Abstract
Background
The World Health organization (WHO) recommends that children engage in 60 min daily moderate-to-vigorous physical activity (dMVPA). Just half of children in the UK achieve these levels (with similarly low levels in other high-income countries). Thus, the dMVPA target is a focus of national obesity strategies. However, the potential impact of increased physical activity on prevalence and inequalities in childhood overweight is unknown. Using objective data from the Millennium Cohort Study (∼18 000 children born 2000–02) we simulated a series of hypothetical physical activity intervention scenarios: achievement of the target, and more realistic increases demonstrated in trials.
Methods
Predicted probabilities of overweight and obesity (using measured heights and weights at age 11) were estimated in multinomial marginal structural models, adjusting for dMVPA (measured with accelerometers at age 7) and confounding. Inequalities were assessed according to household income quintiles [risk ratios (RRs) and risk differences (RDs)]. Intervention scenarios were simulated by re-estimating predicted probabilities of overweight/obesity after manipulating (increasing) dMVPA by varying amounts, for different eligibility criteria and with varying uptake. Analyses included 6493 children with accelerometer data. Survey weights and multiple imputation addressed sampling design, attrition and item missingness.
Results
In all, 27% children were overweight/obese, with relative and absolute inequalities in the expected direction; 51% children were achieving 60 min dMVPA, with those from the lowest income quintile achieving, on average, 3 min more dMVPA than those from the highest income quintile. A simulation of universal achievement of the dMVPA target reduced the prevalence of overweight/obesity to 22%, but increased relative inequalities (absolute inequalities were unchanged). Smaller increases in dMVPA (informed by intervention evidence) did little to reduce prevalence or inequalities, even when targeting high-risk groups.
Conclusions
Universal achievement of the WHO dMVPA target, if attainable, would reduce prevalence of childhood overweight and obesity but not inequalities. Scale-up of more realistic interventions would have limited impact.
Keywords: Health inequalities, childhood overweight, physical activity, policy, mediation, cohort
Key Messages
Childhood overweight is one of the greatest public health challenges of the 21st century and it most affects those from less advantaged backgrounds.
Just half of children in the UK meet the WHO recommendation to participate in at least 60 min moderate-to-vigorous physical activity daily (with similarly low levels in many other high-income countries).
Objective data from a contemporary UK-representative cohort were used to simulate the potential impacts of meeting the WHO target and of more realistic increases in physical activity demonstrated in trials, as if scaled up under varying levels of eligibility and uptake.
Findings indicate that, if achievable, meeting the WHO target would reduce the current UK prevalence of childhood overweight (∼27%) to Swedish levels (∼22%), but would not alter inequalities (due to a weak reverse socioeconomic gradient in physical activity).
Scale-up of interventions found to be effective in trials is unlikely to substantially reduce either prevalence or inequalities, even when targeted at high-risk groups, including those living in deprived neighbourhoods
Introduction
One in five children in the UK are overweight (including obese) by the time they start school, rising to one in three by age 11 years,1 with similarly high rates in other high-income countries2 and across the globe.3 Childhood overweight carries a higher risk of poor mental well-being, premature onset of chronic illness and a shortened life expectancy,4–6 and children living in less advantaged socioeconomic circumstances are at greater risk of overweight than their more advantaged peers.7 Reducing the prevalence of childhood overweight, and the unfair burden in less advantaged groups, is therefore a government priority in the UK,8,9 Europe10 and globally.11 One potential strategy for the prevention or reduction of overweight is to increase physical activity levels, which are generally low in the UK (only half of 7-year-olds partake in 60 min of daily moderate-to-vigorous activity (dMVPA)).12 Trials have demonstrated that physical activity can be increased in children and young people (with small to medium effect sizes13–16) via a number of strategies (from positive behavioural reinforcement and role modelling to the provision of information, structured activities or equipment)17 and in a range of settings (communities, schools and families). As such, increasing physical activity levels features highly on policy agendas, at both international18 and national8,19–21 levels, with the goal [set by the World Health Organization (WHO)] that every child achieve 60 min dMVPA.18 The UK’s 2016 Obesity Action Plan,8 and its 2018 instalment ‘Chapter 2’,9 adopted the WHO target and suggested that half these minutes might be delivered in school settings.
The extent to which efforts to increase physical activity in childhood (including achievement of the dMVPA target) might alter prevalence and inequalities in overweight is contingent upon several factors. First is effectiveness, that is by how much an intervention can increase physical activity. Also crucial is whether some socioeconomic groups experience greater increases in physical activity after the intervention than others (differential effectiveness), the proportion of eligible participants who enrol in the intervention (uptake) and whether this varies between socioeconomic groups (differential uptake). Additionally, when interventions are implemented at scale, policy makers must make choices around eligibility, with the view to maximizing public benefit in a context of constrained resources and giving due regard to access and the equality of any benefits.22 Eligibility options may be universal (the intervention is offered to everyone), targeted (only those at increased risk are eligible) or indicated (the intervention is offered to individuals already affected by the condition of interest).23 Proportionate universalism, which offers some services to all groups and additional (often more intensive and tailored) services to those more in need, is increasingly advocated for inequality reduction.24 The potential population-level impacts of rolling policies out under different scenarios of eligibility, uptake and effectiveness cannot be examined in trial settings. However, multiple policy options can be explored through simulations in observational data, informed (where possible) by intervention evidence.
The aim of this paper was to examine how population-level interventions to increase physical activity in mid childhood might reduce prevalence and inequalities in childhood overweight and obesity (separately). A number of policy scenarios were simulated, ranging from universal achievement of the physical activity target (60 min dMVPA) to more conservative and realistic increases in physical activity typically shown in intervention evidence. Simulations were carried out using nationally representative, contemporary data from the UK Millennium Cohort Study (MCS), which holds objective measures of dMVPA and body mass index (BMI) for more than 6000 children born at the turn of the century.
Methods
Study characteristics
The Millennium Cohort Study (MCS) is a longitudinal study of children born in the UK between September 2000 and January 2002.25 Families were selected through Child Benefit Records, and initially contacted via opt-out letters from the Department for Work and Pensions. A disproportionately stratified clustered sampling design was used to over-represent children living in Wales, Scotland and Northern Ireland, disadvantaged areas and, in the case of England, areas with high proportions of ethnic minority groups.26 The first study contact with the cohort child was carried out at around age 9 months. Interviews were carried out by trained interviewers in the home with the main respondent (usually the mother). Information was collected from 18 818 infants (of which 18 296 were singletons). We use data from the initial survey and those carried out subsequently at ages 3 (n = 15 381), 5 (n = 15 041), 7 (n =13 681) and 11 years (n =13 112). Data were downloaded from the UK Data Service, University of Essex and University of Manchester in April 2014, and the physical activity data were downloaded from the same source in August 2016. Ethics approval was granted for each of the main MCS surveys27 and for the accelerometer data collection28; no approval was required for the present analysis.
Measures
Outcome: overweight and obesity
At age 11, children were weighed without shoes or outdoor clothing by trained interviewers using Tanita HD-305 scales (Tanita UK Ltd, Middlesex, UK). Weights were recorded in kilograms to one decimal place. Heights were measured with the Leicester Height Measure Stadiometer (Seca Ltd, Birmingham, UK) and recorded to the nearest millimetre. International Obesity Task Force (IOTF) age- and sex-specific cut-offs for BMI were used to classify children as thin/healthy weight, overweight or obese.29
Exposure: socioeconomic circumstances (SECs)
Socioeconomic inequalities in overweight/obesity were measured according to quintile of equivalized household income, reported at age 5 years.
Mediator: physical activity
Physical activity was measured when the MCS children were aged 7, for 7 consecutive days, using the Actigraph GT1M accelerometer (Actigraph, Pensacola, FL), which has been demonstrated to reliably measure children’s physical activity. Accelerometers were programmed to use a 15-s sampling epoch and to record activity as counts and steps. Daily moderate-to-vigorous physical activity (dMVPA) was defined as >2241 counts per min (cpm), and sedentary behaviour as <100 cpm. Time spent in dMVPA and sedentary activity was standardized to account for total valid wear time. Further information on data collection, cleaning and variable creation is reported elsewhere.28 The dMVPA variable was not normally distributed, therefore medians are reported in descriptive analyses and a Box–Cox transformed measure ( = 0.34) was used in the regression models.30 The appropriateness of the assumed linear association between dMVPA and the probability of being overweight or obese was confirmed using locally weighted scatterplot smoothers and testing for quadratic terms.
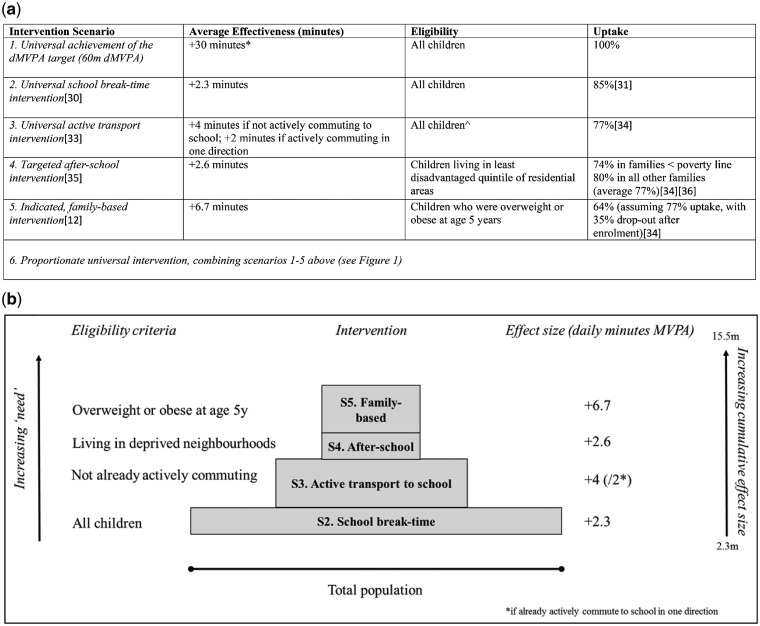
The observed dMVPA variable was manipulated to represent increases in dMVPA which might be achieved through a series of hypothetical interventions. Choice of interventions was informed by: the international dMVPA target; content of the UK childhood obesity action plan8,9 (which emphasised the role of schools); existing meta-analyses and reviews of physical activity interventions that have been trialled in mid childhood in high-income countries; the views of policy experts; and discussions with a parents’ and carers’ advisory group. These scenarios are described in Figure 1, with greater detail provided in Supplement 1, available as Supplementary data at IJE online.
Figure 1.
(a) Key characteristics of the six intervention scenarios. *average effectiveness required to shift proportion of children achieving 60 min dMVPA to 95%. ^All children were eligible for the active transport intervention, although they could only benefit if not already actively commuting to school. (b) Visual representation of a proportionate universal physical activity intervention (Scenario 6).
Confounding
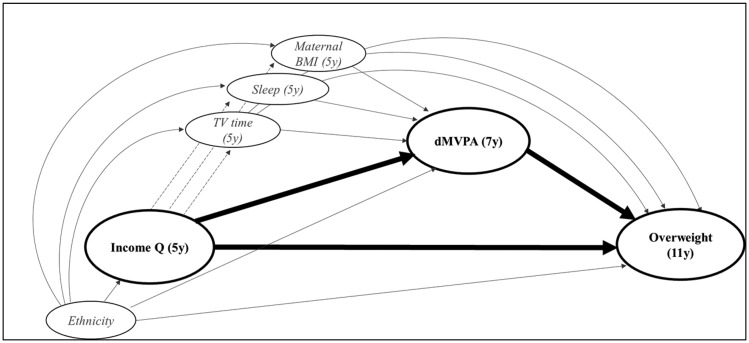
We adjusted for the following factors which were identified as potential confounders, as guided by a directed acyclic graph (Figure 2). Child’s ethnicity (White, Mixed, Pakistani or Bangladeshi, Indian, Black or Black British, Other) was considered a potential baseline confounder, as it may influence both socioeconomic circumstances and overweight/obesity. Three potential intermediate confounders of the relationship between physical activity and overweight/obesity were accounted for (all reported by the main respondent): maternal BMI when the child was 5 years old (as a proxy for family diet); whether the child had a regular bedtime at age 5 years (always, usually, sometimes, never or almost never); and the number of hours spent by the child watching television (TV) daily at age 7 years (<1 h, 1–3 h, 3+ h). For maternal BMI and bedtime routines, information reported at 3 years (y) was used if missing at 5 y.
Figure 2.
Directed acyclic graph to demonstrate association between socioeconomic circumstances (SECs), daily moderate to vigorous physical activity (dMVPA) and overweight and obesity (BMI status).
Variables representing eligibility: whether usual mode of travel to and from school was active (walking/cycling), according to main respondent report at 7 y (Scenario 3); high area deprivation (highest quintile of the Index of Multiple Deprivation, based on main residence at age 7 y) (Scenario 4); and overweight/obese at age 5 y (Scenario 5).
Variable used to simulate differential uptake: income poverty (using the Organization for Economic Co-operation and Development definition: <60% UK median income) at age 7 was used to assign differential uptake (Scenario 4).
Sex: There was little evidence that inequalities in overweight (RR: 0.98, P = 0.774) and obesity (Relative Risk Ratio (RRR): 0.84, P = 0.112) varied in girls compared with boys. The association between dMVPA and overweight did not vary by sex (RRR: 1.02, P = 0.928), although the negative association between dMVPA and obesity was half as strong for girls as for boys (RRR: 2.19, P = 0.023). Inclusion of a sex interaction made no difference to overall conclusions, so the results are presented for boys and girls combined.
Analysis
Descriptive statistics (percentages, means, medians, with chi-square and t tests) were used in exploratory analyses of the association between SECs, dMVPA, overweight and obesity.
The association between SECs and BMI status was estimated using multinomial regression in marginal structural models (MSM), with healthy weight as the reference group. Baseline confounding was accounted for using inverse probability treatment weights (IPTW).31 Probabilities (and 95% confidence intervals) obtained from the regression model were used to estimate prevalence of healthy weight, overweight and obesity, overall and in each income quintile. Summary measures of relative and absolute inequalities were then estimated by repeating regression models with income quintile as a continuous term (thus fitting a linear socioeconomic gradient). Relative inequalities are given by the ratio of the fitted probabilities of overweight and obesity between the highest and lowest income quintiles [risk ratio (RR); 95% confidence interval (CI)], and absolute inequalities are given by the difference between the fitted probabilities between the highest and lowest income quintiles [risk difference (RD) and 95% CI]. This provided an estimate of the total direct effect (TDE) of SECs on overweight/obesity.
Next, dMVPA was entered into the marginal structural model as a continuous variable, this time accounting for baseline and intermediate confounding with IPTWs. The probabilities from the adjusted model provide the controlled direct effect (CDE) of SECs on overweight/obesity—that is, the estimated effect of SECs on overweight/obesity when dMVPA was fixed at observed levels (referred to as the ‘observed’ CDE).
The intervention scenarios were then simulated by re-estimating the predicted probabilities of overweight and obesity after modifying the dMVPA variable. This provided a series of ‘simulated’ CDEs (representing the expected effect of SECs on overweight and obesity, when dMVPA was fixed at the new, hypothetical levels under each scenario). To simulate effectiveness, an increase in dMVPA was applied to the observed dMVPA variable. For example, in Scenario 5 (indicated family-based intervention), an average increase of 6.7 min was applied to the dMVPA variable. This increase was only assigned to children who were eligible for the given intervention (in Scenario 5 this was children who were overweight/obese at age 5). In the scenarios where uptake was <100%, an increase in dMVPA was only applied to a proportion of eligible children (e.g. in Scenario 5, the average 6.7 min-increase in dMVPA was only applied to 64% of children who were overweight/obese at age 5). Further details on computation are provided in Supplement 2, available as Supplementary data at IJE online. Even in the absence of a mediating effect of dMVPA in the association between SECs and overweight/obesity, simulations of targeted or indicated physical activity interventions might still have the potential to reduce inequalities, through producing greater increases in physical activity in less advantaged groups.
There was no evidence for an interaction between SECs and dMVPA (RRR: 0.98, P = 0.819 for overweight, RRR: 1.18, P = 0.122 for obesity). IPTWs were trimmed at the 1st and 99th centiles to remove the excessive influence of extreme values on the results, and multiplied by an MCS weight capturing survey design, attrition up to the age 7 sweep and inclusion in the physical activity study [mean 0.98 (range: 0.30–1.6); see Supplement 3, available as Supplementary data at IJE online]. Analyses were performed in Stata SE 13.1 (Stata Corporation, TX, USA).
Working sample
Of the original cohort, 72% took part in the MCS age 7 survey and all were invited to take part in the accelerometer study; 12 768 singleton children (93%) consented to take part and 9772 (71%) returned the accelerometers. Of these, two-thirds (6497) had data registered for ≥10 h on at least 2 out of the 7 days (a period shown to produce reliable estimates of physical activity32). Of these children, 1467 were missing data on one or more of the confounding or outcome variables; to deal with missing data, we used multiple imputation by chained equations in 20 datasets for 1463 children (who had sufficient auxiliary information), giving an analytical sample size of 6493. Imputation was carried out under a missing at random assumption. Further detail of the imputation model is provided in Supplement 4, available as Supplementary data at IJE online.
Sensitivity analyses
We repeated the main analyses using an alternative measure of SECs [maternal education, dichotomized as ‘low’ (<GCSEs A*-C) and ‘higher’ (GCSEs A*-C and above)] and adiposity [body fat mass, established using Tanita BF-522W scales (Tanita UK Ltd, Middlesex, UK), classified as normal, overfat or obese, with age- and sex-specific cut-offs33]. We also repeated models adjusting for an earlier measure of BMI status (at age 5) as an intermediate confounder, in order to account for potential reverse causality between dMVPA and BMI.
Finally, we modelled a more realistic variation of Scenario 1 (Scenario 1b) whereby dMVPA was only increased in children who were achieving less than 60 min dMVPA, to 60 min [standard deviation (SD): 5].
Results
Sample characteristics
Table 1 presents characteristics of those with accelerometer data (column A), those with complete data on all variables of interest (column B), those in the main analytical (imputed) sample (column C) and the original MCS sample (column D). In general, characteristics were consistent across samples. In the main analytical sample, 22% children were overweight and 6.0% obese, median dMVPA was 61 min and 51% of children met the WHO dMVPA target.
Table 1.
Characteristics of the MCS across analytical samples
| Weighted % (observed n) unless indicated otherwise |
||||
|---|---|---|---|---|
| A. All children with accelerometer data (n = 6497) | B. Complete case (n=5615) | C. Analytical (imputed) sample (with M = 20) (n = 6493) | D. Original MCS sample (n = 18 981) | |
| Income quintile (measured at age 5 years) | ||||
| Highest (1) | 19 (1433) | 20 (1329) | 19 | 20 (2614) |
| 2 | 19 (1434) | 19 (1292) | 19 | 20 (2855) |
| 3 | 21 (1353) | 21 (1212) | 21 | 20 (2908) |
| 4 | 20 (1154) | 20 (996) | 20 | 20 (3209) |
| Lowest (5) | 21 (927) | 20 (786) | 22 | 20 (3346) |
| Not present at relevant sweep | n/a | n/a | n/a | 3940 |
| Item missing | 196 | n/a | n/a | 109 |
| Sex | ||||
| Male | 51 (3176) | 51 (2739) | 51 | 51 (9775) |
| Female | 49 (3321) | 49 (2876) | 49 | 49 (9206) |
| Not present at relevant sweep | n/a | n/a | n/a | n/a |
| Item missing | 0 | n/a | n/a | 0 |
| Baseline confounding (reported at age 9 months) | ||||
| Ethnicity | ||||
| White | 87 (5788) | 88 (5062) | 88 | 89 (15 730) |
| Mixed | 0·8 (41) | 0·8 (34) | 0·7 | 9·4 (195) |
| Indian | 2·0 (146) | 2·0 (124) | 1·9 | 1·9 (503) |
| Pakistani/Bangladeshi | 5·3 (253) | 4·7 (191) | 4·9 | 3·9 (1323) |
| Black or Black British | 3·2 (161) | 2·7 (124) | 2·9 | 2·7 (721) |
| Other | 1·6 (96) | 1·4 (80) | 1·4 | 1·6 (370) |
| Not present at relevant sweep | n/a | n/a | n/a | n/a |
| Item missing | 12 | n/a | n/a | 139 |
| Intermediate confounding (reported at age 5 years) | ||||
| Maternal BMI (mean, SE) | 25 (0·11) | 25 (0·11) | 25 (0·11) | 25 (0·07) |
| Not present at relevant sweep | n/a | n/a | n/a | 3940 |
| Item missing | 201 | n/a | n/a | 2518 |
| Regular bedtime? | ||||
| Never or almost never | 4·4 (243) | 3·8 (187) | 4·4 | 4·8 (760) |
| Sometimes | 5·2 (295) | 4·8 (240) | 5·2 | 5·1 (860) |
| Usually | 26 (1773) | 26 (1550) | 25·9 | 27 (4125) |
| Always | 65 (4137) | 65 (3638) | 64·5 | 63 (9227) |
| Not present at relevant sweep | n/a | n/a | n/a | 3940 |
| Item missing | 49 | n/a | n/a | 69 |
| Screen time daily | ||||
| < 1 h | 19 (1337) | 19 (1184) | 19 | 20 (2684) |
| 1-3 h | 65 (4205) | 65 (3647) | 65 | 65 (8748) |
| 3+ h | 16 (948) | 16 (784) | 16 | 15 (2173) |
| Not present at relevant sweep | n/a | n/a | n/a | 3940 |
| Item missing | 7 | n/a | n/a | 1436 |
| Physical activity (measured at age 7) | ||||
| dMVPA (median, SE) | 61 (0·42) | 61 (0·44) | 61 (0·42) | 61 (0·42) |
| Achieving 60 mins per day | 51 (3119) | 49 (2725) | 51 | 51 (3182) |
| Not present at relevant sweep | n/a | n/a | n/a | 5300 |
| Item missing | n/a | n/a | n/a | 7184 |
| BMI status (measured at age 11) | ||||
| Healthy | 74 (4543) | 74 (4305) | 73 | 71 (8319) |
| Overweight | 21 (1125) | 21 (1064) | 21 | 22 (2639) |
| Obese | 5·6 (270) | 5·4 (246) | 6·0 | 6·7 (806) |
| Not present at relevant sweep | n/a | n/a | n/a | 5869 |
| Item missing | 559 | n/a | n/a | 1348 |
| Variables for targeting interventions (reported at age 7 years) | ||||
| Area deprivation | ||||
| Most deprived quintile | 21 (1243) | 19 (998) | 22 | 22 (3573) |
| Not present at relevant sweep | n/a | n/a | n/a | 5300 |
| Item missing | 1 | 1 | n/a | 2 |
| Active travel to and from school | ||||
| No | 45 (3012) | 46 (2822) | 45 | 45 (6675) |
| One way | 3·4 (233) | 3·5 (206) | 3·4 | 3·4 (485) |
| Both ways | 52 (3012) | 51 (2580) | 52 | 52 (6432) |
| Not present at relevant sweep | n/a | n/a | n/a | 5300 |
| Item missing | 16 | 7 | n/a | 98 |
Column A, B: to account for sample design and inclusion in the physical activity (PA) study; column C: to account for sample design and inclusion in the PA study (since PA data were not imputed); column D: to account for sample design and attrition to relevant sweep.
PA, physical activity; dMVPA, moderate-to-vigorous physical activity; SE, standard error; M, number of imputed subsamples.
Descriptive analyses
There was a weak reverse socioeconomic gradient in dMVPA: children from the highest income quintile had the lowest levels of dMVPA [median 59, standard error (SE): 0·75], reaching 62 (SE: 1·2) in the lowest income quintile (Supplementary Table S2, Supplement 5, available as Supplementary data at IJE online). Median minutes spent in dMVPA at age 7 were lower in children who were overweight (58, 1.09) or obese (53, 1.9) than those who were healthy weight (62, 0.52).
All potential confounding variables were associated with SECs, BMI status and dMVPA (Supplementary Table S3, Supplement 5, available as Supplementary data at IJE online).
Relative and absolute inequalities were observed in both overweight and obesity (Table 2). The observed CDE, adjusting for dMVPA and intermediate confounding, was almost identical to the TDE, indicating that the association between SECs and overweight and obesity was largely unmediated by dMVPA (Table 2). This was expected, due to the weak, reverse socioeconomic gradient in dMVPA shown in Supplementary Table S2, available as Supplementary data at IJE online. Given this, a universal physical activity intervention might reduce overall prevalence but would not be expected to change inequalities in overweight and obesity. However, interventions targeting low SEC families or those considered to be at higher risk might still alter inequalities if the intervention is accessible and effective for its intended recipients.
Table 2.
Observed and adjusted analyses: prevalence of healthy weight, overweight and obesity; and relative and absolute inequalities
| Prevalence of healthy weight, overweight, obesity: overall and according to quintiles of household income |
Inequalities in healthy weight, overweight, obesity |
|||||||
|---|---|---|---|---|---|---|---|---|
| Overall | 1 (highest) | 2 | 3 | 4 | 5 (lowest) | Risk ratio | Risk difference | |
| A: Unadjusteda: | ||||||||
| Healthy | 73.0% | 80.4% | 75.7% | 71.8% | 71.3% | 67.1% | – | – |
| Overweight | 21.1% | 17.0% | 19.1% | 22.7% | 20.7% | 25.3% | 1·4 (1·1, 1·7) | 7·3% (3.2, 11·4) |
| Obese | 5.9% | 2·7% | 5·3% | 5·5% | 8.0% | 7·7% | 2·4 (1·5, 3·4) | 5.0% (2·6, 7·5) |
| B. Total direct effecta,b | ||||||||
| Healthy | 73.0% | 80.5% | 75.7% | 72.0% | 71.1% | 67.0% | – | – |
| Overweight | 21.2% | 16.9% | 19.1% | 22.7% | 20.9% | 25.4% | 1.4 (1.1, 1.7) | 6.7% (2.5, 10.9) |
| Obese | 5.9% | 2.6% | 5.2% | 5.3% | 8.0% | 7.6% | 2.2 (1.3, 3.2) | 4.6% (2.0, 7.1) |
| C: Controlled direct effecta,b,c,d | ||||||||
| Healthy | 73.0% | 80.1% | 75.5% | 72.1% | 71.7% | 67.4% | – | – |
| Overweight | 21.2% | 17.2% | 19.1% | 22.6% | 20.7% | 25.3% | 1·4 (1·1, 1·7) | 7·1% (2·8, 11·3) |
| Obese | 5·8% | 2·7% | 5·4% | 5·4% | 7·7% | 7·4% | 2·2 (1·3, 3·2) | 4·6% (2·1, 7·1) |
The total direct effect gives the effect of SECs on overweight after adjustment for baseline confounding. The controlled direct effect gives the effect of SECs on overweight observed when dMVPA is held at the observed level. Degree of mediation is inferred by attenuation in the coefficient of SECs between the total and controlled direct effects.
Weighted to account for sample design and attrition.
Adjusting for mother’s ethnicity (using inverse probability treatment weights).
Adjusting for maternal BMI at age 5, bedtime routines, TV time (using inverse probability treatment weights).
Adjusting for dMVPA.
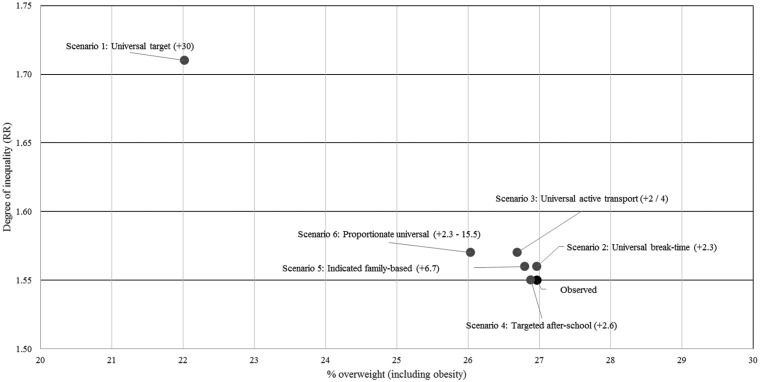
Intervention scenarios
Table 3 presents, for the simulated CDEs (Scenarios 1–6): the proportion of children who would meet the dMVPA target; prevalence of overweight and obesity (overall and according to income quintile); and relative and absolute inequalities in overweight and obesity. Figures from the observed (CDE) model are repeated at the top of Table 3 to allow comparison with each scenario. Figure 3 provides a visual representation of the prevalence of overweight including obesity (x-axis) and relative inequalities (y-axis) for each scenario and the observed CDE.
Table 3.
Intervention scenarios 1–6: proportion meeting WHO dMVPA target, prevalence of overweight and obesity, relative and absolute inequalities
| % achieving 60 min dMVPAd |
Prevalence of healthy weight, overweight, obesity, overall and according to income quintilea |
Inequalities in overweight, obesitya |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | 1 (highest) | 2 | 3 | 4 | 5 (lowest) | Risk ratio | Risk difference | ||
| Observed controlled direct effect | |||||||||
| 51·0% | Healthy | 73.0% | 80.1% | 75.5% | 72.1% | 71.7% | 67.4% | – | – |
| Overweight | 21.2% | 17.2% | 19.1% | 22.6% | 20.7% | 25.3% | 1·4 (1·1, 1·7) | 7·1% (2·9, 11·3) | |
| Obese | 5.8% | 2·7% | 5·4% | 5·4% | 7.7% | 7·4% | 2·3 (1·3, 3·3) | 4·6% (2·1, 7·1) | |
| Simulated controlled direct effect, Scenario 1: achievement of 60 min dMVPA target (+30m dMVPA for every child), with 100% uptake | |||||||||
| 96·1% | Healthy | 77.9% | 83.8% | 80.2% | 77.1% | 77.0% | 72.9% | – | – |
| Overweight | 18.2% | 14.4% | 16.3% | 19.4% | 17.9% | 22.1% | 1·5 (1·2, 1·9) | 7·7% (3·4, 11·9) | |
| Obese | 3·9% | 1·7% | 3·6% | 3·6% | 5·2% | 5·0% | 2·9 (1·3, 4·4) | 3·3% (1·2, 5·3) | |
| Simulated controlled direct effect, Scenario 2: universal break-time intervention (+2·3 dMVPA), with 85% uptake | |||||||||
| 54·7% | Healthy | 73.4% | 80.4% | 75.9% | 72.5% | 72.1% | 67.8% | – | – |
| Overweight | 21.0% | 17.0% | 18.9% | 22.3% | 20.5% | 25.0% | 1·4 (1·1, 1·7) | 7·1% (2·9, 11·3) | |
| Obese | 5·6% | 2·6% | 5·2% | 5·2% | 7·4% | 7·1% | 2·3 (1·3, 3·3) | 4·5% (2·0, 6·9) | |
| Simulated controlled direct effect, Scenario 3: active transportation (+4 /+2 m dMVPAb), with 77% uptake if not already actively commuting | |||||||||
| 54·2% | Healthy | 73.3% | 80.4% | 75.8% | 72.4% | 72.0% | 67.6% | – | |
| Overweight | 21.0% | 17.0% | 18.9% | 22.4% | 20.5% | 25.2% | 1·4 (1·2, 1·7) | 7·2% (3, 11·4) | |
| Obese | 5·7% | 2·6% | 5·3% | 5·2% | 7·5% | 7·2% | 2·3 (1·3, 3·3) | 4·6% (2·1, 7·0) | |
| Simulated controlled direct effect, Scenario 4: targeted after-school intervention (+2·6m dMVPA), in deprived areas, with differential uptakec | |||||||||
| 51·6% | Healthy | 73.1% | 80.1% | 75.5% | 72.1% | 71.8% | 67.6% | – | |
| Overweight | 21.1% | 17.2% | 19.1% | 22.5% | 20.6% | 25.2% | 1·4 (1·1, 1·7) | 7·0% (2·8, 11·2) | |
| Obese | 5·8% | 2·7% | 5·4% | 5·3% | 7·6% | 7·3% | 2·3 (1·3, 3·2) | 4·5% (2·0, 7·0) | |
| Simulated controlled direct effect, Scenario 5: indicated family-based intervention (+6·7m dMVPA ) in overweight/obese at 5 y, with 64% uptake | |||||||||
| 53·2% | Healthy | 73.2% | 80.2% | 75.6% | 72.3% | 71.8% | 67.6% | – | |
| Overweight | 21.1% | 17.1% | 19.0% | 22.5% | 20.6% | 25.2% | 1·4 (1·1, 1·7) | 7·1% (2·9, 11·3) | |
| Obese | 5·7% | 2·7% | 5·3% | 5·3% | 7·6% | 7·3% | 2·3 (1·3, 3·3 ) | 4·5% (2·0, 7·0) | |
| Simulated controlled direct effect, Scenario 6: proportionate universal intervention, combining scenarios 2-5 | |||||||||
| 60·2% | Healthy | 74.0 | 80.8% | 76.3% | 73.0% | 72.7% | 65% | – | |
| Overweight | 20.6% | 16.7% | 18.6% | 22.0% | 20.2% | 24.7% | 1·4 (1·1, 1·7) | 7·1% (2·9, 11·2) | |
| Obese | 5·4% | 2·5% | 5·0% | 5·0% | 7·2% | 6·9% | 2·3 (1·3, 3·3·) | 4·3% (1·9, 6·7) | |
The observed controlled direct effect gives the effect of SECs on overweight observed when dMVPA is held at the observed level. Scenarios 1–6 present the controlled direct effect of SECs on overweight which would be expected if dMVPA was increased by the amount relevant to each hypothetical scenario.
Weighted to account for sample design and attrition, and adjusted for confounding with inverse probability treatment weights.
+4 min was modelled for children who were not taking active transport in either direction and 2 min for those actively commuting in one direction only.
Modelling 74% uptake in children living in families below the poverty line and 80% in those above it.
proportion achieving 60 minutes in the observed data and after manipulation of the continuous dMVPA variable.
Figure 3.
Prevalence and relative inequalities (risk ratios, RR) in overweight (including obesity) according to intervention scenarios (minutes increase in dMVPA in parentheses).
A universal 30-min increase in dMVPA would result in 95% children achieving the dMVPA target (Scenario 1). The resultant decline in overweight and obesity was moderate: from 21% to 18% for overweight, and from 5.8% to 3.9% for obesity. As expected (given the small mediating role of physical activity, Table 2) inequalities remained similar to those observed, with a small increase in relative inequality and a decrease in absolute inequality driven by the overall drop in prevalence of overweight and obesity. Confidence intervals around the observed CDE and in Scenario 1 were wide and overlapping.
Scenarios 2–4, representing more realistic increases in dMVPA, had minimal benefits in terms of reductions in prevalence of overweight and obesity. Relative and absolute inequalities were also unchanged, even for interventions targeted at children living in deprived areas (Scenario 4) and those previously identified as being overweight or obese (Scenario 5). A proportionate universal intervention (Scenario 6) combined Scenarios 2–5 in one package. Despite the breadth of interventions included, and the greater increases in dMVPA simulated for higher-risk groups, this package resulted in only small decreases in the prevalence of overweight and obesity, and inequalities persisted. As seen in Scenario 1, confidence intervals around these estimates were relatively wide and overlapped with the confidence intervals for the observed CDE.
Sensitivity analyses
Scenario 1 b, which shifted activity levels up to a mean of 60 min (SD: 5) only in children not currently meeting the WHO target, produced a more modest decrease in overweight and obesity (to 25.2%). Relative inequalities were slightly lower [overweight: 1·4 (1·2, 1·7), obesity: 2·4 (1·4, 3·4)], whereas absolute inequalities remained similar for overweight [7.8% (3.4, 12.08)], and fell slightly for obesity [3.4% (1·2, 5.5)] (data not shown).
Analyses repeated in the complete case sample showed similar estimates to those in the main analysis (Supplement 6, available as Supplementary data at IJE online). Analyses repeated with an alternative measure of SECs (‘low’ vs ‘higher’ maternal education) produced slightly smaller inequalities (because two more heterogeneous groups were being compared) but similar changes in prevalence and inequalities in the intervention scenarios, compared with the observed results (data available on request). Finally, we repeated analyses using an alternative measure of adiposity (fat mass). The prevalences of overfat and obesity were different (with more children being classified as obese). However, the extent of change in prevalence and inequalities after modelling each of the scenarios was consistent with that observed for BMI (data available on request). Finally, we repeated models adjusting for baseline BMI status (at age 5) in order to account for reverse causation between BMI and later physical activity; findings were largely unchanged (see Supplement 7, available as Supplementary data at IJE online).
Discussion
Summary of findings
A simulation of the impact of achieving the ambitious WHO physical activity target showed a reduction in population levels of childhood overweight (including obesity) from 27% to 22%. However, more realistic scenarios, informed by effect increases in dMVPA achieved in trials and with input from policy experts and parents and carers, did not substantially alter the prevalence of overweight/obesity. Neither the universal achievement of the WHO physical activity target (Scenario 1), nor more realistic universal interventions (Scenarios 2, 3) reduced inequalities. Even interventions that targeted specific high-risk groups (Scenarios 4 and 5) or were offered as a comprehensive package of interventions, with support increasing according to need (Scenario 6), had limited impact on inequalities.
Comparison with other research
The current analysis corroborates the widely demonstrated finding that children from less advantaged backgrounds are at greater risk of overweight/obesity.34–36 Physical activity, or energy expenditure, is an accepted determinant of adiposity.37 It is therefore the focus of prevention and treatment programmes38,39 and of policies to reduce the prevalence of overweight/obesity and the greater burden in less advantaged groups.8,18 However, studies examining physical activity by socioeconomic circumstances show mixed results, potentially due to differences in the way physical activity is measured. For example, in the MCS, parents from more advantaged SECs were more likely to report that their child takes part in arranged sporting activities or activities as a family, and less likely to report sedentary behaviours such as TV viewing and personal computer (PC) time.35 In contrast, objective data in the MCS [as shown here (Supplementary Table S2, available as Supplementary data at IJE online) and elsewhere12] indicate that children from less advantaged backgrounds are no less active and no more sedentary12 than their more advantaged peers. This social patterning in measured physical activity has been reported elsewhere,40,41 with some evidence that children from less advantaged families may be more active (possibly due to lower rates of car ownership in less advantaged groups42). Reported physical activity has been found to attenuate the association between SECs and overweight/obesity in children35,43 and adults44,45; however, the conflicting socioeconomic patterns in objectively measured and reported physical activity imply that these findings may be subject to report bias or residual confounding. At the time of writing, and to our knowledge, this was the first study to examine these relationships using objectively measured physical activity data, and to simulate the potential for physical activity interventions to reduce childhood overweight/obesity and the higher burden in less advantaged social groups.
Strengths and limitations
Analyses were carried out with objective measures of physical activity and heights and weights, in a large, UK-representative and contemporary cohort. The availability of longitudinal data allowed for appropriate temporal ordering of physical activity and childhood overweight/obesity variables, during an important period in childhood (between ages 7 and 11 years, when decreases in physical activity46 and increases in overweight/obesity1 and inequalities36 occur). Comprehensive socioeconomic and demographic information allowed us to simulate interventions under a range of eligibility criteria (including children who were overweight or obese in early childhood, not actively commuting to school, or living in deprived areas). A novel application of marginal structural models, to manipulate the mediator as if altered by intervention,47 was used to simulate a series of intervention scenarios, informed by policy targets and effect sizes from trial evidence, as if rolled out at the population level and allowing for suboptimal and differential uptake. Thus, these findings address an important knowledge gap that cannot be addressed through trials.
The school setting has been emphasized in the UK government’s obesity action plan8,9 and identified as a key policy action area in the European WHO Region10 as a means of striving towards achievement of the WHO target. We therefore examined a number of a priori intervention scenarios, most of which might be rolled out nationally in schools: school break-time activities and equipment, active school commuting and after-school clubs, in addition to family-based programmes. The characteristics of these intervention scenarios (i.e. effectiveness, eligibility and uptake) were guided by trial evidence from meta-analyses and reviews. In most cases it was possible to identify interventions that had been trialled in mid childhood and in high-income countries. However, there were a number of gaps in the evidence. First, baseline physical activity levels of participants were rarely reported in the reviews, and few studies have documented effectiveness in different socioeconomic groups. Second, there is little evidence about either uptake or differential uptake of interventions, and so we modelled levels based on a priori assumptions rather than evidence. Third, few intervention studies followed study participants in the medium or long term. Fourth, although proportionate universalism has become a widely advocated approach for improving population health and reducing inequalities,24 what constitutes an appropriate mix of universal and more intensive services has not been conceptualized. We therefore modelled a hypothetical proportionate universal intervention. Finally, the most successful universal interventions are likely to be those which tackle barriers to physical activity in all aspects of children’s lives—home, family, school, communities and the physical environment.17 For targeted or indicated approaches, tailoring the content of interventions to families’ needs may increase effectiveness. It was not possible to model such policy approaches, due to a lack of trial evidence in this area. Nevertheless, Scenario 1 (universal achievement of the dMVPA target) serves to demonstrate that, even if substantially larger increases in dMVPA could be achieved (through community-wide interventions, for example), this would do little to narrow socioeconomic differences in childhood overweight/obesity.
We faced further challenges in data availability: for example, in simulating the impact of the active transport intervention we were unable to take into account distance between homes and schools or any barriers to active commuting (e.g. busy roads or lack of pavements). We examined a hypothetical proportionate universal intervention, which combined a number of interventions (Scenarios 2–5). In reality, families and children eligible for all elements of this proportionate universal package may find it hard to engage with every intervention on offer in the context of already busy lives, and so it is possible that effects would be even less positive than those shown in the present analysis. The limitations of the scenarios are addressed in greater detail in Supplement 1, available as Supplementary data at IJE online.
A limitation of these analyses relates to the ability to infer causation from observational data, which relies on there being no residual confounding. This is particularly important for the association between physical activity and BMI status. Although we were able to adjust for a range of intermediate confounding factors, many will be subject to measurement error. For example, maternal BMI was used as a proxy for household diet, and bedtime routines will not accurately reflect duration or quality of sleep. Furthermore, there will be other factors that may confound the association between physical activity and overweight/obesity that we were not able to adjust for, such as the influence of domestic routines. Although we adjusted for TV time, it was not possible to fully account for the inter-relationship between sedentary behaviour and physical activity. Increases in dMVPA achieved through intervention may replace sedentary behaviours, in which case the potential for physical activity interventions to reduce overweight/obesity and inequalities may have been underestimated. Longitudinal data available in MCS allowed us to examine the association between physical activity (at age 7 y) and later overweight/obesity (at age 11 y), while accounting for potential reverse causation from earlier BMI status (at 5 y) in a sensitivity analysis. Nevertheless it remains possible that the association between dMVPA and overweight/obesity is confounded. The association between dMVPA and BMI in the MCS was −0.02 kg/m2 (−0.02, −0.010) (and −0.01 kg/m2 (−0.01, −0.005) after adjustment]. Few physical activity interventions have evaluated the impact on increases in physical activity and BMI. However, triangulation of findings from meta-analyses that have documented average decreases in BMI (∼−0.05 kg/m2, ref Harris48) with those that have reported average increases in physical activity (∼4 min, ref Metcalf16) suggests that BMI might be expected to decrease by 0.0125 kg/m2 for every 1-min increase in dMVPA, similar to the MCS.
Like all cohort studies, the MCS is subject to sampling bias and attrition, and particularly so for intensive add-on studies such as the collection of accelerometer data. Sampling and attrition weights were used to account for the fact that less than half of the original cohort had physical activity measured28 and analyses repeated using several different samples (Table 1; Supplementary Table S3, available as Supplementary data at IJE online) indicated that the effects of any response bias were minimal. Finally, the most successful obesity interventions are those that tackle both diet and physical activity together.49,50 We were unable to model the impact of such interventions, due to the lack of reliable dietary information in the MCS.
Implications for policy and further research
The WHO recommendation that all children achieve 60 min dMVPA has been endorsed across the globe, and national targets have been set to reflect this. Our analysis indicates that if this target were to be achieved in the UK, the prevalence of childhood overweight (including obesity) would fall from around 27% to levels currently observed in Sweden (∼22%).51 This is a substantial reduction, but the dramatic and widespread increase in physical activity required may be unachievable at the population level, particularly since the capacity of schools (which are a major focus of the UK obesity action plan8,9) to contribute to this agenda is likely to be limited in the context of stretched resources and busy timetables. Furthermore, it is unlikely that steps to increase physical activity will reduce inequalities in childhood overweight/obesity, even if rolled out as progressive universal or targeted interventions. Additional efforts beyond this target are required if the unfair burden of overweight/obesity in less advantaged groups is to be alleviated. The methodological approach used in this study might be used to evaluate potential impacts of reaching the WHO dMVPA target in other nations, or to anticipate the consequences of other policies or targets being considered by policy makers before they are rolled out at scale. Future research might also examine how physical activity interventions might benefit inequalities in other childhood outcomes known to be associated with physical activity, including mental well-being,52 cognitive development,53,54 bone health,55 chronic disease and all-cause mortality.56,57 However, research seeking to inform policy decisions around the reduction of inequalities in overweight/obesity should examine policy scenarios that also focus on the upstream influences on children’s diets (such as taxes on high-sugar foods and diets in early years settings).
Funding
This work was supported by the England Department of Health and Social Care Children’s Policy Research Unit (grant number 10090001). This is an independent piece of research commissioned and funded by the Department of Health and Social Care. The views expressed are not necessarily those of the Department.
Research at the UCL Great Ormond Street Institute of Child Health and Great Ormond Street Hospital for Children receives a proportion of its funding from the Department of Health and Social Care’s National Institute for Health Research Biomedical Research Centres funding scheme. The Millennium Cohort Study is funded by grants to former and current directors of the study from the Economic and Social Research Council (Professor Heather Joshi, Professor Lucinda Platt and Professor Emla Fitzsimons) and a consortium of government funders. The study sponsors played no part in the design, data analysis and interpretation of this study, the writing of the manuscript or the decision to submit the paper for publication, and the authors’ work was independent of their funders.
Supplementary Material
Acknowledgements
We would like to thank all the Millennium Cohort families for their participation, and the director of the Millennium Cohort Study and colleagues in the management team at the Centre for Longitudinal Studies, UCL Institute of Education. We would also like to thank members of the Policy Research Unit in the Health of Children, Young People and Families: Terence Stephenson, Ruth Gilbert, Russell Viner, Miranda Wolpert, Ewan King, Steve Morris, Helen Roberts and Enver Solomon for their comments on the manuscript. We are also grateful to policy experts and parents and carers from the Families Research Advisory Group (hosted by the National Children’s Bureau) for their comments on the intervention scenarios. All MCS data used in this analysis are available from UK Data Service, University of Essex and University of Manchester.
Conflicts of interest: A.P., C.L. and S.H. report grants from England Department of Health and Social Care, during the conduct of the study. All other authors declare no conflicts of interest.
References
- 1.Lifestyles Statistics Team, Health and Social Care Information Centre. National Child Measurement Programme: England, 2014/15 School Year. London: Department of Health, 2015. [Google Scholar]
- 2. Wijnhoven TM, van Raaij JM, Spinelli A. et al. WHO European Childhood Obesity Surveillance Initiative: body mass index and level of overweight among 6–9-year-old children from school year 2007/2008 to school year 2009/2010. BMC Public Health 2014;14:806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ng M, Fleming T, Robinson M.. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reilly JJ, Kelly J.. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 2011;35:891–98. [DOI] [PubMed] [Google Scholar]
- 5. Griffiths LJ, Parsons TJ, Hill AJ.. Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes 2010;5:282–304. [DOI] [PubMed] [Google Scholar]
- 6. Ebbeling CB, Pawlak DB, Ludwig DS.. Childhood obesity: public-health crisis, common sense cure. Lancet 2002;360:473–82. [DOI] [PubMed] [Google Scholar]
- 7. Chung A, Backholer K, Wong E, Palermo C, Keating C, Peeters A.. Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obes Rev 2016;17:276–95. [DOI] [PubMed] [Google Scholar]
- 8.Cabinet Office, Department of Health, HM Treasury, Prime Minister’s Office. Childhood Obesity: A Plan for Action. London: HM Government, 2016. [Google Scholar]
- 9.Department of Health and Social Care: Global Public Health Directorate: Obesity FaN. In: Childhood Obesity: A Plan for Action. London: HM Government, 2018.
- 10.Nutrition, Physical Activity and Obesity Programme, WHO Regional Office for Europe’s Division of Non-Communicable Diseases and Promoting Health through the Life-Course. Factsheets on Health Enhancing Physical Activity in the 28 European Union Member States of the WHO European Region. Copenhagen: WHO Regional Office for Europe, 2015. [Google Scholar]
- 11.World Health Organization. Report on the Commission on Ending Childhood Obesity. Geneva: World Health Organization, 2016. [Google Scholar]
- 12. Griffiths LJ, Cortina-Borja M, Sera F. et al. How active are our children? Findings from the Millennium Cohort Study. BMJ Open 2013;3:e002893.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown HE, Atkin AJ, Panter J, Wong G, Chinapaw MJM, van Sluijs EMF.. Family-based interventions to increase physical activity in children: a systematic review, meta-analysis and realist synthesis. Obes Rev 2016;17:345–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Biddle SJH, Braithwaite R, Pearson N.. The effectiveness of interventions to increase physical activity among young girls: a meta-analysis. Prev Med 2014;62:119–31. [DOI] [PubMed] [Google Scholar]
- 15. Dellert JC, Johnson P.. Interventions with children and parents to improve physical activity and body mass index: a meta-analysis. Am J Health Promot 2014;28:259–67. [DOI] [PubMed] [Google Scholar]
- 16. Metcalf B, Henley W, Wilkin T.. Effectiveness of interventions on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ 2012;345:e5888. [DOI] [PubMed] [Google Scholar]
- 17. van Sluijs EMF, McMinn AM, Griffin SJ.. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ 2007;335:703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Global Recommendations on Physical Activity for Health. Global Strategy on Diet, Physical Activity and Health. Geneva: WHO, 2010. [PubMed] [Google Scholar]
- 19.Australian Government Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines. Canberra: AGDH, 2014. [Google Scholar]
- 20.US Department of Health and Human Services. Physical Activity Guidelines for Americans ODPHP Publication No U0036. Washington, DC: USDHHS, 2008.
- 21. Tremblay MS, Warburton DE, Janssen I. et al. New Canadian physical activity guidelines. Appl Physiol Nutr Metab 2011;36:36–46; 47–58. [DOI] [PubMed] [Google Scholar]
- 22.NHS England, Commisisoning Strategy, Equality and Health Inequalites Unit. Guidance for NHS Commissioners on Equality and Health Inequalities Legal Duties. London: NHS England, 2015. [Google Scholar]
- 23. Gordon RS. An operational classification of disease prevention. Public Health Rep 1983;98:107–09. [PMC free article] [PubMed] [Google Scholar]
- 24. Marmot M, Allen J, Goldblatt P. et al. Fair Society, Healthy Lives. The Marmot Review. London: University College London, 2010. [Google Scholar]
- 25. Connelly R, Platt L.. Cohort Profile: UK Millennium Cohort Study (MCS). Int J Epidemiol 2014;43:1719–25. [DOI] [PubMed] [Google Scholar]
- 26. Plewis I. Millennium Cohort Study: Technical Report on Sampling. 3rd edn London: Centre for Longitudinal Studies, 2004. [Google Scholar]
- 27. Hansen K. Millennium Cohort Study: A Guide to the Datasets. First, Second, Third, Fourth and Fifth Surveys. London: Centre for Longitudinal Studies, 2014. [Google Scholar]
- 28. Griffiths L, Rich C, Geraci M. et al. Technical Report on the Enhancement of Millennium Cohort Study Data with Accelerometer-derived Measures of Physical Activity and Sedentary Behaviour in Seven Year Olds. London: Centre for Longitudinal Studies, 2013. [Google Scholar]
- 29. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH.. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320: 01–06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Riani M, Atkinson A.. Robust diagnostic data analysis: transformations in regression. Technometrics 2000;42:384–94. [Google Scholar]
- 31. Robins JM, Hernán MÁ, Brumback B.. Marginal structural models and causal inference in epidemiology. Epidemiology 2000;11:550–60. [DOI] [PubMed] [Google Scholar]
- 32. Rich C, Geraci M, Griffiths L, Sera F, Dezateux C, Cortina-Borja M.. Quality control methods in accelerometer data processing: defining minimum wear time. PLoS One 2013;8:e67206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McCarthy HD, Cole TJ, Fry T, Jebb SA, Prentice AM.. Body fat reference curves for children. Int J Obes (Lond) 2006;30:598–602. [DOI] [PubMed] [Google Scholar]
- 34. El-Sayed AM, Scarborough P, Galea S.. Socioeconomic inequalities in childhood obesity in the United Kingdom: a systematic review of the literature. Obes Facts 2012;5:671–92. [DOI] [PubMed] [Google Scholar]
- 35. Goisis A, Sacker A, Kelly Y.. Why are poorer children at higher risk of obesity and overweight? A UK cohort study. Eur J Public Health 2016;26:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rougeaux E, Hope S, Law C, Pearce A.. Have health inequalities changed during childhood in the New Labour generation? Findings from the UK Millennium Cohort Study. BMJ Open 2017;7:e012868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Government Office for Science. Reducing Obesity: Future Choices. London: Department of Business, Universities and Skills, 2007. [Google Scholar]
- 38.National Institute for Health and Care Excellence. Preventing Excess Weight Gain. NICE Guideline [NG7]. London: NICE, 2015.
- 39.National Institute for Health and Care Excellence. Obesity Prevention. Clinical Guideline [CG43]. London: NICE, 2015. [PubMed]
- 40. Riddoch CJ, Mattocks C, Deere K. et al. Objective measurement of levels and patterns of physical activity. Arch Dis Child 2007;92:963–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kelly LA, Reilly JJ, Fisher A. et al. Effect of socioeconomic status on objectively measured physical activity. Arch Dis Child 2006;91:35–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pouliou T, Sera F, Griffiths L. et al. Environmental influences on children’s physical activity. J Epidemiol Community Health 2015;69:77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nevill AM, Duncan MJ, Lahart I, Sandercock G.. Modelling the association between weight status and social deprivation in English school children: Can physical activity and fitness affect the relationship? Ann Hum Biol 2016;43:497–504. [DOI] [PubMed] [Google Scholar]
- 44. Borodulin K, Zimmer C, Sippola R, Mäkinen TE, Laatikainen T, Prättälä R.. Health behaviours as mediating pathways between socioeconomic position and body mass index. Int J Behav Med 2012;19:14–22. [DOI] [PubMed] [Google Scholar]
- 45. Gearon E, Backholer K, Hodge A, Peeters A.. The mediating role of dietary factors and leisure time physical activity on socioeconomic inequalities in body mass index among Australian adults. BMC Public Health 2013;13:1214.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Farooq MA, Parkinson KN, Adamson AJ. et al. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br J Sports Med 2018;52:1002-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chittleborough CR, Mittinty MN, Lawlor DA, Lynch JW.. Effects of simulated interventions to improve school entry academic skills on socioeconomic inequalities in educational achievement. Child Dev 2014;85:2247–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: A meta-analysis. CMAJ 2009;180:719–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Johns DJ, Hartmann-Boyce J, Jebb SA, Aveyard P.. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J Acad Nutr Diet 2014;114:1557–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Waters E, Silva SA, Hall B, Brown T, Campbell K, Gao Y.. Interventions for preventing obesity in children (review). Cochrane Database Syst Rev 2012;12:CD001871. [Google Scholar]
- 51.Public Health England. Child Obesity International Comparisons Data Factsheet. London: PHE Publications, 2016. [Google Scholar]
- 52. Spruit A, Assink M, van Vugt E, van der Put C, Stams GJ.. The effects of physical activity interventions on psychosocial outcomes in adolescents: a meta-analytic review. Clin Psychol Rev 2016;45:56–71. [DOI] [PubMed] [Google Scholar]
- 53. Jackson WM, Davis N, Sands SA, Whittington RA, Sun LS.. Physical activity and cognitive development: a meta-analysis. J Neurosurg Anesthesiol 2016;28:373–80. [DOI] [PubMed] [Google Scholar]
- 54. Tandon PS, Tovar A, Jayasuriya AT. et al. The relationship between physical activity and diet and young children’s cognitive development: a systematic review. Prev Med Rep 2016;3:379–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Tan VP, Macdonald HM, Kim S. et al. Influence of physical activity on bone strength in children and adolescents: a systematic review and narrative synthesis. J Bone Miner Res 2014;29:2161–81. [DOI] [PubMed] [Google Scholar]
- 56. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT.. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Marcus BH, Williams DM, Dubbert PM. et al. Physical Activity Intervention Studies. What We Know and What We Need to Know: A Scientific Statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation 2006;114:2739–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.