies that found no effect were less intensively focused on weight loss, as both had a further aim in addition to weight loss, with Mouttapa et al. aiming to additionally provide a dietary intervention31 and van Genugten et al. to also prevent weight-gain.34 While they met the criteria for the study, these findings suggest that the intensity of the intervention plays a key role, for example, in the study by van Genugten et al., even though the intervention was rigorously developed using behaviour change theory, the intervention could be finished within 90 minutes.34 This may suggest that though tailoring was not found to be successful in that case, it may have been that the behavioural ‘dose’ of the intervention was not high enough. The other studies suggest that the effect of tailored eHealth interventions for weight loss is effective up until 1 year with no evidence at follow-up after this point.
Limitations
The number of completed studies using tailored strategies and the Internet to support weight loss in our results belies the number of studies available for review. Despite significant effort, we were unable to secure data on weight for four studies, as weight was not reported in the published record or provided on request, and our results must be considered in this context.
Our review featured participants predominantly from the general population (82.5% of participants) and this suggests that effective tailored approaches can be delivered via the Internet in a scalable manner for weight loss. However, we did not include interventions addressing weight-loss maintenance or weight-gain prevention as part of this review, which are also important foci for population-wide obesity strategies. We note that these are important areas deserving of research attention, however interventions that address these aims differ in intensity to those addressing weight loss and so we advise a delineation of behaviour type to explicate if and how tailoring is effective. The use of tailored eHealth tools in weight-gain prevention and weight-loss maintenance should be examined in future work as we attempt to support both those at risk of becoming overweight and those who need to maintain weight loss in a cost-effective, scalable and effective manner.
Conclusions
eHealth interventions for weight loss are promising in terms of being scalable and effective,7 but it is necessary to find strategies that help eHealth interventions channel the effectiveness of traditional in-person behavioural counselling approaches.2,7,42 Tailoring is one approach that shows promise. We have found tailoring to have a small but beneficial effect on weight loss in four out of six studies in this review, yet tailoring approaches varied considerably even for one clearly defined health outcome (weight loss) and mode of delivery (Internet). To ameliorate this going forward and to build on previous research, we propose a model of tailoring depth, suggesting that there may be conceptual differences in tailoring approaches. Concepts of deep- vs surface-level tailoring could be tested experimentally to assess the mechanisms or effects of tailoring on the basis of input type, be it theoretical determinants, behavioural input or other tailoring input type. In order to develop the science of tailoring within the domain of eHealth interventions for behaviour change, it is vital to improve research designs (e.g. use tailoring vs generic control group) and methodologies (e.g. use the tailoring strategies and guidelines recommended in this field)16 and in the wider domain of health behaviour change (e.g. by reporting behaviour-change techniques).43
Supplemental Material
Supplemental material, Supplemental Material1 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health
Supplemental Material
Supplemental material, Supplemental Material2 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health
Supplemental Material
Supplemental material, Supplemental Material3 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health
Supplemental Material
Supplemental material, Supplemental Material4 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health
Conflict of interest
There are no conflicting interests related to this research.
Contributorship
KR and SD conceived the study and devised and piloted the search strategy in consultation with CL. KR and SD conducted title and abstract screening and full text review. KR conducted data extraction and CL and SD checked this for accuracy. KR and SD completed the quality review. KR wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Funding
This work was supported by the Irish Research Council [grant number EPSPG/2016/182].
Guarantor
SD
Peer review
This manuscript was reviewed by two individuals who have chosen to remain anonymous.
Supplementary Material
Supplementary material is available for this article online.
References
- 1.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384: 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Looney SM, Raynor HA. Behavioral Lifestyle Intervention in the Treatment of Obesity. Health Serv Insights 2013; 6: 15–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eysenbach G. The law of attrition. J Med Internet Res 2005; 7: e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hutchesson MJ, Rollo ME, Krukowski R, et al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obes Rev 2015; 16: 376–392. [DOI] [PubMed] [Google Scholar]
- 6.Arem H, Irwin M. A review of web-based weight loss interventions in adults. Obes Rev 2011; 12: e236–e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology 2007; 132: 2226–2238. [DOI] [PubMed] [Google Scholar]
- 8.Neve M, Morgan PJ, Jones PR, et al. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev 2010; 11: 306–321. [DOI] [PubMed] [Google Scholar]
- 9.Sorgente A, Pietrabissa G, Manzoni GM, et al. Web-based interventions for weight loss or weight loss maintenance in overweight and obese people: a systematic review of systematic reviews. J Med Internet Res 2017; 19: e229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lustria MLA, Noar SM, Cortese J, et al. A meta-analysis of web-delivered tailored health behavior change interventions. J Health Commun 2013; 18: 1039–1069. [DOI] [PubMed] [Google Scholar]
- 11.Noar SM, Grant Harrington N, Van Stee SK, et al. Tailored health communication to change lifestyle behaviors. Am J Lifestyle Med 2011; 5: 112–122. [Google Scholar]
- 12.Lustria ML, Cortese J, Gerend MA, et al. A model of tailoring effects: a randomized controlled trial examining the mechanisms of tailoring in a web-based STD screening intervention. Health Psychol 2016; 35: 1214–12324. [DOI] [PubMed] [Google Scholar]
- 13.Arie D. The psychology of tailoring-ingredients in computer-tailored persuasion. Soc Personal Psychol Compass 2008; 2: 765–784. [Google Scholar]
- 14.Morrison LG. Theory-based strategies for enhancing the impact and usage of digital health behaviour change interventions: a review. Digit Health 2015; 1: 2055207615595335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hawkins RP, Kreuter M, Resnicow K, et al. Understanding tailoring in communicating about health. Health Educ Res 2008; 23: 454–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harrington NG, Noar SM. Reporting standards for studies of tailored interventions. Health Educ Res 2012; 27: 331–342. [DOI] [PubMed] [Google Scholar]
- 17.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med 2010; 51: 214–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ryan K Dockray S, andLinehan C. A systematic review of tailored eHealth weight loss interventions. PROSPERO 2017; CRD42017072901. Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017072901 (2017, accessed 30 July 2018).
- 20.Bos-Touwen I, Jonkman N, Westland H, et al. Tailoring of self-management interventions in patients with heart failure. Curr Heart Fail Rep 2015; 12: 223–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patrick K, Marshall SJ, Davila EP, et al. Design and implementation of a randomized controlled social and mobile weight loss trial for young adults (project SMART). Contemp Clin Trials 2014; 37: 10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Genugten L, van Empelen P, Flink I, et al. Systematic development of a self-regulation weight-management intervention for overweight adults. BMC Public Health 2010; 10: 649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morris SB. Estimating effect sizes from pretest–posttest-control group designs. Organ Res Methods 2008; 11: 364–386. [Google Scholar]
- 24.Napolitano MA, Hayes S, Bennett GG, et al. Using Facebook and text messaging to deliver a weight loss programme to college students. Obesity 2013; 21: 25–31. [DOI] [PubMed] [Google Scholar]
- 25.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum, 1988. [Google Scholar]
- 26.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheung KL, Schwabe I, Walthouwer JM, et al. Effectiveness of a video-versus text-based computer-tailored intervention for obesity prevention after one year: a randomized controlled trial. Int J Environ Res Public Health 2017; 14: 1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Melchart D, Low P, Wuhr E, et al. Effects of a tailored lifestyle self-management intervention (TALENT) study on weight reduction: a randomized controlled trial. Diabetes Metab Syndr Obes 2017; 10: 235–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Napolitano MA, Whiteley JA, Mavredes MN, et al. Using social media to deliver weight loss programming to young adults: design and rationale for the Healthy Body Healthy U (HBHU) trial. Contemp Clin Trials 2017; 60: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Godino JG, Merchant G, Norman GJ, et al. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): a 2 year, parallel-group, randomised, controlled trial. Lancet Diabetes Endocrinol 2016; 4: 747–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mouttapa M, Robertson TP, McEligot AJ, et al. The Personal Nutrition Planner: A 5-week, computer-tailored intervention for women. J Nutr Educ Behav 2011; 43: 165–172. [DOI] [PubMed] [Google Scholar]
- 32.Rothert K, Strecher VJ, Doyle LA, et al. Web-based weight management programs in an integrated health care setting: a randomized, controlled trial. Obesity 2006; 14: 266–272. [DOI] [PubMed] [Google Scholar]
- 33.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss programme. Arch Intern Med 2006; 166: 1620–1625. [DOI] [PubMed] [Google Scholar]
- 34.Van Genugten L, van Empelen P, Boon B, et al. Results from an online computer-tailored weight management intervention for overweight adults: randomized controlled trial. J Med Internet Res 2012; 14: e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: the case for tailoring print materials. Ann Behav Med 1999; 21: 276. [DOI] [PubMed] [Google Scholar]
- 36.Resnicow K, Baranowski T, Ahluwalia JS, et al. Cultural sensitivity in public health: defined and demystified. Ethn Dis 1999; 9: 10–21. [PubMed] [Google Scholar]
- 37.Marcus AC, Mason M, Wolfe P, et al. The efficacy of tailored print materials in promoting colorectal cancer screening: results from a randomized trial involving callers to the National Cancer Institute's Cancer Information Service. J Health Commun 2005; 10: 83–104. [DOI] [PubMed] [Google Scholar]
- 38.Lie SS, Karlsen B, Oord ER, et al. Dropout From an eHealth Intervention for Adults with type 2 diabetes: a qualitative study. J Med Internet Res 2017; 19: e187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process 1991; 50: 248–287. [Google Scholar]
- 40.Perski O, Blandford A, West R, et al. Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Transl Behav Med 2017; 7: 254–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Foley P, Steinberg D, Levine E, et al. Track: a randomized controlled trial of a digital health obesity treatment intervention for medically vulnerable primary care patients. Contemp Clin Trials 2016; 48: 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ritterband LM, Gonder-Frederick LA, Cox DJ, et al. Internet interventions: in review, in use, and into the future. Prof Psychol Res Pr 2003; 34: 527. [Google Scholar]
- 43.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46: 81–95. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental Material1 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health
Supplemental material, Supplemental Material2 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health
Supplemental material, Supplemental Material3 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health
Supplemental material, Supplemental Material4 for A systematic review of tailored eHealth interventions for weight loss by Kathleen Ryan, Samantha Dockray and Conor Linehan in Digital Health