Short abstract
Background
Wearable sensors and other smart technology may be especially beneficial in providing remote monitoring of sub-clinical changes in pregnancy health status. Yet, limited research has examined perceptions among pregnant patients and providers in incorporating smart technology into their daily routine and clinical practice.
Objective
The purpose of this study was to examine the perceptions of pregnant women and their providers at a rural health clinic on the use of wearable technology to monitor health and environmental exposures during pregnancy.
Methods
An anonymous 21-item e-survey was administered to family medicine or obstetrics and gynecology (n=28) providers at a rural health clinic; while a 21-item paper survey was administered to pregnant women (n=103) attending the clinic for prenatal care.
Results
Smartphone and digital technology use was high among patients and providers. Patients would consider wearing a mobile sensor during pregnancy, reported no privacy concerns, and felt comfortable sharing information from these devices with their physician. About seven out of 10 women expressed willingness to change their behavior during pregnancy in response to receiving personalized recommendations from a smartphone. While most providers did not currently use smart technologies in their medical practice, about half felt it will be used more often in the future to diagnose and remotely monitor patients. Patients ranked fetal heart rate and blood pressure as their top preference for health monitoring compared to physicians who ranked blood pressure and blood glucose. Patients and providers demonstrated similar preferences for environmental monitoring, but patients as a whole expressed more interests in tracking environmental measures compared to their providers.
Conclusions
Patients and providers responded positively to the use of wearable sensor technology in prenatal care. More research is needed to understand what factors might motivate provider use and implementation of wearable technology to improve the delivery of prenatal care.
Keywords: Mobile health, wearable sensors, pregnancy health monitoring, environmental sensing, patient acceptability, physician perception
Introduction
Wearable sensors, smart textiles, and other mobile health (mHealth) innovations present exciting new opportunities to enhance the diagnosis, clinical monitoring, and management of pregnancy health outside of traditional care settings. Rapid technical advancements in wearable devices now extend the capabilities of clinical health care monitoring and have significant potential to improve early detection of pregnancy complications. Pregnancy is a life stage that involves rapid physiologic and behavioral changes, and some higher risk women may benefit from more vigilant outpatient monitoring. In the area of women’s health, smart technology has already been used to motivate weight loss, improve patient compliance in chronic disease care including diabetes, heart disease, breast cancer, and osteoporosis, and to support mental health.1,2
Presently, there are a number of consumer-based wearable technologies that measure physical activity and other changes in lifestyle behaviors, as well as continuously monitor physiologic parameters (e.g. blood pressure), but none that target pregnant women. While there is a need for continuous and longitudinal monitoring to capture changes in lifestyle behaviors and the emergence of early risk factors associated with pregnancy complications, very few studies have examined the implementation of wearable sensors to augment routine or higher risk prenatal care. Even fewer studies have investigated the patient’s and provider’s perceptions on the efficacy of employing these technology solutions to continuously monitor pregnancy health and environmental conditions and the subsequent impact on clinical decision-making.3
Wearable sensor and other smart technologies may play an important part in the early detection of adverse pregnancy-related health events along with motivating improvement in patient and provider interactions for effective pregnancy health management. Wearable sensor technologies generate large-scale, multi-dimensional datasets that can be exploited to identify lifestyle, environmental, and behavioral risk factors in the subclinical phase of an adverse pregnancy outcome.3 A recent study employed mobile sensors to track blood pressure changes in high-risk pregnant women with hypertensive disorders and demonstrated a relatively high prediction accuracy.4
Wearable technologies and other smart digital devices are also being used to motivate patient adherence to prescribed medications; whereby smart pillboxes now have the capability to wirelessly sync up with a patient’s smartphone to provide daily reminders, track medication usage, and geo-locate a misplaced pillbox.5 Apple’s ResearchKit is radically advancing the way medical research is performed by making significant improvements in the way researchers enroll, obtain consent, collect data, and communicate with participants. For example ResearchKit is already being used to understand why some women develop postpartum depression (PPD) and others do not by engaging women around the world in a genetic research study.6 Researchers can now track the emotional state of a woman post-pregnancy using a combination of wearable sensors, cloud computing, Artificial Intelligence algorithms, and smartphones to facilitate early detection of PPD.7 While a significant challenge involving the integration of high volumes of heterogeneous clinical and health data to inform intelligent decision support systems and detect clinical abnormalities remains, computer scientists are teaming up with physicians to enhance pattern recognition of pregnancy-induced hypertensive disorders through the use of electronic health records and advances in semantic interoperability.8
Smart technology may be especially beneficial in providing remote monitoring of sub-clinical changes in health status during pregnancy (e.g. the progression of gestational hypertension) that occur outside of scheduled prenatal care visits. Yet, limited research has examined the interests, preferences, and perceptions of pregnant patient users and health care professionals in incorporating these types of wearable health and environmental monitoring and smart digital devices into their daily routine and clinical practice. The present study seeks to understand how pregnant women and their health care providers in the rural South are already using smart digital devices (e.g. smartphone applications (apps), wearable devices) and their perceptions on incorporating these smart tools to monitor pregnancy health. The goal of this study was to assess the interests, level of comfort, and potential concerns among health care providers and their patients in using wearable technology to monitor pregnancy health in a rural, medically underserved clinic in Southern Appalachia. We also evaluated the perceived benefits and barriers of wearable health technologies and the types of health and environmental monitoring data that patients and providers would like to see captured during pregnancy. This research will address an important gap in perceptions and reception of incorporating wearable and smart digital device technology into prenatal care among a pregnant population and their physicians.
Methods
Study setting
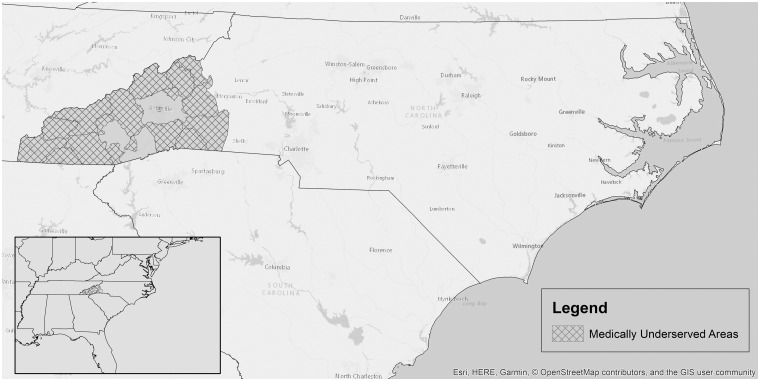
Recruitment of pregnant patients and their medical providers took place at the Mountain Area Health Education Center (MAHEC), a rural health clinic that serves the entire 16 county region of Western North Carolina (WNC) (Figure 1). The WNC region is deemed a primary care health professional shortage area (HPSA) and has historically high rates of preterm birth and low birth weight infants when compared to state and national averages. The lack of access to and availability of health services in rural WNC positions wearable sensors and remote patient monitoring as an especially appealing new model to expand access to prenatal care, achieve remote patient monitoring, and augment health care decision-making to improve maternal and infant health outcomes in the region.
Figure 1.
Map of Mountain area health education center (MAHEC) 16 county service area (grey) and corresponding medically underserved locations (hatched).
Survey design
A 21-item survey was developed to examine the perceptions and experience of using wearable technology to monitor pregnancy health and included three sections: (a) background and demographic information (e.g. age, race/ethnicity, education); (b) current digital device ownership and examples of use (e.g. weekly usage of digital devices, weekly activities performed on digital device); and (c) new uses of digital devices and receptivity to using this technology to monitor pregnancy health (e.g. use of Global Positioning System (GPS) tracker during pregnancy, privacy concerns about data stored on smartphone, type of health monitoring). The survey was developed and distributed using either Qualtrics online software7 or in paper format, and was piloted with 30 individuals.
Two separate surveys were uniquely adapted to be completed by medical providers or their pregnant patients. Providers were asked about perceived benefits, clinical uses, and barriers or limitations of wearable sensors or smart digital technologies for their patient population, as well as in what scenarios would they consider the adoption of wearables into clinical practice to monitor their patient’s pregnancy health. Patients were asked about their concerns and level of comfort in using wearable monitoring devices while pregnant, including carrying a GPS tracker, data privacy concerns, likely scenarios of use, and the potential for behavioral change. Both patients and providers were asked about what types of health and environmental monitoring data they would like to see captured during pregnancy. The study protocol was approved by the institutional review boards at North Carolina State University in Raleigh, North Carolina, USA (IRB#9266) and Mission Health System in Asheville, North Carolina, USA (IRB#16-08-1602). The Institutional Review Board (IRB) from both institutions waived the requirement to obtain a signed consent form for all participants because the only record linking the subject and research would be the consent document and the principal risk would be potential harm resulting from a breach of confidentiality. Therefore, our study used a participant information letter in lieu of a formal consent form.
Survey dissemination to patients and providers
Patients were invited to participate in the survey from January–April 2017. A rolling “first-come-first-served” enrollment strategy was implemented to recruit pregnant patients attending a MAHEC clinic for prenatal care until target sample sizes were met. Upon check-in at her appointment, each woman may have picked up a brochure detailing the proposed research objectives at the front desk and then voluntarily decided to participate in an anonymous paper or electronic survey by navigating to a secure link using Qualtrics (Qualtrics, Provo, Utah, USA).9 Paper surveys were enclosed in a sealable envelope and handed to the clinic staff following completion. Inclusion criteria for patient enrollment included women who were: 18–45 years of age; pregnant or who had recently given birth (<1 year postpartum); spoke English as their primary language; and were willing to complete the paper or e-survey.
The electronic survey was administered to all obstetrics and gynecology (OB/GYN) and family medicine providers (ntotal∼44 providers) at MAHEC via email from December 2016–January 2017. Medical providers specializing in women’s health at the rural health clinic received an email detailing the proposed research objectives and were invited to voluntarily participate by navigating to a secure and confidential link using the Qualtrics Research Suite to complete the survey anonymously (Qualtrics, Provo, Utah, USA). Inclusion criteria for enrollment included medical providers who were: employed by MAHEC; specialized in women’s health; and were willing to complete the e-survey.
Paper survey responses were manually inputted and numerically coded in Excel and all survey responses were descriptively analyzed using SAS® software Version 9.4 (SAS Institute Inc., Cary, North Carolina, USA).10
Results
A total of 103 pregnant women completed the patient survey and 28 health care providers (n=13 OB/GYN and n=15 family medicine) completed the provider survey. Tables 1 and 2 show the demographic characteristics of pregnant patients and providers who responded to the survey. The mean age of patients was 27 years (standard deviation (SD) 6.4) and 86% were white (n=89). About half of the patient sample (n=51) had a high school degree and 31% (n=32) had a college or professional degree. Roughly one in four patients were either single or in an unmarried relationship. Most patients spoke English as their primary language (n=99, 96%) and only 6% of the sample (n=6) identified as Hispanic/Latina origin.
Table 1.
Demographic characteristics of 103 pregnant patients at the Mountain Area Health Education Center (MAHEC) who responded to the survey.
| Maternal characteristics | Patient responses n (%) |
|---|---|
| Mean age in years (SD) | 27.4 (6.4) |
| Race | |
| White | 89 (86.4%) |
| Black | 5 (4.9%) |
| Asian | 1 (1.0%) |
| Mixed race | 7 (6.8%) |
| Other | 1 (1.0%) |
| Ethnicity | |
| Hispanic/Latino | 6 (5.8%) |
| Not Hispanic/Latino | 97 (94.2%) |
| Primary language | |
| English | 99 (96.1%) |
| Spanish | 1 (1.0%) |
| Other | 2 (1.9%) |
| Declined to answer | 1 |
| Education | |
| Some high school | 7 (6.8%) |
| High school/General Education Diploma (GED) | 51 (49.5%) |
| Associate’s degree | 13 (12.6%) |
| College graduate/professional degree | 32 (31.1%) |
| Current relationship status | |
| Married | 58 (56.9%) |
| Separated | 1 (1.0%) |
| Single | 10 (9.8%) |
| Unmarried relationship | 32 (31.4%) |
| Divorced | 1 (1.0%) |
| Widowed | 0 |
| Declined to answer | 1 |
| Mean week of pregnancy (SD) | 30.7 (7.7) |
| Pre-pregnancy chronic condition | |
| Diabetes | 5 (4.9%) |
| Hypertension | 10 (9.7%) |
| Depression | 18 (17.5%) |
| Other | 7 (6.8) |
SD: standard deviation.
Table 2.
Demographic characteristics of 28 obstetrics and gynecology (OB/GYN) and family medicine providers at the Mountain Area Health Education Center (MAHEC).
| Provider characteristics | OB/GYN (n=13) | Family medicine (n=15) | Totaln (%) |
|---|---|---|---|
| Age | |||
| 21–30 | 4 (33.2%) | 6 (40.0%) | 10 (35.7) |
| 31–40 | 5 (41.5%) | 6 (40.0%) | 11 (39.3) |
| 41–50 | 3 (24.9%) | 3 (20.0%) | 6 (21.4) |
| 51+ | 0 | 0 | 0 |
| Gender | |||
| Male | 12 (92.3%) | 9 (60.0%) | 21 (75.0) |
| Female | 1 (7.7%) | 6 (40.0%) | 7 (25.0) |
| Race | |||
| White | 11 (91.7%) | 13 (86.7%) | 24 (85.7) |
| Asian | 1 (8.3%) | 1 (6.7%) | 2 (7.1) |
| Native Hawaiian or other Pacific | 0 | 1 (6.7%) | 1 (3.5) |
| Islander | 1 (3.5) | ||
| Ethnicity | |||
| Hispanic/Latino | 0 | 0 | 0 |
| Not Hispanic/ Latino | 12 (100.0%) | 15 (100.0%) | 27 (96.4) |
| Professional title | |||
| Resident | 5 (38.5%) | 8 (53.3%) | 13 (46.4) |
| Doctor of Medicine (MD) faculty | 8 (61.5%) | 7 (46.7%) | 15 (53.6) |
| Years in clinical practice | |||
| 0–5 | |||
| 6–10 | 6 (46.2%) | 10 (66.7%) | 16 (57.1) |
| 11–15 | 4 (30.8%) | 3 (20.0%) | 7 (25.0) |
| 16–20 | 1 (7.7%) | 1 (6.7%) | 2 (7.1) |
| 21–25 | 1 (7.7%) | 1 (6.7%) | 2 (7.1) |
| 26+ | 1 (7.7%) | 0 | 1 (3.5) |
The mean age for providers was 34.6 years (SD 7.4) with a larger proportion of the sample who identified as a non-Hispanic white male (n=24, 86%). The proportion of provider respondents who were residents (n=13, 46%) was roughly equal to the number of physician faculty (n=15, 54%) and the majority of the provider sample were early career with 0–5 years of clinical practice (n=16, 57%).
Patient responses
Current use of digital devices
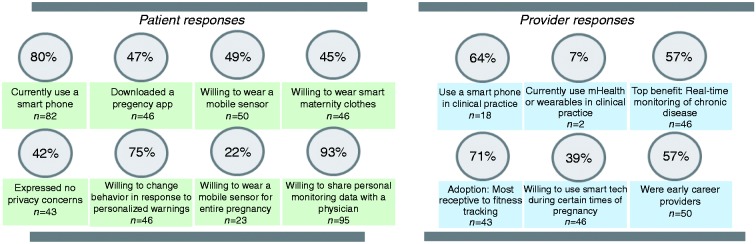
More than 80% of respondents reported using their smartphone often or all the time for the following top reported activities: texting (n=92, 89%), Internet access (n=81, 79%), phone calls (n=77, 75%), social networking (n=71, 69%), taking photos/videos (n=66, 67%), and email (n=60, 58%). Roughly half of all pregnant respondents reported having downloaded a pregnancy-related health app (n=48, 47% yes versus n=55, 53% no). While 82% of respondents (n=84) reported use of GPS technology on their smartphone, only 44% (n=45) of women would consider carrying a GPS tracker while pregnant to monitor environmental exposure (see Figure 2).
Figure 2.
Current digital device ownership and perceived new uses of digital devices or wearable health technology during pregnancy among patient and physician respondents.
Receptivity to wearing mobile sensors
Roughly half of participants (n=50, 49%) answered “yes” when asked if they would consider wearing a mobile sensor during pregnancy and 45% of respondents (n=46) would consider wearing a sensor embedded in their maternity clothes to monitor health indicators while pregnant.
Privacy concerns
A total of 42% of patients (n=43) reported “no” when asked if they had privacy concerns about data stored on their smartphone or personal monitoring device. Roughly three out of 10 patient respondents went on to report that they would have privacy concerns about data stored on their smartphone or personal monitoring device being moved to a companion website or smartphone app. A large majority of pregnant women in this sample (n=95, 93%) would feel comfortable sharing information from personal monitoring devices with their doctor. Most women (n=91, 88%) believed that this type of information would improve their health and decrease the risk of disease, injury, or an adverse pregnancy health event.
Duration of monitoring
Patient response to the question “How long would you be willing to wear a GPS tracker while pregnant?” were mixed, but 22% of women (n=23) reported a willingness to wear a GPS tracker for the entire pregnancy.
Behavioral modification
An overwhelming majority of patients responded with a willingness (n=78, 75%) to change their behavior during pregnancy in response to receiving personalized recommendations (based on height, weight, physiological monitoring) from their smartphone. When patients were asked which of the following scenarios they would consider wearing sensors to monitor health and the environment, they ranked pregnancy health (n=79, 76%) first followed by chronic disease management (n=73, 71%), personal health and diet monitoring (n=69, 67%), fitness tracking (n=69, 67%), and workplace health and safety (n=59, 57%).
Provider responses
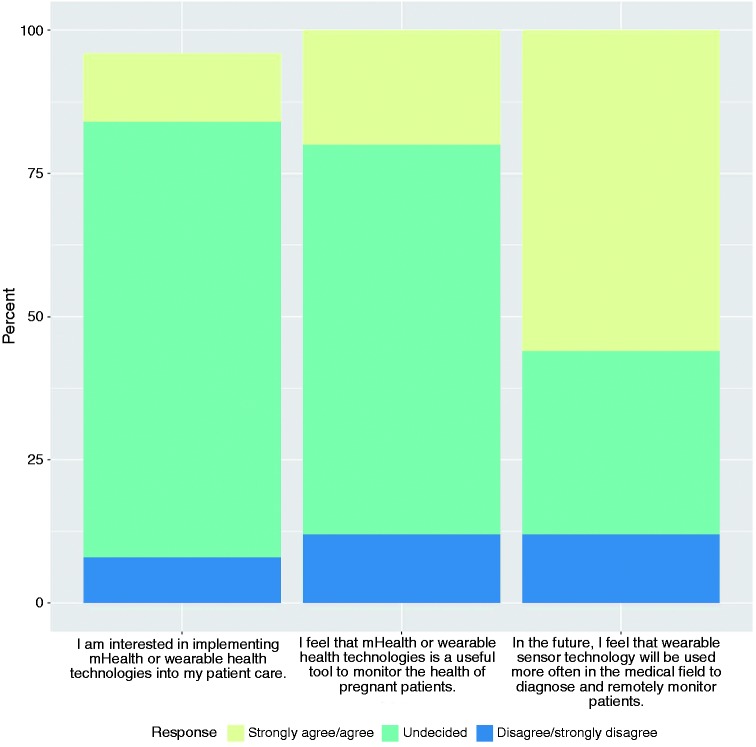
More than half of providers (n=18, 64%) reported frequent use of a smartphone in their clinical practice (Figure 2). The top three clinical tasks that involved the use of smartphones among providers were: (a) access professional clinical reference tools (n=20, 71%); (b) email colleagues (n=18, 64%); and (c) check drug recommendations for prescribing and safety information (n=17, 61%). A small proportion of the physician sample (n=2, 7%) currently used mHealth or wearable sensor technologies in their medical practice, while most physicians reported being undecided (n=19, 68%) concerning their interests in implementing this type of technology into patient care. Although, about half of providers (n=14, 50%) felt that wearable sensor technology will be used more often in the medical field to diagnose and remotely monitor patients in the future (Figure 3).
Figure 3.
Physician responses on level of comfort in incorporating wearable sensor technology into their patient care.
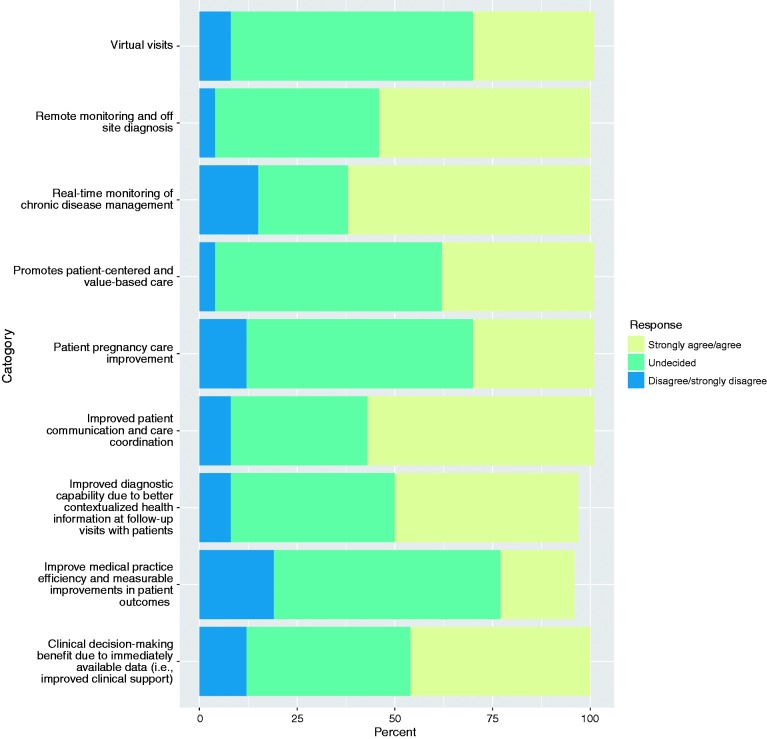
Potential benefit and perceived limitations of wearables
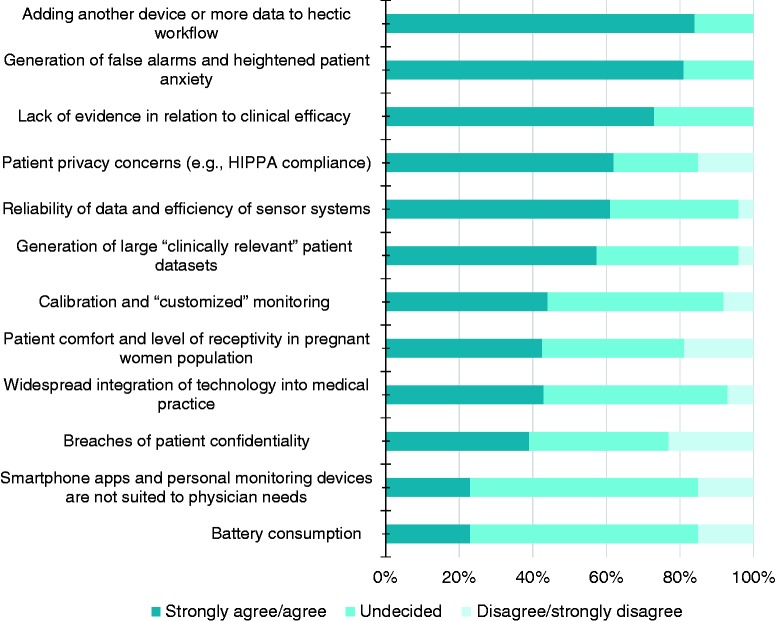
Physicians perceived the top benefits of wearable health technologies were: (a) real-time monitoring of chronic disease management (n=14, 57%); (b) improved patient communication and care coordination (n=15, 54%); (c) remote monitoring and off-site diagnosis (n=13, 50%) (d) clinical decision-making (n=11, 43%) (see Figure 4). When asked about the potential physician barriers/limitations in using wearable sensor technology to care for their patient population, many responded that adding another device or more data to an already hectic workflow (n=22, 78%), generation of false alarms and heightened patient concern (n=21, 75%), as well as safeguarding patient privacy (n=16, 57%) and reliability of data (n=16, 57%) were primary concerns (see Figure 5). When considering the adoption of wearable sensors to monitor a patient’s health and environment during pregnancy, providers were the most receptive to fitness tracking/personal health and diet monitoring (n=20, 71%), chronic disease management (n=19, 68%), and promote behavioral change (n=18, 64%).
Figure 4.
Perceived benefit in using wearable sensor technology in patient care among physicians.
Figure 5.
Perceived barriers/limitations in using wearable sensor technology in patient care among physicians.
Duration of monitoring
Providers were asked a similar question concerning at what time point during pregnancy would they consider implementing the use of wearable sensor technology as part of their patient’s clinical care and 39% (n=11) responded only during certain times.
Health and environmental monitoring during pregnancy: providers and patients
We observed differences between provider and patient preferences concerning the types of health and environmental monitoring data each group would like to see tracked during pregnancy (see Table 3). For example, the top three provider preferences for health monitoring were blood glucose, blood pressure, and chronic conditions compared to the patient preferences of infant heart rate, blood pressure, and blood glucose. Only about a third of physicians (36%) reported a preference for tracking fetal heart rate compared to 84% of patients. However, providers and patients demonstrated similar preferences for the types of desired environmental monitoring; yet, patients as a whole expressed more interest in tracking environmental measures during pregnancy compared to their providers. Although a few physicians cautioned against false alarms and the potential for increased patient worry in open-ended responses, many felt that this type of wearable technology might be best used in motivated higher-risk pregnancies.
Table 3.
Patient and provider preferences concerning the types of health and environmental monitoring data both would like to track during pregnancy.
|
Patient preferences |
Provider preferences |
|||
|---|---|---|---|---|
| Health n (%) | Environmental n (%) | Health n (%) | Environmental n (%) | |
| #1 | Infant heart rate80 (78%) | Chemical/pesticides68 (66%) | Blood glucose21 (75%) | Chemical/pesticides8 (29%) |
| #2 | Blood pressure72 (70%) | Water quality64 (62%) | Blood pressure19 (68%) | Water quality8 (29%) |
| #3 | Blood glucose66 (64%) | Air quality53 (51%) | Chronic conditions14 (50%) | Air quality7 (25%) |
Responses are for the combined categories of “all the time” and “often.”
Discussion
Unlike other mHealth studies that only address the effectiveness of smart and wearable technology,11–13 our study examined the current use, perceptions of, and interests in the use of smart technology and other digital health applications in prenatal care among providers and patients. Digital use at this rural health clinic was high among our sample of patients and providers. Roughly 80% of patients reported smartphone ownership, a number comparable to ownership reported in the American public at large (77%), with eight out of 10 patients reporting access to the Internet.14 Smartphone usage for professional purposes among physicians in our sample was also higher than usage reported by a representative sample of US physicians (89% vs 79%, respectively).15–17 A large proportion of providers would never use their mobile devices for e-prescribing (82%), to diagnose or treat conditions (71%), or for patient engagement (57%). This finding suggests that while the use of digital technology has grown among consumers and providers alike, the adoption of mHealth technologies by providers in the realm of women’s health care, especially in a rural care setting, may be lagging.
Most physicians in our sample did not currently use mHealth technology or wearables in their patient care. While an overwhelming seven out of 10 providers remained undecided on this issue, roughly half of physician respondents anticipated that digital health and wearable technology will be used more often in the future to diagnose and remotely monitor patients. This finding revealed that there is an overall agreement among these providers concerning the potential clinical benefit, but many may not be ready to adopt these technologies in their clinical practice. Yet, a recent American Medical Association (AMA) survey demonstrated that 85% of providers are increasingly becoming more accepting of digital health tools as advantageous in their practice.18 This ambiguity among women’s health providers may be attributed to their expressed concerns about additional increases in an already hectic workload and tempered by an insufficient evidence base supporting the clinical implementation of digital technology in improving the quality of prenatal care, as well as its ability to ensure the protection of patient information and enhanced patient safety.19
The recent transition to electronic medical record (EMR) keeping has greatly increased the amount of time that providers spend on their clinical documentation.20 In fact a study by the AMA observed that provider Electronic Health Record (EHR) use monopolizes their day-to-day tasks.21 For every hour a provider spends with their patients, they spend another two hours on EHR keeping. This finding highlights potential reasons why physicians may be reluctant to adopt new technologies, namely due to the significant increase in workload that technology adds to a provider’s already demanding schedule. However, this finding also sheds light on how technology may be leveraged in the future to reduce physician workload and improve provider-patient interactions.
A major barrier for provider’s utilization of smart and wearable technology is the lack of evidence demonstrating that these new technologies increase quality of health care.22,23 A recent review of the impact of technology-enabled care in the field of psychiatry observed that digital technologies may lead to significant improvements in care by facilitating more effective communication between patients and providers and lending to overall improvements in patient-provider rapport.24 The AMA is currently focused on the use of digital tools aimed at helping providers to be more efficient and effective in the care that they provide, as well as more responsive to patient care needs through increased support for team-based care, promotion of care coordination, reduced cognitive workload, and the facilitation of digital and mobile patient engagement.19
Providers perceived real-time monitoring of chronic disease management and remote monitoring/off-site diagnosis as the leading benefits of wearable health technologies. One way that remote monitoring may improve prenatal care is through the reduction of clinical visits in low-risk pregnancies. According to current clinical guidelines, the frequency of prenatal care visits in an uncomplicated pregnancy should occur every four weeks for the first 28 weeks, every two weeks between 28 and 36 weeks of gestation, and weekly from 36 weeks on. The uniformity of this 14 or more visit schedule has largely been adopted by providers based on tradition, and this model of care is motivated by the detection of pregnancy-related risks, such as hypertensive disorders. A higher frequency of visits has not corresponded with improved patient health outcomes and this practice is not well-substantiated by the literature, especially for low-risk pregnancies.25–28 Moreover, some would argue this model has led to a shift in the locus of control from the patient to the provider and has likely played a role in the medicalization of pregnancy more toward a disease treatment model of care. Yet results of an Expert Panel on the Content of Prenatal Care in 1989 recommended a more flexible visit schedule that is responsive to the individual needs of each woman (i.e. more visits for new mothers or higher-risk pregnancies and fewer visits for multiparous or low-risk women).29
While nearly three decades have passed since this recommendation of reduced prenatal care visits coupled by mounting research demonstrating that a schedule with fewer visits for low-risk pregnancies is not associated with elevated adverse maternal or fetal outcomes including preterm delivery, preeclampsia, and low birth weight,30 little has been gained in the way of new prenatal care models, even in the presence of emerging technologies that allow for remote monitoring of physiologic parameters in pregnant women that is both simple and cost-effective.31 New patient-centered models of care that not only consist of fewer office visits but also integrate virtual care options may allow a woman to connect with her care team outside of routine visits and in a more on-demand fashion, leading to improvements in patient satisfaction. This virtual model has significant potential to shift the current prenatal clinic’s culture from a disease-centric model to a wellness care model that will further serve to empower patients to take more of an active role in their pregnancy health.
In spite of a substantial body of evidence that demonstrates the safety of a reduced visit schedule, medical practices have been slow to adopt this model of care.32 Provider hesitation may in part be due to the results of studies that show lower patient satisfaction with reduced visit schedules.26,28,33 A new model of care that reduces pre-planned office visits but also increases virtual connections with clinical staff and other pregnant women, leveraging new technologies for enhanced patient-provider communications and connectedness, has the potential to address lingering concerns about patient satisfaction. A recent study at the Mayo Clinic examined the implementation of remote prenatal monitoring with digital health tools.34 Results showed that women with low-risk pregnancies who were randomized to the intervention group with reduced number of office visits and remote monitoring had equivalent health outcomes as their low-risk counterparts in the standard of care group. The intervention group also reported higher patient satisfaction and lower maternal stress, as well as no change in perceived quality of care. In a similar study of remote monitoring of prenatal care, patients randomized to the reduced schedule of visits (n=8) supplemented with digital monitoring of blood pressure and weight reported higher patient satisfaction and no difference in pregnancy outcomes.35
A new model of care has the potential to reduce the number of visits in uncomplicated pregnancies and increase outpatient monitoring in higher risk pregnancies, while fostering patient-provider connectivity via advances in telemedicine and remote monitoring technology. In our patient population, 90% of women reported that they would feel comfortable sharing information from personal monitoring devices with their doctor. Further, remote monitoring may lead to health care savings by allowing for the timely identification of adverse pregnancy events in the absence of an increase in ambulatory or hospital-based interventions.36 Smart and wearable technologies have significant capability to provide high-quality, personalized prenatal care to all pregnant women. Digital technologies may help move health care toward a more patient-centric model and provide a more seamless user experience for expectant mothers.
Compared to a general reluctance among physicians, patients were more open to using technology to improve their pregnancy care, and approximately five out of 10 patients in our sample would consider wearing a mobile sensor during pregnancy. Similar findings were observed in a 2016 survey on reactions to telemedicine, remote patient monitoring/sensors, and drones/robotics that showed US health care consumers are increasingly interested in using technology-enabled care.37 Roughly 70% of consumers expressed a willingness to use at least one of the technologies, whereby half of respondents were interested in using telemedicine for chronic disease monitoring, and caregivers were a primary population who expressed interests in using sensor technology. This finding is be especially relevant for expectant mothers, a group that might be particularly interested and engaged in continuous health monitoring of parameters such as blood pressure and other health parameters involving their unborn child (e.g. fetal monitoring).
More than a third of pregnant women in our sample expressed a willingness to carry a GPS tracker while pregnant to monitor environmental exposures, a similar finding was observed among 38% of consumers who engaged in caregiving and who also demonstrated interests in using GPS-locational tracking for their loved ones.37 Some research suggests that receptivity toward the use of sensor technology is highest among older adults, for example locational tracking among consumers was higher in baby boomers and seniors (43% and 45%, respectively) compared to millennials and Generation X consumers (33% and 33%, respectively).37 Although some research suggests that pregnant women may be an ideal population to test wearable sensors and other smart technologies, as many patients are younger (e.g. mean age for our survey was 27 years) and are more familiar with technology than elderly patients with chronic conditions, who have difficulty understanding wearable technology, often requiring training in order to use and understand its full potential.11
Limitations
We recognize that there are some limitations to our study. First, our survey results may be influenced by self-selection and our surveyed population is not representative of physicians nationwide. Because pregnant women were recruited using a rolling “first-come-first-served” basis and self-selected into the study, we were unable to keep track of how many women picked up a brochure and subsequently declined participation. However, as a reference point, on average the clinic treats approximately each year the clinic treats approximately 1650 new obstetric patients and/or women who transferred care. Moreover while surveys are desirable for an overall high response rate, we observed a low response rate for open-ended questions that have the ability to provide greater detail about physicians' and patients' perceptions of wearable sensor technology.
Future studies
Rigorous longitudinal studies coupled with innovative methodological development are needed to evaluate the diagnostic capabilities of wearable sensors during pregnancy, especially in higher risk pregnancies, as well as acceptability among patients and providers and compliance in self-management of chronic conditions. With nearly 20% of US residents living in rural areas, yet only 9% of physicians working in rural areas, wearable sensors and other digital health technologies have the potential to revolutionize diagnostic and disease management in a rural environment decreasing rural and urban health disparities.38
Patient concerns over privacy and maintaining confidentiality of data on protected health information and location have been cited in several studies.11 Patients in our sample did not express concerns over privacy issues, and only 38% of providers thought that patient confidentiality was a barrier to mHealth technologies. Health monitoring using vital signs and other physiological measures from wearable sensors has been gaining momentum over the past few years, but widespread integration of these technologies into routine medical practice, particularly prenatal care, has remained limited due to concerns around patient privacy, clinical efficacy, and uncertainty in the reliability of these emerging wearable technologies. Further, the large quantities of data generated from the use of these smart technologies far outstrips a provider’s time availability, and most providers are not equipped with the necessary skills to accurately discern important health trends in these data or use these data as the basis for sound clinical decision-making. There is currently a shift in research focus away from deploying these devices in real-world settings to advancing data mining techniques to design intelligent “personalized” algorithms for anomaly detection and decision-based awareness.39
A key challenge concerning wearable systems that support complex and non-invasive health care applications is the integration and interpretation of sensor signals in diagnostic procedures that accurately predict the changeover from a healthy to a disease state in a patient.40 A recent review summarized the key data mining tasks as acquisition, preprocessing, transformation, modelling, and evaluation, with the end goal being that each of these tasks results in anomaly detection, prediction, and diagnosis/decision-making.41 Mobile tracking technologies have the potential to improve traditional exposure assessment methods (e.g. questionnaire, cross-sectional samples) by reducing participant burden with passive collection of health data on a large number of participants, but more research is needed to better understand public acceptance, utility in enhanced clinical decision-making, and perceived additional burden among physicians.
Conclusions
Wearable technologies have the potential to improve patient-provider interactions for effective pregnancy health management, especially for rural underserved populations, as well as providing a cost-effective means for remote monitoring of uncomplicated pregnancies or higher risk women. The present study observed that patients and providers responded favorably to the implementation of mHealth or wearable sensor technology in prenatal care, though patients had a generally more positive reaction than providers. Unlike patients, providers were undecided about current implementation but felt that in the future, mHealth would be a valuable tool. The AMA is placing increased focus on the importance of the development of evidence-based, valid, and effective digital health tools that improve patient care and launch the health care system into 21st century care. More in-depth research is needed on the factors that influence provider acceptance of using smart technology in prenatal care, as well as feasibility studies to monitor patient acceptability and compliance to self-monitoring protocols. Observational studies demonstrating the adequate data quality and validity in detecting emerging conditions are needed to inform the future of mHealth and wearable technology developments. More research on what providers require in order to implement mHealth applications in clinical practice is needed before the successful adoption in prenatal care.
Acknowledgements
The authors would like to thank the patients and providers at MAHEC for helping to inform the next steps of this research.
Conflict of interest
The authors have no conflicting financial interests to report.
Contributorship
JR, DB, and MS researched literature and conceived the study. JR, SG, MS, DB, and CC were involved in protocol development, gaining ethical approval, patient recruitment and data analysis. JR wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approval
Institutional review board approval was obtained from the North Carolina State University (IRB#9266) and Mission Health System (IRB#16-08-1602).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Guarantor
Jennifer Runkle.
Peer review
This manuscript was reviewed by two reviewers, the authors have elected for these individuals to remain anonymous.
References
- 1.Derbyshire E, Dancey D. Smartphone medical applications for women's health: What is the evidence-base and feedback? Int J Telemed Appl 2013; 11p. https://www.hindawi.com/journals/ijta/2013/782074/citations/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gritters J. Wearable health trackers: A revolution in cancer care. J Natl Cancer Inst 2017; 109: 1--6. [DOI] [PubMed] [Google Scholar]
- 3.Penders J, Altini M, Hoof CV, et al. Wearable sensors for healthier pregnancies. IEEE 2015; 103: 179–191. [Google Scholar]
- 4.Moreira MWL, Rodrigues JJPC, Oliveira AMB, et al. Smart mobile system for pregnancy care using body sensors. In: 2016 International Conference on Selected Topics in Mobile and Wireless Networking (MoWNeT), Cairo, Egypt, 11--13 April 2016. New York: IEEE.
- 5.Tiny Logics. Smart pillbox, https://pillbox.tinylogics.com/pages/about-us (2018, accessed 8 January 2018).
- 6.PPD Act. Postpartum depression: Action towards causes and treatment 2018, http://www.pactforthecure.com/ (accessed 12 January 2018).
- 7.Moreira MWL, Rodrigues JJPC, Kumar N, et al. Postpartum depression prediction through pregnancy data analysis for emotion-aware smart systems. Inf Fusion 2019; 47: 23–31. [Google Scholar]
- 8.Moreira MWL, Rodrigues JJPC, Sangaiah AK, et al. Semantic interoperability and pattern classification for a service-oriented architecture in pregnancy care. Future Gener Comput Syst 2018; 89: 137–147. [Google Scholar]
- 9.Qualtrics. The survey output for this paper was generated using Qualtrics software. Copyright 2018. Qualtrics and all other Qualtrics product or service names are registered trademarks of Qualtrics, Provo, UT, USA, http://www.qualtrics.com
- 10.SAS Institute Inc. The survey data analysis for this paper was generated using SAS software, Version 9.4 for Linux, 2018. Cary, NC: SAS Institute Inc.
- 11.Chan M, Esteve D, Fourniols JY, et al. Smart wearable systems: Current status and future challenges. Artif Intell Med 2012; 56: 137–156. [DOI] [PubMed] [Google Scholar]
- 12.Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Med 2013; 10: e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Signorini M, Lanzola G, Torti E, et al. Antepartum fetal monitoring through a wearable system and a mobile application. Technologies 2018; 6: 44. [Google Scholar]
- 14.Smith A. Record shares of Americans now own smartphones, have home broadband. Pew Research Center, http://www.pewresearch.org/fact-tank/2017/01/12/evolution-of-technology/ (2017, accessed 12 January 2018).
- 15.Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): A regional survey. BMC Med Inform Decis Mak 2012; 12: 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ventola CL. Mobile devices and apps for health care professionals: Uses and benefits. P T 2014; 39: 356–364. [PMC free article] [PubMed] [Google Scholar]
- 17.Statista. Physicians' usage of smartphones for professional purposes in the U.S. from 2012 to 2015, https://www.statista.com/statistics/416951/smartphone-use-for-professional-purposes-among-us-physicians/ (March 2015, accessed 12 July 2018).
- 18.Sarasohn-Kahn J. Doctors are growing to like digital health tools, says the AMA. Healthcare IT News, 5 October 2016, https://www.healthcareitnews.com/blog/doctors-are-growing-digital-health-tools-says-ama (accessed 31 October 2018).
- 19.American Medical Association (AMA) adopts principles to promote safe, effective mHealth applications, 16 November 2016. [press release], https://www.ama-assn.org/ama-adopts-principles-promote-safe-effective-mhealth-applications (2016, accessed 16 November 2018).
- 20.Poissant L, Pereira J, Tamblyn R, et al. The impact of electronic health records on time efficiency of physicians and nurses: A systematic review. J Am Med Inform Assoc 2005; 12: 505–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Health S., Physician EHR. use, workload trumping face time with patients, https://ehrintelligence.com/news/physician-ehr-use-workload-trumping-face-time-with-patients (6 September 2018).
- 22.Berger RG, Kichak JP. Computerized physician order entry: Helpful or harmful? J Am Med Inform Assoc 2004; 11: 100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yarbrough AK, Smith TB. Technology acceptance among physicians: A new take on TAM. Med Care Res Rev 2007; 64: 650–672. [DOI] [PubMed] [Google Scholar]
- 24.Parish MB, Fazio S, Chan S, et al. Managing psychiatrist-patient relationships in the digital age: A summary review of the impact of technology-enabled care on clinical processes and rapport. Curr Psychiatry Rep 2017; 19: 90. [DOI] [PubMed] [Google Scholar]
- 25.Binstock MA, Wolde-Tsadik G. Alternative prenatal care. Impact of reduced visit frequency, focused visits and continuity of care. J Reprod Med 1995; 40: 507–512. [PubMed] [Google Scholar]
- 26.Carroli G, Villar J, Piaggio G, et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet 2001; 357: 1565–1570. [DOI] [PubMed] [Google Scholar]
- 27.McDuffie RS, Jr, Beck A, Bischoff K, et al. Effect of frequency of prenatal care visits on perinatal outcome among low-risk women. A randomized controlled trial. JAMA 1996; 275: 847–851. [PubMed] [Google Scholar]
- 28.Sikorski J, Wilson J, Clement S, et al. A randomised controlled trial comparing two schedules of antenatal visits: The Antenatal Care Project. BMJ 1996; 312: 546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosen MG, Merkatz IR, Hill JG. Caring for our future: A report by the Expert Panel on the Content of Prenatal Care. Obstet Gynecol 1991; 77: 782–787. [PubMed] [Google Scholar]
- 30.Ridgeway JL, LeBlanc A, Branda M, et al. Implementation of a new prenatal care model to reduce office visits and increase connectivity and continuity of care: Protocol for a mixed-methods study. BMC Pregnancy Childbirth 2015; 15: 323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vegesna A, Tran M, Angelaccio M, et al. Remote patient monitoring via non-invasive digital technologies: A systematic review. Telemed J E Health 2017; 23: 3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gregory KD, Johnson CT, Johnson TRB, et al. The content of prenatal care: Update 2005. Women's Health Issues 2006; 16: 198–215. [DOI] [PubMed] [Google Scholar]
- 33.Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev 2015; 7: CD000934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Butler Tobah YS, LeBlanc A, Branda M, et al. A novel approach to prenatal care. Obstet Gynecol 2016; 127: 7S–8S. [Google Scholar]
- 35.Marko KI, Krapf JM, Meltzer AC, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: A prospective observational trial. JMIR Res Protoc 2016; 5: e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gyselaers W, Storms V, Grieten L. New technologies to reduce medicalization of prenatal care: A contradiction with realistic perspectives. Expert Rev Med Devices 2016; 13: 697–699. [DOI] [PubMed] [Google Scholar]
- 37.Reh G, Korenda L, Cruse CB. Will patients and caregivers embrace technology-enabled health care? Findings from the Deloitte 2016. Survey of US health care consumers, https://www2.deloitte.com/content/dam/insights/us/articles/3164_Technology-enabled-health-care/Technology-enabled-health-care.pdf (accessed 13 September 2018).
- 38.AHRQ. National healthcare quality and disparities report. AHRQ Pub. No. 17-0001. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/research/findings/nhqrdr/nhqdr16/index.html (2016, accessed june 2018).
- 39.Banaee H, Ahmed MU, Loutfi A. Data mining for wearable sensors in health monitoring systems: A review of recent trends and challenges. Sensors (Basel) 2013; 13: 17472–17500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nangalia V, Prytherch DR, Smith GB. Health technology assessment review: Remote monitoring of vital signs–current status and future challenges. Crit Care 2010; 14: 233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sow D, Turaga DS, Schmidt M. Mining of sensor data in healthcare: A survey In: Aggarwal CC. (ed.) Managing and mining sensor data. Boston, MA: Springer US, 2013, pp.459–504. [Google Scholar]