Abstract
Background:
Falls are an important cause of morbidity and mortality in older Americans and are more common in those with vision impairment (VI). However, there are few nationally-representative data on the prevalence of falls, fear of falling (FoF), and activity limitation due to FoF in this population.
Objectives:
To determine the prevalence of falls, FoF, and activity limitation due to FoF in a nationally-representative study of older adults with self-reported VI in the U.S.
Design:
Cross-sectional analysis of panel survey data.
Setting:
The National Health and Aging Trends Study, a nationally-representative survey administered annually from 2011–2016 to U.S. Medicare beneficiaries age≥65.
Participants:
There were 11,558 unique respondents who contributed 36,229 participant-observations.
Measurements:
We performed logistic regression to calculate the unadjusted and adjusted prevalence of self-reported history of >1 fall in the past year, any fall in the past month, FoF, and activity limitation due to FoF in participants with and without self-reported VI.
Results:
The weighted proportion of participants reporting VI was 8.6% (95%CI,8.0–9.2%). The unadjusted prevalence of >1 fall in the past year was 27.6% (95%CI,25.5–29.7%) in participants with self-reported VI and 13.2% (95%CI,12.7–13.7%) in those without self-reported VI. The prevalence of FoF and FoF limiting activity was 48.3% (95%CI,46.1–50.6%) and 50.8% (95%CI 47.3–54.2%), respectively, in respondents with self-reported VI and 26.7% (95%CI,25.9–27.5%) and 33.9% (95%CI,32.4–35.4%), respectively, in those without self-reported VI.
Conclusion:
The prevalence of falls, FoF, and activity limitation due to FoF is high in older adults with self-reported VI. FoF and resulting activity limitation are associated with declines in quality of life and this is the first study to provide nationally-representative data on the prevalence of these outcomes among older Americans with self-reported VI. Findings demonstrate the need to treat avoidable VI and to develop interventions to prevent falls and fall-related outcomes in this population.
Keywords: vision, ophthalmology, falls, aging, epidemiology, survey, fear of falling, NHATS
INTRODUCTION
Vision impairment (VI) and blindness affect 1 in 11 Americans age 65 and older in the United States.1 Due to aging of the population, the number of older adults with VI is predicted to increase through at least 2050.2 VI is associated with decreased independence,3 poorer subjective well-being,4 and an increased risk of falls.5–13 In a given year, approximately 30% of adults over age 65 will fall5 and VI increases this risk more than 2-fold.14 Falls are a substantial cause of morbidity and mortality,15 and in 2015 were associated with annual medical costs in the U.S. of $50 billion.16 Fear of falling (FoF) and activity limitation due to FoF are also more common in older adults with VI17,18 and are associated with declines in health-related quality of life and independence.19,20
Data on the prevalence of falls and fall-related outcomes in visually impaired older adults are needed to understand the magnitude of this problem and design targeted population health interventions.21 Crews and colleagues analyzed data from the Behavioral Risk Factor Surveillance System (BRFSS) and found that 46.7% of adults age 65 and older with self-reported severe VI or blindness had fallen in the prior year compared to 27.7% of controls.8 However, they included respondents who reported a single fall in the past year, which might overestimate clinically relevant fall risk, as the American and British Geriatrics Societies recommend using a threshold of >1 fall in the past year to screen for fall risk.22 Additionally, this study calculated fall prevalence in those who reported severe VI and did not count individuals with milder forms of VI that are more common in the general population. Finally, the study did not report prevalence estimates adjusted for potential confounders that have been associated with both VI23,24 and fall risk25,26 in prior investigations.
Several studies have also found an association between VI and FoF and have demonstrated that those with FoF are more likely to experience activity restriction.17,18,27 A study by Nguyen et al showed that among older adults with age-related macular degeneration (AMD), declines in vision were associated with less physical activity and that FoF mediated the relationship between vision loss and activity restriction.27 In another study, investigators found that 40–50% of patients with Fuchs’ corneal dystrophy, glaucoma, or AMD reported limiting their activity due to FoF compared to only 16% of controls.18 Finally, in a population-based study from Ireland, researchers found that worse self-reported vision was independently associated with both FoF and activity restriction due to FoF.17 Importantly, the population prevalence of FoF and associated activity restriction in older Americans with self-reported VI has not been reported,28 though this is critical data for designing interventions to address these adverse outcomes.
The purpose of the current study was to provide up-to-date data on the prevalence of falls, as well as to contribute novel epidemiologic data on the prevalence of FoF and activity limitation due to FoF among older adults with self-reported VI in the U.S. In order to explore these relationships, we analyzed nationally-representative survey data from the National Health and Aging Trends Study (NHATS), which includes information about patient health characteristics, demographics, socioeconomics, and healthcare utilization. The current study provides needed epidemiologic data to illustrate the scope of falls and fall-related outcomes in visually impaired older Americans. These data may be important for developing and testing interventions that aim to decrease falls, FoF, and activity limitation due to FoF in this large and growing population.
METHODS
The University of Michigan Institutional Review Board deemed this study exempt since NHATS consists of publically available non-identifiable data.
Data and Analysis Sample
NHATS is an annual survey that is administered through in-person interviews to a nationally representative cohort of adults age 65 and older and enrolled in Medicare. The sampling frame was defined using the Medicare enrollment database. In round 1, a three stage stratified sampling design was used that included selection of 95 primary sampling units (counties or groups of counties); selection of 655 secondary sampling units (zip codes or zip code fragments); and selection of respondents who were Medicare beneficiaries age 65 or older on September 30, 2010. The oldest age groups and non-Hispanic black persons were oversampled. In round 1, NHATS achieved a 71% response rate, corresponding to 8,245 individuals and an effective sample size of 6,461 after accounting for the differential probability of selection.29 The sample was replenished in 2015 to account for attrition due to loss to follow-up and death.30
For this study, data were available for 2011–2016 and we included all participants with complete data in a given year for all of the variables in our models. Accordingly, complete data was available for 92% of participant-observations, and our analytic sample consisted of 11,558 unique participants who contributed 36,229 participant-observations.
Variable Definitions
VI was self-reported as difficulty recognizing someone across the street and/or reading newspaper print, even when using corrective lenses. We classified a participant as having self-reported VI if they reported VI in a given year. Falls were defined as “any fall, slip or trip in which you lose your balance and land on the floor or ground or at a lower level.” Participants were asked if they had any fall in the past month and if they fell more than once in the past 12 months. FoF was determined from a question that asked participants if they had worried about falling down in the last month; this was followed by an additional question asking whether worry about falling ever caused them to limit their activities. To determine the number of medical comorbidities that a participant had, we counted the number of chronic conditions reported, including a history of myocardial infarction, heart disease, hypertension, arthritis, osteoporosis, diabetes, lung disease, stroke, and cancer.31
Analyses
Based on the NHATS survey design, we used 2011–2016 NHATS data to calculate the weighted proportions of participants for each covariate stratified by whether participants self-reported any VI in a given year. We report unadjusted P values from Pearson chi-squared tests for categorical variables and t-tests for continuous or ordinal variables. We calculated the unadjusted prevalence of falls and fall-related outcomes for participants with and without self-reported VI. We then performed multivariable logistic regression and used the “margins” post-estimation command in Stata (StataCorp, College Station, TX, USA) to calculate prevalence estimates while adjusting for age, sex, race/ethnicity, educational attainment, Medicaid eligibility, number of medical comorbidities, body mass index (BMI), proxy respondent, and survey round. All models accounted for the clustering of multiple observations from the same participant. Analyses were conducted using Stata version 14 and accounted for the complex design of the survey, including cross-sectional sample weights, sampling units, and strata.
RESULTS
Characteristics of Study Sample
Characteristics of the study sample are presented in Table 1. The total weighted proportion of participants who reported any form of VI was 8.6% (95% confidence interval [CI], 8.0–9.2%). Participants were more likely to report VI if they were older, female, non-white, less educated, dual-eligible for Medicaid, had a lower BMI (p=0.04), more medical comorbidities, or required a proxy respondent (p<0.001 for all comparisons, except as noted).
Table 1.
Summary statistics of study samplea
| Characteristic | Participants with Any Self-Reported VIb (n=3,933) |
Participants with No Self-Reported VI (n=32,296) |
P-valuec |
|---|---|---|---|
| Total, % (95% CI) | 8.6 (8.0–9.2) | 91.4 (90.8–92.0) | |
| Age, years, % (95% CI) | <0.001 | ||
| 65–69 | 14.2 (12.3–16.4) | 22.5 (21.7–23.2) | |
| 70–74 | 17.5 (15.7–19.6) | 29.3 (29.3–30.2) | |
| 75–79 | 17.3 (15.3–19.4) | 20.7 (20.0–21.5) | |
| 80–84 | 17.4 (15.6–19.3) | 14.6 (14.0–15.2) | |
| 85–89 | 17.9 (16.2–19.7) | 8.8 (8.2–9.3) | |
| 90+ | 15.7 (14.2–17.4) | 4.1 (3.7–4.5) | |
| Sex, % (95% CI) | <0.001 | ||
| Male | 34.4 (32.0–37.0) | 44.7 (43.5–45.9) | |
| Female | 65.6 (63.0–68.0) | 55.3 (54.1–56.5) | |
| Race/Ethnicity, % (95% CI) | <0.001 | ||
| White | 68.2 (64.3–72.0) | 80.8 (79.1–82.4) | |
| Black | 11.45 (9.8–13.3) | 7.9 (7.1–8.7) | |
| Hispanic | 13.7 (11.0–16.9) | 6.1 (5.1–7.2) | |
| Other | 6.6 (4.5–9.6) | 5.2 (4.4–6.2) | |
| Education, % (95% CI) | <0.001 | ||
| <High school degree | 36.5 (33.3–39.8) | 17.8 (16.4–19.2) | |
| High school degree | 28.2 (25.6–31.0) | 26.7 (25.3–28.1) | |
| >High school degree | 35.2 (32.0–38.6) | 55.5 (53.4–57.7) | |
| Medicaid Beneficiary | <0.001 | ||
| Yes | 28.1 (25.1–31.3) | 11.2 (10.3–12.2) | |
| No | 71.9 (68.6–74.9) | 88.8 (87.7–89.7) | |
| Body Mass Index, mean (95% CI) | 27.4 (27.0–27.8) | 27.8 (27.6–27.9) | 0.04 |
| Comorbidities, mean (95% CI) | 2.9 (2.9–3.0) | 2.3 (2.3–2.3) | <0.001 |
| Proxy Respondent, % (95% CI) | <0.001 | ||
| No proxy | 78.6 (76.1–81.0) | 96.5 (96.1–96.9) | |
| Proxy | 21.3 (19.0–23.9) | 3.5 (3.1–3.9) | |
CI: confidence interval, VI: vision impairment
Data are presented as weighted proportions of US population of Medicare beneficiaries age ≥65, accounting for the study design of the National Health and Aging Trends Study
Includes participants who self-reported near and/or distance vision impairment
P values are unadjusted and calculated using design-adjusted Pearson chi-squared test for categorical variables and t-test for continuous/ordinal variables.
Prevalence of Falls and Fall-Related Outcomes
Table 2 illustrates the prevalence of falls and fall-related outcomes for participants with and without self-reported VI. All unadjusted and adjusted prevalence estimates were significantly higher for those with self-reported VI compared to participants without self-reported VI (p<0.001 for all comparisons). The unadjusted prevalence of each of the fall and fall-related outcomes was nearly twice as high among those with self-reported VI. After adjusting for age, sex, and other covariates, the difference in prevalence was smaller; however, there was still a ≥25% increase in the prevalence for all four outcomes in those with self-reported VI.
Table 2.
Prevalence of falls and fall-related outcomes in Medicare beneficiaries age 65 and oldera
| Unadjusted Prevalence Estimates | ||
|---|---|---|
| No VIb (n=32,296) |
Any VI (n=3,933) |
|
| Falls, % (95% CI) | ||
| >1 fall in past year | 13.2 (12.7–13.7) | 27.6 (25.5–29.7) |
| Any fall in past month | 10.3 (9.8–10.7) | 18.8 (17.4–20.3) |
| FoF, % (95% CI) | 26.7 (25.9–27.5) | 48.3 (46.1–50.6) |
| FoF limiting activity, % (95% CI) | 33.9 (32.4–35.4) | 50.8 (47.3–54.2) |
| Adjusted Prevalence Estimatesc | ||
| Falls, % (95% CI) | ||
| >1 fall in past year | 13.5 (13.0–14.0) | 20.6 (18.5–22.8) |
| Any fall in past month | 10.5 (10.0–10.9) | 14.5 (13.1–16.0) |
| FoF, % (95% CI) | 27.2 (26.4–28.1) | 37.5 (35.1–39.9) |
| FoF limiting activity, % (95% CI) | 30.7 (28.9–32.5) | 38.9 (35.4–42.4) |
CI: confidence interval, VI: vision impairment, FoF: fear of falling
Data are presented as weighted proportions of US population of Medicare beneficiaries age ≥65, accounting for the study design of the National Health and Aging Trends Study
Participants were classified as having “any VI” if they reported distance and/or near VI in a given year
Adjusted for age, sex, race/ethnicity, educational attainment, Medicaid eligibility, number of medical comorbidities, body mass index, proxy respondent, and survey round.
Sociodemographic Associations with Falls and Fall-Related Outcomes
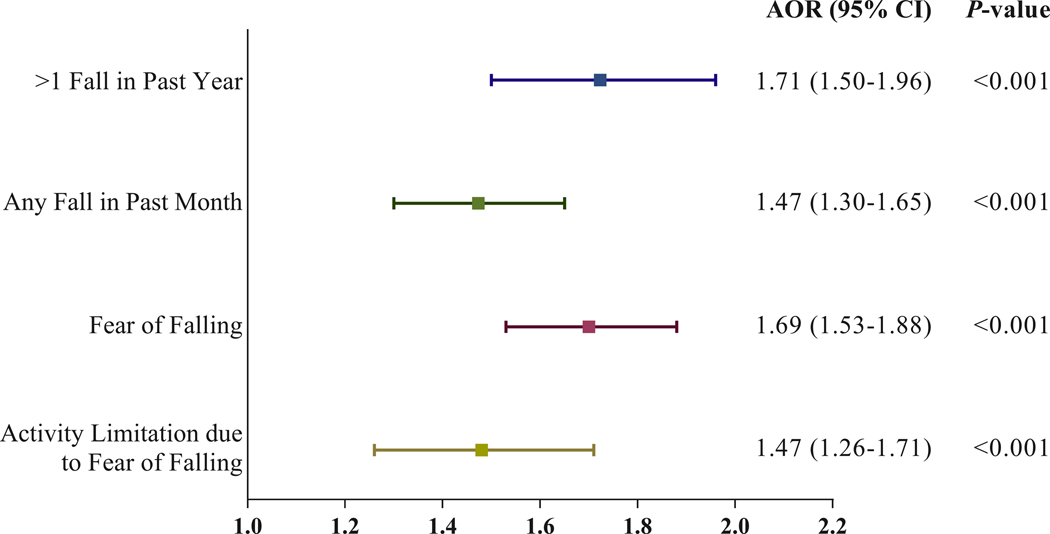
Table 3 presents the results of multivariable logistic models showing the adjusted associations between sociodemographic and economic characteristics with falls and fall-related outcomes. The odds of reporting a fall in the past month or recurrent falls in the past year were significantly greater among those who self-reported VI and were older, male, white, less educated, dual-eligible for Medicaid, had more medical comorbidities, and required a proxy respondent. The odds of reporting FoF were significantly higher in those who had self-reported VI and were older, female, white, dual-eligible for Medicaid, had a higher BMI, more medical comorbidities, and required a proxy respondent. The odds of activity limitation due to FoF were significantly greater among those who had self-reported VI and were male, Medicaid eligible, had more medical comorbidities, and required a proxy respondent.
Table 3.
Fully adjusted logistic models of the association of vision impairment with falls and fall-related outcomesa
| >1 fall in past year | Any fall in past month | FoF | FoF limiting activity | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Vision Impairmentb | ||||||||
| No VI | reference | reference | reference | reference | ||||
| VI | 1.71 (1.50–1.96) | <0.001 | 1.47 (1.30–1.65) | <0.001 | 1.69 (1.53–1.88) | <0.001 | 1.47 (1.26–1.71) | <0.001 |
| Age, years | ||||||||
| 65–69 | reference | reference | reference | reference | ||||
| 70–74 | 1.06 (0.94–1.20) | 0.33 | 1.06 (0.88–1.27) | 0.55 | 1.06 (0.96–1.16) | 0.26 | 0.92 (0.74–1.14) | 0.44 |
| 75–79 | 1.01 (0.85–1.19) | 0.93 | 0.96 (0.80–1.14) | 0.61 | 1.34 (1.19–1.51) | <0.001 | 0.92 (0.73–1.16) | 0.46 |
| 80–84 | 1.14 (0.98–1.32) | 0.09 | 1.20 (1.01–1.44) | 0.04 | 1.89 (1.66–2.14) | <0.001 | 1.04 (0.84–1.30) | 0.69 |
| 85–89 | 1.33 (1.11–1.58) | 0.002 | 1.23 (1.01–1.51) | 0.04 | 2.45 (2.14–2.80) | <0.001 | 1.15 (0.90–1.48) | 0.26 |
| 90+ | 1.33 (1.11–1.60) | 0.003 | 1.24 (0.99–1.54) | 0.06 | 2.84 (2.36–2.42) | <0.001 | 1.00 (0.80–1.24) | 0.98 |
| Sex | ||||||||
| Male | reference | reference | reference | reference | ||||
| Female | 0.86 (0.78–0.96) | 0.01 | 0.83 (0.75–0.91) | <0.001 | 1.52 (1.40–1.66) | <0.001 | 0.85 (0.75–0.96) | 0.01 |
| Race/Ethnicity | ||||||||
| White | reference | reference | reference | reference | ||||
| Black | 0.63 (0.56–0.69) | <0.001 | 0.73 (0.66–0.81) | <0.001 | 0.59 (0.52–0.68) | <0.001 | 1.05 (0.86–1.29) | 0.63 |
| Hispanic | 0.73 (0.59–0.90) | 0.003 | 1.05 (0.85–1.30) | 0.63 | 1.22 (1.01–1.47) | 0.04 | 1.17 (0.86–1.59) | 0.31 |
| Other | 0.47 (0.34–0.63) | <0.001 | 0.68 (0.52–0.90) | 0.01 | 0.73 (0.55–0.97) | 0.03 | 0.91 (0.69–1.21) | 0.53 |
| Education | ||||||||
| <High school degree | reference | reference | reference | reference | ||||
| High school degree | 0.86 (0.74–0.99) | 0.04 | 0.82 (0.72–0.95) | 0.01 | 0.96 (0.84–1.10) | 0.59 | 0.83 (0.71–0.96) | 0.02 |
| >High school degree | 0.90 (0.79–1.04) | 0.14 | 0.86 (0.75–0.98) | 0.03 | 0.99 (0.87–1.12) | 0.87 | 0.90 (0.74–1.08) | 0.25 |
| Medicaid Beneficiary | ||||||||
| Yes | reference | reference | reference | reference | ||||
| No | 0.81 (0.71–0.92) | 0.001 | 0.84 (0.72–0.98) | 0.03 | 0.74 (0.65–0.85) | <0.001 | 0.68 (0.59–0.79) | <0.001 |
| Body Mass Index | 1.01 (1.00–1.02) | 0.11 | 1.00 (0.99–1.01) | 0.47 | 1.03 (1.02–1.04) | <0.001 | 1.00 (0.98–1.01) | 0.64 |
| Comorbidities | 1.37 (1.32–1.41) | <0.001 | 1.26 (1.22–1.30) | <0.001 | 1.38 (1.34–1.42) | <0.001 | 1.29 (1.23–1.34) | <0.001 |
| Proxy Respondent | ||||||||
| No proxy | reference | reference | reference | reference | ||||
| Proxy | 2.78 (2.31–3.35) | <0.001 | 2.06 (1.72–2.46) | <0.001 | 1.18 (1.01–1.38) | 0.04 | 2.16 (1.65–2.83) | <0.001 |
CI: confidence interval, VI: vision impairment, OR: odds ratio, FoF: fear of falling
All models were adjusted for NHATS survey round
Participants were classified as having “any VI” if they reported distance and/or near VI in a given year
DISCUSSION
In this study of a nationally-representative sample of U.S. Medicare beneficiaries age 65 and older, we found that falls, FoF, and activity limitation due to FoF were all significantly more prevalent among those with self-reported VI. This study contributes important and novel epidemiologic data on the prevalence of FoF and activity limitation due to FoF in older adults with self-reported VI, while also confirming prior investigations that have reported a high prevalence of recurrent falls in this population. Approximately one-half of those with self-reported VI had FoF (compared to 27% without self-reported VI) and activity limitation due to FoF (compared to 34% without self-reported VI), while more than one in four (28%) reported recurrent falls in the prior year (compared to 13% without self-reported VI). Findings from this study suggest the importance of falls prevention interventions for this at-risk population in order to limit the morbidity, mortality, and healthcare expenditures associated with falls,15,16 as well as the declines in well-being, quality of life, and independence that may accompany FoF and associated activity restriction.19,20
Our study confirms the findings of prior investigations that have described a strong association between VI and an increased likelihood of falls.5–13 In an investigation by Crews et al using nationally-representative data from BRFSS, the investigators reported a higher prevalence of falls than in the current study (46.7% vs 27.6%).8 The lower prevalence of falls in our study is likely due to differences between the two studies in the definition of VI and in the criteria used to define falls. Our study estimated fall prevalence using the American and British Geriatrics Societies’ recommendations for assessing fall risk among those who report recurrent falls (rather than a single fall) in the past year.22 In other studies based on objectively measured vision, rather than self-report, investigators have shown that different measures of vision loss, including impaired visual acuity,9 visual field defects,10,12 reduced contrast sensitivity,9,11 and decreased depth perception13 were all associated with an increase in falls. In a review of the literature on VI and falls, Rubenstein and Josephson showed that the mean odds or relative risk of falls in those with VI (inconsistently defined across studies) was 2.5 (range, 1.6–3.5),21 which was larger than the effect size for age >80 years, cognitive impairment, depression, impaired activities of daily living, and arthritis.14
We examined the sociodemographic characteristics that were independently associated with falls and found that our models confirmed prior reports that have described an association between falls and increasing age, lower socioeconomic status, white race, and having more medical comorbidities.32–34 Although prior investigations have reported a significant association between higher BMI and recurrent falls,35,36 we did not find this independent association in our data.
Our study also demonstrated a high prevalence of FoF and activity restriction due to FoF, which to our knowledge is the first report of the population prevalence of these fall-related outcomes in older adults with self-reported VI in the U.S. In a systematic review, Scheffer et al found that the reported prevalence of FoF among community-dwelling older adults ranged from 3 to 85% depending on the study and its measurement strategy.37 They found that the main risk factors for FoF were a history of falls, being female, and being older. Their review did not identify VI as an important risk factor, though based on our study VI is strongly associated with FoF and resultant activity restriction.
Other studies have also found an association between VI and FoF.38–40 In a Japanese clinic-based study, Yuki et al showed that 23–25% of patients with moderate to severe glaucoma reported FoF (compared to 12% of controls and patients with mild glaucoma). In our study, nearly 1 in 2 older adults with self-reported VI endorsed FoF. This difference may be due to different cultural and environmental contexts, the relatively asymptomatic nature of glaucoma until late stages of the disease compared to other causes of VI,41 and/or differences in the ascertainment of FoF. Several other studies on VI and FoF also demonstrated a strong positive relationship but it is difficult to directly compare their results to our study since they quantified participants’ level of FoF on an interval scale rather than its presence or absence.38,40
In our multivariable models, we found that FoF was independently associated with being female, white, Medicaid eligible, and having a higher BMI or more medical comorbidities. Prior investigations in older adults with38–40 and without VI20,42 have also detected these associations and have reported comparable effect sizes.20 The association between BMI and FoF in this study suggests that those with a higher BMI are more likely to fear falling even when they are no more likely to actually fall. It is not clear why certain characteristics were associated with falls but not fall-related outcomes or visa-versa. Future work could examine potential mediators of these relationships, such as objective and subjective measures of balance.
Our study also found that 51% of older adults with self-reported VI had activity limitation due to FoF compared to 34% of controls. Several prior studies have examined the relationship between VI and activity limitation due to FoF. Wang et al found that 40–50% of patients with Fuchs’ corneal dystrophy, glaucoma, or AMD,18 reported restricting activity due to FoF, a result that is similar to the unadjusted prevalence reported in this study. In a population-based study from Ireland, researchers found that self-reported, but not objectively measured, VI was significantly associated with increased FoF and activity restriction due to FoF, however they did not report survey-weighted prevalence estimates for these outcomes. Finally, Nguyen and colleagues demonstrated that worse vision was associated with decreased physical activity in subjects with glaucoma and AMD and that this relationship was mediated by FoF for those with AMD.27 Our study makes an important contribution to the existing literature on VI and activity restriction due to FoF by providing needed epidemiologic data and insight into important associations with this outcome.
Limitations
There were several limitations to this study. NHATS relies on self-report, which can be subject to recall bias. Although self-reported vision is not perfectly correlated with visual acuity, self-reported vision status has been widely used in prior population-based studies,43–45 and previous studies have found that the two measures may have a strong positive association.46,47 NHATS respondents were also asked to recall falls from the prior year, though the validity of the NHATS falls questions has not been tested against prospective falls diaries, which are known to be more accurate and are considered the gold-standard for falls reporting.48 Data from NHATS also did not allow us to determine the severity of falls. In addition, our results may not fully represent those who did not have complete data, particularly those who did not report Medicaid dual eligibility and/or BMI, as these two variables together accounted for the majority of missing data. Finally, this study did not determine whether the relationship between VI, falls, and fall-related outcomes is causative, bidirectional, or simply associational.
Conclusions
Older Americans with self-reported VI have a high prevalence of falls, FoF, and activity-restriction due to FoF compared to their normal sighted peers. This study provides important and novel epidemiologic data on the prevalence of FoF and related activity restriction in older adults with self-reported VI, while also confirming the strong association between VI and falls. Data from this study help to define the scope of these problems and may inform future studies and interventions aimed at decreasing the likelihood of falls and fall-related outcomes in visually impaired older adults. Future studies should investigate the effectiveness of falls prevention interventions in this population. Moreover, since VI is avoidable or treatable in a large majority of cases,21 this may represent a modifiable target for interventions to decrease falls and fall-related outcomes for some older adults. These outcomes represent critical public health concerns that are likely to impact a growing number of individuals as the population continues to age.
Figure 1. Forest plot depicting the association of self-reported vision impairment with falls and fall-related outcomes.
The figure depicts the adjusted odds ratios and 95% confidence intervals for the fully adjusted association of self-reported vision impairment with each fall and fall-related outcome.
CI: confidence interval, AOR: adjusted odds ratio
ACKNOWLEDGEMENTS
The authors would like to thank Abigail Kumagai,1 Katherine Bissen,1 and Alison Granger1 for their role in preparing data for analysis and formatting results for dissemination.
Sponsors’ Role
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript
This research was supported by grants from the National Eye Institute (K23 EY027848) to JRE; a pilot grant to JRE from the Institute for Social Research at the University of Michigan funded by the National Institute on Aging (P30 AG012846); an unrestricted grant from Research to Prevent Blindness to the Department of Ophthalmology and Visual Sciences at the University of Michigan; and the Lighthouse Guild.
Footnotes
Department of Ophthalmology and Visual Sciences, University of Michigan, Ann Arbor, MI
This work was presented in part at the Association for Research in Vision and Ophthalmology annual meeting (April 29-May 3, 2018) and the World Ophthalmology Congress (June 16–19, 2018).
Impact Statement: we certify that this work is novel. This research contributes important nationally-representative epidemiological data about the prevalence of falls and fall-related outcomes in visually impaired older Americans. These findings are crucial for defining the scope of this problem, optimally allocating healthcare resources, and designing appropriate interventions.
Conflict of Interest
The authors have no commercial, proprietary, or financial interest in any of the products or companies described in this article.
REFERENCES
- 1.Vision Problems in the U.S. - Prevalence of Age-Related Eye Disease in America. http://www.visionproblemsus.org/index.html. Accessed October 2, 2017.
- 2.Chan T, Friedman DS, Bradley C, Massof R. Estimates of Incidence and Prevalence of Visual Impairment, Low Vision, and Blindness in the United States. JAMA Ophthalmol. November 2017. doi: 10.1001/jamaophthalmol.2017.4655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger S, Porell F. The association between low vision and function. J Aging Health. 2008;20(5):504–525. doi: 10.1177/0898264308317534 [DOI] [PubMed] [Google Scholar]
- 4.Rafaely L, Carmel S, Bachner YG. Subjective well-being of visually impaired older adults living in the community. Aging Ment Health. 2017;0(0):1–8. doi: 10.1080/13607863.2017.1341469 [DOI] [PubMed] [Google Scholar]
- 5.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;(9):CD007146. doi: 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reed-Jones RJ, Solis GR, Lawson KA, Loya AM, Cude-Islas D, Berger CS. Vision and falls: a multidisciplinary review of the contributions of visual impairment to falls among older adults. Maturitas. 2013;75(1):22–28. doi: 10.1016/j.maturitas.2013.01.019 [DOI] [PubMed] [Google Scholar]
- 7.Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health. 2004;94(5):823–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crews JE, DPA, Chou C-F, Stevens JA Saaddine JB. Falls Among Persons Aged ≥65 Years With and Without Severe Vision Impairment - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(17):433–437. doi: 10.15585/mmwr.mm6517a2 [DOI] [PubMed] [Google Scholar]
- 9.Ivers RQ, Cumming RG, Mitchell P, Attebo K. Visual impairment and falls in older adults: the Blue Mountains Eye Study. J Am Geriatr Soc. 1998;46(1):58–64. [DOI] [PubMed] [Google Scholar]
- 10.Coleman AL, Cummings SR, Yu F, et al. Binocular visual-field loss increases the risk of future falls in older white women. J Am Geriatr Soc. 2007;55(3):357–364. doi: 10.1111/j.1532-5415.2007.01094.x [DOI] [PubMed] [Google Scholar]
- 11.de Boer MR, Pluijm SMF, Lips P, et al. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. J Bone Miner Res Off J Am Soc Bone Miner Res. 2004;19(9):1539–1547. doi: 10.1359/JBMR.040504 [DOI] [PubMed] [Google Scholar]
- 12.Freeman EE, Muñoz B, Rubin G, West SK. Visual field loss increases the risk of falls in older adults: the Salisbury eye evaluation. Invest Ophthalmol Vis Sci. 2007;48(10):4445–4450. doi: 10.1167/iovs.07-0326 [DOI] [PubMed] [Google Scholar]
- 13.Lord SR, Dayhew J. Visual risk factors for falls in older people. J Am Geriatr Soc. 2001;49(5):508–515. [DOI] [PubMed] [Google Scholar]
- 14.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18(2):141–158. [DOI] [PubMed] [Google Scholar]
- 15.Albert SM, Freedman VA. Public Health and Aging: Maximizing Function and Well-Being. 2nd ed New York, NY: Springer Publishing Company; 2010. [Google Scholar]
- 16.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. March 2018. doi: 10.1111/jgs.15304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donoghue OA, Ryan H, Duggan E, et al. Relationship between fear of falling and mobility varies with visual function among older adults. Geriatr Gerontol Int. 2014;14(4):827–836. doi: 10.1111/ggi.12174 [DOI] [PubMed] [Google Scholar]
- 18.Wang MY, Rousseau J, Boisjoly H, et al. Activity limitation due to a fear of falling in older adults with eye disease. Invest Ophthalmol Vis Sci. 2012;53(13):7967–7972. doi: 10.1167/iovs.12-10701 [DOI] [PubMed] [Google Scholar]
- 19.Grimbergen YAM, Schrag A, Mazibrada G, Borm GF, Bloem BR. Impact of falls and fear of falling on health-related quality of life in patients with Parkinson’s disease. J Park Dis. 2013;3(3):409–413. doi: 10.3233/JPD-120113 [DOI] [PubMed] [Google Scholar]
- 20.Denkinger MD, Lukas A, Nikolaus T, Hauer K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2015;23(1):72–86. doi: 10.1016/j.jagp.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 21.National Academies of Sciences, Engineering, and Medicine. Making Eye Health a Population Health Imperative: Vision for Tomorrow. Washington D.C: The National Academies Press; 2016. [PubMed] [Google Scholar]
- 22.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi: 10.1111/j.1532-5415.2010.03234.x [DOI] [PubMed] [Google Scholar]
- 23.Congdon N, O’Colmain B, Klaver CCW, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol Chic Ill 1960. 2004;122(4):477–485. doi: 10.1001/archopht.122.4.477 [DOI] [PubMed] [Google Scholar]
- 24.Crews JE, Chou C-F, Sekar S, Saaddine JB. The Prevalence of Chronic Conditions and Poor Health Among People With and Without Vision Impairment, Aged ≥65 Years, 2010–2014. Am J Ophthalmol. 2017;182:18–30. doi: 10.1016/j.ajo.2017.06.038 [DOI] [PubMed] [Google Scholar]
- 25.Paliwal Y, Slattum PW, Ratliff SM. Chronic Health Conditions as a Risk Factor for Falls among the Community-Dwelling US Older Adults: A Zero-Inflated Regression Modeling Approach. BioMed Res Int. 2017;2017:5146378. doi: 10.1155/2017/5146378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryu E, Juhn YJ, Wheeler PH, et al. Individual housing-based socioeconomic status predicts risk of accidental falls among adults. Ann Epidemiol. 2017;27(7):415–420.e2. doi: 10.1016/j.annepidem.2017.05.019 [DOI] [PubMed] [Google Scholar]
- 27.Nguyen AM, Arora KS, Swenor BK, Friedman DS, Ramulu PY. Physical activity restriction in age-related eye disease: a cross-sectional study exploring fear of falling as a potential mediator. BMC Geriatr. 2015;15:64. doi: 10.1186/s12877-015-0062-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White UE, Black AA, Wood JM, Delbaere K. Fear of falling in vision impairment. Optom Vis Sci Off Publ Am Acad Optom. 2015;92(6):730–735. doi: 10.1097/OPX.0000000000000596 [DOI] [PubMed] [Google Scholar]
- 29.Montaquila J, Freedman V, Edwards B, Kasper J. National Health and Aging Trends Study (NHATS) Round 1 Sample Design and Selection NHATS Technical Paper #1. Baltimore, MD: Johns Hopkins University School of Public Health; 2012. www.nhats.org. [Google Scholar]
- 30.DeMatteis J, Freedman V, Kasper J. National Health and Aging Trends Study (NHATS) Round 5 Sample Design and Selection NHATS Technical Paper #16. Baltimore, MD: Johns Hopkins University School of Public Health; 2016. www.nhats.org. [Google Scholar]
- 31.Freedman VA, Kasper JD, Spillman BC. Successful Aging Through Successful Accommodation With Assistive Devices. J Gerontol Ser B. 2017;72(2):300–309. doi: 10.1093/geronb/gbw102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi: 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 33.Chang VC, Do MT. Risk factors for falls among seniors: implications of gender. Am J Epidemiol. 2015;181(7):521–531. doi: 10.1093/aje/kwu268 [DOI] [PubMed] [Google Scholar]
- 34.Hu J, Xia Q, Jiang Y, Zhou P, Li Y. Risk factors of indoor fall injuries in community-dwelling older women: a prospective cohort study. Arch Gerontol Geriatr. 2015;60(2):259–264. doi: 10.1016/j.archger.2014.12.006 [DOI] [PubMed] [Google Scholar]
- 35.Handrigan GA, Maltais N, Gagné M, et al. Sex-specific association between obesity and self-reported falls and injuries among community-dwelling Canadians aged 65 years and older. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2017;28(2):483–494. doi: 10.1007/s00198-016-3745-x [DOI] [PubMed] [Google Scholar]
- 36.Cho B-Y, Seo D-C, Lin H-C, Lohrmann DK, Chomistek AK. BMI and Central Obesity With Falls Among Community-Dwelling Older Adults. Am J Prev Med. 2018;54(4):e59–e66. doi: 10.1016/j.amepre.2017.12.020 [DOI] [PubMed] [Google Scholar]
- 37.Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37(1):19–24. doi: 10.1093/ageing/afm169 [DOI] [PubMed] [Google Scholar]
- 38.Ramulu PY, van Landingham SW, Massof RW, Chan ES, Ferrucci L, Friedman DS. Fear of falling and visual field loss from glaucoma. Ophthalmology. 2012;119(7):1352–1358. doi: 10.1016/j.ophtha.2012.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yuki K, Tanabe S, Kouyama K, et al. The association between visual field defect severity and fear of falling in primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2013;54(12):7739–7745. doi: 10.1167/iovs.13-12079 [DOI] [PubMed] [Google Scholar]
- 40.van Landingham SW, Massof RW, Chan E, Friedman DS, Ramulu PY. Fear of falling in age-related macular degeneration. BMC Ophthalmol. 2014;14:10. doi: 10.1186/1471-2415-14-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Janz NK, Wren PA, Lichter PR, Musch DC, Gillespie BW, Guire KE. Quality of life in newly diagnosed glaucoma patients : The Collaborative Initial Glaucoma Treatment Study. Ophthalmology. 2001;108(5):887–897; discussion 898. [DOI] [PubMed] [Google Scholar]
- 42.Singh T, Bélanger E, Thomas K. Is Fear of Falling the Missing Link to Explain Racial Disparities in Fall Risk? Data from the National Health and Aging Trends Study. Clin Gerontol. April 2018:1–6. doi: 10.1080/07317115.2018.1468377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Campbell VA, Crews JE, Moriarty DG, Zack MM, Blackman DK. Surveillance for sensory impairment, activity limitation, and health-related quality of life among older adults--United States, 1993–1997. MMWR CDC Surveill Summ Morb Mortal Wkly Rep CDC Surveill Summ. 1999;48(8):131–156. [PubMed] [Google Scholar]
- 44.Tanna AP, Kaye HS. Trends in self-reported visual impairment in the United States: 1984 to 2010. Ophthalmology. 2012;119(10):2028–2032. doi: 10.1016/j.ophtha.2012.04.018 [DOI] [PubMed] [Google Scholar]
- 45.Lam BL, Lee DJ, Zheng DD, Davila EP, Christ SL, Arheart KL. Disparity in prevalence of self-reported visual impairment in older adults among U.S. race-ethnic subgroups. Ophthalmic Epidemiol. 2009;16(3):144–150. doi: 10.1080/09286580902863007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yip JLY, Khawaja AP, Broadway D, et al. Visual acuity, self-reported vision and falls in the EPIC-Norfolk Eye study. Br J Ophthalmol. 2014;98(3):377–382. doi: 10.1136/bjophthalmol-2013-304179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.El-Gasim M, Munoz B, West SK, Scott AW. Associations between self-rated vision score, vision tests, and self-reported visual function in the Salisbury Eye Evaluation Study. Invest Ophthalmol Vis Sci. 2013;54(9):6439–6445. doi: 10.1167/iovs.12-11461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x [DOI] [PubMed] [Google Scholar]