Abstract
Background
This pilot study aimed to ascertain whether the local application of ascorbic acid (AA), of T3, and of rat (r) bone marrow mesenchymal stem cells (BMSCs), alone or in all possible combinations, promoted healing after an Achilles tendon injury in a rat model.
Methods
An Achilles tendon defect was produced in 24 6–8-week-old male inbred Lewis rats. The animals were then randomly divided into eight groups of three rats each. The tendon defect was filled with 50 μL of phosphate-buffered saline (PBS) containing (1) 50 μg/mL AA (AA group), (2) 10−7 M T3 (T3 group), (3) 4 × 106 rBMSCs (rBMSC group), (4) 50 μg/mL AA + 10−7 M T3 (AA + T3 group), (5) 4 × 106 rBMSCs + 50 μg/mL AA (rBMSC + AA group), (6) 4 × 106 rBMSCs + 10−7 M T3 (rBMSC + T3 group), (7) 4 × 106 rBMSCS + 50 μg/mL AA + 10−7 M T3 (rBMSC + AA + T3 group), and (8) PBS only (control group: CTRL). All treatments were administered by local injection immediately after the tendons had been damaged; additionally, AA was injected also on the second and fourth day from the first injection (for groups 1, 4, 5, and 7), and T3 was injected again every day for 4 days (for groups 2, 4, 6, and 7). At 30 days from initial treatment, tendon samples were harvested, and the quality of tendon repair was evaluated using histological and histomorphological analysis. The structure and morphology of the injured Achilles tendons were evaluated using the modified Svensson, Soslowsky, and Cook score, and the collagen type I and III ratio was calculated.
Results
The group treated with AA combined with T3 displayed the lowest Svensson, Soslowsky, and Cook total score value of all tissue sections at histopathological examination, with fiber structure close to regular orientation, normal-like tendon vasculature, and no cartilage formation. AA + T3 also showed the highest collagen I and the lowest collagen III values compared to all other treatments including the CTRL.
Conclusion
There are potential benefits using a combination of AA and T3 to accelerate tendon healing.
Keywords: Ascorbic acid; Thyroid hormones; T3, bone marrow mesenchymal stem cells; Tendon
Introduction
About 3 to 5 million patients worldwide experience tendon injuries each year [1]. Tendon healing is slow and often incomplete: the currently available techniques for surgical intervention and repair are inadequate [2–5]. New procedures should be developed to produce better outcome. In this context, tissue engineering (the combination of cells, growth factors, and carriers into functional tissue) is a promising therapeutic option in tendon regenerative medicine.
Recently, cell-based, and especially stem cell-based, strategies for tendon regeneration have attracted enormous attention. Bone marrow mesenchymal stem cells (BMSCs) have been extensively studied, displaying tenogenic differentiation capacity [6], and are currently the most widely used type of stem cell [7, 8], since they have potential for improving tendon repair [6], accelerating healing, and regenerating normal tissue. At present, however, BMSCs alone seem ineffective [9, 10], and recent biological approaches, such as BMSCs in combination with growth factors, and specialized delivery systems are being explored to enhance tendon healing [11–13].
Our previous reports have shown that tendons express thyroid hormone (TH) receptor isoforms and that T3 and T4 hormones enhance tenocyte proliferation in vitro [14, 15]. Moreover, T3 and T4 contrast apoptosis in healthy tenocytes in a dose- and time-dependent manner [14, 15]. THs (especially T3) stimulate cellular proliferation and type I collagen formation, the major fibrillar collagen in tendons. Furthermore, we have shown that, in the presence of ascorbic acid (AA), T3 increases collagen I expression, and additionally, T3 also increases ECM protein secretion in the presence of AA and, in particular, biglycan and COMP (cartilage oligomeric matrix protein) expression [14, 16, 17]. Robinson et al. recently demonstrated that biglycan is required for mechanical proprieties in the tendon and for collagen fiber realignment after loading [18]. COMP is known to co-localize with collagen I [19], and a marked reduction of COMP in tendon injury has recently been demonstrated, suggesting the possibility of its use as a marker for tendon injury [20]. In addition, AA on its own triggers the proliferation of tendon-derived cells [16, 17]. AA also decreases nitric oxide synthesis (NOS) in the same experimental condition. NOS inhibition exerts beneficial effects on tendon regeneration and function in a murine of Achilles tendon rupture [21]. When AA is combined with T3, it synergistically induces an increase in tenocyte proliferation [17].
The role of thyroid hormones in stem cell function is still unclear and further study is required. Previous investigations have shown that the thyroid hormone T3 exerts a dose-dependent effect on the chondrogenic and osteogenic differentiation of BMSC in female rats, promoting chondrogenic matrix formation and collagen synthesis respectively [22, 23]. T3 treatment increases the differentiation of BMSCs induced to cardiomyocytes and promotes their maturation [24]. The combined treatment of BMSC with exercise and thyroid hormones enhances new neuronal cell generation and attenuates apoptosis in ischemia strokes in mice [25].
There is some uncertainty as to whether BMSC transplantation alone is sufficient to achieve satisfactory outcomes in tendon repair and healing. Therefore, it is necessary to assess the effects of combining other therapies with cell therapy to increase their therapeutic efficacy in tendon injury. In trying to translate all these findings into clinical practice, it would be reasonable, first of all, to hypothesize that AA and T3 in combination would be beneficial to human tendon healing in vivo. Moreover, no studies have yet been performed to understand the influence of thyroid hormones on BMSCs in tendon regeneration, nor of thyroid hormones and BMSCs in combination with AA.
Therefore, the present pilot study, using a rat Achilles tendon injury model, aimed to verify the roles of rBMSC, AA, and T3 in promoting healing after local inoculation at the site of injury. rBMSC, AA, and T3 were used alone and in every possible combination and compared with an untreated control. After a period of 30 days, the efficacy of local administration of all combinations of rBMSCs, AA, and T3 on healing was evaluated.
Materials and methods
Ethics
All the experiments were conducted according to the protocols of good animal experimentation under the Italian Health Ministry approval n°513/2016-PR and in accordance with international laws and policies (Directive 2010/63/EU of the European Parliament and of the Council, Italian Legislative Decree 26/2014, Guide for the Care and Use of Laboratory Animals, NIH publication 85-23, 1985).
Isolation, culture, and characterization of rat BMSCs
rBMSCs were isolated from the bone marrow of the tibia and femur of three 6–8-week-old male inbred Lewis rats (ENVIGO, Wyton, UK), as previously described [26]. The bone marrow cells were seeded into a tissue culture flask in MesenCult Basal Medium (STEMCELL Technologies, Vancouver, Canada), supplemented with penicillin/streptomycin (100 U/mL–100 μg/mL) and 10% FBS, and incubated at 37 °C, in a 5% CO2 atmosphere with 95% relative humidity. Three days after seeding, floating cells were removed, and the medium was replaced with a fresh medium. Adherent cells were allowed to reach approximately 80% confluence (12–17 days for the first passage). Cells were detached following treatment with StemPro accutase (ThermoFischer Scientific, USA) and replaced every 6–8 days at approximately 80% confluence. Cells at second passage (P2) were used unless otherwise stated. When the cells in the culture flasks were nearly confluent, the cells in the primary culture were sub-cultured and collected for the study. In addition, mesenchymal stem cells (MSCs) were tested by flow cytometry (Becton Dickinson, Franklin Lakes, New Jersey, USA) using specific surface markers, being negative for CD45 and positive for CD90 [27]. Debris particles were excluded from the analysis by gating on forward and side scatter (FSC and SSC) morphological parameters. Dead cells were gated out by propidium iodide (0.07 μg/mL, Sigma-Aldrich, Saint Louis, USA) staining; 10.000 viable and non-debris events in the morphological gate were recorded for each sample. Cells were acquired on a CytoFLEX flow Cytometer (Beckman Dickinson, CA, USA). The analysis was performed using CytExpert Software (Beckman Dickinson). The stem cell characteristics of bone MSCs were routinely confirmed by their trilineage differentiation abilities (adipocytes, osteoblasts, and chondrocytes) when cultured under appropriate conditions in vitro before being used for experimental procedures as previously described [27, 28]. Adipocytes were visualized by Oil Red-O staining, osteoblasts evidenced by alizarin red, and chondrocytes were visualized with Alcian Blue. Isolated rBMSCs (P0) were cryopreserved according to standard procedures in liquid nitrogen in 90% fetal bovine serum + 10% DMSO and stored in liquid nitrogen in vials until transplantation.
Animal surgery and pilot study design
Twenty-four 6–8-week-old male inbred Lewis rats (ENVIGO) were housed under controlled conditions in the Interdepartmental Service Centre - Station for Animal Technology, University of Rome “Tor Vergata” (Italy), supplied with standard diets (4RF18; Mucedola srl, Italy) and water ad libitum. Under general anesthesia induced using an intramuscular injection of tiletamine/zolazepam (50 mg/kg) (Zoletil 100, Virbac Italia SRL, Italy) and xylazine (10 mg/kg) (Rompun Bayer AG, Germany), the right Achilles tendon was laid open by a skin incision approximately 10-mm long on the medial aspect of the right hind limb of each rat. In each animal, an Achilles tendon defect 2 mm in diameter was produced as previously described [29] with some modifications. Briefly, the Achilles tendon was separated from the surrounding tissue, and the medial, more prominent component of the Achilles tendon, the m. flexor digitorum superficialis, was isolated. Using a sterile punch (diameter 2 mm), which was placed around the Achilles tendon at a distance of approximately 2 mm from the calcaneus, a full-thickness hole, 2 mm in diameter, was made. The skin was closed by a continuous suture using absorbable 4.0 absorbable monofilament sutures. The animals were divided into eight groups (with three rats per group). The injured tendon was filled with 50 μL of phosphate-buffered saline (PBS), a physiological buffer solution which contained (1) 50 μg/mL AA (AA group), (2) 10−7 M T3 (T3 group), (3) 4 × 106 rBMSCs (rBMSC group), (4) 50 μg/mL AA + 10−7 M T3 (AA + T3 group), (5) 4 × 106 rBMSCs + 50 μg/mL AA (rBMSC + AA group), (6) 4 × 106 rBMSCs + 10−7 M T3 (rBMSC + T3 group), (7) 4 × 106 rBMSCS + 50 μg/mL AA + 10−7 M T3 (rBMSC + AA + T3 group), and (8) PBS only (control group: CTRL). Additionally, AA was injected again on the second and fourth day following the initial injection (for groups 1, 4, 5, and 7), while T3 was injected again every day for 4 days (for groups 2, 4, 6, and 7). Post-operatively, antibiotics and analgesics were administered: 0.5 mL/kg Baytril (Bayer AG, Germany) and 0.1 mL/kg/day Rimadyl (Veterfarma SpA, Italy). After 30 days, the animals were anesthetized and then euthanized using CO2 in specially designed chambers. Tendons were explanted, embedded in optimal cutting temperature (O.C.T.) compound medium (Sakura Finetek USA, Inc., Torrance, CA, USA), and quickly frozen in liquid nitrogen-cooled isopentane for sectioning at a thickness of 12 μm using a Leica (Leica Biosystems, Wetzlar, Germany) cryostat, and then stained with hematoxylin and eosin or Picro-Sirius red solution for histological and histomorphometric analyses and examined under white light and polarized light microscopy, respectively. Sections were examined independently by two pathologists in a blinded, random order.
Histological and histomorphometric examination
For histological and histomorphometric analyses, three sections per animal and three animals per group were evaluated for each experimental group. Three sections of each specimen were placed onto one slide at an approximate distance of 250 μm. Six areas were selected from each section to cover the entire surface of the tendon and were collected using an optical microscope (BX51, Olympus Italia Srl, Milano, Italy) at × 10 magnification, coupled to Aperio ScanScope (Aperio ScanScope CS, Aperio Technologies, Leica Biosystems, USA) digital image analysis system. A modified, semi-quantitative score obtained by the three different scores of Soslowsky, Svensson, and Cook’s scoring systems was used (Table 1) [30–32]. These scores take into account four different parameters: fiber structure, cellularity, vascularity, and cartilage formation. Each parameter was scored on a 4-point scale of 0–3, as follows: 0, normal; 1, slightly abnormal; 2, abnormal; and 3, markedly abnormal. The samples were scored according to whether there was a significant abnormal appearance. The total score is the sum of the values of each parameter varied between 0 (normal tendon) and 12 (severest abnormality) [33]. For the validation study, pathologists were additionally asked to make overall examinations for each specimen. The specimens were anonymized and randomized by an IRCCS Rizzoli Orthopedic Institute employee not involved in the study. For polarization microscopy, each section (three sections per animal, three animals per group) were imaged using × 8 magnification. To prevent variations in illumination and magnification, all pictures were recorded by the same person. The sections underwent further evaluation using computerized image analysis software (Aperio Area Quantification FL Algorithm). Color intensity and color amount (i.e., positively stained area) were measured by Aperio ScanScope CS (Aperio Area Quantification FL Algorithm, Aperio ScanScope CS Leica Biosystems). Collagen type I and type III percentages were calculated by these automated measurement of the red-orange fiber area (collagen type I) and pale green fiber area (collagen type III) from Picro-Sirius red staining [34].
Table 1.
Semi-quantitative histomorphometric scoring system as modified by Svensson, Soslowsky, and Cook
| Parameter | Grade 0 | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|---|
| Fiber structure, Svenson and Solowsky scores | Normal parallel collagen fibers | Mild changes (< 25% slightly separated fibers) | Moderate changes (25–50% disorganized, separated, and deteriorated fibers) | Marked changes (> 50% disorganized and hyalinized fibers) |
| Cellularity (aspect), Cook scores | Elongated nuclei and absence of cytosol | Oval nucleus and absence of cytosol | Round nucleus and little cytosol | Round nucleus and abundant cytosol |
| Vascularity, Svensson score | Few vessels, parallel to the fiber | Slight increase of vessels | Moderate increase of vessels | Marked increase of vessels |
| Cartilage formation | No cartilage | Isolated cartilage nodules | Moderate cartilage formation (25–50%) | Extensive cartilage formation (> 50%) |
Statistical analysis
Data are expressed as mean values ± standard deviation (SD). Statistical analysis was performed using the STATA v.14.2 software with data reported at a statistical significance level of p < 0.05. Two-level regression models (group-treatment = level 1 unit; rat = level 2 unit) with a random intercept term at level 2 and the treatment group as fixed effects, followed by adjusted Bonferroni post hoc test, were used to compare histomorphometric results (total score and collagen ratio). The estimates of the fixed and random parameters were obtained by using the restricted maximum likelihood method. The denominator degrees of freedom of the null sampling distributions of test statistics for fixed effects were computed by using the repeated method to take the bias associated with the small sample into account.
Results
Identification of rBMSC
Once they had been isolated and cultured, the rBMSCs were analyzed for immunophenotype by flow cytometry, which confirmed the expression of CD90 and the lack of CD45 (Fig. 1a). In addition, rBMSCs were functionally characterized by differentiation into adipocytes, osteoblast, and chondrocytes (Fig. 1b–d), displaying the typical characteristics of MSCs [35].
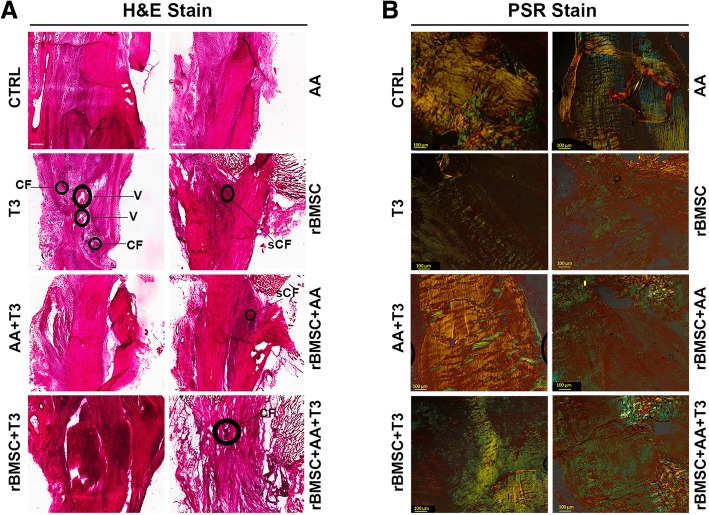
Fig. 1.
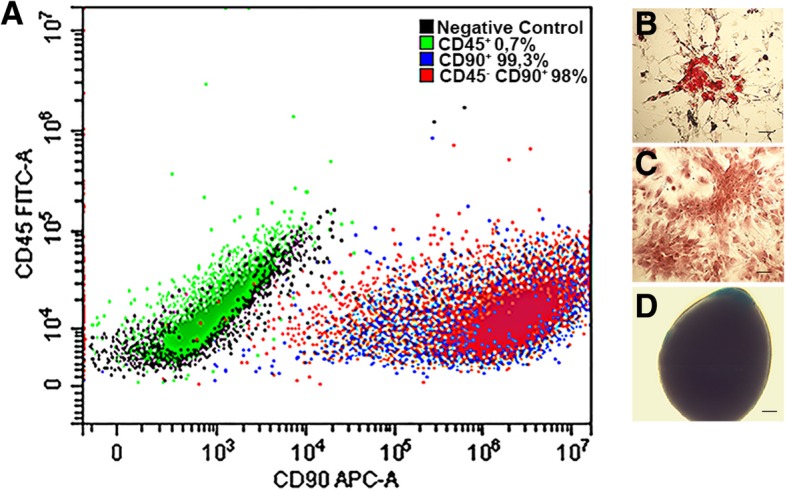
rBMSC characterization. An example of rBMSCs phenotype and functional analysis. a Flow cytometry analysis of MSCs for surface markers (CD45+ isotype control, CD90+ isotype control, negative control) showed that isolated bone marrow-derived cells expressed CD90, but not the hematopoietic marker CD45, confirming that only mesenchymal cells had been isolated (CD45−CD90+ cells population). b–d In vitro differentiation of mesenchymal cells: the cells were incubated in lineage-specific induction media and then analyzed by histochemical and cytological staining for b adipocytes (Oil Red-O staining), c osteoblasts (alizarin red staining), and d chondrocytes (Alcian Blue staining)
Local injection of AA + T3 ameliorated tendon repair
Surgical procedures and treatments (Fig. 2) did not determine any additional accidental damage and no clinical signs of necrosis or tissue infection. At gross examination post mortem, scar tissue was visible at the site of the core lesion in the center of each tendon. Macroscopically, no differences were visible between the groups. No macroscopic signs of necrosis or tendon degeneration were observed. The paratenon covering the tendon was of normal thickness, as were the collagen fibers of the epitenon, and no inflammatory infiltrate or other morphological changes were seen. Intra-class correlation for histology scores was excellent for inter-observer reliability (0.79–0.97 depending on score/sub-score). The lesions could be identified clearly on H&E staining. Histological analysis indicated incomplete restoration of structural integrity (Fig. 3).
Fig. 2.
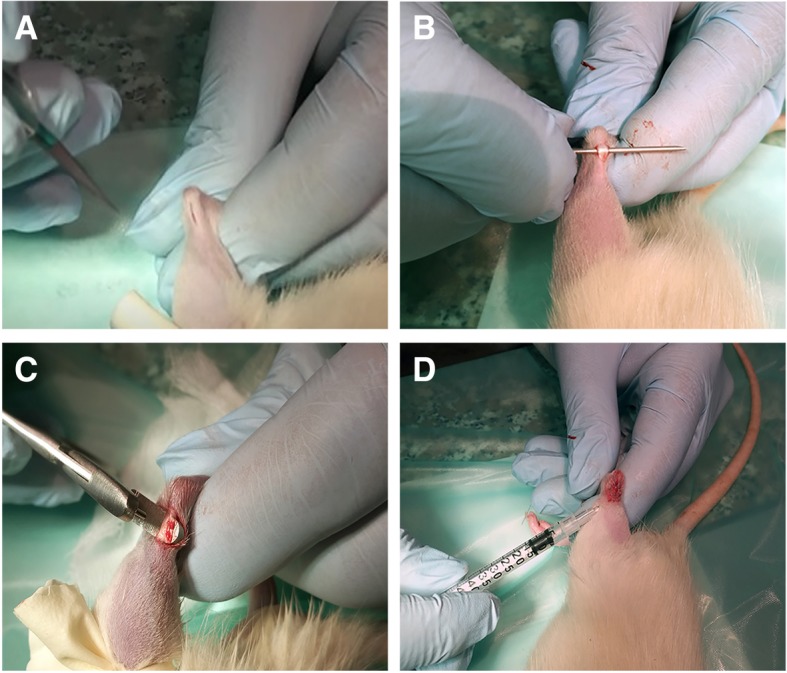
Surgical procedure. a, b Under general anesthesia, the right Achilles tendon was laid open by a skin incision approximately 10-mm long on the medial aspect of the right hind limb. c A 1-mm sterile punch was placed around the Achilles tendon at a distance of approximately 2 mm from the calcaneal bone. d Treated area: the skin was closed by a continuous suture and each treatment locally micro-injected
Fig. 3.
Histological analysis of tendon healing at 30 days from injury/start of treatment. a The injured Achilles tendons were then stained with H&E for each type of treatment, and the quality of tendon repair was evaluated based on properties displayed. [CF (cartilage formation), V (vessel); SCF (slight cartilage f)] (× 500). b longitudinal sections of the right hind limb rat Achilles tendons stained by Picro-Sirius red staining (PSR): (magnification × 4, scale bar = 500 μm). The thicker, mature collagen fibers appear red-orange (type I collagen); the thinner collagen fibers appear pale green (type III collagen)
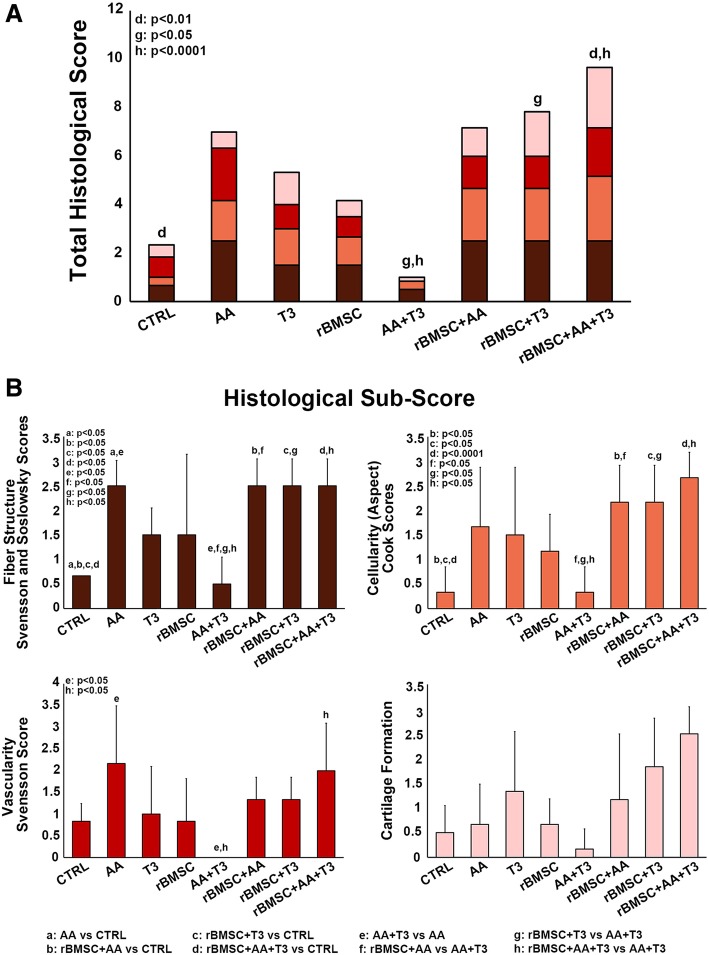
Semi-quantitative histomorphometric results are reported in Fig. 4. The total histological score was lower in the AA + T3-treated group (score 1) than in all the other group treatments (AA score 7; T3 score 5.3; rBMSC score 4.16; rBMSC + AA score 7.16; rBMSC + T3 score 7.16; rBMSC + T3 + AA score 9.66) including the CTRL group (score 2.3) (Fig. 4a). Specifically, in the group treated with AA + T3, score values were lower for fiber structure (close to regular orientation, score 0.5) than those in the CTRL group (0.7); vasculature (vessels run inconspicuous coursing parallel to the collagen fiber bundles in the septa, like in a normal tendon, score 0) than those in the CTRL group (score 0.8); and cartilage formation (slight cartilage formation was only observed in one section, score 0.1) than those in the CTRL group (slight formation of cartilage in three sections for one of the three animals, and in two sections for the second of the three animals, score 0.5). The rBMSC group had the same histology score as the CTRL group for cartilage formation (slight cartilage formation was observed in two of the three sections for the first animal and in one section only for the other two animals in the group) (Fig. 4b). The AA + T3 group total scores were significantly lower than those of the rBMSC + T3 group (p < 0.005) and the rBMSC + AA + T3 group (p < 0.0001). The rBMSC + AA + T3 group scored significantly higher than the CTRL group. Specifically, the AA + T3 group sub-scores were lower for fiber structure in comparison with the AA group, the rBMSC + AA group, the rBMSC + T3 group, and the rBMSC + AA + T3 group (p < 0.005); for cellularity scores, the AA + T3 group sub-scores were lower than for all other groups and, most significantly, than for the rBMSC + AA group, the rBMSC + T3 group, and the rBMSC + AA + T3 group (p < 0.005); for vascularity, the AA + T3 group sub-scores were significantly lower than for the AA group and the rBMSC + AA + T3 group (p < 0.005), and the AA + T3 group cartilage formation sub-scores were lower than all the other group treatments (Fig. 4b). In the AA + T3 group, the vascularity sub-score value was similar to that of a healthy tendon (Fig. 4b), and the value was significantly lower than that for the AA + T3 group and for the rBMSC + AA + T3 group (p < 0.005) (Fig. 4b).
Fig. 4.
Stacked histograms of the semi-quantitative histomorphometric score for treated and untreated control groups. a Total score for healthy tendon score, including cartilage formation, vascularity, cell aspect, and fiber structure scores (mean, n = 3). b Detailed sub-scores. One-way ANOVA test and adjusted Bonferroni (two-way) post hoc test
Analysis of the collagen ratio revealed that the association AA + T3 exerted greater effect on tendon healing than all the other treatments. Specifically, the collagen type I value was significantly higher than in the rBMSC + AA group and the rBMSC + AA + T3 group (p < 0.05; p < 0.01); the AA + T3 group collagen type III value was significantly lower than in the rBMSC + AA group and the rBMSC + AA + T3 group (p < 0.05; p < 0.01) (Fig. 5). The collagen type I value of the rBMSC + AA + T3 group was significantly lower than the CTRL (p < 0.05), and the collagen type III value was significantly higher in the rBMSC+AA+T3 group than the CTRL group (p < 0.05) (Fig. 5).
Fig. 5.
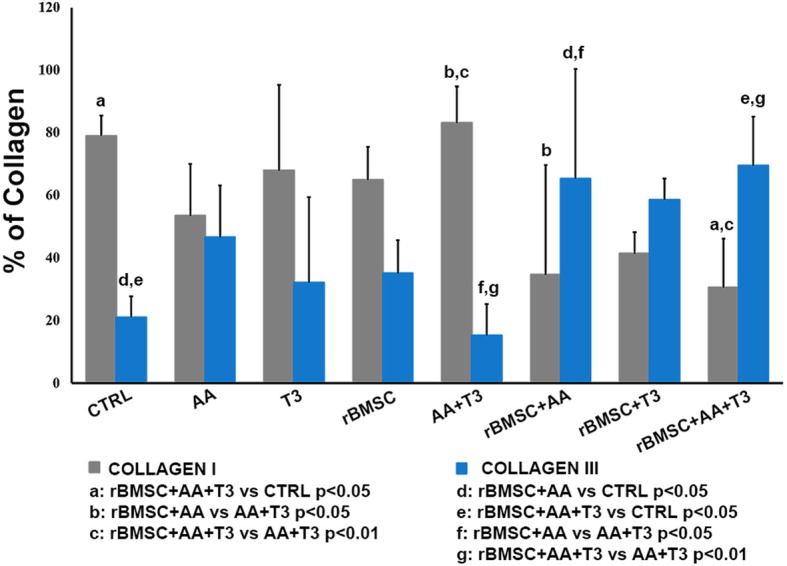
Histograms of type I and type III collagen content, expressed in percentages, for treated and untreated control groups (mean ± SD, n = 3). One-way ANOVA test and adjusted Bonferroni (two-way) post hoc test
Discussion
We wished to test the effect of local micro-injection of AA, T3, and rBMSCs, individually and in every possible combination, on tendon healing in damaged rat tendons. Our investigation logically follows prior studies which demonstrated the relevance of ascorbic acid and T3 in combination with the biological function of tenocytes. Novel preliminary findings demonstrate the efficacy of ascorbic acid in combination with the T3 hormone in improving tendon healing, confirming our previous in vitro studies [14, 16, 17]. Histological evaluation confirmed better restoration of normal tendon architecture with an optimal alignment of tendon fibers and blood vessels, although the continued presence of high cellularity suggests that the regenerative process was not complete. Furthermore, in the tendons treated with AA + T3, the analysis of the collagen ratios demonstrated a higher expression of collagen type I, and lower expression of collagen type III, than in all the other groups, including the CTRL group. Comparison of the AA + T3 treatment with the AA alone, and the T3 alone, showed that the co-administration of AA and T3 yielded greater beneficial effects than the administration of either separately. The histological score values and the collagen ratios were worse for AA alone, and for T3 alone, than for the CTRL group, although they were better than for the rBMSC + AA group, the rBMSC + T3 group, and the rBMSC + AA + T3 group. This was not the case for the histological score value of the rBMSC group. The healing process of an injured tendon passes through three main phases, featuring distinctive cellular and molecular cascades: (i) inflammatory; (ii) reparative (proliferation), characterized by cellularity and matrix production, which is mostly collagen type III; and (iii) remodeling (consolidation and maturation), replacing collagen type III with collagen type I and fiber organization [36]. Taken together, the results indicate that ascorbic acid acts in synergy with T3 to accelerate tendon healing.
Our results agree not only with our own previous data, but also with other studies [3, 37]. Ascorbic acid stimulates a wide range of tissue functions; it contributes not only to increased collagen synthesis and cross-linking, but also plays key roles in stem cell function, such as in the differentiation of mesenchymal stem cells into tenocytes [37, 38]. Supplementation with ascorbic acid also enhances tendon healing in mouse models [39]. Moreover, thyroid hormones are major determinants of tissue function, playing well-defined roles in cell signaling. The role of thyroid hormones in tenocyte physiology is a novel area of study in this field [14, 15, 40, 41]. Moreover, THs regulate the function of stem cells, controlling self-renewal, proliferation, and differentiation. In vivo studies suggest high intracellular level requirement of T3 to support normal myogenesis and muscle repair after cardiotoxin injury [42]. All the animals in the groups treated with rBMSC healed less well than all the other groups, including the CTRL group, when analyzed histopathologically and histomorphologically. The group which received rBMSC only showed better results than the rBMSC + AA group, the rBMSC + T3 group, and the rBMSC + AA + T3 group. At present, the use of mesenchymal stem cells in tendon healing is still the subject of controversy, debate, and study. Indeed, only three BMSC-based therapies have shown favorable outcomes in rat studies with improved histological and biomechanical tendon properties [43]. However, in accordance with our investigation, several other studies were not able to demonstrate beneficial effects of BMSC on tendon healing. Furthermore, no difference in collagen production or in extracellular matrix organization has been demonstrated. The source of stem cells for implantation is still under debate. In the present investigation, the cells used were derived from the bone marrow, but recent developments suggest that stem cells derived from the tendons themselves show the greatest promise to improve healing [44]. Moreover, it should be underlined that growth factors in combination with the cells have recently been shown to require controlled spatiotemporal delivery to the repair site to improve tendon healing [12, 44]. Consequently, greater enhancement of tendon healing could be obtained by specialized delivery approaches, for example, by tissue engineering using a variety of scaffolds [12, 44]. The exact mechanisms of tendon healing and the precise roles that different cell types play in the process are, as yet, not clear, and further studies are necessary to develop a range of suitable techniques involving stem cells to favor and hasten tendon regeneration and repair [45].
Our results do not confirm the findings of previous studies regarding the use of AA in combination with MSCs [39, 46]. This is likely because of the different methodology and different model used and the different source of the stem cells. Kang et al. used AA to stimulate MSCs before transplantation in a mouse tendonitis model, using adipose-derived cells [39]. Durant et al. used an in vitro model employing tendon-derived stem cells, which may have had some bearing on the results obtained [46]. T3 has not been used in previous in vivo studies. Hence, no direct comparisons can be made yet, and therefore, further work is required to understand the precise mechanisms involved and the full extent of possible benefits in any clinical applications which may be developed to improve, enhance, and/or accelerate tendon healing.
Conclusions
There are several limitations to the present pilot study. First, owing to our focus on histological and histomorphometric examination of repair, only one middle-term evaluation point was used. It remains inconclusive whether or not the effects of using BMSCs, AA, and T3 alone, and in every possible treatment combination, lead to short- and long-term structural and functional benefits to tendon healing. Secondly, the effectiveness of AA combined with T3 in improving strength and stiffness following the repair of rat tendons requires further analysis.
Despite these considerations, the present study would appear to [14–17] confirm the hypothesis that AA used in combination with T3 improves tendon healing in vivo, based upon the best histological score evaluation achieved and on collagen I and III ratio measurement. In the present investigation, for the first time, T3 has been utilized for tendon healing in an animal model, and that, apart from our previous in vitro study, no other studies have been made that investigate the activity of T3 in tendons. For this reason, our experimental model combining AA with T3 and with BMSCs is unique to date. Our results must stimulate two further areas of investigation—on the one hand, into the comprehension of the underlying mechanistic processes of T3 in a tendon environment and the associated complex interaction between T3, AA, and BMSCs; secondly, our data suggest that AA in combination with T3 could be used to develop possible cell-free therapy for improved tendon healing. Furthermore, it will be important to identify optimum delivery methods and doses of AA + T3 to improve tendon healing and avoid potential toxicity and, ultimately, to translate this approach into clinical applications in humans.
Acknowledgments
The authors thank Dr. C. Gargioli, from the Department of Biology, University of Rome “Tor Vergata”, Rome, Italy for his invaluable contribution to the discussion.
Funding
This study was financed by the PCFF Foundation, Pescara, Italy.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Abbreviations
- AA
Ascorbic acid
- BMSCs
Bone marrow mesenchymal stem cells
- COMP
Cartilage oligomeric matrix protein
- CTRL
Control group
- ECM
Extracellular matrix
- FSC
Forward scatter
- H&E
Hematoxylin and eosin
- r
Rat
- SD
Standard deviation
- SSC
Side scatter
- TH
Thyroid hormones
Authors’ contributions
CG and CALP carried out the isolation, culture, and functional characterization of rat BMSCs. MF, SB, and FV performed the histological and histomorphometric examinations. LC performed the data analysis. MG performed the histological flow cytometry. RB, RC, and MM operated on the experimental animals. FO operated on the animal surgery and made substantial contributions to the design of the study, data acquisition, and analysis. NM made substantial contributions to the conception of this project, critically analyzed and interpreted the data, and revised the manuscript for intellectual content. ACB conceived the study, made substantial contributions to its design and coordination, data acquisition, analysis, and interpretation, and drafted the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethical approval was obtained from Italian Health Ministry approval n°513/2016-PR.
Not applicable. Consent was not necessary for our study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Francesco Oliva, Email: olivafrancesco@hotmail.it.
Nicola Maffulli, Email: n.maffulli@qmul.ac.uk.
Clarissa Gissi, Email: gissi.clarissa@libero.it.
Francesca Veronesi, Email: francesca.veronesi@ior.it.
Lucia Calciano, Email: lucia.calciano@univr.it.
Milena Fini, Email: milena.fini@ior.it.
Silvia Brogini, Email: silvia.brogini@ior.it.
Marialucia Gallorini, Email: marialuciagallorini@gmail.com.
Cristina Antonetti Lamorgese Passeri, Email: cristinaalp94@gmail.com.
Roberta Bernardini, Email: roberta.bernardini@uniroma2.it.
Rosella Cicconi, Email: rosella.cicconi@uniroma2.it.
Maurizio Mattei, Email: mattei@uniroma2.it.
Anna Concetta Berardi, Email: annacberardi@yahoo.it.
References
- 1.Sharma P, Maffulli N. Biology of tendon injury: healing, modeling and remodeling. J Musculoskelet Neuronal Interact. 2006;6(2):181–190. [PubMed] [Google Scholar]
- 2.Woo SL, Hildebrand K, Watanabe N, Fenwick JA, Papageorgiou CD, Wang JH. Tissue engineering of ligament and tendon healing. Clin Orthop Relat Res. 1999;(367 Suppl):S312–23. [DOI] [PubMed]
- 3.Maffulli N, Wong J, Almekinders LC. Types and epidemiology of tendinopathy. Clin Sports Med. 2003;22(4):675–692. doi: 10.1016/S0278-5919(03)00004-8. [DOI] [PubMed] [Google Scholar]
- 4.Goh JC, Ouyang HW, Teoh SH, Chan CK, Lee EH. Tissue-engineering approach to the repair and regeneration of tendons and ligaments. Tissue Eng. 2003;9(Suppl 1):S31–S44. doi: 10.1089/10763270360696969. [DOI] [PubMed] [Google Scholar]
- 5.Gaspar D, Spanoudes K, Holladay C, Pandit A, Zeugolis D. Progress in cell-based therapies for tendon repair. Adv Drug Deliv Rev. 2015;84:240–256. doi: 10.1016/j.addr.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 6.Dai L, Hu X, Zhang X, Zhu J, Zhang J, Fu X, et al. Different tenogenic differentiation capacities of different mesenchymal stem cells in the presence of BMP-12. J Transl Med. 2015;13:200. doi: 10.1186/s12967-015-0560-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yin Z, Guo J, Wu TY, Chen X, Xu LL, Lin SE, et al. Stepwise differentiation of mesenchymal stem cells augments tendon-like tissue formation and defect repair in vivo. Stem Cells Transl Med. 2016;5(8):1106–1116. doi: 10.5966/sctm.2015-0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raggi C, Berardi AC. Mesenchymal stem cells, aging and regenerative medicine. Muscles Ligaments Tendons J. 2012;2(3):239–242. [PMC free article] [PubMed] [Google Scholar]
- 9.Khan MR, Dudhia J, David FH, De Godoy R, Mehra V, Hughes G, et al. Bone marrow mesenchymal stem cells do not enhance intra-synovial tendon healing despite engraftment and homing to niches within the synovium. Stem Cell Res Ther. 2018;9(1):169. doi: 10.1186/s13287-018-0900-7m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gulotta LV, Kovacevic D, Ehteshami JR, Dagher E, Packer JD, Rodeo SA. Application of bone marrow-derived mesenchymal stem cells in a rotator cuff repair model. Am J Sports Med. 2009;37(11):2126–2133. doi: 10.1177/0363546509339582. [DOI] [PubMed] [Google Scholar]
- 11.Govoni M, Berardi AC, Muscari C, Campardelli R, Bonafè F, Guarnieri C, et al. An engineered multiphase three-dimensional microenvironment to ensure the controlled delivery of cyclic strain and human growth differentiation factor 5 for the tenogenic commitment of human bone marrow mesenchymal stem cells. Tissue Eng Part A. 2017;23(15–16):811–822. doi: 10.1089/ten.TEA.2016.0407. [DOI] [PubMed] [Google Scholar]
- 12.Yan Z, Yin H, Nerlich M, Pfeifer CG, Docheva D. Boosting tendon repair: interplay of cells, growth factors and scaffold-free and gel-based carriers. J Exp Orthop. 2018;5(1):1. doi: 10.1186/s40634-017-0117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaudhury S. Mesenchymal stem cell applications to tendon healing. Muscles Ligaments Tendons J. 2012;2(3):222–229. [PMC free article] [PubMed] [Google Scholar]
- 14.Oliva F, Berardi AC, Misiti S, Verga Falzacappa C, Iacone A, Maffulli N. Thyroid hormones enhance growth and counteract apoptosis in human tenocytes isolated from rotator cuff tendons. Cell Death Dis. 2013;4:e705. doi: 10.1038/cddis.2013.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oliva F, Piccirilli E, Berardi AC, Tarantino U, Maffulli N. Influence of thyroid hormones on tendon homeostasis. Adv Exp Med Biol. 2016;920:133–138. doi: 10.1007/978-3-319-33943-6_12. [DOI] [PubMed] [Google Scholar]
- 16.Berardi AC, Oliva F, Berardocco M, la Rovere M, Accorsi P, Maffulli N. Thyroid hormones increase collagen I and cartilage oligomeric matrix protein (COMP) expression in vitro human tenocytes. Muscles Ligaments Tendons J. 2014;4(3):285–291. [PMC free article] [PubMed] [Google Scholar]
- 17.di Giacomo V, Berardocco M, Gallorini M, Oliva F, Colosimo A, Cataldi A, et al. Combined supplementation of ascorbic acid and thyroid hormone T3 affects tenocyte proliferation. The effect of ascorbic acid in the production of nitric oxide. Muscles Ligaments Tendons J. 2017;7(1):11–18. doi: 10.11138/mltj/2017.7.1.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson KA, Sun M, Barnum CE, Weiss SN, Huegel J, Shetye SS, et al. Decorin and biglycan are necessary for maintaining collagen fibril structure, fiber realignment, and mechanical properties of mature tendons. Matrix Biol. 2017;64:81–93. doi: 10.1016/j.matbio.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Södersten F, Hultenby K, Heinegård D, Johnston C, Ekman S. Immunolocalization of collagens (I and III) and cartilage oligomeric matrix protein in the normal and injured equine superficial digital flexor tendon. Connect Tissue Res. 2013;54(1):62–69. doi: 10.3109/03008207.2012.734879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hakimi O, Ternette N, Murphy R, Kessler BM, Carr A. A quantitative label-free analysis of the extracellular proteome of human supraspinatus tendon reveals damage to the pericellular and elastic fibre niches in torn and aged tissue. PLoS One. 2017;12(5):e0177656. doi: 10.1371/journal.pone.0177656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moraes SA, Oliveira KR, Crespo-López ME, Picanço-Diniz DL, Herculano AM. Local NO synthase inhibition produces histological and functional recovery in Achilles tendon of rats after tenotomy: tendon repair and local NOS inhibition. Cell Tissue Res. 2013;353(3):457–463. doi: 10.1007/s00441-013-1662-2. [DOI] [PubMed] [Google Scholar]
- 22.Assis HA, Elert NC, Azevedo ALBP, Braga IS, Serakides R, de Melo ON, et al. Dose-dependent effect of triiodothyronine on the chondrogenic differentiation of mesenchymal stem cells from the bone marrow of female rats. J Pharm Pharmacol. 2018;70(1):89–100. doi: 10.1111/jphp.12842. [DOI] [PubMed] [Google Scholar]
- 23.Boeloni JN, Ocarino NM, Melo AB, Silva JF, Castanheira P, Goes AM, et al. Dose-dependent effects of triiodothyronine on the osteogenic differentiation of rat bone marrow mesenchymal stem cells. Horm Res. 2009;72(2):88–97. doi: 10.1159/000232161. [DOI] [PubMed] [Google Scholar]
- 24.Shi ST, Wu XX, Hao W, Wang X, Miao HT, Zhen L, et al. Triiodo-L-thyronine promotes the maturation of cardiomyocytes derived from rat bone marrow mesenchymal stem cells. J Cardiovasc Pharmacol. 2016;67(5):388–393. doi: 10.1097/FJC.0000000000000363. [DOI] [PubMed] [Google Scholar]
- 25.Akhoundzadeh K, Vakili A, Sameni HR, Vafaei AA, Rashidy-Pour A, Safari M, et al. Effects of the combined treatment of bone marrow stromal cells with mild exercise and thyroid hormone on brain damage and apoptosis in a mouse focal cerebral ischemia model. Metab Brain Dis. 2017;32(4):1267–1277. doi: 10.1007/s11011-017-0034-0. [DOI] [PubMed] [Google Scholar]
- 26.Lennon DP, Haynesworth SE, Young RG, Dennis JE, Caplan AI. A chemically defined medium supports in vitro proliferation and maintains the osteochondral potential of rat marrow-derived mesenchymal stem cells. Exp Cell Res. 1995;219(1):211–222. doi: 10.1006/excr.1995.1221. [DOI] [PubMed] [Google Scholar]
- 27.Zhang T, Lee YW, Rui YF, Cheng TY, Jiang XH, Li G. Bone marrow-derived mesenchymal stem cells promote growth and angiogenesis of breast and prostate tumors. Stem Cell Res Ther. 2013;4(3):70. doi: 10.1186/scrt221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen X, McClurg A, Zhou GQ, McCaigue M, Armstrong MA, Li G. Chondrogenic differentiation alters the immunosuppressive property of bone marrow-derived mesenchymal stem cells, and the effect is partially due to the upregulated expression of B7 molecules. Stem Cells. 2007;25(2):364–370. doi: 10.1634/stemcells.2006-0268. [DOI] [PubMed] [Google Scholar]
- 29.Schramme M, Hunter S, Campbell N, Blikslager A, Smith R. A surgical tendonitis model in horses: technique, clinical, ultrasonographic and histological characterisation. Vet Comp Orthop Traumatol. 2010;23(4):231–239. doi: 10.3415/VCOT-09-10-0106. [DOI] [PubMed] [Google Scholar]
- 30.Soslowsky LJ, Carpenter JE, DeBano CM, Banerji I, Moalli MR. Development and use of an animal model for investigations on rotator cuff disease. J Shoulder Elb Surg. 1996;5(5):383–392. doi: 10.1016/S1058-2746(96)80070-X. [DOI] [PubMed] [Google Scholar]
- 31.Cook JL, Feller JA, Bonar SF, Khan KM. Abnormal tenocyte morphology is more prevalent than collagen disruption in asymptomatic athletes’ patellar tendons. J Orthop Res. 2004;22(2):334–338. doi: 10.1016/j.orthres.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Svensson M, Kartus J, Christensen LR, Movin T, Papadogiannakis N, Karlsson J. A long-term serial histological evaluation of the patellar tendon in humans after harvesting its central third. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):398–404. doi: 10.1007/s00167-004-0590-9. [DOI] [PubMed] [Google Scholar]
- 33.Sandri M, Filardo G, Kon E, Panseri S, Montesi M, Iafisco M, et al. Fabrication and pilot in vivo study of a collagen-BDDGE-elastin core-shell scaffold for tendon regeneration. Front Bioeng Biotechnol. 2016;4:52. doi: 10.3389/fbioe.2016.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Majewski M, Ochsner PE, Liu F, Flückiger R, Evans CH. Accelerated healing of the rat Achilles tendon in response to autologous conditioned serum. Am J Sports Med. 2009;37(11):2117–2125. doi: 10.1177/0363546509348047. [DOI] [PubMed] [Google Scholar]
- 35.Javazon EH, Colter DC, Schwarz EJ, Prockop DJ. Rat marrow stromal cells are more sensitive to plating density and expand more rapidly from single-cell-derived colonies than human marrow stromal cells. Stem Cells. 2001;19(3):219–225. doi: 10.1634/stemcells.19-3-219. [DOI] [PubMed] [Google Scholar]
- 36.Docheva D, Müller SA, Majewski M, Evans CH. Biologics for tendon repair. Adv Drug Deliv Rev. 2015;84:222–239. doi: 10.1016/j.addr.2014.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.D’Aniello C, Cermola F, Patriarca EJ, Minchiotti G. Vitamin C in stem cell biology: impact on extracellular matrix homeostasis and epigenetics. Stem Cells Int. 2017:8936156. 10.1155/2017/8936156. [DOI] [PMC free article] [PubMed]
- 38.Shaw G, Lee-Barthel A, Ross ML, Wang B, Baar K. Vitamin C-enriched gelatin supplementation before intermittent activity augments collagen synthesis. Am J Clin Nutr. 2017;105(1):136–143. doi: 10.3945/ajcn.116.138594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kang KK, Lee EJ, Kim YD, Chung MJ, Kim JY, Kim SY, et al. Vitamin C improves therapeutic effects of adipose-derived stem cell transplantation in mouse tendonitis model. In Vivo. 2017;31(3):343–348. doi: 10.21873/invivo.11065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oliva F, Berardi AC, Misiti S, Maffulli N. Thyroid hormones and tendon: current views and future perspectives. Muscles Ligaments Tendons J. 2013;3(3):201. [PMC free article] [PubMed] [Google Scholar]
- 41.Oliva F, Piccirilli E, Berardi AC, Frizziero A, Tarantino U, Maffulli N. Hormones and tendinopathies: the current evidence. Br Med Bull. 2016;117(1):39–58. doi: 10.1093/bmb/ldv054. [DOI] [PubMed] [Google Scholar]
- 42.Salvatore D. Deiodinases and stem cells: an intimate relationship. J Endocrinol Investig. 2018;41(1):59–66. doi: 10.1007/s40618-017-0737-4. [DOI] [PubMed] [Google Scholar]
- 43.Chong AK, Ang AD, Goh JC, Hui JH, Lim AY, Lee EH, et al. Bone marrow-derived mesenchymal stem cells influence early tendon-healing in a rabbit Achilles tendon model. J Bone Joint Surg Am. 2007;89(1):74–81. doi: 10.2106/JBJS.E.01396. [DOI] [PubMed] [Google Scholar]
- 44.Lui PP, Wong OT, Lee YW. Transplantation of tendon-derived stem cells pre-treated with connective tissue growth factor and ascorbic acid in vitro promoted better tendon repair in a patellar tendon window injury rat model. Cytotherapy. 2016;18(1):99–112. doi: 10.1016/j.jcyt.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 45.Schneider M, Angele P, Järvinen TAH, Docheva D. Rescue plan for Achilles: therapeutics steering the fate and functions of stem cells in tendon wound healing. Adv Drug Deliv Rev. 2017. 10.1016/j.addr.2017.12.016. [DOI] [PubMed]
- 46.Durant TJ, Dyment N, McCarthy MB, Cote MP, Arciero RA, Mazzocca AD, et al. Mesenchymal stem cell response to growth factor treatment and low oxygen tension in 3-dimensional construct environment. Muscles Ligaments Tendons J. 2014;4(1):46–51. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.