Abstract
Background
Pain is a common symptom with cancer, and 30% to 50% of all people with cancer will experience moderate to severe pain that can have a major negative impact on their quality of life. Non‐opioid drugs are commonly used to treat mild to moderate cancer pain, and are recommended for this purpose in the WHO cancer pain treatment ladder, either alone or in combination with opioids.
A previous Cochrane review that examined the evidence for nonsteroidal anti‐inflammatory drugs (NSAIDs) or paracetamol, alone or combined with opioids, for cancer pain was withdrawn in 2015 because it was out of date; the date of the last search was 2005. This review, and another on NSAIDs, updates the evidence.
Objectives
To assess the efficacy of oral paracetamol (acetaminophen) for cancer pain in adults and children, and the adverse events reported during its use in clinical trials.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and Embase from inception to March 2017, together with reference lists of retrieved papers and reviews, and two online study registries.
Selection criteria
We included randomised, double‐blind, studies of five days' duration or longer, comparing paracetamol alone with placebo, or paracetamol in combination with an opioid compared with the same dose of the opioid alone, for cancer pain of any intensity. Single‐blind and open studies were also eligible for inclusion. The minimum study size was 25 participants per treatment arm at the initial randomisation.
Data collection and analysis
Two review authors independently searched for studies, extracted efficacy and adverse event data, and examined issues of study quality and potential bias. We did not carry out any pooled analyses. We assessed the quality of the evidence using GRADE and created a 'Summary of findings' table.
Main results
Three studies in adults satisfied the inclusion criteria, lasting up to one week; 122 participants were randomised initially, and 95 completed treatment. We found no studies in children. One study was parallel‐group, and two had a cross‐over design. All used paracetamol as an add‐on to established treatment with strong opioids (median daily morphine equivalent doses of 60 mg, 70 mg, and 225 mg, with some participants taking several hundred mg of oral morphine equivalents daily). Other non‐paracetamol medication included non‐steroidal anti‐inflammatory drugs (NSAIDs), tricyclic antidepressants, or neuroleptics. All studies were at high risk of bias for incomplete outcome data and small size; none was unequivocally at low risk of bias.
None of the studies reported any of our primary outcomes: participants with pain reduction of at least 50%, and at least 30%, from baseline; participants with pain no worse than mild at the end of the treatment period; participants with Patient Global Impression of Change (PGIC) of much improved or very much improved (or equivalent wording). What pain reports there were indicated no difference between paracetamol and placebo when added to another treatment. There was no convincing evidence of paracetamol being different from placebo with regards to quality of life, use of rescue medication, or participant satisfaction or preference. Measures of harm (serious adverse events, other adverse events, and withdrawal due to lack of efficacy) were inconsistently reported and provided no clear evidence of difference.
Our GRADE assessment of evidence quality was very low for all outcomes, because studies were at high risk of bias from several sources.
Authors' conclusions
There is no high‐quality evidence to support or refute the use of paracetamol alone or in combination with opioids for the first two steps of the three‐step WHO cancer pain ladder. It is not clear whether any additional analgesic benefit of paracetamol could be detected in the available studies, in view of the doses of opioids used.
Keywords: Adult; Humans; Acetaminophen; Acetaminophen/administration & dosage; Administration, Oral; Analgesics, Non‐Narcotic; Analgesics, Non‐Narcotic/administration & dosage; Analgesics, Opioid; Analgesics, Opioid/administration & dosage; Anti‐Inflammatory Agents, Non‐Steroidal; Anti‐Inflammatory Agents, Non‐Steroidal/administration & dosage; Antidepressive Agents, Tricyclic; Antidepressive Agents, Tricyclic/administration & dosage; Antipsychotic Agents; Antipsychotic Agents/administration & dosage; Cancer Pain; Cancer Pain/drug therapy; Drug Therapy, Combination; Patient Preference; Quality of Life; Randomized Controlled Trials as Topic
Plain language summary
Paracetamol for cancer pain
Bottom line
There is no evidence to show that paracetamol is useful in treating people with cancer pain, either alone or combined with a morphine‐like drug. Nor is there evidence to disprove that it is useful. There are no good studies evaluating paracetamol for management of cancer pain.
Background
One person in two or three who gets cancer will suffer from pain that becomes moderate or severe in intensity. The pain tends to get worse as the cancer progresses. In 1986, the World Health Organization recommended taking morphine‐like drugs (opioids) for moderate to severe pain from cancer, and non‐opioid drugs like paracetamol, alone for mild to moderate pain, or alongside opioids in people with moderate to severe pain.
Study characteristics
In this review we set out to examine all the evidence on how well paracetamol (alone or with morphine‐like drugs) worked in adults and children with cancer pain. We also wanted to know how many people had side effects, and how severe those side effects were, for example, whether they caused people to stop taking their medicines.
In March 2017, we found three studies with 122 participants. All compared paracetamol plus opioid with the same dose of opioid alone. The studies were small, and were of poor quality. They used different study designs and different ways of showing their pain results. Outcomes of importance to people with cancer pain were not reported.
Key findings
We found no evidence that taking paracetamol alone made any difference to the level of pain experienced. We found no evidence that taking paracetamol together with a morphine‐like drug was better than the morphine‐like drug alone. Paracetamol did not appear to improve quality of life. No conclusions could be reached about side effects. The amount of information and the differences in how studies were reported meant that no conclusions could be made.
Quality of the evidence
The quality of the evidence was very low. Very low‐quality evidence means that we are very uncertain about the impact of paracetamol for treating cancer pain. We do not know whether using paracetamol alone, or in combination with an opioid such as codeine or morphine, is worthwhile.
Summary of findings
for the main comparison.
| Paracetamol plus opioid compared with the same dose of opioid alone for cancer pain | ||||||
|
Patient or population: people with cancer pain Settings: inpatient or outpatient Intervention: paracetamol plus opioid Comparison: same dose of opioid alone | ||||||
| Outcomes | Probable outcome with opioid + paracetamol | Probable outcome with opioid alone | RR (95% CI) | No of studies, participants | Quality of the evidence (GRADE) | Comments |
| Participants with at least 30% or at least 50% reduction in pain | No data | No data | N/A | Very low | Very low quality because no or inadequate data | |
| PGIC much or very much improved | No data | No data | N/A | Very low | Very low quality because no or inadequate data | |
| Mean pain intensity at end of study | No difference between treatment groups | 3 studies, 93 participants | Very low | Very low quality because no or inadequate data | ||
| Pain no worse than mild at one or two weeks (or equivalent) | No data | No data | N/A | Very low | Very low quality because no or inadequate data | |
| Mean quality of life or "well‐being" | No difference between treatment groups | N/A | 3 studies, 93 participants | Very low | Very low quality because no or inadequate data | |
| Participant preference | Better: 15/52 | Better: 9/52 (No different: 28/52) |
Not calculated | 2 studies, 52 participants | Very low | Very low quality because no or inadequate data |
| Adverse events | No difference between groups for specific opioid‐related adverse events | N/A | 2 studies, 80 participants (maximum) | Very low | Very low quality because no or inadequate data | |
| Serious adverse events | None specifically reported. 1 death due to underlying disease ‐ treatment unclear | N/A | 3 studies, 93 participants | Very low | Very low quality because no or inadequate data | |
| CI: Confidence interval; RR: Risk Ratio | ||||||
| Descriptors for levels of evidence (EPOC 2015):
High quality: This research provides a very good indication of the likely effect. The likelihood that the effect will be substantially different† is low.
Moderate quality: This research provides a good indication of the likely effect. The likelihood that the effect will be substantially different† is moderate.
Low quality: This research provides some indication of the likely effect. However, the likelihood that it will be substantially different† is high.
Very low quality: This research does not provide a reliable indication of the likely effect. The likelihood that the effect will be substantially different† is very high. † Substantially different: a large enough difference that it might affect a decision. | ||||||
Background
A previous Cochrane review that examined the evidence for nonsteroidal anti‐inflammatory drugs (NSAIDs) or paracetamol, alone or combined with opioids, for cancer pain was withdrawn in 2015 because it was out of date (McNicol 2015); the date of the last search was 2005.
This is one of three reviews on the efficacy and safety of oral non‐opioid medicines to treat cancer pain, in this case focusing on paracetamol in adults and children. Another review will examine oral NSAIDs in adults (Derry 2017). A separate review will examine the efficacy of NSAIDs for cancer pain in children (Cooper 2017).
Description of the condition
Cancer is estimated to cause over eight million deaths per annum ‐ approximately 13% of deaths worldwide (IARC 2012). Globally, 32 million people are living with cancer, and detailed information for individual countries is available on the WHO website for the International Agency for Research on Cancer (http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx). In the UK alone in 2014, there were around 350,000 new cases of cancer annually, with around 50% of people surviving for 10 years or more after diagnosis (Cancer Research UK 2016).
Cancer pain is perhaps one of the most feared symptoms associated with the disease. Pain may be the first symptom to cause someone to seek medical advice that leads to a diagnosis of cancer, and 30% to 50% of all people with cancer will experience moderate to severe pain (Portenoy 1999). Pain can occur at any time as the disease progresses, but the frequency and intensity of pain tends to increase as the cancer advances (Portenoy 1999; Van den Beuken‐van Everdingen 2016). For people with advanced cancer, some 75% to 90% will experience pain having a major impact on daily living (Wiffen 2016). Pain had a significant negative correlation with quality of life in people with cancer in China, Japan, and Palestine, for example (Deng 2012; Dreidi 2016; Mikan 2016). A recent systematic review has shown that approximately 40% of patients suffered pain after curative treatment, 55% during cancer treatment and 66% in advanced disease. Pain related to cancer is frequently described as distressing or intolerable by more than one‐third of patients (Breivik 2009; Van den Beuken‐van Everdingen 2016).
Cancer pain can be the result of the cancer itself, interventions to treat the cancer, and sometimes other underlying pains. Cancer‐related pain is a mosaic of different types of pain generated through different mechanisms. The biology of pain from bone metastasis may well differ from pain due to obstruction of a viscus (internal organ) or invasion of soft tissue, resulting in differences in responsiveness to analgesics that act via different mechanisms. Prevalence of pain is also linked to cancer type, with head and neck cancer showing the highest prevalence. Age also has an impact, with younger patients experiencing more pain (Prommer 2015). For this review, we will not consider postsurgical pain or specific neuropathic pain conditions.
The current World Health Organization (WHO) cancer pain ladder for adults recommends the use of non‐opioid analgesics, including paracetamol, as the first step on the ladder, with or without an adjuvant (WHO 2017). Non‐opioid analgesics are also to be used on the second and third steps, together with weak or strong opioids. The current National Institute for Health and Care Excellence (NICE) in the UK advises that non‐opioid analgesics alone be used for treating mild pain (0 to 3 on a 0 to 10 pain scale), together with a weak opioid such as codeine or tramadol for mild to moderate pain (3 to 6), and with a strong opioid such as morphine for severe pain (6 to 10) (NICE 2016). Some authorities have suggested that the second step on the ladder could be removed, and replaced with low doses of strong opioids such as morphine (Twycross 2014).
Children with cancer consider pain as the most prevalent symptom, usually resulting from treatment side effects or painful procedures (Twycross 2015). The amount and quality of research on pharmacological treatments for children tends to be poor (Mercadante 2014).
Description of the intervention
Paracetamol (acetaminophen) is available in a very large number of formulations and products with different names, including Panadol and Tylenol. Paracetamol plus codeine often comes with the generic name co‐codamol, and paracetamol plus dihydrocodeine as co‐dydramol. A listing of brand names by country is available but the list is too long to be given here (Drugs.com 2016). Worldwide paracetamol use is measured in thousands of tonnes annually, and questions have been asked about the benefits and risk of such extensive use (Moore 2016).
Paracetamol was first identified as the active metabolite of two older antipyretic drugs, acetanilide and phenacetin, in the late nineteenth century (Axelrod 2003). Since then, it has become one of the most popular antipyretic and analgesic drugs worldwide, and is often also used in combination with other drugs. It became available in the UK on prescription in 1956, and without prescription (over‐the‐counter) in 1963 (PIC 2015). Nonprescription medications are less expensive, more accessible, and have favourable safety profiles relative to many prescription treatments. There have been calls for the position of paracetamol as a widely‐available analgesic to be re‐evaluated, based on an assessment of evidence over the past 130 years (Brune 2015).
Despite a low incidence of adverse effects, paracetamol has a recognised potential for hepatotoxicity and is thought to be responsible for approximately half of all cases of liver failure in the UK (Hawton 2001), and about 40% in the USA (Norris 2008). One study, evaluating all cases of acute liver failure leading to registration for transplantation (ALFT) across seven European countries for a three‐year period, showed that paracetamol overdose was responsible for one‐sixth of cases of ALFT, though this varied considerably between each country (Gulmez 2015). Acute paracetamol hepatotoxicity at therapeutic doses has been judged to be extremely unlikely, despite reports of so‐called 'therapeutic misadventure' (Prescott 2000). However, it has been observed that non‐overdose ALFT is more likely to follow therapeutic‐dose paracetamol exposure than similar NSAID exposure (Gulmez 2013). Legislative changes have been introduced in the UK to restrict pack sizes and the maximum number of tablets permitted in nonprescription sales (CSM 1997), on the basis of evidence that poisoning is lower in countries that restrict availability (Gunnell 1997; Hawton 2001). The contribution of these changes, which were inconvenient and costly (particularly to people with chronic pain), to any observed reductions in incidence of liver failure or death, remains uncertain (Bateman 2014a; Bateman 2014b; Hawkins 2007; Hawton 2013). Changes have also been made in the USA, and professionals have been advised not to dispense prescription combination drugs with more than 325 mg paracetamol (FDA 2015).
There is a substantial public health impact of paracetamol toxicity. In the USA, incidence proportions peaked at age two years and ages 16 to 18 years (Altyar 2015). There have been concerns over the safety of paracetamol in people with compromised hepatic function (people with severe alcoholism, cirrhosis, or hepatitis), but these have not been substantiated (Dart 2000; PIC 2015).
The use of paracetamol during pregnancy has been questioned following reports that it is linked to behavioural problems and hyperkinetic disorders in children whose mothers took it during pregnancy (Liew 2014), and suggestions that it can interfere with sex hormones (Mazaud‐Guittot 2013).
In an analysis of single‐dose studies in migraine, there was no evidence that adverse events were more common with paracetamol 1000 mg than with placebo, and no serious adverse events occurred with paracetamol alone (Derry 2013).
Oral paracetamol has long been used as a first‐line analgesic for a variety of acute and chronic conditions. It has modest efficacy in acute pain and migraine (Derry 2013; Toms 2008), but some randomised trials, systematic reviews, and meta‐analyses have suggested that there is no good evidence for a clinically relevant benefit of paracetamol (as monotherapy) in many chronic pain conditions, such as osteoarthritis and back pain (Machado 2015; Moore 2014a; Williams 2014). There are few or no data for a range of other common painful conditions, including dysmenorrhoea and chronic neck pain. Moreover, accumulating evidence from observational studies indicates a considerable degree of paracetamol toxicity, especially at the upper end of standard analgesic doses (Roberts 2016).
How the intervention might work
The lack of significant anti‐inflammatory activity of paracetamol implies a mode of action distinct from that of NSAIDs; yet, despite years of use and research, the mechanisms of action of paracetamol are not fully understood. NSAIDs act by inhibiting the activity of cyclo‐oxygenase (COX), now recognised to consist of two isoforms (COX‐1 and COX‐2), which catalyse the production of prostaglandins responsible for pain and inflammation. Paracetamol has previously been shown to have no significant effects on COX‐1 or COX‐2 (Schwab 2003), but is now being considered as a selective COX‐2 inhibitor (Hinz 2008). Significant paracetamol‐induced inhibition of prostaglandin production has been demonstrated in tissues in the brain, spleen, and lung (Botting 2000; Flower 1972). A 'COX‐3 hypothesis', wherein the efficacy of paracetamol is attributed to its specific inhibition of a third COX isoform enzyme, COX‐3 (Botting 2000; Chandrasekharan 2002), now has little credibility, and a central mode action of paracetamol is thought to be likely (Graham 2005). Paracetamol metabolism is subject to genetic variation (Zhao 2011).
There is some experimental research in rats to suggest that paracetamol may have an effect in neuropathic pain via cannabinoid receptors (Curros‐Criado 2009; Dani 2007). One single case report suggested intravenous paracetamol was effective for phantom limb pain (Gulcu 2007).
Why it is important to do this review
A previous Cochrane review examined the evidence for NSAIDs or paracetamol, alone or combined with opioids, for cancer pain (McNicol 2015), with the last search date in 2005. There have been few subsequent systematic reviews of the evidence. Nabal found little evidence of efficacy for combinations with opioids (Nabal 2012). A review of paracetamol and NSAIDs concluded that while the role of these non‐opioid drugs remains controversial, the evidence for paracetamol alone was limited (Mercadante 2013).
The evidence of effectiveness of the WHO pain ladder for cancer has been examined several times in the past two decades. These studies reported varying degrees of success, typically between 20% and 100% of people with cancer pain achieving good relief (Azevedo São Leão Ferreira 2006; Carlson 2016; Jadad 1995), with some suggesting that as many as 50% of people with cancer pain are undertreated (Deandrea 2008).
In many countries, opioids are severely restricted, if available at all. This means that many people with cancer will have considerable pain and suffering unless non‐opioid analgesics can be used. This review was designed with the intention of informing policy makers such as the WHO on the possible utility of paracetamol to treat cancer‐related pain. It is hoped that the review will inform patients and carers on the value or otherwise of paracetamol in this context.
Other relevant Cochrane reviews include an assessment of codeine alone and with paracetamol (Straube 2014), and an evaluation of tramadol alone and with paracetamol (Wiffen 2017). For our purposes we wanted to assess any additional efficacy of paracetamol by comparing paracetamol plus opioid with the same dose of opioid alone, a different question to that addressed by those reviews. A number of other reviews have evaluated the evidence for opioids, including buprenorphine (Schmidt‐Hansen 2015a), transdermal fentanyl (Hadley 2013), hydromorphone (Bao 2016), morphine (Wiffen 2016), oxycodone (Schmidt‐Hansen 2015b), and tapentadol (Wiffen 2015).
The standards used to assess evidence in pain trials have changed substantially in recent years, with particular attention being paid to trial duration, withdrawals, and statistical imputation following withdrawal, all of which can substantially alter estimates of efficacy (Moore 2013b). The most important change is the move away from using mean pain scores, or mean change in pain scores, to the number of people who have a large decrease in pain (by at least 50%) (Dworkin 2008; Moore 2013a). Pain intensity reduction of 50% or more correlates with improvements in comorbid symptoms, function, and quality of life generally (Moore 2014). These standards are set out in the PaPaS author and referee guidance for pain studies of the Cochrane Pain, Palliative and Supportive Care Group (PaPaS 2012).
Three additional issues potentially affect how evidence is evaluated.
The first issue is study size and the overall amount of information available for analysis. There are issues over both random chance effects with small amounts of data, and potential bias in small studies, especially in pain (Dechartes 2013; Dechartres 2014; Fanelli 2017; Moore 1998; Nguyen 2017; Nüesch 2010; Thorlund 2011). Cochrane reviews have been criticised for perhaps overemphasising results of underpowered studies or analyses (AlBalawi 2013; Turner 2013). On the other hand, it may be unethical to ignore potentially important information from small studies or to randomise more participants if a meta‐analysis including small, existing studies provided conclusive evidence. In this review, we have therefore chosen to limit analyses to studies with a minimum of 25 participants randomised per treatment group, which we believe has not been done previously.
The second issue is that of study duration. Previous reviews have examined studies of any duration, even in some cases single‐dose studies, or studies lasting one day or less, often with intravenous or intramuscular formulations (McNicol 2015; Mercadante 2013). While short term studies and non‐oral formulations may have some relevance in some circumstances, they have little relevance to the vast majority of people with cancer pain who will be treated with oral paracetamol over weeks, months, or even years. We have therefore chosen to include only studies with five days' duration or longer.
The third issue is that of comparators. Many cancer pain studies involve direct comparisons of one or more formulations of the same drug, as particularly noted for oral morphine (Wiffen 2016). This type of design has limited importance in evaluating the analgesic contribution of a drug, if that is not already well‐established (McQuay 2005). For that reason, we have limited this review to the two comparators that speak to the efficacy of paracetamol in cancer pain, namely the comparison of paracetamol versus placebo, and paracetamol plus opioid versus the same dose of opioid alone. The latter comparison would be similar to methods used for determining dose‐response of analgesics in acute pain (McQuay 2007), or caffeine as an analgesic adjuvant in acute pain (Derry 2014).
Objectives
To assess the efficacy of oral paracetamol (acetaminophen) for cancer pain in adults and children, and the adverse events reported during its use in clinical trials.
Methods
Criteria for considering studies for this review
Types of studies
To be included, studies had to:
be randomised (described as 'randomised' anywhere in the manuscript);
ideally be double‐blind, but we would have included single‐blind or open studies because we expected there to be a limited literature on this important topic, and we desired to be as inclusive as possible;
include a minimum of 25 participants randomised per treatment arm; for cross‐over studies this meant a minimum of 25 participants at the initial randomisation.
have a study duration of at least five days of continuous treatment, with outcomes reported at the end of that period.
We excluded non‐randomised studies, studies of experimental pain, case reports and clinical observations. Studies had to be fully published or available as extended abstracts (e.g. from clinical trial websites); we excluded short (usually conference) abstracts as these are often unreliable (PaPaS 2012).
Types of participants
We included studies of adults with cancer pain of any intensity. We did not find any eligible studies in children. We did not consider postsurgical pain or specific neuropathic pain conditions.
Types of interventions
Orally administered paracetamol for cancer pain, where paracetamol alone was compared with placebo, or where paracetamol was combined with an opioid and compared with the same dose of opioid alone.
Types of outcome measures
Pain had to be measured using a validated assessment tool. For pain intensity, for example, this could be a 100 mm visual analogue scale (VAS) or 11‐point numerical rating scale (no pain to worst pain imaginable), or a four‐point categorical scale (none, mild, moderate, severe), and for pain relief, for example, this could be a 100 mm VAS (no relief to complete relief), or five‐point categorical scale (none, a little, some, a lot, complete or words to that effect). Measures of 30% or greater (moderate) and 50% or greater (substantial) reduction of pain over baseline are recommended outcomes for chronic pain studies from the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) (Dworkin 2008).
A 30% or greater reduction of pain from baseline corresponds to much or very much improved on Patient Global Impression of Change (PGIC), and 50% or greater reduction corresponds to very much or completely improved. We would also use results equivalent to no pain or mild pain, because these are also outcomes acceptable to people with various types of pain (Moore 2013a).
Primary outcomes
Number of participants with pain reduction of 50% or greater from baseline.
Number of participants with pain reduction of 30% or greater from baseline.
Number of participants with pain no worse than mild (Moore 2013a).
Number of participants with PGIC much improved or very much improved (or equivalent wording).
Secondary outcomes
Quality of life.
Use of rescue medication.
Participant satisfaction or preference.
Serious adverse events, including death.
Other adverse events, particularly reports of effects of treatment on somnolence, appetite, or thirst (Wiffen 2014).
Withdrawals due to lack of efficacy, adverse events, or any cause.
Search methods for identification of studies
Electronic searches
We searched the following databases without language or date restrictions.
The Cochrane Central Register of Controlled Trials (CENTRAL) (via CRSO) on 27 March 2017.
MEDLINE (via Ovid) from 1946 to 27 March 2017.
Embase (via Ovid) from 1974 to 27 March 2017.
We used a combination of MeSH (or equivalent) and text word terms and tailored search strategies to individual databases. The search strategies for CENTRAL, MEDLINE, and Embase are in Appendix 1, Appendix 2, and Appendix 3, respectively.
Searching other resources
We searched the metaRegister of controlled trials in ClinicalTrials.gov (www.clinicaltrials.gov) and the WHO International Clinical Trials Registry Platform (ICTRP) (http://apps.who.int/trialsearch/) for unpublished and ongoing trials. In addition, we checked reference lists of reviews and retrieved articles for additional studies and performed citation searches on key articles. We did not contact authors for additional information.
Data collection and analysis
Selection of studies
Two review authors (RAM, SD) independently read the abstract of each study identified by the search, eliminated studies that clearly did not satisfy inclusion criteria, and obtained full copies of the remaining studies. Two review authors (RAM, SD) then read these studies independently to select relevant studies for inclusion. In the event of disagreement, a third review author (PW) was available to adjudicate. We did not anonymise the studies before assessment. We have included a PRISMA flow chart in the review to show the status of identified studies as recommended in Section 11.2.1 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We included studies in the review if they satisfied our inclusion criteria, irrespective of whether measured outcome data were reported in a 'usable' way.
Data extraction and management
Two review authors (RAM, SD) independently extracted data using a standard form and checked for agreement before entry into Review Manager (RevMan) (RevMan 2014). We included information about the number of participants treated and demographic details, type of cancer, drug and dosing regimen, study design (placebo or active control) and methods, study duration and follow‐up, analgesic outcome measures and results, withdrawals and adverse events. If necessary, we would have collated multiple reports of the same study, so that each study rather than each report was the unit of interest in the review. We collected characteristics of the included studies in sufficient detail to complete a Characteristics of included studies table.
Assessment of risk of bias in included studies
Two review authors (RAM, SD) independently assessed risk of bias for each study, using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Chapter 8, Higgins 2011) and adapted from those used by the Cochrane Pregnancy and Childbirth Group, with any disagreements resolved by discussion. We completed a 'Risk of bias' table for each included study using the 'Risk of bias' tool in RevMan (RevMan 2014).
We assessed the following for each study.
Random sequence generation (checking for possible selection bias). We assessed the method used to generate the allocation sequence as: low risk of bias (any truly random process, e.g. random number table; computer random number generator); unclear risk of bias (method used to generate sequence not clearly stated). We excluded studies using a non‐random process (e.g. odd or even date of birth; hospital or clinic record number).
Allocation concealment (checking for possible selection bias). The method used to conceal allocation to interventions prior to assignment determines whether intervention allocation could have been foreseen in advance of, or during, recruitment or changed after assignment. We assessed the methods as: low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes); unclear risk of bias (method not clearly stated); high risk of bias, where study did not conceal allocation (e.g. open list).
Blinding of participants and personnel (checking for possible performance bias). We assessed the methods used to blind study participants and personnel from knowledge of which intervention a participant received. We assessed methods as: low risk of bias (study stated that it was blinded and described the method used to achieve blinding, such as identical tablets matched in appearance or smell, or a double‐dummy technique); unclear risk of bias (study stated that it was blinded but did not provide an adequate description of how it was achieved); high risk of bias (study participants or personnel, or both, not blinded).
Blinding of outcome assessment (checking for possible detection bias). We assessed the methods used to blind study participants and outcome assessors from knowledge of which intervention a participant received. We assessed the methods as: low risk of bias (study had a clear statement that outcome assessors were unaware of treatment allocation, and ideally described how this was achieved); unclear risk of bias (study stated that outcome assessors were blind to treatment allocation but lacked a clear statement on how it was achieved); high risk of bias (outcome assessment not blinded).
Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data). We assessed the methods used to deal with incomplete data as: low risk (fewer than 10% of participants did not complete the study or used ‘baseline observation carried forward’ analysis, or both); unclear risk of bias (used 'last observation carried forward' analysis); high risk of bias (used 'completer' analysis).
Reporting bias due to selective outcome reporting (reporting bias). We checked if an a priori study protocol was available and if all outcomes of the study protocol were reported in the publications of the study. We assessed the methods used to deal with incomplete data as: low risk of reporting bias if the study protocol was available and all of the study’s prespecified (primary and secondary) outcomes that were of interest in the review were reported in the pre‐specified way, or if the study protocol was not available but it was clear that the published reports included all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon); high risk of reporting bias if not all of the study’s pre‐specified primary outcomes were reported; one or more primary outcomes was reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting was provided, such as an unexpected adverse effect); one or more outcomes of interest in the review were reported incompletely so that they could not be entered in a meta‐analysis; the study report did not include results for a key outcome that would be expected to have been reported for such a study; and unclear risk of bias risk of bias if insufficient information is available to permit judgement of ‘Low risk’ or ‘High risk’.
Size of study (checking for possible biases confounded by small size (Dechartes 2013; Dechartres 2014; Moore 1998; Nüesch 2010; Thorlund 2011)). We assessed studies as being at low risk of bias (200 participants or more per treatment arm); unclear risk of bias (50 to 199 participants per treatment arm); high risk of bias (fewer than 50 participants per treatment arm).
Measures of treatment effect
We planned to use dichotomous data to calculate risk difference (RD) or risk ratio (RR) with 95% confidence intervals (CIs) using a fixed‐effect model, and calculate numbers needed to treat for one additional beneficial outcome (NNT) as the reciprocal of the absolute risk reduction (McQuay 1998). For unwanted effects, the number needed to treat becomes the number needed to treat for one additional harmful outcome (NNH), and is calculated in the same manner.
We planned to use the following terms to describe adverse outcomes in terms of harm or prevention of harm.
When significantly fewer adverse outcomes occurred with paracetamol than with control (placebo or active control), we used the term number needed to treat to prevent one event (NNTp).
When significantly more adverse outcomes occurred with paracetamol compared with control (placebo or active control) we used the term number needed to treat for an additional harmful outcome or cause one event (NNH).
We did not plan to use continuous data for the primary outcome because it is inappropriate where there is an underlying skewed distribution, as is usually the case with analgesic response.
Unit of analysis issues
The unit of randomisation was the individual participant.
Dealing with missing data
We planned to use intention‐to‐treat (ITT) analyses: participants who were randomised, took the study medication, and gave a minimum of one post‐baseline assessment. We have reported per‐protocol data in the absence of ITT data.
Assessment of heterogeneity
We planned to assess statistical heterogeneity using L'Abbé plots, a visual method for assessing differences in results of individual studies (L'Abbé 1987), and by use of the I2 statistic. We anticipated that there could be an effect of differences between participants, environment (inpatient versus outpatient), and outcome measures. We planned to explore these with subgroup and sensitivity analyses where there were sufficient data, recognising the difficulties of assessing heterogeneity with small numbers of small studies (Gavaghan 2000; IntHout 2015). In the event, there were insufficient data to assess heterogeneity.
Assessment of reporting biases
We planned to use dichotomous data of known utility (Moore 2010a; Moore 2013a). The review would not depend on what additional information authors of the original studies chose to report or not.
We planned to undertake an assessment of publication bias if there were sufficient data for meta‐analysis, using a method designed to detect the amount of unpublished data with a null effect required to make any result clinically irrelevant (usually taken to mean an NNT of 10 or higher) (Moore 2008). In the event, there were insufficient data to assess publication bias.
Data synthesis
We planned to undertake a quantitative synthesis and present data in forest plots if there were sufficient data. In the event of substantial clinical heterogeneity, we would switch off the totals in the forest plots.
We would undertake a meta‐analysis only if participants, interventions, comparisons, and outcomes were judged to be sufficiently similar to ensure an answer that is clinically meaningful.
We would undertake a meta‐analysis only where there were data from at least two studies and 200 participants for analysis.
We planned to use RevMan for meta‐analysis (RevMan 2014) and Excel for NNT and NNH.
In the event, there were insufficient data for pooling of data for any outcome.
Quality of the evidence
We used the GRADE system to assess the quality of the evidence related to the key outcomes listed in Types of outcome measures, as appropriate (Appendix 4). Two review authors (RAM, SD) independently rated the evidence for each outcome.
We paid particular attention to inconsistency, where point estimates vary widely across studies or confidence intervals (CIs) of studies show minimal or no overlap (Guyatt 2011), and to the potential for publication bias, based on the amount of unpublished data required to make the result clinically irrelevant (Moore 2008).
Lastly, there may be circumstances where the overall rating for a particular outcome needs to be adjusted as recommended by GRADE guidelines (Guyatt 2013a). For example, if there are so few data that the results are highly susceptible to the random play of chance, or if a study uses last observation carried forward (LOCF) imputation in circumstances where there are substantial differences in adverse event withdrawals, one would have no confidence in the result, and would need to downgrade the quality of the evidence by three levels, to very low quality. In circumstances where there were no data reported for an outcome, we have reported the level of evidence as very low quality (Guyatt 2013b).
In addition, we are aware that many Cochrane reviews are based largely or wholly on small underpowered studies, and that there is a danger of drawing erroneous conclusions of evidence based on inadequate information (AlBalawi 2013; Brok 2009; Roberts 2015; Turner 2013).
'Summary of findings' table
We have included a 'Summary of findings' table as set out in the Pain, Palliative and Supportive Care Review Group author guide (PaPaS 2012) and recommended in Chapter 4.6.6 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We present the main findings in a simple tabular format, to include key information concerning the quality of evidence, the magnitude of effect of the interventions examined, the sum of available data on the outcomes of at least 30% and at least 50% pain relief, PGIC much or very much improved, pain no worse than mild at one or two weeks, adverse events, and serious adverse events. In addition, we have also included other measures of efficacy or harm (mean pain intensity at end of study, quality of life or well‐being at end of treatment, and patient satisfaction or preference).
For the 'Summary of findings' table we used the following descriptors for levels of evidence (EPOC 2015).
High:
This research provides a very good indication of the likely effect. The likelihood that the effect will be substantially different† is low.
Moderate:
This research provides a good indication of the likely effect. The likelihood that the effect will be substantially different† is moderate.
Low:
This research provides some indication of the likely effect. However, the likelihood that it will be substantially different† is high.
Very low:
This research does not provide a reliable indication of the likely effect. The likelihood that the effect will be substantially different† is very high.
† Substantially different: a large enough difference that it might affect a decision.
Subgroup analysis and investigation of heterogeneity
We planned several possible subgroup analyses, depending on the availability of data.
Because we expected that many studies would have a cross‐over design that could impede meta‐analysis (Elbourne 2002), we planned to examine cross‐over and parallel‐group designs separately.
We planned to investigate whether subgroup analysis by dose of paracetamol (up to 2000 mg/day, 2001 mg/day to 4000 mg/day) was possible.
We planned to analyse separately studies with paracetamol alone, and paracetamol combined with opioid. We anticipated that these studies might also reflect different levels of initial pain intensity.
We planned no other subgroup analyses because the data were expected to be sparse, with small numbers of small trials. In the event, there were insufficient data for any subgroup analysis.
Sensitivity analysis
We did not plan any sensitivity analyses because the data were expected to be sparse, with small numbers of small trials.
Results
Description of studies
Results of the search
Searches identified 261 articles in CENTRAL, 326 articles in MEDLINE, 834 articles in Embase, and four additional study reports in clinical trial registries. After screening and assessment of relevant full texts, we included three studies and excluded six studies.
Two studies are awaiting classification. NCT00152854 has completed, but with only 12 participants and no study results posted; there were insufficient data to judge methodological criteria and it would probably be excluded because of its small size. We have been unable to obtain the full text of Pacilio 1989.
One study with an estimated enrolment of 140 participants is ongoing, with an expected completion date of April 2019 (NCT02706769). This double‐blind study appears to use a randomised withdrawal design, in which participants taking daily regular strong opioids plus 4 x 1000 mg paracetamol are randomised to continue with opioid plus paracetamol or opioids alone.
Figure 1 illustrates the flow of studies in the review.
1.
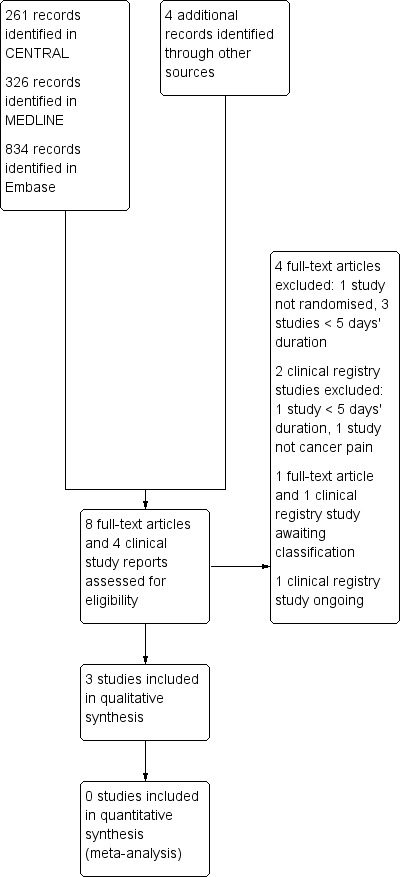
Study flow diagram.
Included studies
We included three studies (Axelsson 2003; Cubero 2010; Israel 2010), all of which were randomised, double‐blinded, and placebo‐controlled. They initially randomised 122 participants, of whom 95 completed the studies.
One study (Cubero 2010) used a parallel group design and had a treatment duration of one week. Two studies used a cross‐over design, with treatment periods of one week (Axelsson 2003) and five days (Israel 2010). Neither cross‐over study had a washout period, but Israel 2010 stated that data from only the last four days were used in analyses to avoid carryover effects. We used results from both parts of the cross‐over.
All studies used paracetamol as an add‐on to established treatment with strong opioids and other non‐paracetamol medication. Cubero 2010 switched participants abruptly ("stop/start") from stable doses of morphine to equivalent doses of methadone, with or without paracetamol. No studies tested paracetamol alone.
Each study included both male and female participants with various types of cancer; mainly colorectal, prostate, breast, and pancreas. The mean ages ranged from 56 to 72 years (range 19 to 86). In Axelsson 2003, participants had baseline pain intensity on opioid treatment of less than 4/10 (median 2 on scale 0 to 3); in Cubero 2010, participants had a median baseline pain intensity on treatment of 5/10 for the paracetamol arm and 3.5/10 for the placebo arm; in Israel 2010, participants had a baseline pain intensity of at least 2/10.
The median daily dose of oral morphine was 70 mg (range 20 mg to 440 mg) in Axelsson 2003, 60 mg (40 mg to 540 mg) in Cubero 2010, and 225 mg (200 mg to 900 mg, plus one participant taking 9000 mg) in Israel 2010.
Further details are in the Characteristics of included studies table.
Two studies are awaiting assessment. NCT00152854 was a randomised, double‐blind cross‐over study in which paracetamol or placebo was added to existing opioid therapy for periods of seven days. Participants were taking at least 60 mg morphine equivalents per day. The study has completed, but we were unable to find any results, other than only 12 participants completed. Pacilio 1989 compared paracetamol with flupirtine in cancer pain; no further details were available, and would probably not be included.
Excluded studies
We excluded six studies (ACTRN12610000893000; Axelsson 2008; Danninger 1993; JPRN‐UMIN000009292; Nickles 2016; Stockler 2004), because the treatment periods were less than five days or they were not randomised. Further details are in the Characteristics of excluded studies table.
Risk of bias in included studies
Risk of bias in individual studies is shown in Figure 2.
2.
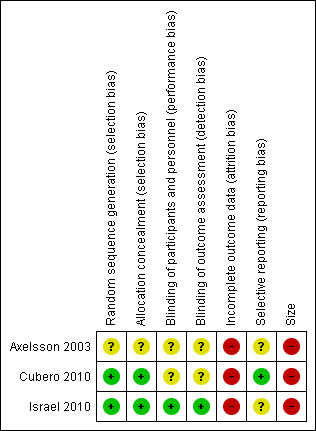
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All three studies were randomised, but one did not adequately describe the methods used to generate the random sequence or to conceal the allocation sequence (Axelsson 2003, reported as a letter).
Blinding
All three studies were double‐blind, but only one adequately described the method used to maintain the blinding (Israel 2010).
Incomplete outcome data
We judged all three studies at high risk of attrition bias because they had substantial attrition (> 10%) and analysed only the participants who completed the study.
Selective reporting
We judged one study to have low risk of bias because there was an on‐line protocol (Cubero 2010). The other two studies were at unclear risk of bias for selective reporting. We did not have access to protocols to check for missing outcomes, but all relevant outcomes specified in the publication were reported.
Other potential sources of bias
All three studies included fewer than 50 participants per treatment arm and we judged them at high risk of bias due to size.
Effects of interventions
See: Table 1
Efficacy
A summary of results for efficacy outcomes in individual studies is available in Appendix 5 and Table 1.
Pain outcomes
No studies tested paracetamol alone.
None of the studies reported any of our primary outcomes: participants with pain reduction of at least 50%, and at least 30%, from baseline; participants with pain no worse than mild at the end of the treatment period; participants with PGIC of much improved or very much improved (or equivalent wording).
All studies (93 participants analysed) reported no difference between paracetamol plus opioid and placebo plus opioid for mean pain intensity measures at the end of the treatment period. Cubero 2010 also found no difference between treatment arms for time to return to baseline pain intensity following an abrupt switch from morphine to methadone, either with or without paracetamol.
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Quality of life
Two studies (71 participants analysed) reported that there was no difference between participants treated with paracetamol and placebo for quality of life assessments at the end of the treatment period (Axelsson 2003; Cubero 2010). The other study (22 participants analysed) reported no difference in 'well‐being' between the interventions (Israel 2010).
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Use of rescue medication
Israel 2010 reported no difference between paracetamol and placebo arms for use of rescue medication for episodes of breakthrough pain. Cubero 2010 used requirement for rescue medication to adjust the dose of methadone.
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Participant satisfaction or preference
The two cross‐over studies reported that pain was better with paracetamol in 15/52 participants, better with placebo in 9/52 participants, and no different in 28/52 participants after five or seven days of treatment (Axelsson 2003; Israel 2010).
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Harm
A summary of results for adverse outcomes in individual studies is available in Appendix 6.
Serious adverse events
None of the studies specifically reported any serious adverse events, but there was one death due to underlying disease in Cubero 2010. It was not clear which treatment the participant was receiving.
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Other adverse events
Axelsson 2003 did not report on adverse events. Cubero 2010 reported no difference between groups for intensity of symptoms of constipation, xerostomia (dry mouth), nausea, vomiting, and somnolence. Israel 2010 found no difference between groups for intensity of nausea, drowsiness, unclear thinking, and constipation.
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Withdrawal due to adverse events
None of the studies specifically reported on withdrawals due to adverse events.
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Withdrawal due to lack of efficacy
Four participants in Cubero 2010 withdrew early due to intense pain following the switch from morphine to methadone, but there were no data for treatment arms with, and without paracetamol. One participant in Israel 2010 withdrew early because of 'unstable pain' while receiving paracetamol.
We assessed this as very low‐quality evidence because of high risk of bias and small size.
Discussion
Summary of main results
Few studies met the criteria for inclusion, particularly the nature of the efficacy results presented. Thus, the results of the studies available for paracetamol for cancer pain are insufficient to allow any conclusions to be drawn about its efficacy or harm in treating cancer pain. The evidence is insufficient to support or refute its use.
No studies were found for the use of paracetamol alone in mild or moderate cancer pain. No studies were found using paracetamol alone or in combination with an opioid in children.
The three available studies examined the use of paracetamol plus an opioid versus the opioid alone in studies where average pain scores were indicative of mild to moderate pain, with scores of between 2/10 and 5/10 on a 0 to 10 VAS scale. These showed no obvious additional benefit of paracetamol in terms of pain relief, quality of life, or participant satisfaction or preference. However, the median doses of daily morphine used were 60 mg, 70 mg, and 225 mg, with some individuals taking up to several hundred mg daily or more. In the circumstance, it may be argued that any additional analgesic effect of oral paracetamol would be difficult to detect.
Excluded studies were of short duration, not randomised, or type of pain was not cancer pain. We know of one study outside our scope that randomly compared non‐steroidal anti‐inflammatory drugs (NSAIDs), aspirin, and paracetamol, without placebo, in a cross‐over design for one week each, but in a small number (typically 15) of participants (Ventafridda 1990). The paracetamol dose was apparently 1500 mg daily, and it demonstrated less pain relief at that dose than NSAIDs or aspirin at the doses used.
Reviews of opioids for cancer pain have used a primary efficacy outcome of people with moderate or severe cancer pain reduced to mild pain or no pain within 14 days of starting treatment, and some have reported that as many as 96% can achieve this outcome where it is reported (Hadley 2013; Wiffen 2016). While this is a methodologically difficult outcome to evaluate in people with initial mild or moderate pain, it was one of the primary outcomes sought, but it was not reported in the three included studies.
Reporting of harms provided no useful information, and could not be expected to do so given the small size of the studies, individually and together.
Where there are small numbers of small studies, there is a situation where a positive bias in favour of a therapy might be found (Dechartes 2013; Dechartres 2014; Fanelli 2017; Nguyen 2017; Nüesch 2010) even by the random play of chance (Brok 2009; Moore 1998; Thorlund 2011), and overemphasising results of underpowered studies or analyses has been criticised (AlBalawi 2013; Roberts 2015; Turner 2013). Despite having only small studies in this review, no positive effect of paracetamol was evident.
The lack of evidence of effect of paracetamol for cancer pain is similar to the situation with musculoskeletal (Machado 2015; Saragiotto 2016), and neuropathic pain (Wiffen 2016), as well as a number of other chronic pain conditions (Moore 2016).
Overall completeness and applicability of evidence
This review highlights our lack of knowledge about the effectiveness of paracetamol for cancer pain. The WHO ladder recommends non‐opioid analgesics for mild to moderate pain in the first two steps of the WHO ladder (WHO 2017), and paracetamol in many countries is the mainstay of the first two steps.
No studies addressed the use of paracetamol alone (first step), and while the three included studies addressed paracetamol added to opioids, there was only low‐quality evidence for all outcomes. Only 122 participants were randomised in the three included studies, fewer than the 140 in an ongoing study that might be more instructive (NCT02706769), at least for the combination of paracetamol with strong opioids.
None of the studies reported on any of the primary outcomes of efficacy, which are known to be important to people with pain (Moore 2013a). None of the available evidence addresses other important outcomes, such as quality of life, reducing sweats, or improving sleep.
Quality of the evidence
Our GRADE judgement was very low quality for all outcomes. Very low quality means that this research does not provide a reliable indication of the likely effect. The likelihood that the effect will be substantially different is very high.
Studies were small in size and number. All were at high risk of bias for incomplete outcome data and size; no study was unequivocally at low risk of bias for all criteria.
Potential biases in the review process
We are unaware of any biases in the review process. A number of the authors prescribe or have prescribed paracetamol for cancer pain, or have been involved with its use in people with cancer pain.
Agreements and disagreements with other studies or reviews
Our findings are in broad agreement with a previous Cochrane review (McNicol 2015) and other reviews in adults (Mercadante 2013; Nabal 2012), and children (Mercadante 2014). In this review, we included only studies with a minimum treatment period of five days, excluding some studies of short duration in these earlier reviews, but allowing any pain relieving effects of paracetamol that might be seen in clinical practice to emerge.
Authors' conclusions
Implications for practice.
For people with cancer pain
The amount and quality of evidence around the use of paracetamol for treating cancer pain is low. The small amount of evidence we have does not indicate that it has any pain‐relieving effects or makes any improvement to quality of life. No judgement can be made about adverse events or withdrawals.
For clinicians
There is no evidence for paracetamol alone. The evidence we have is from add‐on studies with oral morphine doses of 60 mg daily or above, when any additional analgesic effect of oral paracetamol would be difficult to detect. It may be possible to reduce the drug burden for people with cancer pain taking such large amounts of oral morphine equivalents, but we have no evidence that this is the case.
The amount and quality of evidence around the use of paracetamol for treating cancer pain is low. There is no evidence supporting or refuting the use of paracetamol on the first and second steps of the WHO ladder. The small amount of evidence we have for the use of paracetamol combined with opioids does not indicate that it has any additional pain‐relieving effects or makes any improvement to quality of life. No judgement can be made about adverse events or withdrawals.
For policy makers
The amount and quality of evidence around the use of paracetamol for treating cancer pain is low. There is no evidence supporting or refuting the use of paracetamol on the first step of the WHO ladder. The small amount of evidence we have for the use of paracetamol combined with strong opioids does not indicate that it has any additional pain‐relieving effects or makes any improvement to quality of life. No judgement can be made about adverse events or withdrawals.
For funders
The amount and quality of evidence around the use of paracetamol for treating cancer pain is low. There is no evidence supporting or refuting the use of paracetamol on the first step of the WHO ladder. The small amount of evidence we have for the use of paracetamol combined with strong opioids does not indicate that it has any additional pain‐relieving effects or makes any improvement to quality of life. No judgement can be made about adverse events or withdrawals.
Implications for research.
General
This review on paracetamol for cancer pain reveals major problems with the evidence available. The WHO pain ladder is now over 30 years old, and remains probably the most‐used and best‐understood pain guidance worldwide. Despite its obvious importance there are few studies that clearly demonstrate how best to perform a study on the lower two steps, which relate to the treatment of mild and moderate pain with non‐opoid drugs like paracetamol, alone or in combination with weak opioids. As best we know there are no ongoing studies examining the use of paracetamol alone for mild to moderate pain for the first step of the WHO ladder. We know of one ongoing study examining paracetamol plus opioid for the second or third step of the ladder. In this study, participants with moderate to severe pain (3/10 to 9/10) who are taking daily opioid plus 4 x 1000 mg paracetamol are randomised to continued treatment with the combination or the opioid alone.
Design
Several methodological issues stand out.
The first is the use of outcomes of value to people with cancer pain. Existing trials are designed more for purposes of registration and marketing than informing and improving clinical practice, often because the outcomes chosen are average pain scores, or statistical differences, and rarely how many individuals achieve satisfactory pain relief. In the situation where initial pain is mild or moderate, some consideration needs to be given to what constitutes a satisfactory outcome. The situation is somewhat different to that of strong opioids in cancer pain that are used for moderate to severe pain.
The second is the time taken to achieve good pain relief. We have no information about what constitutes a reasonable time to achieve a satisfactory result. Initially, this may best be approached with a Delphi methodology.
The third is design. Studies with cross‐over design often have significant attrition. Parallel group designs may be preferable, and while this is a matter of debate (Bell 2006), considerable thinking has already gone into study design.
The fourth is size. The studies were small, and, combined with cross‐over design and consequent attrition, ended up reporting on very few participants. Much larger studies of several hundred participants or more are needed.
The fifth is the dose of opioid allowable in add‐on studies to test the analgesic efficacy or effectiveness of oral paracetamol. In the circumstance of high oral opioid doses, additional benefit is unlikely to be measurable, and some upper limit of opioid dose may be needed.
The sixth is that in the current era of precision medicine investigator may have an opportunity to conduct clinical trials involving specific aetiologies of cancer pain, or accrue sufficient numbers of participants to conduct well‐powered subgroup analyses.
There are some other design issues that might be addressed. Most important might be a clear decision concerning the gold‐standard treatment comparator. Placebo‐controlled studies in cancer pain are unlikely to be ethically feasible (Bell 2006). It may be that low‐dose oral morphine is a suitable comparator, as a suggested alternative treatment for mild to moderate pain (Twycross 2014).
Measurement (endpoints)
Trials need to consider the additional endpoints of no worse than mild pain and the impact of morphine on symptoms that raise serious concerns such as consciousness, appetite, and thirst, outcomes identified previously as important (Wiffen 2014). The choice of measures to be used in cancer pain studies is not necessarily straightforward.
Other
Prospective randomised trials are the obvious design of choice, but other pragmatic designs may be worth considering. Studies could incorporate initial randomisation but a pragmatic design in order to provide immediately‐relevant information on effectiveness and costs. Such designs in pain conditions have been published (Moore 2010b).
What's new
| Date | Event | Description |
|---|---|---|
| 19 February 2020 | Amended | Clarification added to Declarations of interest. |
| 5 February 2019 | Review declared as stable | See Published notes. |
History
Protocol first published: Issue 4, 2017 Review first published: Issue 7, 2017
| Date | Event | Description |
|---|---|---|
| 28 May 2019 | Amended | Contact details updated. |
Notes
A restricted search in January 2019 did not identify any potentially relevant studies likely to change the conclusions. Therefore, this review has now been stabilised following discussion with the authors and editors. The review will be re‐assessed for updating in five years. If appropriate, we will update the review before this date if new evidence likely to change the conclusions is published, or if standards change substantially which necessitates major revisions.
Acknowledgements
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Pain, Palliative and Supportive Care Review Group. Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, National Health Service (NHS), or the Department of Health.
Institutional support was provided by the Oxford Pain Relief Trust.
Appendices
Appendix 1. Search strategy for CENTRAL (via CRSO)
MESH DESCRIPTOR Acetaminophen EXPLODE ALL TREES (1951)
((acetaminophen or paracetamol or Panadol or Tylenol)):TI,AB,KY (6135)
1 OR 2 (6135)
MESH DESCRIPTOR Neoplasms EXPLODE ALL TREES (48784)
(neoplasm* or malignan* or tumour* or tumor* or cancer* or carcinoma*):TI,AB,KY (112035)
4 OR 5
MESH DESCRIPTOR Pain EXPLODE ALL TREES (34252)
(pain* or nocicept* or neuropath*):TI,AB,KY (99145)
7 OR 8 (104045)
3 AND 6 AND 9 (261)
Appendix 2. Search strategy for MEDLINE (via Ovid)
Acetaminophen/ (16153)
(acetaminophen or paracetamol or Panadol or Tylenol).mp. (22308)
1 or 2 (22308)
exp Neoplasms/ (2960845)
(neoplasm* or malignan* or tumour* or tumor* or cancer* or carcinoma*).mp. (3243178)
4 or 5 (3576397)
exp Pain/ (348792)
(pain* or nocicept* or neuropath*).mp. (681490)
7 or 8 (755409)
randomized controlled trial.pt. (456415)
controlled clinical trial.pt. (93323)
randomized.ab. (348139)
placebo.ab. (171162)
drug therapy.fs. (1966014)
randomly.ab. (239416)
trial.ab. (363498)
10 or 11 or 12 or 13 or 14 or 15 or 16 (2660928)
3 and 6 and 9 and 17 (326)
Appendix 3. Search strategy for Embase (via Ovid)
Acetaminophen/ (66355)
(acetaminophen or paracetamol or Panadol or Tylenol).mp. (82360)
1 or 2 (82360)
exp Neoplasms/ (4021032)
(neoplasm* or malignan* or tumour* or tumor* or cancer* or carcinoma*).mp. (4471110)
4 or 5 (4961166)
exp Pain/ (1137329)
(pain* or nocicept* or neuropath*).mp. (1309716)
7 or 8 (1577050)
(random* or factorial* or crossover or "cross over" or cross‐over).tw. (1253304)
(placebo* or (doubl* adj blind*) or (singl* adj blind*)).tw. (331342)
(assign* or allocat*).tw. (420314)
crossover procedure/ (55920)
double‐blind procedure/ (487853)
Randomized Controlled Trial/ (487853)
10 or 11 or 12 or 13 or 14 or 15 (1674765)
3 and 6 and 9 and 16 (834)
Appendix 4. GRADE: criteria for assigning grade of evidence
The GRADE system uses the following criteria for assigning a quality level to a body of evidence (Chapter 12, Higgins 2011).
High: randomised trials; or double‐upgraded observational studies.
Moderate: downgraded randomised trials; or upgraded observational studies.
Low: double‐downgraded randomised trials; or observational studies.
Very low: triple‐downgraded randomised trials; or downgraded observational studies; or case series/case reports.
Factors that may decrease the quality level of a body of evidence are:
limitations in the design and implementation of available studies suggesting high likelihood of bias;
indirectness of evidence (indirect population, intervention, control, outcomes);
unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses);
imprecision of results (wide confidence intervals);
high probability of publication bias.
Factors that may increase the quality level of a body of evidence are:
large magnitude of effect;
all plausible confounding would reduce a demonstrated effect or suggest a spurious effect when results show no effect;
dose‐response gradient.
Appendix 5. Summary of results in individual studies: efficacy
| Study | Intervention | Participants with at least 50% and at least 30% reduction in pain | Participants with pain no worse than mild | Participants with PGIC of much improved or very much improved | Other measures of pain intensity or pain relief |
| Axelsson 2003 | In addition to morphine MR: (1) Paracetamol 4 x 100 mg daily (2) Placebo |
Not reported | Not reported | Not reported | Less pain with: (1) 9/30 (2) 8/30 No difference: 13/30 End of period questionnaires for PI and QoL did not detect any difference |
| Cubero 2010 | In addition to calculated dose of methadone: (1) Paracetamol 4 x 750 mg daily (2) Placebo |
Not reported | Not reported | Not reported | Mean decrease in PI at 7 days: (1) 1.09/10 (± 3.19) (2) 0.79/10 (± 2.32) Same effect for faces scale No significant difference in PI or QoL, or time to return to baseline PI between groups |
| Israel 2010 | In addition to all usual stable non‐paracetamol medication: (1) Paracetamol 4 x 1000 mg daily (2) Placebo | Not reported | Not reported | Not reported | No difference in rated PI (mean data) Pain better with: (1) 6/22 (2) 1/22 Undecided 15/22 |
| MR: modified release; PGIC: Patient Global IMpression of Change; PI: pain intensity; QoL: quality of life. | |||||
Appendix 6. Summary of results in individual studies: rescue medication, adverse events, withdrawals
| Study | Intervention | Use of rescue or breakthrough medication | Participants with any adverse event and serious adverse events | Participants with specific adverse events | Withdrawals |
| Axelsson 2003 | In addition to morphine MR: (1) Paracetamol 4 x 100 mg daily (2) Placebo |
Not reported | Not reported | Not reported | 12 participants dropped out after median 2 days (0 ‐ 9) due to rapid deterioration, septicaemia, nausea, difficulty swallowing, and other causes not obviously related to the study |
| Cubero 2010 | In addition to calculated dose of methadone: (1) Paracetamol 4 x 750 mg daily (2) Placebo |
Not reported, methadone dose adjusted according to use | No difference between groups for intensity of symptoms: constipation, xerostomia, nausea, vomiting, somnolence | Not reported | 6 participants withdrew early due to intense pain (4), somnolence (1), incoercible vomiting (1); 1 withdrew informed consent; 1 died due to underlying disease |
| Israel 2010 | In addition to all usual stable non‐paracetamol medication: (1) Paracetamol 4 x 1000 mg daily (2) Placebo | No difference in breakthrough medication | Not reported | No difference between groups for intensity of nausea, drowsiness, unclear thinking, and constipation | (1) 1 Participant had unstable pain and another had protocol violation in second treatment period (2) 3 participants had fever, 1 had rapid deterioration, 2 had protocol violations in first period; 1 had fever in second period 8/9 withdrawals had used regular paracetamol before study |
| MR: modified release. | |||||
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Axelsson 2003.
| Methods | Randomised, double‐blind, placebo‐controlled, cross‐over study Treatment for 7 days with each intervention, no washout |
|
| Participants | Advanced cancer (mainly prostate, pancreas, breast, colorectal), well‐controlled pain (< 4/10), stable opioid doses) receiving oral modified‐release morphine with concurrent paracetamol Excluded: chemotherapy, radiotherapy, strontium therapy within 2 months, started amitriptyline within 1 month, started corticosteroids or NSAIDs within 2 weeks N = 42 (30 completed) Completers: M 19, F 11 Median age 72 years (range 38 to 86) Median PI 2 (range 0 to 3) Median 24‐hour dose morphine 70 mg (range 20 mg to 440 mg) |
|
| Interventions | In addition to stable dose of oral modified‐release morphine: Paracetamol 4 x 1000 mg daily Placebo |
|
| Outcomes | Average daily PI: NRS (0 to 10) Additional morphine consumed Quality of life at baseline and end of each treatment period At end of study, judgement about in which period pain and QoL was better |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Method used to blind participants and personnel not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Method used to blind outcome assessment not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis; 12/42 (29%) did not complete |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available, report as letter only. All relevant specified outcomes reported |
| Size | High risk | < 50 participants per treatment arm |
Cubero 2010.
| Methods | Randomised, double‐blind, placebo‐controlled, parallel group study Participants switched (stop/start) from oral morphine to equivalent dose of oral methadone plus either oral paracetamol or placebo Treatment for 1 week |
|
| Participants | Cancer patients (mainly colorectal, prostate, breast) on stable dose morphine ≥ 1 week
Excluded: receiving radiotherapy, severe hepatic or renal dysfunction, cognitive alterations, use of paracetamol within 48 hours N = 49 (all completing) M 26, F 23 Median age 59 (19 to 81) Median baseline PI: 5/10 (paracetamol), 3.5/10 (placebo) PI range 0 to 10 Median dose of oral morphine 60 mg (40 mg to 540 mg) |
|
| Interventions | In addition to calculated dose of methadone: Paracetamol 4 x 750 mg daily, n = 24 Placebo, n = 25 NSAIDs, tricyclic antidepressants, neuroleptics, dipyrone etc. allowed if dose stable ≥ 1 week Extra methadone (25% daily dose not more frequently than 2 hours) for breakthrough pain | |
| Outcomes | Daily PI (NRS 0 to 10 and 6‐faces scale)
Time to return to baseline PI Adverse events (symptoms) Additional analgesia Quality of life at baseline and end of study |
|
| Notes | NCT00525967; completed, no results | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "generated aleatory numbers" |
| Allocation concealment (selection bias) | Low risk | "envelopes … handled by a pharmacist in charge of giving medications to patients" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Method used to blind participants and personnel not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Method used to blind outcome assessment not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6/49 (12%) withdrew; do not appear to be included in analyses |
| Selective reporting (reporting bias) | Low risk | NCT record available, no results posted. All relevant specified outcomes reported |
| Size | High risk | < 50 participants per treatment arm |
Israel 2010.
| Methods | Randomised, double‐blind, placebo‐controlled, cross‐over study Treatment for 5 days with each intervention, no washout |
|
| Participants | Cancer patients (mainly colorectal, prostate, pancreas) on stable dose oral morphine ≥ 200 mg daily ≥ 1 week, baseline PI ≥ 2/10 Excluded: pain primarily neuropathic, receiving radiotherapy or other therapy likely to impact on pain scores, clinical jaundice, expected survival < 2 weeks, unable to comply with protocol N = 31 (22 completed) Completers: M 12, F 10 Mean age 56 (28 to 79) Baseline daily oral opioid 255 mg morphine equiv (range 200 mg to 900 mg, plus 1 participant taking 9000 mg) 26/31 had used regular oral paracetamol before study | |
| Interventions | In addition to all usual stable non‐paracetamol medication: Paracetamol 4 x 1000 mg daily Placebo | |
| Outcomes | Daily PI: NRS (0 to 10), used mean for last 4 days Use of rescue medication Adverse events Overall well‐being (0 to 10) At end of study, judgement about in which period pain was better |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer‐generated randomization schedule" |
| Allocation concealment (selection bias) | Low risk | remote allocation: "research pharmacist at a distant site" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "identical‐appearing placebo" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "identical‐appearing placebo" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis; 9/31 (29%) did not complete |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. All relevant specified outcomes reported |
| Size | High risk | < 50 participants per treatment arm |
F: female; N: number of participants in study; n: number of participants in treatment arm; NRS: numerical rating scale; M: male; NSAIDs: non‐steroidal anti‐inflammatory drugs; PI: pain intensity.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12610000893000 | Each treatment period only 3 days |
| Axelsson 2008 | Not randomised |
| Danninger 1993 | Each treatment period only 1 day |
| JPRN‐UMIN000009292 | Mucositis, not cancer pain |
| Nickles 2016 | Each treatment period only 3 days |
| Stockler 2004 | Each treatment period only 2 days |
Characteristics of studies awaiting assessment [ordered by study ID]
NCT00152854.
| Methods | Randomised, double‐blind, placebo‐controlled, cross‐over study Treatment for 7 days, then cross‐over |
| Participants | Ambulatory cancer patients, established opioid regimen of > 60 mg/day of morphine equivalents Exclude: severe pain; radiotherapy within 6 weeks; started chemo or hormone therapy within 4 weeks; change to NSAID or corticosteroid medication within 1 week or during study; contraindication to or use of paracetamol within 2 days N = 12 M and F eligible No baseline pain requirement reported, other than participants with no pain were excluded |
| Interventions | In addition to established opioid regimen: Paracetamol 4 x 1000 mg daily Placebo |
| Outcomes | PI: 0 to 10 NRS (daily, and weekly questionnaires) Preference for treatment period |
| Notes | Vardy J (Principal Investigator) Study started July 2005, completed December 2012 No results posted 30 March 2017 |
Pacilio 1989.
| Methods | Double‐blind study |
| Participants | Cancer pain |
| Interventions | Paracetamol Flupirtine |
| Outcomes | |
| Notes | Unable to obtain copy |
F: female; NRS: numerical rating scale; M: male; NSAIDs: non‐steroidal anti‐inflammatory drugs; PI: pain intensity
Characteristics of ongoing studies [ordered by study ID]
NCT02706769.
| Trial name or title | A double‐blind randomised parallel group trial of paracetamol versus placebo in conjunction with strong opioids for cancer related pain Randomised withdrawal design |
| Methods | Randomised, double‐blind, parallel group Duration 14 days |
| Participants | Cancer patients receiving daily regular strong opioids plus 4 x 1000 mg paracetamol. PI > 3/10 and < 9/10 in previous 24 hours, stable for 3 consecutive days Exclude: unstable pain, significant renal or liver disease, weight < 50 kg Estimated participants 140 M and F Age 16 years or more |
| Interventions | In addition to strong opioid Paracetamol 4 x 1000 mg daily Placebo |
| Outcomes | 30% increase in total Brief Pain Inventory between day 0 and day 14 in the active drug group versus the placebo group |
| Starting date | April 2016 |
| Contact information | University of Edinburgh |
| Notes | Estimated completion date April 2019 |
F: female; M: male; PI: pain intensity
Differences between protocol and review
We have included some additional outcomes in the 'Summary of findings' table in order to give some indication of any measured effect where none of our primary outcomes were reported: mean pain intensity at the end of treatment; quality of life or well‐being at end of treatment; patient preference for treatment in cross‐over studies.
Selective reporting bias added to risk of bias, and slightly amended components in the 'Risk of bias' table.
Contributions of authors
RAM, SD, and PW drafted the initial protocol, and other authors commented on that draft to produce the final version.
SD and RAM searched for studies, carried out data extraction, and assessed risk of bias. SD, RAM, and PW prepared a draft of the full review, and all authors contributed to the final version.
Sources of support
Internal sources
-
Oxford Pain Relief Trust, UK.
General institutional support
External sources
-
The National Institute for Health Research (NIHR), UK.
NIHR Cochrane Programme Grant: 13/89/29 ‐ Addressing the unmet need of chronic pain: providing the evidence for treatments of pain
Declarations of interest
PW: none known.
SD: none known.
RAM has received grant support from Grünenthal relating to individual patient‐level analyses of trial data regarding tapentadol in osteoarthritis and back pain (2015). He has received honoraria for attending boards with Menarini concerning methods of analgesic trial design (2014), with Novartis (2014) about the design of network meta‐analyses, and RB on understanding pharmacokinetics of drug uptake (2015). He has received honoraria from Omega Pharma (2016) and Futura Pharma (2016) for providing advice on trial and data analysis methods.
EDM: none known.
RFB: none known. RFB is a specialised pain physician and has managed patients with cancer pain.
DBC: none known. DBC is a specialised pain physician and has managed patients with cancer pain.
MM: none known.
BW: none known. BW is a specialist Palliative Medicine Consultant physician and manages patients with advanced life‐threatening illnesses, including cancer.
This review was identified in a 2019 audit as not meeting the current definition of the Cochrane Commercial Sponsorship policy. At the time of its publication it was compliant with the interpretation of the existing policy. As with all reviews, new and updated, at update this review will be revised according to 2020 policy update.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Axelsson 2003 {published data only}
- Axelsson B, Borup S. Is there an additive analgesic effect of paracetamol at step 3? A double‐blind randomized controlled study. Palliative Medicine 2003;17(8):724‐5. [DOI: 10.1177/026921630301700816] [DOI] [PubMed] [Google Scholar]
Cubero 2010 {published data only}
- Cubero DI, Giglio A. Early switching from morphine to methadone is not improved by acetaminophen in the analgesia of oncologic patients: a prospective, randomized, double‐blind, placebo‐controlled study. Supportive Care in Cancer 2010;18(2):235‐42. [DOI: 10.1007/s00520-009-0649-8] [DOI] [PubMed] [Google Scholar]
Israel 2010 {published data only}
- Israel FJ, Parker G, Charles M, Reymond L. Lack of benefit from paracetamol (acetaminophen) for palliative cancer patients requiring high‐dose strong opioids: a randomized, double‐blind, placebo‐controlled, crossover trial. Journal of Pain and Symptom Management 2010;39(3):548‐54. [DOI: 10.1016/j.jpainsymman.2009.07.008] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12610000893000 {published data only}
- Mitchell G (Principal Investigator). A single patient multiple cross‐over study to determine the efficacy of paracetamol in relieving pain suffered by patients with advanced cancer taking regular opioids. www.anzctr.org.au/ACTRN12610000893000.aspx (accessed 30 March 2017) 2010. [ANZCTR: ACTRN12610000893000] [DOI] [PubMed]
Axelsson 2008 {published data only}
- Axelsson B, Stellborn P, Ström G. Analgesic effect of paracetamol on cancer related pain in concurrent strong opioid therapy. A prospective clinical study. Acta Oncologica 2008;47(5):891‐5. [DOI: 10.1080/02841860701687259] [DOI] [PubMed] [Google Scholar]
Danninger 1993 {published data only}
- Danninger R, Jakse R, Beubler E. Randomized crossover‐comparison of 2 g‐ and 4 g‐doses of paracetamol per day in the case of mild to moderate pain caused by head and neck cancers. European Journal of Pain 1993;14(1):14‐8. [EMBASE: 132642 xx] [Google Scholar]
JPRN‐UMIN000009292 {published data only}
- Ken‐ichi Kaneko (Principle Investigator). Efficacy and safety of acetaminophen in the treatment of patients with head and neck cancer. upload.umin.ac.jp/cgi‐open‐bin/ctr_e/ctr_view.cgi?recptno=R000010522 (accessed 30 March 2017).
Nickles 2016 {published data only}
- Nickles J, Mitchell GK, Hardy J, Senior H, Carmont S‐A, Schluter PJ, et al. Single‐patient multiple crossover studies to determine the effectiveness of paracetamol in relieving pain suffered by patients with advanced cancer taking regular opioids: A pilot study. Palliative Medicine 2016;30(8):800‐2. [ANZCTR: ACTRN12609000870257; DOI: 10.1177/0269216316635012] [DOI] [PubMed] [Google Scholar]
Stockler 2004 {published data only}
- Stockler M, Vardy J, Pillai A, Warr D. Acetaminophen (paracetamol) improves pain and well‐being in people with advanced cancer already receiving a strong opioid regimen: a randomized, double‐blind, placebo‐controlled cross‐over trial. Journal of Clinical Oncology 2004;22(16):3389‐94. [DOI: 10.1200/JCO.2004.09.122] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
NCT00152854 {published data only}
- Vardy J (Principal Investigator). A randomised, placebo‐controlled, crossover trial of acetaminophen in cancer patients on strong opioids. clinicaltrials.gov/ct2/show/NCT00152854 (accessed 30 March 2017) 2016. [CTG: NCT00152854]
Pacilio 1989 {published data only}
- Pacilio G, Pizza C, Vetrano A, Mastrantoni M, Ceccarelli G. A double‐blind study on the effect of flupirtine as compared to paracetamol in the cancer pain. Riforma Medica 1989;104(1‐2):29‐32. [EMBASE: 1989176982] [Google Scholar]
References to ongoing studies
NCT02706769 {unpublished data only}
- University of Edinburgh. A double‐blind randomised parallel group trial of paracetamol versus placebo in conjunction with strong opioids for cancer related pain. clinicaltrials.gov/ct2/show/NCT02706769 (accessed 30 March 2017) 2016.
Additional references
AlBalawi 2013
- AlBalawi Z, McAlister FA, Thorlund K, Wong M, Wetterslev J. Random error in cardiovascular meta‐analyses: how common are false positive and false negative results?. Interational Journal of Cardiology 2013;168(2):1102‐7. [DOI: 10.1016/j.ijcard.2012.11.048] [DOI] [PubMed] [Google Scholar]
Altyar 2015
- Altyar A, Kordi L, Skrepnek G. Clinical and economic characteristics of emergency department visits due to acetaminophen toxicity in the USA. BMJ Open 2015;5(9):e007368. [DOI: 10.1136/bmjopen-2014-007368] [DOI] [PMC free article] [PubMed] [Google Scholar]
Axelrod 2003
- Axelrod J. Journey of a late blooming biochemical neuroscientist. Journal of Biology and Chemistry 2003;278(1):1‐13. [DOI] [PubMed] [Google Scholar]
Azevedo São Leão Ferreira 2006
- Azevedo São Leão Ferreira K, Kimura M, Jacobsen Teixeira M. The WHO analgesic ladder for cancer pain control, twenty years of use. How much pain relief does one get from using it?. Support Care Cancer 2006;14(11):1086‐93. [DOI: 10.1016/j.critrevonc.2013.01.001] [DOI] [PubMed] [Google Scholar]
Bao 2016
- Bao YJ, Hou W, Kong XY, Yang L, Xia J, Hua BJ, et al. Hydromorphone for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 10. [DOI: 10.1002/14651858.CD011108.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bateman 2014a
- Bateman DN, Carroll R, Pettie J, Yamamoto T, Elamin ME, Peart L, et al. Effect of the UK's revised paracetamol poisoning management guidelines on admissions, adverse reactions, and costs of treatment. British Journal of Clinical Pharmacology 2014;78(3):610‐8. [DOI: 10.1111/bcp.12362] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bateman 2014b
- Bateman DN. Pack size and paracetamol overdose: 16 years later. Clinical Toxicology 2014;52:821‐3. [DOI: 10.3109/15563650.2014.952432] [DOI] [PubMed] [Google Scholar]
Bell 2006
- Bell RF, Wisløff T, Eccleston C, Kalso E. Controlled clinical trials in cancer pain. How controlled should they be? A qualitative systematic review. British Journal of Cancer 2006;94(11):1559‐67. [DOI: 10.1038/sj.bjc.6603162] [DOI] [PMC free article] [PubMed] [Google Scholar]
Botting 2000
- Botting RM. Mechanism of action of acetaminophen: is there a cyclooxygenase 3?. Clinical Infectious Diseases 2000;31(5):S203‐10. [DOI: 10.1086/317520] [DOI] [PubMed] [Google Scholar]
Breivik 2009
- Breivik H, Cherny N, Collett B, Conno F, Filbet M, Foubert AJ, et al. Cancer‐related pain: a pan‐European survey of prevalence, treatment, and patient attitudes. Annals of Oncology 2009;20(8):1420‐33. [DOI: 10.1093/annonc/mdp001] [DOI] [PubMed] [Google Scholar]
Brok 2009
- Brok J, Thorlund K, Wetterslev J, Gluud C. Apparently conclusive meta‐analyses may be inconclusive ‐ trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta‐analyses. International Journal of Epidemiology 2009;38(1):287‐98. [DOI: 10.1093/ije/dyn188] [DOI] [PubMed] [Google Scholar]
Brune 2015
- Brune K, Renner B, Tiegs G. Acetaminophen/paracetamol: a history of errors, failures and false decisions. European Journal of Pain 2015;19(7):953‐65. [10.1002/ejp.621] [DOI] [PubMed] [Google Scholar]
Cancer Research UK 2016
- Cancer statistics for the UK. www.cancerresearchuk.org/health‐professional/cancer‐statistics (accessed 21 November 2016).
Carlson 2016
- Carlson CL. Effectiveness of the World Health Organization cancer pain relief guidelines: an integrative review. Journal of Pain Research 2016;9:515‐34. [10.2147/JPR.S97759. eCollection 2016] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chandrasekharan 2002
- Chandrasekharan NV, Dai H, Roos KL, Evanson NK, Tomsik J, Elton TS, et al. COX‐3, a cyclooxygenase‐1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure and expression. Proceedings of the National Academy of Sciences of the United States of America 2002;99(21):13926‐31. [DOI: 10.1073/pnas.162468699] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2017
- Cooper TE, Heathcote LC, Anderson B, Grégoire MC, Ljungman G, Eccleston C. Non‐steroidal anti‐inflammatory drugs (NSAIDs) for cancer‐related pain in children and adolescents. Cochrane Database of Systematic Reviews 2017, Issue 2. [DOI: 10.1002/14651858.CD012563] [DOI] [PMC free article] [PubMed] [Google Scholar]
CSM 1997
- Committee on Safety of Medicines. Medicines Control Agency. Paracetamol and aspirin. Current Problems in Pharmacovigilance 1997;23:9. [Google Scholar]
Curros‐Criado 2009
- Curros‐Criado MM, Herrero JF. Antinociceptive effects of NCX‐701 (nitro‐paracetamol) in neuropathic rats: enhancement of antinociception by co‐administration with gabapentin. British Journal of Pharmacology 2009;158(2):601‐9. [DOI: 10.1111/j.1476-5381.2009.00343.x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dani 2007
- Dani M, Guindon J, Lambert C, Beaulieu P. The local antinociceptive effects of paracetamol in neuropathic pain are mediated by cannabinoid receptors. European Journal of Pharmacology 2007;573(1‐3):214‐5. [DOI: 10.1016/j.ejphar.2007.07.012] [DOI] [PubMed] [Google Scholar]
Dart 2000
- Dart RC, Kuffner EK, Rumack BH. Treatment of pain or fever with paracetamol (acetaminophen) in the alcoholic patient: a systematic review. American Journal of Medicine 2000;7(2):123‐34. [PUBMED: 11319580] [DOI] [PubMed] [Google Scholar]
Deandrea 2008
- Deandrea S, Montanari M, Moja L, Apolone G. Prevalence of undertreatment in cancer pain. A review of published literature. Annals of Oncology 2008;19(12):1985‐91. [DOI: 10.1093/annonc/mdn419] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dechartes 2013
- Dechartres A, Trinquart L, Boutron I, Ravaud P. Influence of trial sample size on treatment effect estimates: meta‐epidemiological study. BMJ 2013;346:f2304. [DOI: 10.1136/bmj.f2304] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dechartres 2014
- Dechartres A, Altman DG, Trinquart L, Boutron I, Ravaud P. Association between analytic strategy and estimates of treatment outcomes in meta‐analyses. JAMA 2014;312:623‐30. [DOI: 10.1001/jama.2014.8166] [DOI] [PubMed] [Google Scholar]
Deng 2012
- Deng D, Fu L, Zhao YX, Wu X, Zhang G, Liang C, et al. The relationship between cancer pain and quality of life in patients newly admitted to Wuhan Hospice Center of China. American Journal of Hospital Palliative Care 2012;29(1):53‐9. [DOI: 10.1177/1049909111418636] [DOI] [PubMed] [Google Scholar]
Derry 2013
- Derry S, Moore RA. Paracetamol (acetaminophen) with or without an antiemetic for acute migraine headaches in adults. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD008040.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Derry 2014
- Derry CJ, Derry S, Moore RA. Caffeine as an analgesic adjuvant for acute pain in adults. Cochrane Database of Systematic Reviews 2014, Issue 12. [DOI: 10.1002/14651858.CD009281.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Derry 2017
- Derry S, Wiffen PJ, Moore RA, McNicol ED, Bell RF, Carr DB, et al. Oral nonsteroidal anti‐inflammatory drugs (NSAIDs) for cancer pain in adults. Cochrane Database of Systematic Reviews 2017, Issue 4. [DOI: 10.1002/14651858.CD012638] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dreidi 2016
- Dreidi MM, Hamdan‐Mansour AM. Pain, sleep disturbance, and quality of life among Palestinian patients diagnosed with cancer. Journal of Cancer Education 2016;31(4):796‐803. [DOI: 10.1007/s13187-015-0946-5] [DOI] [PubMed] [Google Scholar]
Drugs.com 2016
- Anonymous. Paracetamol. www.drugs.com/international/paracetamol.html (accessed 10 May 2016).
Dworkin 2008
- Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. Journal of Pain 2008;9(2):105‐21. [DOI: 10.1016/j.jpain.2007.09.005] [DOI] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [DOI] [PubMed] [Google Scholar]
EPOC 2015
- Effective Practice, Organisation of Care (EPOC). 23. Worksheets for preparing a Summary of Findings using GRADE. Resources for review authors. epoc.cochrane.org/epoc‐specific‐resources‐review‐authors (accessed 30 November 2016).
Fanelli 2017
- Fanelli D, Costas R, Ioannidis JP. Meta‐assessment of bias in science. Proceedings of the National Academy of Sciences of the United States of America 2017; Vol. 114, issue 14:3714‐9. [DOI: 10.1073/pnas.1618569114] [DOI] [PMC free article] [PubMed]
FDA 2015
- Hertz S. Review of Acetaminophen for the Withdrawn or Removed List. www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/drugs/pharmacycompoundingadvisorycommittee/ucm449535.pdf May 13 2015 (Accessed May 30 2017):44 et seq.
Flower 1972
- Flower RJ, Vane JR. Inhibition of prostaglandin synthetase in brain explains the anti‐pyretic activity of paracetamol (4‐acetamidophenol). Nature 1972;240(5381):410‐1. [PUBMED: 4564318] [DOI] [PubMed] [Google Scholar]
Gavaghan 2000
- Gavaghan DJ, Moore RA, McQuay HJ. An evaluation of homogeneity tests in meta‐analyses in pain using simulations of individual patient data. Pain 2000;85(3):415‐24. [DOI] [PubMed] [Google Scholar]
Graham 2005
- Graham GG, Scott KF. Mechanism of action of paracetamol. American Journal of Therapeutics 2005;12(1):46‐55. [DOI: 10.1097/00045391-200501000-00008] [DOI] [PubMed] [Google Scholar]
Gulcu 2007
- Gulcu N, Karaaslan K, Ozturan KE, Kocoglu H. Intravenous paracetamol for pain relief in a patient with neuropathic pain. Acta Anaesthesiologica Scandinavica 2007;51(7):956‐7. [DOI: 10.1111/j.1399-6576.2007.01362.x] [DOI] [PubMed] [Google Scholar]
Gulmez 2013
- Gulmez SE, Larrey D, Pageaux GP, Lignot S, Lassalle R, Jové J, et al. Transplantation for acute liver failure in patients exposed to NSAIDs or paracetamol (acetaminophen): the multinational case‐population SALT study. Drug Safety 2013;36(2):135‐44. [DOI: 10.1007/s40264-012-0013-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gulmez 2015
- Gulmez SE, Larrey D, Pageaux GP, Bernuau J, Bissoli F, Horsmans Y, et al. Liver transplant associated with paracetamol overdose: results from the seven‐country SALT study. British Journal of Clinical Pharmacology 2015;80(3):599‐606. [DOI: 10.1111/bcp.12635] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gunnell 1997
- Gunnell D, Hawton K, Garnier V, Bismuth C, Fagg J. Use of paracetamol for suicide and non‐fatal poisoning in the UK and France: are restrictions on availability justified?. Journal of Epidemiology and Community Health 1997;51(2):175‐9. [PUBMED: 9196648] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence ‐ inconsistency. Journal of Cinical Epidemiology 2011;64(12):1294‐302. [DOI: 10.1016/j.jclinepi.2011.03.017] [DOI] [PubMed] [Google Scholar]
Guyatt 2013a
- Guyatt G, Oxman AD, Sultan S, Brozek J, Glasziou P, Alonso‐Coello P, et al. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. Journal of Clinical Epidemiology 2013;66:151‐7. [DOI: 10.1016/j.jclinepi.2012.01.006] [DOI] [PubMed] [Google Scholar]
Guyatt 2013b
- Guyatt GH, Oxman AD, Santesso N, Helfand M, Vist G, Kunz R, et al. GRADE guidelines: 12. Preparing summary of findings tables ‐ binary outcomes. Journal of Clinical Epidemiology 2013;66:158‐72. [DOI: 10.1016/j.jclinepi.2012.01.012] [DOI] [PubMed] [Google Scholar]
Hadley 2013
- Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD010270.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawkins 2007
- Hawkins LC, Edwards JN, Dargan PI. Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: a review of the literature. Drug Safety 2007;30(6):465‐79. [PUBMED: 17536874] [DOI] [PubMed] [Google Scholar]
Hawton 2001
- Hawton K, Townsend E, Deeks J, Appleby L, Gunnell D, Bennewith O, et al. Effects of legislation restricting pack sizes of paracetamol and salicylate on self poisoning in the United Kingdom: before and after study. BMJ 2001;322(7296):1203‐7. [DOI: 10.1136/bmj.322.7296.1203] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawton 2013
- Hawton K, Bergen H, Simkin S, Dodd S, Pocock P, Bernal W, et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: interrupted time series analyses. BMJ 2013;346:f403. [DOI: 10.1136/bmj.f403] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hinz 2008
- Hinz B, Cheremina O, Brune K. Acetaminophen (paracetamol) is a selective cyclooxygenase‐2 inhibitor in man. Federation of American Societies for Experimental Biology Journal 2008;22(2):383‐90. [DOI: 10.1096/fj.07-8506com] [DOI] [PubMed] [Google Scholar]
IARC 2012
- International Agency for Research on Cancer. GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. globocan.iarc.fr/Pages/fact_sheets_cancer.aspx (accessed 21 November 2016).
IntHout 2015
- IntHout J, Ioannidis JP, Borm GF, Goeman JJ. Small studies are more heterogeneous than large ones: a meta‐meta‐analysis. Journal of Clinical Epidemiology 2015;68:860‐9. [DOI: 10.1016/j.jclinepi.2015.03.017] [DOI] [PubMed] [Google Scholar]
Jadad 1995
- Jadad AR, Browman GP. The WHO analgesic ladder for cancer pain management. Stepping up the quality of Its evaluation. JAMA 1995;274(23):1870‐3. [PubMed] [Google Scholar]
Liew 2014
- Liew Z, Ritz B, Rebordosa C, Lee PC, Olsen J. Acetaminophen use during pregnancy, behavioral problems, and hyperkinetic disorders. JAMA Pediatrics 2014;168(4):313‐20. [DOI: 10.1001/jamapediatrics.2013.4914] [DOI] [PubMed] [Google Scholar]
Machado 2015
- Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta‐analysis of randomised placebo controlled trials. BMJ 2015;350:h1225. [DOI: 10.1136/bmj.h1225] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mazaud‐Guittot 2013
- Mazaud‐Guittot S, Nicolas Nicolaz C, Desdoits‐Lethimonier C, Coiffec I, Ben Maamar M, Balaguer P, et al. Paracetamol, aspirin, and indomethacin induce endocrine disturbances in the human fetal testis capable of interfering with testicular descent. Journal of Clinical Endocrinology and Metabolism 2013;98(11):1757‐67. [DOI: 10.1210/jc.2013-2531] [DOI] [PubMed] [Google Scholar]
McQuay 1998
- McQuay H, Moore A. An Evidence‐based Resource for Pain Relief. Oxford: Oxford University Press, 1998. [ISBN: 0‐19‐263048‐2] [Google Scholar]
McQuay 2005
- McQuay HJ, Moore RA. Placebo. Postgraduate Medical Journal 2005;81(953):155‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
McQuay 2007
- McQuay HJ, Moore RA. Dose‐response in direct comparisons of different doses of aspirin, ibuprofen and paracetamol (acetaminophen) in analgesic studies. British Journal of Clinical Pharmacology 2007;63(3):271‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mercadante 2013
- Mercadante S, Giarratano A. The long and winding road of nonsteroidal anti‐inflammatory drugs and paracetamol in cancer pain management: a critical review. Critical Reviews in Oncology/Hematology 2013;87:140‐5. [DOI: 10.1016/j.critrevonc.2013.01.001] [DOI] [PubMed] [Google Scholar]
Mercadante 2014
- Mercadante S, Giarratano A. Pharmacological management of cancer pain in children. Clinical Reviews in Oncology and Hematology 2014;91(1):93‐7. [DOI: 10.1016/j.critrevonc.2014.01.005] [DOI] [PubMed] [Google Scholar]
Mikan 2016
- Mikan F, Wada M, Yamada M, Takahashi A, Onishi H, Ishida M, et al. The association between pain and quality of life for patients with cancer in an outpatient clinic, an inpatient oncology ward, and inpatient palliative care units. American Journal of Hospital Palliative Care 2016;33(8):782‐90. [DOI: 10.1177/1049909116630266] [DOI] [PubMed] [Google Scholar]
Moore 1998
- Moore RA, Gavaghan D, Tramèr MR, Collins SL, McQuay HJ. Size is everything ‐ large amounts of information are needed to overcome random effects in estimating direction and magnitude of treatment effects. Pain 1998;78(3):209‐16. [DOI: 10.1016/S0304-3959(98)00140-7] [DOI] [PubMed] [Google Scholar]
Moore 2008
- Moore RA, Barden J, Derry S, McQuay HJ. Managing potential publication bias. In: McQuay HJ, Kalso E, Moore RA editor(s). Systematic Reviews in Pain Research: Methodology Refined. Seattle: IASP Press, 2008:15‐24. [ISBN: 978–0–931092–69–5] [Google Scholar]
Moore 2010a
- Moore RA, Moore OA, Derry S, Peloso PM, Gammaitoni AR, Wang H. Responder analysis for pain relief and numbers needed to treat in a meta‐analysis of etoricoxib osteoarthritis trials: bridging a gap between clinical trials and clinical practice. Annals of the Rheumatic Diseases 2010;69(2):374‐9. [DOI: 10.1136/ard.2009.107805] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 2010b
- Moore RA, Derry S, McQuay HJ, Straube S, Aldington D, Wiffen P, et al. Clinical effectiveness: an approach to clinical trial design more relevant to clinical practice, acknowledging the importance of individual differences. Pain 2010;149(2):173‐6. [DOI: 10.1016/j.pain.2009.08.007] [DOI] [PubMed] [Google Scholar]
Moore 2013a
- Moore RA, Straube S, Aldington D. Pain measures and cut‐offs ‐ 'no worse than mild pain' as a simple, universal outcome. Anaesthesia 2013;68(4):400‐12. [DOI: 10.1111/anae.12148] [DOI] [PubMed] [Google Scholar]
Moore 2013b
- Moore RA. What works for whom? Determining the efficacy and harm of treatments for pain. Pain 2013;154 Suppl 1:S77‐86. [DOI: 10.1016/j.pain.2013.03.024] [DOI] [PubMed] [Google Scholar]
Moore 2014
- Moore RA, Derry S, Taylor RS, Straube S, Phillips CJ. The costs and consequences of adequately managed chronic non‐cancer pain and chronic neuropathic pain. Pain Practice 2014;14(1):79‐94. [DOI: 10.1111/papr.12050] [DOI] [PubMed] [Google Scholar]
Moore 2014a
- Moore RA, Derry S, Wiffen PJ, Straube S, Aldington DJ. Overview review: comparative efficacy of oral ibuprofen and paracetamol (acetaminophen) across acute and chronic pain conditions. European Journal of Pain 2014;19(9):1213‐23. [DOI: 10.1002/ejp.649] [DOI] [PubMed] [Google Scholar]
Moore 2016
- Moore RA, Moore N. Paracetamol and pain: the kiloton problem. European Journal of Hospital Pharmacy 2016;23(4):187‐8. [DOI: 10.1136/ejhpharm-2016-000952] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nabal 2012
- Nabal M, Librada S, Redondo MJ, Pigni A, Brunelli C, Caraceni A. The role of paracetamol and nonsteroidal anti‐inflammatory drugs in addition to WHO Step III opioids in the control of pain in advanced cancer. A systematic review of the literature. Palliative Medicine 2012;26(4):305‐12. [DOI: 10.1177/0269216311428528] [DOI] [PubMed] [Google Scholar]
Nguyen 2017
- Nguyen TL, Collins GS, Lamy A, Devereaux PJ, Daurès JP, Landais P, et al. Simple randomization did not protect against bias in smaller trials. Journal of Clinical Epidemiology 2017;84:105‐13. [DOI: 10.1016/j.jclinepi.2017.02.010] [DOI] [PubMed] [Google Scholar]
NICE 2016
- National Institute for Health and Care Excellence. Palliative cancer care ‐ pain. cks.nice.org.uk/palliative‐cancer‐care‐pain (accessed 02 February 2017).
Norris 2008
- Norris W, Paredes AH, Lewis JH. Drug‐induced liver injury in 2007. Current Opinion in Gastroenterology 2008;24(3):287‐97. [DOI: 10.1097/MOG.0b013e3282f9764b] [DOI] [PubMed] [Google Scholar]
Nüesch 2010
- Nüesch E, Trelle S, Reichenbach S, Rutjes AW, Tschannen B, Altman DG, et al. Small study effects in meta‐analyses of osteoarthritis trials: meta‐epidemiological study. BMJ 2010;341:c3515. [DOI: 10.1136/bmj.c3515] [DOI] [PMC free article] [PubMed] [Google Scholar]
PaPaS 2012
- Cochrane Pain, Palliative and Supportive Care Group. PaPaS author and referee guidance. papas.cochrane.org/papas‐documents (accessed 21 November 2016).
PIC 2015
- PharmWeb. Paracetamol Information Centre. www2.pharmweb.net/pwmirror/pwy/paracetamol/pharmwebpic.html (accessed 18 January 2016).
Portenoy 1999
- Portenoy RK, Lesage P. Management of cancer pain. Lancet 1999;353(9165):1695‐700. [DOI: 10.1016/S0140-6736(99)01310-0] [DOI] [PubMed] [Google Scholar]
Prescott 2000
- Prescott LF. Therapeutic misadventure with paracetamol: fact or fiction?. American Journal of Therapeutics 2000;7(2):99‐114. [PUBMED: 11319578] [DOI] [PubMed] [Google Scholar]
Prommer 2015
- Prommer EE. Pharmacological management of cancer‐related pain. Cancer Control 2015;22(4):412‐25. [PUBMED: 26678968] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roberts 2015
- Roberts I, Ker K, Edwards P, Beecher D, Manno D, Sydenham E. The knowledge system underpinning healthcare is not fit for purpose and must change. BMJ 2015;350:h2463. [DOI: 10.1136/bmj.h2463] [DOI] [PubMed] [Google Scholar]
Roberts 2016
- Roberts E, Delgado Nunes V, Buckner S, Latchem S, Constanti M, Miller P, et al. Paracetamol: not as safe as we thought? A systematic literature review of observational studies. Annals of the Rheumatic Diseases 2016;75(3):552‐9. [DOI: 10.1136/annrheumdis-2014-206914] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saragiotto 2016
- Saragiotto BT, Machado GC, Ferreira ML, Pinheiro MB, Abdel Shaheed C, Maher CG. Paracetamol for low back pain. Cochrane Database of Systematic Reviews 2016, Issue 6. [DOI: 10.1002/14651858.CD012230] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmidt‐Hansen 2015a
- Schmidt‐Hansen M, Bromham N, Taubert M, Arnold S, Hilgart JS. Buprenorphine for treating cancer pain. Cochrane Database of Systematic Reviews 2015, Issue 3. [DOI: 10.1002/14651858.CD009596.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmidt‐Hansen 2015b
- Schmidt‐Hansen M, Bennett MI, Arnold S, Bromham N, Hilgart JS. Oxycodone for cancer‐related pain. Cochrane Database of Systematic Reviews 2015, Issue 2. [DOI: 10.1002/14651858.CD003870.pub5] [DOI] [PubMed] [Google Scholar]
Schwab 2003
- Schwab JM, Schluesener HJ, Laufer S. COX‐3: just another COX or the solitary elusive target of paracetamol?. Lancet 2003;361(9362):981‐2. [DOI: 10.1016/S0140-6736(03)12841-3] [DOI] [PubMed] [Google Scholar]
Straube 2014
- Straube C, Derry S, Jackson KC, Wiffen PJ, Bell RF, Strassels S, et al. Codeine, alone and with paracetamol (acetaminophen), for cancer pain. Cochrane Database of Systematic Reviews 2014, Issue 9. [DOI: 10.1002/14651858.CD006601.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thorlund 2011
- Thorlund K, Imberger G, Walsh M, Chu R, Gluud C, Wetterslev J, et al. The number of patients and events required to limit the risk of overestimation of intervention effects in meta‐analysis ‐ a simulation study. PLOS One 2011;6(10):e25491. [DOI: 10.1371/journal.pone.0025491] [DOI] [PMC free article] [PubMed] [Google Scholar]
Toms 2008
- Toms L, McQuay HJ, Derry S, Moore RA. Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD004602.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 2013
- Turner RM, Bird SM, Higgins JP. The impact of study size on meta‐analyses: examination of underpowered studies in Cochrane reviews. PLOS One 2013;8(3):e59202. [DOI: 10.1371/journal.pone.0059202] [DOI] [PMC free article] [PubMed] [Google Scholar]
Twycross 2014
- Twycross R, Wilcock A, Howard P. Palliative Care Formulary. Nottingham: Palliativedrugs.com Ltd, 2014. [Google Scholar]
Twycross 2015
- Twycross A, Parker R, Williams A, Gibson F. Cancer‐related pain and pain management: sources, prevalence, and the experiences of children and parents. Journal of Paediatric Oncology Nursing 2015;32(6):369‐84. [DOI: 10.1177/1043454214563751] [DOI] [PubMed] [Google Scholar]
Van den Beuken‐van Everdingen 2016
- Beuken‐van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan‐Heijnen VC, Janssen DJ. Update on prevalence of pain in patients with cancer: systematic review and meta‐analysis. Journal of Pain and Symptom Management 2016;51:1070‐90. [DOI: 10.1016/j.jpainsymman.2015.12.340] [DOI] [PubMed] [Google Scholar]
Ventafridda 1990
- Ventafridda V, Conno F, Panerai AE, Maresca V, Monza GC, Ripamonti C. Non‐steroidal anti‐inflammatory drugs as the first step in cancer pain therapy: double‐blind, within‐patient study comparing nine drugs. Journal of International Medical Research 1990;18(1):21‐9. [DOI: 10.1177/030006059001800104] [DOI] [PubMed] [Google Scholar]
WHO 2017
- Anonymous. WHO analgesic ladder. www.who.int/cancer/palliative/painladder/en/ (accessed 10 April 2017).
Wiffen 2014
- Wiffen PJ, Derry S, Moore RA. Impact of morphine, fentanyl, oxycodone or codeine on patient consciousness, appetite and thirst when used to treat cancer pain. Cochrane Database of Systematic Reviews 2014, Issue 5. [DOI: 10.1002/14651858.CD011056.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiffen 2015
- Wiffen PJ, Derry S, Naessens K, Bell RF. Oral tapentadol for cancer pain. Cochrane Database of Systematic Reviews 2015, Issue 9. [DOI: 10.1002/14651858.CD011460.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiffen 2016
- Wiffen PJ, Wee B, Moore RA. Oral morphine for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 4. [DOI: 10.1002/14651858.CD003868.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiffen 2017
- Wiffen PJ, Derry S, Moore RA. Tramadol with or without paracetamol (acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 1. [DOI: 10.1002/14651858.CD012508] [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2014
- Williams CM, Maher CG, Latimer J, McLachlan AJ, Hancock MJ, Day RO, et al. Efficacy of paracetamol for acute low‐back pain: a double‐blind, randomised controlled trial. Lancet 2014;384(9954):1586‐96. [DOI: 10.1016/S0140-6736(14)60805-9] [DOI] [PubMed] [Google Scholar]
Zhao 2011
- Zhao L, Pickering G. Paracetamol metabolism and related genetic differences. Drug Metabolism Reviews 2011;43(1):41‐52. [DOI: 10.3109/03602532.2010.527984] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
McNicol 2015
- McNicol ED, Strassels S, Goudas L, Lau J, Carr DB. NSAIDS or paracetamol, alone or combined with opioids, for cancer pain. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD005180.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
wife 2017b
- Wiffen PJ, Derry S, Moore RA, McNicol ED, Bell RF, Carr DB, et al. Oral paracetamol (acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 4. [DOI: 10.1002/14651858.CD012637] [DOI] [PMC free article] [PubMed] [Google Scholar]


